Abstract
Introduction
Patients living with biliary tract cancer (BTC) experience a decline in health-related quality of life (HRQoL). This study aimed to obtain a comprehensive understanding of the patient experience of BTC-related signs/symptoms and the impacts of these on daily functioning and HRQoL.
Methods
Patients with BTC participated in qualitative semi-structured concept elicitation interviews. Signs/symptoms and impacts of BTC were initially explored by targeted literature searches and interviews with five clinicians. Patient interviews were transcribed and coded using qualitative research software. Concept saturation was assessed over five interview waves. A sign/symptom or impact was defined as “salient” if mentioned by ≥ 50% of patients, with a mean disturbance rating of ≥ 5 (0–10 scale). A conceptual model of the patient experience of BTC-related signs/symptoms and impacts was produced.
Results
Twenty-three patients from the USA (78% women; median age: 54 years), diagnosed as having early (n = 3), locally advanced (n = 11) or metastatic (n = 9) disease, were interviewed. Sixty-six signs/symptoms and 12 impacts were identified. Of these, 46 signs/symptoms and 8 impacts were not identified from the targeted literature or clinician interviews. Concept saturation was reached by the fourth of five interview waves. Fourteen disease-related signs/symptoms (including fatigue/lack of energy, abdominal pain, lack of appetite, insomnia and diarrhoea) and three impacts (physical, emotional and cognitive impacts) were deemed “salient”. The conceptual model included 50 signs/symptoms and 12 impacts.
Conclusion
Patients with BTC reported a range of signs/symptoms and impacts that negatively affect daily functioning and HRQoL.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40487-021-00159-z.
Keywords: Biliary tract cancer, Interview study, Qualitative research
Key Summary Points
| Why carry out this study? |
| Patients living with biliary tract cancer (BTC) experience a decline in health-related quality of life (HRQoL). |
| This study aimed to obtain a comprehensive understanding of the patient experience of BTC-related signs/symptoms and the impacts of these on daily functioning and HRQoL. |
| What was learned from the study? |
| Qualitative interviews in patients diagnosed with BTC identified signs/symptoms and impacts associated with the disease experience, including some that may not have been previously identified by the literature and clinicians experienced in treating BTC. |
| Understanding patient experience can inform the selection of patient-reported outcomes in clinical trials of BTC treatments. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to 10.6084/m9.figshare.14762973.
Introduction
Biliary tract cancer (BTC; also known as bile duct cancer) includes malignancy of the perihilar, distal and intrahepatic bile ducts and gall bladder [1]. While the incidence of BTC is low in Western countries (0.35–2 cases per 100,000 population), studies report that the frequency of cases has increased progressively over the past four decades [2, 3]. The incidence of BTC is generally higher in Asian and South American countries when compared with the rest of the world [4]. In Northeast Thailand, BTC is the most common type of cancer and, accordingly, the region has the highest prevalence of BTC worldwide (> 80 cases per 100,000 population) [5–7]. With the exception of the earlier stages of gall bladder cancer, which have 5-year survival rates of between 50% and 80%, the prognosis for BTC is poor across all stages of disease, with 5-year survival rates of 5–30% [4]. One factor that is likely to contribute to these poor survival rates is that BTCs are often diagnosed at an inoperable or even at a metastatic stage [8–10]. Further, despite potentially curative surgical removal for localized disease, relapse rates are high [11]. For patients with late-stage disease, palliative treatment may be the only option, usually in the form of chemotherapy.
Patients with BTC have reduced health-related quality of life (HRQoL) due to a combination of tumour- and treatment-related signs or symptoms (signs/symptoms) and the impact of these signs/symptoms on functioning. Tumour-related signs/symptoms vary depending on tumour type, location and stage of the disease [12]. Signs/symptoms reported in the literature include jaundice/yellow skin colour, pain/discomfort in stomach area, back pain, other unspecified pain, nausea, fatigue/lack of energy, weight loss, sleep problems, lack of appetite and general unwell feeling [13–18]. Impacts mentioned in the literature include anxiety, inability to do usual activities, depressive mood, trouble meeting the needs of the family and financial difficulties [13, 16, 18]. Patients’ HRQoL tends to decline as the disease becomes more advanced. This may, in part, be associated with patients undergoing more invasive surgical procedures, systemic chemotherapeutic treatments and/or palliative treatments during the later stages of BTC [19, 20].
Patient-reported outcome (PRO) questionnaires are increasingly being utilized to assess outcomes in cancer and are often recommended by regulatory agencies to evaluate the impact of the disease and treatment on patient-reported symptoms, functioning and HRQoL [21–23]. In the development of a new PRO questionnaire or the assessment of whether an existing questionnaire is fit for purpose, the concepts that need to be covered are identified from the published literature, interviews with clinicians experienced in treating the target patient population and, most importantly, interviews with patients [24]. Concept elicitation interviews with patients can capture in-depth qualitative information of the experience of patients living with a disease and can be used to assess whether a PRO questionnaire effectively captures relevant concepts of the patient experience, such as disease- and treatment-related symptoms.
There is a lack of data on the lived experience of patients with BTC, particularly studies that consider the patient experience at different disease stages; the limited studies available focus on the patient experience of specific oncological treatments [25, 26] or patient involvement in care [27]. This lack of data may be reflective of the relative rarity of BTCs. The aim of the current study was to obtain a comprehensive understanding of the patient experience of BTC-related signs/symptoms and impacts on daily functioning and HRQoL, at different stages of disease and for various BTC subtypes, to guide patient-centred outcomes measurement.
Methods
This was a qualitative patient interview study, which led to the development of a conceptual model of the patient experience of BTC. An initial literature search (identifying BTC-related signs/symptoms, impacts and existing PRO questionnaires) and qualitative interviews with clinicians were also performed to guide the patient interviews. The qualitative interview, research protocol, interview guide and all patient communication documents were reviewed and approved by the New England Institutional Review Board (NEIRB) in January 2019.
Targeted Literature Search
A preliminary all-stage conceptual model of disease-related signs/symptoms and impacts in patients with BTC was developed from targeted literature searches in PubMed of published articles from 1 January 2013 to 16 August 2018. This data search was used to inform a clinical trial starting 16 April 2019. Search terms included BTC disease-related, patient experience and PRO terms (Supplementary Table 1).
Qualitative Interviews
Clinician Interviews
Semi-structured interviews were conducted over the telephone with clinicians experienced in treating BTC in Italy, Japan, Spain, South Korea and the USA. Interviews lasted approximately 75 min and were conducted by three trained interviewers (one male and two female research consultants, educated to MSc or PhD level, including author Xandra Lie) experienced in qualitative research across a wide range of therapeutic areas. Interviewers were without bias or assumptions regarding this study. There was no relationship between interviewers and clinicians prior to study commencement. The interviews were conducted using a standardized interview guide with open-ended and prompted questions to explore the symptoms and impacts that the clinicians observed in patients with BTC. Clinicians reviewed the concepts identified from the review of the literature.
Patient Interviews
Twenty-three patients from the USA were recruited for the interview study with assistance from the patient advocacy group, the Cholangiocarcinoma Foundation (CCF) (https://cholangiocarcinoma.org/). Participants provided consent online and then answered several screening questions to confirm eligibility. Eligibility criteria included being ≥ 18 years old with a diagnosis of BTC, including cholangiocarcinoma (perihilar, distal or intrahepatic) and/or gall bladder carcinoma, based on histological/radiological confirmation and physician diagnosis confirmation forms. Patients with early (stage I, gall bladder and perihilar BTC, or distal or intrahepatic BTC), locally advanced (stage II–IVA, gall bladder or perihilar BTC, or stage II–III, distal or intrahepatic BTC) and metastatic (stage IVB, gall bladder or perihilar BTC, or stage IV, distal or intrahepatic BTC) disease were included in this study. All 23 recruited patients participated in this study.
Patient Interview Procedure
A semi-structured interview guide was developed, informed by data gathered from the qualitative literature review and clinician interviews. The telephone interviews were conducted by three trained interviewers (one male and two female research consultants, educated to MSc or PhD level) with experience in conducting individual patient concept elicitation interviews, and lasted between 75 and 90 min each; other project team members were occasionally present on the calls for training purposes (with permission from the patient). There was no relationship between interviewers and patients prior to study commencement. Participants were made aware that the output of the interview may contribute to the development of new BTC treatments. Participants were asked a set of open-ended questions, and interviewers followed up with probing questions as needed to explore the patient experience of concepts that patients did not mention spontaneously. Patients were asked about their first experience of the condition and how their experience may have changed over time, and were asked to list and discuss the current signs/symptoms and impacts of the condition and its treatments. To further explore the underlying causes of symptoms, during the interview patients were asked whether they thought symptoms were “disease-related”, “treatment-related” or “disease- and treatment-related”, as well as whether a symptom was experienced before, during or after treatment. No further interviews were conducted, and patients did not provide feedback on the findings. The interview methodology utilized in this study is in line with recommendations provided by the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Good Research Practices Task Force [24].
Data Analysis
The subtype of participants’ BTC (intrahepatic, perihilar or gall bladder cancer) was recorded to enable sub-group analysis. Prior to descriptive coding, patient interviews were recorded, transcribed and anonymized for thematic analysis. The interview transcripts were then coded, using a codebook developed from the preliminary conceptual model using qualitative research software (Atlas.ti v8, Atlas.ti Scientific Software Development GmbH, Germany). Two researchers coded the same transcripts independently, testing for inter-coder agreement after each transcript and discussing changes to the codebook and coding rules. After three transcripts, the coders achieved good inter-coder agreement (predefined as Krippendorff’s C-alpha binary > 0.7 [28]), and the remaining transcripts were divided among the coders. During coding, spot checks were conducted to ensure the codes made sense based on patient response and code language, and groupings were refined as needed. The frequency of concepts was cross-checked with live capture sheets that were filled in during the interviews by the interviewers. Concepts were deemed “salient” if ≥ 50% of patients mentioned the concept and it had a disturbance rating of ≥ 5 on a scale of 0–10, where 0 is “not disturbing” and 10 is “very disturbing”.
Concept Saturation
The principle of concept saturation was used to assess the adequacy of the sample size [24]. A sample size of 12–25 participants is optimal for concept elicitation interviews and for reaching saturation of concept [29–31]. Transcripts were grouped chronologically into five groups (four groups consisting of five interviews and one group with three interviews). To evaluate concept saturation, the concepts derived from each group were compared with concepts from previous groups to determine whether any new concepts were present. If new concepts appeared in the transcripts from the next group, saturation had not yet been achieved. Data saturation was not discussed with patients.
All-Stage Conceptual Model
Signs/symptoms or impacts related to BTC were used to construct a model of concepts for the patient experience of early, locally advanced and metastatic disease stages and BTC subtypes. An initial conceptual model was created from the reviews of the literature and was refined and finalized based on the qualitative clinician and patient interviews. The final conceptual model highlighted the concepts that were considered salient. Signs/symptoms or impacts deemed by patients and clinicians to be exclusively treatment-related were not included in the conceptual model.
Results
Targeted Literature Search
No recent BTC-related qualitative research studies were identified from the literature review. Six non-qualitative studies were identified (two retrospective cohort studies and four prospective studies) [14, 32–36], and 19 concepts related to signs/symptoms or impacts of BTC were extracted from these and included in the preliminary conceptual model. These studies used validated questionnaires to assess patients’ HRQoL in the physical, mental and social domains in the context of BTC [14, 32–36]. The preliminary conceptual model developed from the literature was used to help guide the qualitative interviews.
Qualitative Interviews
Clinician Interviews
Five clinicians, specialized in hepato-oncology and with experience in treating patients with BTC, prioritized four (out of 14) signs/symptoms of BTC (abdominal pain, lack of appetite, fatigue/lack of energy, pruritus/itching) and two (out of five) disease-related impacts (decreased physical functioning and insomnia) identified in the literature searches. Based on the clinician interviews, several key changes were made to the preliminary conceptual model. Constipation and diarrhoea were removed because they were considered treatment-related. Revised groupings were made for (1) nausea/queasiness; (2) itching; (3) jaundice, yellow skin/yellow eyes/changes in urine; and (4) fever/chills. Based on the clinician interviews, additional symptoms, including vomiting, difficulty eating/feeling of fullness and muscle loss, were identified.
Patient Interviews
A total of 23 patients from the USA who had BTC were interviewed (78% women; median age: 54 years [range 27–80]). Patients were diagnosed as having early (n = 3), locally advanced (n = 11) or metastatic (unresectable; n = 9) disease and with BTC subtypes of gall bladder cancer (n = 1), intrahepatic (n = 17) or perihilar (n = 5). Patient demographics and clinical characteristics are summarized in Table 1. Procedures and pharmaceutical therapies received as part of BTC treatment are summarized in Supplementary Table 2. Patient interviews identified 78 concepts (66 signs/symptoms and 12 impacts). For some interviews, insufficient time was available to discuss all disturbance ratings. Consequently, the number of patients who mentioned a disturbance rating for a sign/symptom or impact does not always equal the number of patients who mentioned the sign/symptom or impact (Figs. 1 and 2). Of these, 46 signs/symptoms and eight impacts had not been identified from the targeted literature searches or clinician interviews.
Table 1.
Demographic and clinical characteristics of patients participating in qualitative interviews
| Demographic characteristic | Patients (N = 23) |
|---|---|
| Sex, n (%) | |
| Female | 18 (78) |
| Male | 5 (22) |
| Age, years | |
| Mean (SD) | 55 (12.8) |
| Median (range) | 54 (27–80) |
| Tumour status at time of interview, n (%) | |
| Earlya | 3 (13) |
| Locally advancedb | 11 (48) |
| Metastaticc | 9 (39) |
| Ethnicity, n (%) | |
| Caucasian | 23 (100) |
| Disease subtype, n (%) | |
| Perihilar | 5 (22) |
| Intrahepatic | 17 (74) |
| Gall bladder | 1 (4) |
| Education, n (%) | |
| Bachelor’s/graduate degree | 14 (61) |
| Some years of college education | 4 (17) |
| High school | 5 (22) |
BTC biliary tract cancer, SD standard deviation
aStage I, gall bladder and perihilar BTC, or distal or intrahepatic BTC
bStage II–IVA, gall bladder or perihilar BTC, or stage II–III, distal or intrahepatic BTC
cStage IVB, gall bladder or perihilar BTC, or stage IV, distal or intrahepatic BTC
Fig. 1.
BTC signs/symptoms by frequency and average disturbance rating (N = 23). For some interviews, insufficient time was available to discuss all disturbance ratings. Consequently, the number of patients who mentioned a disturbance rating for a sign/symptom does not always equal the number of patients who mentioned the sign/symptom. Eight signs/symptoms received no disturbance rating. Salient signs/symptoms are underlined. BTC biliary tract cancer
Fig. 2.
BTC impacts by frequency and average disturbance rating (N = 23). For some interviews, insufficient time was available to discuss all disturbance ratings. Consequently, the number of patients who mentioned a disturbance rating for an impact does not always equal the number of patients who mentioned the impact. BTC biliary tract cancer
Signs/symptoms not previously identified from the targeted literature search and clinician interviews were related to pain and discomfort (e.g. stomach pain, dull ache, tenderness), gastrointestinal (GI) signs/symptoms (intestinal gas), strength (muscle tension, weakness), weight changes (weight gain), hair (hair loss, hair change), pain and discomfort in other parts of the body (headaches, head/ear pressure changes), skin (nail changes, rash), general unwell feeling (flu-like symptoms, aching all over) and urogenital (dark urine, urinary tract infection, urgency to urinate). Signs/symptoms related to circulatory issues (e.g. sepsis, blood clot), throat/mouth signs/symptoms (e.g. dry mouth, cannot drink fluid), the senses (change in taste, problem with hearing, sensitivity to noise), the eyes (vision changes, dry eyes) and extremities (hand and foot syndrome, swollen ankles/arms/legs, neuropathy) were not identified in the literature search or mentioned by the clinicians. Several signs/symptoms and impacts identified in the patient interviews were variations of concepts previously identified in the literature search and clinician interviews. In the literature search, insomnia was associated only with itching; however, patients mostly mentioned insomnia in association with worries and anxieties, aching and pain.
Across the three disease stages, 14 disease-related signs/symptoms (Table 2) and two treatment-related signs/symptoms were deemed salient. Fatigue/lack of energy was reported by all patients, with the highest mean disturbance rating (7.9, the mean of 21 patients’ ratings) of all signs/symptoms. Abdominal pain was the second most commonly reported symptom (mentioned by 19 patients), with a high mean disturbance rating of 7.6 (the mean of 16 patients’ ratings). Other salient disease-related signs/symptoms were lack of appetite, difficulty eating/feeling of fullness, abdominal bloating, diarrhoea, nausea/queasiness, constipation, insomnia, other pain, itchy skin, fever/chills, sensitivity to cold and muscle loss. Patients also deemed three impacts to be salient (Table 3); these were physical impacts (difficulty walking) mentioned by 22 patients, with a mean disturbance rating of 7.5 (the mean of 15 patients’ ratings), emotional impacts (depression) mentioned by 17 patients, with a mean disturbance rating of 8.5 (the mean of 15 patients’ ratings), and cognitive impacts (memory loss, fuzzy brain) mentioned by 14 patients, with a mean disturbance rating of 8.2 (the mean of 15 patients’ ratings).
Table 2.
Salient sign and symptom concepts and example quotations elicited from patients with BTC (N = 23)
| Sign/symptom | Patients mentioning sign/symptom, n (%)a | Mean disturbance rating (number of patients rated)b | Example patient quotation (stage, subtype) |
|---|---|---|---|
| Fatigue/lack of energy | 23 (100) | 7.9 (21) | “I’m just fatigued. The fatigue is probably the biggest [symptom] … Chemo obviously makes it a little worse, but even just in general, like even between my stints, I am just really tired.” (metastatic, perihilar) |
| Abdominal pain | 19 (83) | 7.6 (16) | “At the time of diagnosis, the [abdominal pain] was the worst pain I’ve ever had. I remember thinking, ‘This is worse than natural childbirth’. It was truly the worst pain, I couldn’t move. I remember I was kind of hunched over, and I couldn’t straighten up.” (metastatic, intrahepatic) |
| Lack of appetite | 18 (78) | 5.8 (16) | “… a lot of times, I don’t even have the sensation that I’m hungry. I just have to eat knowing that you need the nourishment and stuff. I’m still that way.” (locally advanced, intrahepatic) |
| Difficulty eating/feeling of fullness | 18 (78) | 5.8 (13) | “I would become hungry, but once I started to eat, I became full very quickly.” (metastatic, intrahepatic) |
| Abdominal bloating | 16 (70) | 5.8 (9) | “Sometimes it’s like, ‘Gosh, I feel like I’m maybe too full,’ and I kind of look down and it’s like, ‘You're looking a little puffy today.’ And then a day or so later I don’t see it.” (locally advanced, intrahepatic) |
| Diarrhoea | 17 (74) | 6.1 (14) | “That was pretty much throughout the whole six months of the … the gastrointestinal issues … I started having violent diarrhoea, and so I wasn’t keeping any of the nutrients.” (locally advanced, intrahepatic) |
| Nausea/queasiness | 15 (65) | 6.4 (15) | “… Nauseous all the time. I mainly just wanted to eat simple foods, like soup or mashed potatoes.” (metastatic, intrahepatic) |
| Constipation | 12 (52) | 6.4 (10) | “I can go from being extremely constipated to having five, six, seven loose stools in a day.” (metastatic, intrahepatic) |
| Insomnia | 18 (78) | 7.3 (9) | “I live alone, and you get in bed, and your mind starts wandering. Yeah. I have terrible problems with insomnia.” (locally advanced, perihilar) |
| Other pain | 14 (61) | 6.9 (11) | “To touch in my armpit areas hurts … it's more just if I touch it. Because I'm washing under my armpit or if I were to just touch underneath my armpits, it feels really tender and sore, which is a weird spot. Because I've never had anything like it.” (early, intrahepatic) |
| Itchy skin | 14 (61) | 7.2 (13) | “I would just have this terrible itching, mainly up in the upper body but sometimes my legs too.” (early, intrahepatic) |
| Fever/chills | 15 (65) | 6.4 (13) | “It was horrible because I’d be hot and then take stuff off and then I’d be cold, and I’d put it on. It was back and forth like a yo-yo all day long.” (locally advanced, gall bladder) |
| Sensitivity to cold | 13 (57) | 6.1 (11) | “Ever since I’ve been on chemotherapy, I find that I don’t tolerate the cold like I used to. I get cold very easily, and that’s something that has not gone away.” (locally advanced, intrahepatic) |
| Muscle loss | 16 (70) | 6.2 (11) | “I think due to the fatigue and the lack of nourishment, they [muscle] just atrophied.” (metastatic, intrahepatic) |
Patient-reported signs and symptoms of BTC could be related to disease and/or current or past treatments
BTC biliary tract cancer
aSpontaneously mentioned or prompted
bFor some interviews, insufficient time was available to discuss all disturbance ratings. Consequently, the number of patients who mentioned a disturbance rating for a sign/symptom does not always equal the number of patients who mentioned the sign/symptom
Table 3.
Salient impact concepts and example quotations elicited from patients with BTC (N = 23)
| Impact | Patients mentioning impact, n (%)a | Mean disturbance rating (number of patients rated)b | Example patient quotation (stage, subtype) |
|---|---|---|---|
| Physical impacts (difficulty walking) | 22 (96) | 7.5 (15) | “I’ve kind of, the last few months, just gotten to where I ask for a wheelchair at the airport, because I figure why should I spend all my energy trying to get from one end of the airport to the other, when they can just take me. I have given in to that symptom, just because I have to work hard to breath when I’m walking very far.” (metastatic, intrahepatic) |
| Emotional impacts (depression) | 17 (74) | 8.5 (15) | “Yeah, the depression, and it really, really hit me after treatment, to the point to where my doctor added an antidepressant for me.” (locally advanced, intrahepatic) |
| Cognitive impacts (memory loss, fuzzy brain) | 14 (61) | 8.2 (13) | “Or the brain fog and you can’t concentrate on anything and [the children] want to tell me all about the game they’re playing or how the day was. It’s like it’s not sinking in at all. They could be speaking in a foreign language and I wouldn’t have known.” (locally advanced, gall bladder) |
BTC biliary tract cancer
aSpontaneously mentioned or prompted
bFor some interviews, insufficient time was available to discuss all disturbance ratings. Consequently, the number of patients who mentioned a disturbance rating for an impact does not always equal the number of patients who mentioned the impact
Signs/Symptoms and Impacts Across Disease Subtypes
The following signs/symptoms were mentioned by patients across all disease subtypes of intrahepatic, perihilar and gall bladder: fatigue/lack of energy, insomnia, dry mouth, cough/throat irritation/voice change, hair loss, abdominal pain, other pain, back pain, sensitivity to cold, change in taste, muscle loss or weight loss. The salient sign/symptom of itchy skin was mentioned by 10 of 17 patients with the intrahepatic subtype and four of five patients with the perihilar subtype, but not by the patient with the gall bladder subtype. Emotional and cognitive impacts and experiencing difficulties in meeting the needs of family were impacts mentioned by all patients. Concepts relating to physical impacts were mentioned by all patients with the perihilar subtype and by 16 of 17 patients with intrahepatic BTC. Financial burden was mentioned by nine of 17 patients with the intrahepatic subtype and by two of five patients with the perihilar subtype. Across the disease subtypes patients generally reported similar salient signs/symptoms. Impacts were also similar across subtypes. Physical impacts were mentioned by 16 of 17 patients with intrahepatic BTC and by five of five patients with perihilar BTC. Emotional impacts were mentioned by 13 of 17 patients with intrahepatic BTC and by three of five patients with perihilar BTC. Cognitive impacts were mentioned by 10 of 17 patients with intrahepatic BTC and by three of five patients with perihilar BTC. The single patient with gall bladder BTC did not mention physical impacts but did mention emotional and cognitive impacts.
Signs/Symptoms and Impacts by Disease Stage
While fatigue, insomnia and GI signs/symptoms were salient signs/symptoms experienced by patients at all disease stages, several signs/symptoms and impacts were particularly relevant in specific disease stages. A total of 27 signs/symptoms and nine impacts were mentioned by patients with early-stage BTC (n = 3). Nail changes (which were not included in the all-stage conceptual model due to being deemed by patients and clinicians to be treatment-related) and rash were signs/symptoms specific to the early stage. Jaundice and weight loss were not reported by patients with early-stage cancer. A total number of 41 signs/symptoms and 11 impacts were mentioned by patients with locally advanced BTC (n = 11). Three patients with locally advanced BTC mentioned flu-like symptoms (not including chills or cough), while rash, abdominal tenderness and intestinal gas were each only mentioned by one patient. The impact “inability to travel” was specific to locally advanced BTC. For patients with metastatic BTC (n = 9), 41 signs/symptoms and 10 impacts were mentioned. Signs/symptoms specific to patients with metastatic BTC included heartburn, problems with hearing, headaches, intestinal pain, mouth sensitivity and hypercalcaemia.
Concept Saturation
Concept saturation was reached by the fourth and third of five interview waves for signs/symptoms and impacts, respectively. Of the 79 concepts identified, 49% (39 concepts) were mentioned in the first wave.
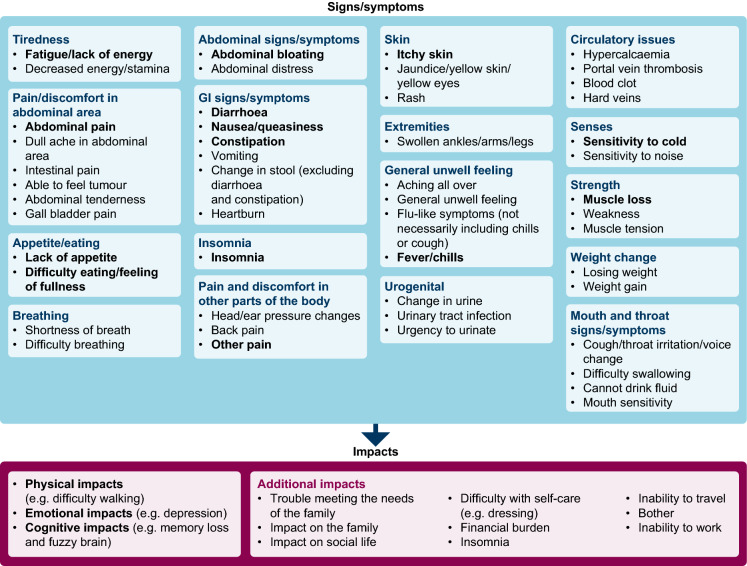
Conceptual Model of the BTC Patient Experience
The final all-stage conceptual model for the patient experience of BTC includes 50 signs/symptoms and 12 impacts (Fig. 3). Of these, 14 signs/symptoms and three impacts were salient. Salient signs/symptoms were fatigue/lack of energy, abdominal pain, lack of appetite, difficulty eating/feeling of fullness, abdominal bloating, diarrhoea, nausea/queasiness, constipation, insomnia, other pain, itchy skin, fever/chills, sensitivity to cold and muscle loss. All salient impacts were reported in all three stages of BTC and were physical impacts (e.g. difficulty walking), emotional impacts (e.g. depression) and cognitive impacts (e.g. memory loss, fuzzy brain). An additional two signs/symptoms (hair loss and change in taste) were salient but were not included in the final model because they were deemed to be associated with some treatments (treatment-related signs/symptoms are summarized in Supplementary Table 3).
Fig. 3.
All-stage disease-specific conceptual model for the patient experience of BTC. Bold signifies salient concepts, defined as mentioned by > 50% of patients (N = 23) and an average disturbance rating of > 5. BTC biliary tract cancer, GI gastrointestinal
Discussion
Direct patient input through semi-structured qualitative interviews provides a comprehensive understanding of disease and treatment experience from the patient perspective and is crucial to inform fit-for-purpose patient-centred outcome measurement strategies for clinical trials. In this qualitative study, targeted literature searches and clinician interviews were conducted to develop a preliminary BTC conceptual model and to guide patient interviews. The concept elicitation method was used to gain a further understanding of the experience with BTC directly from patients. Following the patient interviews, the preliminary conceptual model was refined and finalized to represent a patient-centred perspective of the lived experience of BTC. To our knowledge, the all-stage conceptual model developed in the current study is the first of its kind. Patients with BTC experience reduced HRQoL [19, 36, 37], and this was reflected in the current study. Patients with BTC mentioned 46 signs/symptoms and eight impacts of BTC that had not been identified from the targeted literature and clinician interviews, highlighting the importance of obtaining information on the patient experience directly from patients and suggesting a need to ensure fit-for-purpose patient-centred outcomes measurement in BTC clinical trials.
Signs/symptoms not previously identified from the targeted literature search and clinician interviews were related to pain and discomfort, GI signs/symptoms, senses, strength, weight gain, hair, mouth and throat signs/symptoms, skin, extremities and general unwell feeling. Several concepts that were not previously reported were variations of concepts identified in the targeted literature search and clinician interviews. For example, in the preliminary literature search, insomnia was associated only with itching; however, patients interviewed in this study mostly mentioned insomnia in association with worries and anxieties, aching and pain, emphasizing the importance of performing qualitative interviews in gaining patient perspectives.
Across disease stages and of all reported concepts, those rated most disturbing by patients were emotional and cognitive impacts. Physical impacts, while more frequently reported than emotional and cognitive impacts, were deemed slightly less disturbing by patients. These findings demonstrate the significance of psychosocial assessment in BTC and suggest the need for psychosocial supportive care for patients with BTC at all stages of the disease. Overall, the all-stage disease-specific conceptual model for BTC comprises 50 sign/symptoms and 12 impacts related to BTC. Seventeen of these concepts were deemed to be salient; that is, they were prevalent and highly disturbing (reported by more than 50% of patients, with a disturbance rating of ≥ 5 out of 10).
Diagnosis of BTC in patients typically occurs at a later stage in the disease [8]; this is reflected in this study by fewer patients recruited with early-stage BTC than the number of patients with locally advanced or metastatic stages. The small sample size of patients with early-stage BTC (n = 3) in this study should be considered when interpreting data, and suggests that the findings of this study are more applicable to drug development in advanced disease. Patients with early-stage BTC experienced a smaller number of symptoms than did patients with later stages of BTC, although some salient signs/symptoms that occurred at the early stage of BTC were commonly reported throughout the disease stages. The salient signs/symptoms experienced by patients at all disease stages were fatigue, insomnia and GI signs/symptoms.
This study had several strengths. It had a specific focus on BTC, and the collection of signs/symptoms and impacts from qualitative patient interviews was robust and overarching. Sample sizes were adequate, as demonstrated by the saturation of concepts at the fourth and third of five waves for signs/symptoms and impacts, respectively. Further, the study population was representative in terms of age; a pooling of data from several BTC studies calculated a median age (interquartile range) of 58 (51–65) years [38], which is comparable to the current study in which a median age of 54 years was determined.
Various key factors influence the risk of developing BTC, including age, sex, ethnicity and the presence of comorbidities [38–40]. The cohort of patients in this study was solely from the USA, which in general presents lower rates of BTC than those seen in Asian and South American populations [4]. Sex ratios can vary according to geographical location and ethnicity; for example, in Chile, of 23,716 deaths between 2000 and 2012 due to gall bladder cancer and extrahepatic cholangiocarcinoma subtypes, 74% were women [4]. Interestingly, perihilar cholangiocarcinoma incidence and mortality in Thailand are generally higher for men than women [41]. In the USA (between 1999 and 2013) and South Korea (between 2006 and 2015), incidence rates for intrahepatic and extrahepatic cholangiocarcinoma were higher for men than women [40, 42]. In the current study, 78% of patients were women, which does not reflect the overall sex distribution and which may be due to the greater willingness of women to participate in such studies compared with men. Most patients were college-educated. The sample size of patients with early-stage BTC was small (n = 3). Most of the patients in this study had intrahepatic cholangiocarcinoma (n = 17), which is not representative of the natural distribution of BTC subtypes; gall bladder cancer is the most common BTC subtype worldwide [40]. Furthermore, no patients with extrahepatic distal BTC were recruited in this study, which may be because the prevalence of distal BTC is much lower than that of perihilar BTC in the USA [43]. Responses are likely to have been affected by treatments received around the time of the interview. Based on this study, recommendations for future research may include recruiting patients of different ethnicities and geographical locations and increasing the sample sizes of patients with different BTC subtypes to gain an even wider understanding of the patient experience of BTC.
Conclusions
In conclusion, patients with BTC reported a range of signs/symptoms and impacts of their disease that negatively affect their daily functioning and quality of life, including some that had not been previously identified. The all-stage conceptual model developed in this study provides insights into the experience of patients living with BTC, which can aid patient–clinician dialogue and act as a tool for informing patients of what to expect at different disease stages and possibly from their treatments. Clinical trials targeting BTC should assess patient perspectives on how their disease and treatment impacts their quality of life, to provide a complementary view to traditional efficacy and safety outcomes.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the study participant(s) for their involvement in the study.
Medical Writing/Editorial Assistance
Medical writing support was provided by Olivia McKenna, PhD, of Oxford PharmaGenesis, Oxford, UK, and was funded by AstraZeneca.
Funding
This project was funded by AstraZeneca, Gaithersburg, MD, USA. Research and publication fees are funded by the study sponsor.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Design and conception: Nikunj Patel, Nana Rokutanda, Christina Workman, Oren Meyers, Gordon Cohen, Xandra Lie, Chad Gwaltney; First draft: Nikunj Patel, Nana Rokutanda, Christina Workman, Oren Meyers, Gordon Cohen, Xandra Lie, Chad Gwaltney, Afsaneh Barzi, Davide Melisi, Teresa Macarulla, Makoto Ueno, Melinda Bachini. All authors revised critically and approved the final version for publication.
Disclosures
Nikunj Patel, Nana Rokutanda, Christina Workman and Gordon Cohen are employees of AstraZeneca and hold shares in AstraZeneca. Xandra Lie and Oren Myers are employees of IQVIA, which received funds from AstraZeneca to conduct the analysis of the study data. Chad Gwaltney received consulting fees from IQVIA to participate in the design, execution and analysis of this study. Melinda Bachini has received honorarium from Taiho, Quod Erat Demonstrandum (QED) clinical services Ltd, Incyte and EMD Serono (for participating in patient advisory boards, review of patient materials and speaking engagements). Afsaneh Barzi, Davide Melisi, Teresa Macarulla, Makoto Ueno and Seung Tae Kim have nothing to declare.
Ethics Approval
The qualitative interview, research protocol, interview guide, and all patient communication documents were reviewed and approved by the New England Institutional Review Board (NEIRB) in January 2019.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Consent to Participate
All patients provided consent to participate online.
Consent for Publication
All participating patients provided consent online.
References
- 1.Tariq NU, McNamara MG, Valle JW. Biliary tract cancers: current knowledge, clinical candidates and future challenges. Cancer Manag Res. 2019;11:2623–2642. doi: 10.2147/CMAR.S157092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taylor-Robinson SD, Toledano MB, Arora S, Keegan TJ, Hargreaves S, Beck A, et al. Increase in mortality rates from intrahepatic cholangiocarcinoma in England and Wales 1968–1998. Gut. 2001;48(6):816–820. doi: 10.1136/gut.48.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saha SK, Zhu AX, Fuchs CS, Brooks GA. Forty-year trends in cholangiocarcinoma incidence in the US: intrahepatic disease on the rise. Oncologist. 2016;21(5):594–599. doi: 10.1634/theoncologist.2015-0446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marcano-Bonilla L, Mohamed EA, Mounajjed T, Roberts LR. Biliary tract cancers: epidemiology, molecular pathogenesis and genetic risk associations. Chin Clin Oncol. 2016;5(5):61. doi: 10.21037/cco.2016.10.09. [DOI] [PubMed] [Google Scholar]
- 5.Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6(2):172–187. doi: 10.5009/gnl.2012.6.2.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60(6):1268–1289. doi: 10.1016/j.jhep.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 7.Bridgewater JA, Goodman KA, Kalyan A, Mulcahy MF. Biliary tract cancer: epidemiology, radiotherapy, and molecular profiling. Am Soc Clin Oncol Educ Book. 2016;35:e194–203. doi: 10.1200/EDBK_160831. [DOI] [PubMed] [Google Scholar]
- 8.Lamarca A, Edeline J, McNamara MG, Hubner RA, Nagino M, Bridgewater J, et al. Current standards and future perspectives in adjuvant treatment for biliary tract cancers. Cancer Treat Rev. 2020;84:101936. [DOI] [PubMed]
- 9.Anderson C, Kim R. Adjuvant therapy for resected extrahepatic cholangiocarcinoma: a review of the literature and future directions. Cancer Treat Rev. 2009;35(4):322–327. doi: 10.1016/j.ctrv.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 10.DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007;245(5):755–762. doi: 10.1097/01.sla.0000251366.62632.d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Endo I, Gonen M, Yopp AC, Dalal KM, Zhou Q, Klimstra D, et al. Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Ann Surg. 2008;248(1):84–96. doi: 10.1097/SLA.0b013e318176c4d3. [DOI] [PubMed] [Google Scholar]
- 12.Rizvi S, Khan SA, Hallemeier CL, Kelley RK, Gores GJ. Cholangiocarcinoma—evolving concepts and therapeutic strategies. Nat Rev Clin Oncol. 2018;15(2):95–111. doi: 10.1038/nrclinonc.2017.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Butt Z, Parikh ND, Beaumont JL, Rosenbloom SK, Syrjala KL, Abernethy AP, et al. Development and validation of a symptom index for advanced hepatobiliary and pancreatic cancers: the National Comprehensive Cancer Network Functional Assessment of Cancer Therapy (NCCN-FACT) Hepatobiliary-Pancreatic Symptom Index (NFHSI) Cancer. 2012;118(23):5997–6004. doi: 10.1002/cncr.27588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woradet S, Promthet S, Songserm N, Parkin DM. Factors affecting health-related quality of life in patients with cholangiocarcinoma in the northeastern region of Thailand. Cancer Nurs. 2015;38(6):E46–51. doi: 10.1097/NCC.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 15.Woradet S, Songserm N, Promthet S, Parkin DM. Health-related quality of life and survival of cholangiocarcinoma patients in northeastern region of Thailand. PLoS ONE. 2016;11(9):e0163448. doi: 10.1371/journal.pone.0163448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murad SD, Heimbach JK, Gores GJ, Rosen CB, Benson JT, Kim WR. Excellent quality of life after liver transplantation for patients with perihilar cholangiocarcinoma who have undergone neoadjuvant chemoradiation. Liver Transpl. 2013;19(5):521–528. doi: 10.1002/lt.23630. [DOI] [PubMed] [Google Scholar]
- 17.Kaupp-Roberts SD, Yadegarfar G, Friend E, O'Donnell CM, Valle JW, Byrne C, et al. Validation of the EORTC QLQ-BIL21 questionnaire for measuring quality of life in patients with cholangiocarcinoma and cancer of the gallbladder. Br J Cancer. 2016;115(9):1032–1038. doi: 10.1038/bjc.2016.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dengsø K, Bangsgaard L, Marcussen AM, Christensen BM, Hillingsø J, Thomsen T. Patients' descriptions of initial symptoms of cholangicarcinoma and the journey to diagnosis: a qualitative study. J Neoplasm. 2017;2(2):14. [Google Scholar]
- 19.Friend E, Yadegarfar G, Byrne C, Johnson CD, Sezer O, Pucciarelli S, et al. Development of a questionnaire (EORTC module) to measure quality of life in patients with cholangiocarcinoma and gallbladder cancer, the EORTC QLQ-BIL21. Br J Cancer. 2011;104(4):587–592. doi: 10.1038/sj.bjc.6606086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Somjaivong B, Thanasilp S, Preechawong S, Sloan R. The influence of symptoms, social support, uncertainty, and coping on health-related quality of life among cholangiocarcinoma patients in northeast Thailand. Cancer Nurs. 2011;34(6):434–442. doi: 10.1097/NCC.0b013e31820d0c3f. [DOI] [PubMed] [Google Scholar]
- 21.Brod M, Tesler LE, Christensen TL. Qualitative research and content validity: developing best practices based on science and experience. Qual Life Res. 2009;18(9):1263–1278. doi: 10.1007/s11136-009-9540-9. [DOI] [PubMed] [Google Scholar]
- 22.CHMP . Reflection paper on the regulatory guidance for the use of health-related quality of life (HRQL) measures in the evaluation of medicinal products. London: European Medicines Agency; 2005. [Google Scholar]
- 23.Food, Administration D Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims. Fed Regist. 2009;74(235):65132–65133. [Google Scholar]
- 24.Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, et al. Content validity—establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO good research practices task force report: part 1—eliciting concepts for a new PRO instrument. Value Health. 2011;14(8):967–977. doi: 10.1016/j.jval.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 25.Koeberle D, Saletti P, Borner M, Gerber D, Dietrich D, Caspar CB, et al. Patient-reported outcomes of patients with advanced biliary tract cancers receiving gemcitabine plus capecitabine: a multicenter, phase II trial of the Swiss Group for Clinical Cancer Research. J Clin Oncol. 2008;26(22):3702–3708. doi: 10.1200/JCO.2008.16.5704. [DOI] [PubMed] [Google Scholar]
- 26.Mikkelsen MK, Nielsen DL, Vinther A, Lund CM, Jarden M. Attitudes towards physical activity and exercise in older patients with advanced cancer during oncological treatment—a qualitative interview study. Eur J Oncol Nurs. 2019;41:16–23. doi: 10.1016/j.ejon.2019.04.005. [DOI] [PubMed] [Google Scholar]
- 27.Ibrahim F, Sandström P, Björnsson B, Larsson AL, Drott J. 'I want to know why and need to be involved in my own care…': a qualitative interview study with liver, bile duct or pancreatic cancer patients about their experiences with involvement in care. Support Care Cancer. 2019;27(7):2561–2567. doi: 10.1007/s00520-018-4548-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krippendorff K. Content analysis: an introduction to its methodology. Beverly Hills: Sage Publications; 1980. [Google Scholar]
- 29.Fusch P, Ness LR. Are we there yet? Data saturation in qualitative research. Qual Rep. 2015;20(9):1408–1416. [Google Scholar]
- 30.Guest G, Bunce A, Johnson L. How many interviews are enough?: An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82. [Google Scholar]
- 31.Turner-Bowker DM, Lamoureux RE, Stokes J, Litcher-Kelly L, Galipeau N, Yaworsky A, et al. Informing a priori sample size estimation in qualitative concept elicitation interview studies for clinical outcome assessment instrument development. Value Health. 2018;21(7):839–842. doi: 10.1016/j.jval.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 32.Elberg Dengso K, Hillingso J, Marcussen AM, Thomsen T. Health-related quality of life and anxiety and depression in patients diagnosed with cholangiocarcinoma: a prospective cohort study. Acta Oncol. 2017;56(2):198–204. doi: 10.1080/0284186X.2016.1266088. [DOI] [PubMed] [Google Scholar]
- 33.Shun SC, Chiou JF, Lai YH, Yu PJ, Wei LL, Tsai JT, et al. Changes in quality of life and its related factors in liver cancer patients receiving stereotactic radiation therapy. Support Care Cancer. 2008;16(9):1059–1065. doi: 10.1007/s00520-007-0384-y. [DOI] [PubMed] [Google Scholar]
- 34.Wu TT, Li WM, Li HC, Ao GK, Zheng F, Lin H. Percutaneous intraductal radiofrequency ablation for extrahepatic distal cholangiocarcinoma: a method for prolonging stent patency and achieving better functional status and quality of life. Cardiovasc Intervent Radiol. 2017;40(2):260–269. doi: 10.1007/s00270-016-1483-2. [DOI] [PubMed] [Google Scholar]
- 35.Koyama K, Fukunishi I, Kudo M, Sugawara Y, Makuuchi M. Psychiatric symptoms after hepatic resection. Psychosomatics. 2003;44(1):86–87. doi: 10.1176/appi.psy.44.1.86. [DOI] [PubMed] [Google Scholar]
- 36.Yang Z, Wan C, Li W, Cun Y, Meng Q, Ding Y, et al. Development and validation of the simplified Chinese version of EORTC QLQ-HCC18 for patients with hepatocellular carcinoma. Cancer Invest. 2015;33(8):340–346. doi: 10.3109/07357907.2015.1036280. [DOI] [PubMed] [Google Scholar]
- 37.Bridgewater J, Lopes A, Palmer D, Cunningham D, Anthoney A, Maraveyas A, et al. Quality of life, long-term survivors and long-term outcome from the ABC-02 study. Br J Cancer. 2016;114(9):965–971. doi: 10.1038/bjc.2016.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McGee EE, Jackson SS, Petrick JL, Van Dyke AL, Adami HO, Albanes D, et al. Smoking, alcohol, and biliary tract cancer risk: a pooling project of 26 prospective studies. J Natl Cancer Inst. 2019;111(12):1263–1278. doi: 10.1093/jnci/djz103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Castro FA, Koshiol J, Hsing AW, Devesa SS. Biliary tract cancer incidence in the United States—demographic and temporal variations by anatomic site. Int J Cancer. 2013;133(7):1664–1671. doi: 10.1002/ijc.28161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van Dyke AL, Shiels MS, Jones GS, Pfeiffer RM, Petrick JL, Beebe-Dimmer JL, et al. Biliary tract cancer incidence and trends in the United States by demographic group, 1999–2013. Cancer. 2019;125(9):1489–1498. doi: 10.1002/cncr.31942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sripa B, Pairojkul C. Cholangiocarcinoma: lessons from Thailand. Curr Opin Gastroenterol. 2008;24(3):349–356. doi: 10.1097/MOG.0b013e3282fbf9b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim BW, Oh CM, Choi HY, Park JW, Cho H, Ki M. Incidence and overall survival of biliary tract cancers in South Korea from 2006 to 2015: using the National Health Information Database. Gut and liver. 2019;13(1):104–113. doi: 10.5009/gnl18105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Banales JM, Marin JJG, Lamarca A, Rodrigues PM, Khan SA, Roberts LR, et al. Cholangiocarcinoma 2020: the next horizon in mechanisms and management. Nat Rev Gastroenterol Hepatol. 2020;17(9):557–588. doi: 10.1038/s41575-020-0310-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.