Supplemental Digital Content is available in the text.
Keywords: epidemiology, intensive care units, pediatric, patient admission, primary prevention, respiratory tract infections, severe acute respiratory syndrome coronavirus 2
Abstract
OBJECTIVES:
To characterize the impact of public health interventions on the volume and characteristics of admissions to the PICU.
DESIGN:
Multicenter retrospective cohort study.
SETTING:
Six U.S. referral PICUs during February 15, 2020–May 14, 2020, compared with the same months during 2017–2019 (baseline).
Patients:
PICU admissions excluding admissions for illnesses due to severe acute respiratory syndrome coronavirus 2 and readmissions during the same hospitalization.
INTERVENTIONS:
None.
MEASUREMENTS AND MAIN RESULTS:
Primary outcome was admission volumes during the period of stay-at-home orders (March 15, 2020–May 14, 2020) compared with baseline. Secondary outcomes were hospitalization characteristics including advanced support (e.g., invasive mechanical ventilation), PICU and hospital lengths of stay, and mortality. We used generalized linear mixed modeling to compare patient and admission characteristics during the stay-at-home orders period to baseline. We evaluated 7,960 admissions including 1,327 during March 15, 2020–May 14, 2020. Daily admissions and patients days were lower during the period of stay-at-home orders compared with baseline: median admissions 21 (interquartile range, 17–25) versus 36 (interquartile range, 30–42) (p < 0.001) and median patient days 93.0 (interquartile range, 55.9–136.7) versus 143.6 (interquartile range, 108.5–189.2) (p < 0.001). Admissions during the period of stay-at-home orders were less common in young children and for respiratory and infectious illnesses and more common for poisonings, endocrinopathies and for children with race/ethnicity categorized as other/unspecified. There were no differences in hospitalization characteristics except fewer patients received noninvasive ventilation during the period of stay-at-home orders.
CONCLUSIONS:
Reductions in PICU admissions suggest that much of pediatric critical illness in younger children and for respiratory and infectious illnesses may be preventable through targeted public health strategies.
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic fundamentally altered the way children work, play, and learn. In the United States, transmission events of SARS-CoV-2 were first identified in January of 2020. By March 16, 2020, all 50 states declared states of emergency, allowing enactment of stay-at-home orders alongside closure of schools, parks, and businesses (1). Universal mask wearing was also encouraged or mandated in many places. These sweeping public health interventions aimed at slowing the spread of the virus likely had significant unintended effects on the activities and health of children, the ripples of which have been observed in reports of decreased admission volumes to PICUs in the United States, Latin America, and Europe (2–6). This natural experiment raises the question of whether a substantial fraction of pediatric critical illness is preventable.
To better understand the proportion of pediatric critical illness that may be preventable, we studied the impact of United States public health interventions on the volume and characteristics of non-coronavirus disease (COVID) PICU admissions during a 2-month period early in the pandemic when most states enacted stay-at-home orders (7). We hypothesized that infectious diseases, primarily affecting younger children, decreased in response to pandemic measures.
MATERIALS AND METHODS
We conducted a retrospective, multicenter study across six U.S. pediatric regional referral centers in the Midwest, West, and South. The sites range in size from 12 to 84 beds, baseline annual PICU admission volumes were 650 to 4,000 patients, and all have active pediatric training programs. No site reported significant changes in referral patterns or PICU capacity between 2019 and 2020, and no site diverted pediatric admissions to repurpose beds for adult admissions.
We included PICU admissions during the study period February 15–May 14 during 2017–2020. Each site’s state began limiting gatherings and activities between March 10, 2020, and March 14, 2020, and each site was under a stay-at-home order by March 24, 2020, until at least May 8, 2020 (8) (Supplemental Table 1, http://links.lww.com/CCM/G594). We excluded repeat PICU readmissions during the same hospitalization and admissions for COVID. The primary analyses compared admissions during the stay-at-home order period, defined as March 15, 2020–May 14, 2020, to the same time period, March 15–May 14, during years 2017–2019 (baseline). We also compared daily admission volumes during February 15, 2020–March 14, 2020, to the same period during the baseline years (2017–2019).
We collected patient and admission characteristics including age, sex, race/ethnicity, admission source, primary diagnosis, preexisting medical conditions, severity of illness scores (Pediatric Risk of Mortality [PRISM] III score, Pediatric Index of Mortality risk of mortality), and elective admission status (9–11) (Supplemental Table 2, http://links.lww.com/CCM/G594). Hospitalization characteristics collected included use of continuous renal replacement therapy (CRRT), extracorporeal membrane oxygenation (ECMO), noninvasive ventilation (NIV) and invasive mechanical ventilation (including duration), PICU and hospital lengths of stay, and inhospital mortality.
Our primary outcome was volume of PICU admissions defined as number of admissions during the study period. Secondary outcomes included utilization of advanced support (CRRT, ECMO, NIV, invasive mechanical ventilation), PICU and hospital lengths of stay, and mortality.
Definitions
Primary diagnoses were grouped using Virtual Pediatric Systems (VPS)-defined categories (Supplemental Table 3, http://links.lww.com/CCM/G594). “Infectious” diagnoses include infectious diseases (e.g., septic shock) not primarily focused on the respiratory tract or CNS. The “Poisoning/adverse effects” category was primarily representative of drug intoxication. Primary diagnosis categories representing fewer than 3% of total admissions were combined and categorized as “Other.” Preexisting chronic conditions were classified as complex chronic conditions, noncomplex chronic conditions, or not a chronic condition based on the Pediatric Medical Complexity Algorithm 3.0 using a process derived from previously published work (Supplemental Tables 4 and 5, http://links.lww.com/CCM/G594) (12, 13). A “complicated PICU stay” was defined by receipt of either CRRT, ECMO, or invasive mechanical ventilation. A complete list of variable definitions is available in Supplemental Table 2 (http://links.lww.com/CCM/G594).
Statistical Analyses
Summary statistics were stratified by year of admission and reported as median and interquartile range (IQR) for continuous variables and frequency (percentage) for categorical variables. We compared median daily admission volumes and patient days across predefined time periods using the Wilcoxon rank-sum test. We used generalized linear mixed modeling to test for characteristics associated with admission during March 15, 2020–May 14, 2020, compared with the same months during 2017–2019 (baseline). We chose this analysis to account for sources of variability (e.g., site effects) not incorporated when reporting raw rates. We evaluated patient, admission, and hospitalization characteristics in univariate analyses. Continuous independent variables were scaled with mean zero and sd of one to facilitate model convergence. Categorical independent variables with more than two levels were assessed for overall significance using a likelihood ratio test. A random intercept was included for hospital to account for correlation. Very few subjects had repeated admissions within the study period (n = 421 [5.6%]) and a sensitivity analysis with a random intercept for subject showed negligible differences. Thus, we did not include a random intercept for subject. A multivariable model was developed by including independent variables associated with admission in 2020 (p < 0.1) with final variables selected using backward selection based on Akaike information criterion. There was not an interaction between diagnosis category and age nor evidence of collinearity. We used two-sided tests and a significance level of 0.05. Analyses were conducted using R Version 4.0.2 (2020-06-22; Vienna, Austria). This study was reviewed and approved by each site’s Institutional Review Board.
RESULTS
We evaluated 13,103 admissions during 2017–2020 between the dates of February 15 and May 14. We excluded 59 admissions for COVID and 601 PICU readmissions (Supplemental Fig. 1, http://links.lww.com/CCM/G594). Of the included admissions, 7,960 occurred between March 15 and May 14 (Table 1). Admission characteristics of the site contributing data extracted from the electronic health record (EHR) differed from the remaining VPS sites in the distribution of primary diagnoses and elective admissions (Supplemental Table 6, http://links.lww.com/CCM/G594).
TABLE 1.
Patient and Admission Characteristics Based on Year of Admission: March 15 to May 14
| Characteristic | 2017 (n = 2,079) | 2018 (n = 2,092) | 2019 (n = 2,462) | 2020 (n = 1,327) |
|---|---|---|---|---|
| Age category, n (%) | ||||
| < 5 yr | 1,032 (49.6) | 1,053 (50.3) | 1,273 (51.7) | 551 (41.5) |
| 5–10 yr | 376 (18.1) | 347 (16.6) | 393 (16.0) | 223 (16.8) |
| 10–18 yr | 553 (26.6) | 576 (27.5) | 666 (27.1) | 458 (34.5) |
| > 18 yr | 118 (5.6) | 116 (5.5) | 130 (5.3) | 95 (7.2) |
| Female sex, n (%) | 949 (45.6) | 939 (44.9) | 1,136 (46.1) | 607 (45.7) |
| Preexisting chronic conditions by Pediatric Medical Complexity Algorithm, n (%)a | ||||
| No chronic conditions | 1,036 (49.8) | 978 (46.7) | 1,191 (48.4) | 636 (47.9) |
| Complex chronic condition(s) | 510 (24.5) | 568 (27.2) | 712 (28.9) | 354 (26.7) |
| Noncomplex chronic condition(s) | 193 (9.3) | 171 (8.2) | 213 (8.7) | 142 (10.7) |
| Race/ethnicity, n (%)a | ||||
| White | 862 (41.5) | 844 (40.3) | 991 (40.3) | 517 (39.0) |
| Hispanic or Latino | 370 (17.8) | 382 (18.3) | 493 (20.0) | 256 (19.3) |
| Black or African American | 284 (13.7) | 248 (11.9) | 335 (13.6) | 152 (11.5) |
| Other/unspecified | 213 (10.2) | 242 (11.6) | 296 (12.0) | 203 (15.3) |
| Admission source, n (%)a | ||||
| Emergency department/direct admit | 1,013 (48.7) | 978 (46.7) | 1,279 (51.9) | 703 (53.0) |
| Operating room | 396 (19.0) | 365 (17.4) | 457 (18.6) | 234 (17.6) |
| Ward | 283 (13.6) | 314 (15.0) | 320 (13.0) | 159 (12.0) |
| Another ICU | 50 (2.4) | 60 (2.9) | 61 (2.5) | 36 (2.7) |
| Elective admission, n (%) | 397 (19.1) | 387 (18.5) | 484 (20.0) | 255 (19.2) |
| Primary diagnosis, n (%) | ||||
| Respiratory | 722 (34.7) | 723 (34.6) | 1,021 (41.5) | 304 (22.9) |
| Neurologic | 241 (11.6) | 280 (13.4) | 309 (12.6) | 207 (15.6) |
| Infectious | 207 (10.0) | 208 (9.9) | 180 (7.3) | 95 (7.2) |
| Injury | 142 (6.8) | 115 (5.5) | 137 (5.6) | 107 (8.1) |
| Oncologic | 100 (4.8) | 83 (4.0) | 113 (4.6) | 78 (5.9) |
| Poisoning/adverse effects | 90 (4.3) | 78 (3.7) | 102 (4.1) | 112 (8.4) |
| Cardiovascular | 86 (4.1) | 94 (4.5) | 78 (3.2) | 59 (4.4) |
| Endocrine | 64 (3.1) | 59 (2.8) | 87 (3.5) | 90 (6.8) |
| Other | 288 (13.9) | 309 (14.8) | 325 (13.2) | 205 (15.4) |
| Undetermined | 139 (6.7) | 143 (6.8) | 110 (4.5) | 70 (5.3) |
| Pediatric Risk of Mortality III, median (IQR)a | 2 (0–5) | 2 (0–5) | 2 (0–5) | 3 (0–6) |
| Pediatric Index of Mortality risk of mortality (%), median (IQR)a | 0.78 (0.25–2.9) | 0.83 (0.24–2.87) | 0.79 (0.25–2.52) | 0.82 (0.33–2.96) |
IQR = interquartile range.
aData element available from five sites (n = 6,708 admissions).
Number of patients with data available: n = 1,742 (2017), n = 1,717 (2018), n = 2,117 (2019), and n = 1,132 (2020).
Percentages may not sum to 100 due to rounding.
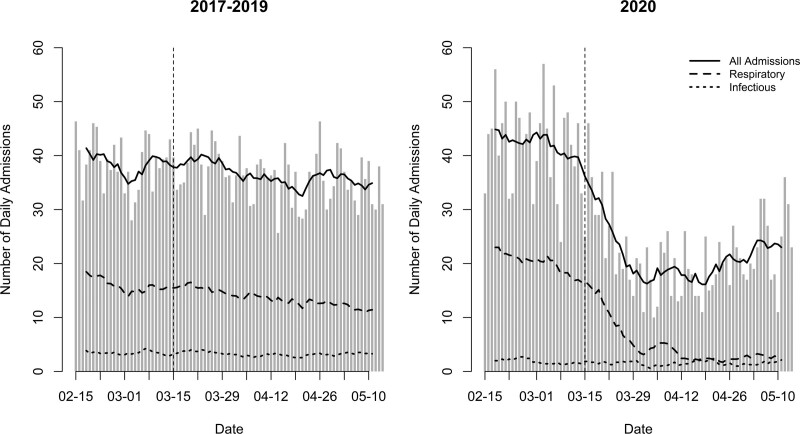
Admission volumes were markedly lower during the 2020 period of stay-at-home orders compared with baseline (Fig. 1). Daily admission volumes decreased 41.7% to a median 21 (IQR, 17–25) during the stay-at-home period from 36 (IQR, 30–42) during the baseline period (p < 0.001). Similarly, daily patient days decreased by 35.2% to a median 93.0 (IQR, 55.9–136.7) from 143.6 (IQR, 108.5–189.2) (p < 0.001). These differences were primarily reflected in lower volumes of respiratory diagnoses with median 4 (IQR, 2–6) daily admissions versus 13 (IQR, 10–16.5) (p < 0.001) and infectious diagnoses with median 1 (IQR, 1–2) daily admission versus 3 (IQR, 2–4) (p < 0.001) during the stay-at-home period compared with baseline, respectively.
Figure 1.
Moving 7-d average of daily PICU admissions during the baseline (averaged over 2017–2019) and 2020 study periods. Stay-at-home orders were initiated at all sites by March 24, 2020.
To ensure that 2020 was not an unusual year prior to the initiation of stay-at-home orders, we also compared admission volumes during the month leading up to the stay-at-home orders (February 15–March 14) with the same month during 2017–2019 (Fig. 1). Admission volumes during this period were similar in 2020 compared with 2017–2019: median daily admissions 44 (IQR, 36–47) versus 38.5 (IQR, 32–45.3) (p = 0.069) and daily patient days 162.3 (IQR, 142.4–214.2) versus 148.1 (IQR, 121.1–227.0) (p = 0.181).
In univariate analyses, younger patients and patients of White race/ethnicity compared with patients categorized as “other” were less likely to be admitted in 2020 versus the baseline period (Supplemental Fig. 2, http://links.lww.com/CCM/G594). The distribution of patients with preexisting chronic conditions did not differ between 2020 and baseline. Admissions were less likely from the ward or operating room compared with admission from the emergency department/direct admission. Admission for a primary respiratory or infectious diagnosis was less frequent in 2020 compared with the baseline period. Conversely, admissions with primary diagnosis categories of neurologic, injury, poisoning/adverse events, and endocrine were more likely in 2020. Patients admitted in 2020 had higher PRISM III scores compared with the baseline period.
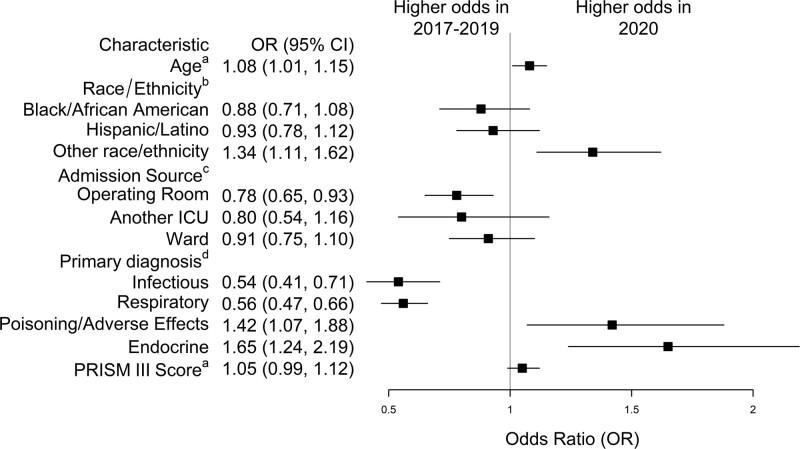
In multivariable analyses, younger patients and patients of White race/ethnicity compared with patients categorized as “other” were less likely to be admitted in 2020 versus the baseline period (Fig. 2). Admissions were less likely to be from the operating room compared with admission from the emergency department/direct admission. Primary respiratory (odds ratio [OR], 0.56; 95% CI, 0.47–0.66; p < 0.001) and infectious diagnoses (OR, 0.54; 95% CI, 0.41–0.71; p < 0.001) were less likely in 2020 compared with the baseline period. Poisoning/adverse effects (OR, 1.42; 95% CI, 1.07–1.88; p = 0.02) and endocrinopathies (OR, 1.65; 95% CI, 1.24–2.19; p = 0.001) were more common in 2020.
Figure 2.
Multivariable model of patient and admission factors independently associated with admission during March 15, 2020–May 14, 2020, versus the same time period during the baseline period (2017–2019). Model includes data from 6,688 admissions across five hospitals. aOdds ratios (ORs) for continuous variables are per sd (age = 6.6 yr, Pediatric Risk of Mortality [PRISM] III score = 5.5 points). bReference: White, non-Hispanic (largest group). cReference: emergency department/direct admit. dReference: any other diagnosis.
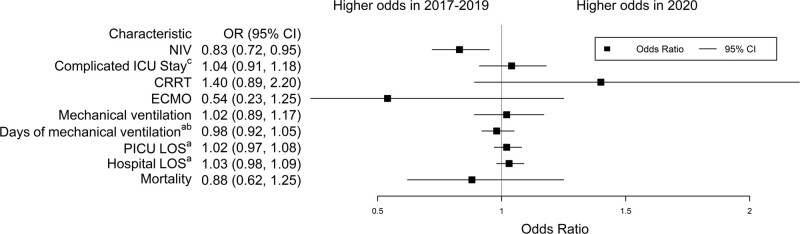
Next, we compared hospitalization characteristics between 2020 and the baseline period (Supplemental Table 7, http://links.lww.com/CCM/G594). In univariate regression, there were no differences in the distribution of subjects supported with CRRT, ECMO, invasive mechanical ventilation, or those with a complicated PICU stay (Fig. 3). Fewer patients in 2020 were supported with NIV compared with the baseline period. There was no difference in duration of invasive mechanical ventilation, PICU or hospital lengths of stay, or mortality.
Figure 3.
Univariate models of hospitalization outcomes associated with admission during March 15, 2020–May 14, 2020, versus the same time period during the baseline period (2017–2019). aOdds ratios (ORs) for continuous variables are per 1 sd (duration of invasive mechanical ventilation = 7.9 d, PICU length of stay [LOS] = 10.4 d, hospital LOS = 30.3 d). bVariable available from five centers (n = 6,708 admissions). Remainder from six centers (n = 7,960 admissions). cComplicated PICU stay includes: continuous renal replacement therapy (CRRT), extracorporeal membrane oxygenation (ECMO), or invasive mechanical ventilation. NIV = noninvasive ventilation.
DISCUSSION
These findings clearly demonstrate that the implementation of public health measures intended to decrease SARS-CoV-2 transmission was associated with significant changes in the patterns of pediatric critical illness observed across a geographically diverse sample of U.S. pediatric centers. These findings are consistent with previous reports that stay-at-home orders affected the distribution of lower acuity pediatric acute care visits (14–27). In our cohort, decreasing social interaction was associated with fewer life-threatening illnesses in younger children and due to infectious diseases. Conversely, these measures were associated with more critical illnesses due to poisonings and endocrinopathies.
The decreased volume of pediatric critical illness is striking. We observed a 41.7% reduction in PICU admissions and a 35.2% reduction in patient days associated with stay-at-home orders. This observation implies that a significant portion of life-threatening illness in children could be prevented with public health-related behavioral modifications. Based on previously published U.S. healthcare cost data, these findings imply potentially preventable hospitalization costs in the billions of dollars annually for critically ill children (28, 29). Importantly, the similar rates of protection of patients with preexisting conditions suggest that some of the costliest PICU stays are avoidable (29, 30). While stay-at-home orders have many undesirable social and economic consequences, these observations suggest that further analysis to determine the most effective components of the public health measures and to identify less intrusive, sustainable strategies could result in large medical and financial benefits.
Adult studies have suggested that decreased hospitalizations may reflect an increased proportion of patients being managed at home (31, 32). This explanation is unlikely to account for the observed changes in our data. With very limited exceptions, pediatric critical illnesses are not amenable to management at home. In support of this assertion, when comparing 2020 with the baseline period, we found similar proportions of patients with a complicated PICU stay, lengths of PICU and hospital stays, and overall mortality rates. This finding suggests that PICU admissions were decreased across the spectrum of illness severity, rather than only for those with less severe disease. Recent reports have also described excess overall mortality during the COVID pandemic, raising concerns that the pandemic has led to hospital avoidance and delayed presentations (33–37). To date, however, the 2020 mortality rate in individuals younger than 20 years old has remained similar or lower than expected, and our data do not provide evidence of widespread delays in seeking care (38). Taking these findings together, we conclude that the decreased PICU admission volume during the study period is the result of a lower frequency of life-threatening illness in children.
Our results suggest that the lower volume is primarily attributable to a reduction in rates of respiratory illnesses, which has been reported across pediatric hospitalizations globally (2–4, 6, 14, 15, 23, 26, 39). This finding is also consistent with adult data showing a decline in non-COVID respiratory illness (40). In both age ranges, the likely cause is decreased transmission of common infectious diseases. For example, U.S. influenza transmission abruptly ended in mid-March 2020 as public health restrictions were being implemented (41). While our data do not rule out alternate explanations for this observation such as virus-virus competition or other epidemiologic factors, the strong temporal association with the implementation of activity restrictions is highly suggestive that those interventions were causative of reduced non-COVID respiratory disease transmission.
We also found that the stay-at-home period was associated with a higher risk of pediatric critical illness due to both poisoning/adverse events and endocrinopathies. The Centers for Disease Control and Prevention reported increased visits for mental health illnesses associated with the public health restrictions across all age groups (21). Our data are consistent with this report given that most admissions in the Poisonings/adverse events category are related to intentional ingestions, suggesting that this increase represents mental illness exacerbated by social isolation or reduced access to mental health services (42). Similarly, our study suggests an increase in endocrinopathy admissions, primarily diabetic ketoacidosis. This finding is consistent with other reports of increased rates and more severe presentations of diabetic ketoacidosis attributed to SARS-CoV-2 infections (43, 44).
Our study is strengthened by inclusion of a multicenter cohort of referral PICUs admitting patients from geographically and ethnically diverse urban and rural regions throughout the United States and by the observation that all of the centers saw similar impacts from stay-at-home orders and physical distancing measures. However, our study has several limitations. This study relies on appropriate designation of diagnoses by data entry personnel, which may not always be accurate. One of the six centers collected data from the EHR rather than VPS, limiting the uniformity of the data particularly related to determination of primary diagnosis and elective admissions. Additionally, EHR data extraction was limited and led to missing data elements such as illness severity scores and durations of mechanical ventilation. However, inclusion of this site increased the generalizability of our results, strengthening the study overall. Also, fluctuations in admission volumes may be in part a result of minor changes in operations or referral patterns at individual sites. We anticipate that the 3-year baseline period, geographic site diversity, and statistical design accounted for these factors. Finally, our population is likely representative of the broad catchment area of these six PICUs during the study period evaluated, however, generalizability beyond these sites, across seasons, and during the period following the stay-at-home orders requires further study.
CONCLUSIONS
The physical distancing measures put in place to decrease transmission of SARS-CoV-2 were associated with widespread and substantial reductions in PICU admissions, suggesting that a considerable portion of pediatric critical illness may be preventable, particularly those due to respiratory and infectious illnesses. These findings may have important implications for child health and public policy. Further study is warranted to identify which strategies most effectively decrease transmission of childhood infections while avoiding the negative consequences of social isolation.
ACKNOWLEDGMENTS
We acknowledge the tremendous work of our data extraction team members including Deana Rich (Seattle Children’s Hospital), Jairo Chavez (Ann & Robert H. Lurie Children’s Hospital of Chicago), Laura Krulik, BSN, RN (Children’s Hospital Colorado), and Danielle Worthington (Nationwide Children’s Hospital). Virtual Pediatric Systems (VPS) data was provided by the VPS sites. No endorsement or editorial restriction of the interpretation of these data or opinions of the authors has been implied or stated.
Supplementary Material
Footnotes
*See also p. 2137.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Dr. Maddux’s institution received funding from the National Institutes of Health (NIH) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K23HD096018) and institutional funds from the University of Colorado’s Section of Pediatric Critical Care Medicine; she received support for article research from the NIH. The remaining authors have disclosed that they do not have any potential conflicts of interest.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
This work was completed at Dr. Harris’s prior institution: Northwestern University Feinberg School of Medicine, Chicago, IL and Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL.
REFERENCES
- 1.National Governors Association: Status of State COVID-19 Emergency Orders [Database on the Internet]. 2020. Available at: https://www.nga.org/state-covid-19-emergency-orders/. Accessed December 28, 2020
- 2.Araujo OR, Almeida CG, Lima-Setta F, et al. ; Brazilian Research Network in Pediatric Intensive Care (BRnet-PIC): The impact of the novel coronavirus on Brazilian PICUs. Pediatr Crit Care Med. 2020; 21:1059–1063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Graciano AL, Bhutta AT, Custer JW. Reduction in paediatric intensive care admissions during COVID-19 lockdown in Maryland, USA. BMJ Paediatr Open. 2020; 4:e000876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sperotto F, Wolfler A, Biban P, et al. ; Italian Network of Pediatric Intensive Care Unit Research Group (TIPNet): Unplanned and medical admissions to pediatric intensive care units significantly decreased during COVID-19 outbreak in Northern Italy. Eur J Pediatr. 2021; 180:643–648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vásquez-Hoyos P, Diaz-Rubio F, Monteverde-Fernandez N, et al. ; LARed Network: Reduced PICU respiratory admissions during COVID-19. Arch Dis Child. 2020. Oct 7. [online ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Williams TC, MacRae C, Swann OV, et al. Indirect effects of the COVID-19 pandemic on paediatric healthcare use and severe disease: A retrospective national cohort study. Arch Dis Child. 2021. Jan 15. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kates J, Michaud J, Tolbert J: Stay-At-Home Orders to Fight COVID-19 in the United States: The Risks of a Scattershot Approach. Policy Watch, 2020. Available at: https://www.kff.org/policy-watch/stay-at-home-orders-to-fight-covid19/. Accessed December 8, 2020
- 8.Moreland A, Herlihy C, Tynan MA, et al. ; CDC Public Health Law Program; CDC COVID-19 Response Team, Mitigation Policy Analysis Unit: Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement - United States, March 1-May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:1198–1203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pollack MM, Patel KM, Ruttimann UE. PRISM III: An updated Pediatric Risk of Mortality score. Crit Care Med. 1996; 24:743–752 [DOI] [PubMed] [Google Scholar]
- 10.Slater A, Shann F, Pearson G; Paediatric Index of Mortality (PIM) Study Group: PIM2: A revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003; 29:278–285 [DOI] [PubMed] [Google Scholar]
- 11.Straney L, Clements A, Parslow RC, et al. ; ANZICS Paediatric Study Group and the Paediatric Intensive Care Audit Network: Paediatric Index of Mortality 3: An updated model for predicting mortality in pediatric intensive care*. Pediatr Crit Care Med. 2013; 14:673–681 [DOI] [PubMed] [Google Scholar]
- 12.Edwards JD, Houtrow AJ, Vasilevskis EE, et al. Chronic conditions among children admitted to U.S. pediatric intensive care units: Their prevalence and impact on risk for mortality and prolonged length of stay*. Crit Care Med. 2012; 40:2196–2203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simon TD, Haaland W, Hawley K, et al. Development and validation of the Pediatric Medical Complexity Algorithm (PMCA) Version 3.0. Acad Pediatr. 2018; 18:577–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Angoulvant F, Ouldali N, Yang DD, et al. COVID-19 pandemic: Impact caused by school closure and national lockdown on pediatric visits and admissions for viral and non-viral infections, a time series analysis. Clin Infect Dis. 2021; 72:319–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Britton PN, Hu N, Saravanos G, et al. COVID-19 public health measures and respiratory syncytial virus. Lancet Child Adolesc Health. 2020; 4:e42–e43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dann L, Fitzsimons J, Gorman KM, et al. Disappearing act: COVID-19 and paediatric emergency department attendances. Arch Dis Child. 2020; 105:810–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dean P, Zhang Y, Frey M, et al. The impact of public health interventions on critical illness in the pediatric emergency department during the SARS-CoV-2 pandemic. J Am Coll Emerg Physicians Open. 2020; 1:1542–1551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dopfer C, Wetzke M, Zychlinsky Scharff A, et al. COVID-19 related reduction in pediatric emergency healthcare utilization - a concerning trend. BMC Pediatr. 2020; 20:427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Even L, Lipshaw MJ, Wilson PM, et al. Pediatric emergency department volumes and throughput during the COVID-19 pandemic. Am J Emerg Med. 2020. Sep 28. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamill JK, Sawyer MC. Reduction of childhood trauma during the COVID-19 level 4 lockdown in New Zealand. ANZ J Surg. 2020; 90:1242–1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hartnett KP, Kite-Powell A, DeVies J, et al. ; National Syndromic Surveillance Program Community of Practice: Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:699–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Isba R, Edge R, Jenner R, et al. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch Dis Child. 2020; 105:704. [DOI] [PubMed] [Google Scholar]
- 23.Nagakumar P, Bush A, Gupta A. Childhood acute respiratory illnesses: Will normal inadequate services be resumed? Arch Dis Child. 2021. Jan 8. [online ahead of print] [DOI] [PubMed] [Google Scholar]
- 24.Pines JM, Zocchi MS, Black BS, et al. ; US Acute Care Solutions Research Group: Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med. 2021; 41:201–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scaramuzza A, Tagliaferri F, Bonetti L, et al. Changing admission patterns in paediatric emergency departments during the COVID-19 pandemic. Arch Dis Child. 2020; 105:704–706 [DOI] [PubMed] [Google Scholar]
- 26.Taquechel K, Diwadkar AR, Sayed S, et al. Pediatric asthma health care utilization, viral testing, and air pollution changes during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020; 8:3378–3387.e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bellan M, Gavelli F, Hayden E, et al. Pattern of emergency department referral during the Covid-19 outbreak in Italy. Panminerva Med. 2020. Jun 16. [online ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Gupta P, Rettiganti M. Relationship of hospital costs with mortality in pediatric critical care: A multi-institutional analysis. Pediatr Crit Care Med. 2017; 18:541–549 [DOI] [PubMed] [Google Scholar]
- 29.Moore BJ, Freeman WJ, Jiang HJ. Costs of Pediatric Hospital Stays, 2016. HCUP Statistical Brief #250. Agency for Healthcare Research and Quality, 2019. Available at: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb250-Pediatric-Stays-Costs-2016.jsp. Accessed December 28, 2020 [PubMed] [Google Scholar]
- 30.Chan T, Rodean J, Richardson T, et al. Pediatric critical care resource use by children with medical complexity. J Pediatr. 2016; 177:197–203.e1 [DOI] [PubMed] [Google Scholar]
- 31.Bhambhvani HP, Rodrigues AJ, Yu JS, et al. Hospital volumes of 5 medical emergencies in the COVID-19 pandemic in 2 US medical centers. JAMA Intern Med. 2021; 181:272–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blecker S, Jones SA, Petrilli CM, et al. Hospitalizations for chronic disease and acute conditions in the time of COVID-19. JAMA Intern Med. 2021; 181:269–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lazzerini M, Barbi E, Apicella A, et al. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020; 4:e10–e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weinberger DM, Chen J, Cohen T, et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Inter Med. 2020; 180:1336–1344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Place R, Lee J, Howell J. Rate of pediatric appendiceal perforation at a children’s hospital during the COVID-19 pandemic compared with the previous year. JAMA Netw Open. 2020; 3:e2027948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Woolf SH, Chapman DA, Sabo RT, et al. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. 2020; 324:510–513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Woolf SH, Chapman DA, Sabo RT, et al. Excess deaths from COVID-19 and other causes, March-July 2020. JAMA. 2020; 324:1562–1564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rossen LM, Branum AM, Ahmad FB, et al. Excess deaths associated with COVID-19, by age and race and ethnicity - United States, January 26-October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:1522–1527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li H, Yu G, Duan H, et al. Changes in children’s healthcare visits during coronavirus disease-2019 pandemic in Hangzhou, China. J Pediatr. 2020; 224:146–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Birkmeyer JD, Barnato A, Birkmeyer N, et al. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood). 2020; 39:2010–2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.World Health Organization: Influenza Laboratory Surveillance Information by the Global Influenza Surveillance and Response System (GISRS) [Database on the Internet]. 2021. Available at: https://apps.who.int/flumart/Default?ReportNo=7. Accessed April 26, 2021
- 42.Green EL: Student Suicides Push Las Vegas Schools to Open. New York Times 2021, Sect. Section A. Available at: https://www.nytimes.com/2021/01/24/us/politics/student-suicides-nevada-coronavirus.html. Accessed January 24, 2021
- 43.Rubino F, Amiel SA, Zimmet P, et al. New-onset diabetes in COVID-19. N Engl J Med. 2020; 383:789–790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Unsworth R, Wallace S, Oliver NS, et al. New-onset type 1 diabetes in children during COVID-19: Multicenter regional findings in the U.K. Diabetes Care. 2020; 43:e170–e171 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.