Highlights
-
•
Cardiovascular and cardiometabolic diseases are largely preventable, and are propagated by a poor diet.
-
•
Poor diet may be due to a lack of supply and access to healthy foods, agricultural subsidies, and marketing.
-
•
Improving national dietary intake starts with enhancing dietary guidelines, enacting legislative changes to optimize agricultural subsidies and food advertising, and incentivizing a plant-forward diet.
Keywords: Food system, Agricultural policy, Primary prevention, Cardiometabolic disease, Nutrition, Social determinants of health
The INTERHEART and INTERSTROKE studies found that modifiable health and lifestyle factors— including unfavorable levels of consumption of fruits and vegetables, physical activity, alcohol, abdominal obesity, psychological factors, smoking, lipids, blood pressure and diabetes— accounted for at least 90% of the risk for myocardial infarction (MI) and stroke worldwide [1,2]. Accordingly, the most effective way of preventing MI and atherosclerotic cardiovascular disease (ASCVD) in general is to follow a healthy lifestyle throughout one's lifetime [3]. Pharmacologic therapies typically only furnish a 10–25% reduction of relative risk, [4], [5], [6] while lifestyle measures may reduce risk by over 80% [7]. While statins, antihypertensives, and other preventive therapeutics play a critical role in the treatment of patients with or at risk for ASCVD, lifestyle improvement, including a healthier diet, remains at the core of all preventive efforts [3].
National attempts at chronic disease prevention, however, have historically been inadequate. Before the COVID pandemic, the leading causes of premature mortality in the United States (U.S.) were ASCVD, cancer, and diabetes, which are largely preventable [7] and yet accounted for sixty percent of all mortality in the U.S. and over $850 billion in healthcare costs and lost productivity annually [8,9]. Nearly one-fourth of our $3.5 trillion annual healthcare spending could be saved by improving our patients’ lifestyle habits and eliminating preventable diseases. Our patients cannot solely be blamed for their poor lifestyle habits. The decisions of an individual are often shaped by circumstances and social determinants of health – education, socioeconomic status, legislation, upbringing, adverse childhood experiences, structural racism, and more [10].
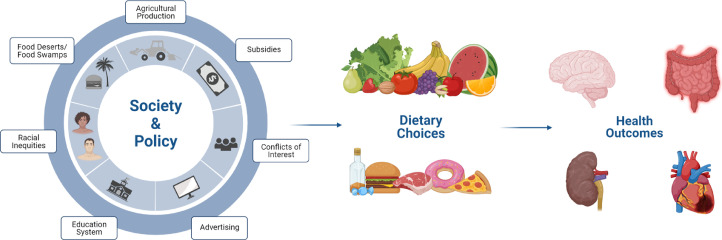
While the epidemiological evidence supporting a diet rich in whole fruits, vegetables, whole grains, and legumes is clear, [11,12] over 90% of Americans consume below the minimum recommended level of these foods daily [13]. Moreover, 98% of Americans exceed the recommended daily amount of solid fats and added sugars [13]. These nutritional inadequacies are explained partially by access to, availability, and proximity of healthy food. In low-income neighborhoods, grocery stores face the challenge of low profit margins and high overhead costs, exacerbated by having a consumer-base that often has less time for home meal preparation [14]. This combination of factors creates food deserts (i.e., where fully-provisioned grocery stores are scarce) and food swamps (i.e., where there is an abundance of inexpensive, processed convenience foods) [15]. Such a dearth of fresh produce can lead to poor nutrition, highlighting an individual's context as a major social determinant of health [16,17]. Even if the government were to step in and erect grocery stores on every block, U.S. Department of Agriculture (USDA) data indicate that the U.S. food system supplies only 75% of the daily vegetable servings recommended for the standard 2000-calorie diet [18] – in other words, even if people had access to vegetables, there would not be enough to go around. Fig. 1.
Fig. 1.
Additionally, grocery stores’ success in food deserts is dependent on demand for healthy food, as simply the presence of healthy food is insufficient to improve food purchasing habits [19]. Those with easy access to farmers’ markets and grocery stores, and an existing desire to purchase healthy foods, are more able to tap into the limited supply of produce than those who live in rural areas or areas underserved by grocery chains [20,21]. Access needs to be paired with financial dis-incentivization of unhealthy foods, a potent method of reducing consumption of energy-dense foods and improving cardiometabolic health, [22] as was shown by Mexico's soda tax [23]. This strategy is especially effective at motivating those who are younger, female sex, have lower income, and are of non-White race/ethnicity, as these groups tend to rank cost of food more important than taste when making food purchase decisions [24].
As agricultural policy dictates production, government-issued payments directly encourage overproduction of commodities that are the basic ingredients of processed, energy-dense foods [25]. Although this supply may be a result of the demands of the American palate, this does not justify the ample production of health-impairing foods. Some data suggest that agricultural subsidies do little to impact food production or price, [26] implying that this money may be better spent elsewhere. Moreover, between 1995 and 2012, 23 Congress members and their families received farm subsidies, highlighting a clear conflict of interest [27]. Federal agricultural subsidies over the last 25 years have amounted to nearly $200 billion for corn, soybean, sorghum, livestock, and dairy alone [28]. Much of the former three are converted into agricultural feed, and a large portion of all five are the raw materials for sweetened drinks, processed foods, and high-fat meat and dairy products [25]. Furthermore, in 2015, the U.S. government spent $22.2 billion in direct and indirect subsidies to the dairy sector, allowing them to sell dairy products at below market value [29]. Subsidized foods can often be less expensive for consumers, as they are partially paid for by the government; [30] hence, individuals with fewer financial means are more likely to buy inexpensive foods made from subsidized ingredients, which are by nature unhealthy [24]. A study of more than 10,000 participants showed that over half of calories consumed are from major subsidized food commodities, nearly all of which are of poor nutritional value, underlining the importance of subsidizing fruits and vegetables instead of the raw materials for energy-dense, processed foods [22,31]. Food policy, health, and societal factors are inextricably linked, [32] and disproportionately affect low-income individuals who are most sensitive to the cost of healthy foods.
The conflict between agribusiness and healthful dietary choices stems, in part, from the USDA's diverging internal mandates, to both promote the agricultural industry and steer the U.S. Dietary Guidelines. These guidelines, which dictate how billions of dollars are spent on the National School Lunch Program (NSLP), the Supplemental Nutrition Assistance Program (SNAP), and the Special Supplemental Nutrition Program for Women, Infants and Children (WIC), disproportionately affect the health of low-income groups that rely on these programs. Moreover, the U.S. Dietary Guidelines Advisory Committee is comprised of advisors to General Mills, Kraft, Campbell's, and a number of pharmaceutical companies [33]. In light of these potential conflicts of interest, it is imperative that food policy reflects the current scientific consensus that a diet high in fiber and low in cholesterol and saturated fat, exemplified by a plant-based diet, is paramount to prevent cardiometabolic disease. Rerouting government subsidies towards fruit and vegetable programs would stimulate production, ameliorating our current production deficit, and ideally helping to promote their consumption.
These legislative changes would reorient our production and recommendation of healthful foods; yet such changes do not necessarily portend widespread acceptance of fruit and vegetable consumption. The privatization of food distribution in a free market complicates the acceptance of healthy foods by the public. Food companies spend over $11 billion on television advertisements annually; [34] of this, 80% is spent on soda, fast food, candy, and unhealthy snacks, and less than 0.5% is spent on fruits and vegetables [35,36]. Many companies go as far as to employ child psychologists to understand how to draw children towards their products, [37] and more than 98% of television food advertisements seen by children are for products high in fat, sugar, and/or sodium [38], [39], [40]. Furthermore, with the advent of personalized advertising across media platforms, Black teenagers are more than twice as likely as White teenagers to see commercials for these unhealthy items [36,41,42]. These advertisements may have a long-lasting negative impact on the health and well-being of children and teenagers, as research shows that what we eat during childhood strongly influences lifelong dietary choices [43,44]. Moreover, families that cook less at home and buy more prepackaged foods are more likely to buy foods that are unhealthy if they are shown ads for unhealthy foods [24,45]. This targeted advertising is driven by the shareholder value movement, obligating private food corporations to yield increasing returns to investors; [46,47] as such, realigning financial incentive with health as opposed to profits is critical.
Reducing corporate incentive to market unhealthy foods to children, while simultaneously improving the quality of food available in schools, is essential to properly nourish our youth [48]. School feeding programs worldwide account for $100 billion annually, and are directly correlated with cognition and educational achievement [49]. Reassuringly, improving school meals to fulfill more nutritional guidelines has been shown to have no detrimental effect on revenue, making this a financially feasible decision even for poorly funded school districts [50]. Nutrition education initiatives have shown promise; the Food, Health, & Choices intervention was a nutrition education curriculum in New York public schools that costed $8.5 million, but was estimated to save $8.1 million in direct medical costs, and 1600 quality-adjusted life-years [51]. While dietary interventions through school meal programs and post-intervention follow up studies are needed to better evaluate the effects of improved school meal quality on the cardiometabolic health outcomes of schoolchildren, a small randomized controlled trial in children did find that healthier dietary patterns led to improved cardiometabolic health [52].
Diet, a key element of our health, is largely determined by the food system, including availability, agricultural subsidies, education, and advertising. These factors differ enormously from individual to individual and region to region, leading to vastly different health outcomes. Quality of diet, exercise, non-smoker status, and body mass index are all correlated with race, ethnicity, level of education, and household income, underlining the importance of these factors in influencing our health. Figure 1 outlines some of the societal and policy factors that influence dietary choices and ultimately shape health outcomes.
In order to address and eventually overcome inequities in healthcare, we need to address societal factors contributing to poor health in the first place. The North Karelia project in Finland was a brilliantly executed collaboration between health services, schools, non-governmental organizations, the food industry, and media that illustrated the immense potential such a collaboration has to reduce the prevalence of ischemic heart disease [53]. This project developed and disseminated healthy, easy-to-prepare recipes, while reducing the salt and fat content in dairy products and baked goods sold by restaurants and food distributors. Dairy farmers were provided with resources to switch to berry farming, television broadcasts began including programs focused on healthy lifestyles, using popular figures as role models, and community-based initiatives provided reliable nutrition education. This broad, comprehensive initiative reduced the national rates of ischemic heart disease by 65%, all-cause mortality by 45%, and increased life expectancy by over six years. Similar government-industry partnerships in the U.S. involving the food industry, agricultural policy legislators, the USDA, and the Centers for Disease Control, paired with robust lifestyle education in schools and community centers, and media programs with advertising regulations, holds enormous potential to improve our country's cardiovascular health.
1. Limitations
Our understanding of the sociocultural factors, institutions, and laws that shape dietary choices is colored by our personal experiences in academic and clinical medicine, and the insights provided to us by the dozens of patients we interact with on a daily basis. Public behavior, especially when it comes to diet, is a dynamic entity that is strongly influenced by cultural factors spanning from the individual to the national and international levels, and consequently is challenging to study objectively. Our interpretation of this data was initiated as a genuine attempt to illustrate areas for improvement in our society that we believe could benefit the health of patients in our country that needlessly ail with preventable diseases.
Conclusions
In sum, we propose implementing the following policy advancements: 1) shifting agricultural subsidies towards fruits and vegetables, 2) revamping NSLP, SNAP, and WIC to focus on providing plant-based options to the individuals who utilize these programs, and 3) creating comprehensive public initiatives to improve our national advertising and dietary culture. Overall, reorienting federal funding to address these factors could reduce billions of dollars of healthcare spending downstream. If we want to prevent the chronic diseases that plague our nation, it begins with addressing foundational inequities engendered by our agricultural, legislative, and social systems.
Author contributions
All authors contributed to the conceptualization, preparation of the original draft, editing of the manuscript, and provided final review of the manuscript.
Funding
Dr. Michos is supported by the Amato Fund in Women's Cardiovascular Health Research at Johns Hopkins University.
Note
Given her role as Co-editor in Chief, Dr. Erin D. Michos had no involvement in the peer-review of this article and has no access to information regarding its peer-review. Full responsibility for the editorial process for this article was delegated to Dr. Nathan D. Wong.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: R.J.O.: Research Grants: Purjes Foundation, Greenbaum Foundation. Consultant: BrightPlate. Non-compensated: Scientific Advisory Board, Physicians Committee for Responsible Medicine. Board Member, Center for Nutrition Studies. E.D.M.: Advisory boards: Esperion, Amarin, Novartis, and Astra Zeneca.
Acknowledgements
G.R. would like to thank Dr. Alexis C. Wood, Dr. Nigel Crawford, and Dr. Weena Joshi for their advice and support.
Contributor Information
Gautam Ramesh, Email: gramesh@health.ucsd.edu.
Robert J. Ostfeld, Email: rostfeld@montefiore.org.
Erin D. Michos, Email: edonnell@jhmi.edu.
References
- 1.Yusuf S., Hawken S., Ounpuu S., et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 2.O'Donnell M.J., Xavier D., Liu L., et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–123. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 3.Arnett D.K., Blumenthal R.S., Albert M.A., et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2019;74:1376–1414. doi: 10.1016/j.jacc.2019.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilt T.J., Bloomfield H.E., MacDonald R., et al. Effectiveness of statin therapy in adults with coronary heart disease. Arch Intern Med. 2004;164:1427–1436. doi: 10.1001/archinte.164.13.1427. [DOI] [PubMed] [Google Scholar]
- 5.Cholesterol Treatment Trialists Collaboration. Fulcher J., O'Connell R., et al. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet. 2015;385:1397–1405. doi: 10.1016/S0140-6736(14)61368-4. [DOI] [PubMed] [Google Scholar]
- 6.Blood Pressure Lowering Treatment Trialists Collaboration Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet. 2021;397:1625–1636. doi: 10.1016/S0140-6736(21)00590-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ford E.S., Bergmann M.M., Kroger J., Schienkiewitz A., Weikert C., Boeing H. Healthy living is the best revenge: findings from the European Prospective Investigation Into Cancer and Nutrition-Potsdam study. Arch Intern Med. 2009;169:1355–1362. doi: 10.1001/archinternmed.2009.237. [DOI] [PubMed] [Google Scholar]
- 8.Virani S.S., Alonso A., Aparicio H.J., et al. Heart Disease and Stroke Statistics-2021 Update: a Report From the American Heart Association. Circulation. 2021;143:e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Health and Economic Costs of Chronic Diseases. https://www.cdc.gov/chronicdisease/about/costs/index.htm [Accessed July 18, 2021 ].
- 10.Mannoh I., Hussien M., Commodore-Mensah Y., Michos E.D. Impact of social determinants of health on cardiovascular disease prevention. Curr Opin Cardiol. 2021 Sep 1;36(5):572–579. doi: 10.1097/HCO.0000000000000893. [DOI] [PubMed] [Google Scholar]
- 11.Willett W., Rockstrom J., Loken B., et al. Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet. 2019;393:447–492. doi: 10.1016/S0140-6736(18)31788-4. [DOI] [PubMed] [Google Scholar]
- 12.Miller V., Mente A., Dehghan M., et al. Fruit, vegetable, and legume intake, and cardiovascular disease and deaths in 18 countries (PURE): a prospective cohort study. Lancet. 2017;390:2037–2049. doi: 10.1016/S0140-6736(17)32253-5. [DOI] [PubMed] [Google Scholar]
- 13.Krebs-Smith S.M., Guenther P.M., Subar A.F., Kirkpatrick S.I., Dodd K.W. Americans do not meet federal dietary recommendations. J Nutr. 2010;140:1832–1838. doi: 10.3945/jn.110.124826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Engler-Stringer R., Fuller D., Abeykoon A.M.H., Olauson C., Muhajarine N. An examination of failed grocery store interventions in former food deserts. Health Educ Behav. 2019;46:749–754. doi: 10.1177/1090198119853009. [DOI] [PubMed] [Google Scholar]
- 15.Cooksey-Stowers K., Schwartz M.B., Brownell K.D. Food swamps predict obesity rates better than food deserts in the United States. Int J Environ Res Public Health. 2017:14. doi: 10.3390/ijerph14111366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braveman P., Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. 2014;129(Suppl 2):19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dhurandhar E.J. The food-insecurity obesity paradox: a resource scarcity hypothesis. Physiol Behav. 2016;162:88–92. doi: 10.1016/j.physbeh.2016.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wallinga D. Agricultural policy and childhood obesity: a food systems and public health commentary. Health Aff. 2010;29:405–410. doi: 10.1377/hlthaff.2010.0102. [DOI] [PubMed] [Google Scholar]
- 19.Allcott H., Diamond R., Dubé J.-.P., Handbury J., Rahkovsky I., Schnell M. Food deserts and the causes of nutritional inequality. Q J Econ. 2019;134:1793–1844. [Google Scholar]
- 20.Gundersen C., Ziliak J.P. Food insecurity and health outcomes. Health Aff. 2015;34:1830–1839. doi: 10.1377/hlthaff.2015.0645. [DOI] [PubMed] [Google Scholar]
- 21.Decker D., Flynn M. Food insecurity and chronic disease: addressing food access as a healthcare issue. R I Med J. 2018;101:28–30. [PubMed] [Google Scholar]
- 22.Penalvo J.L., Cudhea F., Micha R., et al. The potential impact of food taxes and subsidies on cardiovascular disease and diabetes burden and disparities in the United States. BMC Med. 2017;15:208. doi: 10.1186/s12916-017-0971-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Batis C., Rivera J.A., Popkin B.M., Taillie L.S. First-year evaluation of mexico's tax on nonessential energy-dense foods: an observational study. PLoS Med. 2016;13 doi: 10.1371/journal.pmed.1002057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glanz K., Basil M., Maibach E., Goldberg J., Snyder D. Why Americans eat what they do: taste, nutrition, cost, convenience, and weight control concerns as influences on food consumption. J Am Diet Assoc. 1998;98:1118–1126. doi: 10.1016/S0002-8223(98)00260-0. [DOI] [PubMed] [Google Scholar]
- 25.Franck C., Grandi S.M., Eisenberg M.J. Agricultural subsidies and the American obesity epidemic. Am J Prev Med. 2013;45:327–333. doi: 10.1016/j.amepre.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 26.Norwood F.B., Oltenacu P.A., Calvo-Lorenzo M.S., Lancaster S. Oxford University Press; 2015. Agricultural and food controversies: what everyone needs to know. [Google Scholar]
- 27.Environmental Working Group . News Release—Taxpayers Paid $6.1 Million in Farm Subsidies to Members of Congress, Families [webpage] June 28, 2012. https://www.ewg.org/news-insights/news-release/taxpayers-paid-61-million-farm-subsidies-members-congress-families Accessed Aug 23, 2021 at. [Google Scholar]
- 28.EWG's Farm Subsidy Database. The United States Farm Subsidy Information. https://farm.ewg.org/region.php?fips=00000 [accessed July 18, 2021 ].
- 29.http://www.greyclark.com/wp-content/uploads/2018/02/US-Subsidies-Post-2014-Farm-Bill-FEB-2018.pdf [Accessed July 18, 2021].
- 30.USDA Food and Nutrition Service. Agriculture and Consumer Protection Act of 1973. https://www.fns.usda.gov/agriculture-and-consumer-protection-act-1973 [Accessed July 18, 2021 ].
- 31.Siegel K.R., McKeever Bullard K., Imperatore G., et al. Association of Higher Consumption of Foods Derived From Subsidized Commodities With Adverse Cardiometabolic Risk Among US Adults. JAMA Intern Med. 2016;176:1124–1132. doi: 10.1001/jamainternmed.2016.2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Glickman D., Veneman A.M. The essential role of food and farm policy in improving health. Health Aff. 2013;32:1519–1521. doi: 10.1377/hlthaff.2013.0857. [DOI] [PubMed] [Google Scholar]
- 33.Herman J. Saving U.S. dietary advice from conflicts of interest. Food Drug Law J. 2010;65:285–316. ii. [PubMed] [Google Scholar]
- 34.Nestle M., Jacobson M.F. Halting the obesity epidemic: a public health policy approach. Public Health Rep. 2000;115:12–24. doi: 10.1093/phr/115.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harris J., Frazier W., Kumanyika S., Ramirez A. Increasing disparities in unhealthy food advertising targeted to Hispanic and Black youth. 2019. http://uconnruddcenter.org/files/Pdfs/TargetedMarketingReport2019.pdf [Accessed July 18, 2021].
- 36.Fischer N.M., Duffy E.Y., Michos E.D. Protecting Our Youth: support Policy to Combat Health Disparities Fueled by Targeted Food Advertising. J Am Heart Assoc. 2021;10 doi: 10.1161/JAHA.120.018900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.James P. All-of-government approach needed to tackle obesity. Interview by Fiona Fleck. Bull World Health Organ. 2013;91:551–552. doi: 10.2471/BLT.13.030813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Powell L.M., Szczypka G., Chaloupka F.J. Trends in exposure to television food advertisements among children and adolescents in the United States. Arch Pediatr Adolesc Med. 2010;164:794–802. doi: 10.1001/archpediatrics.2010.139. [DOI] [PubMed] [Google Scholar]
- 39.Cairns G., Angus K., Hastings G., Caraher M. Systematic reviews of the evidence on the nature, extent and effects of food marketing to children. A retrospective summary. Appetite. 2013;62:209–215. doi: 10.1016/j.appet.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 40.Harris J.L., Pomeranz J.L., Lobstein T., Brownell K.D. A crisis in the marketplace: how food marketing contributes to childhood obesity and what can be done. Annu Rev Public Health. 2009;30:211–225. doi: 10.1146/annurev.publhealth.031308.100304. [DOI] [PubMed] [Google Scholar]
- 41.Cervi M.M., Agurs-Collins T., Dwyer L.A., Thai C.L., Moser R.P., Nebeling L.C. Susceptibility to food advertisements and sugar-sweetened beverage intake in non-hispanic black and non-hispanic white adolescents. J Community Health. 2017;42:748–756. doi: 10.1007/s10900-016-0313-4. [DOI] [PubMed] [Google Scholar]
- 42.Zimmerman F.J., Shimoga S.V. The effects of food advertising and cognitive load on food choices. BMC Public Health. 2014;14:342. doi: 10.1186/1471-2458-14-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ventura A.K., Worobey J. Early influences on the development of food preferences. Curr Biol. 2013;23:R401–R408. doi: 10.1016/j.cub.2013.02.037. [DOI] [PubMed] [Google Scholar]
- 44.Mills S., White M., Brown H., et al. Health and social determinants and outcomes of home cooking: a systematic review of observational studies. Appetite. 2017;111:116–134. doi: 10.1016/j.appet.2016.12.022. [DOI] [PubMed] [Google Scholar]
- 45.Boswell R.G., Kober H. Food cue reactivity and craving predict eating and weight gain: a meta-analytic review. Obes Rev. 2016;17:159–177. doi: 10.1111/obr.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nestle M. Interview with Marion Nestle. Health Promot Pract. 2008;9:16–18. doi: 10.1177/1524839907310527. [DOI] [PubMed] [Google Scholar]
- 47.Cohen D.A., Lesser L.I. Obesity prevention at the point of purchase. Obes Rev. 2016;17:389–396. doi: 10.1111/obr.12387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Latimer L.A., Pasch K.E., Bartholomew J.B. Elementary school lunch categorisation and correlations with dietitian recommendations. Perspect Public Health. 2016;136:43–49. doi: 10.1177/1757913915581184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bundy D.A., Drake L.J., Burbano C. School food, politics and child health. Public Health Nutr. 2013;16:1012–1019. doi: 10.1017/S1368980012004661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cohen J.F., Gorski M.T., Hoffman J.A., et al. Healthier standards for school meals and snacks: impact on school food revenues and lunch participation rates. Am J Prev Med. 2016;51:485–492. doi: 10.1016/j.amepre.2016.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Graziose M.M., Koch P.A., Wang Y.C., Lee Gray H., Contento I.R. Cost-effectiveness of a nutrition education curriculum intervention in elementary schools. J Nutr Educ Behav. 2017;49 doi: 10.1016/j.jneb.2016.10.006. 684-691 e681. [DOI] [PubMed] [Google Scholar]
- 52.Macknin M., Stegmeier N., Thomas A., et al. Three healthy eating patterns and cardiovascular disease risk markers in 9 to 18 year olds with body mass index >95%: a randomized trial. Clin Pediatr. 2021;60:474–484. doi: 10.1177/00099228211044841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pekka P., Pirjo P., Ulla U. Influencing public nutrition for non-communicable disease prevention: from community intervention to national programme–experiences from Finland. Public Health Nutr. 2002;5:245–251. [PubMed] [Google Scholar]