An epidemiologic and modeling study found that condom use remained relatively low and stable among US adolescent sexual minority males from 2011 to 2017 and moderate increases may reduce human immunodeficiency virus transmission.
Supplemental digital content is available in the text.
Abstract
Background
We examined condom use patterns and potential population-level effects of a hypothetical condom intervention on human immunodeficiency virus (HIV) transmission among adolescent sexual minority males (ASMM).
Methods
Using 3 data sets: national Youth Risk Behavior Survey 2015 to 2017 (YRBS-National), local YRBS data from 8 jurisdictions with sex of partner questions from 2011 to 2017 (YRBS-Trends), and American Men's Internet Survey (AMIS) 2014 to 2017, we assessed associations of condom use with year, age, and race/ethnicity among sexually active ASMM. Using a stochastic agent-based network epidemic model, structured and parameterized based on the above analyses, we calculated the percent of HIV infections averted over 10 years among ASMM ages 13 to 18 years by an intervention that increased condom use by 37% for 5 years and was delivered to 62% of ASMM at age 14 years.
Results
In YRBS, 51.8% (95% confidence interval [CI], 41.3–62.3%) and 37.9% (95% CI, 32.7–42.3%) reported condom use at last sexual intercourse in national and trend data sets, respectively. In AMIS, 47.3% (95% CI, 44.6–49.9%) reported condom use at last anal sex with a male partner. Temporal trends were not observed in any data set (P > 0.1). Condom use varied significantly by age in YRBS-National (P < 0.0001) and YRBS-Trends (P = 0.032) with 13- to 15-year-olds reporting the lowest use in both; age differences were not significant in AMIS (P = 0.919). Our hypothetical intervention averted a mean of 9.0% (95% simulation interval, −5.4% to 21.2%) of infections among ASMM.
Conclusions
Condom use among ASMM is low and appears to have remained stable during 2011 to 2017. Modeling suggests that condom use increases, consistent with previous interventions, have potential to avert 1 in 11 new HIV infections among ASMM.
Adolescent sexual minority males (ASMM) are at substantial risk for human immunodeficiency virus (HIV) acquisition. In the United States, male-male sex was the primary risk factor recorded in 94% of diagnosed HIV infections among 13- to 19-year-old males in 2017,1 and recent cohort studies among urban ASMM have found HIV incidences from 3.4 to 6.4/100 person-years.2–4 Despite advances in HIV prevention, diagnoses among U.S. ASMM remained stable from 2012 to 2017,1 indicating the need to increase HIV prevention efforts for this population.
Condoms are highly effective at preventing HIV transmission,5–7 but a recent meta-analysis found that 50% of ASMM used a condom at last sex and 44% reported condomless anal sex in the last 6 months,8 consistent with subsequent studies.4,9–14 Similar to trends among adolescents overall15 and adult men who have sex with men (MSM),16 1 study suggested that condom use at last sex has been declining among male adolescents who report only male partners.17 However, the majority of ASMM have male and female partners,18 and previous estimates have not been stratified by race/ethnicity or age.
Human immunodeficiency virus prevention has expanded to include preexposure prophylaxis (PrEP) and treatment as prevention,17,18 and previous epidemic modeling has demonstrated PrEP’s potential impact on HIV incidence among ASMM.19–22 However, low HIV testing rates23 and developmental, provider-related, and regulatory barriers to PrEP use3 may limit antiretroviral-based prevention’s potential among ASMM. Moreover, condoms are unique in protecting against numerous sexually transmitted infections. Multiple promising interventions to increase condom use among ASMM and young MSM have been studied recently,24–28 although few studies included boys in early high school or who have not sexually debuted. Modeling potential population-level effects of trends in and interventions to promote condom use may motivate and inform development and implementation of these interventions.
Here, we began by examining recent temporal patterns in condom use among ASMM using 3 data sets. Given rapid behavior change during adolescence29 and racial/ethnic disparities in HIV burden,1 we stratified analyses by age and race/ethnicity. We then incorporated results from these analyses into an epidemic model to explore potential population-level effects of a hypothetical condom intervention on HIV transmission among ASMM.
METHODS
Data Sources
Youth Risk Behavior Surveillance System
Youth Risk Behavior Surveillance System (YRBSS) includes biennial national, state, territorial, tribal government, and local school-based surveys of representative samples of 9th to 12th grade students.30 Since 2015, the national Youth Risk Behavior Survey (YRBS) has included questions about sexual orientation and sex of sex partners, allowing identification of ASMM. Some jurisdictions began including these questions as early as 2003 with increasing, sometimes inconsistent use over time. We analyzed 2 YRBS data sets: national data from 2015 to 2017 (YRBS-National) for national representativeness and a compiled data set of 8 jurisdictions that included these questions in all surveys from 2011 to 2017 (YRBS-Trends) for trend analyses. These jurisdictions (Delaware, Florida, Hawaii, Illinois, Michigan, New York City, Rhode Island, San Diego) represent ~57 million people, 18% of the 2017 US population.31s In YRBS analyses, we defined ASMM as male participants reporting any lifetime sexual contact with men.
American Men’s Internet Survey
The American Men’s Internet Survey (AMIS) is an annual Web-based behavioral survey of US cisgender males 15 years or older reporting oral or anal sex with a man in the last year.32s,33s Participants are recruited through convenience sampling using website and social media advertisements. We analyzed 2014 to 2017 data to: (1) address potential limitations of YRBS, including relatively few ASMM and not specifying sex of partners or sex act type when measuring condom use, and (2) examine condom use in a sample of ASMM who are potentially reachable through web-based interventions and, on average, older and at higher HIV risk. Because recruitment strategies, eligibility, and outcome definitions differ between YRBS and AMIS, comparing their sample compositions and behaviors provides insight into study design effects on our understanding of HIV risk among ASMM. In AMIS analyses, we defined ASMM as participants aged 15 to 18 years to match YRBS as closely as possible.
Outcome Definitions
Our primary interest was in condom use among sexually active ASMM. Youth Risk Behavior Surveillance System includes 1 condom use question, asked of respondents reporting 1 or more partners in the past 3 months: “The last time you had sexual intercourse, did you or your partner use a condom?” The American Men's Internet Survey measures condom use in several ways; we selected use during receptive or insertive anal sex at last sex with the most recent male partner for comparability with YRBS and to evaluate acts most relevant to HIV transmission. For ASMM reporting 1 or more female partners, we also examined condom use at most recent vaginal or anal sex with a woman.
Statistical Analysis
Youth Risk Behavior Surveillance System: We calculated proportions and 95% confidence intervals (95% CIs) of condom use at last sexual intercourse among ASMM overall and stratified by sex of partners, age, race/ethnicity, and year in YRBS-National and YRBS-Trends. We used separate logistic regression models to examine associations between condom use and year (linear), age group (ordinal), and sex of partners (binary). We compared condom use by race/ethnicity using Rao-Scott design-adjusted χ2 tests. Youth Risk Behavior Surveillance System analyses used survey procedures in SAS v9.4 to account for complex sample design.34s
American Men's Internet Survey: Analytic methods differed from YRBS because AMIS did not involve complex sampling. We calculated proportions and 95% CIs of condom use at last sex with male partners overall and stratified by age, race/ethnicity, and year, and with female partners overall. We used McNemar's test to compare use at last anal sex with most recent male partner and at last vaginal or anal sex with most recent female partner among ASMM who reported both. We used Pearson χ2 tests to compare use at last sex with a male partner by race/ethnicity and Mantel-Haenszel tests for trend to examine temporal trends and ordinal associations by age. American Men's Internet Survey analyses used Stata v15.
Epidemic Modeling
We used results from these analyses to design and parameterize epidemic modeling examining population-level effects of a hypothetical condom intervention on HIV transmission among ASMM. We used a stochastic dynamic network model comprising ASMM aged 13 to 18 years (including adolescents before and after initiation of sex with other men) and adult MSM aged 19 to 39 years (~54,000 men total), detailed elsewhere.35s,36s Features include relationship formation and dissolution, sexual acts, HIV care cascade, adult PrEP use, and intrahost viral dynamics. We used approximate Bayesian computation to estimate values for 3 calibration parameters yielding simulated epidemics matching 2 HIV prevalence targets: 7% among sexually active 18-year-old ASMM37s and 28.3% among adult MSM38s for comparability with previous models examining HIV prevention among ASMM.19–22 The model was implemented using EpiModel.19,39s,40s Specific model features and parameterization for condom use depended on outcomes of the empirical analyses and are described under Results; a preestablished decision rule required disaggregating condom use probabilities in the model for variables significantly predicting condom use in 2 or more of 3 data sets.
A reanalysis (personal communication, Dr. Catherine Rasberry) of a published study11 found that being shown how to use condoms during sex education was associated with a 1.37-fold increase (95% CI, 1.14–1.64; estimated using Poisson regression) in condom use among non-ASMM and no change among ASMM in Florida high schools. Assuming this study observed no effect among ASMM because their experiences were not represented in local sex education curricula and in the absence of school-based interventions with demonstrated effects on ASMM condom use, we conceptualized our hypothetical intervention as a comprehensive, LGBTQ-inclusive sex education curriculum that achieved the same effect among ASMM. We modeled this intervention as a relative change in condom use probabilities based on 5 parameters: coverage, age at intervention, effect size, effect duration, and susceptibility. In the primary analysis, our intervention was delivered to 62% of all ASMM (regardless of sexual debut; equal to the proportion of ASMM shown how to use condoms during sex education in Rasberry et al11) when they turn 14 years old (approximating sex education in 9th grade). Condom use probabilities increased by 37% over baseline levels among intervention recipients. Without data regarding effect duration, we assumed the condom use increase persisted 5 years after intervention initiation to cover the modeled ASMM age range (through 18 years).
To explore potential impact of implementation strategies for condom interventions and address uncertainty in intervention parameters, we modeled 6 sets of scenarios. First, we examined effects of intervention coverage, varied across quartiles from 25% to 100% to reflect differential uptake of comprehensive, inclusive sex education by schools. Second, we tested alternative effect sizes using the lower and upper bounds of the 95% CI from the Raspberry et al11 reanalysis, corresponding with 14% and 64% relative increases in condom use. Third, we evaluated the effect of behavior change persisting 1 to 10 years. Fourth, we hypothesized that susceptibility may depend on whether ASMM have initiated anal sex with other males before receiving the intervention. We operationalized this as all ASMM receiving the intervention having an increased condom use probability, only those who had had anal sex with another male before receiving the intervention (sexually debuted), or only those who had not had anal sex with another male before receiving the intervention. Finally, timing of sex education differs across jurisdictions, with possible benefits to intervening at later ages when more ASMM have begun having sex with other males or when intervention effects cover a period of higher risk. We therefore examined (A) independent effects of implementing an intervention affecting all ASMM at different ages (13–18 years) and (B) joint effects of an intervention affecting only sexually debuted ASMM, varying intervention age from 13 to 18 years and effect duration from 1 to 5 years.
For each scenario, we conducted 100 simulations and calculated means and 95% simulation intervals (SIs, middle 95% of observed values, reflecting the inherent stochasticity inherent in the specified model) for HIV prevalence among 18-year-olds after 10 years as well as number of infections averted per 100,000 person-years at risk and percentage of infections averted (PIA) compared with no intervention over 10 years among ASMM aged 13 to 18 years. All simulations included background PrEP use by adult MSM beginning 3 years before our intervention’s implementation with 20% coverage among those meeting CDC guidelines,41s averaging the 2 most recent National HIV Behavioral Surveillance MSM cycles.42s We assumed no PrEP use among ASMM to evaluate potential independent effects of condom use by ASMM and because PrEP was approved for adolescents in 2018 with limited uptake to date.
RESULTS
Study Population
Among 14,861 men participating in the 2015 and 2017 national YRBS cycles, 12,555 (84%) provided data on sex of partners, of whom 448 (3.6%) reported male partners. Of these ASMM, 200 (45%) were currently sexually active, of whom 193 (97%) responded to questions about condom use and were included in this analysis.
Among 70,637 male participants in the YRBS-Trends data set, 62,537 (89%) provided data on sex of partners, of whom 3118 (5.0%) reported male partners. Of these, 1006 (32%) were currently sexually active, with 953 (95%) responding to condom use questions and included in this analysis.
Among 39,591 MSM participating in AMIS from 2014 to 2017, 2353 (5.9%) were aged 15 to 18 years, of whom 1773 (75%) reported anal sex with men in the last year. Of these, 1528 (86%) reported having anal sex the last time they had sex with their most recent male partner, 1386 (91%) of whom responded to questions about condom use at last sex and were included in this analysis.
Table 1 compares sociodemographics and sexual behaviors among ASMM in our analyses. Notably, ASMM in AMIS were older on average and more likely to report being gay and having exclusively male partners than in either YRBS data set. The YRBS-Trends was the most racially/ethnically diverse with 53% ASMM of color; YRBS-National included fewer Hispanic/Latinx ASMM and AMIS fewer non-Hispanic Black ASMM.
TABLE 1.
Characteristics of Sexually Active Adolescent Sexual Minority Males Participating in the YRBS and AMIS
| YRBS-National | YRBS-Trends* | AMIS | |
|---|---|---|---|
| n, %, or median (IQR) | n, %, or median (IQR) | n, %, or median (IQR) | |
| Total | 193 | 953 | 1386 |
| Year | |||
| 2011 | — | 30% | — |
| 2013 | — | 23% | — |
| 2014 | — | — | 9% |
| 2015 | 53% | 24% | 26% |
| 2016 | — | — | 30% |
| 2017 | 47% | 23% | 36% |
| Age | |||
| ≤12 | 0% | 1% | — |
| 13–15 | 16% | 18% | 6% |
| 16–17 | 63% | 52% | 40% |
| 18 | 21% | 30% | 54% |
| Race/Ethnicity | |||
| Hispanic/Latinx | 13% | 22% | 26% |
| Non-Hispanic Black | 19% | 21% | 5% |
| Non-Hispanic White | 61% | 47% | 58% |
| Other | 8% | 11% | 12% |
| Sexual orientation | |||
| Gay or lesbian | 29% | 25% | 68% |
| Bisexual | 24% | 35% | 23% |
| Heterosexual | 24% | 28% | 1.4% |
| Other sexual identity | — | — | 0.4% |
| Not sure/do not know | 23% | 10% | 0.9% |
| Prefer not to answer/missing | — | — | 6.1% |
| Sex of sex partners | |||
| Male | 39% | 39% | 81% |
| Both | 61% | 61% | 19% |
| Ever tested for HIV | |||
| Yes | 24% | 30% | 36% |
| No | 65% | 56% | 61% |
| Not sure/do not know | 11% | 14% | 1% |
| Prefer not to answer/missing | — | — | 1% |
| Age at first sexual intercourse, sex of partner and act not specified† | 14.2 (12.6–14.9) | 13.9 (12.3–15.4) | — |
| Age at first oral or anal sex with a male partner | — | — | 15 (14–16) |
| Age at first anal sex with a male partner | — | — | 16 (15–17) |
| No. partners, last 3 mo | 1 (1–1.31) | 1 (1–2.87) | — |
| No. oral or anal male sex partners, last 12 months‡ | — | — | 3 (1–5) |
Included only those who reported at least 1 partner in the last 3 months for YRBS or 12 months for AMIS and have condom use data. For YRBS-National and YRBS-Trends, percents are weighted using SAS survey procedures to account for complex sample design.34s
*The majority of the YRBS-Trends sample was from Florida (33%), Illinois (30%), Michigan (20%), and New York City (11%); ≤2.5% each were from Delaware, Hawaii, Rhode Island, and San Diego. YRBS-National and AMIS are both national data sets.
†YRBS assessed age at first sexual intercourse as follows: “How old were you when you had sexual intercourse for the first time?”
‡Missing data for 200 (14%) AMIS respondents.
Condom Use
Table 2 presents condom use at last sex overall and by age, year, and race/ethnicity across data sets. In YRBS, among ASMM in high school with 1 or more sex partners in the past 3 months, 51.8% (95% CI, 41.3–62.3%) and 37.9% (32.7–42.3%) reported using a condom at last sexual intercourse in national and trend data sets, respectively. Use did not differ between ASMM who reported only male partners versus male and female partners in either data set (P > 0.6 for both; results not shown).
TABLE 2.
Condom use At Last Sex* Among Adolescent Sexual Minority Males by Study Year, Age, and Race/Ethnicity
| YRBS-National | YRBS-Trends | AMIS | |
|---|---|---|---|
| Overall | 51.8% (41.3–62.3%) | 37.9% (32.7–42.3%) | 47.3% (44.6–49.9%) |
| Study year | |||
| 2011 | — | 42.4% (35.4–49.4%) | |
| 2013 | — | 34.8% (26.2–43.4%) | — |
| 2014 | — | — | 47.9% (38.7–57.2%) |
| 2015 | 51.6% (38.9–64.3%) | 37.9% (26.1–49.6%) | 49.7% (44.4–55.1%) |
| 2016 | — | — | 49.3% (44.3–54.2%) |
| 2017 | 52.0% (33.7–70.3%) | 36.3% (26.5–46.1%) | 43.7% (39.3–48.2%) |
| P† | 0.971 | 0.368 | 0.126 |
| Age | |||
| ≤ 12 | — | 11.8% (0.0–25.1%) | — |
| 13–15‡ | 35.4% (14.0–56.7%) | 31.8% (21.2–42.4%) | 54.8% (43.5–65.7%) |
| 16–17 | 61.8% (49.2–74.5%) | 37.8% (31.0–44.7%) | 44.8% (40.6–49.0%) |
| 18 | 52.1% (33.0–71.1%) | 46.6% (34.3–58.8%) | 48.3% (44.6–51.9%) |
| P§ | <0.0001 | 0.032 | 0.919 |
| Race/ethnicity | |||
| Hispanic/Latinx | 28.7% (13.8–43.7%) | 32.6% (23.4–41.7%) | 46.2% (41.0–51.5%) |
| Non-Hispanic Black | 69.6% (46.8–92.3%) | 49.6% (35.7–63.5%) | 41.5% (29.4–54.4%) |
| Non-Hispanic White | 53.7% (37.6–69.9%) | 35.6% (27.8–43.4%) | 48.3% (44.8–51.8%) |
| Other | 60.1% (27.2–92.9%) | 45.3% (31.4–59.3%) | 46.6% (38.8–54.6%) |
| P∥ | 0.047 | 0.099 | 0.707 |
For YRBS-National and YRBS-Trends, analyses are weighted using SAS survey procedures to account for complex sample design.34s
*YRBS and AMIS assessed condom use at last sex differently as follows: YRBS assessed condom use at last sexual intercourse among those with ≥1 partner in the last 3 months. It did not define “sexual intercourse” or specify the sex of partner at last sexual intercourse. The denominator included ASMM who reported ever having had sexual intercourse, who separately reported sexual intercourse with ≥1 partner in the past 3 months (“currently sexually active”), and who provided data regarding condom use.12,34s AMIS assessed condom use at last anal sex among those reporting anal sex with their most recent male partner in the last year. The denominator included all ASMM who reported anal sex with men in the past 12 months, who reported anal sex at last sex with their most recent male sex partner, and who provided data about condom use at last anal sex with this partner.
†P values from analyses of linear temporal trends in condom use from logistic regression models in YRBS and Mantel-Haenszel test for trend in AMIS.
‡AMIS only recruited participants ages 15 years and older. As a result, the 13- to 15-year-old category includes only 15–year-old ASMM. In YRBS, 15-year-olds represented 86% and 84% of this category in the National and Trends data sets, respectively.
§P values from analyses of the association between age as an ordinal variable and condom use from logistic regression models in YRBS and Mantel-Haenszel test for trend in AMIS.
∥P values from analyses of the association between race/ethnicity and condom use from Rao-Scott design-adjusted χ2 tests in YRBS and Pearson χ2 test in AMIS.
Among 15- to 18-year-old ASMM reporting anal sex with 1 or more male partners in the last year in AMIS, 47.3% (95% CI, 44.6–49.9%) reported condom use at last anal sex with a male partner. A similar proportion of those in AMIS reporting vaginal or anal sex with 1 or more female partners in the last year reported condom use at last vaginal or anal sex with a female partner (51.4%; 95% CI, 45.1–57.7%). Among those reporting sex with male and female partners, condom use at last sex was similar between partner types (49.7% female, 45.7% male; P = 0.41).
In YRBS-National, condom use varied significantly by age and was highest among 16- to 17-year-olds (61.8%), followed by 18-year-olds (52.1%) and 13- to 15-year-olds (35.4%) (P < 0.0001). In YRBS-Trends, condom use steadily increased across age groups from 11.8% among 12-year-olds and younger to 46.6% among 18-year-olds (P = 0.032). In AMIS, condom use was consistent across age (P = 0.919). No temporal trends were observed overall or within age groups in any data set (P > 0.05 for all).
In both YRBS samples, the frequency of reporting condom use at last sexual intercourse was highest among non-Hispanic Black ASMM, followed by ASMM of “other” racial/ethnic categories, then non-Hispanic White, then Hispanic/Latinx ASMM (Table 2). However, these differences were only significant in YRBS-National, and no differences by race/ethnicity were observed in AMIS.
Population-Level Effects of Changes in Condom Use
Age was significantly associated with condom use in 2 data sets and, therefore, met the criterion for inclusion in the model based on our decision rule. Study year and race/ethnicity did not meet this criterion; thus, condom use remained stable over time and did not differ between racial/ethnic groups in the model. We selected YRBS-Trends as the source of age-specific marginal condom use estimates (13- to 15-year-olds = 31.8%, 16- to 17-year-olds = 37.8%, 18-year-olds = 46.6%), as we considered this data set to represent a good balance between precision and representativeness. We specified age mixing between ASMM and adult MSM using data from a diverse cohort study of Chicago-area ASMM.43s Condom use is a dyadic process between people of potentially different ages. We thus back-calculated the unique set of 1-sided age-specific probabilities that yielded the abovementioned marginal probabilities across modeled partnerships given reported age mixing, assuming that condom use for 2 ASMM reflected the mean of their 1-sided age-specific values and for an ASMM-adult pair reflected the ASMM's age-specific value. These 1-sided values were 13- to 15-year-olds, 28%; 16- to 17-year-olds, 38%; 18-year-olds, 55%.
The simulation of our primary hypothetical intervention, which resulted in a 1.37-fold increase in condom use among 62% of all ASMM beginning at age 14 years and lasting 5 years, averted 9.0% of HIV infections among ASMM over 10 years (PIA; 95% SI, −5.4% to 21.2%) or 60.4 infections per 100,000 person-years at risk (number of infections averted; 95% SI, −32.5 to 149.2). After 10 years, HIV prevalence among 18-year-olds was 4.0% (95% SI, 3.0%–5.0%) with the intervention compared with 4.7% (3.7%–5.8%) without, a 14% difference (Fig. 1).
Figure 1.
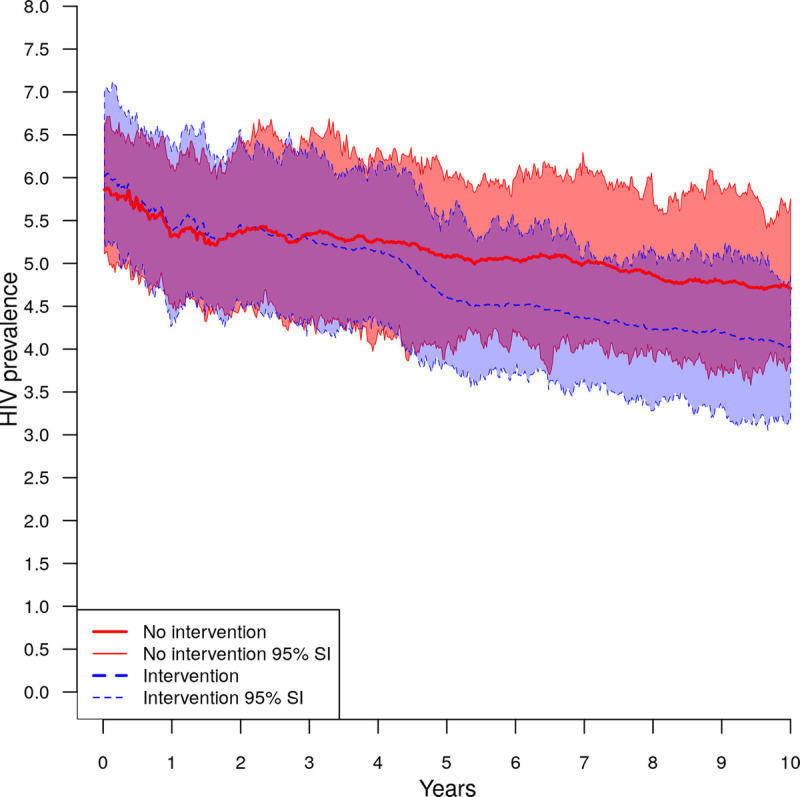
Effect of hypothetical condom use intervention on HIV prevalence among 18-year-old ASMM compared with no intervention.
Supplemental Digital Content 2 (http://links.lww.com/OLQ/A687) presents complete results for other scenarios. In summary, the PIA increased linearly as intervention coverage increased from 3.7% (95% SI, −11.9% to 18.5%) at 25% coverage to 13.5% (0.9%–25.9%) at 100% coverage, representing a PIA of approximately 1.4% for every 10% increase in intervention coverage. Varying effect size also resulted in an approximately linear increase in PIA from 5.7% (−9.7% to 21.0%) with a 1.14-fold increase in condom use to 11.6% (−0.2% to 25.4%) with a 1.64-fold increase. By contrast, changing the duration of intervention effect resulted in a rapid and roughly linear rise in PIA from 1.2% (−13.8% to 15.0%) at 1 year to 9.0% (−5.4% to 21.2%) at 5 years, at which point additional increases in duration effect up to 10 years did not affect PIAs (Fig. 2). Fourth, when varying age at intervention delivery, the PIA increased from 7.5% when implementing at age 13 years to 9.1–9.7% at ages 14 to 16 years, then decreased at older ages to a low of 6.1% at 18 years (Fig. 2). Fifth, the PIA was 4.4% (95% SI, −12.2% to 18.5%) if the intervention was only effective among sexually debuted ASMM and 8.0% (−2.3% to 18.3%) when effective only among ASMM before sexual debut, compared with 9.0% (−5.4% to 21.2%) when effective among all ASMM. Finally, we examined the effects of varying both age at intervention implementation and duration of behavior change when only sexually debuted ASMM were affected by the intervention (Fig. 3). Implementation at age 17 years yielded the highest PIA (range, 3.9%–7.1%) at all effect durations except 4 years, followed by implementation at age 16 years. The intervention had little impact on PIAs when its effect duration was short and it was implemented at younger ages.
Figure 2.
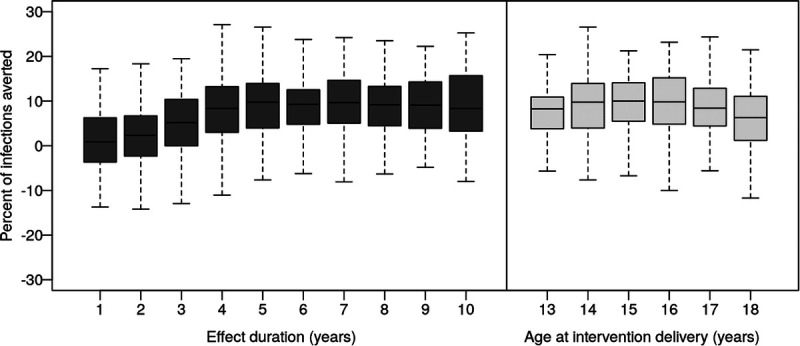
Percent of HIV infections averted among ASMM by hypothetical condom use intervention, independently varying effect duration and age at delivery.
Figure 3.
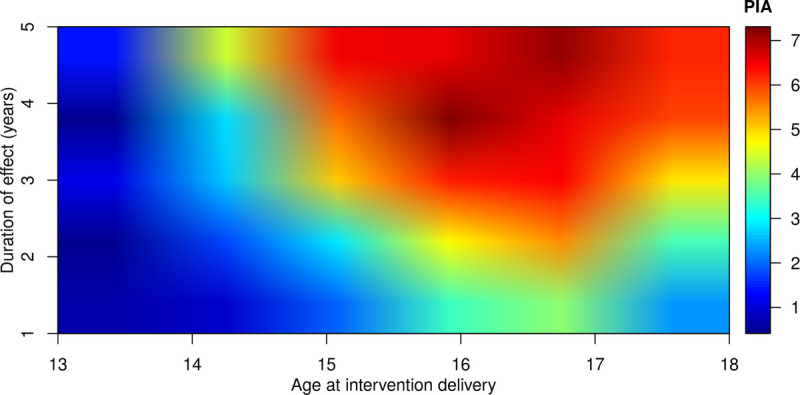
PIA among ASMM by hypothetical condom use intervention affecting only ASMM who had had anal sex before the intervention, varying effect duration and age at delivery.
DISCUSSION
Across 3 U.S. samples, we found that 38% to 52% of sexually active ASMM reported using condoms at last sex and that these percentages remained stable from 2011 to 2017. We observed inconsistent patterns in condom use across age groups and race/ethnicity, with some indication that use may be higher among 16- to 17-year-olds than 13- to 15-year-olds and that Black ASMM, despite or as a result of having the highest HIV prevalence,1 may have the highest use. Our model suggests that increases in condom use consistent with previous interventions have potential to avert 1 in 11 new HIV infections among ASMM and that timing condom use interventions correctly and achieving sustained effects will be critical to their success.
Overall estimates of condom use at last sex among sexually active ASMM were relatively similar across data sets and sex of partners, ranging from 38% in YRBS-Trends to 52% in YRBS-National, and consistent with other studies among ASMM.8–12 Differences in populations and local condom and sex education policies and programs in jurisdictions included in YRBS-Trends versus the rest of the United States may have contributed to disparities between YRBS estimates. However, despite differences in populations, sampling strategies, and outcome measurement between YRBS and AMIS, national estimates from the 2 studies were similar (51.8% vs 47.3%). Indeed, estimates from all 3 data sets converged at age 18 years, when we would expect school-based versus online sampling and differences in definitions of sex to have the least impact as the proportion of ASMM online and who have had anal sex with other males increases with age. Combined with our finding that condom use did not differ by sex of partners, this suggests that not specifying type of sex and partner sex may not significantly affect ASMM condom use estimates from YRBS.
Although ASMM reported lower condom use than adult MSM16 and other adolescents,12 it is encouraging that we did not observe declines in condom use as has been noted in these other populations.15,16 Another study of ASMM in YRBS observed a decline in condom use from 2005 to 2015,9 but men who have sex with both men and women, who represent a majority of ASMM in YRBS,14 were excluded; included jurisdictions varied by year such that differences in underlying populations may have contributed to observed trends; and the decrease occurred primarily from 2005 to 2007.
Our epidemic model demonstrated that increases in condom use by ASMM consistent with those observed from an intervention among non-ASMM adolescents could avert up to 13.5% of HIV infections among ASMM over 10 years. Results varied by intervention coverage, effect size and duration, age at delivery, and susceptibility. Universal coverage resulted in the highest population-level effect across all analyses, suggesting the importance of promoting access to effective, inclusive sex education nationally. Varying effect duration, age at delivery, and susceptibility illustrated that timing interventions correctly and implementing interventions with sustained effects is critical. Interventions must be effective during later adolescence when ASMM experience the greatest HIV risk due to increasing sexual activity23 and mixing with adult MSM,44s but implementing too late misses opportunities to prevent a substantial proportion of infections or may result in lower intervention effect if ASMM establish condom use norms at first anal sex. Depending on effect duration and susceptibility, intervening between ages 14 and 17 years may be most effective. Most U.S. school districts require relatively few instructional hours for sex education,45s which may limit the size and duration of its effects on condom use46s,47s and, especially when delivered in middle school or early high school, its potential impact on HIV incidence. Routinely providing inclusive, evidence-based sex education or other condom interventions in sequenced and repeated doses across grade levels may ensure sustained effects and address uncertainty regarding the best time for intervention delivery. For similar reasons, implementing the intervention at age 14 years in our primary analysis delayed the impact on HIV prevalence until at least year 3, limiting the potential PIA over 10 years.
The study has limitations. Condom use measures in our empirical analyses relied on self-report and were therefore subject to recall error and social desirability bias. Measuring condom use at last sex may reduce recall error but may not reflect use over longer periods or across partner types and contexts.48s In YRBS-National, ASMM were few and only identifiable from 2015–2017, the jurisdictions in YRBS-Trends are not nationally representative, and AMIS’ representativeness is unknown. In addition, we modeled condom use as homogeneous within age group, relied on YRBS-Trends, and used adolescents' condom probabilities for partnerships with adult MSM. The model does not include potential transmission from female partners despite many ASMM reporting sex with males and females. However, because HIV prevalence is low among female adolescents in the United States,1 this is unlikely to influence transmission significantly. We modeled condom use effects in isolation despite many interventions to increase condom use, such as sex education, also aiming to affect other behaviors impacting HIV transmission, for example, delaying sexual debut or increasing PrEP use. The 95% SIs for PIAs are wide, in part, due to the relatively small number of 13- to 18-year-olds in the model. In addition, our HIV prevalence targets were selected for comparability against previous models in this population and come from prospective studies in Atlanta; they may, therefore, overestimate HIV transmission among ASMM in the United States. Finally, when available, school-based condom interventions for ASMM may differ in effectiveness and implementation from our hypothesized intervention. Research is needed to identify effective, scaleable interventions for ASMM.
Increasing condom use could reduce HIV burden among ASMM and, unlike HIV-specific interventions like PrEP, impact other sexually transmitted infections with major adolescent burdens and prevent pregnancies among female partners. Characterizing effect size and duration, potential reach, and costs of condom interventions can inform effective implementation. While considerable work has explored these domains for heterosexual adolescents,49s ASMM have not received similar attention, despite greater HIV incidence and many existing sexual health curricula not addressing their needs. Research is needed to identify the most effective, efficient strategies for improving condom use among ASMM and explore the relative effectiveness of implementing condom and other behavioral interventions independently and in combination on the HIV epidemic in this population.
Supplementary Material
For further references, please see “Supplemental References,” http://links.lww.com/OLQ/A686.
Footnotes
Conflict of Interest: None declared.
Sources of Funding: Supported by the Centers for Disease Control and Prevention (U38 PS004646) and received additional support from the Center for Studies in Demography and Ecology (NIH R24 HD042828) at the University of Washington and the Centers for AIDS Research at the University of Washington/Fred Hutch (NIH P30 AI027757) and Emory University (NIH P30 AI050409).
Disclaimer: The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the U.S. Centers for Disease Control and Prevention.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (http://www.stdjournal.com).
Contributor Information
Deven T. Hamilton, Email: dth2@uw.edu.
Elizabeth M. Rosenthal, Email: emrosenthal@albany.edu.
Li Yan Wang, Email: lgw0@cdc.gov.
Richard L. Dunville, Email: dgo2@cdc.gov.
Maria Aslam, Email: lfx0@cdc.gov.
Lisa C. Barrios, Email: lic8@cdc.gov.
Maria Zlotorzynska, Email: maria.zlotorzynska@emory.edu.
Travis H. Sanchez, Email: travis.sanchez@emory.edu.
Patrick S. Sullivan, Email: pssulli@emory.edu.
Eli S. Rosenberg, Email: erosenberg2@albany.edu.
Steven M. Goodreau, Email: goodreau@uw.edu.
REFERENCES
- 1.Centers for Disease Control and Prevention . Diagnoses of HIV infection among adolescents and young adults in the United States and 6 dependent areas, 2012–2017. HIV Surveillance Supplemental Report 2019; 24. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-24-5.pdf. Accessed February 8, 2021. [Google Scholar]
- 2.Garofalo R Hotton AL Kuhns LM, et al. Incidence of HIV infection and sexually transmitted infections and related risk factors among very young men who have sex with men. J Acquir Immune Defic Syndr 2016; 72:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hosek SG Landovitz RJ Kapogiannis B, et al. Safety and feasibility of antiretroviral preexposure prophylaxis for adolescent men who have sex with men aged 15 to 17 years in the United States. JAMA Pediatr 2017; 171:1063–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balaji AB An Q Smith JC, et al. High human immunodeficiency virus incidence and prevalence and associated factors among adolescent sexual minority males—3 cities, 2015. Clin Infect Dis 2018; 66:936–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith DK Herbst JH Zhang X, et al. Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. J Acquir Immune Defic Syndr 2015; 68:337–344. [DOI] [PubMed] [Google Scholar]
- 6.Giannou FK Tsiara CG Nikolopoulos GK, et al. Condom effectiveness in reducing heterosexual HIV transmission: A systematic review and meta-analysis of studies on HIV serodiscordant couples. Expert Rev Pharmacoecon Outcomes Res 2016; 16:489–499. [DOI] [PubMed] [Google Scholar]
- 7.Johnson WD, O'Leary A, Flores SA. Per-partner condom effectiveness against HIV for men who have sex with men. AIDS 2018; 32:1499–1505. [DOI] [PubMed] [Google Scholar]
- 8.Valencia R Wang LY Dunville R, et al. Sexual risk behaviors in adolescent sexual minority males: A systematic review and meta-analysis. J Prim Prev 2018; 39:619–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Phillips G Kalmin MM Turner B, et al. Condom and substance use at last sex: Differences between MSMO and MSWO high school youth. Int J Environ Res Public Health 2018; 15:995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raifman J, Beyrer C, Arrington-Sanders R. HIV education and sexual risk behaviors among young men who have sex with men. LGBT Health 2018; 5:131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rasberry CN Condron DS Lesesne CA, et al. Associations between sexual risk-related behaviors and school-based education on HIV and condom use for adolescent sexual minority males and their non-sexual-minority peers. LGBT Health 2018; 5:69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rasberry CN Lowry R Johns M, et al. Sexual risk behavior differences among sexual minority high school students—United States, 2015 and 2017. MMWR Morb Mortal Wkly Rep 2018; 67:1007–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thoma BC, Huebner DM. Parent-adolescent communication about sex and condom use among young men who have sex with men: An examination of the theory of planned behavior. Ann Behav Med 2018; 52:973–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kann L McManus T Harris WA, et al. Youth risk behavior surveillance—United States, 2017. MMWR Surveill Summ 2018; 67:1–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention . Youth risk behavior survey data summary & trends report 2007–2017. Available at: http://cdc.gov/healthyyouth/data/yrbs/pdf/trendsreport.pdf. Accessed February 8, 2021.
- 16.Paz-Bailey G Mendoza MC Finlayson T, et al. Trends in condom use among MSM in the United States: The role of antiretroviral therapy and seroadaptive strategies. AIDS 2016; 30:1985–1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen MS Chen YQ McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365:493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grant RM Lama JR Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med 2010; 363:2587–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goodreau SM Hamilton DT Jenness SM, et al. Targeting human immunodeficiency virus pre-exposure prophylaxis to adolescent sexual minority males in higher prevalence areas of the United States: A modeling study. J Adolesc Health 2018; 62:311–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamilton DT Goodreau SM Jenness SM, et al. Potential impact of HIV preexposure prophylaxis among black and white adolescent sexual minority males. Am J Public Health 2018; 108(S4):S284–S291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamilton DT Rosenberg ES Jenness SM, et al. Modeling the joint effects of adolescent and adult PrEP for sexual minority males in the United States. PLoS One 2019; 14:e0217315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang LY Hamilton DT Rosenberg ES, et al. Cost-effectiveness of pre-exposure prophylaxis among adolescent sexual minority males. J Adolesc Health 2000; 66:100–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma A Wang LY Dunville R, et al. HIV and sexually transmitted disease testing behavior among adolescent sexual minority males: Analysis of pooled youth risk behavior survey data, 2005–2013. LGBT Health 2017; 4:130–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stein R Shapatava E Williams W, et al. Reduced sexual risk behaviors among young men of color who have sex with men: Findings from the Community-Based Organization Behavioral Outcomes of Many Men, Many Voices (CBOP-3MV) Project. Prev Sci 2015; 16:1147–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mustanski B Greene GJ Ryan D, et al. Feasibility, acceptability, and initial efficacy of an online sexual health promotion program for LGBT youth: The Queer Sex Ed intervention. J Sex Res 2015; 52:220–230. [DOI] [PubMed] [Google Scholar]
- 26.Mustanski B Parsons JT Sullivan PS, et al. Biomedical and Behavioral Outcomes of Keep It Up!: An eHealth HIV Prevention Program RCT. Am J Prev Med 2018; 55:151–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ybarra ML Liu W Prescott TL, et al. The effect of a text messaging based HIV prevention program on sexual minority male youths: A national evaluation of information, motivation and behavioral skills in a randomized controlled trial of Guy2Guy. AIDS Behav 2018; 22:3335–3344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hergenrather KC Emmanuel D Durant S, et al. Enhancing HIV prevention among young men who have sex with men: A systematic review of HIV behavioral interventions for young gay and bisexual men. AIDS Educ Prev 2016; 28:252–271. [DOI] [PubMed] [Google Scholar]
- 29.Patton GC Sawyer SM Santelli JS, et al. Our future: A Lancet commission on adolescent health and wellbeing. Lancet 2016; 387:2423–2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention . Youth Risk Behavior Surveillance System (YRBSS). Available at: https://www.cdc.gov/healthyyouth/data/yrbs/index.htm. Accessed February 8, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


