Supplemental digital content is available in the text.
Key Words: SARS-CoV-2, Physiatry, Internal Medicine, Physiotherapy, Activities of Daily Living
Abstract
Objectives
The aims of the study were to describe an interdisciplinary inpatient rehabilitation program for patients recovering from COVID-19 and to evaluate functional outcomes.
Design
This is an analysis of retrospective data captured from the electronic health record of COVID-19 patients admitted to the rehabilitation unit (N = 106). Rehabilitation approaches are described narratively. Functional gain was evaluated using the Activity Measure for Postacute Care 6 Clicks, basic mobility and daily activities.
Results
Interdisciplinary approaches were implemented to address the medical, physical, communication, cognitive, and psychosocial needs of COVID-19 patients. COVID-19 patients exhibited significant improvements in basic mobility (Activity Measure for Postacute Care for basic mobility, P < 0.001, Cohen d = 1.35) and daily activities (Activity Measure for Postacute Care for daily activities, P < 0.001, Cohen d = 1.06) from admission to discharge. There was an increase in ambulatory distance as well as the percentage of the patients who were able to breathe on room air. At discharge, fewer patients required supplemental oxygen on exertion. Eighty percent of the patients were discharged home after an average length of stay of 17 days. Greater functional improvement was associated with younger age, longer intubation duration, and participation in psychotherapy, but not a history of delirium during hospitalization.
Conclusions
Early rehabilitation is associated with improved mobility and independence in activities of daily living after COVID-19.
What Is Known
Hospitalized survivors of COVID-19 experience multiorgan dysfunction, limited mobility, and limitations in activities of daily living necessitating inpatient rehabilitation.
What Is New
We demonstrate that early interdisciplinary rehabilitation promotes functional gain after COVID-19 and describe correlates of functional improvement.
COVID-19 is associated with complex multisystem impairments1–3 that result in physical, cognitive, and psychiatric symptoms4–8 that impact function, necessitating inpatient rehabilitation. Several barriers and challenges to rehabilitation exist, particularly for individuals who remain COVID-19–positive during hospitalization. These may include ongoing infectiousness, high medical acuity and complexity, limited opportunities for social interaction, and inability to tolerate the minimum of 3 hrs daily of rehabilitation therapy required by traditional inpatient rehabilitation facilities. Additional options for rehabilitation—such as subacute rehabilitation and skilled nursing facilities—may not provide patients with the interdisciplinary medical care and intensive rehabilitation necessary to improve functional outcomes.
In addition to these challenges, the therapeutic modifications required and functional outcomes associated with inpatient rehabilitation for COVID-19 are not yet well described. Guidelines for COVID-19 rehabilitation have commented on early admission to inpatient rehabilitation, delayed admission to skilled nursing facilities, and a push for discharge home if appropriate family assistance is available.9–11 Existing studies suggest beneficial effects on respiratory function12 and endurance.13 However, there is little empirical data investigating whether inpatient rehabilitation for COVID-19 is associated with improved physical functioning and independence in activities of daily living.
During the first wave of COVID-19, our medical center created a hybrid medical/rehabilitation unit, the COVID-19 recovery unit (CRU).14 The unit was led by an internist and a physiatrist with a heavy emphasis on interdisciplinary approaches to early COVID-19 rehabilitation. The objectives of this study were to (1) describe the unit setting and rehabilitation interventions administered, (2) evaluate functional gains in mobility and activities of daily living, and (3) explore correlates of functional gain.
METHODS
Sample
This was an observational study via retrospective electronic health record extraction of 106 patients admitted to the CRU between April 24, 2020, and July 17, 2020, at which time the unit closed. Criteria for admission were ongoing medical and rehabilitation needs, less than 6 liters of oxygen requirements at rest, and anticipation of at least one additional week of inpatient-level care.14 Most patients were treated in intensive care before transfer to the CRU, although this was not a strict criterion for admission. Patients were weaned off sedation and ventilation within the acute/intensive care unit setting rather than on traditional step-down units because of limited availability to transfer patients during the surge of cases. Our hospital continued to maintain a traditional general inpatient rehabilitation unit. COVID-19 patients who went to this traditional inpatient rehabilitation unit were deemed able to tolerate the standard 3 hrs/d of therapy, whereas those were suspected of being unable to initially tolerate this intensity of rehabilitation flowed to the CRU. Exclusion criteria to the CRU included ongoing mechanical ventilation or a need for 24-hr 1:1 observation (e.g., for agitation or risk of self-harm). The previously mentioned admission and exclusion criteria were determined by acute care physical and occupational therapists and a consult physiatrist. The Weill Cornell Medicine Institutional Review Board approved the retrospective data extraction from the electronic health record; the requirement for informed consent was waived. This study conforms to all Strengthening the Reporting of Observational Studies in Epidemiology guidelines and reports the required information accordingly (see Supplementary Checklist, Supplemental Digital Content 1, http://links.lww.com/PHM/B412). Patient demographic and clinical data are provided in Table 1.
TABLE 1.
Demographic and clinical characteristics of 106 patients admitted to the CRU
| N = 106 | |
|---|---|
| n (%) or Mean (SD) | |
| Demographic characteristics | |
| Age, yr | 64 (14) |
| Sex | |
| Male | 79 (74.5%) |
| Female | 27 (25.5%) |
| Race/ethnicity | |
| White | 30 (28.3%) |
| Latino | 19 (17.9%) |
| Black | 14 (13.2%) |
| Asian | 22 (20.8%) |
| Other | 13 (12.3%) |
| Unknown/not documented in chart | 8 (7.5%) |
| Pre-COVID status | |
| Functional level | |
| Home independent | 69 (65.1%) |
| Home with assistance | 8 (7.5%) |
| Facility | 4 (3.8%) |
| Unknown/not documented in chart | 25 (23.6%) |
| Employment status | |
| Working | 36 (34%) |
| Retired | 18 (17%) |
| Unemployed | 9 (8.5%) |
| Disabled | 8 (7.5%) |
| Unknown/not documented in chart | 35 (33%) |
| History of cognitive disorder | 6 (5.7%) |
| Preexisting vascular or metabolic disease (e.g., hypertension, hyperlipidemia, diabetes mellitus, obstructive sleep apnea) | 43 (40.6%) |
| Acute hospitalization | |
| Documented delirium | 56 (52.8%) |
| Length of intubation, median (interquartile range), d | 13 (0–20.5) |
| Documented hypoxia or hypoxemic respiratory failure | 81 (76.4%) |
| Tracheostomy | 33 (31.1%) |
| Length of stay on acute floor, d | 35 (23.78) |
| CRU course | |
| Received psychotherapy | 43 (40.6%) |
| AMPAC: DA scores | |
| Admission T score | 34.6 (7.8) |
| Discharge T score | 43.5 (9.4) |
| AMPAC: BM scores | |
| Admission T score | 34.5 (8.2) |
| Discharge T score | 45.3 (9.0) |
| CRU length of stay, d | 17.3 (8.9) |
| Total hospital length of stay, d | 53 (28.3) |
| Discharge disposition | |
| Home (with or without services) | 85 (80%) |
| Subacute rehabilitation or skilled nursing facility | 10 (9%) |
| Transferred back to acute medical floor | 6 (6%) |
| Transferred to another unit or hospital after CRU closed | 5 (5%) |
Setting and Interdisciplinary Interventions
The CRU was a 30-bed, converted inpatient psychiatric unit that included large spaces previously used for milieu groups and meetings as well as individual therapy rooms, which were transformed into rehabilitation gyms and space for group activities on the CRU. In all other aspects, the unit had the layout of a traditional medical ward with a centralized nursing station. The available space allowed for COVID-19–positive and COVID-19–negative patients to separately engage in therapy sessions out of their rooms. In adherence to the medical center’s infection prevention guidelines, the CRU housed two separate therapy gyms for positive/negative patients. Each gym had air filtration, cleaning protocols, signage, and verbal communication between treating team members. Social distancing between patients was observed in all spaces. Rehabilitation equipment was chosen based on the ability to be cleaned. Outside the gyms was a makeshift staircase with four 6-inch steps and bilateral handrails used for physical therapy (PT). The hallways measured 200 and 150 feet in length with markers every 50 and 20 feet, respectively.
Patients on the CRU received daily PT and occupational therapy (OT), as well as speech-language pathology (SLP), neuropsychology, psychiatry, neurology, and pulmonology consultation as needed. The OT/PT staff were reassigned from other units, and nursing staff consisted of float nurses from other services and travel nurses. While the unit physiatrist was able to manage much of patients’ ongoing medical needs, the presence of embedded internal medicine (hospitalist) physicians enabled real-time collaboration on a wide variety of cardiac, pulmonary, and renal sequelae of COVID-19, including recommendations for oxygen delivery. Internists provided care analogous to a step-down medical setting for patients who decompensated. Physiatry was thus able to focus on managing bracing/splinting, musculoskeletal, and neurologic issues that arose in patients, as well as evaluated and managed symptoms that limited function or therapy participation (e.g., tone/spasticity management). Registered nurses from a separate preexisting inpatient rehabilitation unit floated to the CRU to assist the CRU nurses with training and adjusting to a rehabilitation setting. Nurse-to-patient ratios were 4:1 or 5:1 based on staffing.
On average, patients received PT and OT sessions 5–6 d/wk, for approximately 60–90 mins per day each. Speech-language pathology sessions varied between 30 and 60 mins, 3–5 d/wk. The flexible dosing of rehabilitation enabled personalized care, which was greater in frequency and intensity than patients would typically receive at bedside on acute medical floors in our hospital (i.e., typically 30-min PT or OT sessions, 2–3 times each week), although less intense than in a traditional inpatient rehabilitation facility (90-min PT and OT sessions, 6 times each week).
Vital signs were continually monitored. Each rehabilitation therapist was given a portable pulse oximeter. Dinamap devices were in both therapy gyms. Vital sign monitoring was implemented because of the nature of the disease and concern for the negative impact of overexertion. Vital sign monitoring enabled rehabilitation therapists to pace activities by conservatively pushing patients while implementing rest breaks based on heart rate and oxygen saturation levels.
A clinical neuropsychologist and neuropsychology fellow were embedded on the unit and implemented cognitive and psychological screening evaluations as well as individual and group-based cognitive-behavioral interventions.7,15 Consultation/liaison psychiatry was consulted for patients with more severe psychiatric symptoms, sleep difficulty, and/or residual delirium.
Interdisciplinary communication was essential to the CRU. Morning huddles occurred daily and consisted of charge nurse reports on patient clinical status and updates on implementation of team-based goals. Unlike the acute care discharge planning process where the discharge date was typically determined by the medical team, estimated discharge date on the CRU was determined by the primary PT/OT team based on patient functional status. Patient beds on the CRU were billed acute hospital beds. Financial support for rehabilitation was provided by our hospital and medical college as well as part-time staff redeployment.
Therapeutic Interventions
Table 2 outlines specific impairments and interventions implemented in response to the complex clinical presentations of this patient population. At times, standard of care was sufficient to target sequelae of COVID-19, whereas on other occasions, modifications were necessary. Techniques such as conservative activity pacing, frequent monitoring of oxygen saturation, and change in oxygen delivery methods were especially crucial for progress with functional mobility, activity tolerance, and outcomes. Flexible durations of PT/OT sessions and integration of cognitive-behavioral strategies to manage anxiety and isolation were also among the most important and unique modifications required for the COVID-19 population.
TABLE 2.
Impairment-specific assessment and interventions used on the CRU
| Impairment | Discipline(s) | Example Assessment Methods | Standard of Care Approaches to Rehabilitation After Critical Illness | Unique Modifications for COVID-19 |
|---|---|---|---|---|
| Upper extremity range of motion | OT | Generalized observations and goniometry | Range-of-motion exercises, both against gravity and gravity eliminated | Custom static splints: hand splints, wrist cock up splints, pan splints, anterior elbow shells, radial nerve palsy splints, and claw hand splints |
| Upper extremity strength | OT | Manual muscle testing; dynamometer testing; pinchometer testing | TherEx with TheraBands, theraputty; free weights; weight bearing; neuromuscular electrical stimulation | - Pacing upper body strengthening and weight bearing to accommodate for endurance and change in oxygen saturations - Minimizing isometrics and concentrics and starting with eccentric exercises to reduce Valsalva and desaturation risk - Splinting for functional use of limbs |
| Upper extremity motor control and coordination | OT | 9-Hole Peg Test and gross motor control assessment (finger to nose, diadochokinetics, digital opposition) | Reaching with targets, coin manipulation, neuromuscular electrical stimulation | - Using electromyography results to tailor treatment based on nerve injury and presentation - Using low-profile dynamic splints for wrist drop and digital extension when performing dexterous tasks and ADL |
| Seated and standing tolerance | OT, PT, neuropsychology | 6-MIN WALK TEST and 2-Min Step Test | Seated and standing ADL tasks, ambulation | - Change oxygen delivery method - Conservative pacing and increased recovery times due to shortness of breath and tachycardia - Use of upper limb support to decrease rate of perceived exertion despite good balance - Use of mindfulness, cognitive-behavioral therapy techniques, and cotreatment with neuropsychology |
| Dynamic balance | OT, PT | Timed Up and Go | Standing reaching tasks, dribble soccer ball, shoot basketball | No modifications needed |
| Lower extremity strength | PT | Manual Muscle Testing and 5 Times Sit to Stand Test | TherEx without resistance; TheraBands; NuStep with resistance; use of ankle-foot orthosis or ace wrap | - Limited isometric exercises, increased focus on TherEx closely related to functional activities |
| Ambulation | PT, neuropsychology | Gait speed, 6-Min Walk Test, and 2-Min Step Test | Ambulation, with assistive devices as needed | - Conservatively paced activities in sitting despite lower limb manual muscle testing >3/5 (seated recumbent bicycle) - Conservative pacing (i.e., 10 steps at a time) and increased recovery time when initiating ambulation due to shortness of breath and tachycardia - Change oxygen delivery method, occasional use of a nonrebreather - Use assistive device to decrease rate of perceived exertion despite good balance - Cotreatment with neuropsychology for patients with anxiety toward walking due to shortness of breath |
| Swallow | SLP | Bedside swallowing examination; Modified Barium Swallow | Dysphagia exercise program, oral muscle exercises, improving timing of swallow trigger, management of secretions, increasing cough strength | - Elicit consistent swallow trigger using ice chips - Management of excessive pharyngeal secretions - Practice of increasing cough strength was contraindicated because of aerosolization of respiratory particles and rapid fatigue because of compromised respiratory function |
| Communication/speech | SLP | Informal assessments targeting functional language, cognition, and speech production | Oral muscle exercises; strategies to increase speech intelligibility; word retrieval tasks | - Focus on dysarthria, via improving breath support, oral muscle exercises, speech production, and clarity rather than language remediation - For trached patients, tolerance of the Passy-Muir Speaking Valve was implemented |
| Cognition—orientation | OT, PT, SLP, neuropsychology | Montreal Cognitive Assessment; Orientation-Log; Brief Memory and Executive Test | Orientation questioning/use of whiteboard, in room stimulation | - Collaboration with doctors, nursing and all therapy disciplines to reinforce use of white board and to consistently reorient and engage patients when in or out of room - Out of room treatment to orient to unit and place - Toileting programs to encourage bowel/bladder awareness and control, when relevant - Personal journals and calendars - iPads for family communication |
| Cognition—executive functioning and memory | OT, neuropsychology | Montreal Cognitive Assessment; Symbol-Digit Modalities Test; Trail Making Test; Weekly Calendar Planning Activity; Brief Memory and Executive Test | Cognitive exercises for skill acquisition and remediation, cognitive strategy instruction | - Collaboration with neuropsychology (when appropriate) to coordinate similarly structured cognitive tasks for generalization - Maximizing out of room engagement in cognitively based activities and incorporation of families into treatment planning in preparation for discharge home (medication management, bill paying, folding laundry) |
ADL, activity of daily living.
Musculoskeletal
Patients presented with varying levels of unilateral and bilateral weakness. The causes of these deficits were thought to commonly reflect critical illness polyneuropathy and on occasion were thought to be related to previous prone positioning while intubated. During ambulation, ace wrapping and off-the-shelf ankle-foot orthoses were used, as well as supportive bracing and customized splinting.
Cardiopulmonary
Patients required varying titrations and forms of supplemental oxygen as well as increased recovery times relative to usual care, often with a resting/recovery duration greater than or equal to that of the activity. Patients were eventually trained and educated on using portable pulse oximeters to monitor heart rate and oxygen saturations at rest and with activity. Tachycardia with low level exercise was prominent in this patient population further adding to the importance of pacing all activities.
Neurologic
Neurologic sequelae observed included sensory loss, impaired nerve conduction, myopathies, brachial plexopathies, and weakness. Commonly used were neuromuscular re-education techniques, neuromuscular electrical stimulation, and adaptation exercises for vestibular hypofunction.
Dysphagia
Bedside clinical evaluations and modified barium swallow evaluations were conducted with safety measures in place including enhanced sterilization procedures and having patients avoid opening their mouth to assess vocal quality. Although these techniques as well as fiberoptic endoscopic evaluations are considered aerosol generating, the latter was deemed to carry increased exposure risk based on published guidelines16 and discussion with our institution’s ENT physicians. Thus, fiberoptic endoscopic evaluations were not used during the pandemic for COVID-19–positive or COVID-19–negative patients at our institution. Patients commonly presented with fatigue and compromised stamina resulted in poor ability to masticate harder solids effectively, despite having full dentition. Initiation was an important factor as well, given that some patients had not swallowed for quite a while and had a delay in the timing of the swallow trigger. Ice chips were always encouraged to practice swallow integrity, after oral care.
Communication
Speech-language pathology assisted in managing tracheostomies. During these sessions, oxygen saturation, heart rate, and respiratory rate were monitored throughout. Speaking valve trials were conducted with full SLP supervision, for monitoring tolerance, quality, volume, and pitch of speech.
Cognition
Many patients required cognitive remediation, which often targeted orientation, memory, attention, executive functioning, and awareness.7 Given visitation restrictions, the use of iPads and room whiteboards were used for orientation. Neuropsychology also provided individual/group cognitive remediation by using compensatory strategies (e.g., memory books) and providing strategies and education on factors that could impact cognitive functioning, such as sleep and anxiety.
Psychological Interventions and Procedures to Mitigate Social Isolation
Neuropsychology evaluated and treated patients who exhibited cognitive difficulties, anxiety, or amotivation or those who express feelings of isolation or low mood. Treatment included individual cognitive-behavioral therapy (1–2 times per week) and/or group psychotherapy (twice weekly). Groups focused on building resilience and skill building to mitigate isolation, anxiety, low mood, sleep disturbance, and cognitive difficulties.15 Because of the diversity of symptom presentations and patient racial, ethnic, and cultural backgrounds, social groups were created specifically to cohort patients facing similar challenges and those who spoke the same native languages.
Assessment of Functional Outcomes
The primary assessment of functional outcome was the Activity Measure for Postacute Care 6 Clicks for basic mobility (AMPAC-BM) and daily activities (AMPAC-DA), completed on admission to the CRU and just before discharge. The AMPAC-BM and AMPAC-DA assess functional/activity limitations using six items each, with each item being scored from 1 to 4 based on the difficulty a patient has or how much help is needed from another person. The AMPAC-BM items include items assessing transfers, ambulation, and stair climbing, and AMPAC-DA items include items assessing upper and lower body dressing, grooming, and feeding. Scores are standardized to T scores (mean of 50 and SD of 10); lower scores represent greater need for assistance and reduced functional independence. The AMPAC-BM and AMPAC-DA demonstrate strong convergent validity (correlation with the Functional Independence Measure), internal consistency, interrater reliability, responsiveness to change, and correlation with discharge destination.17–19
Also extracted from the electronic health record were discharge disposition, categorized as home, transfer to another rehabilitation facility, nursing facility, or an acute medical floor. We also extracted—at admission and discharge—ambulatory status (yes/no), distance ambulated in feet, ability to breathe on room air at rest (yes/no), and requirement of supplemental oxygen on exertion (yes/no). We chose to investigate the association between age, delirium, and participation in psychotherapy as correlates of functional gain because of previous research indicating that these factors predict rehabilitation outcome in other populations.20–22 We were particularly interested in evaluating relationships between functional gain and delirium and psychotherapy, because of the high rates of previous delirium in our cohort and because of patients’ significant psychosocial needs. We also investigated the association between intubation (as a marker of illness severity) and functional gain.
Statistical Analysis
Paired samples t tests were used to evaluate admission to discharge change in AMPAC-BM, AMPAC-DA, and ambulatory distance (feet). Effect sizes are reported as Cohen d. We calculated the number (percent) of patients who met the established 90% confidence interval minimal detectable change on the AMPAC 6 Clicks, the mean rate of AMPAC change (total admission to discharge change in AMPAC-BM and AMPAC-DA divided by length of stay), and the number (percent) who were discharged home. We calculated the percentage of patients—at admission and discharge—who were ambulatory, who could breathe on room air at rest, and who required supplemental oxygen on exertion during physical therapy. We calculated change scores for the AMPAC-BM and AMPAC-DA from admission to discharge and used nonparametric statistical tests (Mann-Whitney U and Spearman rank-order correlation) to evaluate the relationship between change in AMPAC-BM and AMPAC-DA T scores and age, whether patients were intubated (yes/no), intubation length, documented delirium in the intensive care unit (yes/no), and whether patients participated in at least one individual and/or group psychotherapy session led by neuropsychology (yes/no). We used nonparametric tests for this latter analysis because AMPAC-BM and AMPAC-DA change scores deviated significantly from normality.
RESULTS
Table 1 provides information on COVID-19 patient demographic, medical, and clinical characteristics.
Functional Outcomes
COVID-19 patients exhibited a significant improvement in AMPAC-DA T score from admission to discharge (Fig. 1) with a large effect size: t(105) = 10.97, P < 0.001, mean T score change = 8.96 (95% confidence interval [CI] = 7.34–10.58), Cohen d = 1.06. Similarly, patients exhibited a significant improvement in AMPAC-BM T score from admission to discharge with a large effect size: t(104) = 13.85, P < 0.001, mean T score change = 10.63 (95% CI = 9.10 to 12.15), Cohen d = 1.35. Eighty of the patients (76%) met the minimum detectable change cutoff for the AMPAC-BM and 66 (62%) met the minimum detectable change cutoff for the AMPAC-DA.17 Patients made an average daily gain on the AMPAC-DA of 0.65 (SD = 0.73) T score points and an average daily gain of 0.74 T score points (SD = 0.58) on the AMPAC-BM. Sixty-six percent of the patients were ambulatory at admission. At discharge, 92% were ambulatory. There was a significant improvement in distance ambulated in feet from admission to discharge with a large effect size: t(102) = 8.57, P < 0.001, mean change = 224.1 (95% CI = 172.2 to 275.93), Cohen d = 0.85. At admission, 68% of the patients could breathe on room air and 23% required increased oxygen on exertion. At discharge, 81% could breathe on room air and 14% required increased oxygen on exertion.
FIGURE 1.
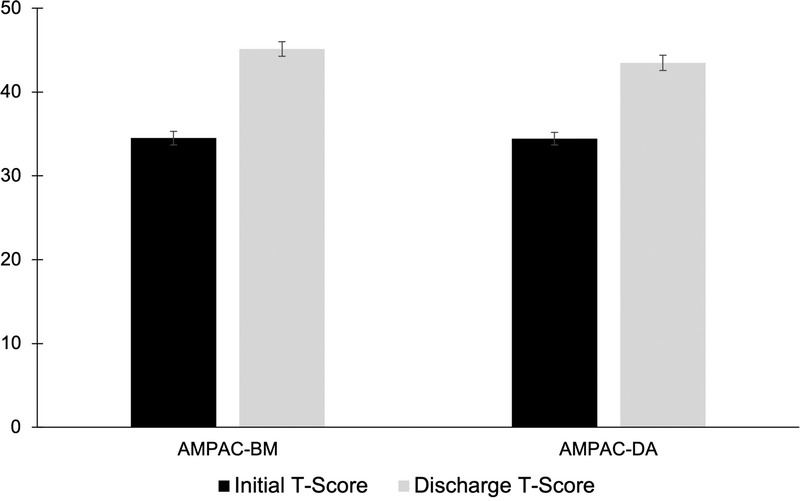
Mean change in T score on the AMPAC 6-Clicks Scales assessing DA and BM from admission to discharge. Error bars represent standard error of the mean.
Eighty-five patients (80%) were discharged home, whereas 10 (9%) were discharged to a skilled nursing facility or subacute rehabilitation facility, six (6%) required medical transfer off the unit to an acute medical floor, and five (5%) were transferred to another unit/hospital for further rehabilitation after the unit closed in July 2020.
There were no medical emergencies, unplanned decannulations, codes, rapid responses, or deaths on the CRU. Twelve falls occurred on the unit. Line dislodgements were minimal as lines were typically only used to attach to supplemental oxygen and Foley catheters.
Correlates of Functional Gain
Age correlated negatively but modestly with improvement in AMPAC-BM (rs = −0.27, P = 0.005) but not AMPAC-DA (rs = −0.11, P = 0.26). Length of intubation was positively correlated with gain in AMPAC-BM (rs = 0.33, P = 0.001) and with AMPAC-DA (rs = 0.25, P = 0.012). On the AMPAC-DA, the patients who had been intubated had greater functional gain than those who were not intubated (mean difference = 5.2, 95% CI = 2.26 to 8.14, Mann-Whitney U = 855, P = 0.004, Cohen d = 0.65). Similarly, on the AMPAC-BM, the patients who had been intubated had greater functional gain than those who were not intubated (mean difference = 5.91, 95% CI = 3.25 to 8.57, Mann-Whitney U = 683.5, P < 0.001, Cohen d = 0.82). Patients who had documented delirium did not differ in their change in function compared with patients who did not have delirium (AMPAC-DA: mean difference = 2.7, 95% CI = −0.47 to 5.89, Mann-Whitney U = 1159, P = 0.127, Cohen d = 0.33; AMPAC-BM: mean difference = 2.4, 95% CI = −0.56 to 5.42, Mann-Whitney U = 1184, P = 0.227, Cohen d = 0.38). Compared with patients who did not engage in individual/group psychotherapy, patients who received individual/group psychotherapy had greater functional gains in basic mobility (AMPAC-BM: mean difference = 3.97, 95% CI = 0.96 to 6.98, Mann-Whitney U = 997, P = 0.029, Cohen d = 0.52), and a gain in daily activities at a trend level (AMPAC-DA: mean difference = 2.25, 95% CI = −1.03 to 5.54, Mann-Whitney U = 1071.5, P = 0.068, Cohen d = 0.27; Fig. 2).
FIGURE 2.
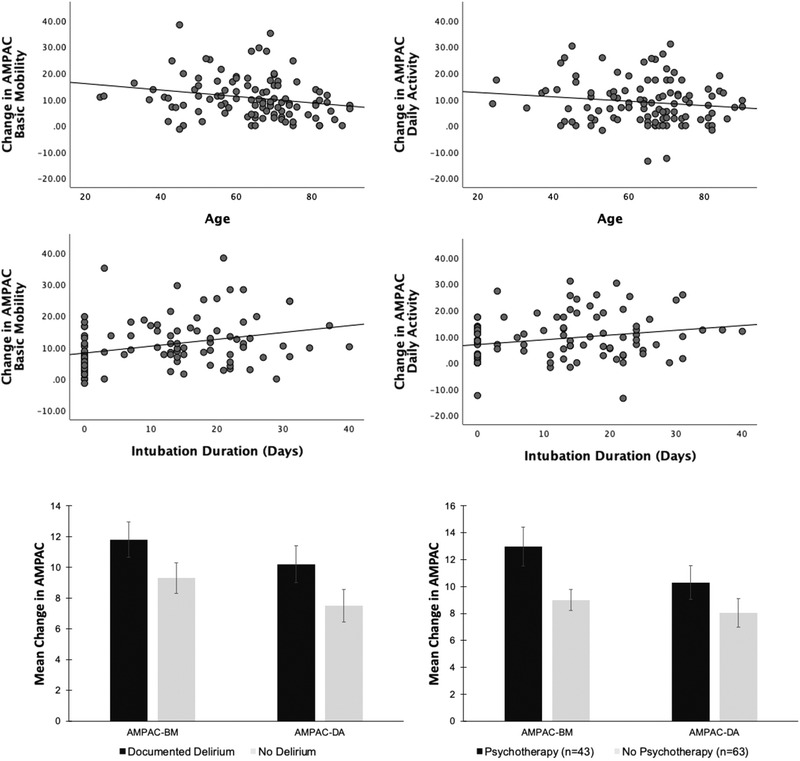
Change in T score from admission to discharge on the AMPAC subscales by age, intubation duration, delirium documented during intensive care, and engagement in individual and/or group psychotherapy while on the CRU. Error bars represent standard error of the mean.
DISCUSSION
We developed an inpatient, intensive interdisciplinary rehabilitation program co-led by physiatry and internal medicine to address the functional limitations of hospitalized COVID-19 patients. Patients made significant gains in basic mobility and activities of daily living, as well as distance ambulated, with large effect sizes for all measures. There was an increase in the percentage of patients who were able to breathe on room air. At discharge, fewer patients required supplemental oxygen on exertion. Eighty percent of patients were discharged home. Greater functional gain was associated with having been intubated and the length of intubation, younger age, and participation in individual/group psychotherapy but was not associated with a history of delirium.
Many have argued in the literature for the need for early inpatient rehabilitation for COVID-19 survivors.23–25 Here, we demonstrate that such a program can improve mobility and limitations in activities of daily living, as well as increase walking capacity and pulmonary function. Our results are consistent with, and expand upon, initial work with relatively small samples that has demonstrated that inpatient rehabilitation can enhance respiratory function, endurance, and activity tolerance after COVID-19.12,13,26 Our findings are also consistent with research that has shown outpatient rehabilitation programs to be efficacious for COVID-19 patients after hospitalization.27
Although our unit had many similarities to traditional inpatient rehabilitation, other aspects were unique. First, integrating internal medicine (hospitalist) physicians as part of the core team allowed us to admit patients who were more medically complex and less stable than traditional rehabilitation. It also enabled us to start rehabilitation earlier than traditional inpatient rehabilitation (e.g., as soon as patients were on nasal cannula) and to incorporate more intensive and integrated medical management of the patients. We note that only 6 of 106 patients had to be transferred off the unit to an acute medical unit. Integration of internal medicine facilitated management of cardiac, pulmonary, and renal complications, including for patients who decompensated, and also enabled flexible oxygen delivery, which may have increased tolerance and participation in rehabilitation. Second, dosing of rehabilitation was flexible (between 60 and 90 mins daily) and could be titrated on an individual basis. Third, therapy-specific modifications described in Table 2 were implemented, most impactfully conservative activity pacing, frequent monitoring of vitals and oxygen saturation, and a heightened focus on dysphagia treatment for trached patients. Furthermore, our setting enabled participation in rehabilitation therapies outside of the room, which was important for socialization and increasing the breadth of interventions available, in contrast with other programs in which rehabilitation was conducted entirely within patient rooms.28 Overall, our unit blended features of traditional inpatient rehabilitation, long-term acute care hospitals, and early mobilization programs.
Participation in individual and group psychotherapy led by neuropsychology was associated with improved functional gain in mobility. Although a causal link cannot be established, it is possible that addressing anxiety, isolation, and stress led to greater participation and engagement in rehabilitation and less disability.29 Our finding is consistent with research demonstrating that psychological interventions embedded in inpatient spinal cord injury rehabilitation are associated with improved functional outcomes at discharge,30 and that inpatient psychotherapy for critical illness survivors can improve postdischarge psychiatric outcomes.31 However, it is also possible that patients experiencing greater functional gains were more willing and able to participate in psychotherapy. Nonetheless, this finding highlights the value of an interdisciplinary approach in which interventions targeting cognitive and emotional function are integrated within acute medicine/rehabilitation services. We also speculate that a disease-specific unit in which all patients were recovering from COVID-19 may have contributed to positive outcomes by streamlining care and enabling patients to discuss their unique experience with, and support, one another in psychotherapy and social groups.
Interestingly, patients who were intubated and were intubated for longer durations had greater functional recovery than those patients who were not intubated. Although this may reflect a regression to the mean or a “lower baseline” from which to demonstrate recovery, it does indicate that our interdisciplinary rehabilitation program had benefits for those patients who underwent prolonged and invasive medical procedures. We also demonstrate that functional gain was not associated with the previous presence of delirium, suggesting that our approach was equally effective for patients who had and had not experienced delirium in the intensive care unit. Qualitatively, we note that those patients who benefited from services on the unit tended to initially present as highly medically complex and deconditioned, requiring an initial lower “dose” of rehabilitation (i.e., less than 3 hrs/d). Staff also observed qualitatively that patients who seemed to not benefit as much had a high burden of preexisting, chronic illnesses.
Additional unique modifications on the CRU may have enabled successful functional outcomes. While interdisciplinary rounds are common in traditional inpatient rehabilitation settings, daily rounds and PT/OT driven estimated discharge dates were unique to this program delivered in acute care. This facilitated a rehabilitation-centric approach from the entire medical team as well as rehabilitation sessions with minimal interruptions to allow patients to complete their daily treatments. This approach also streamlined complex medical care by allowing for frequent bedside assessments performed by consulting services outside therapy times. Extensive in-services provided by nurses, respiratory therapists, and SLP helped educate both the core rehabilitation team and the hospital medicine team.
Limitations
This COVID-19 rehabilitation program was feasible because of the financial commitment and institutional capabilities of this large, urban, academic institution, which may not be possible in smaller hospital systems. However, we were able to admit patients who were highly racially, ethnically, and demographically diverse and thus captured a patient population that is largely underrepresented in rehabilitation literature. Additional staffing and equipment were also essential and may not be feasible elsewhere. The patients on the CRU were from the first wave of the COVID-19 pandemic in spring 2020, which may not be representative of the rehabilitation needs of subsequent waves of COVID-19 survivors. Our study was not a randomized trial in which we can definitely attribute functional gains to rehabilitation interventions.
CONCLUSIONS
Inpatient rehabilitation for COVID-19, in a hybrid medicine/rehabilitation unit coled by physiatry and internal medicine, is associated with significant functional gains. Our approach may inform interdisciplinary rehabilitation approaches in other medical centers, both for COVID-19 and for other patient populations with critical illness and multisystem/multiorgan dysfunction.
Footnotes
Presented at the 2020 Annual Meeting of the American Congress of Rehabilitation Medicine, Virtual Conference, October 23, 2020.
All authors contributed substantively to the manuscript.
AJ receives salary support through a K12 Career Development Award from the National Center of Medical Rehabilitation Research/National Institute of Child Health and Human Development (1K12HD093427-04), via a subaward from Georgetown University.
Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.ajpmr.com).
Contributor Information
Nija Patel, Email: nip9059@nyp.org.
Chelsea Steinberg, Email: chs9162@nyp.org.
Ruchi Patel, Email: rup9005@nyp.org.
Cheryl Chomali, Email: chc9111@nyp.org.
Gargi Doulatani, Email: gad4001@med.cornell.edu.
Leroy Lindsay, Email: lel9053@med.cornell.edu.
Abhishek Jaywant, Email: abj2006@med.cornell.edu.
REFERENCES
- 1.Wade DT: Rehabilitation after COVID-19: an evidence-based approach. Clin Med (Lond) 2020;20:359–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iaccarino MA Tenforde AS Zafonte RD, et al. : Neurological manifestation of COVID-19 and the enhanced role of physiatrists. Am J Phys Med Rehabil 2020;99:858–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrenelli E Negrini F De Sire A, et al. : Systematic rapid living review on rehabilitation needs due to Covid-19: update to May 31st, 2020. Eur J Phys Rehabil Med 2020;56:508–14 [DOI] [PubMed] [Google Scholar]
- 4.Chen X Laurent S Onur OA, et al. : A systematic review of neurological symptoms and complications of COVID-19. J Neurol 2021;268:392–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lopez M Bell K Annaswamy T, et al. : COVID-19 guide for the rehabilitation clinician: a review of nonpulmonary manifestations and complications. Am J Phys Med Rehabil 2020;99:669–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mai F, Del Pinto R, Ferri C: COVID-19 and cardiovascular diseases. J Cardiol 2020;76:453–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jaywant A Vanderlind WM Alexopoulos GS, et al. : Frequency and profile of objective cognitive deficits in hospitalized patients recovering from COVID-19. Neuropsychopharmacology 2021:1–6. doi: 10.1038/s41386-021-00978-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taquet M Luciano S Geddes JR, et al. : Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 2021;8:130–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yonter SJ Alter K Bartels MN, et al. : What now for rehabilitation specialists? Coronavirus disease 2019 questions and answers. Arch Phys Med Rehabil 2020;101:2233–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McNeary L, Maltser S, Verduzco-Gutierrez M: Navigating coronavirus disease 2019 (Covid-19) in physiatry: a CAN report for inpatient rehabilitation facilities. PM R 2020;12:512–5 [DOI] [PubMed] [Google Scholar]
- 11.Boldrini P Bernetti A Fiore P, SIMFER Executive Committee, SIMFER Committee for International Affairs : Impact of COVID-19 outbreak on rehabilitation services and physical and rehabilitation medicine physicians’ activities in Italy. An official document of the Italian PRM Society (SIMFER). Eur J Phys Rehabil Med 2020;56:316–8 [DOI] [PubMed] [Google Scholar]
- 12.Liu K Zhang W Yang Y, et al. : Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Complement Ther Clin Pract 2020;39:101166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hermann M Pekacka-Egli AM Witassek F, et al. : Feasibility and efficacy of cardiopulmonary rehabilitation after COVID-19. Am J Phys Med Rehabil 2020;99:865–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta R Gupta A Ghosh AK, et al. : A paradigm for the pandemic: a Covid-19 recovery unit. NEJM Catal Innov Care Deliv 2020. doi: 10.1056/CAT.20.0238 [DOI] [Google Scholar]
- 15.Jaywant A Vanderlind WM Boas SJ, et al. : Behavioral interventions in acute COVID-19 recovery: a new opportunity for integrated care. Gen Hosp Psychiatry 2021;69:113–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miles A Connor NP Desai RV, et al. : Dysphagia care across the continuum: a multidisciplinary dysphagia research society taskforce report of service-delivery during the COVID-19 global pandemic. Dysphagia 2021;36:170–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jette DU Stilphen M Ranganathan VK, et al. : Validity of the AM-PAC “6-Clicks” inpatient daily activity and basic mobility short forms. Phys Ther 2014;94:379–91 [DOI] [PubMed] [Google Scholar]
- 18.Jette DU Stilphen M Ranganathan VK, et al. : Interrater Reliability of AM-PAC “6-Clicks” basic mobility and daily activity short forms. Phys Ther 2015;95:758–66 [DOI] [PubMed] [Google Scholar]
- 19.Pfoh ER Hamilton A Hu B, et al. : The Six-Clicks Mobility Measure: a useful tool for predicting discharge disposition. Arch Phys Med Rehabil 2020;101:1199–203 [DOI] [PubMed] [Google Scholar]
- 20.Gordan W Gerber D David DS, et al. : Relationship of speech-language pathology inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: the SCIRehab project. J Spinal Cord Med 2012;35:565–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bushi S, Barrett AM, Oh-Park M: Inpatient rehabilitation delirium screening: impact on acute care transfers and functional outcomes. PM R 2020;12:766–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Black-Schaffer RM, Winston C: Age and functional outcome after stroke. Top Stroke Rehabil 2004;11:23–32 [DOI] [PubMed] [Google Scholar]
- 23.Stein J, Visco CJ, Barbuto S: Rehabilitation medicine response to the COVID-19 pandemic. Am J Phys Med Rehabil 2020;99:573–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tay MRJ Ong PL Puah SH, et al. : Acute functional outcomes in critically ill COVID-19 patients. Front Med (Lausanne) 2021;7:615997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Korupolu R Francisco GE Levin H, et al. : Rehabilitation of critically ill COVID-19 survivors. J Int Soc Phys Rehabil Med 2020;3:45 [Google Scholar]
- 26.Puchner B Sahanic S Kirchmair R, et al. : Beneficial effects of multi-disciplinary rehabilitation in postacute COVID-19: an observational cohort study. Eur J Phys Rehabil Med 2021;57:189–98 [DOI] [PubMed] [Google Scholar]
- 27.Hameed F Palatulan E Jaywant A, et al. : Outcomes of a COVID-19 recovery program for patients hospitalized with SARS-CoV-2 infection in New York City: a prospective cohort study. PM R 2021;13:609–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Groah S Pham C Rounds A, et al. : COVID patients benefit from inpatient rehabilitation. SSRN 2021:3751322 [Google Scholar]
- 29.Ma J Hua T Zeng K, et al. : Influence of social isolation caused by coronavirus disease 2019 (COVID-19) on the psychological characteristics of hospitalized schizophrenia patients: a case-control study. Transl Psychiatry 2020;10:411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heinemann AW Wilson CS Huston T, et al. : Relationship of psychology inpatient rehabilitation services and patient characteristics to outcomes following spinal cord injury: the SCIRehab project. J Spinal Cord Med 2012;35:578–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peris A Bonizzoli M Iozzelli D, et al. : Early intra-intensive care unit psychological intervention promotes recovery from post traumatic stress disorders, anxiety and depression symptoms in critically ill patients. Crit Care 2011;15:R41. [DOI] [PMC free article] [PubMed] [Google Scholar]


