Abstract
Background
Goals of care (GOC) conversations in the emergency department (ED) are often a brief discussion of code status rather than a patient-oriented dialogue. We aimed to develop a guide to facilitate conversations between ED clinicians and patients to elicit patient values and establish goals for end-of-life care, while maintaining ED efficiency. Paths of ED Care, a conversation guide, is the product of this work.
Design
A multidisciplinary/multispecialty group used recommended practices to adapt a GOC conversation guide for ED patients. ED clinicians used the guide and provided feedback on content, design, and usability. Patient-clinician interactions were recorded for discussion analysis, and both were surveyed to inform iterative refinement. A series of discussions with patient representatives, multidisciplinary clinicians, bioethicists, and health care designers yielded feedback. We used a process similar to the International Patient Decision Aid Standards and provide comparison to these.
Results
A conversation guide, eight pages with each page 6 by 6 inches in dimension, uses patient-oriented prompts and includes seven sections: 1) evaluation of patient/family understanding of disease, 2) explanation of possible trajectories, 3) introduction to different pathways of care, 4) explanation of pathways, 5) assessment of understanding and concerns, 6) code status, and 7) personalized summary.
Limitations
Recruitment of sufficient number of patients/providers to the project was the primary limitation. Methods are limited to qualitative analysis of guide creation and feasibility without quantitative analysis.
Conclusions
Paths of ED Care is a guide to facilitate patient-centered shared decision making for ED patients, families, and clinicians regarding GOC. This may ensure care concordant with patients’ values and preferences. Use of the guide was well-received and facilitated meaningful conversations between patients and providers.
Keywords: conversation guide, emergency medicine, goals of care
Introduction
We face an aging population, increased longevity with chronic illness, and more patients visiting emergency departments (EDs) at end-of-life—potentially receiving unwanted care. 1 Intensity of care at end-of-life does not always improve quality of life or quality of death. 2
In Dying in America, the Institute of Medicine analyzes the gaps in care for patients near end-of-life. Barriers include personal/cultural variability in approach to dying, few palliative and end-of-life care specialists, and a rising elderly population within a health care culture that does not readily engage in discussions on death/dying. 3 With more older Americans, 4 clinicians will be increasingly challenged to bridge end-of-life care with patient/family values and communicate to prioritize alignment.
Barriers to obtaining patient-centered goals of care (GOC) in the ED has been previously evaluated,5,6 and publications have called for focused research in this area within emergency medicine (EM).7–9 The 2016 Society of Academic Emergency Medicine Consensus Conference focused on shared decision making (SDM), including at end-of-life. Early palliative team involvement improves patient care, although palliative consultation from the ED is infrequent. 7 SDM has been shown to be a feasible endeavor in the ED. 10
With a common commitment to treat patients with dignity and respect at the end-of-life, we engaged patients, caregivers, emergency clinicians, geriatricians, intensivists, palliative care specialists, bioethicists, and health care designers to produce a conversation guide, Paths of ED Care, to facilitate meaningful GOC discussions and SDM in the ED. We aimed to develop a guide that would elicit what is important to the patients/families at end-of-life, aligning care and values.
Methods
Multidisciplinary conversations established the goal of the conversation guide: ensuring concordance of patient wishes and treatment with mutual understanding of the current situation of illness. The study was conducted at Mayo Clinic St Marys Hospital, a quaternary care hospital with 77,000 ED visits annually. Patients and providers were recruited as a dyad. Early in the process only ED clinicians who volunteered to participate were included, but this was later broadened to include all ED clinicians. Inclusion criteria for patient/family were the following: presentation to the ED, patients at risk for critical illness as determined by Elders Risk Assessment (ERA) Score 16+ (Supplementary Figure 1), 11 age greater than 60 years, two or more hospitalizations in the last 6 months, ability to provide informed consent, medical stability, and ability to participate without delaying care. During the latter part of the trial we expanded criteria to include ED clinician gestalt, rather than ERA score, with the goal of increasing recruitment. This change allowed us to recruit patients without the burden of accessing the ERA score within the medical record, a step that was perceived to be a barrier to recruitment. ERA scores were initially collected as part of eligibility screening, and were ultimately gathered for all patients, including those who were recruited after this criterion was eliminated. Exclusion criteria were the following: Glasgow Coma Scale score <15, altered mental status, incarcerated/police custody, or communication barriers that precluded guide use. Signed informed consent was required for both patient and clinician participants per Institutional Review Board of Mayo Clinic in Rochester, Minnesota.
The primary designer observed the milieu of the ED in order to understand the context in which the guide would be used. These observations were shared with the team developing the conversation guide. Roundtable discussions and iterative revision process using team feedback resulted in a pilot version.
Emergency medicine physicians, nurse practitioners, and physician assistants (“ED clinicians”) were asked to use the guide. Trained research coordinators obtained consent, recorded the encounter, and took notes using an observation guide. We used a predefined observation grid to identify patterns of patient-clinician conversations, nonverbal behaviors, and attitudes, incorporating results into subsequent iterations. A brief structured interview with the patient/family and clinician included targeted questions for each group.
We performed iterative revisions and feedback cycles (Figure 1)12–14 until we had a guide that was discrete, intuitive, required minimal training, met patient/caregiver and clinician needs, and facilitated continuity with downstream specialists.
Figure 1.
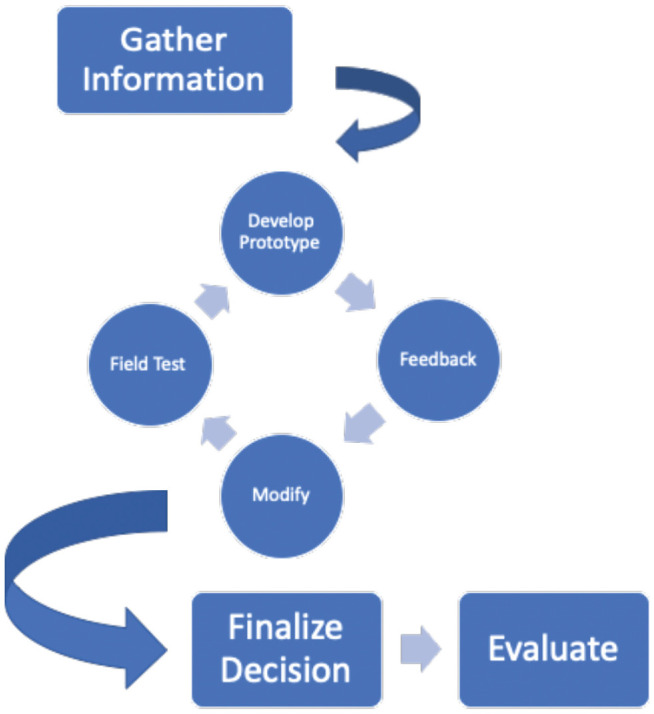
Iterative refinement process for creation of the conversation guide.
After developing our conversation guide, we did a retrospective comparison of our process compared to International Patient Decision Aid Standards (IPDAS) criteria.15,16
Results
We recruited 25 patients, and 10 unique providers participated in the study. Care providers included EM-boarded physicians, EM residents, nurse practitioners, and physician assistants. Feedback was not segmented by role. The median ERA score was 15.5 (mean 13.7; n = 24, missing = 1). The most common chief complaint was shortness of breath. Other common complaints included weakness/fatigue, abdominal pain, and gastrointestinal bleeding. Enrollee demographics were not collected. We initially created an electronic guide. After initial experimentation, we agreed that transitioning to a single-use paper form the clinician brings to the bedside would be more beneficial. Feedback on this iteration included adding graphic representation, inclusion of patient values by naming different potential concerns, and conversion to paper to improve accessibility and allow the patient/family to keep the guide for reference.
Prior to implementation of the guide, observations of overall ED workflow revealed a common theme of fragmentation in patient and digital interactions. Activity was near-constant with frequent interruption. Clinicians had limited time to spend on any single case, switched modes often between patient interactions, medical record use, forming hypotheses, and documentation. The information-scape was fragmented—code status, advanced directives, alternate decision makers, advance care planning, and ERA were scattered across modules.
Multispecialty stakeholder discussions, informed by observations of the ED milieu and local patient flow, resulted in a vision of a guide to help clinicians co-create a care plan with patients that might 1) centralize information related to advance care planning, 2) improve ease of obtaining GOC, 3) provide a way to initiate GOC conversations, 4) help clinicians navigate deeper discussion of patients’ priorities and values, 5) provide a location to indicate patient preferences for downstream clinicians, and 6) identify patient resource needs to transition to discharge.
As part of our development process, we evaluated existing resources and their relative applicability to our setting. The Serious Illness Conversation Guide (SICG) 17 is a high-quality resource, and we began with modifications to the SICG to meet ED needs.
The revised eight-page prototype, Paths of ED Care, included seven sections: 1) evaluation of patient and family understanding of disease, 2) presentation of care team view (possible trajectories of disease), 3) introduction of different pathways of care, 4) care pathway explanation, 5) assessment of patient/family understanding and concerns, 6) discussion of code status, and 7) personalized summary. Patient-oriented prompts facilitated dialogue between patients and clinicians. The patient choice to pursue either relief of symptoms or repair (curative/procedural interventions) was introduced, based on feedback from our design team patient representative. A frank discussion on code status and a form to document discussion highlights to encourage sharing with loved ones and downstream care teams concluded the guide.
The third version included new images tying together the pathway theme with GOC concepts. A splitting walkway introduced the concept of choice and a fallen tree represented an impetus to discuss code status. Hand-written text was converted to typeface. Feedback on this prototype centered on nonintuitive flow of the conversation, and a near-universal patient sentiment of discomfort with some imagery. Clinicians and patients appreciated the content, and there were no concerns regarding time to use.
The final prototype, an eight-page, 6 by 6 inch paper guide, was completed in January 2020 (Figure 2). It included reversion to a typical page flow, removal of the fallen tree, and the blank form. Prior versions are available in the Supplementary Figure 2.
Figure 2.
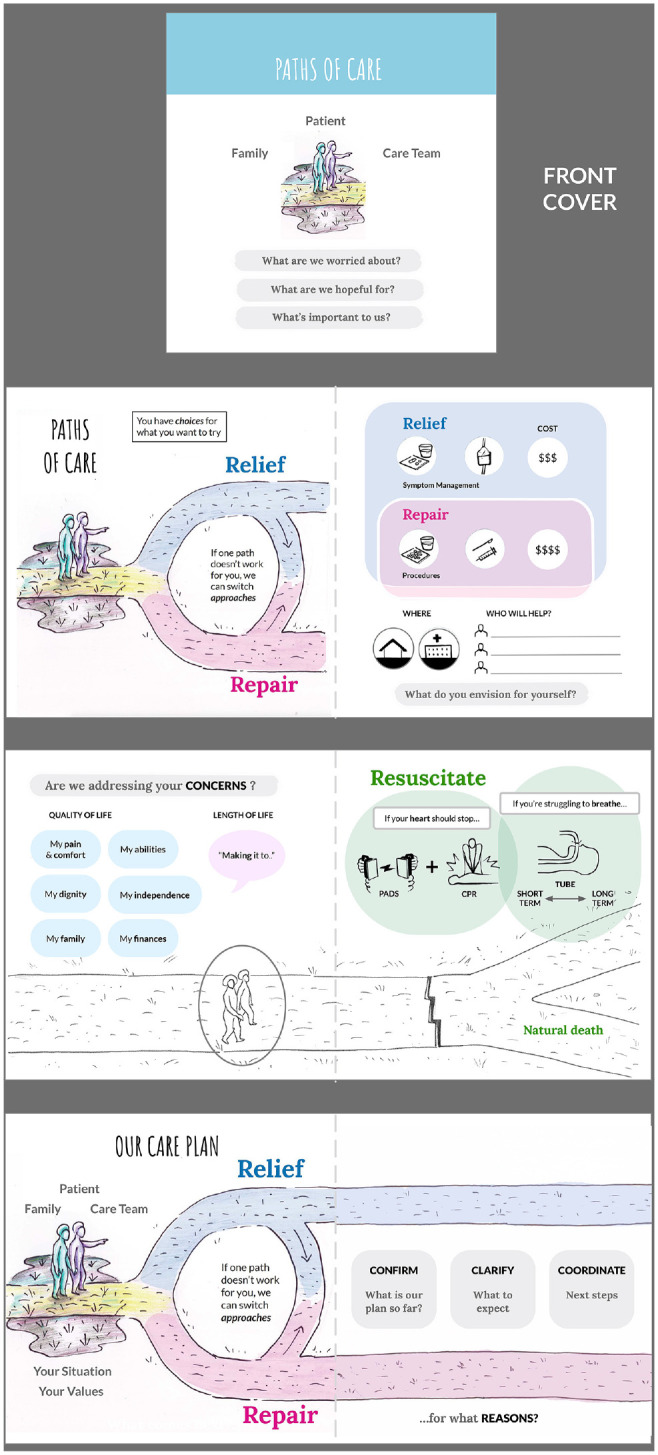
Paths of ED care decision aid.
Feedback on our conversation guide indicated surprise and appreciation for how brief, yet in-depth, conversations were. Patients appreciated having a meaningful conversation with their clinician, and felt they were able to spend more time with the physician than usual. No clinicians indicated that the conversation took excessive time to use. The mean time to complete the conversation was 9.7 minutes (SD 5.1 minutes). An assessment of each component of the IPDAS15,16 is available in Table 1.
Table 1.
Comparison of Utilized Design Process with International Patient Decision Aid Standards
| Part 1: Content | |
| Providing information about options in sufficient detail for decision making | |
| Describe the health condition | This DA applies to multiple different health conditions that present to the ED when decisions about goals of care need to be made. |
| List the options | Options are presented as two paths with equipoise. Also, the option of switching paths is presented. |
| List the option of doing nothing | We did not present an option of “doing nothing” because we believe that the less aggressive path still involves actively caring for that patient and “doing nothing” can feel like abandonment for the patients. |
| Describe the natural course without options | Yes, we describe the “relief” path, allowing natural course. |
| Describe procedures | Yes, although are nonspecific because this DA applies to different health conditions. Some illnesses and patients might be offered surgery, critical care admission, hospitalization, and so on, depending on their illness. |
| Describe positive features (benefits) | The DA includes prompts on what are the things important to the specific patient, such as pain control, independence, length of life. |
| Describe negative features of options (harms/side effects/disadvantages) | Negative features are not clearly stated. |
| Include chances of positive/negative outcomes | Includes the option of allowing natural death versus going through CPR and intubation. |
| Presenting probabilities of outcomes in an unbiased and understandable way | |
| Use event rates specifying the population and time period | Timing of death is very different for each individual, so event rates and time periods are not included. |
| Compare outcome probabilities using the same denominator, time period, scale | |
| Describe uncertainty around probabilities | |
| Use visual diagrams | |
| Use multiple methods to view probability (words, numbers, diagrams) | |
| Allow patient to select a way of viewing probabilities (words, numbers, diagrams) | |
| Allow patient to view probabilities based on their own situation (i.e., age) | |
| Place problem in context of other events | |
| Use both positive and negative frames (i.e., showing both survival and death rates) | |
| Include methods for clarifying and expressing patient values | |
| Describe the procedure and outcomes to help patients imagine what is like to experience their physical, emotional, social effects | Yes. We specifically focus on addressing patient’s concerns and invite to speak of personal goals. |
| Ask patient to consider which positive and negative features matter most | Yes |
| Suggest ways for patient to share what matters most with others | Yes |
| Include structured guidance in deliberation and communication | |
| Provide steps to make a decision | Yes, it presents binary options for relief versus repair and gives prompts to encourage thinking on what are each person values. |
| Suggest ways to talk about the decision with a health professional | Yes, the DA has the terms “our care plan” and specifically mentions the patient, family, and care team. |
| Include tools to discuss options with others | Yes, the DA is given to the patients to take home and discuss with others if they are not ready to make a decision. |
| Part 2: Development Process: Does the decision aid . . . | |
| Present information in a balanced manner | |
| Able to compare positive/negative features of options | Yes |
| Shows negative/positive features w/equal details (fonts, order, display of stats) | Yes |
| Have a systematic development process | |
| Include developers’ credentials/qualifications | Yes, we included patients and their families, clinicians (emergency physicians, nurse practitioners, physician assistants, internal medicine and palliative medicine specialists), nurses, communication specialists, designers, among others. |
| Finds out what users (patients, practitioners) need to discuss options | Yes, the DA is focused around the patient-provider conversation. Feedback from all stakeholders was utilized during the development process. |
| Has peer review by patient/professional experts not involved in development and field testing | This portion of the process is ongoing. The finalized guide is being used in situ with additional feedback being collected. |
| Is field tested with users (patients facing the decision, practitioners presenting options) | Yes, during the development process the different versions of the DA were presented to patients and providers. This DA has been going several iterations of field testing. |
| The field test with users show the patient decision aid is acceptable, balanced for undecided patients, understood by those with limited reading skills | Yes, clinical trial is ongoing. We have video and audio recording of the guide while being used, and specific feedback is requested in writing from both patients and providers. |
| Uses up-to-date scientific evidence that is cited in a reference section or technical document | |
| Provides references to evidence used | Several references were used to create the guide; however, these references are not included in the DA. |
| Report steps to find, appraise, summarize evidence | Not included in the DA. |
| Report date of last update | Not included in the DA. |
| Report how often patient decision aid is updated | Not included in the DA. |
| Describe the quality of scientific evidence | Not included in the DA. |
| Uses evidence from studies of patients similar to those of target audience | No. As discussed previously, this DA is to generate a conversation around the goals of care and includes very broad illnesses. |
| Disclose conflict of interest | |
| Report source funding to develop and distribute the patient decision aid | Not included in the DA. |
| Report whether authors or their affiliations stand to gain or lose by choices patients make after using the decision aid | Not included in the DA. |
| Use plain language | |
| Is written at a level that can be understood by the majority of patients in the target group | Yes |
| Is written at a grade 8 equivalent level or less according to readability score (SMOG or FRY) | Yes. Using SMOG criteria modified for short passages the guide is written at a grade 7 level. |
| Provides ways to help patients understand information other than reading (audio, video, in-person discussion) | Yes, it has drawings and its meant to be discussed in person. |
| Internet based | Does not apply |
| Stories used | Does not apply |
| Part 3: Effectiveness: Does the decision aid ensure decision making is informed and values based? | |
| Decision processes leading to decision quality | |
| Recognize a decision needs to be made | Yes |
| Know options and their features | Yes |
| Understands that values affect decision | Yes (this is a strength in this DA) |
| Be clear about option features that matter most | Yes |
| Discuss values with their practitioner | Yes |
| Become involved in preferred ways | Not specifically addressed |
| Decision quality | |
| Improves the match between the chosen option and the features that matter most to the informed patient | Yes |
CPR, cardiopulmonary resuscitation; DA, decision aid.
Discussion
This conversation guide is novel and is intended for ED use. This setting requires efficient decisions about GOC. The fragmented environment, frequent interruptions, and lack of care continuity have created barriers to having patient-centered GOC conversations.
Paths of ED Care does not include instructions and is designed with novice users in mind. ED clinicians receive minimal training to discuss patient preferences regarding end-of-life 18 yet often need to urgently engage patients in these decisions. Utilization of this guide may bridge the confidence and skills gap to enable more clinicians to provide care that is concordant with patient values.
Our conversation guide was developed with SDM in mind, although the form evolved throughout the process away from more traditional SDM tools. Use of the IPDAS criteria as comparison illustrates the similarities between traditional SDM guide and our conversation guide. Of the 50 items on the checklist, our conversation guide fulfills 30, and of the 20 that were not met, 9 were prompts to include probabilities of different events, which is not possible to do with the broad context of GOC at end-of-life (Table 1).
Limitations
The primary challenge in this study was enrollment. We were initially required by our institutional review board (IRB) to involve only clinicians who were involved in ED GOC initiatives, resulting in a potentially biased sample, and limiting the patients who were eligible due to the dyad recruitment method. Broadening the clinicians who were able to recruit increased the pool of potential patients. We also adjusted the inclusion criteria from objective criteria (ERA score) to gestalt during the study, which may affect the results. The first field-testing period overlapped with implementation of a new electronic medical record, creating systems, and technical and human factors challenges. These barriers prompted us to reduce the number of participants per iteration cycle. After a few months of recruitment, we were granted permission by the IRB to enroll all ED clinicians in the study, and they were consented at a scheduled department meeting. The changes in our recruitment criteria lowered the average ERA score. By the original criteria the minimum score would be 16, and the mean was 15.5. There are many ways to assess if a patient is appropriate for GOC conversations, and we do not think that moving away from the initial inclusion criteria by ERA score compromises the value of the study and the applicability of the conversation to many individuals.
The choice between relief and repair may represent a less nuanced approach to the conversation and does not account for situations in which the patient may want to pursue a degree of repair within the broader context of seeking symptomatic relief.
We did not utilize a formal checklist for decision aid development, such as the IPDAS checklist, which would have strengthened our methodology, 16 though most of the criteria were fulfilled.
Conclusion
Using iterative development, we created a GOC conversation guide for use in the ED. We found that the approach was well received and the time taken to have conversations were not a burden to ED clinicians. Feedback on the quality of the tool improved throughout the phases of development, and we believe the current iteration is feasible to deploy in the ED setting. Our next study phase will focus on feasibility of implementing this product within our department and, ultimately, externally. This will serve as additional peer review of the guide and as an opportunity to learn from the experiences with different settings, clinicians, and patients.
Supplemental Material
Supplemental material, sj-docx-1-mpp-10.1177_23814683211058082 for Paths of Emergency Department Care: Development of a Decision Aid to Facilitate Shared Decision Making in Goals of Care Discussions in the Acute Setting by Laura E. Walker, M. Fernanda Bellolio, Claudia C. Dobler, Ian G. Hargraves, Robert J. Pignolo, Kevin Shaw, Jacob J. Strand, Bjorg Thorsteinsdottir, Michael E. Wilson and Erik P. Hess in MDM Policy & Practice
Supplemental material, sj-png-2-mpp-10.1177_23814683211058082 for Paths of Emergency Department Care: Development of a Decision Aid to Facilitate Shared Decision Making in Goals of Care Discussions in the Acute Setting by Laura E. Walker, M. Fernanda Bellolio, Claudia C. Dobler, Ian G. Hargraves, Robert J. Pignolo, Kevin Shaw, Jacob J. Strand, Bjorg Thorsteinsdottir, Michael E. Wilson and Erik P. Hess in MDM Policy & Practice
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Financial support for this study was provided entirely by a grant from the Emergency Medicine Foundation, a philanthropic foundation. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Authors’ Note: This work was performed in the Emergency Department of Mayo Clinic in Rochester, Minnesota, with support from the Knowledge and Evaluation Research Unit at Mayo Clinic. This study was previously presented at the American College of Emergency Medicine Scientific Assembly, 2018.
ORCID iDs: Laura E Walker  https://orcid.org/0000-0002-1127-327X
https://orcid.org/0000-0002-1127-327X
M Fernanda Bellolio  https://orcid.org/0000-0002-1632-4750
https://orcid.org/0000-0002-1632-4750
Bjorg Thorsteinsdottir  https://orcid.org/0000-0002-4397-728X
https://orcid.org/0000-0002-4397-728X
Supplemental Material: Supplemental material for this article is available on the Medical Decision Making Policy & Practice website at https://journals.sagepub.com/home/mpp.
Contributor Information
Laura E. Walker, Department of Emergency Medicine.
M. Fernanda Bellolio, Department of Emergency Medicine.
Claudia C. Dobler, Mayo Clinic, Rochester, Minnesota; Institute for Evidence-Based Healthcare, Bond University, Gold Coast, Australia
Ian G. Hargraves, Knowledge and Evaluation Research Unit
Robert J. Pignolo, Division of Geriatric and Gerontologic Medicine
Kevin Shaw, Knowledge and Evaluation Research Unit.
Jacob J. Strand, Department of General Internal Medicine Center for Palliative Medicine
Bjorg Thorsteinsdottir, Department of Community Internal Medicine, Program in Biomedical Ethics.
Michael E. Wilson, Department of Pulmonary and Critical Care Medicine
Erik P. Hess, Department of Emergency Medicine, Vanderbilt University Medical Center, Nashville, Tennessee
References
- 1. A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators. JAMA. 1995;274(20):1591–8. [PubMed] [Google Scholar]
- 2. Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480–8. doi: 10.1001/archinternmed.2008.587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Institute of Medicine; Committee on Approaching Death: Addressing Key End-of-life Issues. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Institute of Medicine; 2015. [Google Scholar]
- 4. Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States. US Census Bureau; 2014. p 25–1140. [Google Scholar]
- 5. Grudzen CR, Richardson LD, Hopper SS, Ortiz JM, Whang C, Morrison RS. Does palliative care have a future in the emergency department? Discussions with attending emergency physicians. J Pain Symptom Manage. 2012;43(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lamba S, Nagurka R, Zielinski A, Scott SR. Palliative care provision in the emergency department: barriers reported by emergency physicians. J Palliat Med. 2013;16(2):143–7. [DOI] [PubMed] [Google Scholar]
- 7. George NR, Kryworuchko J, Hunold KM, et al. Shared decision making to support the provision of palliative and end-of-life care in the emergency department: a consensus and research agenda. Acad Emerg Med. 2016; 23(12):1394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chan GK. End-of-life and palliative care in the emergency department: a call for research, education, policy and improved practice in this frontier area. J Emerg Nurs. 2006;32(1):101–3. [DOI] [PubMed] [Google Scholar]
- 9. Quest TE, Asplin BR, Cairns CB, Hwang U, Pines JM. Research priorities for palliative and end-of-life care in the emergency setting. Acad Emerg Med. 2011;18(6):e70–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Flynn D, Knoedler MA, Hess EP, et al. Engaging patients in health care decision in the emergency department through shared decision-making: a systematic review. Acad Emerg Med. 2012;19(8):959–67. [DOI] [PubMed] [Google Scholar]
- 11. Crane SJ, Tung EE, Hanson GJ, et al. Use of an electronic administrative database to identify older community dwelling adults at high-risk for hospitalization or emergency department visits: the Elders Risk Assessment Index. BMC Health Serv Res. 2010;10(1):338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Breslin M, Mullan RJ, Montori V. The design of a decision aid about diabetes medications for use during the consultation with patients with type 2 diabetes. Patient Educ Couns. 2008;73(3):465–72. [DOI] [PubMed] [Google Scholar]
- 13. Coylewrite M, Shepel K, LcBlanc A, et al. Shared decision making in patients with stable coronary artery disease: PCI choice. PLoS One. 2012;7(11):e49827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zeballos-Palacios CL, Hargraves IG, Noseworthy PA, et al. Developing a conversation aid to support shared decision making: reflections on anticoagulation choice. Mayo Clin Proc. 2019;94(4):686–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Holmes-Rovner M. International Patient Decision Aid Standards (IPDAS): beyond decision aids to usual design of patient education materials. Health Expect. 2007;10(2):103–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. International Patient Decision Aid Standards (IPDAS) Collaboration. IPDAS 2005: criteria for judging the quality patient decision aids [cited June 27, 2021]. Available from: http://www.ipdas.ohri.ca/IPDAS_checklist.pdf
- 17. Ariadne Labs. Serious illness conversation guide and tools [cited January 31, 2020]. Available from: https://www.ariadnelabs.org/wp-content/uploads/sites/2/2018/04/Serious-Illness-Conversation-Guide
- 18. Kraus CK, Greenberg MR, Ray DE, Dy SM. Palliative care education in emergency medicine residency training: a survey of program directors, associate program directors, and assistant program directors. J Pain Symptom Manage. 2016;51(5):898–906. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-mpp-10.1177_23814683211058082 for Paths of Emergency Department Care: Development of a Decision Aid to Facilitate Shared Decision Making in Goals of Care Discussions in the Acute Setting by Laura E. Walker, M. Fernanda Bellolio, Claudia C. Dobler, Ian G. Hargraves, Robert J. Pignolo, Kevin Shaw, Jacob J. Strand, Bjorg Thorsteinsdottir, Michael E. Wilson and Erik P. Hess in MDM Policy & Practice
Supplemental material, sj-png-2-mpp-10.1177_23814683211058082 for Paths of Emergency Department Care: Development of a Decision Aid to Facilitate Shared Decision Making in Goals of Care Discussions in the Acute Setting by Laura E. Walker, M. Fernanda Bellolio, Claudia C. Dobler, Ian G. Hargraves, Robert J. Pignolo, Kevin Shaw, Jacob J. Strand, Bjorg Thorsteinsdottir, Michael E. Wilson and Erik P. Hess in MDM Policy & Practice


