Abstract
COVID-19 emerged in 2019 and has since killed more than two and a half million people worldwide. Several studies have investigated the role of COVID-19 on the prevalence of mental health outcomes, with general findings indicating elevated rates of mental health issues as compared to the pre-COVID-19 era. However, the effect of specific demographic features is less clear. As such, we investigated whether anxiety, depressive, and eating pathology symptoms varied by gender, age, status as a medical provider (compared to the general public), race, or region of origin. Forty-three effect sizes from 36 studies indicated that all three symptoms increased from pre- to peri‑COVID-19-eras across all regions. No symptom varied by age, status as a medical provider, or race, though females were significantly more likely to experience eating pathology than males. Findings from our study indicate that worldwide, regardless of age, status as a medical provider, race, or region of origin, respondents experienced significantly elevated rates of psychopathology symptoms during the onset of the COVID-19 pandemic.
Keywords: COVID-19, SARS-CoV-2, Anxiety, Depression, Eating pathology
1. Introduction
In late 2019, Novel Coronavirus Disease COVID-19 emerged as a grave threat to world health, rapidly crossing borders and infecting millions of people worldwide. Shortly after its emergence, COVID-19 was designated by the World Health Organization (WHO, 2020) as a pandemic, and national and local governments acted to protect the health and safety of their citizens. Governments instated quarantine, “safer-at-home,” physical distancing, and lock-down orders, and the public response to those measures was substantial. Media outlets and empirical studies reported widespread mental health concerns, complicated by sharp economic declines, long-term unemployment, and the mass closures of businesses and schools. Further, the uncertainty of these hardships, particularly during the months immediately following the emergence of COVID-19, likely exacerbated stress for many around the world. Indeed, increase in psychological distress was reflected in a recent study of a psychiatric inpatient unit. In a study of 4550 inpatients, researchers found evidence of increased psychopathology (i.e., suicidal ideation) and the need for longer hospital stays during the COVID-19 era, as compared to the pre-COVID-19 era (Boldrini et al., 2021).
In the months preceding COVID-19, the WHO released its annual reports of the global prevalence rates of anxiety, depression, and eating pathology diagnoses (4%, 5%, and 9%, respectively; WHO, 2019). These values were similar to the five years preceding 2019, indicating that the prevalence rates of these specific forms of psychopathology were relatively stable.1 Immediately following the onset of COVID-19, many studies noted steep increases in the experience of anxiety, depressive, and eating pathology symptoms (Qiu et al., 2021, Taylor et al., 2020a; Wang et al., 2020). However, there is considerable variability in these data, suggesting, perhaps, that effect sizes could reflect statistical outliers derived from small samples with unusually high rates of psychopathology. Further, demographic variables may confer variable risk for the experience of anxiety, depressive, and eating pathology symptoms. For instance, as young people experience lower rates of morbidity and mortality due to COVID-19 (WHO, 2020), they may experience less fear and less psychopathology during the early months of the COVID-19 pandemic. Likewise, women experienced higher prevalence rates of anxiety, depressive, and eating pathology symptoms even prior to the pandemic, and thus could be particularly at risk for psychological impact during the initial phase of the outbreak (Elbay et al., 2020; Gonzalez-Sanguino et al., 2020; Özdin and Bayrak Özdin, 2020; Wang et al., 2020; Zhu et al., 2020). Further, some hypothesize that medical providers, who witnessed the devastating and debilitating effects of COVID-19 firsthand, would exhibit elevated rates of anxiety, depressive, and eating pathology symptoms. Still others conceptualized race/ethnicity as a moderating factor between the onset of COVID-19 and psychopathology, generally attributing this moderating effect to misinformation and racist remarks expressed by national and international leaders (Lee and Crunk, 2020; Tanhan et al., 2020). The documented elevated rates of psychopathology during early months of the COVID-19 pandemic leave many questions unanswered and nuances left unexplored.
Thus, the present study sought to address these questions via a systemic review and meta-analysis. First, we estimated prevalence rates of anxiety, depressive, and eating pathology symptoms during the early months of COVID-19. Next, we compared these prevalence rates to those prior to the early months of COVID-19. Finally, we explored the moderating effects of race, age, gender, status as a medical provider, and region of origin on prevalence rates of anxiety, depressive, and eating pathology symptoms during the early months of COVID-19.
We hypothesized that, as compared to pre-pandemic reports, peri‑pandemic effects would indicate elevated rates of anxiety, depressive, and eating pathology symptoms. Given that risks of COVID-19-related morbidity and mortality increase with age (Centers for Disease Control and Prevention [CDC], 2020; WHO, 2020), we expected that as participants increased in age, so would their prevalence of these psychopathology symptoms. We also expected that symptoms would be more prevalent in women, as women experienced higher rates of anxiety, depressive, and eating pathology symptoms even before the onset of the pandemic. As medical providers are often exposed to the virus itself and are witness to its catastrophic and lethal results, we hypothesized that they would report elevated psychopathology symptoms in comparison to the general population.
Next, given the increase in xenophobic and racist sentiments (Associated Press, 2020; British Broadcasting Corporation, 2020; Los Angeles Times, 2020; National Public Radio, 2020; New York Times, 2020; Wall Street Journal, 2020; Washington Post, 2020), we hypothesized differences based on race, with participants identifying as Asian reporting elevated rates of anxiety, depressive, and eating pathology symptoms. Finally, with regard to region of origin, we hypothesized that samples comprised of participants from the broader Pacific region of the world (given they were the first to experience the effects of COVID-19), as opposed to participants from Europe, the Americas, the Mediterranean, or Africa, would report elevated anxiety, depressive, and eating pathology symptoms.
This study has notable strengths, including a summary and analysis of the prevalence rates of anxiety, depressive, and eating pathology symptoms during the early months following the emergence of COVID-19. Further, we place these findings within the context of the pre-COVID-19 era rates. We also investigate the moderating role of many important demographic features: age, gender, status as a medical provider, race, and region of origin. Finally, we discuss clinical implications and suggestions for mental health providers during the COVID-19 pandemic.
2. Methods
2.1. Search strategy
The review was conducted according to the PRISMA guidelines (www.prisma-statement.org/). The search strategy targeted studies that reported information on prevalence rates of anxiety, depressive, and eating pathology symptoms, published any time until July 31 of 2020. Computer-based internet databases used for this search included: PsycInfo, and GoogleScholar. The combinations of keywords used in the database search included: "suicid*" OR "anxiety" OR "depress*" OR “eating” AND "COVID" OR "COVID-19″ OR "Coronavirus" OR “SARS-COV-2.” A secondary search examined the reference list of all retained articles. Both published and unpublished reports were considered in the review process. The initial data searches were conducted by K.M.S. Subsequent data checking and searches were overseen by A.L., and mismatches in classification of studies were resolved by consensus. We then compared prevalence rates of psychopathology between prior to and during the COVID-19 pandemic.
2.2. Eligibility criteria and selection of studies
Studies were eligible for inclusion if they contained estimates of prevalence rates of anxiety, depressive, and/or eating pathology symptoms within the context of the COVID-19 pandemic. Only studies that included these estimates as the outcome variable were included. We excluded treatment studies, qualitative studies, case studies, editorials, and commentaries. We also excluded articles if they combined the prevalence rate of two or more outcome variables (e.g., combined prevalence of anxiety and depressive symptoms). Articles were first screened based on title and abstracts and then, if they still met criteria, the entire article was reviewed. Articles published in English were included. Most studies were cross-sectional and were self-report.
2.3. Data extraction
Information extracted from each study included the prevalence rate of anxiety, depressive, or eating pathology symptoms, author names, sample age, percentage of sample that was female, percentage of sample that was male, if participants were recruited based on status as a medical provider, percentage of the sample that was White, Black, and Asian, location of the study (i.e., Africa, Eastern Mediterranean, Europe, Americas, Southeast Asia, and Pacific), title of measures that were used, and description of the comparison population.
2.4. Coded variables
Each study was coded based on study name, outcome variable (i.e., 1 = anxiety, 2 = depressive, 3 = eating pathology), effect size (usually number of participants who did and did not meet criteria for psychopathology), mean age of the sample in years, percent of the sample that identified as male, percentage that identified as female, if the sample was recruited specifically to include medical providers (i.e., 1 = yes, 2 = no), region from where the sample was recruited (i.e., Africa, Eastern Mediterranean, Europe, Americas, Southeast Asia, and Pacific), and race as percent of the sample that identified as Asian, White, and Black.
2.5. Statistical analysis
All effect sizes were transformed into a single common metric, event rate, which indicated the number of participants in each sample endorsing anxiety, depressive, and eating pathology symptoms. We conducted analyses to determine prevalence rates of anxiety, depressive, and eating pathology symptoms within all included studies and compared these values to pre-pandemic rates. Then we conducted moderator analyses to determine if there were significant differences in prevalence rates of anxiety, depressive, and eating pathology symptoms based on age, gender, status as a medical provider, race, or region of origin. Given the significant evidence of heterogeneity (I-squared = 99.160) and consistent with the broader literature, all analyses employed random effects models. The elevated level of heterogeneity between effect sizes indicates that between samples, there were significantly differing experiences of psychopathology, perhaps pointing to specific features within each sample accounting for between-study variance. Funnel plots were used to assess the precision of estimates. All analyses were conducted using Comprehensive Meta-Analysis (Borenstein et al., 2005).
3. Results
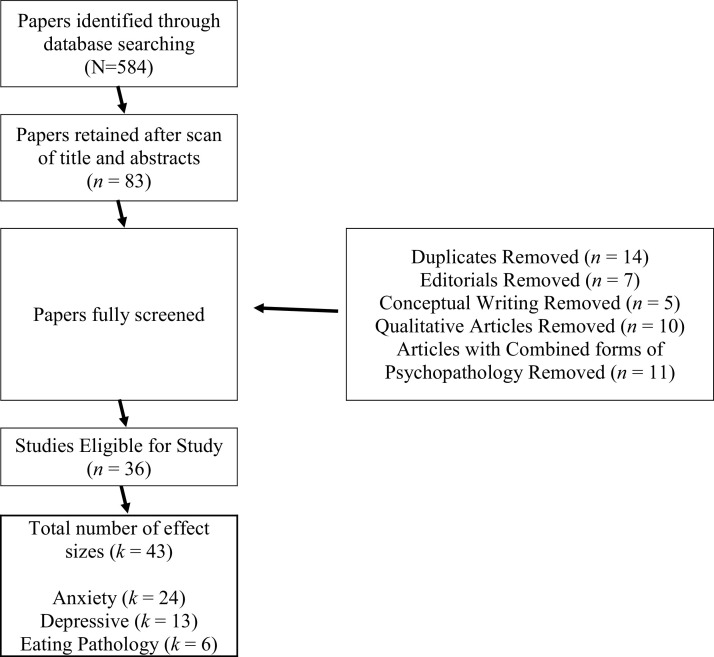
A total of 584 articles were identified using the search terms. Fig. 1 depicts the PRISMA flowchart of eligible papers for the present study. Initial scan of titles and abstracts led to 83 studies being retained. Review of the full manuscripts led to the exclusion of duplicates, editorials, conceptual pieces, qualitative articles, and articles that reported combinations of psychopathology. In all, 36 studies were eligible, with 43 unique effects. See Table 1 for effect sizes related to each included study.
Fig. 1.
PRISMA Reporting of papers and effect sizes included in the present study.
Table 1.
Studies and effects sizes of peri-COVID-19 measures of anxiety, depressive, and eating pathology symptoms.
 |
3.1. Pre-COVID-19 prevalence rates of symptoms of psychopathology
We estimated the pre-COVID-19 prevalence rate of anxiety, depressive, and eating pathology symptoms by searching the literature and extracting pre-pandemic prevalence rates from large, diverse studies that were published prior to 2019 (the year in which COVID-19 was first identified).
3.2. Pre-COVID-19 prevalence rates of anxiety symptoms
The pre-pandemic rate of anxiety symptoms was estimated using three large studies. A 2008 study of 5030 community members from the general population (Lowe et al., 2008) found that 5% of the sample endorsed anxiety symptoms, when measured using the Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al., 2006). Likewise, when using the Kessler Psychological Distress Scale (Kessler-10; Kessler et al., 2002), 14.4% of a sample of 8841 adults in the general population also endorsed anxiety symptoms (Slade et al., 2011). Finally, a systematic review (Baxter et al., 2013) that included studies of prevalence rates of anxiety symptoms published between 1980 and 2009 determined the global prevalence rate of anxiety symptoms to be 7.3%. Based on effect sizes from Lowe et al. (2008), Slade et al. (2011), and Baxter et al., 2013), the pre-pandemic rate of anxiety symptoms was estimated to range from 5% to 14.4%.
3.3. Pre-COVID-19 prevalence rates of depressive symptoms
Likewise, the pre-pandemic rate of depressive symptoms was also estimated from three studies. A study of 9178 adult community members (Ell et al., 2006) found that 8.5% of participants endorsed depressive symptoms, when using the Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001). Further, Slade et al. (2011) studied 8841 adults using the Kessler-10 and found that 6.2% of their sample also endorsed depressive symptoms. Finally, an epidemiological study of community members within 27 states in America (Ko et al., 2012) indicated the prevalence rate of depressive symptoms to be 11.5%. Based on effect sizes from these large studies (Ell et al., 2006; Ko et al., 2012, Slade et al., 2011), we determined pre-pandemic rate of depressive symptoms to range from 6.2% to 11.5%.
3.4. Pre-COVID-19 prevalence rates of eating pathology symptoms
While conducting literature searches for the present study, we noticed that effect sizes measuring peri‑COVID-19 era prevalence rates of symptoms of specific eating disorders—such as Anorexia Nervosa, Bulimia Nervosa, or Avoidant/Restrictive Food Intake Disorder—were relatively sparse. However, in efforts to represent eating pathology in our study, we included effect sizes that measured symptoms of general eating pathology. Thus, using effect sizes from the literature, we estimated symptoms of general eating pathology (e.g., skipping meals and binging on large quantities of food) during the peri‑COVID-19 era and we then compared those to estimates of symptoms of general eating pathology during the pre-COVID-19 era. In doing so, we compared pre- and peri‑COVID-19 era prevalence rates of similar phenomena: symptoms of general eating pathology, as opposed to specific eating disorders. The pre-pandemic prevalence rate of symptoms of eating pathology was estimated from three studies. In a study of 2822 community-based participants (Eisenberg et al., 2011), 9.4% endorsed symptoms of eating pathology. In another study, among a sample of 3610 participants aged 10–18 years (Zeiler et al., 2016), 23.6% endorsed symptoms of eating pathology. Finally, among 496 community-based adolescents (Stice et al., 2013), 13.1% of the sample endorsed symptoms of eating pathology. Taken together, effect sizes from these studies indicated that the pre-pandemic prevalence rate of symptoms of eating pathology ranged from 9.4% to 23.6%.
3.5. Peri-COVID-19 prevalence rates of anxiety, depressive, and eating pathology symptoms
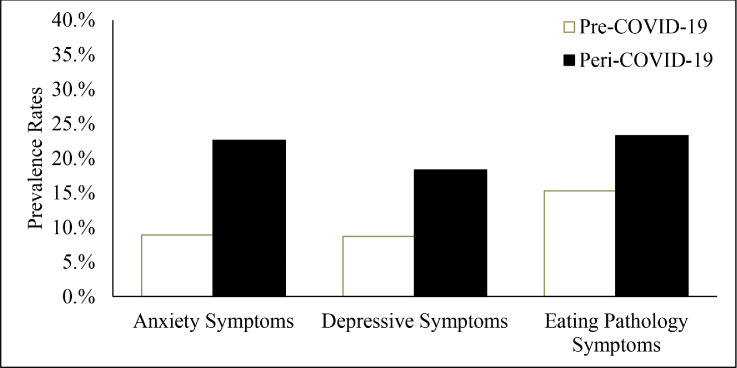
We then estimated the prevalence rates of anxiety, depressive, and eating pathology symptoms during the COVID-19 pandemic (i.e., the peri‑COVID-19 era). Table 2 and Fig. 2 depict these peri‑COVID-19 era rates of anxiety, depressive, and eating pathology symptoms: during the peri‑COVID-19 era, there was substantial evidence of anxiety (k = 24, ER = 22.6%, 95% CI 18.3% - 27.6%), depressive (k = 13, ER = 18.3%, 95% CI 13.5% - 24.3%), and eating pathology (k = 6, ER = 23.2%, 95% CI 18.4% - 28.9%) symptoms.
Table 2.
Event Rates of anxiety, depressive, and eating pathology symptoms before and during the COVID-19 pandemic.
| Pre-COVID-19 Era | Peri-COVID-19 Era | |||
| Anxiety Symptoms | 8.9% | (5.5%−14.4%) | 22.60% | (18.3% - 27.6%) |
| Depressive Symptoms | 8.7% | (6.2% - 11.5%) | 18.30% | (13.5% - 24.3%) |
| Eating Pathology Symptoms | 15.30% | (9.4% - 23.6%) | 23.30% | (18.4% - 28.9%) |
Fig. 2.
Prevalence rates of anxiety, depressive, and eating pathology symptoms prior to and during COVID-19 pandemic.
3.6. Comparison of Pre- versus Peri-COVID-19 prevalence rates of anxiety, depressive, and eating pathology symptoms
Table 2 and Fig. 2 depict the prevalence rates of symptoms. They indicate that across anxiety (pre-COVID-19 = 8.9%; peri‑COVID-19 = 22.6%; z-score = 17.34, p < .001), depressive (pre-COVID-19 = 8.7%; peri‑COVID-19 = 18.3%; z-score = 15.12, p < .001), and eating pathology (pre-COVID-19 = 15.3%; peri‑COVID-19 = 23.3%; z-score = 16.17, p < .001) symptoms, participants reported significantly elevated rates in the peri‑ as compared to the pre-COVID-19 era.
3.7. Peri-COVID-19 era moderating effects
The third aim was to investigate the moderating roles of race, age, gender, status as a medical provider, and region of origin on peri‑COVID-19 era prevalence rates of anxiety, depressive, and eating pathology symptoms. The following section presents these results. Again, these analyses were conducted using data extracted from the literature regarding the prevalence rates of symptoms of psychopathology during the peri‑COVID-19 era.
3.8. Race
Using a series of meta-regressions, we determined if any particular race was at elevated risk for symptoms of psychopathology during the COVID-19 pandemic. Anxiety (Asian [B = −0.015, 95% CI −0.035 – 0.004, p = .12], White [B = 0.025, 95% CI −0.06 – 0.04, p = .13], or Black [B = 0.22, 95% CI −0.06, 0.52, p = .13]) and depressive (Asian [B = −0.13, 95% CI −0.03 – 0.01, p = .27], White [B = 0.018, 95% CI −0.14 – 0.05, p = .27], or Black [B = 0.205, 95% CI −0.16 - 0.57, p = .27]) symptoms did not vary based on race. Finally, symptoms of eating pathology were not reported sufficiently in the literature to result in adequately powered analyses, thus we did not report if symptoms of eating pathology varied by race.
3.9. Age
We then determined if symptoms of psychopathology varied by age. Using a series of meta-regressions, we found that anxiety (B = 0.004, 95% CI −0.08 – 0.09, p = .92) and depressive (B = 0.006, 95% CI −0.016 – 0.11, p = .91) symptoms did not vary by age. Again, effect sizes related to symptoms of eating pathology were insufficient for adequately powered analyses. Thus, those are not reported.
3.10. Gender
We were then interested if symptoms of psychopathology varied by gender. Meta-regressions indicated that although anxiety (B = −0.005, CI −0.018 – 0.005, p = .268) and depressive (B = 0.008, CI = −0.013 – 0.014, p = .905) symptoms did not vary by gender, symptoms of eating pathology (B = −0.013, CI – 0.022 – 0.004, p = .049) were significantly more prevalent in female participants than in male participants.
3.11. Status as a medical provider
Given that many medical providers risked exposure to COVID-19, we investigated if status as a medical provider conferred significant risk of symptoms of psychopathology. Meta-regression indicated that anxiety (B = −0.04, 95% CI −0.61 – 0.52, p = .87) and depressive (B = 0.19, 95% CI −0.53 – 0.91, p = .60) symptoms did not vary between samples who were and were not recruited on the basis as a medical provider. Symptoms of eating pathology were omitted from meta-regression based on insufficient number of effect sizes.
3.12. Region of origin
We then investigated the symptoms of psychopathology by region of origin, designations determined by the World Health Organization. That is, we conducted moderator analysis by region of origin (versus all others) to examine levels of psychopathology symptoms: Americas (k = 4, ER = 41.2%, 95% CI 38.5% - 43.9%, p < .001), Eastern Mediterranean (k = 1, ER = 50.9%, 95% CI 49.9%−51.8%, p = .067), Europe (k = 12, ER = 28.9%, 95% CI 22.0% - 36.9%, p < .001), Pacific (k = 29, ER = 17.6%, 95% CI 15.1% - 20.3%, p < .001). Effect sizes indicated there were significant evidence of symptoms of psychopathology across all reported regions.
When investigating group differences in symptoms of psychopathology, effect sizes from the Americas (k = 4, ER = 41.2% [38.5–43.9%]) did not differ (z-score =1.3293, p = .18) from all other regions (k = 42, ER = 30.5% [30.1–30.8%]). Likewise, effect sizes from Europe (k = 12, ER = 28.9, 95% CI 22.0%–36.9%, p < .001) did not differ significantly (z-score = −0.262, p = .79) from all other regions (k = 34, ER = 31.5% [31.1–1.9%]). However, effect sizes from Eastern Mediterranean (k = 1, ER = 50.9%, 95% CI [49.9%−51.8%]) were significantly elevated (z-score = 2.8068, p = .004) as compared to all other regions (k = 45, ER = 26.5%, 95% CI [26.1 – 26.9]). Finally, effect sizes from the Pacific (k = 29, ER = 17.6%, 95% CI [15.1–20.3%]) were significantly lower (z-score = 3.0908, p = .002) than all other regions (k = 17, ER = 39.9% [39.2–40.6%]).
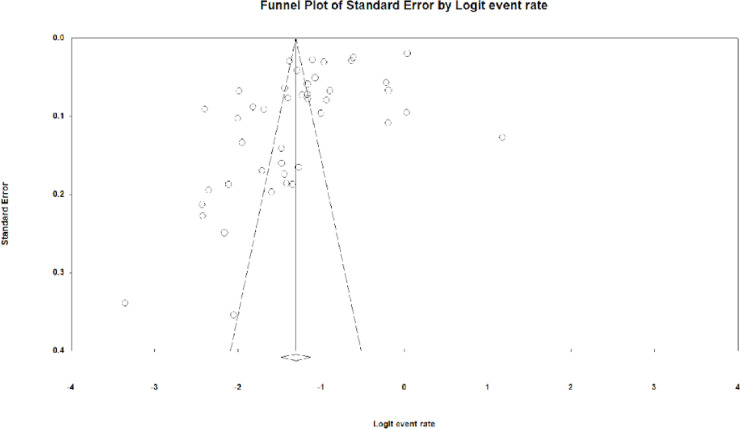
3.13. Publication bias
Overall, there was significant evidence of publication bias (Egger's regression intercept = −8.17, 95% CI −12.96 - −3.38, p = .001). Further, upon inspection of funnel plots (see Fig. 3 ), we found significant evidence indicating that there were many effect sizes missing to the right of the mean, likely indicating that there is substantial evidence of symptoms of psychopathology that is left out of the literature.
Fig. 3.
Funnel plots for evidence of missing studies regarding prevalence rates of psychopathology during COVID-19.
4. Discussion
The present study sought (1) to estimate the peri‑COVID-19 era prevalence rates of anxiety, depressive, and eating pathology symptoms, (2) compare pre- and peri‑COVID-19 era prevalence rates of anxiety, depressive, and eating pathology symptoms, and (3) explore the moderating roles of race, age, gender, status as a medical provider, and region of origin on the peri‑COVID-19 era prevalence rates of anxiety, depressive, and eating pathology symptoms. Overall, findings indicated that (1) there was substantial evidence of anxiety, depressive, and eating pathology symptoms within the peri‑COVID-19 era, (2) peri‑COVID-19 era prevalence rates of anxiety, depressive, and eating pathology symptoms are elevated as compared to pre-COVID-19 era rates, and (3) with few exceptions, elevations appear to be pervasive, as symptoms of psychopathology did not vary by race, age, gender, status as a medical provider, and region of origin. However, there is one notable exception to that trend: women, as compared to men, experienced increased eating pathology symptoms. These results, as well as implications, strengths, and limitations are discussed below.
It should be noted that this project was conceived in an effort to understand the role of the COVID-19 era on mental health outcomes. We used data that were available in the literature to estimate peri‑COVID-19 era prevalence rates of anxiety, depressive, and eating pathology symptoms and compare those to analogous figures in the pre-COVID-19 era. In our efforts, we were largely guided by the precedence of work set by other researchers. Literature searches indicated that anxiety and depressive symptoms were among the most commonly studied mental health outcomes during the peri‑COVID-19 era, whereas symptoms of other disorders (including specific eating disorders) were less commonly studied. With regard to specific eating disorders, such as Anorexia Nervosa (AN), Bulimia Nervosa (BN), and Avoidant/Restrictive Food Intake Disorder (ARFID), researchers tended, instead, to study symptoms related to more general psychopathology during the COVID-19 era, and many opted to study symptoms related to the broad category of “eating pathology.” Although this mental health outcome was more general than the specific and well-defined eating disorders of AN, BN, or ARFID, due to a specific interest within our research group, we likewise opted to study the general outcome of “eating pathology” in the present project. Thus, the types of psychopathology presented in this manuscript (i.e., anxiety, depressive, and eating pathology symptoms) may not necessarily reflect the most optimal or well-defined outcomes of interest. Further, authors put forth considerable and concerted effort to compare analogous phenomena between the pre- and peri‑COVID-19 rates. Specifically, we opted to study prevalence rates of symptoms of psychopathology in both eras, ensuring that our findings are based on direct comparisons of analogous experiences.
In Aim 1 of our study, we estimated the peri‑COVID-19 era prevalence rates of anxiety, depressive, and eating pathology symptoms. Indeed, across studies, participants endorsed statistically and clinically significant symptoms of all disorders: anxiety symptoms (prevalence rate of 22.6%), depressive symptoms (prevalence rate of 18.3%), and eating pathology symptoms (prevalence rate of 23.3%). These results were consistent with both peer-reviewed literature and media reports that demonstrated evidence of psychological symptoms during the COVID-19 era, and they supported our hypothesis that we would find significant evidence of anxiety, depressive, and eating pathology symptoms during the COVID-19 era. Further, these results highlight the widespread nature of these phenomena. A significant portion of all participants reported that during COVID-19, they experienced symptoms of psychopathology, manifested in a variety of symptom presentations. This strong response leads to considerations regarding the ability of mental healthcare providers to treat anxiety, depressive, and eating-pathology symptoms in a sizable portion of the population. Notably, although these results highlight that many across the globe experienced symptoms of psychopathology during the COVID-19 era, these results did not provide insight into the relative risk of anxiety, depressive, and eating pathology symptoms before versus after COVID-19 emerged. Thus, it was unclear if the peri‑COVID-19 era was associated with an increased experience of anxiety, depressive, and eating pathology symptoms.
To address this question, in the second aim of our study, we compared the pre- versus peri‑COVID-19 era prevalence rates of anxiety (pre-COVID-19 = 8.9%; peri‑COVID-19 = 22.6%), depressive (pre-COVID-19 = 8.7%; peri‑COVID-19 = 18.3%), and eating pathology (pre-COVID-19 = 15.3%; peri‑COVID-19 = 23.3%) symptoms. Findings supported previous literature and our hypothesis, such that participants experienced statistically significantly increased prevalence rates of symptoms of anxiety, depression, and eating pathology in the peri‑ as compared to the pre-COVID-19 era. Notably, the peri‑COVID-19 era was not associated with increased symptomology in merely one aspect of mental health. Instead, across studies, participants endorsed symptoms related to a variety of disorders, with the COVID-19 era producing unanimously deleterious effects. The most substantial increase appears to be within anxiety symptoms. This finding may highlight common reactions to stress during the COVID-19 era. For example, anxiety is often characterized by rumination, repeated attempts at preparing for worst-case scenarios, futile attempts at problem solving, and the overestimation of the likelihood of catastrophic events. Since many people endorsed symptoms of anxiety during the peri‑COVID-19 era, this may indicate that, during the pandemic, they attempted to strategize ways to keep themselves and their families safe from objectively bad outcomes. The latter may include contracting the virus, experiencing acute or lasting effects of the virus and/or economic downturns, or struggling to educate children given the loss of in-person schooling—especially as many parents are continuing to work and are not prepared or equipped to implement full-time childhood education. That is, the substantial increase in anxiety symptoms likely reflects concerted, yet to a degree thwarted attempts, to prepare for an uncertain, unprecedented course of events.
We then explored the role of demographic features as moderators of anxiety, depressive, and eating pathology symptoms in the peri‑COVID-19 era. In Aim 3, we determined if particular aspects of samples—race, age, gender, status as a medical provider, and region of origin—were associated with increased prevalence rates of anxiety, depressive, and eating pathology symptoms in the peri‑COVID-19 era. Generally, none of these moderators were found to significantly predict differences in anxiety, depressive, and eating pathology symptoms, indicating that symptomology was pervasive. Across the whole, findings from Aim 3 indicate that regardless of demographic features, the diverse sample of participants all endorsed elevations in anxiety, depressive, and eating pathology symptoms following the emergence of COVID-19. There was substantial evidence of widespread and insidious increase in symptoms of psychopathology.
Race. Following the emergence of COVID-19, national leaders and others on the international stage articulated racist and xenophobic rhetoric regarding the initial outbreak and the subsequent spread of COVID-19. As such, we hypothesized that anxiety, depressive, and eating pathology symptoms would vary based on race. However, upon investigation, moderator analyses of available literature did not support this hypothesis, as psychopathology symptoms were experienced at similar rates across racial groups. This could suggest that, although national and international leaders articulated racist sentiments, social bonds and support on the more local level buffered individuals of particular racial groups from dramatically increased experience of psychopathology symptoms. Alternatively, these findings could indicate that—in a global climate characterized by intensifying beliefs of nationalism and racism— anxiety, depressive, and eating pathology symptoms have increased, regardless of race and in all members of society. Indeed, nationalism and racially motivated oppression, especially when enacted through violent means, place all members of society, not just particular racial groups, at risk of substantial harm.
Age. Younger people tend to encounter relatively low rates of COVID-19-related morbidity and mortality; thus we hypothesized that as the mean age of samples increased, participants would be more likely to experience of anxiety, depressive, and eating pathology symptoms. Again, our findings did not support this hypothesis; moderator analyses indicated that symptoms of psychopathology did not vary by age, in either direction, such that young people were no more or less likely to experience symptoms of psychopathology as compared to older members of the population. Perhaps these findings, too, are a testament to the widespread and ubiquitous nature of psychopathology symptoms during the peri‑COVID-19 era. Younger individuals were not immune to changes during COVID-19, and young people experienced transitions from in-person to online schooling, loss of celebrations marking achievements and milestones (such as graduations), and disruptions to extracurricular events. Likewise, older samples experienced loss of in-person contact with children and grandchildren, and middle-age members of society shouldered a substantial burden of raising children, many times without support of childcare (whether that be through formal childcare services or through the support of extended family members). These findings give credence to the society-wide burden of the COVID-19 pandemic, regardless of age.
Gender. We next investigated gender as a moderator of the experience of anxiety, depressive, and eating pathology symptoms. Evidence indicates that men, as compared to women, are more likely to have serious morbidity and mortality related to COVID-19, such that men, as compared to women, who contract COVID-19 are more likely to be hospitalized, encounter severe complications, and/or die from the disease (Xie et al., 2020; Guan et al., 2020). Given the substantially poorer outcomes that men experience, we hypothesized that men would experience increased symptoms of psychopathology, as compared to their female counterparts. However, and very much to our surprise, moderator analyses from our work indicated that there were no significant gender-based differences in symptoms of anxiety or depression, such that men and women did not vary in their experience of anxiety or depressive symptoms. This finding was surprising, given that men are objectively more at-risk of falling severely ill and/or dying from COVID-19 than women. However, when placed in the context of the broader literature, these results seem to be consistent with a maladaptive and ill-fated approach to COVID-19. Men, although at increased risk of dying from COVID-19, are less likely to wear masks or to report believing that they will be significantly affected (Capraro and Barcelo, 2020). Further, reports indicate that men are more likely than women to believe that wearing masks is “shameful, not cool, a sign of weakness, and a stigma” (Capraro and Barcelo, 2020, p 1). Thus, while being male is a risk factor for poorer outcomes related to COVID-19, it may act as a buffer from experiencing elevated of symptoms of psychopathology. Notably, women experienced greater symptoms of eating pathology during COVID-19—consistent with pre-COVID-19 rates of eating pathology—suggesting that pre-pandemic gender-based differential between eating pathology symptoms held.
Medical providers. Next, we were interested in whether status as a medical provider conferred significant risk for symptoms of psychopathology. Specifically, we hypothesized that status as a medical provider would be associated with increased risk of anxiety, depressive, and eating pathology symptoms. However, moderator analyses again indicated that symptoms were elevated across the entire sample, regardless of status as a medical provider. This may be due to the televised nature of the pandemic; through 24-hour news media cycles, even those who are not medical providers have had access to nearly real-time data and news stories documenting mask shortages, bed shortages, and deaths and infections due to COVID-19. Regardless of status as a medical provider, increased rates of anxiety, depressive, and eating pathology symptoms were evident.
Region of origin. Finally, we were interested in the peri‑COVID-19 prevalence rates of anxiety, depressive, and eating pathology symptoms by region of origin. COVID-19 emerged and was first identified within the Pacific region (WHO, 2020). Despite this, our findings indicated that the increase in psychopathology symptoms did not vary by region. Again, this may reflect a global response to the pandemic, as cases quickly spread worldwide.
Limitations. This study has many notable strengths including the diverse and widespread nature of samples, the estimation of three types of psychopathology, efforts to place prevalence rates of peri‑COVID-19 era psychopathology symptoms in context with similar phenomena in the pre-COVID-19 era, and moderator analyses investigating many aspects of demographic features. However, our study has limitations that should be also noted. First, as previously mentioned, there was significant evidence of publication bias, and psychopathology has been left out of the literature. As such, certain findings should be interpreted with caution. For example, although the Americas and Mediterranean regions appear to have more symptoms of psychopathology, these studies also had fewer effect sizes, and the effects that did emerge may be skewed. Further, despite the wide scope of international studies collected, it is unclear whether findings are wholly generalizable, as statistical analyses were limited to few racial groups.
Next, most studies relied exclusively on self-report measures, leading to some limitations in the inferences that can be made. For example, participants may exaggerate their experiences of psychopathology on self-report measures in efforts to convey the distress that they are currently experiencing. Alternatively, they may minimize the effects of psychopathology, and without the interpersonal interactions that would take place in-person interviews, these approaches go unnoticed and unmeasured by research studies. Further, they were primarily completed over web-based formats excluding participants who do not have reliable access to internet or electronic devices. That is, they may have inadvertently excluded some of the poorest members of populations, samples that would likely be facing particular challenges during the pandemic (e.g., the inability to adequately social distance due to close living environments and public transit, loss of health care insurance, lack of financial safety nets including depleted savings accounts and lack of financial support from family or friends). Across studies, similar measures were generally used, including the Patient Health Questionnaire-9 (PHQ-9), the Generalized Anxiety Disorder-7 (GAD-7), Self -Rating Anxiety Scale (SAS), and Self-Rating Depression Scale (SDS). Notably, many studies employed abbreviated versions of these scales, and those studies did not articulate specifically which items were included in their abbreviated measures.
Additionally, in this project we sought to estimate the relatively increased prevalence rates of psychopathology during the COVID-19 era; however, we did not investigate the mechanisms by which these increased rates came about. Recent literature within an Italian sample points to vulnerability and helplessness as contributors to the development and exacerbation of psychopathology (Rossi et al., 2021). It is possible that these factors contribute psychopathology to other populations. However, given that we did not examine important contributing factors in this project, we are unsure if similar mechanisms contributed to increased symptomology across the globe, or if these varied by location, age, gender, or other demographic features.
Combining findings from the present study with Rossi et al. (2021), it is possible that upon the onset of COVID-19 many people experienced helplessness and vulnerability within the broader population, as they were unsure of ways to keep themselves and loved ones safe during the pandemic. There is some evidence, however, within the published literature that indicates that by counteracting feelings of vulnerability and helplessness, and empowering patients to take an active role in their mental and physical health, patients can reduce symptoms and improve quality of life. Specifically, a study of more than one thousand patients living with cardiovascular disease indicated that by implementing “care managers” (healthcare providers specifically employed to provide education regarding symptoms, course, and resources around their disease) into healthcare teams, patients improved their health knowledge, self-management skills, and readiness to make changes in health behaviors (Ciccone et al., 2010). It is possible that by employing similar care managers within large healthcare systems, patients can learn about COVID-19 (e.g., transmission rates, prevalence rates, symptomology, prevention, and course of illness) and be empowered to reduce their risk of contracting COVID-19. Importantly, by reducing the likelihood of contracting COVID-19 or becoming seriously ill with COVID-19, this approach could ease the burden on healthcare systems and providers who have experienced extreme demand during the pandemic.
A major aim of our work was to assess for longitudinal studies that measured the effect of the COVID-19 pandemic on psychopathology. We had hoped to find longitudinal studies that assessed participants for anxiety, depression, at eating pathology symptoms at baseline, before the onset, and then again at follow-up, after the onset of COVID-19. Unfortunately, these data were not typically found in the literature. In fact, most studies employed cross-sectional methods that measured psychopathology during the time of COVID-19. Thus, we were unable to examine the role of the COVID-19 pandemic stringently within individual samples. Whereas we aimed to investigate the prevalence of psychopathology across many regions of the world, the majority of studies included in our review were conducted in the Pacific region, stemming primarily from China.
5. Conclusion
The far-reaching effects of COVID-19 corresponded with increased experience of anxiety, depressive, and eating pathology symptoms during the early months of the pandemic. Regardless of gender, age, race, status as a medical provider, or geographic location, participants reported increased symptoms of psychopathology in the peri‑ as compared to the pre-COVID-19 era. Specifically, the COVID-19-era produced pervasive and unanimous effects related to anxiety, depressive, and eating pathology symptoms across all demographics studied. Given the pervasive nature of psychopathology in the time of COVID-19, healthcare providers should routinely assess all patients for significant anxiety, depressive, and eating pathology symptoms, as well as engage in concerted efforts to reduce barriers to mental health treatment.
Author statement
Katherine Musacchio Schafer, Amy Lieberman, and Thomas Joiner are funded supported in part by the Military Suicide Research Consortium (MSRC), an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs under Award Nos. (W81XWH-16–20,003). Opinions, interpretations, conclusions and recommendations are those of the authors and are not necessarily endorsed by the MSRC or the Department of Defense.
CRediT authorship contribution statement
Katherine Musacchio Schafer: Conceptualization, Writing – review & editing. Amy Lieberman: Data curation, Investigation, Writing – review & editing. Anna C. Sever: Data curation, Investigation, Writing – review & editing. Thomas Joiner: Writing – review & editing, Conceptualization.
Declaration of Competing Interest
There are no conflicts of interest to disclose.
Acknowledgments
This work was supported in part by the Military Suicide Research Consortium (MSRC), an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs under Award Nos. (W81XWH-16–20003). Opinions, interpretations, conclusions and recommendations are those of the authors and are not necessarily endorsed by the MSRC or the Department of Defense
Footnotes
Notably, these values reported by WHO (2019) differ from the values in the Abstract and Results section of the present work. The values reported by WHO (2019) reflect diagnoses of anxiety, depression, and eating pathology whereas in the present study we report symptom metrics.
References
- Baxter A.J., Scott K.M., Vos T., Whiteford H.A. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol. Med. 2013;43(5):897. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- Boldrini T., Girardi P., Clerici M., Conca A., Creati C., Di Cicilia G., Lomoriello A.S. Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in Italy: reduced psychiatric hospitalizations and increased suicidality. Prog. Neuro Psychopharmacol. Biol. Psychiatry. 2021;110 doi: 10.1016/j.pnpbp.2021.110304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capraro, V., & Barcelo, H. (2020, May 11). The effect of messaging and gender on intentions to wear a face covering to slow down COVID-19 transmission., 10.31234/osf.io/tg7vz. [DOI] [PMC free article] [PubMed]
- Ciccone M.M., Aquilino A., Cortese F., Scicchitano P., Sassara M., Mola E., Bux F. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo) Vasc. Health Risk Manag. 2010;6:297. doi: 10.2147/vhrm.s9252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg D., Nicklett E.J., Roeder K., Kirz N.E. Eating disorder symptoms among college students: prevalence, persistence, correlates, and treatment-seeking. J. Am. Coll. Health. 2011;59(8):700–707. doi: 10.1080/07448481.2010.546461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbay R.Y., Kurtulmuş A., Arpacıoğlu S., Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ell K., Unützer J., Aranda M., Sanchez K., Lee P.J. Routine PHQ-9 depression screening in home health care: depression prevalence, clinical and treatment characteristics, and screening implementation. Home Health Care Serv Q. 2006;24(4):1–19. doi: 10.1300/J027v24n04_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., ÁngelCastellanos M., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., Du B. Clinical characteristics of coronavirus disease 2019 in China. New Engl. J. Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Ko J.Y., Farr S.L., Dietz P.M., Robbins C.L. Depression and treatment among US pregnant and nonpregnant women of reproductive age, 2005–2009. J. Women’s Health. 2012;21(8):830–836. doi: 10.1089/jwh.2011.3466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A., Crunk E.A. Fear and psychopathology during the COVID-19 crisis: neuroticism, hypochondriasis, reassurance-seeking, and coronaphobia as fear factors. OMEGA J. Death Dying. 2020 doi: 10.1177/0030222820949350. [DOI] [PubMed] [Google Scholar]
- Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med. Care. 2008:266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Özdin S., Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020927051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu S.C., Jiang J., Liu X., Chen M.H., Yuan X. Can corporate social responsibility protect firm value during the COVID-19 pandemic? Int. J. Hosp. Manag. 2021;93:102759. doi: 10.1016/j.ijhm.2020.102759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi C., Bonanomi A., Oasi O. Psychological Wellbeing during the COVID-19 Pandemic: the influence of personality traits in the Italian population. Int. J. Environ. Res. Public Health. 2021;18(11):5862. doi: 10.3390/ijerph18115862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T., Grove R., Burgess P. Kessler psychological distress scale: normative data from the 2007 Australian national survey of mental health and wellbeing. Aust. N. Z. J. Psychiatry. 2011;45(4):308–316. doi: 10.3109/00048674.2010.543653. [DOI] [PubMed] [Google Scholar]
- Stice E., Marti C.N., Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J. Abnorm Psychol. 2013;122(2):445. doi: 10.1037/a0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tanhan A., Yavuz K.F., Young J.S., Nalbant A., Arslan G., Yıldırım M., Çiçek İ. A proposed framework based on literature review of online contextual mental health services to enhance wellbeing and address psychopathology during COVID-1. 9. 2020 [Google Scholar]
- Taylor C.B., Fitzsimmons-Craft E.E., Graham A.K. Digital technology can revolutionize mental health services delivery: the COVID-19 crisis as a catalyst for change. Int. J. Eating Disord. 2020 doi: 10.1002/eat.23300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Tong Z., Guan X., Du B., Qiu H. Clinical characteristics of patients who died of coronavirus disease 2019 in China. JAMA Netw. Open. 2020;3(4) doi: 10.1001/jamanetworkopen.2020.5619. e205619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeiler M., Waldherr K., Philipp J., Nitsch M., Dür W., Karwautz A., Wagner G. Prevalence of eating disorder risk and associations with health-related quality of life: results from a large school-based population screening. Eur. Eating Disord. Rev. 2016;24(1):9–18. doi: 10.1002/erv.2368. [DOI] [PubMed] [Google Scholar]
- Zhu J., Sun L., Zhang L., Wang H., Fan A., Yang B., Xiao S. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Front. Psychiatry. 2020:11. doi: 10.3389/fpsyt.2020.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]