Introduction
Leukemia cutis is defined as the cutaneous infiltration of neoplastic leukocytes in patients with underlying hematologic malignancies and has a heterogeneous clinical presentation.1 Most commonly, leukemia cutis presents with single or multiple erythematous papulonodules. Herein, we describe a unique clinical presentation of leukemia cutis in a patient with relapsed T-cell acute lymphoblastic leukemia (T-ALL). As the diagnosis of leukemia cutis has important treatment and prognostic implications, prompt clinical recognition and histopathologic confirmation is imperative.
Case report
A 59-year-old woman with previously diagnosed T-ALL presented to her outpatient hematologist with fatigue and a new rash initially involving her face. Blood work revealed relapsed T-ALL, and she was admitted for inpatient salvage chemotherapy with nelarabine. Over the next 2 weeks of admission, the eruption subsequently progressed to involve her trunk, upper extremities, and lower extremities. The patient denied any associated symptoms, recent travel, hiking or known tick bites, new medications, or herbal supplements.
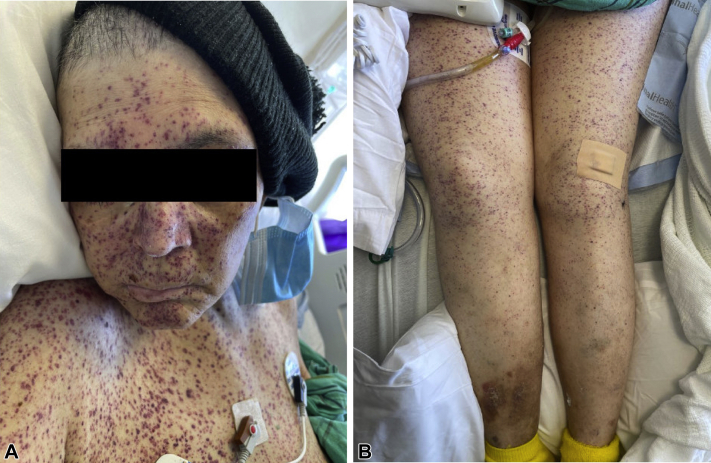
On physical examination, there were innumerable widespread nonblanching, red-to-violaceous, round macules and thin papules that involved the head and neck, trunk, upper extremities, lower extremities, palms, and soles (Fig 1, A and B). We performed a punch biopsy of a red papule on the left thigh for hematoxylin and eosin staining, which revealed a superficial perivascular infiltrate comprised of atypical lymphocytes with enlarged hyperchromatic nuclei, irregular contours, and scant amounts of cytoplasm, consistent with leukemia cutis (Fig 2, A and B). Immunoperoxidase studies revealed atypical lymphocytes that expressed CD3 with a predominance of CD8 expression over CD4. The cells also expressed CD5 and CD43, with a subset of cells also reactive for CD45RO. The neoplastic cells in peripheral blood specimens demonstrated similar immunophenotype staining. A Ki-67 assessment demonstrated a high proliferative index of 80%. Bacterial, acid-fast bacilli, and fungal tissue cultures were negative. Human T-lymphotropic virus type I serology was also negative.
Fig 1.
Diffuse red-to-violaceous macules and thin papules involving (A) the face and trunk and (B) bilateral lower extremities.
Fig 2.
Superficial perivascular infiltrate comprised of atypical lymphocytes with enlarged hyperchromatic nuclei with irregular contours and scant amount of cytoplasm. (A and B, Hematoxylin-eosin stain; original magnifications: A, ×4; B, ×40.)
Discussion
Acute lymphoblastic leukemia (ALL) is defined as the malignant transformation and clonal proliferation of lymphoid progenitor cells, either T-ALL or B-cell acute lymphoblastic leukemia (B-ALL). ALL is most commonly a pediatric disease; however, it does account for 20% of leukemia in adults.2 ALL is rare and has an overall incidence of 17.3 per 1 million in the United States, with T-cell lymphoblastic leukemia comprising 15% of these cases.3 T-ALL is associated with an older age of onset, male sex predominance, and poor outcomes compared to the B-ALL subtype.2 Chemotherapy is the standard of care for adult patients with T-ALL, and studies have demonstrated a 5-year overall survival rate of approximately 50%. Relapse is rare, occurring in less than 7% of cases, but is associated with worsened outcomes.4
Leukemia cutis may present in up to 20% of patients with chronic lymphocytic leukemia and up to 70% of patients with mature T-cell leukemia. However, leukemia cutis rarely presents in patients with precursor B- or T-cell lymphoblastic leukemia and may be seen in only 1% of cases.1 Within ALL, B-ALL also has a higher likelihood of presenting with cutaneous manifestations compared to T-ALL.5 Regardless, leukemia cutis is considered a poor prognostic factor, although specific prognostic data on leukemia cutis in patients with T-ALL are unavailable, likely due to the rarity of these cases. In a review of patients with hematologic malignancies, it was shown that 88% of patients with leukemia cutis died within 1 year of diagnosis.6
The clinical presentations of leukemia cutis are heterogeneous, with erythematous papules or nodules being the most common. Other presentations include plaques, macules, ecchymoses, purpuric lesions, noduloulcerative lesions, and erythroderma.6,7 In ALL specifically, most patients present with single or multiple papules, nodules, and plaques. The most common sites of involvement are the face, head, neck, and trunk.6 Of note, cutaneous manifestations of leukemia may include leukemia cutis with the direct infiltration of neoplastic cells or with nonspecific skin findings, such as petechiae and purpura secondary to underlying thrombocytopenia or coagulopathies.7 Regardless, leukemia cutis should be considered a separate entity from these nonspecific cutaneous manifestations, which may occur in 30% to 40% of patients with leukemia. Importantly, a widespread petechiae-like eruption secondary to leukemia cutis is rarely described in the literature.
A few cases of leukemia cutis in patients with ALL presenting as red-to-violaceous macules and thin papules have been reported. One case describes a 19-year-old male presenting with a widespread purpuric eruption on the face, neck, torso, and upper extremities. Histology revealed a dense perivascular infiltration of abnormal lymphocytes in the papillary dermis and mid dermis. The abnormal cells had scant cytoplasm with hyperchromatic nuclei, and more than 50% stained positively for surface markers of T cells. Histology and blood work confirmed a diagnosis of ALL presenting with leukemia cutis.8 An additional case describes a 3-day-old male newborn who presented with multiple violaceous, nonblanching macules and a few papules on the upper trunk and face. The presentation was characterized as “blueberry muffin” lesions. A skin biopsy revealed dermal lymphoblastic infiltrates, which confirmed the diagnosis of neonatal ALL.9 Additional unique presentations of leukemia cutis associated with T-ALL have been reported, including a case of erythematous papules and annular plaques, some with associated petechiae.10 A widespread petechiae-like eruption in a patient with T-ALL, as seen in our patient, has not yet been reported in the literature.
Leukemia cutis may present with a wide variety of clinical presentations and should always remain a consideration for patients with underlying hematologic malignancies. Herein, we present a rare cutaneous manifestation of leukemia cutis in a patient with relapsed T-ALL, characterized by widespread red-to-violaceous macules and thin papules. Unfortunately, our patient succumbed to her disease shortly after hospitalization. Despite the rarity and variable presentation of leukemia cutis, this diagnosis should remain on the differential for patients with T-ALL, as early identification may allow for more rapid initiation of appropriate treatment.
Conflicts of interest
None disclosed.
Footnotes
Authors Nohria and Criscito are cofirst authors.
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Cho-Vega J.H., Medeiros L.J., Prieto V.G., Vega F. Leukemia cutis. Am J Clin Pathol. 2008;129(1):130–142. doi: 10.1309/WYACYWF6NGM3WBRT. [DOI] [PubMed] [Google Scholar]
- 2.Rafei H., Kantarjian H.M., Jabbour E.J. Recent advances in the treatment of acute lymphoblastic leukemia. Leuk Lymphoma. 2019;60(11):2606–2621. doi: 10.1080/10428194.2019.1605071. [DOI] [PubMed] [Google Scholar]
- 3.Ferrando A.A., Neuberg D.S., Staunton J., et al. Gene expression signatures define novel oncogenic pathways in T cell acute lymphoblastic leukemia. Cancer Cell. 2002;1(1):75–87. doi: 10.1016/S1535-6108(02)00018-1. [DOI] [PubMed] [Google Scholar]
- 4.Marks D.I., Rowntree C. Management of adults with T-cell lymphoblastic leukemia. Blood. 2017;129(9):1134–1142. doi: 10.1182/BLOOD-2016-07-692608. [DOI] [PubMed] [Google Scholar]
- 5.Sander C.A., Medeiros L.J., Abruzzo L.V., Horak I.D., Jaffe E.S. Lymphoblastic lymphoma presenting in cutaneous sites: a clinicopathologic analysis of six cases. J Am Acad Dermatol. 1991;25(6):1023–1031. doi: 10.1016/0190-9622(91)70302-I. [DOI] [PubMed] [Google Scholar]
- 6.Su W.P. Clinical, histopathologic, and immunohistochemical correlations in leukemia cutis. Semin Dermatol. 1994;13(3):223–230. [PubMed] [Google Scholar]
- 7.Rao A.G., Danturty I. Leukemia cutis. Indian J Dermatol. 2012;57(6):504. doi: 10.4103/0019-5154.103086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chao S.C., Lee J.Y., Tsao C.J. Leukemia cutis in acute lymphocytic leukemia masquerading as viral exanthem. J Dermatol. 1999;26(4):216–219. doi: 10.1111/J.1346-8138.1999.TB03459.X. [DOI] [PubMed] [Google Scholar]
- 9.Schlegel S., Hamm H., Reichel A., et al. Neonatal acute lymphoblastic leukemia with t(9;11) translocation presenting as blueberry muffin baby: successful treatment by ALL-BFM induction therapy, allogeneic stem cell transplantation from an unrelated donor, and PCR-MRD-guided post-transplant follow-up. Am J Case Rep. 2020;21:e927153. doi: 10.12659/AJCR.927153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mansoori P., Taheri A., O'Neill S.S., Sangueza O.P. T-lymphoblastic leukemia/lymphoma with annular skin rash and epidermotropism. Am J Dermatopathol. 2018;40(9):676–678. doi: 10.1097/DAD.0000000000001113. [DOI] [PubMed] [Google Scholar]