Highlights
-
•
Low income individuals are less likely to receive smoking cessation counseling.
-
•
Low income individuals are less likely to have their blood pressure checked.
-
•
Low income individuals are less likely to be receive exercise counseling.
-
•
Low income individuals are less likely to receive dietary counseling.
-
•
Low income individuals are less likely to have their cholesterol levels checked.
Keywords: Income, Socioeconomic, Disparity, Prevention
Abstract
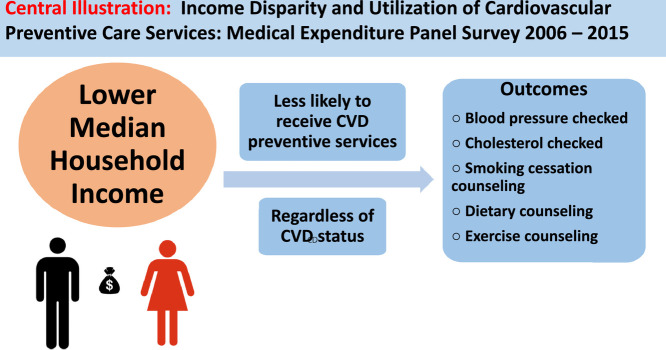
Objective
: Associations between income disparity and utilization of cardiovascular disease (CVD) preventive care services, such as receipt of lifestyle advice and screening for CVD risk factors in populations with and without CVD, are not well understood. The purpose of this study was to evaluate associations between income and utilization of CVD-preventive services among U.S. adults.
Methods
: We included adults ≥18 years with and without CVD from the 2006 to 2015 Medical Expenditure Panel Survey. We categorized participants as high-income (>400% of federal poverty level [FPL]), middle income (200–400% of FPL), low-income (125–200% of FPL) and very low (VL)-income (<125% of FPL). We used logistic regression to compare the likelihood of receiving CVD-preventive services by income strata, adjusting for sociodemographic factors and comorbidities.
Results
: The study included 185,081 participants (representing 194.6 million U.S. adults) without CVD, and 32,862 participants (representing 37 million U.S. adults) with CVD. VL-income adults without CVD were less likely than high-income adults to have blood pressure measured within past 2 years [odds ratio [OR] 0.41 (95% confidence interval [CI] 0.37–0.45)] or cholesterol levels checked within past 5 years [0.36 (0.33–0.38)] or receive counseling about diet modifications [0.77 (0.74–0.81)], exercise [0.81 (0.77–0.85)], or smoking cessation [0.71 (0.63–0.79)] within past year. VL-income adults with CVD were also less likely to have blood pressure [0.32 (0.22–0.46)] or cholesterol [0.33 (0.26–0.42)] checked and receive counseling about exercise [0.84 (0.76–0.93)] or smoking cessation [0.78 (0.61–0.99)]. Additional subgroup analyses restricted to participants who had seen a healthcare provider within the preceding 12 months, as well as secondary analyses stratified by sex, race and ethnicity, showed similar disparities between high-income and VL-income participants.
Conclusions
: VL-income adults were less likely to be screened for CVD risk factors or receive CVD-prevention counseling than high-income adults, regardless of CVD status. More work must be done to reduce disparities in access to and utilization of CVD-preventive services among adults in different income groups.
Graphical abstract
Abbreviations
- SES
socioeconomic status
- CVD
cardiovascular disease
- MEPS
Medical Expenditure Panel Survey
- FPL
federal poverty level
- VL
very low
1. Introduction
Socioeconomic status (SES)–often measured using individual income level, individual educational level attained, individual employment status, or neighborhood-level socioeconomic characteristics–is a social determinant of health associated with cardiovascular disease (CVD) [1,2]. Lower individual and neighborhood-level SES are associated with an increased incidence and prevalence of CVD, including coronary heart disease, heart failure and stroke [1,[3], [4], [5], [6]]. Individuals of lower SES have worse cardiovascular outcomes, such as CVD-related mortality [7]. Additionally, lower SES has been associated with increased prevalence of risk factors, such as hypertension, hyperlipidemia, obesity, smoking and physical activity [8], [9], [10], [11], [12].
Modifiable CVD risk factors are associated with worse cardiovascular outcomes such as myocardial infarction, stroke, heart failure and death. One way to reduce morbidity and mortality from CVD may be to prevent CVD altogether or prevent its progression by providing preventive care services, such as lifestyle counseling (i.e., smoking cessation, physical activity, dietary management) and screening for risk factors (i.e., hypertension and hyperlipidemia) to reduce CVD risk. However, while lower SES has been associated with lower utilization of some preventive care services, the relationship between SES and utilization of preventive services with a focus on CVD prevention is less well understood, especially in a representative sample of the United States (U.S.) population [13]. Furthermore, whether this relationship varies depending on an individual's preexisting CVD status is also unknown.
Therefore, we examined the relationship between SES and utilization of CVD risk-related preventive care services, hypothesizing that SES would be directly associated with utilization of these services in people without CVD, but not as much as those with CVD. Using data from a nationally representative U.S. sample and household income as a proxy for SES, we compared utilization of CVD preventive care services among people with and without an existing diagnosis of CVD and at varying income levels. Elucidating socioeconomic disparities in the utilization of CVD preventive care services may aid in the future development of interventions to decrease disparities in access to health care and improve cardiovascular outcomes for people with lower SES.
2. Methods
2.1. Data source and study design
We used data from the Medical Expenditure Panel Survey (MEPS) to conduct this retrospective observational study. MEPS is a nationwide series of surveys of individuals and families, physicians, hospitals, pharmacies and employers, conducted by the Agency for Healthcare Research and Quality [14,15]. Results are reported annually and include information about demographic and socioeconomic characteristics, patients' experiences, medical comorbidities, prescription medications, utilization of healthcare resources, healthcare costs and payment sources. Because person-level weighting and variance estimation were used to account for survey nonresponse and national population characteristics, MEPS offers a nationally representative U.S. sample. More detailed information regarding the MEPS data collection process can be found in other publications [16], [17], [18]. Following Department of Health and Human Services recommendations, our study was exempt from Institutional Review Board review because it employed a publicly accessible and de-identified dataset.
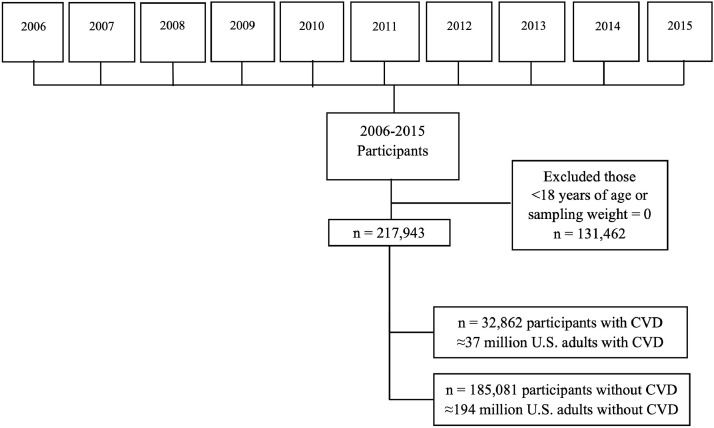
We used MEPS data collected between 2006 and 2015, representing 349,405 participants (Fig. 1). We excluded participants less than 18 years old and those with a sampling weight of zero (to preserve the nationally representative sample). We then divided the population into two groups: individuals without CVD and those with CVD. Individuals with CVD were identified by self-report or International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for the diagnoses of coronary artery disease (ICD-9: 410, 413, and 414), stroke (ICD-9: 433–437), heart failure (ICD-9: 428), cardiac dysrhythmia (ICD-9: 427) or peripheral artery disease (ICD-9: 440, 443, 447).
Fig. 1.
flowchart of participant inclusion process using data from Medical Expenditure Panel Survey (MEPS), 2006 to 2015.
2.2. Study variables
We categorized a participant's SES by using the individual's household income. We classified income into 4 distinct subgroups: [1] high-income if household income was greater than 400% of the federal poverty level (FPL), [2] middle-income if household income was between 200 and 400% of the FPL, [3] low-income if household income was between 125 and 200% of FPL and [4] very low (VL)-income if household income was less than 125% of FPL. Income served as the primary exposure variable.
Other baseline sociodemographic variables and covariates included age (18–39, 40–64, 67–74 or 75+ years old), sex (female or male), race/ethnicity (self-reported non-Hispanic White, Black, Hispanic or Asian adult), geographic region (Northeast, Midwest, South or West), education level attained (less than high school, high school/Graduate Educational Development [GED] or some college or higher), health insurance status (uninsured, private, Medicare or Medicaid), employment status (currently employed including self-employed and part-time employed, currently unemployed, or currently unemployed but employed in last 12 months), marital status (married, separated/divorced or never married), clinician visit within the last 12 months, and modified Charlson Comorbidity Index [19,20] (0, 1, 2 or greater).
2.3. Outcomes
The primary outcomes were utilization of the following CVD risk preventive care services: smoking cessation counseling ("advised to quit smoking", if the participant was a current smoker), blood pressure (BP) measurement ("blood pressure checked within the last two years"), exercise counseling ("advised to exercise more"), dietary counseling ("advised by a healthcare professional to eat fewer high fat/cholesterol foods") and lipid panel testing (cholesterol levels checked within the last five years"). These outcomes were ascertained from the MEPS survey completed annually by the participants. Responses were categorical (yes or no).
2.4. Statistical analysis
We used χ2 tests to compare baseline sociodemographic characteristics of MEPS participants by income group, separating participants into those without CVD and those with CVD. We compared unadjusted rates of utilization of CVD risk-related preventive services across income groups among participants with and without CVD, using χ22 tests, with a p-value <0.05 considered as statistically significant. We then examined the association between income and utilization or receipt of CVD risk preventive services in both participants with and without CVD. For each of the outcomes, we used logistic regression to calculate odds ratios and compare the likelihood of utilizing or receiving CVD risk preventive services among participants in different income groups, with the high-income group serving as the reference group. We adjusted for age, race/ethnicity, sex, region, health insurance, educational status and Charlson Comorbidity Index in our models. To account for possible variation in participant adherence to visits with primary healthcare providers, we conducted subgroup analyses of participants with and without CVD, restricted to only those who had visited their healthcare provider at least once within the 12 months prior to the survey. We also conducted further secondary analyses comparing the likelihood of utilization of CVD risk preventive services by income level, stratified by sex (male and female), race (non-Hispanic White, Black and Asian) and ethnicity (Hispanic) participants; models for these subgroup analyses were not adjusted for additional variables. Analyses were conducted using Stata, version 14 (StataCorp, College Station, TX), incorporating variance estimation and person-level weights to maintain the nationally representative study sample.
3. Results
3.1. Study demographics
The MEPS sample from 2006 to 2015 included 349,405 individuals. After exclusion of individuals younger than 18 and those with a person-weight of zero, there were 185,081 participants (representing 194 million U.S. adults) without CVD and 32,862 participants (representing 37 million U.S. adults) with CVD in our study sample (Fig. 1). Baseline characteristics for participants without and with CVD, respectively, are shown in Tables 1a-b. Among participants without CVD, there were fewer participants in the lower income groups (VL-income, low-income) than in the high-income group. Low- and VL-income individuals were younger and were more likely to be male, Black or Hispanic adults, or from the South region of U.S. than high-income individuals. Low- and VL-income participants were also more frequently uninsured, on Medicaid, unmarried, unemployed, and had attained lower levels of education than high-income participants. Among participants with CVD, there were again fewer participants in the lower income groups than in the high-income group. Compared to high-income participants, VL-income individuals were also more likely to be younger, male, Black or Hispanic adults, from the South, uninsured or on Medicaid, unmarried, unemployed, and had attained lower levels of education. VL-income participants also had more comorbidities and were less likely to attend regular clinician visits, regardless of CVD status.
Table 1a.
Weighted baseline characteristics of MEPS participants without CVD between 2006 and 2015, categorized by level of income.
| Characteristic | High-incomeaN or weighted% | Middle-incomeaN or weighted% | Low-incomeaN or weighted% | VL-incomeaN or weighted% | P-value |
|---|---|---|---|---|---|
| Total participants | 75,883 | 57,375 | 24,060 | 27,762 | |
| Weighted sample | 79.8 million | 60.3 million | 25.3 million | 29.2 million | |
| Age groups (years) | |||||
| 18–39 | 35.4 | 47.1 | 48.7 | 54.4 | <0.001 |
| 40–64 | 52.2 | 41.3 | 35.6 | 34.1 | |
| 65–74 | 8.9 | 6.9 | 8.3 | 5.9 | |
| ≥75 | 3.5 | 4.7 | 7.4 | 5.6 | |
| Sex | |||||
| Female | 50.8 | 48.9 | 46.4 | 42.1 | <0.001 |
| Male | 49.2 | 51.1 | 53.6 | 57.9 | |
| Race/ethnicity | |||||
| Non-Hispanic White | 77.7 | 65.3 | 53.8 | 47.4 | <0.001 |
| Black | 7.4 | 12.4 | 15.2 | 20.6 | |
| Asian | 6.9 | 5.0 | 5.0 | 4.8 | |
| Hispanic | 8.0 | 17.3 | 26.0 | 27.2 | |
| Region | |||||
| Northeast | 21.0 | 16.6 | 16.1 | 16.2 | <0.001 |
| Midwest | 21.7 | 22.5 | 19.4 | 19.2 | |
| South | 33.4 | 37.6 | 39.3 | 40.4 | |
| West | 23.9 | 23.3 | 25.2 | 24.2 | |
| Education | |||||
| Less than high school | 6.5 | 17.0 | 28.3 | 37.7 | <0.001 |
| High school/GED | 54.2 | 57.6 | 53.5 | 47.4 | |
| Some college or higher | 39.3 | 25.4 | 18.2 | 14.9 | |
| Insurance status | |||||
| Uninsured | 5.9 | 16.2 | 28.5 | 33.6 | <0.001 |
| Private | 84.1 | 69.5 | 43.5 | 22.9 | |
| Medicaid | 1.1 | 4.7 | 13.6 | 31.3 | |
| Medicare | 8.9 | 9.6 | 14.4 | 12.2 | |
| Employment status | |||||
| Currently unemployed | 18.5 | 23.4 | 34.0 | 52.5 | <0.001 |
| Currently employed | 78.6 | 73.1 | 61.2 | 41.8 | |
| Currently unemployed butemployed in past 12 months | 2.9 | 3.5 | 4.8 | 5.7 | |
| Marital status | |||||
| Married | 66.0 | 52.1 | 43.9 | 31.9 | <0.001 |
| Divorced | 12.1 | 18.3 | 22.5 | 24.4 | |
| Never married | 21.9 | 29.6 | 33.6 | 43.7 | |
| Charlson comorbidity index | |||||
| 0 | 87.2 | 87.3 | 86.3 | 84.6 | <0.001 |
| 1 | 9.4 | 9.9 | 10.3 | 12.2 | |
| ≥2 | 3.4 | 2.8 | 3.4 | 3.2 | |
| Regular healthcare visit | |||||
| Yes | 81.3 | 72.7 | 65.7 | 63.0 | <0.001 |
| No | 18.7 | 27.3 | 34.4 | 37.0 | |
Abbreviations: MEPS, Medical Expenditure Panel Survey; CVD, cardiovascular disease; VL, very low; N, number of participants.
Income level is one's household income, given as proportion of federal poverty level (FPL): high-income (≥400% FPL), middle-income (200 to <400% FPL), low-income (125 to <200% FPL), very low-income (<125% FPL).
Table 1b.
Baseline characteristics MEPS participants with CVD between 2006 and 2015 across income strata.
| Characteristic | High-incomeaN or weighted% | Middle-incomeaN or weighted% | Low-incomeaN or weighted% | VL-incomeaN or weighted% | P-value |
|---|---|---|---|---|---|
| Total participants | 11,830 | 9530 | 5258 | 6244 | |
| Weighted sample | 13.3 million | 10.7 million | 5.9 million | 7.1 million | |
| Age groups (years) | |||||
| 18–39 | 9.8 | 11.4 | 11.0 | 15.3 | <0.001 |
| 40–64 | 44.8 | 38.1 | 31.3 | 42.6 | |
| 65–74 | 25.4 | 22.2 | 23.1 | 18.3 | |
| ≥75 | 20.0 | 28.3 | 34.6 | 23.8 | |
| Sex | |||||
| Female | 54.6 | 48.9 | 43.0 | 40.0 | <0.001 |
| Male | 45.4 | 51.1 | 57.0 | 60.0 | |
| Race/ethnicity | |||||
| Non-Hispanic white | 86.6 | 78.9 | 75.4 | 65.1 | <0.001 |
| Black | 6.5 | 10.0 | 12.4 | 18.9 | |
| Asian | 2.6 | 2.3 | 2.0 | 2.7 | |
| Hispanic | 4.3 | 8.8 | 10.2 | 13.3 | |
| Region | |||||
| Northeast | 20.3 | 17.9 | 15.9 | 17.1 | <0.001 |
| Midwest | 23.3 | 24.4 | 22.5 | 22.0 | |
| South | 34.8 | 39.1 | 42.2 | 42.1 | |
| West | 21.6 | 18.6 | 19.4 | 18.8 | |
| Education | |||||
| Less than high school | 7.2 | 20.0 | 30.0 | 40.2 | <0.001 |
| High school/GED | 54.6 | 57.2 | 52.5 | 45.1 | |
| Some college or higher | 38.2 | 22.8 | 17.5 | 14.7 | |
| Insurance status | |||||
| Uninsured | 2.7 | 6.6 | 9.4 | 12.3 | <0.001 |
| Private | 57.1 | 40.8 | 21.3 | 12.1 | |
| Medicaid | 1.3 | 6.1 | 13.0 | 32.0 | |
| Medicare | 38.9 | 46.5 | 56.3 | 43.6 | |
| Employment status | |||||
| Currently unemployed | 43.9 | 59.2 | 74.8 | 83.5 | <0.001 |
| Currently employed | 53.7 | 38.3 | 22.8 | 14.0 | |
| Currently unemployed butemployed in past 12 months | 2.4 | 2.5 | 2.4 | 2.5 | |
| Marital status | |||||
| Married | 71.2 | 55.6 | 43.7 | 30.4 | <0.001 |
| Divorced | 20.7 | 33.5 | 44.3 | 49.9 | |
| Never married | 8.1 | 10.9 | 12.0 | 19.7 | |
| Charlson comorbidity index | |||||
| 0 | 61.5 | 55.2 | 49.7 | 46.8 | <0.001 |
| 1 | 25.4 | 28.7 | 32.7 | 32.8 | |
| ≥2 | 13.1 | 16.1 | 17.6 | 20.4 | |
| Regular healthcare visit | |||||
| Yes | 92.7 | 91.0 | 88.5 | 86.4 | <0.001 |
| No | 7.4 | 9.0 | 11.5 | 13.6 | |
See Footnotes for Table 1a.
3.2. Primary outcomes
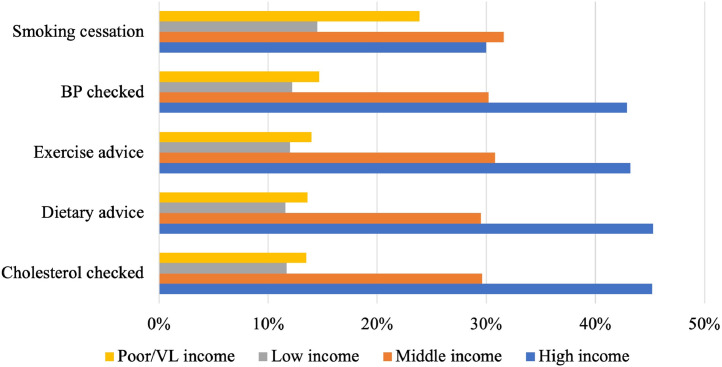
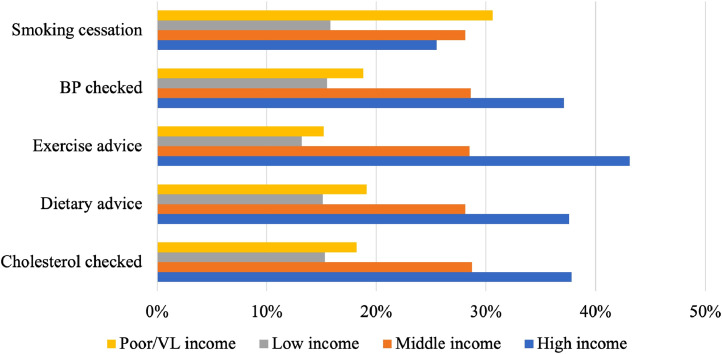
Among participants without CVD, low- and VL-income participants experienced lower unadjusted rates of smoking cessation counseling, BP measurement within the last two years, exercise counseling, dietary counseling and lipid panel measurement within the last two years than high-income participants (Fig. 2a, Supplemental Table S1a). Among participants with CVD, low- and VL-income participants experienced lower unadjusted rates of BP measurement, exercise counseling, dietary counseling, and lipid panel testing than their high-income counterparts; low-income but not VL-income participants received smoking cessation counseling less frequently (Fig. 2b, Supplemental Table S1b).
Fig. 2a.
Unadjusted utilization rates of CVD risk preventive services among MEPS participants without CVD between 2006 and 2015, based on level of income.
Fig. 2b.
Unadjusted utilization rates of CVD risk preventive services among MEPS participants with CVD between 2006 and 2015, based on level of income.
After adjusting for age, race/ethnicity, sex, region, health insurance, educational status and comorbidity index, low- and VL-income participants without CVD were significantly less likely to receive CVD risk preventive services than their high-income counterparts (Table 2a). Low- and VL-income participants who smoked were less likely to be advised to quit smoking than high-income participants [OR 0.70 (95% CI, 0.62–0.79) and OR 0.71 (0.63–0.79), respectively]. Low- and VL-income participants were less likely to have had their BP measured within the last 2 years [OR 0.45 (0.42–0.49) and OR 0.41 (0.37–0.45), respectively]. Low- and VL-income participants were less likely to receive exercise counseling [OR 0.79 (0.75–0.84) and OR 0.81 (0.77–0.85), respectively]. Low- and VL-income participants were less likely to receive dietary counseling [OR 0.77 (0.73–0.81) and OR 0.77 (0.74–0.81), respectively]. Low- and VL-income participants were less likely to have had their cholesterol checked within the last 5 years [OR 0.42 (0.39–0.45) and OR 0.36 (0.33–0.38), respectively].
Table 2a.
Association between income and utilization of CVD risk preventive services among MEPS participants without CVD, based on level of income.
| Preventive Service | High-incomea | Middle-incomeaORb,c (95% CI) | Low-incomeaORb,c (95% CI) | VL-incomeaORb,c (95% CI) |
|---|---|---|---|---|
| Advised to quit smoking (current smokers) | 1 (Ref) | 0.81 (0.72–0.91)* | 0.70 (0.62–0.79)* | 0.71 (0.63–0.79)* |
| Blood pressure checked within the last 2 years | 1 (Ref) | 0.61 (0.57–0.66)* | 0.45 (0.42–0.49)* | 0.41 (0.37–0.45)* |
| Advised to exercise more | 1 (Ref) | 0.92 (0.88–0.96)* | 0.79 (0.75–0.84)* | 0.81 (0.77–0.85)* |
| Advised by a healthcare professional toeat fewer high fat/cholesterol foods | 1 (Ref) | 0.89 (0.86–0.93)* | 0.77 (0.73–0.81)* | 0.77 (0.74–0.81)* |
| Cholesterol levels checked within last 5 years | 1 (Ref) | 0.60 (0.56–0.64)* | 0.42 (0.39–0.45)* | 0.36 (0.33–0.38)* |
Abbreviations: CVD, cardiovascular disease; MEPS, Medical Expenditure Panel Survey; VL, very low; OR, odds ratio; CI, confidence interval.
Income level is one's household income, given as proportion of federal poverty level (FPL): high-income (≥400% FPL), middle-income (200 to <400% FPL), low-income (125 to <200% FPL), very low-income (<125% FPL).
OR models adjust for age, race/ethnicity, sex, region, health insurance, educational status, Charlson Comorbidity Index; the high-income group serves as the reference group.
OR <1 indicates a group is less likely to receive a CVD risk preventive service.
Indicates statistically significant results (p<0.05).
After making the same adjustments as above, low- and VL-income participants with CVD were also significantly less likely to receive CVD preventive services than their high-income counterparts (Table 2b). Low- and VL-income participants who smoked were less likely to be advised to quit smoking than high-income participants [OR 0.64 (0.48–0.86) and OR 0.78 (0.61–0.99), respectively]. Low- and VL-income participants were less likely to have had their BP measured within the last 2 years [OR 0.34 (0.24–0.49) and OR 0.32 (0.22–0.46), respectively]. Low- and VL-income participants were less likely to receive exercise counseling [OR 0.79 (0.71–0.87) and OR 0.84 (0.76–0.93), respectively]. Low-income (but not VL-income) participants were less likely to receive dietary counseling [OR 0.84 (0.76–0.93) and OR 0.95 (0.86–1.04)]. Low- and VL-income participants were less likely to have had their cholesterol checked within the last 5 years [OR 0.34 (0.28–0.42) and OR 0.33 (0.26–0.42), respectively].
Table 2b.
Association between income and utilization of CVD risk preventive services among MEPS participants with CVD, based on level of income.
| Preventive Service | High-incomea | Middle-incomeaORb,c (95% CI) | Low-incomeaORb,c (95% CI) | VL-incomeaORb,c (95% CI) |
|---|---|---|---|---|
| Advised to quit smoking (current smokers) | 1 (Ref) | 0.97 (0.74–1.27) | 0.64 (0.48–0.86)* | 0.78 (0.61–0.99)* |
| Blood pressure checked within the last 2 years | 1 (Ref) | 0.45 (0.32–0.63)* | 0.34 (0.24–0.49)* | 0.32 (0.22–0.46)* |
| Advised to exercise more | 1 (Ref) | 0.89 (0.82–0.97)* | 0.79 (0.71–0.87)* | 0.84 (0.76–0.93)* |
| Advised by a healthcare professional toeat fewer high fat/cholesterol foods | 1 (Ref) | 0.87 (0.80–0.95)* | 0.84 (0.76–0.93)* | 0.95 (0.86–1.04) |
| Cholesterol levels checked within last 5 years | 1 (Ref) | 0.50 (0.41–0.61)* | 0.34 (0.28–0.42)* | 0.33 (0.26–0.42)* |
Abbreviations: CVD, cardiovascular disease; MEPS, Medical Expenditure Panel Survey; VL, very low; OR, odds ratio; CI, confidence interval.
Income level is one's household income, given as proportion of federal poverty level (FPL): high-income (≥400% FPL), middle-income (200 to <400% FPL), low-income (125 to <200% FPL), very low-income (<125% FPL).
OR models adjust for age, race/ethnicity, sex, region, health insurance, educational status, Charlson Comorbidity Index; the high-income group serves as the reference group.
OR <1 indicates a group is less likely to receive a CVD risk preventive service.
Indicates statistically significant results (p<0.05).
3.3. Subgroup analyses
In our subgroup analysis restricted to only individuals without CVD who visited their healthcare provider at least once within the 12 months prior to the survey, results were mostly similar (Table 3a). Low- and VL-income participants who smoked trended less likely to receive smoking cessation counseling than their high-income counterparts, though results were not statistically significant [OR 0.85 (0.73–1.00) and OR 0.87 (0.75–1.01), respectively]. Low- and VL-income participants were less likely to have had their BP measured within the last 2 years [OR 0.65 (0.56–0.75) and OR 0.65 (0.56–0.77), respectively]. Low- and VL-income participants were less likely to receive exercise counseling [OR 0.82 (0.77–0.88) and OR 0.80 (0.75–0.85), respectively]. Low- and VL-income participants were less likely to receive dietary counseling [OR 0.90 (0.85–0.96) and OR 0.87 (0.82–0.93), respectively]. Low- and VL-income participants were less likely to have had their cholesterol checked within the last 5 years [OR 0.57 (0.52–0.62) and OR 0.55 (0.50–0.61), respectively].
Table 3a.
Association between income and utilization of CVD risk preventive services among participants without CVD, restricted to those who visited a provider within past year.
| Preventive Service | High-incomea | Middle-incomeaORb,c (95% CI) | Low-incomeaORb,c (95% CI) | VL-incomeaORb,c (95% CI) |
|---|---|---|---|---|
| Advised to quit smoking (current smokers) | 1 (Ref) | 0.93 (0.81–1.07) | 0.85 (0.73–1.00) | 0.87 (0.75–1.01) |
| Blood pressure checked within the last 2 years | 1 (Ref) | 0.68 (0.60–0.76)* | 0.65 (0.56–0.75)* | 0.65 (0.56–0.77)* |
| Advised to exercise more | 1 (Ref) | 0.91 (0.87–0.95)* | 0.82 (0.77–0.88)* | 0.80 (0.75–0.85)* |
| Advised by a healthcare professional to eatfewer high fat/cholesterol foods | 1 (Ref) | 0.96 (0.92–1.00) | 0.90 (0.85–0.96)* | 0.87 (0.82–0.93)* |
| Cholesterol levels checked within last 5 years | 1 (Ref) | 0.69 (0.64–0.74)* | 0.57 (0.52–0.62)* | 0.55 (0.50–0.61)* |
Abbreviations: CVD, cardiovascular disease; MEPS, Medical Expenditure Panel Survey; VL, very low; OR, odds ratio; CI, confidence interval.
Income level is one's household income, given as proportion of federal poverty level (FPL): high-income (≥400% FPL), middle-income (200 to <400% FPL), low-income (125 to <200% FPL), very low-income (<125% FPL).
OR models adjust for age, race/ethnicity, sex, region, health insurance, educational status, Charlson Comorbidity Index; the high-income group serves as the reference group.
OR <1 indicates a group is less likely to receive a CVD risk preventive service.
Indicates statistically significant results (p<0.05).
In the subgroup analysis restricted to individuals with CVD who visited their healthcare provider at least once within the 12 months prior to the survey, results were similar, though some were no longer statistically significant (Table 3b). Low- and VL-income participants who smoked trended less likely to receive smoking cessation counseling than their high-income counterparts, though results were not statistically significant [OR 0.74 (0.53–1.04) and OR 0.87 (0.61–1.26), respectively]. Low- and VL-income participants were less likely to have had their BP measured within the last 2 years [OR 0.45 (0.26–0.77) and OR 0.47 (0.27–0.82), respectively]. Low- and VL-income participants were less likely to receive exercise counseling [OR 0.70 (0.62–0.79) and OR 0.67 (0.60–0.74), respectively]. Low- and VL-income participants trended less likely to receive dietary counseling but the results were not statistically significant [OR 0.88 (0.77–1.00) and OR 0.93 (0.82–1.06)]. Low- and VL-income participants were less likely to have had their cholesterol checked within the last 5 years [OR 0.54 (0.40–0.73) and OR 0.44 (0.31–0.61), respectively].
Table 3b.
Association between income and utilization of CVD risk preventive services among participants with CVD, restricted to those who visited a provider within past year.
| Preventive Service | High-incomea | Middle-incomeaORb,c (95% CI) | Low-incomeaORb,c (95% CI) | VL-incomeaORb,c (95% CI) |
|---|---|---|---|---|
| Advised to quit smoking (current smokers) | 1 (Ref) | 1.02 (0.73–1.42) | 0.74 (0.53–1.04) | 0.87 (0.61–1.26) |
| Blood pressure checked within the last 2 years | 1 (Ref) | 0.49 (0.30–0.81)* | 0.45 (0.26–0.77)* | 0.47 (0.27–0.82)* |
| Advised to exercise more | 1 (Ref) | 0.86 (0.78–0.94)* | 0.70 (0.62–0.79)* | 0.67 (0.60–0.74)* |
| Advised by a healthcare professional to eat fewer high fat/cholesterol foods | 1 (Ref) | 0.91 (0.82–0.99)* | 0.88 (0.77–1.00) | 0.93 (0.82–1.06) |
| Cholesterol levels checked within last 5 years | 1 (Ref) | 0.55 (0.42–0.72)* | 0.54 (0.40–0.73)* | 0.44 (0.31–0.61)* |
Abbreviations: CVD, cardiovascular disease; MEPS, Medical Expenditure Panel Survey; VL, very low; OR, odds ratio; CI, confidence interval.
Income level is one's household income, given as proportion of federal poverty level (FPL): high-income (≥400% FPL), middle-income (200 to <400% FPL), low-income (125 to <200% FPL), very low-income (<125% FPL).
OR models adjust for age, race/ethnicity, sex, region, health insurance, educational status, Charlson Comorbidity Index; the high-income group serves as the reference group.
OR <1 indicates a group is less likely to receive a CVD risk preventive service.
Indicates statistically significant results (p<0.05).
In the additional analyses stratified by sex, race and ethnicity, results were similar to the primary analyses. Both male and female low and VL-income participants were generally less likely to utilize or receive CVD risk preventive services, compared to high-income participants of the same sex (Tables S2a-S2b). Similarly, regardless of their race (non-Hispanic White, Black or Asian) or ethnicity (Hispanic), low and VL-income participants were less likely to utilize or receive CVD risk preventive services than their high-income counterparts (Tables S3a-S3d).
4. Discussion
In a large, cross-sectional and nationally representative sample of U.S. adults, we observed significant disparity in utilization of CVD risk-related preventive services among participants of differing individual SES. Even after adjusting for baseline demographics, other socioeconomic factors and comorbidities, low-income U.S. adults were less likely to be screened for CVD risk factors (i.e. hypertension, hyperlipidemia) or receive counseling for prevention of CVD (i.e. smoking cessation, exercise counseling, dietary counseling) than high-income adults, regardless of CVD status.
Notably, these disparities persisted in subgroup analyses of individuals who had visited their healthcare provider at least once within the prior 12 months, as well as in secondary analyses stratified by sex, race and ethnicity. These findings highlight striking disparities in provision of CVD risk preventive care. Our findings also suggest that though it is often heavily intertwined with other social determinants of health such as race/ethnicity, education level and insurance status, individual income status may be independently associated with a lower likelihood of utilizing CVD preventive services.
The association between socioeconomic disparity and cardiovascular outcomes is well established. Studies have shown that individuals of lower SES experience worse cardiovascular outcomes and have higher rates of cardiovascular risk factors [5,[21], [22], [23]]. These disparities between socioeconomic classes have only worsened in recent decades [8,24]. Individuals of lower SES have also been shown to be less likely to utilize or receive preventive care services such as cancer screening, vaccinations, eye examinations and dental examinations [13,25]. However, potential differences regarding utilization of specifically CVD risk preventive services among representative socioeconomic populations in the U.S., examining both individuals with and without CVD, are less well understood.
One prior study using data from MEPS found disparities in BP and cholesterol checkups based on age, sex, insurance status, income status and race, but did not assess for other CVD risk preventive services, such as smoking cessation, dietary or exercise counseling, and did not stratify participants based on CVD status [26]. Other studies have shown the disparity in utilization of preventive care services supported by the U.S. Preventive Services Task Force such as BP and cholesterol screening based on insurance status, though not necessarily based on income [27,28]. Insured participants from the 1996 MEPS survey who had a usual source of care were over four times as likely to have their BP or cholesterol checked compared to those who were uninsured and had no usual source of care [28]. This study, however, did not assess for association with other socioeconomic factors such as income, did not assess other CVD preventive factors and did not stratify individuals with and without CVD. Additional studies examining preventive screening for CVD have found that socioeconomically deprived individuals were less likely to receive CVD preventive screening, but these studies were performed in countries outside of the U.S. and also did not stratify individuals based on existing CVD status [29], [30], [31].
The magnitude of the difference in the utilization of CVD preventive services between high- and low-income participants was particularly striking; low- and VL-income participants, both with and without CVD, were 20–70% less likely to receive these services after adjusting for sociodemographic characteristics. Many contributory personal and contextual factors contribute to these disparities, some of which are complex and challenging to measure. There may be individual behavioral factors such as attendance to visits, patient trust in healthcare providers or ability to engage in healthy lifestyle behaviors (e.g., eating healthy foods or exercising), which may be lower in more socioeconomically deprived populations [32], [33], [34]. There may be provider-level factors such as differences in the quality of care that individuals of varying income status receive or lack of available providers in lower-income communities [35,36].
There may be psychosocial factors that affect access to care, such as stress due to poverty, housing insecurity, discrimination, structural racism, and lack of social support [37], [38], [39], [40], [41], [42], [43]. Furthermore, there may be contributing aspects of the physical environment such as distance from a provider, lack of access to grocery stores, lack of public recreation facilities, lack of transportation, lack of neighborhood walkability, lack of neighborhood green spaces or lack of neighborhood safety in low-income neighborhoods [44], [45], [46], [47]. Such factors may decrease socioeconomically disadvantaged people's ability to engage in CVD risk preventive activities. These contextual factors must be further studied to better understand the complex underlying mechanisms mediating the associations observed in this study.
Identifying cardiovascular risk via preventive care services is essential to create optimal and cost-effective behavioral or pharmacologic interventions to reduce CVD burden. These interventions may also ultimately improve quality of life and healthcare experiences, especially in patients with known CVD [48]. Moreover, reducing cardiovascular risk may reduce healthcare expenditures, which may unburden both patients and the U.S. health care system at large [49], [50], [51]. Therefore, targeted interventions to improve utilization of CVD risk preventive services towards populations of lower SES may improve cardiovascular outcomes and reduce healthcare costs.
Still, challenges persist in reducing socioeconomic disparity and its many deleterious downstream effects, including disparities in access to and quality of care between different socioeconomic populations in the U.S [2,52]. This poses challenges in the reduction of disparities in cardiovascular outcomes in all populations. Reducing disparities may require interventions at the individual, healthcare organizational and population level [2,53]. Population-level interventions may have more long-term and far-reaching impact than other interventions, but they are the most controversial. Further discussions are needed at the community, state and federal levels to develop sustainable interventions to address the vast socioeconomic and associated cardiovascular disparities seen in the U.S. population.
4.1. Limitations
There are several limitations to this study. First, since MEPS relies on participant self-report, there may be some recall bias: participants may not accurately recall their experiences and may underestimate their CVD history or misreport their use of services. Second, though our study adjusted for factors such as race/ethnicity, education level and insurance status, these factors are heavily intertwined with income level in characterizing the concept of SES. Third, due to the observational design, we cannot establish causality between income and utilization of CVD risk preventive services. There may be residual confounding due to other unmeasured social determinants of health or clinical comorbidities. Fourth, low-income participants in MEPS were more likely to be Black or Hispanic adults, uninsured and have a lower educational attainment level. There is a longstanding history of socioeconomic and racial inequity in the U.S. [43,54]. We acknowledge that income status alone cannot account for all forms of socioeconomic disparity, and in particular, may not account for structural discrimination and racism that is still prevalent in our society [43].
Notably, a greater share of VL-income participants was in the youngest (18–39 years) age category. It is possible that younger people in general may be less concerned about health and less likely to visit with a provider, which could affect these results. However, we adjusted for age in our analyses and in subgroup analyses restricting to only participants who had seen a provider within the past year, disparities still persisted. Additionally, we noted as well that even among middle and high income participants, when examining the unadjusted data, only 25–45% of people reported receiving CVD risk preventive services such as smoking cessation counseling or having their BP checked. While this could suggest some degree of provider negligence and inertia, we also believe that recall bias likely affects some proportion of participants’ responses.
Moreover, it was notable that VL-income and low-income participants were more likely to live in the South, regardless of participants’ CVD status. It is possible that participants in the South may experience lower cost of living but comparably more expensive or worse access to healthcare; it is also possible that participants in some regions may live in more rural regions than others, thus further impacting their distance to and access to health care resources. We attempted to account for this by adjusting for region in our analyses, but acknowledge that there may be residual confounding that we cannot adjust for due to lack of more granular geographical information about MEPS participants. Finally, given the limitations of the data collection in MEPS, it is difficult to fully adjust for the regularity with which participants visit their doctor. It is possible that low-income populations are less likely to see clinicians and thus less likely to seek CVD risk preventive care services. We attempted to account for this by performing a subgroup analysis of only those who had seen a healthcare provider within the last 12 months. While some findings were no longer statistically significant, results were mostly similar to the overall MEPS population, regardless of CVD status. However, there may still have been additional variation in visit adherence among different income groups.
5. Conclusions
In this large, representative cross-sectional study of U.S. adults, we found that low- and VL-income adults were less likely to be screened for CVD risk factors or receive counseling to prevent CVD than high-income adults, regardless of CVD status. This places socioeconomically disadvantaged populations at greater risk of having uncontrolled CVD risk factors and subsequently developing new or worsening CVD. The possible reasons for these associations are likely complex and require further study. More work must be done to reduce disparities in access to and utilization of CVD preventive care services among adults with differing SES.
CRediT authorship contribution statement
Andi Shahu: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Visualization. Victor Okunrintemi: Methodology, Formal analysis, Writing – original draft, Writing – review & editing. Martin Tibuakuu: Writing – review & editing. Safi U. Khan: Writing – review & editing. Martha Gulati: Writing – review & editing. Francoise Marvel: Writing – review & editing. Roger S. Blumenthal: Writing – review & editing. Erin D. Michos: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Funding
Dr. Michos is supported by the Amato Fund for Women's Cardiovascular Health Research at Johns Hopkins University.
Acknowledgments
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2021.100286.
Appendix. Supplementary materials
References
- 1.White-Williams C., Rossi L.P., Bittner V.A., et al. Addressing social determinants of health in the care of patients with heart failure: a scientific statement from the American Heart Association. Circulation. 2020;141:e841–e863. doi: 10.1161/CIR.0000000000000767. [DOI] [PubMed] [Google Scholar]
- 2.Havranek E.P., Mujahid M.S., Barr D.A., et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 3.Carlsson A.C., Li X., Holzmann M.J., et al. Neighbourhood socioeconomic status and coronary heart disease in individuals between 40 and 50 years. Heart. 2016;102:775–782. doi: 10.1136/heartjnl-2015-308784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reshetnyak E., Ntamatungiro M., Pinheiro L.C., et al. Impact of multiple social determinants of health on incident stroke. Stroke. 2020;51:2445–2453. doi: 10.1161/STROKEAHA.120.028530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schrage B., Lund L.H., Benson L., et al. Lower socioeconomic status predicts higher mortality and morbidity in patients with heart failure. Heart. 2021;107(3):229–236. doi: 10.1136/heartjnl-2020-317216. [DOI] [PubMed] [Google Scholar]
- 6.Shahu A., Herrin J., Dhruva S.S., et al. Disparities in socioeconomic context and association with blood pressure control and cardiovascular outcomes in ALLHAT. J Am Heart Assoc. 2019;8 doi: 10.1161/JAHA.119.012277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stringhini S., Carmeli C., Jokela M., et al. Socioeconomic status and the 25×25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. Lancet. 2017;389:1229–1237. doi: 10.1016/S0140-6736(16)32380-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanjilal S., Gregg E.W., Cheng Y.J., et al. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971-2002. Arch Intern Med. 2006;166:2348–2355. doi: 10.1001/archinte.166.21.2348. [DOI] [PubMed] [Google Scholar]
- 9.Colhoun H.M., Hemingway H., Poulter N.R. Socio-economic status and blood pressure: an overview analysis. J Hum Hypertens. 1998;12:91–110. doi: 10.1038/sj.jhh.1000558. [DOI] [PubMed] [Google Scholar]
- 10.Pigeyre M., Rousseaux J., Trouiller P., et al. How obesity relates to socio-economic status: identification of eating behavior mediators. Int J Obes. 2016;40:1794–1801. doi: 10.1038/ijo.2016.109. [DOI] [PubMed] [Google Scholar]
- 11.Hankonen N., Heino M.T., Kujala E., et al. What explains the socioeconomic status gap in activity? Educational differences in determinants of physical activity and screentime. BMC Public Health. 2017;17:144. doi: 10.1186/s12889-016-3880-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen A., Machiorlatti M., Krebs N.M., Muscat J.E. Socioeconomic differences in nicotine exposure and dependence in adult daily smokers. BMC Public Health. 2019;19:375. doi: 10.1186/s12889-019-6694-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sambamoorthi U., McAlpine D.D. Racial, ethnic, socioeconomic, and access disparities in the use of preventive services among women. Prev Med. 2003;37:475–484. doi: 10.1016/s0091-7435(03)00172-5. [DOI] [PubMed] [Google Scholar]
- 14."Medical Expenditure Panel Survey." Accessed May 29, 2021 http://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp.
- 15.Cohen J.W., Monheit A.C., Beauregard K.M., et al. The Medical Expenditure Panel Survey: a national health information resource. Inquiry. 1996;33:373–389. [PubMed] [Google Scholar]
- 16.Tibuakuu M., Okunrintemi V., Savji N., et al. Nondietary cardiovascular health metrics with patient experience and loss of productivity among US adults without cardiovascular disease: the medical expenditure panel survey 2006 to 2015. J Am Heart Assoc. 2020 doi: 10.1161/JAHA.120.016744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Okunrintemi V., Benson E.-.M.A., Derbal O., et al. Age-specific differences in patient reported outcomes among adults with atherosclerotic cardiovascular disease: medical expenditure panel survey 2006–2015. Am J Prev Cardiol. 2020;3 doi: 10.1016/j.ajpc.2020.100083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Okunrintemi V., Valero-Elizondo J., Patrick B., et al. Gender differences in patient-reported outcomes among adults with atherosclerotic cardiovascular disease. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.010498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 20.de Groot V., Beckerman H., Lankhorst G.J., Bouter L.M. How to measure comorbidity. a critical review of available methods. J Clin Epidemiol. 2003;56:221–229. doi: 10.1016/s0895-4356(02)00585-1. [DOI] [PubMed] [Google Scholar]
- 21.Schultz W.M., Kelli H.M., Lisko J.C., et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. 2018;137:2166–2178. doi: 10.1161/CIRCULATIONAHA.117.029652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Topel M.L., Kim J.H., Mujahid M.S., et al. Neighborhood socioeconomic status and adverse outcomes in patients with cardiovascular disease. Am J Cardiol. 2019;123:284–290. doi: 10.1016/j.amjcard.2018.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schumann B., Kluttig A., Tiller D., Werdan K., Haerting J., Greiser K.H. Association of childhood and adult socioeconomic indicators with cardiovascular risk factors and its modification by age: the CARLA Study 2002-2006. BMC Public Health. 2011;11:289. doi: 10.1186/1471-2458-11-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Odutayo A., Gill P., Shepherd S., et al. Income disparities in absolute cardiovascular risk and cardiovascular risk factors in the United States, 1999-2014. JAMA Cardiol. 2017;2:782–790. doi: 10.1001/jamacardio.2017.1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel R., Lawlor D.A., Ebrahim S. Socio-economic position and the use of preventive health care in older British women: a cross-sectional study using data from the British Women's Heart and Health Study cohort. Fam Pract. 2007;24:7–10. doi: 10.1093/fampra/cml064. [DOI] [PubMed] [Google Scholar]
- 26.Vaidya V., Partha G., Howe J. Utilization of preventive care services and their effect on cardiovascular outcomes in the United States. Risk Manag Healthc Policy. 2011;4:1–7. doi: 10.2147/RMHP.S15777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Faulkner L.A., Schauffler H.H. The effect of health insurance coverage on the appropriate use of recommended clinical preventive services. Am J Prev Med. 1997;13:453–458. [PubMed] [Google Scholar]
- 28.DeVoe J.E., Fryer G.E., Phillips R., Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93:786–791. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lang S.J., Abel G.A., Mant J., Mullis R. Impact of socioeconomic deprivation on screening for cardiovascular disease risk in a primary prevention population: a cross-sectional study. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2015-009984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pappa E., Kontodimopoulos N., Papadopoulos A.A., Pallikarona G., Niakas D., Tountas Y. Factors affecting use of preventive tests for cardiovascular risk among Greeks. Int J Environ Res Public Health. 2009;6:2712–2724. doi: 10.3390/ijerph6102712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rodin D., Stirbu I., Ekholm O., et al. Educational inequalities in blood pressure and cholesterol screening in nine European countries. J Epidemiol Community Health. 2012;66:1050–1055. doi: 10.1136/jech-2011-200273. [DOI] [PubMed] [Google Scholar]
- 32.Wang J., Zuo H., Chen X., Hou L., Ma J. Analysis of factors influencing the frequency of primary care visits among diabetic patients in two provinces in China. BMC Public Health. 2019;19:1267. doi: 10.1186/s12889-019-7591-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Delva J., Johnston L.D., O'Malley P.M. The epidemiology of overweight and related lifestyle behaviors: racial/ethnic and socioeconomic status differences among American youth. Am J Prev Med. 2007;33:S178–S186. doi: 10.1016/j.amepre.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 34.van den Berk-Clark C., McGuire J. Trust in health care providers: factors predicting trust among homeless veterans over time. J Health Care Poor Underserved. 2014;25:1278–1290. doi: 10.1353/hpu.2014.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allen N.B., Diez-Roux A., Liu K., Bertoni A.G., Szklo M., Daviglus M. Association of health professional shortage areas and cardiovascular risk factor prevalence, awareness, and control in the Multi-Ethnic Study of Atherosclerosis (MESA) Circ Cardiovasc Qual Outcomes. 2011;4:565–572. doi: 10.1161/CIRCOUTCOMES.111.960922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Okunrintemi V., Khera R., Spatz E.S., et al. Association of income disparities with patient-reported healthcare experience. J Gen Intern Med. 2019;34:884–892. doi: 10.1007/s11606-019-04848-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Senn T.E., Walsh J.L., Carey M.P. The mediating roles of perceived stress and health behaviors in the relation between objective, subjective, and neighborhood socioeconomic status and perceived health. Ann Behav Med. 2014;48:215–224. doi: 10.1007/s12160-014-9591-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rios R., Aiken L.S., Zautra A.J. Neighborhood contexts and the mediating role of neighborhood social cohesion on health and psychological distress among Hispanic and non-Hispanic residents. Ann Behav Med. 2012;43:50–61. doi: 10.1007/s12160-011-9306-9. [DOI] [PubMed] [Google Scholar]
- 39.Woodward E.N., Walsh J.L., Senn T.E., Carey M.P. Positive social interaction offsets impact of low socioeconomic status on stress. J Natl Med Assoc. 2018;110:371–377. doi: 10.1016/j.jnma.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thoits P.A. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. 2011;52:145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- 41.Williams D.R., Yan Y., Jackson J.S., Anderson N.B. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 42.Sims M., Kershaw K.N., Breathett K., et al. Importance of housing and cardiovascular health and well-being: a scientific statement from the American Heart Association. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/HCQ.0000000000000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Churchwell K., Elkind M.S.V., Benjamin R.M., et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the american heart association. Circulation. 2020;142:e454–e468. doi: 10.1161/CIR.0000000000000936. [DOI] [PubMed] [Google Scholar]
- 44.Mayne S.L., Moore K.A., Powell-Wiley T.M., Evenson K.R., Block R., Kershaw K.N. Longitudinal associations of neighborhood crime and perceived safety with blood pressure: the Multi-Ethnic Study of Atherosclerosis (MESA) Am J Hypertens. 2018;31:1024–1032. doi: 10.1093/ajh/hpy066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sallis J.F., Conway T.L., Cain K.L., et al. Neighborhood built environment and socioeconomic status in relation to physical activity, sedentary behavior, and weight status of adolescents. Prev Med. 2018;110:47–54. doi: 10.1016/j.ypmed.2018.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaiser P., Auchincloss A.H., Moore K., et al. Associations of neighborhood socioeconomic and racial/ethnic characteristics with changes in survey-based neighborhood quality, 2000-2011. Health Place. 2016;42:30–36. doi: 10.1016/j.healthplace.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Powell L.M., Slater S., Mirtcheva D., Bao Y., Chaloupka F.J. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007;44:189–195. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 48.McAlister F.A., Lawson F.M., Teo K.K., Armstrong P.W. Randomised trials of secondary prevention programmes in coronary heart disease: systematic review. BMJ. 2001;323:957–962. doi: 10.1136/bmj.323.7319.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cawley J., Meyerhoefer C., Biener A., Hammer M., Wintfeld N. Savings in medical expenditures associated with reductions in body mass index among US Adults with Obesity, by Diabetes Status. Pharmacoeconomics. 2015;33:707–722. doi: 10.1007/s40273-014-0230-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Valero-Elizondo J., Salami J.A., Ogunmoroti O., et al. Favorable cardiovascular risk profile is associated with lower healthcare costs and resource utilization: the 2012 medical expenditure panel survey. Circ Cardiovasc Qual Outcomes. 2016;9:143–153. doi: 10.1161/CIRCOUTCOMES.115.002616. [DOI] [PubMed] [Google Scholar]
- 51.Feldman D.I., Valero-Elizondo J., Salami J.A., et al. Favorable cardiovascular risk factor profile is associated with lower healthcare expenditure and resource utilization among adults with diabetes mellitus free of established cardiovascular disease: 2012 Medical Expenditure Panel Survey (MEPS) Atherosclerosis. 2017;258:79–83. doi: 10.1016/j.atherosclerosis.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 52.Fiscella K., Franks P., Gold M.R., Clancy C.M. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283:2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 53.Marmot M., Friel S., Bell R., Houweling T.A., Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 54.Carnethon M.R., Pu J., Howard G., et al. Cardiovascular Health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136:e393–e423. doi: 10.1161/CIR.0000000000000534. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.