Abstract
Background
The Japan Multi-institutional Collaborative Cohort (J-MICC) study was launched in 2005 to examine gene–environment interactions in lifestyle-related diseases, including cancers, among the Japanese. This report describes the study design and baseline profile of the study participants.
Methods
The participants of the J-MICC Study were individuals aged 35 to 69 years enrolled from respondents to study announcements in specified regions, inhabitants attending health checkup examinations provided by local governments, visitors at health checkup centers, and first-visit patients at a cancer hospital in Japan. At the time of the baseline survey, from 2005 to 2014, we obtained comprehensive information regarding demographics, education, alcohol consumption, smoking, sleeping, exercise, food intake frequency, medication and supplement use, personal and family disease history, psychological stress, and female reproductive history and collected peripheral blood samples.
Results
The baseline survey included 92,610 adults (mean age: 55.2 [standard deviation, 9.4] years, 44.1% men) from 14 study regions in 12 prefectures. The participation rate was 33.5%, with participation ranging from 19.7% to 69.8% in different study regions. The largest number of participants was in the age groups of 65–69 years for men and 60–64 years for women. There were differences in body mass index, educational attainment, alcohol consumption, smoking, and sleep duration between men and women.
Conclusions
The J-MICC Study collected lifestyle and clinical data and biospecimens from over 90,000 participants. This cohort is expected to be a valuable resource for the national and international scientific community in providing evidence to support longer healthy lives.
Key words: study profile, cohort study, gene–environment interactions, cancer, J-MICC
INTRODUCTION
Since 1981, cancer, a lifestyle-related disease, has been the leading cause of death in Japan and has continued to be a substantial public health burden. In Japan, several cohort studies were started in the 1980s and 1990s to identify factors contributing to the decrease in the incidence of lifestyle-related diseases represented by cancer. Representative large-scale cohort studies for cancer prevention include the following. From 1988 through 1990, the Japan Collaborative Cohort (JACC) study was established, covering 45 regions in Japan, and has followed up approximately 110,000 individuals aged 40 to 79 years.1 From 1990 to 1993, the Japan Public Health Center-based Cohort (JPHC) study began covering 11 public health center regions throughout Japan and has included a total of about 140,000 individuals aged 40 to 69 years.2 However, cancer is still the leading cause of death, resulting in approximately 0.37 million deaths (27.4% of all deaths) in 2018.3
With recent advances in genotyping techniques, gene–environment interactions in lifestyle-related diseases have begun to be investigated in many epidemiological studies.4–8 This is because most multifactorial diseases are considered to be caused by interactions between hazardous environmental factors and the host genome. Elucidating gene–environment interactions requires long-term cohort studies, which cover the etiologically relevant time period to improve the accuracy of measures of exposures by collecting repeated biologic samples and self-reported information.9 Therefore, we launched the Japan Multi-institutional Collaborative Cohort (J-MICC) study in 2005, which includes healthy Japanese individuals. As part of this study, buffy coat, serum, and plasma samples are stored. The J-MICC Study is supported by a research grant for Scientific Research on Special Priority Areas of Cancer from the Japanese Ministry of Education, Culture, Sports, Science and Technology (MEXT).10 The aims of this large-scale, population-based, long-term prospective, genome-cohort study are to examine gene–environment interactions in lifestyle-related diseases, especially cancers. While the J-MICC Study Group reported many cross-sectional studies focusing on the gene–environmental interaction for health outcomes, there were no reports of detailed study design and baseline participant age distribution by study region. Therefore, this report describes the study design and profile of the participants at baseline.
METHODS
Study design and organization
The J-MICC Study is being conducted under a population-based cohort design, managed by 13 research groups (J-MICC Study Group) from 12 prefectures: Chiba Cancer Center Research Institute, Kanagawa Cancer Center Research Institute, University of Shizuoka, Nagoya City University, Aichi Cancer Center Research Institute, Nagoya University, Tsuruga Nursing University, Shiga University of Medical Science, Kyoto Prefectural University of Medicine, Tokushima University Graduate School, Kyushu University, Saga University, and Kagoshima University. Each group has its own independent research site and conducts a cohort study as part of the J-MICC Study, which allows sites to collect and analyze additional information or samples for their own research purposes. The Steering Committee is organized by a representative from each group to manage and control the progress of the whole J-MICC Study. The chief investigator of the J-MICC Study is the chairperson of the Steering Committee. The central office was established at Nagoya University Graduate School of Medicine, where all J-MICC data and half of all blood samples are preserved. The central office also makes efforts to standardize the processes in each cohort study, supplies common tools (eg, data input system, sample management system, posters, brochures), and maintains the study website (http://www.jmicc.com/). The study protocol of the J-MICC Study was approved by the ethics committee of Nagoya University Graduate School of Medicine (approval number: 253), as well as by each group in the research sites. All participants provided written informed consent after a thorough explanation of the outline and objectives of this study.
Study participants
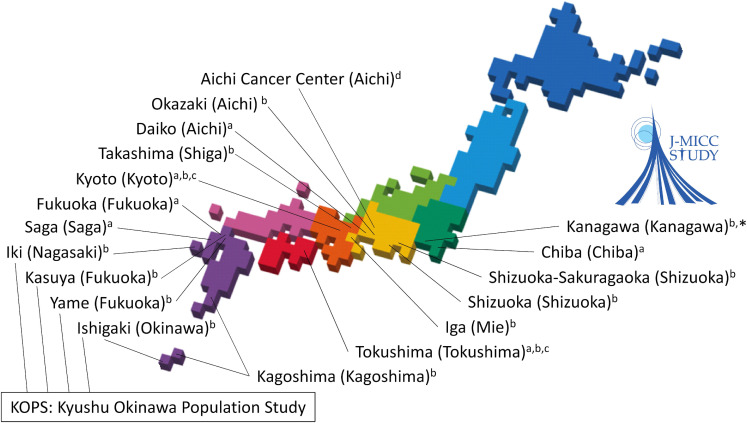
The participants of the J-MICC Study were individuals aged 35 through 69 years living in Japan. At the time of the baseline survey, from 2005–2014, the participants completed questionnaires and provided peripheral blood samples. The baseline study participants were recruited from 14 different regions throughout Japan (Figure 1). The study regions included Chiba, Shizuoka-Sakuragaoka, Shizuoka, Okazaki, Aichi Cancer Center, Daiko, Iga, Takashima, Kyoto, Tokushima, Fukuoka, Saga, Kagoshima, and the Kyusyu and Okinawa Population Study (KOPS) area. The subject sources are inhabitants in communities in four regions (Chiba, Daiko, Fukuoka, and Saga), health checkup examinees in seven regions (Shizuoka-Sakuragaoka, Shizuoka, Okazaki, Iga, Takashima, Kagoshima, and KOPS), and first-visit patients at a cancer hospital in Aichi Cancer Center region. In Kyoto and Tokushima regions, the subject sources are inhabitants in communities and health checkup examinees as well as employees of companies or local governments. In six regions (Shizuoka-Sakuragaoka, Okazaki, Takashima, Kyoto, Fukuoka, and KOPS), individuals under 35 and/or over 70 years of age were also recruited as study participants. In the Fukuoka and Saga regions, individuals aged 50 years or older and 40 years or older in principle were recruited, respectively. In the Fukuoka and KOPS regions, the survey started earlier (in 2004) and Kyushu University has been operating in study regions and collaborating with groups in the J-MICC Study. In the Kanagawa region, the baseline survey started in 2016 and is still ongoing.
Figure 1. Locations of the study regions of the J-MICC Study. *Baseline survey started in 2016 and ongoing. aInhabitants in communities; bHealth checkup examinees; cEmployees of companies or local governments; dFirst-visit patients at a cancer hospital.
Follow-up survey
The secondary survey, which is the same as the baseline survey, is scheduled for approximately 5 years after baseline enrollment, and participants will be followed until 2025. The endpoints of the J-MICC Study are cancer incidence and death from any cause, while incidence of cerebrovascular disease and myocardial infarction has been additionally registered in 10 study regions. As stated,10 information regarding endpoints are collected through population-based cancer registries if available, lists of patients at main hospitals in the study regions, mail questionnaires sent to participants, questionnaires at repeated visits to health checkup facilities, notes from death certificates, information from health insurance data, and secondary survey questionnaires. The incidence data other than those from cancer registries are also confirmed using hospital records. When a participant moves out of the study region, the participant’s follow-up is censored.
Longitudinal analyses of the follow-up survey data will be conducted in the near future.
Data and blood samples collection
At the time of enrollment, the self-administered questionnaire was distributed to the entire target population, which included common questions across all study regions. Table 1 summarizes the common questions covering basic, lifestyle, and clinical characteristics. In addition, blood chemistry data and anthropometric data were obtained from health check-ups at enrollment. The data collected from health check-ups to be sent to the central office were previously reported.10
Table 1. Summary of common questions in the self-administered questionnaire for all study regions at baseline.
| Measurements | Measurement lists |
| Basic characteristics | |
| Demographics | Sex, age at baseline, height, weight, and weight at the age of 20 years |
| Education* | Educational attainment |
| Lifestyle characteristics | |
| Alcohol consumption | Drinking status, age when the individual started drinking, type and amount of alcohol consumed, and drinking frequency |
| Smoking | Smoking status, age when the individual started smoking, number of cigarettes smoked, and information on passive smoking |
| Sleeping | Sleeping duration and subjective assessment of sleep |
| Exercise | Physical activity (including leisure-time, occupational, and household activities) |
| Diet | Food intake frequency |
| Clinical characteristics | |
| Medication and supplements | Types of medications and supplements taken at least once a week |
| Disease history | Personal and family disease history |
| Psychological stress | Self-reported stress and stress management |
| Female reproductive history | Menstruation status, age at the start of menstruation, and information on pregnancy and childbirth |
*Excluding 3 regions (Iga, Fukuoka, and Kyusyu and Okinawa Population Study regions).
We collected blood samples in a 7-mL vacuum tube for serum and a 7-mL EDTA-2Na-containing vacuum tube for plasma and buffy coat. The blood samples sent to the central office consisted of one tube containing 300 µL of buffy coat, four tubes containing 300 µL of serum, and four tubes containing 300 µL of plasma. Some of the blood specimens will be stored at the central office until the end of the J-MICC Study in 2035.11
Baseline data and blood samples (buffy coat, serum, and plasma), anonymized with an identification number (J-MICC ID), are sent to the central office from each participating research group. The secondary survey and follow-up data are linked using the J-MICC ID.
Statistical analyses
For the baseline profile (excluding the Kanagawa region because of the ongoing baseline survey for 5,000 participants), descriptive statistics were calculated for baseline data regarding sex, age, body mass index (BMI) calculated from self-reported height and weight, educational attainment, alcohol consumption, smoking, sleeping duration, leisure time physical activity, psychological stress, and personal (past and present) disease history. In the case of educational attainment, participants from the Iga, Fukuoka, and KOPS regions were excluded from the analysis because the questionnaire used there did not include this item.
RESULTS
Among 247,951 eligible individuals, 83,114 (33.5% in total with response rates ranging from 19.7% to 69.8% in different study regions) consented to participate in the baseline survey of the J-MICC Study. Furthermore, by distributing 2,786,327 fliers via mailboxes in four regions, 18,368 respondents were additionally recruited. In total, 101,482 men and women participated in the baseline survey. After excluding 8,294 respondents under 35 or over 70 years of age and 578 who withdrew consent or became ineligible, the remaining 92,610 participants (40,880 men and 51,730 women with an average age of 55.2 [standard deviation, 9.4] years) in the baseline survey were included in the present analysis (the dataset was fixed on February 2, 2020). Among the participants, 90,319 people (97.5% of total participants) consented to the use of their biospecimens in the J-MICC Study, including genomic analysis (90,252 people; 99.9% of total consenters).
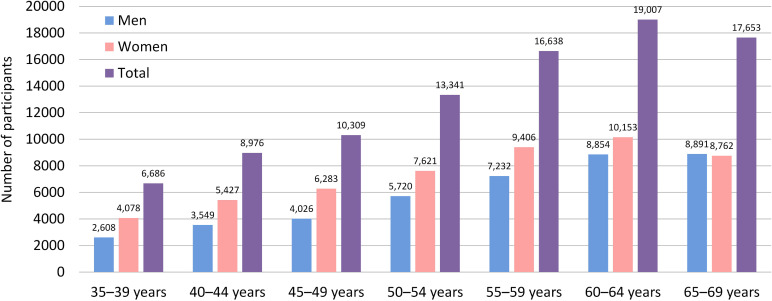
The age-sex distribution of the participants in the baseline survey is presented in Figure 2. Of the respondents, 7.2% belonged to the 35–39 years age group, 9.7% to the 40–44 years age group, 11.1% to the 45–49 years age group, 14.4% to the 50–54 years age group, 18.0% to the 55–59 years age group, 20.5% to the 60–64 years age group, and 19.1% to the 65–69 years age group. The largest number of participants were in the 65–69 age group for men (21.7% of male participants) and the 60–64 age group for women (19.6% of female participants). The number of female participants was higher than that of male participants for all age categories, except for those aged 65–69.
Figure 2. Age-sex distribution of participants in the baseline survey of the J-MICC Study.
The age distribution of the male and female participants in the baseline survey by the study regions is shown in Table 2 and Table 3, respectively. The average age of participants who were enrolled in Chiba, Shizuoka-Sakuragaoka, Shizuoka, Okazaki, Aichi Cancer Center, Daiko, Iga, Takashima, Kyoto, Tokushima, Fukuoka, Saga, Kagoshima, and KOPS regions were 53.9, 54.8, 52.2, 55.8, 55.1, 52.5, 51.2, 57.7, 51.6, 50.6, 60.3, 56.0, 57.5, and 54.7 years, respectively. There were considerable differences in age distributions by study region among both men and women. Notably, the percentage of people aged 35 to 39 years ranged from 0.0% to 16.7% in men and from 0.0% to 16.0% in women. Likewise, the percentage of people aged 40 to 44 years and 45 to 49 years ranged from 0.0% to 16.1% and 0.0% to 15.9% in men and from 0.0% to 16.5% and 0.1% to 18.1% in women, respectively.
Table 2. Age distribution of male participants in the baseline survey of the J-MICC Study by study region.
| Study region | Age, years | Total | Average age (SD) |
|||||||
|
|
||||||||||
| 35–39 | 40–44 | 45–49 | 50–54 | 55–59 | 60–64 | 65–69 | ||||
| Total | N | 2,608 | 3,549 | 4,026 | 5,720 | 7,232 | 8,854 | 8,891 | 40,880 | 56.1 |
| (%) | (6.4) | (8.7) | (9.8) | (14.0) | (17.7) | (21.7) | (21.7) | (100.0) | (9.3) | |
| Chiba | N | 293 | 272 | 292 | 347 | 455 | 562 | 697 | 2,918 | 55.4 |
| (%) | (10.0) | (9.3) | (10.0) | (11.9) | (15.6) | (19.3) | (23.9) | (100.0) | (10.1) | |
| Shizuoka-Sakuragaoka | N | 240 | 277 | 286 | 435 | 521 | 808 | 563 | 3,130 | 55.6 |
| (%) | (7.7) | (8.8) | (9.1) | (13.9) | (16.6) | (25.8) | (18.0) | (100.0) | (9.3) | |
| Shizuoka | N | 265 | 437 | 542 | 585 | 782 | 483 | 312 | 3,406 | 52.7 |
| (%) | (7.8) | (12.8) | (15.9) | (17.2) | (23.0) | (14.2) | (9.2) | (100.0) | (8.7) | |
| Okazaki | N | 262 | 271 | 353 | 376 | 449 | 824 | 955 | 3,490 | 56.7 |
| (%) | (7.5) | (7.8) | (10.1) | (10.8) | (12.9) | (23.6) | (27.4) | (100.0) | (9.7) | |
| Aichi Cancer Center | N | 192 | 225 | 301 | 462 | 837 | 1,119 | 1,159 | 4,295 | 58.2 |
| (%) | (4.5) | (5.2) | (7.0) | (10.8) | (19.5) | (26.1) | (27.0) | (100.0) | (8.6) | |
| Daiko | N | 190 | 161 | 185 | 195 | 206 | 241 | 284 | 1,462 | 53.6 |
| (%) | (13.0) | (11.0) | (12.7) | (13.3) | (14.1) | (16.5) | (19.4) | (100.0) | (10.3) | |
| Iga | N | 100 | 94 | 76 | 115 | 89 | 94 | 68 | 636 | 51.3 |
| (%) | (15.7) | (14.8) | (11.9) | (18.1) | (14.0) | (14.8) | (10.7) | (100.0) | (9.8) | |
| Takashima | N | 72 | 58 | 78 | 87 | 161 | 305 | 477 | 1,238 | 59.3 |
| (%) | (5.8) | (4.7) | (6.3) | (7.0) | (13.0) | (24.6) | (38.5) | (100.0) | (9.1) | |
| Kyoto | N | 431 | 344 | 360 | 369 | 346 | 385 | 341 | 2,576 | 51.7 |
| (%) | (16.7) | (13.4) | (14.0) | (14.3) | (13.4) | (14.9) | (13.2) | (100.0) | (10.3) | |
| Tokushima | N | 224 | 228 | 191 | 225 | 218 | 221 | 107 | 1,414 | 50.8 |
| (%) | (15.8) | (16.1) | (13.5) | (15.9) | (15.4) | (15.6) | (7.6) | (100.0) | (9.6) | |
| Fukuoka | N | 0 | 0 | 0 | 782 | 1,131 | 1,256 | 1,287 | 4,456 | 60.5 |
| (%) | (0.0) | (0.0) | (0.0) | (17.5) | (25.4) | (28.2) | (28.9) | (100.0) | (5.4) | |
| Saga | N | 0 | 569 | 591 | 793 | 1,048 | 1,025 | 1,052 | 5,078 | 56.5 |
| (%) | (0.0) | (11.2) | (11.6) | (15.6) | (20.6) | (20.2) | (20.7) | (100.0) | (8.2) | |
| Kagoshima | N | 79 | 230 | 366 | 435 | 465 | 738 | 847 | 3,160 | 57.5 |
| (%) | (2.5) | (7.3) | (11.6) | (13.8) | (14.7) | (23.4) | (26.8) | (100.0) | (8.6) | |
| KOPS | N | 260 | 383 | 405 | 514 | 524 | 793 | 742 | 3,621 | 55.3 |
| (%) | (7.2) | (10.6) | (11.2) | (14.2) | (14.5) | (21.9) | (20.5) | (100.0) | (9.6) | |
KOPS, Kyusyu and Okinawa Population Study; SD, standard deviation.
Table 3. Age distribution of female participants in the baseline survey of the J-MICC Study by study region.
| Study region | Age, years | Total | Average age (SD) |
|||||||
|
|
||||||||||
| 35–39 | 40–44 | 45–49 | 50–54 | 55–59 | 60–64 | 65–69 | ||||
| Total | N | 4,078 | 5,427 | 6,283 | 7,621 | 9,406 | 10,153 | 8,762 | 51,730 | 54.6 |
| (%) | (7.9) | (10.5) | (12.1) | (14.7) | (18.2) | (19.6) | (16.9) | (100.0) | (9.4) | |
| Chiba | N | 636 | 607 | 703 | 732 | 854 | 894 | 750 | 5,176 | 53.1 |
| (%) | (12.3) | (11.7) | (13.6) | (14.1) | (16.5) | (17.3) | (14.5) | (100.0) | (9.8) | |
| Shizuoka-Sakuragaoka | N | 215 | 288 | 339 | 343 | 406 | 456 | 340 | 2,387 | 53.6 |
| (%) | (9.0) | (12.1) | (14.2) | (14.4) | (17.0) | (19.1) | (14.2) | (100.0) | (9.5) | |
| Shizuoka | N | 195 | 198 | 290 | 296 | 331 | 186 | 104 | 1,600 | 51.2 |
| (%) | (12.2) | (12.4) | (18.1) | (18.5) | (20.7) | (11.6) | (6.5) | (100.0) | (8.6) | |
| Okazaki | N | 220 | 331 | 411 | 411 | 506 | 657 | 524 | 3,060 | 54.7 |
| (%) | (7.2) | (10.8) | (13.4) | (13.4) | (16.5) | (21.5) | (17.1) | (100.0) | (9.4) | |
| Aichi Cancer Center | N | 572 | 656 | 759 | 659 | 791 | 807 | 562 | 4,806 | 52.3 |
| (%) | (11.9) | (13.6) | (15.8) | (13.7) | (16.5) | (16.8) | (11.7) | (100.0) | (9.6) | |
| Daiko | N | 570 | 489 | 542 | 472 | 470 | 558 | 589 | 3,690 | 52.1 |
| (%) | (15.4) | (13.3) | (14.7) | (12.8) | (12.7) | (15.1) | (16.0) | (100.0) | (10.3) | |
| Iga | N | 97 | 121 | 127 | 149 | 137 | 104 | 51 | 786 | 51.0 |
| (%) | (12.3) | (15.4) | (16.2) | (19.0) | (17.4) | (13.2) | (6.5) | (100.0) | (8.7) | |
| Takashima | N | 221 | 139 | 175 | 232 | 347 | 575 | 601 | 2,290 | 56.8 |
| (%) | (9.7) | (6.1) | (7.6) | (10.1) | (15.2) | (25.1) | (26.2) | (100.0) | (9.8) | |
| Kyoto | N | 544 | 552 | 588 | 488 | 444 | 576 | 428 | 3,620 | 51.5 |
| (%) | (15.0) | (15.2) | (16.2) | (13.5) | (12.3) | (15.9) | (11.8) | (100.0) | (10.0) | |
| Tokushima | N | 164 | 169 | 161 | 166 | 148 | 136 | 82 | 1,026 | 50.4 |
| (%) | (16.0) | (16.5) | (15.7) | (16.2) | (14.4) | (13.3) | (8.0) | (100.0) | (9.5) | |
| Fukuoka | N | 0 | 0 | 3 | 1,051 | 1,617 | 1,538 | 1,428 | 5,637 | 60.0 |
| (%) | (0.0) | (0.0) | (0.1) | (18.6) | (28.7) | (27.3) | (25.3) | (100.0) | (5.3) | |
| Saga | N | 0 | 921 | 940 | 1,150 | 1,409 | 1,374 | 1,196 | 6,990 | 55.6 |
| (%) | (0.0) | (13.2) | (13.4) | (16.5) | (20.2) | (19.7) | (17.1) | (100.0) | (8.2) | |
| Kagoshima | N | 60 | 313 | 497 | 617 | 850 | 1,074 | 1,067 | 4,478 | 57.5 |
| (%) | (1.3) | (7.0) | (11.1) | (13.8) | (19.0) | (24.0) | (23.8) | (100.0) | (8.1) | |
| KOPS | N | 584 | 643 | 748 | 855 | 1,096 | 1,218 | 1,040 | 6,184 | 54.3 |
| (%) | (9.4) | (10.4) | (12.1) | (13.8) | (17.7) | (19.7) | (16.8) | (100.0) | (9.7) | |
KOPS, Kyusyu and Okinawa Population Study; SD, standard deviation.
Basic, lifestyle, and clinical characteristics of the male and female participants in the baseline survey by age category are summarized in Table 4 and Table 5, respectively. There were differences in BMI, educational attainment, alcohol consumption, smoking, and sleep duration between men and women. The percentage of overweight adults (BMI 25.0–29.9 kg/m2) was 1.7 times higher for men (26.7%) than for women (15.8%). Approximately 40% of men had ≥16 years of education compared with 13.5% of women. The likelihood of being a former drinker and sleeping ≥9 hours/day increased gradually with higher age categories among men, but no such association was observed among women. The likelihood of being a never smoker increased gradually with higher age categories among women, but no such association was observed among men. For leisure time physical activity, psychological stress, and history of disease, the percentages of participants with ≥300 min/week of leisure-time activity, those perceiving no stress, and those with a history of diseases increased gradually with higher age categories among both men and women. For cancer, when patients first seen at the Aichi Cancer Center, a cancer hospital, were excluded from the analysis, cancer prevalence fell from 8.5% to 4.5% for men and from 7.1% to 5.1% for women.
Table 4. Baseline characteristics of male participants of the J-MICC Study according to age category (N = 40,880).
| Characteristic | Age, years | Total | ||||||||||||||
|
| ||||||||||||||||
| 35–39 | 40–44 | 45–49 | 50–54 | 55–59 | 60–64 | 65–69 | ||||||||||
|
| ||||||||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| Body mass index, kg/m2 | ||||||||||||||||
| <18.5 | 87 | 3.3 | 99 | 2.8 | 105 | 2.6 | 136 | 2.4 | 207 | 2.9 | 281 | 3.2 | 298 | 3.4 | 1,213 | 3.0 |
| 18.5–24.9 | 1,742 | 66.8 | 2,288 | 64.5 | 2,553 | 63.4 | 3,618 | 63.3 | 4,840 | 66.9 | 6,080 | 68.7 | 6,291 | 70.8 | 27,412 | 67.1 |
| 25.0–29.9 | 640 | 24.6 | 952 | 26.9 | 1,198 | 29.8 | 1,730 | 30.3 | 1,989 | 27.5 | 2,278 | 25.7 | 2,141 | 24.1 | 10,928 | 26.7 |
| ≥30.0 | 137 | 5.3 | 206 | 5.8 | 169 | 4.2 | 234 | 4.1 | 194 | 2.7 | 209 | 2.4 | 152 | 1.7 | 1,301 | 3.2 |
| Educational attainment, years | ||||||||||||||||
| <10 | 45 | 2.0 | 94 | 3.1 | 100 | 2.8 | 197 | 4.6 | 460 | 8.4 | 944 | 14.2 | 1,482 | 22.0 | 3,322 | 10.4 |
| 10–15 | 1,005 | 44.8 | 1,442 | 47.1 | 1,674 | 47.4 | 2,052 | 47.8 | 2,843 | 52.1 | 3,503 | 52.6 | 3,324 | 49.4 | 15,843 | 49.5 |
| ≥16 | 1,193 | 53.2 | 1,526 | 49.8 | 1,758 | 49.8 | 2,048 | 47.7 | 2,156 | 39.5 | 2,213 | 33.2 | 1,927 | 28.6 | 12,821 | 40.1 |
| Alcohol consumption | ||||||||||||||||
| Current drinkers | 1,902 | 72.9 | 2,679 | 75.5 | 3,163 | 78.6 | 4,465 | 78.2 | 5,500 | 76.1 | 6,646 | 75.1 | 6,507 | 73.3 | 30,862 | 75.6 |
| Former drinkers | 36 | 1.4 | 74 | 2.1 | 87 | 2.2 | 177 | 3.1 | 281 | 3.9 | 423 | 4.8 | 552 | 6.2 | 1,630 | 4.0 |
| Never drinkers | 670 | 25.7 | 794 | 22.4 | 775 | 19.3 | 1,070 | 18.7 | 1,443 | 20.0 | 1,781 | 20.1 | 1,821 | 20.5 | 8,354 | 20.5 |
| Smoking | ||||||||||||||||
| Current smokers | 879 | 34.0 | 1,310 | 37.1 | 1,416 | 35.3 | 2,052 | 36.0 | 2,364 | 32.7 | 2,368 | 26.8 | 1,772 | 20.0 | 12,161 | 29.8 |
| Former smokers | 713 | 27.6 | 1,066 | 30.2 | 1,393 | 34.7 | 2,206 | 38.7 | 3,097 | 42.9 | 4,160 | 47.1 | 4,382 | 49.4 | 17,017 | 41.7 |
| Never smokers | 990 | 38.3 | 1,159 | 32.8 | 1,200 | 29.9 | 1,444 | 25.3 | 1,763 | 24.4 | 2,305 | 26.1 | 2,722 | 30.7 | 11,583 | 28.4 |
| Sleep duration, hour/day | ||||||||||||||||
| <4.0 | 10 | 0.4 | 12 | 0.3 | 9 | 0.2 | 8 | 0.1 | 12 | 0.2 | 11 | 0.1 | 18 | 0.2 | 80 | 0.2 |
| 4.0–4.9 | 77 | 3.0 | 74 | 2.1 | 73 | 1.8 | 71 | 1.2 | 70 | 1.0 | 113 | 1.3 | 85 | 1.0 | 563 | 1.4 |
| 5.0–5.9 | 364 | 14.0 | 452 | 12.7 | 469 | 11.7 | 639 | 11.2 | 618 | 8.6 | 555 | 6.3 | 560 | 6.3 | 3,657 | 9.0 |
| 6.0–6.9 | 1,027 | 39.5 | 1,400 | 39.5 | 1,553 | 38.6 | 1,999 | 35.0 | 2,415 | 33.4 | 2,372 | 26.8 | 2,087 | 23.5 | 12,853 | 31.5 |
| 7.0–7.9 | 801 | 30.8 | 1,133 | 32.0 | 1,374 | 34.2 | 2,105 | 36.8 | 2,710 | 37.5 | 3,249 | 36.7 | 3,117 | 35.1 | 14,489 | 35.5 |
| 8.0–8.9 | 292 | 11.2 | 437 | 12.3 | 485 | 12.1 | 797 | 14.0 | 1,230 | 17.0 | 2,167 | 24.5 | 2,443 | 27.5 | 7,851 | 19.2 |
| ≥9.0 | 30 | 1.2 | 38 | 1.1 | 59 | 1.5 | 94 | 1.6 | 168 | 2.3 | 380 | 4.3 | 572 | 6.4 | 1,341 | 3.3 |
| Leisure time physical activity, min/week | ||||||||||||||||
| <30 | 1,078 | 42.7 | 1,544 | 44.6 | 1,631 | 41.7 | 2,206 | 39.6 | 2,555 | 36.4 | 2,386 | 27.8 | 1,878 | 22.1 | 13,278 | 33.6 |
| 30–59 | 231 | 9.2 | 302 | 8.7 | 303 | 7.7 | 405 | 7.3 | 487 | 6.9 | 452 | 5.3 | 305 | 3.6 | 2,485 | 6.3 |
| 60–119 | 449 | 17.8 | 550 | 15.9 | 696 | 17.8 | 964 | 17.3 | 1,203 | 17.1 | 1,206 | 14.1 | 951 | 11.2 | 6,019 | 15.2 |
| 120–179 | 255 | 10.1 | 361 | 10.4 | 406 | 10.4 | 626 | 11.2 | 828 | 11.8 | 937 | 10.9 | 906 | 10.7 | 4,319 | 10.9 |
| 180–299 | 206 | 8.2 | 280 | 8.1 | 354 | 9.0 | 560 | 10.0 | 780 | 11.1 | 1,100 | 12.8 | 1,091 | 12.9 | 4,371 | 11.1 |
| ≥300 | 304 | 12.0 | 427 | 12.3 | 525 | 13.4 | 815 | 14.6 | 1,168 | 16.6 | 2,496 | 29.1 | 3,349 | 39.5 | 9,084 | 23.0 |
| Psychological stress during the last year | ||||||||||||||||
| No stress | 30 | 1.2 | 70 | 2.0 | 108 | 2.8 | 180 | 3.2 | 331 | 4.7 | 680 | 7.8 | 955 | 10.9 | 2,354 | 5.9 |
| Low stress | 375 | 15.0 | 494 | 14.3 | 627 | 16.0 | 1,086 | 19.4 | 1,654 | 23.3 | 3,011 | 34.5 | 3,475 | 39.6 | 10,722 | 26.8 |
| Moderate stress | 1,254 | 50.2 | 1,674 | 48.6 | 1,936 | 49.3 | 2,713 | 48.5 | 3,443 | 48.5 | 3,800 | 43.6 | 3,510 | 40.0 | 18,330 | 45.8 |
| High stress | 838 | 33.6 | 1,207 | 35.0 | 1,253 | 31.9 | 1,612 | 28.8 | 1,676 | 23.6 | 1,226 | 14.1 | 840 | 9.6 | 8,652 | 21.6 |
| Personal disease history | ||||||||||||||||
| Diabetes | 28 | 1.1 | 106 | 3.0 | 185 | 4.6 | 352 | 6.6 | 744 | 11.1 | 1,162 | 14.0 | 1,194 | 14.4 | 3,771 | 9.7 |
| Hypertension | 105 | 4.0 | 264 | 7.4 | 559 | 13.9 | 1,087 | 20.2 | 1,835 | 27.0 | 2,847 | 34.1 | 3,305 | 39.1 | 10,002 | 25.6 |
| Dyslipidemia | 147 | 5.6 | 352 | 9.9 | 596 | 14.9 | 923 | 17.2 | 1,320 | 19.7 | 1,618 | 19.7 | 1,569 | 19.0 | 6,525 | 16.9 |
| Coronary heart disease | 11 | 0.4 | 25 | 0.7 | 57 | 1.4 | 120 | 2.3 | 249 | 3.8 | 472 | 5.8 | 662 | 8.1 | 1,596 | 4.2 |
| Stroke | 4 | 0.2 | 16 | 0.5 | 26 | 0.6 | 78 | 1.5 | 150 | 2.3 | 297 | 3.6 | 365 | 4.5 | 936 | 2.4 |
| Cancer | 52 | 2.1 | 76 | 2.2 | 132 | 3.4 | 257 | 5.1 | 577 | 9.0 | 909 | 11.4 | 1,159 | 14.7 | 3,162 | 8.5 |
Table 5. Baseline characteristics of female participants of the J-MICC Study according to age category (N = 51,730).
| Characteristic | Age, years | Total | ||||||||||||||
|
| ||||||||||||||||
| 35–39 | 40–44 | 45–49 | 50–54 | 55–59 | 60–64 | 65–69 | ||||||||||
|
| ||||||||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| Body mass index, kg/m2 | ||||||||||||||||
| <18.5 | 746 | 18.4 | 706 | 13.0 | 639 | 10.2 | 652 | 8.6 | 766 | 8.2 | 725 | 7.2 | 562 | 6.4 | 4,796 | 9.3 |
| 18.5–24.9 | 2,900 | 71.4 | 3,935 | 72.6 | 4,582 | 73.0 | 5,581 | 73.3 | 6,772 | 72.1 | 7,377 | 72.8 | 6,154 | 70.4 | 37,301 | 72.2 |
| 25.0–29.9 | 323 | 8.0 | 630 | 11.6 | 889 | 14.2 | 1,175 | 15.4 | 1,614 | 17.2 | 1,794 | 17.7 | 1,735 | 19.8 | 8,160 | 15.8 |
| ≥30.0 | 90 | 2.2 | 147 | 2.7 | 166 | 2.6 | 208 | 2.7 | 242 | 2.6 | 243 | 2.4 | 294 | 3.4 | 1,390 | 2.7 |
| Educational attainment, years | ||||||||||||||||
| <10 | 58 | 1.7 | 60 | 1.3 | 91 | 1.7 | 190 | 3.4 | 542 | 8.3 | 1,052 | 14.5 | 1,523 | 24.6 | 3,516 | 9.0 |
| 10–15 | 2,413 | 71.4 | 3,682 | 79.2 | 4,367 | 81.0 | 4,471 | 80.6 | 5,273 | 81.0 | 5,619 | 77.5 | 4,314 | 69.8 | 30,139 | 77.5 |
| ≥16 | 908 | 26.9 | 905 | 19.5 | 931 | 17.3 | 887 | 16.0 | 696 | 10.7 | 582 | 8.0 | 346 | 5.6 | 5,255 | 13.5 |
| Alcohol consumption | ||||||||||||||||
| Current drinkers | 1,959 | 48.1 | 2,607 | 48.1 | 2,896 | 46.2 | 3,077 | 40.4 | 3,219 | 34.3 | 3,137 | 31.0 | 2,276 | 26.0 | 19,171 | 37.1 |
| Former drinkers | 158 | 3.9 | 124 | 2.3 | 101 | 1.6 | 150 | 2.0 | 173 | 1.8 | 176 | 1.7 | 157 | 1.8 | 1,039 | 2.0 |
| Never drinkers | 1,956 | 48.0 | 2,690 | 49.6 | 3,275 | 52.2 | 4,386 | 57.6 | 5,999 | 63.9 | 6,817 | 67.3 | 6,320 | 72.2 | 31,443 | 60.9 |
| Smoking | ||||||||||||||||
| Current smokers | 442 | 10.9 | 557 | 10.3 | 649 | 10.4 | 697 | 9.2 | 653 | 7.0 | 474 | 4.7 | 252 | 2.9 | 3,724 | 7.2 |
| Former smokers | 567 | 14.0 | 544 | 10.1 | 610 | 9.8 | 649 | 8.6 | 613 | 6.6 | 514 | 5.1 | 337 | 3.9 | 3,834 | 7.5 |
| Never smokers | 3,042 | 75.1 | 4,292 | 79.6 | 4,975 | 79.8 | 6,230 | 82.2 | 8,089 | 86.5 | 9,124 | 90.2 | 8,145 | 93.3 | 43,897 | 85.3 |
| Sleep duration, hour/day | ||||||||||||||||
| <4.0 | 7 | 0.2 | 17 | 0.3 | 21 | 0.3 | 22 | 0.3 | 15 | 0.2 | 28 | 0.3 | 33 | 0.4 | 143 | 0.3 |
| 4.0–4.9 | 79 | 1.9 | 127 | 2.3 | 158 | 2.5 | 154 | 2.0 | 181 | 1.9 | 171 | 1.7 | 153 | 1.7 | 1,023 | 2.0 |
| 5.0–5.9 | 474 | 11.6 | 853 | 15.7 | 1,093 | 17.4 | 1,226 | 16.1 | 1,211 | 12.9 | 1,022 | 10.1 | 958 | 10.9 | 6,837 | 13.2 |
| 6.0–6.9 | 1,451 | 35.6 | 2,201 | 40.6 | 2,722 | 43.4 | 3,242 | 42.6 | 3,540 | 37.7 | 3,281 | 32.3 | 2,572 | 29.4 | 19,009 | 36.8 |
| 7.0–7.9 | 1,348 | 33.1 | 1,624 | 30.0 | 1,776 | 28.3 | 2,293 | 30.1 | 3,302 | 35.2 | 3,886 | 38.3 | 3,241 | 37.0 | 17,470 | 33.8 |
| 8.0–8.9 | 630 | 15.5 | 546 | 10.1 | 461 | 7.3 | 629 | 8.3 | 1,060 | 11.3 | 1,592 | 15.7 | 1,576 | 18.0 | 6,494 | 12.6 |
| ≥9.0 | 86 | 2.1 | 53 | 1.0 | 45 | 0.7 | 49 | 0.6 | 83 | 0.9 | 166 | 1.6 | 223 | 2.5 | 705 | 1.4 |
| Leisure time physical activity, min/week | ||||||||||||||||
| <30 | 1,931 | 49.2 | 2,602 | 49.2 | 2,811 | 46.3 | 3,071 | 41.7 | 3,235 | 35.7 | 2,795 | 28.9 | 2,123 | 25.8 | 18,568 | 37.4 |
| 30–59 | 346 | 8.8 | 442 | 8.4 | 465 | 7.7 | 510 | 6.9 | 574 | 6.3 | 486 | 5.0 | 408 | 5.0 | 3,231 | 6.5 |
| 60–119 | 508 | 12.9 | 733 | 13.9 | 763 | 12.6 | 1,020 | 13.9 | 1,190 | 13.1 | 1,193 | 12.3 | 970 | 11.8 | 6,377 | 12.9 |
| 120–179 | 384 | 9.8 | 566 | 10.7 | 692 | 11.4 | 856 | 11.6 | 1,150 | 12.7 | 1,312 | 13.6 | 1,059 | 12.9 | 6,019 | 12.1 |
| 180–299 | 311 | 7.9 | 423 | 8.0 | 586 | 9.7 | 825 | 11.2 | 1,129 | 12.5 | 1,275 | 13.2 | 1,163 | 14.1 | 5,712 | 11.5 |
| ≥300 | 446 | 11.4 | 522 | 9.9 | 751 | 12.4 | 1,082 | 14.7 | 1,777 | 19.6 | 2,600 | 26.9 | 2,499 | 30.4 | 9,677 | 19.5 |
| Psychological stress during the last year | ||||||||||||||||
| No stress | 23 | 0.6 | 35 | 0.7 | 61 | 1.0 | 110 | 1.5 | 180 | 1.9 | 358 | 3.6 | 480 | 5.5 | 1,247 | 2.5 |
| Low stress | 435 | 11.0 | 538 | 10.2 | 708 | 11.5 | 1,023 | 13.7 | 1,559 | 16.9 | 2,088 | 20.9 | 2,191 | 25.3 | 8,542 | 16.8 |
| Moderate stress | 1,897 | 47.8 | 2,553 | 48.3 | 2,968 | 48.4 | 3,676 | 49.4 | 4,623 | 50.0 | 4,971 | 49.7 | 4,235 | 48.8 | 24,923 | 49.1 |
| High stress | 1,615 | 40.7 | 2,163 | 40.9 | 2,398 | 39.1 | 2,632 | 35.4 | 2,879 | 31.2 | 2,578 | 25.8 | 1,764 | 20.3 | 16,029 | 31.6 |
| Personal disease history | ||||||||||||||||
| Diabetes | 18 | 0.4 | 39 | 0.7 | 73 | 1.2 | 156 | 2.2 | 375 | 4.3 | 538 | 5.7 | 555 | 6.9 | 1,754 | 3.6 |
| Hypertension | 61 | 1.5 | 155 | 2.9 | 359 | 5.7 | 829 | 11.5 | 1,659 | 18.9 | 2,445 | 25.6 | 2,618 | 32.0 | 8,126 | 16.4 |
| Dyslipidemia | 79 | 1.9 | 186 | 3.4 | 347 | 5.5 | 817 | 11.3 | 1,642 | 18.7 | 2,410 | 25.4 | 2,349 | 28.8 | 7,830 | 15.9 |
| Coronary heart disease | 8 | 0.2 | 12 | 0.2 | 28 | 0.5 | 67 | 1.0 | 146 | 1.7 | 334 | 3.6 | 359 | 4.5 | 954 | 2.0 |
| Stroke | 12 | 0.3 | 14 | 0.3 | 34 | 0.5 | 58 | 0.8 | 106 | 1.2 | 192 | 2.1 | 211 | 2.6 | 627 | 1.3 |
| Cancer | 144 | 3.7 | 218 | 4.3 | 327 | 5.5 | 447 | 6.6 | 657 | 7.9 | 845 | 9.3 | 685 | 8.8 | 3,323 | 7.1 |
DISCUSSION
The present report describes the study design and profile of participants in the baseline survey of the J-MICC Study, which incorporates 14 study regions from 12 prefectures. We found notable differences in the age distributions of the participants among the study region. There are two possible reasons. First, in the Fukuoka and Saga regions, the participants originally enrolled in the J-MICC Study were in principle limited to adults aged 50 years or older and 40 years or older, respectively. Second, according to the 2010 (the middle year of the baseline survey period) National Census of Japan, there was a 1.6-fold difference in the percentage of the population aged 65 years and older between the lowest (17.4%) and highest (27.0%) in the 12 prefectures including the study regions of the J-MICC Study.
Based on the obtained informed consent, we have already analyzed genomic information from a total of 14,539 participants who were selected to be genotyped from 13 study regions (except for the Iga region). Up to March 2020, we have already published several papers regarding genome-wide association analysis or gene–environmental interaction for health outcomes.12–22 Moreover, as a bioresources support system, we provide support for studies using biospecimens and data that were collected at the baseline survey of the J-MICC Study, which was also included in the informed consent. Our support includes providing biological resources and data regarding 92,000 individuals and genotype data for genome-wide association study from approximately 14,000 individuals. Information on support content is provided on the Platform of Supporting Cohort Study and Biospecimen Analysis webpage (http://cohort.umin.jp/english/about/bio-resource.html).
The main strengths of the J-MICC Study are as follows. First, we comprehensively collected data on both living circumstances and genomic information as risk factors of cancer and other lifestyle-related diseases. Such information would be useful to establish personalized or tailor-made lifestyle-related disease prevention methods. Our data might also be useful as a reference tool, because it allows to gain access to data on genotype distributions in a large, healthy Japanese population. Second, the J-MICC Study (started in 2005) was the first Japanese genome-cohort study collecting data from all over Japan, mainly in the western regions. The Japan Public Health Center-based Prospective Study for the Next Generation (JPHC-NEXT), a genome-cohort of over 100,000 people, was launched 6 years later.23 This large-scale, population-based prospective study has been designed to identify risk factors for lifestyle-related diseases, which can in turn contribute to the extension of healthy life expectancy and personalized healthcare. The J-MICC and JPHC-NEXT have conducted a validity study by examining all questionnaires for integrated analysis. Additionally, the Tohoku Medical Megabank Community-Based Cohort Study (TMM CommCohort Study) that began in 2013 was a large scale population-based prospective genome cohort mainly in the east coast of Miyagi and Iwate Prefectures in the Tohoku region to assess the long term impact of the Great East Japan Earthquake and to establish personalized prevention based on the genome, metabolome, and other omics information.24 The JPHC-NEXT, TMM CommCohort Study, Tsuruoka Metabolomics Cohort Study,25 and Yamagata Molecular Epidemiological Cohort Study26 use the same or similar questionnaire established in the J-MICC Study. In the near future, the integration of the J-MICC, JPHC-NEXT, TMM CommCohort Study, and others will finally set up a 300,000-strong cohort research base representing the whole of Japan.
Some potential limitations of the J-MICC Study should also be noted. First, the participation rate was not particularly high (33.5%); hence, our results may have been affected by selection bias. One possible explanation could be that the research sites targeting community inhabitants only mailed invitation letters or distributed leaflets for recruitment. Even in the research sites targeting health checkup examinees, many sites recruited participants only by sending a direct request for survey participation along with the health checkup invitation letter. Second, there were differences between research sites in terms of the recruitment methods (eg, mailing invitation letters or distributing leaflets to the general populations). Also, in some of the research sites, the participants received incentives, such as a small honorarium, which can link to selection bias. These differences, in turn, might be the reason why the region-specific participation rate ranged from 19.7% to 69.8%. Third, it is possible that health check-up attendees are more health conscious, suggesting a healthy volunteer effect in this cohort. For example, current smoking rates among this cohort (male 29.8%, female 7.2%) were slightly lower than those in the 2010 National Health and Nutrition Survey (NHNS) in Japan (male 32.2%, female 8.4%). Furthermore, with respect to history of disease, the rates of diabetes and hypertension among this cohort (diabetes: male 9.7%, female 3.6%; hypertension: male 25.6%, female 16.4%) were also lower compared to those in the 2010 NHNS in Japan (diabetes: male 16.6%, female 9.2%; hypertension: male 57.6%, female 42.2%). Thus, any generalizability of the study findings should be considered with caution. Fourth, our study did not include people over 70 years old. Our study population was 35–69 years of age, and at the beginning of the study, this age group had a greater weight of cancer incidence. Caution should be exercised while extending our findings to the general adult population, including the older adults. Lastly, the incidence rate of early-onset cancers in data from the Aichi Cancer Center will likely be higher than that in other study regions because first-visit patients were recruited at this cancer hospital. The Kanagawa region started the baseline survey about 10 years later than the region where the survey was first launched, so the impact of historical background of this region on the participant characteristics may be different. Thus, there was a problem in simply combining the data from all study regions in the analyses; hence, stratified and sensitivity analyses should be performed in future analyses.
In conclusion, in the J-MICC Study, lifestyle and clinical data and biospecimens were collected from more than 90,000 participants. The present report indicated the study design and identified the baseline characteristics of participants of the J-MICC study. This cohort is expected to be a valuable resource for the national and international scientific community in providing evidence supporting longer healthy lives.
ACKNOWLEDGMENTS
The authors are grateful to all the participants of the baseline survey of the J-MICC Study and the staff at each site for their cooperation. This study was funded by Grants-in-Aid for Scientific Research on Priority Areas of Cancer (No. 17015018) and on Innovative Areas (No. 221S0001), and that for Platform of Supporting Cohort Study and Biospecimen Analysis (CoBiA; JSPS KAKENHI Grant Number JP16H06277) from the Japanese Ministry of Education, Culture, Sports, Science and Technology. This study was supported in part by funding for the BioBank Japan Project from the Japan Agency for Medical Research and Development since April 2015, and the Ministry of Education, Culture, Sports, Science and Technology from April 2003 to March 2015.
Conflicts of interest: None declared.
REFERENCES
- 1.Tamakoshi A, Yoshimura T, Inaba Y, et al. ; JACC Study Group . Profile of the JACC study. J Epidemiol. 2005;15(Suppl 1):S4–S8. 10.2188/jea.15.S4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watanabe S, Tsugane S, Sobue T, Konishi M, Baba S. Study design and organization of the JPHC Study. J Epidemiol. 2001;11(6 Suppl):S3–S7. 10.2188/jea.11.6sup_3 [DOI] [PubMed] [Google Scholar]
- 3.Ministry of Health Labour and Welfare. Summary Report of Vital Statistics, 2018. https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/geppo/nengai18/dl/kekka30-19626.pdf. Published 2019. Accessed February 7, 2020.
- 4.Matsuo K, Hamajima N, Shinoda M, et al. Gene-environment interaction between an aldehyde dehydrogenase-2 (ALDH2) polymorphism and alcohol consumption for the risk of esophageal cancer. Carcinogenesis. 2001;22:913–916. 10.1093/carcin/22.6.913 [DOI] [PubMed] [Google Scholar]
- 5.Suzuki T, Matsuo K, Sawaki A, et al. Alcohol drinking and one-carbon metabolism-related gene polymorphisms on pancreatic cancer risk. Cancer Epidemiol Biomarkers Prev. 2008;17:2742–2747. 10.1158/1055-9965.EPI-08-0470 [DOI] [PubMed] [Google Scholar]
- 6.Park JY, Matsuo K, Suzuki T, et al. Impact of smoking on lung cancer risk is stronger in those with the homozygous aldehyde dehydrogenase 2 null allele in a Japanese population. Carcinogenesis. 2010;31:660–665. 10.1093/carcin/bgq021 [DOI] [PubMed] [Google Scholar]
- 7.Higashibata T, Hamajima N, Naito M, et al. ENOS genotype modifies the effect of leisure-time physical activity on serum triglyceride levels in a Japanese population. Lipids Health Dis. 2012;11:150. 10.1186/1476-511X-11-150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hishida A, Wakai K, Naito M, et al. ; J-MICC Study Group . Polymorphisms of genes involved in lipid metabolism and risk of chronic kidney disease in Japanese - cross-sectional data from the J-MICC study. Lipids Health Dis. 2014;13:162. 10.1186/1476-511X-13-162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White E, Hunt JR, Casso D. Exposure measurement in cohort studies: the challenges of prospective data collection. Epidemiol Rev. 1998;20:43–56. 10.1093/oxfordjournals.epirev.a017971 [DOI] [PubMed] [Google Scholar]
- 10.Hamajima N; J-MICC Study Group . The Japan Multi-institutional Collaborative Cohort Study (JMICC Study) to detect gene-environment interactions for cancer. Asian Pac J Cancer Prev. 2007;8:317–323. [PubMed] [Google Scholar]
- 11.Naito M, Eguchi H, Okada R, et al. ; J-MICC Study Group . Controls for monitoring the deterioration of stored blood samples in the Japan Multi-Institutional Collaborative Cohort Study (J-MICC Study). Nagoya J Med Sci. 2008;70:107–115. 10.18999/nagjms.70.3-4.107 [DOI] [PubMed] [Google Scholar]
- 12.Shimanoe C, Hachiya T, Hara M, et al. A genome-wide association study of coping behaviors suggests FBXO45 is associated with emotional expression. Genes Brain Behav. 2019;18:e12481. 10.1111/gbb.12481 [DOI] [PubMed] [Google Scholar]
- 13.Nakamura Y, Narita A, Hachiya T, et al. A genome-wide association study in the diabetic patients finds the 13q35.43-35.46 locus associated with estimated glomerular filtration rate: the Japan Multi-Institutional Collaborative Cohort Study. J Clin Diabetes. 2018;2:102. [Google Scholar]
- 14.Hishida A, Nakatochi M, Akiyama M, et al. ; Japan Multi-Institutional Collaborative Cohort (J-MICC) Study Group . Genome-wide association study of renal function traits: results from the Japan Multi-Institutional Collaborative Cohort Study. Am J Nephrol. 2018;47:304–316. 10.1159/000488946 [DOI] [PubMed] [Google Scholar]
- 15.Nakatochi M, Kanai M, Nakayama A, et al. Genome-wide meta-analysis identifies multiple novel loci associated with serum uric acid levels in Japanese individuals. Commun Biol. 2019;2:115. 10.1038/s42003-019-0339-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fujii R, Hishida A, Nakatochi M, et al. Association of genetic risk score and chronic kidney disease in a Japanese population. Nephrology (Carlton). 2019;24:670–673. 10.1111/nep.13479 [DOI] [PubMed] [Google Scholar]
- 17.Nishiyama T, Nakatochi M, Goto A, et al. Genome-wide association meta-analysis and Mendelian randomization analysis confirm the influence of ALDH2 on sleep durationin the Japanese population. Sleep. 2019;42:zsz046. 10.1093/sleep/zsz046 [DOI] [PubMed] [Google Scholar]
- 18.Koyama T, Kuriyama N, Ozaki E, et al. Genetic variants of RAMP2 and CLR are associated with stroke. J Atheroscler Thromb. 2017;24:1267–1281. 10.5551/jat.41517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakagawa-Senda H, Hachiya T, Shimizu A, et al. A genome-wide association study in the Japanese population identifies the 12q24 locus for habitual coffee consumption: the J-MICC Study. Sci Rep. 2018;8:1493. 10.1038/s41598-018-19914-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hara M, Hachiya T, Sutoh Y, et al. Genomewide association study of leisure-time exercise behavior in Japanese adults. Med Sci Sports Exerc. 2018;50:2433–2441. 10.1249/MSS.0000000000001712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Usui Y, Matsuo K, Oze I, et al. Impact of PSCA polymorphisms on the risk of duodenal ulcer. J Epidemiol. 2019. 10.2188/jea.JE20190184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iwase M, Matsuo K, Nakatochi M, et al. Differential effect of polymorphisms on body mass index across the life course of Japanese: the Japan Multi-Institutional Collaborative Cohort Study. J Epidemiol. 2020. 10.2188/jea.JE20190296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sawada N, Iwasaki M, Yamaji T, et al. The Japan Public Health Center-based Prospective Study for the Next Generation (JPHC-NEXT): study design and participants. J Epidemiol. 2020;30:46–54. 10.2188/jea.JE20180182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hozawa A, Tanno K, Nakaya N, et al. Study profile of The Tohoku Medical Megabank Community-Based Cohort Study. J Epidemiol. 2020. 10.2188/jea.JE20190271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tsuruoka Metabolomics Cohort Study (in Japanese). http://tsuruoka-mirai.net/modules/contents/aisatsu.html. Accessed March 6, 2020.
- 26.Yamagata University Genomic Cohort Consortium, Narimatsu H. Constructing a contemporary gene-environmental cohort: study design of the Yamagata Molecular Epidemiological Cohort Study. J Hum Genet. 2013;58:54–56. 10.1038/jhg.2012.128 [DOI] [PubMed] [Google Scholar]