Pharmacist-prescribed contraception is intended to increase access; however, the current rate of Utah pharmacy participation leaves many underserved who have the greatest need for additional access.
OBJECTIVE:
To assess pharmacy participation in and accessibility of pharmacist-prescribed contraception after legislation effective in the state of Utah in 2019.
METHODS:
A secret-shopper telephone survey was used to assess participation in pharmacist-prescribed contraception. Geospatial analysis was used to map the distribution of participating pharmacies by population characteristics.
RESULTS:
Of all operating Class A retail pharmacies in Utah, 127 (27%) were providing pharmacist-prescribed contraception 1 year after implementation of the Utah standing order. Oral contraceptive pills were widely accessible (100%); however, other allowed methods were not (vaginal ring 14%; contraceptive patch 2%). Consultation fees and medication costs varied widely. Participating pharmacies were mainly concentrated in population centers. Assuming access to a personal vehicle, urban areas with a high percentage of Hispanic people (Utah's largest minority race or ethnicity group) have access to a participating pharmacy within a 20-minute driving distance. However, access in rural areas with a high percentage Hispanic or other minority were limited. We identified 235 (40%) census tracts with a high proportion of Utah's residents living below the poverty line or of minority race or ethnicity who also had low access to pharmacist-prescribed contraception.
CONCLUSIONS:
Although the pharmacy-based model is intended to increase access to contraception, practical availability 1 year after the authorization of pharmacist-prescribed contraception in Utah suggests that this service does not adequately serve rural areas, particularly rural areas with a high proportion of minorities and those living below the federal poverty line.
Recent family planning research has largely focused on increasing access to and use of long-acting reversible contraceptives.1,2 Although use of these methods has increased, short-acting reversible methods, such as the oral contraceptive pill, remain the most commonly used reversible contraceptive methods in the United States.3,4 Despite recent declines, 45% of U.S. pregnancies are unintended,5 with 95% attributable to inconsistent, incorrect, or nonuse of contraceptives.6 Lack of reliable access contributes to inconsistent or nonuse of contraception.7,8
In the United States, access to hormonal contraception typically involves an initial visit with a health care professional. However, a required health care visit may pose logistical difficulties (time for appointments, scheduling difficulties, costs, other issues) that can function as a barrier to contraceptive use.9,10 Among a nationally representative sample of U.S. adult women aged 18–44 years at-risk for unintended pregnancy, 29% of those who had tried to obtain a hormonal contraception prescription reported difficulties in either obtaining or refilling that prescription.10
Pharmacist-prescribed contraception has been proposed as one method for increasing access to contraceptives by offering more convenient locations, extended hours of operation, and ability to avoid gaps when away from home.7,11–13 Among a sample of English-speaking U.S. adult women at risk for unintended pregnancy, 54% reported choosing their current contraceptive method because it did not require a prescription.11 Among the same sample, 41% of those not using contraception indicated they would begin using a hormonal method if it were readily available at a pharmacy without a prescription.11 These findings suggest that a widely deployed pharmacist-prescribed contraceptive model could increase the overall use and consistency of more effective hormonal contraceptive methods.
Utah is home to 3.2 million people, including nearly 700,000 females of reproductive age.14 Utah is predominately made up of White people who are not Hispanic (77.8%). Hispanic people comprise the largest minority population in Utah (14.4%) with all other race or ethnic groups comprising less than 3% of the population.15 Utah has a higher fertility rate than the United States overall (64.8 vs 59.1 live births per 1,000 females of reproductive age) with a relatively low proportion of pregnancies reported as unintended (21.2% from 2016 to 2018).16 Similar to the United States overall, a higher percentage of live births in adolescents (59%) and young adults (18–19 years; 48.1%) are considered by their mothers to be unintended.16
In 2019, the Utah State Health Department issued a standing order authorized by the State Legislature (2018 Senate Bill 184) allowing pharmacist-prescribed contraception. Under the order, pharmacists who are licensed under the Pharmacy Practice Act and have received special training are able to prescribe oral contraceptive pills, vaginal rings, or contraceptive patches to adult women who have completed a self-assessment indicating no contraindications to contraception. The self-assessment (available at: https://dopl.utah.gov/pharm/hormonal_contraception_questionnaire.pdf) complies with the U.S. Selected Practice Recommendations for Contraceptive Use, 2016. After the initial 30-day prescription, the pharmacist is minimally required to evaluate side effects and patient concerns at 3 months, 12 months, and then annually for 4 years for as long as the patient desires to continue the prescription. Prescriptions continuing longer than 36 months require evidence that the patient has been seen by a primary care or women's health professional within the previous 2 years.17
The purpose of the current study was to evaluate pharmacy participation in and patient accessibility to pharmacist-prescribed contraception, 1 year after the standing order was issued. Specifically, we sought to 1) determine the percentage of pharmacies that had completed the requirements for participation, 2) determine realized accessibility through a secret-shopper method, and 3) evaluate the geographic distribution of participating pharmacies.
METHODS
We used a secret shopper telephone survey to assess pharmacy response to individuals inquiring about pharmacist-prescribed contraception. This method was modeled after similar research conducted in California.18 This study does not meet the requirements for human subject research and was therefore exempt from institutional review board approval, as confirmed by the Brigham Young University Institutional Review Board.
Three female research assistants were trained in the secret-shopper technique and results of the pharmacy contact were recorded in an online survey form. Contacts were made from June 25 to July 17, 2020. We attempted to contact by telephone all of the pharmacies identified by the Utah Health Department as enrolled in contraceptive prescribing (n=173) as of June 25, 2020. Because we assumed that women seeking contraceptives directly from a pharmacy may be unaware of the enrollment list provided by the state health department, we additionally contacted an approximately 15% random sample of nonenrolled pharmacies (n=50) to assess the response. If the pharmacy did not answer, the caller tried again on different days during normal business hours. If the pharmacy did not answer after three attempts, it was considered uncontactable.
Callers posed as adult women interested in obtaining contraception and opened the conversation by stating that they had heard they could get contraception at a pharmacy without a prescription. Based on the response to this question, callers assessed the availability of contraceptive methods, screening expectations, any restrictions, and associated costs while maintaining natural conversation. A generalized script is shown in Appendix 1, available online at http://links.lww.com/AOG/C485. Pharmacies that stated they did not provide contraceptive prescribing were asked for a referral to a participating pharmacy.
Data at the census tract level for population, poverty, race, and ethnicity were compiled from the 2018 5-Year U.S. Census Bureau American Community Survey. A census tract is a small geographic region, typically subdivisions of a county or equivalent entity, with a population size between 1,200 and 8,000 people. Census tracts are defined by the U.S. Census Bureau for the purposes of taking a decennial census and establishing a stable set of geographic units for the presentation of statistical data.19 Race and ethnicity were considered in this study as persons of minority race or ethnicity have an increased likelihood for unmet contraceptive need, even when controlling for poverty.20 Shapefiles indicating land ownership, major cities, major lakes, and major roadways were compiled from the Utah Automated Graphic Reference Center. A shapefile is a set of data formatted so that geographic layers can be read into a geographic information system. It contains all the information about map projections, boundaries, features, and data associated with those features. Data for location of pharmacies were collected from Rxopen.org.21 Results from the secret shopper calling data were merged with pharmacy locations to classify all pharmacies in Utah as either participating or nonparticipating under the pharmacist-prescribed contraception standing order.
For both the enrolled and nonenrolled pharmacies, proportions were calculated to describe pharmacy participation, screening criteria, and service costs. All proportions were calculated overall as well as stratified by pharmacy characteristics (ie, rural vs nonrural; independent vs chain). Rural or nonrural classification was based on methodology and data from the U.S. Census Bureau.22
ArcGIS Pro 2.6.1 was used to generate service areas of 5-, 10-, and 20-minute driving distances around participating pharmacies. The service areas were overlaid on six maps each displaying different demographic characteristics of Utah: population density (calculated as people per square mile), percent below the federal poverty line, percent minority race or ethnicity (calculated as total population minus percent White-only race), percent Hispanic, percent Black or African American, percent Native American, and percent of females of reproductive age in the population without health insurance. We calculated the proportion of all persons who live within a 20-minute drive of a participating pharmacy, as well as the proportion of persons living below the federal poverty line or of minority race or ethnicity.
We further created a raster map of the density of participating pharmacies across Utah using the kernel density function in ArcGIS Pro. A raster map stores data according to pixels in a map, rather than within a polygon file such as a political boundary. Raster maps are commonly used for display of maps that change continually across space, such as elevation or temperature. Kernel density determines the spatial density of points using a method of calculating proximity of features (pharmacies) within a certain area of each pixel on the map. We turned the resulting raster into a highly dense grid of points, spatially joined the points to the census tracts, and averaged the density of participating pharmacies within each census tract. We also calculated the proportion of Utah's residents below the federal poverty line, reproductive-aged females without health insurance, all minority populations and percent of the total Hispanic, Native American, and Black populations using data from the 2018 5-Year U.S. Census Bureau American Community Survey for each census tract. We plotted correlations between pharmacy density and population demographic variables for each census tract as a method of identifying census tracts with limited access to participating pharmacies and high proportions of marginalized persons who are most likely to experience difficulty accessing contraceptives, specifically, those living below the federal poverty line, females without health insurance, and racial and ethnic minorities. Finally, we identified census tracts that were in the top quartile for at least one of our marginalized groups and also had a low density of participating pharmacies to identify underserved areas.
RESULTS
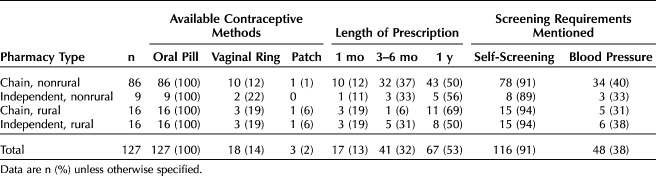
Of the 173 pharmacies identified as enrolled in the program by the Utah State Health Department, 163 could be reached. The remaining 10 pharmacies were permanently closed, unreachable, or duplicates. Of the 163 contactable, enrolled pharmacies, 127 indicated that they were participating in contraceptive prescribing. These 127 enrolled and participating pharmacies comprise 28% of all operating Class A retail pharmacies in Utah. Of the 127 participating pharmacies, most were classified as chain (n=102; 80%) and most were nonrural (n=95; 75%) (Fig. 1). All stated that the oral contraceptive pill was available through the pharmacist-prescribed contraceptive program, whereas only 14% and 2%, respectively, stated that they offer the vaginal ring or the contraceptive patch. Most (91%) indicated that a self-screening assessment would be required and 38% mentioned that blood pressure screening would be required. The remaining pharmacy classifications and descriptive information can be viewed in Table 1.
Fig. 1. Flowchart for pharmacy sampling and participation.
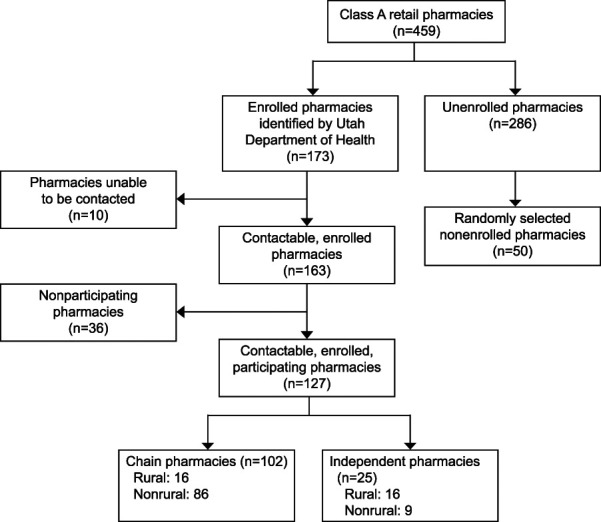
Magnusson. Pharmacist-Prescribed Contraceptives in Utah. Obstet Gynecol 2021.
Table 1.
Pharmacy Classification, Method Availability, Prescription Length, and Screening Procedures for Participating Pharmacies
Pharmacist consultation fees varied widely across the participating pharmacies, ranging from $0 to $70. Only 2% (n=3) of the pharmacies provided a no-cost consultation; 22.8% reported a consultation fee between $20 and $29, the majority (58.3%) reported a fee between $30 and $39%, and 12% reported fees of more than $40. There was no difference in consultation fees by rural compared with nonrural location. The reported monthly medication costs varied across pharmacies. Approximately half (n=60; 47%) reported an estimated cost of $20 per month, 13% reported less than $20 per month, 9% reported more than $20 per month, and one third (31%) stated only that the cost of the medication, “depends on insurance.”
Among the 36 enrolled pharmacies that indicated they were not participating in the program, five stated that they normally offer these services, but had temporarily stopped because of the coronavirus disease 2019 (COVID-19) pandemic. When asked, approximately half (n=19; 53%) provided an alternative pharmacy or clinic where contraceptives could be obtained.
Of the randomly selected sample of 50 nonenrolled pharmacies, 47 were contactable. Of these, 44 (94%) indicated that they do not provide contraception without a prescription from a physician (as was expected) and three (7%) indicated that they do provide that service. Similar to the first sample, half (n=22; 50%) provided an alternative pharmacy or clinic when asked. The sample of nonenrolled pharmacies was classified as follows: chain and nonrural (n=22), independent and nonrural (n=17), chain and rural (n=3), and independent and rural (n=5).
Each of the three nonenrolled pharmacies that indicated participation was classified as independent and nonrural. All three offer a year-long prescription of the oral pill; one also offers the transdermal patch and another the vaginal ring. All three pharmacies explained the self-screen and blood pressure screening that would be necessary. The pharmacist consultation fees for each were $0, $25, and $35; the monthly medication fee was $10 for two pharmacies and $19 for the other.
Appendices 2–10 (available online at http://links.lww.com/AOG/C485) provide descriptive spatial information regarding land designation, Utah population density, and the geographic distribution of the population by sociodemographic characteristics.
Appendix 11 (available online at http://links.lww.com/AOG/C485) shows the participating pharmacies with 5-, 10-, and 20-minute one-way driving distances marked. Participating pharmacies clustered around population centers and were more prevalent where the percent below the federal poverty line and the percent minority were lower. Assuming access to a personal vehicle, urban census tracts (eg, West Valley City) with a high percentage of Hispanic people (Utah's largest minority race or ethnicity group) have access to a participating pharmacy within a 20-minute driving distance. However, access in rural areas with a high percentage Hispanic or other minority were limited. Tracts with a concentration of Black residents are in more urban areas and generally have coverage within a 20-minute one-way drive by car. However, tracts with the highest proportions of Native American populations (Southeast corner of Utah and in the East side of Utah in Uinta County), particularly reservation lands, have very little or no access to pharmacist-prescribed contraceptives.
Appendices 12 and 13 (available online at http://links.lww.com/AOG/C485) provide graphs and details on the spatial analysis used to identify areas that had lower pharmacy density and more marginalized populations. The identified census tracts were mapped and are displayed in Figure 2. A total of 235 (40%) census tracts had a high proportion of Utah's residents living below the poverty line or of minority race or ethnicity and also had low access to pharmacist-prescribed contraception. These census tracts were almost entirely rural, though some were suburban and highly populated (in the Provo-Orem area).
Fig. 2. Census tracts (n=235) that were in the lower participating pharmacy density group and were in the top quartile for percentages of one of Utah's marginalized groups (minority race or ethnicity, percentage of females without health insurance, and percent below the poverty line). Map created with ESRI 2021. ArcGIS Pro: Release 2.8.2. Data from State of Utah, Utah Automated Graphic Reference Center. Available at: https://gis.utah.gov/and United States Census Bureau. American Community Survey 2018 5-Year Estimates Public Use Microdata Sample File. Washington, DC. Accessed at: https://www.census.gov/programs-surveys/acs/microdata/access.2018.html.
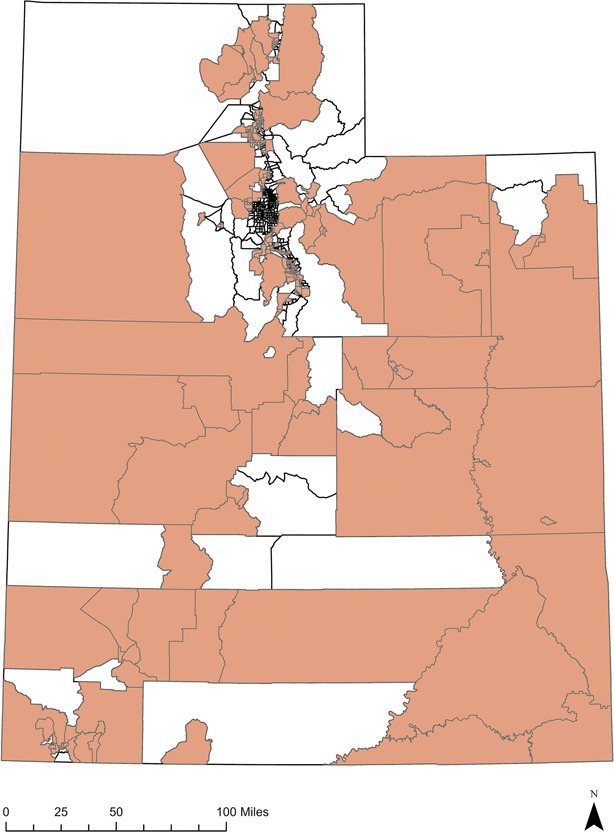
Magnusson. Pharmacist-Prescribed Contraceptives in Utah. Obstet Gynecol 2021.
DISCUSSION
The majority of unintended pregnancies are attributable to inconsistent, incorrect, or nonuse of contraception,6 highlighting the continued need for increased access to effective contraceptive methods. The most progressive initiative for increasing the accessibility of oral contraceptive pills is changing from a prescription-only model to an over-the-counter model. However, these efforts have stalled at the federal level.9 In lieu of over-the-counter contraception, a pharmacist-prescribed contraception model has been implemented in 16 states and the District of Colombia.23
The promise of the pharmacist-prescribed model is increased access owing to extended hours, more convenient locations, ability to obtain medications more quickly, and reduced time commitment.7,11–13 Research in four states identified convenience factors as the most common reasons for using pharmacy access.24 However, these benefits are partially dependent on wide-spread participation by pharmacies. One year into the program, Utah pharmacy participation was low, with fewer than 30% of retail pharmacies participating. This proportion is greater than observed after 1 year in California (5.1%; 2017),18 but less than recent estimates in Oregon (46%; 2019).25 The low implementation rate is in part due to a lack of participation among the largest pharmacy chains (Walgreens, CVS, Walmart, Rite Aid), which make up a substantial portion of all pharmacies.
We did not attempt to assess pharmacy staff awareness of the policy; however, anecdotally, some pharmacists or responding technicians stated that no pharmacies in Utah were able to prescribe contraception and others said that they were legally able to prescribe only contraceptive pills, both of which are false. Pharmacy staff knowledge varied. Several indicated that it was their first time answering these questions and others gave incorrect information, had to review procedures before answering, or did not know and did not attempt to find an answer. Although training of pharmacists is required, pharmacy technicians are often the gatekeepers. Inconsistency in responses suggests some pharmacy staff are not aware of policies and procedures even in participating pharmacies and pose a barrier to persons accessing the service.
Research in Oregon and California found that those seeking contraception from a pharmacist were younger and more likely to be uninsured than those who received their prescription in a clinic.26 In 2018, 12.6% of women aged 19–44 years were uninsured.27 Affordable options for contraception that do not require insurance are needed. Additionally, young adults, who have the highest rate of unintended pregnancy,5 may be hesitant to seek sexual and reproductive health care using parental insurance owing to privacy concerns.28 Pharmacist-prescribed contraception may increase access by providing privacy for insured dependents and affordability for the uninsured.
Pharmacy consultation fees, required at the initial screening by most pharmacies, averaged $30–40. Combined with the average cost of contraception ($20), out-of-pocket cost for uninsured patients averaged $50–60 for an initial 1-month supply. Unlike appointments with physicians, nurse practitioners, or physician assistants, pharmacist consultation fees are generally not covered by insurance. Even if the patient has insurance coverage for the medication, the consultation fees may be a barrier to service utilization.
The Utah standing order permits pharmacy contraceptive access only for women aged 18 years and older, ignoring the significant need for safe, effective contraception for adolescents. This is particularly important because 59% of live births among persons younger than 18 years in Utah result from unintended pregnancies in those younger than 18 years.16 The legislation also requires patients to see a health care professional every 2 years. This suggests that lawmakers see this service as a temporary solution to lapsing insurance coverage. It is unclear how this 2-year limit will be tracked and enforced or the proportion of users who may be affected.
The majority of Utah's census tracts that were home to a high proportion of minority persons, those living in poverty, or females without insurance had low access to participating pharmacies. Even within census tracts that have participating pharmacies within a 5-, 10-, or 20-minute drive, persons relying on public transportation may have significantly longer travel times. This analysis suggests that persons living in rural communities, those living in poverty, and minorities may not currently see significant increases in accessibility.
Despite relatively low participation in Utah, there is reason to believe that this model may be effective in reducing contraceptive use gaps and unintended pregnancies. Research in Oregon observed that in the first 24 months, pharmacist-prescribed contraception averted 51 unintended pregnancies and saved $1.6 million dollars among the Medicaid population.29 More research is needed to understand the effects of pharmacist-prescribed contraception on broader populations.
This research assessed pharmacy participation and the geographic distribution of participating pharmacies. This approach has advantages over prior research, which examined the percentage of all pharmacies that participated, but did not consider the geographic proximity to persons in need of contraception. This study did not consider awareness of potential users or resident uptake; thus, accessibility is defined only as geographic proximity rather than considering awareness and other barriers to service utilization.
Future research is needed to explore both general awareness of the policy and the user experience for pharmacist-prescribed contraception in Utah. Additionally, program effectiveness should be considered in terms of outcomes such as reducing contraceptive use gaps and averting unintended pregnancies. Research is needed to understand the barriers to pharmacy participation to inform public health initiatives aimed at expanding the number of participating pharmacies, particularly in rural areas.
Footnotes
This research was funded by a $1,500 College Undergraduate Research Award from the College of Life Sciences, Brigham Young University. Study methodology was included as part of the grant application process, but the funder did not consult on research design, collection or interpretation of data, writing, or publication venue.
Financial Disclosure The authors did not report any potential conflicts of interest.
Presented at the 2020 Annual Meeting of the American Public Health Association, held virtually, October 24–28, 2020.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/C486.
Contributor Information
Sarah R. Christensen, Email: sarahchristensen360@gmail.com.
Ashley B. Tanner, Email: abrown24@gmail.com.
J. B. Eyring, Email: jb.eyring@gmail.com.
Emily B. Pilling, Email: emilybpilling@gmail.com.
Chantel D. Sloan-Aagard, Email: chantel.sloan@byu.edu.
REFERENCES
- 1.Brandi K, Fuentes L. The history of tiered-effectiveness contraceptive counseling and the importance of patient-centered family planning care. Am J Obstet Gynecol 2020;222:S873–7. doi: 10.1016/j.ajog.2019.11.1271 [DOI] [PubMed] [Google Scholar]
- 2.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol 2010;203:115.e1–7. doi: 10.1016/j.ajog.2010.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones J, Mosher W, Daniels K. Current contraceptive use in the United States 2006-2010, and changes in patterns of use since 1995. Natl Health Stat Rep 2012:1–25. [PubMed] [Google Scholar]
- 4.Kavanaugh ML, Jerman J. Contraceptive method use in the United States: trends and characteristics between 2008, 2012 and 2014. Contraception 2018;97:14–21. doi: 10.1016/j.contraception.2017.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. New Engl J Med 2016;374:843–52. doi: 10.1056/NEJMsa1506575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sonfield A, Hasstedt K, Gold RB. Moving forward: family planning in the era of health reform . Guttmacher Institute;2014. doi: 10.1056/NEJMsa1506575 [DOI] [Google Scholar]
- 7.Smith JD, Oakley D. Why do women miss oral contraceptive pills? An analysis of women's self-described reasons for missed pills. J Midwifery women's Health 2005;50:380–5. doi: 10.1016/j.jmwh.2005.01.011 [DOI] [PubMed] [Google Scholar]
- 8.Pazol K, Whiteman MK, Folger SG, Kourtis AP, Marchbanks PA, Jamieson DJ. Sporadic contraceptive use and nonuse: age-specific prevalence and associated factors. Am J Obstet Gynecol 2015;212:324.e1–8. doi: 10.1016/j.ajog.2014.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sindhu KK, Adashi EY. Over-the-Counter oral contraceptives to reduce unintended pregnancies. JAMA 2020;324:939–40. doi: 10.1001/jama.2019.21862 [DOI] [PubMed] [Google Scholar]
- 10.Grindlay K, Grossman D. Prescription birth control access among US women at risk of unintended pregnancy. J Women's Health 2016;25:249–54. doi: 10.1089/jwh.2015.5312 [DOI] [PubMed] [Google Scholar]
- 11.Landau SC, Tapias MP, McGhee BT. Birth control within reach: a national survey on women's attitudes toward and interest in pharmacy access to hormonal contraception. Contraception 2006;74:463–70. doi: 10.1016/j.contraception.2006.07.006 [DOI] [PubMed] [Google Scholar]
- 12.Killion MM. Improving access to hormonal contraception methods. MCN Am J Maternal/Child Nurs 2020;45:124. doi: 10.1097/NMC.0000000000000600 [DOI] [PubMed] [Google Scholar]
- 13.Rafie S, Kelly S, Gray EK, Wong M, Gibbs S, Harper CC. Provider opinions regarding expanding access to hormonal contraception in pharmacies. Women's Health Issues 2016;26:153–60. doi: 10.1016/j.whi.2015.09.006 [DOI] [PubMed] [Google Scholar]
- 14.U.S. Census Bureau. Age and sex population estimates. In: U.S. Census Bureau American Community Survey. U.S. Census Bureau; 2019. Accessed May 10, 2021. https://data.census.gov/cedsci/table?q=Utah&tid=ACSDP1Y2019.DP05 [Google Scholar]
- 15.U.S. Census Bureau. QuickFacts Utah: population estimates, July 1, 2019. Accessed May 10, 2021. https://www.census.gov/quickfacts/UT [Google Scholar]
- 16.Utah Department of Health. Health indicator report of births from unintended pregnancies. Accessed September 2, 2021. https://ibis.health.utah.gov/ibisph-view/indicator/view/UniPreg.LHD.html
- 17.Utah State Legislature. SB 184: pharmacist dispensing authority amendments. Accessed October 12, 2019. https://le.utah.gov/∼2018/bills/static/SB0184.html [Google Scholar]
- 18.Batra P, Rafie S, Zhang Z, Singh AV, Bird CE, Sridhar A, et al. An evaluation of the implementation of pharmacist-prescribed hormonal contraceptives in California. Obstet Gynecol 2018;131:850–5. doi: 10.1097/ACOG.000000000002572 [DOI] [PubMed] [Google Scholar]
- 19.U.S. Census Bureau. Glossary: census tract. 2019. Accessed September 2, 2021. https://www.census.gov/programs-surveys/geography/about/glossary.html#par_textimage_13
- 20.Dehlendorf C, Park SY, Emeremni CA, Comer D, Vincett K, Borrero S. Racial/ethnic disparities in contraceptive use: variation by age and women's reproductive experiences. Am J Obstet Gynecol 2014. 219:526.e1–9. doi: 10.1016/j.ajog.2014.01.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.RxOpen. Facilities map. Accessed March 17, 2020. http://rxopen.org/ [Google Scholar]
- 22.U.S. Census Bureau. 2020 Census urban and rural classification. Revised December 2, 2019. Accessed May 10, 2021. https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural.html [Google Scholar]
- 23.National Alliance of State Pharmacy Associations. Pharmacist prescribing: hormonal contraceptives. Accessed September 2, 2021. https://naspa.us/resource/contraceptives/
- 24.Rodriguez MI, Edelman AB, Skye M, Darney BG. Reasons for and experience in obtaining pharmacist prescribed contraception. Contraception 2020;102:259–61. doi: 10.1016/j.contraception.2020.05.016 [DOI] [PubMed] [Google Scholar]
- 25.Rodriguez MI, Garg B, Williams SM, Souphanavong J, Schrote K, Darney BG. Availability of pharmacist prescription of contraception in rural areas of Oregon and New Mexico. Contraception 2020;101:210–2. doi: 10.1016/j.contraception.2020.05.016 [DOI] [PubMed] [Google Scholar]
- 26.Rodriguez MI, Edelman AB, Skye M, Anderson L, Darney BG. Association of pharmacist prescription with dispensed duration of hormonal contraception. JAMA Netw Open 2020;3:e205252. doi: 10.1001/jamanetworkopen.2020.5252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.America's Health Rankings. Health of women and children: uninsured women. Accessed May 10, 2021. https://www.americashealthrankings.org/explore/health-of-women-and-children/measure/Uninsured_women/state/ALL [Google Scholar]
- 28.Bessett D, Prager J, Havard J, Murphy DJ, Agénor M, Foster AM. Barriers to contraceptive access after health care reform: experiences of young adults in Massachusetts. Women's Health Issues 2015;25:91–6. doi: 10.1016.j.whi.2014.11.002 [DOI] [PubMed] [Google Scholar]
- 29.Rodriguez MI, Hersh A, Anderson LB, Hartung DM, Edelman AB. Association of pharmacist prescription of hormonal contraception with unintended pregnancies and Medicaid costs: characterizing pharmacist-prescribed hormonal contraception services and users in California and Oregon pharmacies. Obstet Gynecol 2019;133:1238–46. doi: 10.1097/AOG.0000000000003265 [DOI] [PubMed] [Google Scholar]