Abstract
The human cytochrome P450 (CYP) CYP3A4 and CYP3A5 enzymes metabolize more than half of marketed drugs. They share high structural and substrate similarity and are often studied together as CYP3A4/5. However, CYP3A5 preferentially metabolizes several clinically prescribed drugs, such as tacrolimus. Genetic polymorphisms in CYP3A5 makes race-based dosing adjustment of tacrolimus necessary to minimize acute rejection after organ transplantation. Moreover, the differential tissue distribution and expression levels of CYP3A4 and CYP3A5 can aggravate toxicity during treatment. Therefore, selective inhibitors of CYP3A5 are needed to distinguish the role of CYP3A5 from that of CYP3A4 and serve as starting points for potential therapeutic development. To this end, we report the crystal structure of CYP3A5 in complex with a previously reported selective inhibitor, clobetasol propionate (CBZ). This is the first CYP3A5 structure with a type I inhibitor, and along with the previously reported substrate free and type II inhibitor-bound structures, constitute the main CYP3A5 structural modalities. Supported by structure-guided mutagenesis analyses, the CYP3A5-CBZ structure showed that a unique conformation of the F–F′ loop in CYP3A5 enables selective binding of CBZ to CYP3A5. Several polar interactions, including hydrogen bonds, stabilize the position of CBZ to interact with this unique F–F′ loop conformation. Additionally, functional and biophysical assays using CBZ analogs highlight the importance of heme-adjacent moieties for selective CYP3A5 inhibition. Our findings can be used to guide further development of more potent and selective CYP3A5 inhibitors.
Graphical Abstract
INTRODUCTION
The human cytochrome P450 (CYP) superfamily consists of heme-containing enzymes that are responsible for the clearance of various pharmaceuticals and other xenobiotics in the liver. These enzymes catalyze the conversion of lipophilic substrates into hydrophilic intermediates through oxidation or hydroxylation.1 CYP enzymes are estimated to be responsible for metabolizing approximately three-quarters of marketed drugs, and the CYP3A family alone metabolizes half of those drugs.2–3 Because modulation of CYP enzymes may cause clinically significant drug-drug interactions, evaluating drug candidates and new drugs for their potential interactions with CYP, especially CYP3A enzymes, has become an integral component of the drug development process and regulatory agency guidelines.4–5 Approximately 65% of drugs approved by the United States Food and Drug Administration from 2013 to 2017 are CYP3A substrates.5 Therefore, CYP3A enzymes have been the focus of studies related to drug metabolism and drug-induced liver injury.6–8
The CYP3A family consists of four members, CYP3A4, CYP3A5, CYP3A7, and CYP3A43, although only CYP3A4 and CYP3A5 are abundantly expressed in adults.1 CYP3A4 is the most abundantly expressed CYP, accounting for up to 40% of the total CYP in adult human liver and small intestine. Compared to CYP3A4, CYP3A5 is expressed at a much lower level in the liver, but it is the major CYP3A enzyme in the kidney.4, 9 These two enzymes are often grouped together as CYP3A4/5 because they share similar substrates and inhibitors, and many metabolism-related studies do not differentiate between the two.10–13 CYP3A4 plays a more predominant role in drug metabolism; therefore, it is the primary target of research studies and is generally regarded as the representative member of the family. Nevertheless, CYP3A5 exhibits preferential metabolism over CYP3A4 of several clinically relevant drugs, such as tacrolimus, vincristine, and maraviroc.14–16 Kinetics studies showed that CYP3A5 clears tacrolimus twice as fast as does CYP3A4,17 and patients expressing functional CYP3A5 protein require higher tacrolimus dosages to maintain immunosuppression after organ transplantation.18 These discoveries indicate that CYP3A5 also plays an important and unique role in drug metabolism and related diseases, but the lack of a CYP3A5 selective inhibitor has limited further investigation. Apart from its selective metabolism, CYP3A5 differs from CYP3A4 in its frequency of protein expression. Although functional CYP3A4 is expressed in most of the population,19 the CYP3A5*1 allele expressing functional CYP3A5 is found in 85%–91% of Blacks, 40%–68% of Indians, 53% of Chinese, and only 14%–18% of European decent populations.18 The remainder of the population lacking the CYP3A5*1 allele either exhibits no protein expression or expresses a nonfunctional CYP3A5 protein. Moreover, approximately 40% of Blacks exhibit strong functional CYP3A5 protein expression, carrying two CYP3A5*1 alleles. In contrast, the frequency of having two CYP3A5*1 alleles in people of European descent is merely 1%.15 The numerous genetic polymorphisms in CYP3A5 add complexity to adjusting the dosage for CYP3A5-metabolized drugs because patient genotypes further affect individualization of drug dosages. Therefore, the development of a potent inhibitor that selectively targets CYP3A5 will not only help elucidate the role CYP3A5 plays in metabolism and disease but also benefit patients in clinical practice by increasing the efficacy and decreasing the toxicity of certain drugs. Because of the predominant and essential role CYP3A4 plays in hepatic drug metabolism, a CYP3A5 inhibitor that does not inhibit CYP3A4 will prevent drug-drug interactions caused by inhibition of CYP3A4.
Identifying a CYP3A5 selective inhibitor is challenging in part because of the high sequence identity (83%) and structural similarity between CYP3A4 and CYP3A5.20–21 In addition, both enzymes possess a large (≥ 1400 Å) and promiscuous binding pocket that can accommodate structurally diverse compounds.22–24 For example, inhibition by ritonavir is nonselective, as the flexible binding pockets in CYP3A4 and CYP3A5 can adapt to the shape of the inhibitor.25–26 Although several CYP3A5 selective substrates have been reported,15, 27–29 selective inhibitors of CYP3A5 were lacking. Nonetheless, our lab recently identified clobetasol propionate (CBZ) as a selective inhibitor of CYP3A5 which strongly inhibited CYP3A5 with sub-micromolar potency while showing little inhibition of CYP3A4.30 Based on biophysical measurements, we concluded that CBZ binds to CYP3A5 in a position close to the heme which displaces the axial water molecule without coordinating to the heme iron, while CBZ was not observed to perturb the axial water molecule in CYP3A4.30 However, the detailed structural mechanism of selective inhibition remains unclear largely because of a lack of a CYP3A5–CBZ complex crystal structure.
In this study, we investigated the structural basis of CYP3A5 selective inhibition by CBZ by using combined structural and functional analyses. We solved the CYP3A5–CBZ crystal structure and found that key polar interactions orient CBZ for optimal binding to a unique conformation of the F–F′ loop in CYP3A5. Functional studies using mutagenesis and CBZ analogs supported this finding and further demonstrated that the propionate and 2-chloroacetyl groups on CBZ play an important role in CYP3A5 inhibition and most likely its selectivity. Our results form the basis for understanding the selective targeting of CYP3A5 and serve as guidelines for developing new and improved CYP3A5 selective inhibitors which can be used to further explore the therapeutic potential of targeting CYP3A5.
RESULTS
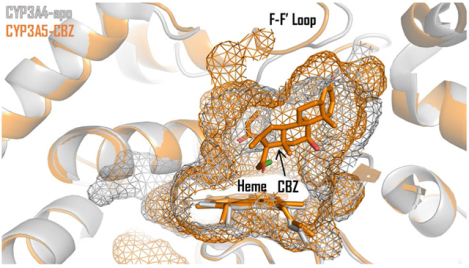
The Crystal Structure of CYP3A5–CBZ Reveals a New Binding Pose for CBZ.
To better understand the selective inhibition of CYP3A5 by CBZ, we solved the crystal structure of the CBZ-bound CYP3A5 complex to a resolution of 2.65 Å by using a truncated CYP3A5 as previously described (Figure 1a, Table S1).24, 26 In the crystal structure, the 2-chloroacetyl group of CBZ resides ~4 Å away from the heme iron and displaced the axial water molecule without coordinating to the heme iron (Figure 1b). This is evidenced by the lack of density for the axial water molecule near the heme group (Figure S1), which is in agreement with the reported biophysical data for a type I inhibitor.30
Figure 1.

Clobetasol propionate (CBZ) binds in the ligand-binding pocket of CYP3A5. (a) Crystal structure model of the CYP3A5–CBZ complex, highlighting its key structural features. (b) The binding pocket of CYP3A5 around CBZ. All side chains for residues within 5 Å of CBZ are shown as cyan sticks. Insert depicts the chemical structure of CBZ. (c) Key polar interactions, represented by dashed lines, occur between CBZ and the backbone amine groups of A305 and G480 and the backbone carbonyl groups of A370 and R372. These residues are shown as cyan sticks. For all panels CBZ is shown in yellow and the heme is shown in black.
CBZ bound to CYP3A5 through hydrophobic contacts and polar interactions. In the CYP3A5–CBZ crystal structure, CBZ formed hydrophobic contacts with residues on helix I, the F–F′ loop, the C-terminal loop, and the loop between helix K and β sheet 1–4, which together restricted movement of CBZ within the pocket (Figure 1b, Figure S2). Notably, CBZ may be further stabilized through its propionate group near the heme because it is sandwiched inside a hydrophobic pocket consisting of residues F213, F304, T309, and L481. Apart from these hydrophobic contacts, CBZ also established multiple polar interactions with CYP3A5, including a hydrogen bond between the hydroxyl group on the CBZ backbone and the backbone carbonyl of residue A370 (3.2 Å between heavy atoms) (Figure 1c). This hydroxyl group could also potentially form a hydrogen bond in solution with the backbone carbonyl of R372 (3.4 Å). Additionally, the carbonyl head group of CBZ was 3.6 Å from the backbone amine group of G480 on the C-terminal loop, which is a distance that is in proximity to form a hydrogen bond in solution. On the opposite end of CBZ, the propionate carbonyl formed a 3.9 Å weak polar interaction with the backbone amine group of residue A305 on helix I. However, this weak polar interaction between CBZ and A305 was limited by steric hindrance from the neighboring F304 (Figure 1c).
The CYP3A5–CBZ Complex Reveals a Novel F–F′ Loop Conformation.
Although most CYPs contain a continuous helix F and helix G forming the top of the ligand-binding pocket, both CYP3A4 and CYP3A5 contain an intervening F–F′ loop (residues 211–218 in the CYP3A5–CBZ structure) and G–G′ loop (residues 236–243 in the CYP3A5–CBZ structure) flanked by helices F and F′, or helices G and G′, respectively (Figure 1a). These flexible loops contribute to the broad substrate profiles of CYP3A4/5 because they can move to accommodate structurally diverse substrates. In the CBZ-bound CYP3A5 complex, the F–F′ loop adopted a novel conformation in which residues F213, F215, F220, and F304 lined up to form a phenylalanine surface that provided a large portion of the hydrophobic environment for CBZ binding (Figure 2a). This particular alignment, or surface, of the phenylalanine residues did not occur in either the ritonavir-bound (Protein Data Bank [PDB]: 5VEU) or glycerol-bound/substrate-free (PDB: 6MJM) CYP3A5 crystal structures (Figure 2b).24, 26 In the ritonavir-bound CYP3A5 structure, ritonavir binding altered the phenylalanine alignment by pushing the F–F′ loop, which includes F213, away from the heme to make room for ritonavir to bind.26 In the glycerol-bound CYP3A5 structure, the F–F′ loop was also positioned further away from the heme with F215 being flipped away from the ligand binding pocket, and F220 was located in a different position from the CBZ-bound CYP3A5 structure.24 In the CBZ-bound CYP3A5 structure, additional hydrophobic interactions between F304 and its neighboring residues, F210 and F213 (4.9 and 5.1 Å between ring centers, respectively), help stabilize the position of the F–F′ loop closer to the heme (Figure 2b).
Figure 2.

The F–F′ loop in the CYP3A5–CBZ crystal structure adopts a novel conformation. (a) The F–F′ loop (residues 211–218) adopts a different conformation in the CBZ-bound CYP3A5 structure (blue) than that in the ritonavir-bound (PDB: 5VEU, green) and glycerol-bound (PDB: 6MJM, yellow) CYP3A5 structures. The entire monomer was used to align the three structures. (b) The F–F′ loop (cyan) adopts a conformation that places F213 and G214 (orange) near CBZ (yellow). This conformation is potentially stabilized in solution by hydrophobic interactions between F210, F213, F215, F220, and F304. (c) The F–F′ loop conformation in the CYP3A5–CBZ complex is not present in CYP3A4 crystal structures. Alignment of the F–F′ loop (residues 211–218) of the CYP3A5-CBZ complex (cyan) with residues 211–218 of all 77 CYP3A4 crystal structures (white) published to date shows that the F–F′ loop conformation in the CYP3A5–CBZ complex is unique. Additionally, D214 of CYP3A4 is not specifically directed toward the ligand-binding pocket. The entire monomer was used to create the alignment. (d) Replacing G214 with D214 (orange) in CYP3A5 prevents the F–F′ loop from forming the conformation found in the CYP3A5–CBZ crystal structure. D214 rotamers 1 and 3 would sterically clash with F213, whereas rotamer 2 would protrude into the hydrophobic pocket. Surface shown for residues F213, G214, F215, and F220.
The Unique F–F′ Loop Conformation in the CYP3A5–CBZ Structure Accounts for the Selectivity of CBZ for CYP3A5.
We compared the amino acid sequence of CYP3A4 to that of CYP3A5 (Figure S2) and the CYP3A5–CBZ structure to all 77 published CYP3A4 crystal structures (Figure 2c). Our analysis suggests that CYP3A4 cannot adopt the same F–F′ loop conformation as that of the CYP3A5–CBZ structure, regardless of ligand binding. Several factors contributed to the inability of CYP3A4 to adopt the unique F–F′ conformation of CYP3A5–CBZ, with the most important being the G214 (CYP3A5) to D214 (CYP3A4) amino acid sequence variant. The glycine residue (G214) in CYP3A5 provided room for CBZ to bind near the surface formed by the F–F′ loop, whereas the presence of an aspartic acid (D214) in CYP3A4 prevented the F–F′ loop from adopting the same conformation because its common rotamers either sterically clashed with F213 or interrupted the hydrophobic surface of the pocket (Figure 2d). Furthermore, the unique F–F′ loop conformation in the CYP3A5–CBZ structure is not present in any published CYP3A4 crystal structures (Figure 2c). D214 in CYP3A4 may also impede the potential hydrogen bond between CBZ and residue G481 (G480 in CYP3A5). In addition, CYP3A4 residue L210, unlike F210 in CYP3A5, could not form π electron interactions with F213, F215, F220, and F304 that stabilizes the conformation of the F–F′ loop.
In addition to limitations on the F–F′ loop, CBZ binding to CYP3A4 in the observed CYP3A5 orientation would be hindered by two other amino acid sequence variations. Residues F57 and M371 in CYP3A4, which are slightly larger than their equivalent residues L57 and I371 in CYP3A5 (Figure 1b), would sterically clash with CBZ if bound in the CYP3A5 position. However, the steric hinderance likely plays a minor role in the selective inhibition as CBZ could move slightly to accommodate the two longer residues.
Together, these observations indicate that the F–F′ loop in CYP3A4 must be in a different conformation to accommodate CBZ binding, and likewise CBZ will adopt a different orientation to fit its binding pocket, which would be less favorable than CBZ binding in CYP3A5. Therefore, the unique F–F′ loop conformation in CYP3A5–CBZ most likely explains the selective inhibition of CYP3A5 by CBZ.
Mutagenesis Studies Support the Critical Role of the Unique F–F′ Loop in Selective CYP3A5 Inhibition by CBZ.
To test whether the F–F′ loop conformation in CYP3A5–CBZ and the predicted inability of CYP3A4 to adopt the same conformation contributes to the selective inhibition of CYP3A5 by CBZ, we performed mutagenesis analyses in CYP3A5 by mutating the key F–F′ loop residue G214 and its neighboring C-terminal loop residue G480. Other residues in the F–F′ loop are either conserved between CYP3A4 and CYP3A5 or are highly similar (K212 in CYP3A5 vs R212 in CYP3A4) (Figure S2). We hypothesized that side chain additions to these key residues, such as G214D or G480L, would cause steric hindrance between the F–F′ loop and CBZ or the C-terminal loop, thereby altering the favorable F–F′ loop conformation and weakening CYP3A5 inhibition by CBZ. We also mutated D214 in CYP3A4 to test whether a D214G substitution would no longer restrict the F–F′ loop from adopting the conformation in CYP3A5, thereby enhancing CYP3A4 inhibition by CBZ.
The effects of amino acid substitutions in CYP3A5 and CYP3A4 on the inhibitory potency of CBZ were determined using a luminescence-based P450-Glo assay (Table S2).31 293T/17 cells were chosen to express the mutant proteins as these cells showed no endogenous CYP3A activity in our control experiment (Figure S3). All mutants remained active except for CYP3A5G214P, and they were inhibited by ketoconazole and ritonavir to the levels of the corresponding wild-type (WT) proteins, indicating that these amino acid substitutions did not alter protein folding (Figures S3 and S4).
Consistent with our hypothesis, changing G214 to D in CYP3A5 (CYP3A5G214D) to mimic the CYP3A4 sequence (D214 in CYP3A4) reduced the inhibitory effect of CBZ on CYP3A5 the most among all substitutions tested. Its dose-response curve shifted dramatically to the right as compared to that of CYP3A5WT (IC50 = 0.30 ± 0.04 μM). CBZ only inhibited CYP3A5G214D activity by 49% at the maximum inhibitor concentration tested (60 μM), indicating that the G214D mutation in CYP3A5 weakened the inhibitory potency of CBZ by at least 200-fold (Figure 3a, Table S2). The G214A substitution in CYP3A5 generated an approximately 50-fold reduction in the potency of CBZ (IC50 value of 0.30 and 16 μM for WT and G214A, respectively) due only to the addition of a methyl group. Importantly, neither G214D nor G214A affected the inhibition of CYP3A5 by ketoconazole or ritonavir (Figure S4), highlighting the unique role of G214 in the CYP3A5 selectivity of CBZ. We also tested whether a G214P substitution in CYP3A5, which was predicted to directly alter the F–F′ loop conformation, would generate an effect similar to that of G214D, but the activity of the CYP3A5G214P mutant was too low to determine its IC50 value accurately (Figure S3). Nevertheless, these results demonstrate that the glycine residue at position 214 is crucial for CBZ to potently inhibit CYP3A5 and support our hypothesis that CYP3A4 cannot adopt the same favorable F–F′ loop conformation because of its aspartic acid in the same position.
Figure 3.

Residues G214 and G480 play important roles in CBZ-mediated CYP3A5 inhibition. (a, b) Dose-response curves showing CBZ-mediated inhibition of CYP3A5 or CYP3A4 mutants determined by the cell-based P450-Glo assay. The percentage inhibition data for each mutant were normalized against their own DMSO controls as 0% inhibition and media-only controls as 100% inhibition. The IC50 values reported are the means and standard deviations of triplicate experiments. For weak inhibition in which an IC50 value could not be determined, the IC50 is reported as “>60 μM” (the highest compound concentration tested).
Mutagenesis studies with G480 also supported the importance of the F–F′ loop conformation in CBZ-mediated CYP3A5 inhibition. Substituting the glycine with bulkier residues at position 480 on the C-terminal loop, which were expected to displace the adjacent F–F′ loop (Figure 2b), reduced the potency of CBZ by at least 20-fold (IC50 value of 0.30, 9 and 8 μM for WT, G480L and G480S, respectively) (Figure 3a, Table S2). The only exception was CYP3A5G480A, which was inhibited by CBZ to the same extent as was CYP3A5WT. This most likely occurred because the alanine side chain was too short to perturb the F–F′ loop that was ~5 Å away. The G480S and G480L substitutions also likely impeded the formation of the hydrogen bond between CBZ and G480 (Figure 1c). However, the magnitude of inhibition loss is greater than what would be expected from the loss of the hydrogen bond alone. Large substitutions at position 214 would likely have a similar effect.
In addition to single amino acid changes, we also explored the combined effect of substituting both G214 and G480 in CYP3A5. The inhibitory potency of CBZ was reduced in CYP3A5G214A but not in CYP3A5G480A. To our surprise, the double mutant CYP3A5G214A/G480A was not only uninhibited by CBZ at low concentrations but also weakly activated by 0.08–20 μM CBZ (Figure 3a). Control experiments using ketoconazole and ritonavir revealed that the double mutant was inhibited to the same extent as CYP3A5WT, indicating the unexpected CYP3A5G214A/G480A activation was specific to CBZ (Figure S4). This suggests that CBZ adopts a new binding position in CYP3A5G214A/G480A to allow the substrate to retain access to the heme group, while CBZ prevents substrate binding to the active site in CYP3A5WT. Although the exact reason for the observed activating effect is unknown, these results further support the critical role of both G214 and G480 in CBZ-mediated CYP3A5 inhibition.
Finally, we tested whether the reciprocal substitution of D214G in CYP3A4 would allow the F–F′ loop to adopt a conformation that is more favorable for CBZ binding and inhibition. CBZ inhibited CYP3A4D214G and CYP3A4WT identically (Figure 3b, Table S2), suggesting that D214 does not play a major role in CBZ binding to CYP3A4. Other aspects of the pocket may have counteracted the potential advantage of the D214G substitution. For example, CYP3A4 residues F57 and M371, which are slightly longer than their corresponding residues in CYP3A5, may preclude CBZ from binding in the exact orientation observed in the CYP3A5–CBZ crystal structure. Therefore, the D214G substitution in CYP3A4 alone was not able to enhance CBZ-mediated inhibition.
F108 Plays an Important Role in CYP3A4 Inhibition.
Both prior30 and our current data (Figure 3b, Table S2) showed that CYP3A4 can be inhibited at high CBZ concentrations. These results indicate that CBZ is a de facto CYP3A4 inhibitor, albeit with poor potency. Therefore, understanding the mechanism of weaker CYP3A4 inhibition by CBZ may help to design more selective inhibitors against CYP3A5. Our combined sequence and structural analyses suggested that the binding position for CBZ in CYP3A4 was different from that observed in the CYP3A5–CBZ crystal structure. Further investigation of the apo-CYP3A4 crystal structure (PDB: 1TQN) suggested that an alternative binding site between the F–F′ loop and the B–B′ loop in CYP3A4 may accommodate CBZ. The phenylalanine (CYP3A4) to leucine (CYP3A5) sequence variation at position 108 in this region plays an important role in catalysis15, 32 and is postulated to be a major contributor to the binding pocket shape difference between the two proteins.24 Therefore, to explore if the alternative binding position of CBZ in CYP3A4 is close to F108, we constructed the mutant CYP3A4F108L to mimic the CYP3A5 sequence and determined its effect on enzyme inhibition. The F108L substitution in CYP3A4 substantially weakened the inhibitory potency of CBZ, as demonstrated by the dramatic right shift of the CYP3A4F108L dose-response curve relative to CYP3A4WT (Figure 3b). In contrast, the F108L substitution in CYP3A4 conferred only minor effects on the inhibitory potencies of ketoconazole and ritonavir (Figure S4). These results are consistent with our structural analysis, indicating that CBZ binds to CYP3A4 in a different manner than it does to CYP3A5 and suggesting that CBZ binds to CYP3A4 in a position close to residue F108.
The Propionate and 2-Chloroacetyl Groups of CBZ are Important for the Inhibition of Both CYP3A4 and CYP3A5.
The CYP3A5–CBZ crystal structure suggested that the two heme-adjacent chemical groups of CBZ, propionate and 2-chloroacetyl, play functional roles in CYP3A5 inhibition. The propionate group may provide stabilizing forces for CBZ binding through its polar interaction with A305 and hydrophobic contacts with residues F213, F304, T309, and L481. Simultaneously, the 2-chloroacetyl group displaces the heme-coordinated water without coordinating with the heme itself (Figure 1b, c). These two groups are most likely oriented differently in CYP3A4. A previous study using electron paramagnetic resonance showed that the axial water in CYP3A4 is not displaced upon CBZ binding,30 which further indicates that the 2-chloroacetyl group in CYP3A4 is in a location different from that observed in the CYP3A5–CBZ complex. Therefore, we hypothesized that in addition to the unique F–F′ loop conformation of CYP3A5, the different positions of the propionate and 2-chloroacetyl groups of CBZ contribute to its selective inhibition of CYP3A5.
To test this hypothesis, we selected 13 commercially available CBZ analogs that mainly differ from CBZ in the 2-chloroacetyl and propionate groups (shown as regions A and B in Figure 4, respectively) and compared their inhibitory potencies to CBZ in the luminescence-based P450-Glo assay using purified full-length CYP3A4 or CYP3A5. As expected, both ketoconazole and ritonavir potently inhibited both enzymes with ritonavir showing no selectivity, while CBZ was a potent and selective inhibitor of CYP3A5 (Figure S5, Table S3).30, 33 In addition, CBZ and its analogs were not time-dependent inhibitors of CYP3A5 (Figure S6).
Figure 4.

Compound structures of CBZ and its analogs. Functional groups that correspond to CBZ 2-chloroacetyl (region A) and propionate (region B) are highlighted in blue and red, respectively. All other structural changes in CBZ analogs are highlighted in magenta.
We first examined the role of the region B group by using two pairs of analogs and showed that removal of the region B group abolished CYP3A5 inhibition by CBZ analogs (Figure 5a–d). For example, clobetasol, a CBZ analog without the propionate group in region B, failed to inhibit CYP3A5 even at the highest concentration tested (60 μM). In contrast, CBZ inhibited CYP3A5 with an IC50 of 0.32 ± 0.06 μM (Figure 5a, b). Similarly, difluprednate was the strongest and most selective CYP3A5 inhibitor among all compounds we tested, yet its region B–deleted analog dexamethasone acetate only weakly inhibited CYP3A5 (35% inhibition at 300 μM) (Figure 5c, d). Although difluprednate contains an additional backbone fluorine atom, as compared with dexamethasone acetate (Figure 4), this difference may minimally affect CYP3A inhibition. Indeed, this was confirmed by the nearly identical IC50 values for CBZ and halobetasol propionate, which only differ by one fluorine atom at the same position (Figure S5, Table S3). The importance of region B in CYP3A5 inhibition was further supported by the observation that betamethasone, diflorasone, and desoximetasone, which contain only a hydroxyl or hydrogen at the region B position, exhibited no or weaker CYP3A5 inhibition than that of CBZ (Figure S5, Table S3). The 3-fold (estimated by IC50 ratio) weaker CYP3A5 inhibition by fluoremetholone acetate, which replaced the propionate group in CBZ with a one carbon shorter acetate group, also provided indirect evidence supporting the critical role of the region B group (Figure S5, Table S3).
Figure 5.

The region B group is essential for CBZ analogs to inhibit CYP3A5 but not CYP3A4. (a–d) Dose-response curves showing the inhibitory potencies of CBZ and analogs with or without region B deletions. (e) Dose-response curve of mometasone furoate showing the effect of region B extension on CYP3A4/5 inhibition. All measurements were determined with the P450-Glo biochemical assay. The percentage inhibition data were normalized against DMSO controls as 0% inhibition and 30 μM ketoconazole as 100% inhibition. The numbers reported are the means and standard deviations of the IC50 (μM) derived from three experiments, each run in triplicate. (f) The CYP3A5–CBZ crystal structure showing the residues surrounding the region B propionate group as molecular surfaces. CBZ is shown in yellow, and the heme is shown in black. Regions A and B of CBZ and analogs are highlited in blue and red, respectively, in (a-f).
In summary, the lack of CYP3A5 inhibition by region B deleted compounds indicated the critical role of the hydrophobic sandwich around the propionate group and the weak polar interaction with the backbone amine group of A305 for productive binding of CBZ to CYP3A5 and thereby potent inhibition (Figure 5f).
Unlike the strong influence on CYP3A5 inhibition, region B played a minor role in CYP3A4 inhibition. CBZ and its propionate-free analog clobetasol inhibited CYP3A4 with similar IC50 values of 8 ± 1 and 13 ± 4 μM, respectively (Figure 5a, b). Deleting the region B group from difluprednate weakened its inhibition of CYP3A4 by approximately 10-fold, which was much less than the >5000-fold weakening of CYP3A5 inhibition (estimated by IC50 ratio) (Figure 5c, d). In addition, betamethasone and diflorasone were still capable of inhibiting CYP3A4 at high concentrations, despite having lost their region B groups (Figure S5, Table S3). Together, these results indicate that a propionate-like group in region B is essential for CBZ analogs to potently inhibit CYP3A5 but not CYP3A4.
We next investigated how region B extensions affect CYP3A4 and CYP3A5 inhibition. We used mometasone furoate in this experiment because its terminal methyl group in region B is replaced by a larger and bulkier furoate group (Figure 4). The IC50 values for CBZ to inhibit CYP3A4 and CYP3A5 were 26-fold and 4-fold higher than that of mometasone furoate, respectively, indicating that extension of the region B group is favored for inhibiting both enzymes (Figure 5a, e). For CYP3A5, the result is consistent with the crystal structure as the furoate group would extend further into the large hydrophobic pocket occupied by the propionate and potentially provide a stronger anchoring effect.
We further investigated the effect of the region A group on CBZ-mediated inhibition. In CYP3A5, the 2-chloroacetyl group extended toward the heme and displaced the heme-coordinated water, whereas CBZ failed to displace the axial water in CYP3A4, suggesting that the 2-chloroacetyl group localizes further away from the heme.30 We tested whether extending the region A group of CBZ would affect its CYP3A4 or CYP3A5 inhibition. Indeed, replacing the short chloroacetyl group in CBZ or chloromethyl group in loteprednol etabonate with a much longer 2-oxopropyl propionate group, as observed in betamethasone dipropionate and prednicarbate, led to consistently weaker CYP3A5 inhibition (Figure 6a–d). However, a similar extension using a relatively shorter 2-oxopropyl acetate group slightly enhanced CYP3A5 inhibition (Figure 6e, f). Based on the CYP3A5-CBZ structure, the longer 2-oxopropyl propionate group would clash with residues T309 and A370 (Figure 6g). By comparison, the shorter 2-oxopropyl acetate group would not only avoid this potential clash but could also form a hydrogen bond between its terminal carbonyl and the side chain of T309. This new hydrogen bond may account for the near 10-fold difference in IC50 values for CYP3A5 inhibition between CBZ and difluprednate (Figure 5a, c).
Figure 6.

The region A group also contributes to CYP3A inhibition by CBZ analogs. (a–f) Dose-response curves showing the inhibitory potencies of CBZ and analogs with or without region A extensions. All measurements were determined with the P450-Glo biochemical assay. The percentage inhibition data were normalized against DMSO controls as 0% inhibition and 30 μM ketoconazole as 100% inhibition. The numbers reported are the means and standard deviations of the IC50 (μM) derived from three experiments, each run in triplicate. (g) The CYP3A5–CBZ crystal structure showing residues adjacent to the region A chloroacetyl group as molecular surfaces. CBZ is colored in yellow, and the heme is colored in black. Regions A and B of CBZ and analogs are highlited in blue and red, respectively, in (a-g).
By contrast, region A extensions affected CYP3A4 inhibition differently. Replacing the region A group with the longer 2-oxopropyl propionate group can either weaken or enhance inhibitory potencies of CBZ analogs against CYP3A4 (Figure 6a–d). The reason for these varied effects is unclear, though this provides another example that CBZ binds differently in CYP3A4. Nonetheless, these results suggest an important role of the region A group in CYP3A4 inhibition by CBZ analogs.
CBZ Analogs May Inhibit CYP3A5 Through the Occupancy of the Active Site.
To further investigate the mechanisms of CYP3A4 and CYP3A5 inhibition by CBZ analogs, we performed UV-Vis based spectroscopy analysis with purified recombinant proteins with N-terminal (CYP3A4) or N- and C-terminal (CYP3A5) truncations.22, 26 As expected, titration with ketoconazole and ritonavir induced a type II shift from 416 nm to 424 nm, which occurs when a ligand displaces the axial water and forms a strong axial coordination with the heme in place of the water molecule, in both CYP3A4 and CYP3A5 (Figure S7). Titration of CYP3A5 with CBZ induced the expected type I spectral shift from 416 nm to 386 nm, which occurs when a ligand displaces the axial water without coordinating to the heme (Figure S7). CBZ has more potential to displace the axial water for CYP3A5 than it did for CYP3A4, as indicated by the lower value of the spectral dissociation constant (Ks) and a larger maximum absorbance change (ΔAmax) (Figure 7a).30 However, when interpreting the results, it must be noted that Ks does not represent the true equilibrium dissociation constant (Kd) as the method only detects ligand binding that affects the iron spin state. Therefore, Ks is only an estimate of Kd, and its value would be equal to or larger than the value of Kd.
Figure 7.

Region B deletion increases Ks in both CYP3A4 and CYP3A5. (a–d) ΔA386nm – ΔA416nm vs compound concentration plots showing the effects of CBZ analog binding on the CYP3A4/5 spectral signals. The reported Ks and ΔAmax values were derived by fitting the data to Equation 2 (see Materials and Methods). The numbers reported are the means and standard deviations calculated from triplicate experiments.
Titration of CBZ analogs also induced type I spectral shifts in CYP3A4 and CYP3A5, albeit to different degrees depending on the analog, indicating that these compounds are type I inhibitors. In CYP3A5, compounds which exhibited weaker inhibition tended to have higher Ks values and a smaller ΔAmax upon titration, in particular the analogs lacking a large region B group (Figure S8, Table S3). For example, dexamethasone acetate and clobetasol exhibited Ks values > 100–fold higher than that of their counterparts difluprednate and CBZ (Figure 7a–d). Other compounds lacking a large region B group, such as betamethasone and diflorasone, also exhibited much higher Ks values for CYP3A5 than did CBZ (Table S3). The correlation between the Ks and IC50 values, as well as the type I spectral shifts induced by these compounds, suggest the analogs, like CBZ, inhibit CYP3A5 through the occupancy of the active site without heme coordination.
By contrast, the effect of region B deletion on Ks is less drastic in CYP3A4. Removing the propionate group from CBZ led to an approximately 20–fold increase in the Ks value for CYP3A4, which is only one tenth of the change observed in CYP3A5 (Figure 7a,b). Similarly, the loss of the region B group in difluprednate increased Ks by 3–fold for CYP3A4, which is minimal compared to the >100–fold increase seen in CYP3A5 (Figure 7c,d). These observations are consistent with results of the biochemical inhibition assay which demonstrated that region B is important for CBZ analogs to inhibit CYP3A5 but not CYP3A4. This further suggests that CBZ binds in a different position in CYP3A4 compared to CYP3A5 as region B deletion had a different impact on ligand-induced spectral changes in the two enzymes.
Hydrogen Bond Formation with the CBZ Backbone Hydroxyl Facilitates CYP3A5 Inhibition.
To investigate whether the hydrogen bond observed between the backbone hydroxyl of CBZ and residue A370 or R372 in the CYP3A5–CBZ crystal structure contributes to CYP3A5 inhibition, we measured the inhibitory potency of the analog clobetasone butyrate against CYP3A5 and its effect on the spectral signal of CYP3A5. This compound differs from CBZ by having the backbone hydroxyl of CBZ replaced with a carbonyl group that is unable to form hydrogen bonds with A370 or R372 (Figure 1c, Figure 4). We hypothesized that this loss of interaction would weaken inhibitor binding and decrease the potency of the inhibitors. Indeed, our biochemical inhibition assay results showed that the IC50 value of clobetasone butyrate for CYP3A5 was approximately 5-fold higher than that of CBZ (Table S3). UV-Vis measurements showed that the Ks for clobetasone butyrate was also ~7-fold higher than that for CBZ (Table S3). Although clobetasone butyrate has one extra methyl group at the end of the region B than does CBZ, this extension should not impair inhibition of CYP3A5, as demonstrated by the potent inhibitory activity of mometasone furoate, which differs from CBZ by having a larger and bulkier furoate group in region B (Figure S5, Table S3). In contrast, this hydroxyl to carbonyl change slightly enhanced CYP3A4 inhibition and maintained similar Ks value in the UV-Vis assay (Table S3). In summary, these results indicate that the CBZ-A370/R372 hydrogen bond contributes to CYP3A5 inhibition and possibly selectivity by stabilizing CBZ in the binding pocket.
DISCUSSION
The development of a potent, selective inhibitor for CYP3A5 is beneficial for scientific research to explore the role of CYP3A5 in metabolism and disease, and for clinical practice to increase the efficacy of certain drugs, without adverse drug-drug interactions caused by inhibition of CYP3A4. Here, we explored the structural mechanism of CYP3A5 selective inhibition by using CBZ, the only reported CYP3A5-selective inhibitor, as a model compound. The crystal structure of CYP3A5 in complex with CBZ showed that the compound binds CYP3A5 as a type I inhibitor which does not coordinate with the heme. The structure also revealed several important structural factors that may contribute to the selective inhibition. These include the unique F–F′ loop conformation that provides the hydrophobic surface for CBZ binding and several polar interactions that stabilize the binding of the inhibitor molecule. The observations from the CYP3A5–CBZ structure were further supported by data from cell-based, biochemical, and biophysical experiments. The structure-activity relationship analysis also revealed that the heme-adjacent 2-chloroacetyl and propionate groups of CBZ play important roles in mediating CYP3A5 inhibition, and that the propionate group contributes to the selectivity for CYP3A5 by increasing the potency of CYP3A5 inhibition while having minimal inhibitory effect on CYP3A4.
One key to developing a selective CYP3A5 inhibitor is to avoid the inhibition of CYP3A4 to prevent adverse drug-drug interactions. In the case of CBZ the ligand is unlikely to bind CYP3A4 in the optimal orientation due to the inability of the F–F′ loop to achieve a preferred conformation as seen in the CYP3A5-CBZ complex. Unfortunately, we were unable to directly determine the binding position of CBZ in CYP3A4 as co-crystallization attempts were unsuccessful, but we have an approximation about how CBZ binds to CYP3A4 based on our comparative structural and activity-based results. First, the inhibitory activities of CBZ analogs on CYP3A4 cannot be explained by the CYP3A5-CBZ crystal structure, which suggests a different binding position for CBZ in CYP3A4. Second, we generated CYP3A5G214D to mimic the D214 in CYP3A4 which presumably blocks CBZ binding near the F–F′ loop and found that the inhibitory potency of CBZ is dramatically reduced even beyond the inhibition seen in CYP3A4WT. This suggests that the binding position of CBZ in CYP3A4WT is not possible in CYP3A5G214D or CYP3A5WT. Lastly, results of the F108L substitution in CYP3A4 suggests that the binding position of CBZ in CYP3A4 is near residue F108. As a result, optimization of CBZ as a selective CYP3A5 inhibitor will need to account for this different binding position in CYP3A4.
While the importance of amino acid sequence divergence at residue position 214 is evident for CYP3A5 selective inhibition by CBZ, other divergent residues associated with the F–F′ loop may also be important for the selectivity. CYP3A5 is the major CYP enzyme responsible for oxidative metabolism of maraviroc, an anti-human immunodeficiency virus drug. A study investigating the CYP3A5-mediated maraviroc metabolism showed that CYP3A5 mutants S206N, G214D, and L219F, which are located on the helix F, F–F′ loop, and helix F′, respectively, altered the rate of catalysis and distribution of metabolites.15 Notably, among all mutants evaluated, the G214D mutant caused the greatest reduction in the formation of oxidative metabolites, and shifted the metabolite formation of CYP3A5 drastically towards that of CYP3A4, which is consistent with our observation in the cell-based inhibition assay, and highlights the biological significance of our structural analysis. Another study demonstrated that the residue F210, which contributes to the phenylalanine contacts on the top of the ligand binding pocket, is at least partially responsible for the faster metabolism of schisantherin E in CYP3A5.29 Similarly, reciprocal substitutions in CYP3A4, which include N206S and L210F near the F–F′ loop, as well as S478D, L479T, G480Q on the adjacent C-terminal loop, were also shown to shift the CYP3A4-mediated aflatoxin B1 metabolism to more resemble CYP3A5.32 These results highlight the critical role of the F–F′ loop in enzyme function, and suggest that G214 is not the only residue that contributes to the unique F–F′ loop conformation seen in CYP3A5.
The ligand binding pockets of CYP3A4 and CYP3A5 are more flexible compared to those of other CYPs due to the presence of the F–F′ and G–G′ loops that form the top of the ligand binding pocket in CYP3A4/5. Because of this, a more rigid compound would confer better selectivity. This is indeed the case for CBZ which only has 5 rotatable bonds, all of which are located in either the 2-chloroacetyl or propionate groups which are not part of the main chemical scaffold. In the biochemical assays, CBZ shows 25-fold selectivity for CYP3A5 inhibition, whereas ritonavir, which has 18 rotatable bonds, inhibits CYP3A4 and CYP3A5 with near equal potency. Similar to CBZ, ketoconazole, which has 7 rotatable bonds, shows 20-fold selectivity for CYP3A4 inhibition. Our recent study also found that CBZ shows selectivity for CYP3A5 against 6 other major CYP enzymes,30 many of which have a continuous helix F and helix G.34–38 The rigid nature of CBZ likely prevents binding to these other less flexible binding pockets. These discoveries suggest that although heme ligation may improve the potency of an inhibitor for CYP3A4/5, the degree of flexibility in the inhibitor plays a major role in determining the selectivity of the ligand for one enzyme or the other. Therefore, designing a rigid compound that will preferentially bind to a unique binding surface of the flexible binding pocket of CYP3A5 is a viable path for selective inhibition.
The development of CYP3A4/5 inhibitors has focused heavily on type II inhibitors which achieve inhibition by ligating to the heme and blocking substrate catalysis.39–43 Our data demonstrated the feasibility of potently and selectively inhibiting CYP3A5 without the need to coordinate with the heme iron. Two recently published CYP3A4 structures in complex with type I inhibitors have also shown that type I ligands can act as potent CYP3A4 inhibitors.44–45 Therefore, the development of type I ligands as potent, selective inhibitors of either CYP3A5 or CYP3A4 should be pursued.
CONCLUSION
Our understanding of the unique role of CYP3A5 in drug metabolism and related diseases is limited because it shares common substrates with CYP3A4 and selective inhibitors against CYP3A5 are lacking. Identifying such inhibitors has been challenging because both CYP3A4 and CYP3A5 have flexible binding pockets that accommodate structurally diverse compounds. The mechanistic insights we report here provide the basis for several proposed guidelines to elucidate and design more potent and selective CYP3A5 inhibitors: (1) Candidate inhibitors should have a rigid structure that selectively fits the CYP3A5 binding pocket. (2) Candidate inhibitors should fit to the unique F–F′ loop conformation in the CYP3A5–CBZ structure. (3) Moieties of the candidate inhibitor scaffolds should utilize the polar interactions and hydrophobic pocket formed by F213, F304, T309, and L481 in CYP3A5 to increase their potency. (4) Care should be taken when modifying heme-adjacent moieties to avoid steric clash with nearby residues and the heme.
MATERIALS AND METHODS
Compounds.
All compounds were purchased from commercial companies. The compound name, catalog number, and vendor information are as follows: Clobetasol propionate (F535) was obtained from AK Scientific (Union City, CA). Ketoconazole (AC513267) was purchased from Abovchem (San Diego, CA). Ritonavir (SML0491), betamethasone (B7005), betamethasone dipropionate (B1152), dexamethasone (D1881), difluprednate (D6288), and loteprednol etabonate (SML0547) were purchased from Millipore-Sigma (St. Louis, MO). Clobetasone butyrate (HY-B1616), desoximetasone (HY-17570), diflorasone (HY-A0158), fluorometholone acetate (HY-B1471), halobetasol propionate (HY-B0878), and mometasone furoate (HY-13693) were obtained from MedChemExpress (Monmouth Junction, NJ). Clobetasol (sc-391181) was purchased from Santa Cruz Biotechnology (Dallas, TX). Prednicarbate (1554909) was purchased from United States Pharmacopeia (Rockville, MD). The identity of each compound was verified with high-resolution mass spectrometry, and their purities (> 97%) were determined by high-performance liquid chromatography equipped with UV-Vis and evaporative light-scattering detectors. Compound quality control data are presented in Table S4.
Expression and Purification of CYP3A4 and CYP3A5 Proteins.
CYP3A4WT and CYP3A5WT expression plasmids for bacterial protein production were constructed by GenScript (Piscataway, NJ). The plasmids were made by inserting DNA fragments encoding modified human CYP3A4 or CYP3A5 between the NdeI/HindIII sites of the pCWori vector (Creative Biogene, Shirley, NY). The coding sequence for CYP3A4, which was optimized for an E. coli expression system, encodes WT CYP3A4 with an N-terminal truncation and a C-terminal 4× His-tag, as previously described.22 The CYP3A5 coding sequence encodes a truncated version of WT CYP3A5 with N- and C-terminal deletions at amino acids 3–22 and 498–502, as well as a C-terminal 4× His-tag.26 The exact protein sequences are shown in Figure S9. Both constructs were verified to be correct by DNA sequencing.
The protocols for expressing the CYP3A4 and CYP3A5 proteins closely followed a previously published method.30 E. coli DH5α_F′_Iq cells (New England Biolabs, Ipswich, MA, catalog no. C2992H) were cotransformed with the expression plasmid and a pGro7 plasmid (Takara Bio USA, Mountain View, CA) that expresses the chaperonin protein GroES–GroEL. The transformed cells were selected by both ampicillin and chloramphenicol resistance. In a typical 12-L protein production system, the cell culture was grown in terrific broth at 37°C until the OD600 reached 0.4–0.5. The cells were grown at 28°C for another 30 min before inducing protein expression with 1 mM isopropyl β-D-1-thiogalactopyranoside, 0.5 mM or 5 mM 5-aminolevulinic acid hydrochloride for CYP3A4 and CYP3A5, respectively, and 3 g/L of L-arabinose. At 44–48 h post induction, the cells were harvested by centrifugation at 6,000 g for 10 min, and the pellets were resuspended in 500 mL of cold lysis buffer containing 500 mM potassium phosphate (KPO4) (pH 7.4), 10 mM β-mercaptoethanol (BME), and 20% glycerol. EDTA-free protease inhibitor cocktail tablets (Millipore-Sigma, catalog no. S8830) were also added according to the manufacturer directions. Resuspended cells were lysed by passing once through an LM-10 microfluidizer (Microfluidics, Westwood, MA) at 18,000 psi. CHAPS was added to 8 mM in the resulting lysate, and the mixture was incubated with stirring for 2 h at 4°C to extract proteins from the spheroplasts. After the incubation, the lysates were centrifuged at 40,000 g, 4°C for 1.5 h, and the supernatants were collected for subsequent protein purification.
CYP3A4 was purified by using Ni-affinity and size-exclusion chromatography columns. All purification steps were carried out at 4°C. In a typical purification, lysate supernatants from 4-L cultures were loaded on a 20-mL HisPrep FF 16/10 Ni-NTA column (Cytiva, Marlborough, MA) that was pre-equilibrated in Buffer A (500 mM KPO4, pH 7.4; 10 mM BME; 8mM CHAPS; and 20% glycerol). The column was then washed with 2 column volumes (CVs) of Buffer A containing 5 mM ATP, 10 mM MgCl2, and 100 mM KCl to remove chaperone proteins and 2 CVs of Buffer A containing 20 mM imidazole to remove loosely bound contaminants. The CYP3A4 protein was eluted with a 20–250 mM imidazole gradient in Buffer A. Fractions that contained partially purified CYP3A4 were pooled and concentrated, and then passed through a HiLoad 26/600 Superdex 200-pg size-exclusion column (Cytiva) pre-equilibrated in Buffer B (50 mM KPO4, pH 7.4; 500 mM NaCl; 10 mM BME; and 20% Glycerol). CYP3A4-containing fractions were loaded onto a 2 × 5 mL HisTrap FF Ni-NTA column (Cytiva), washed with 2 CVs of Buffer B, and eluted with a 0–250 mM imidazole gradient in Buffer B. Fractions containing CYP3A4 with over 95% purity (determined by SDS-PAGE) were pooled, concentrated, and buffer exchanged into Buffer B with a HiPrep 26/10 desalting column (Cytiva). The protein solutions were flash frozen in liquid nitrogen and stored at −80°C.
CYP3A5 was purified by using a previously published protocol,26 with the exception that a Superdex 200 Increase 10/300 GL column (Cytiva) was used for the final purification step. CYP3A4 and CYP3A5 protein concentrations were determined by using the CO difference spectra method described by Guengerich et al.,46 which is a modified protocol based on the work of Omura and Sato.47
Crystallization and Structure Determination.
CYP3A5–CBZ was crystallized by using the sitting drop vapor diffusion method in a 24-well Cryschem plate (Hampton Research, Aliso Viejo, CA). Before crystallization, 25 mg/mL CYP3A5 in storage buffer (100 mM HEPES, 50 mM KOAc, 0.5 mM EDTA, 10 mM BME, and 20% glycerol at pH 7.4) was co-incubated with 0.9 mM CBZ on ice for 1 h. The final concentration of DMSO in the mixture was 4.5%. Each crystallization drop consisted of 1 μL of CYP3A5–CBZ mixture, 1 μL of reservoir precipitant, and 0.1 μL of Anapoe-20 solution (Anatrace, Maumee, OH). The crystallization drops were equilibrated against 0.5 mL of precipitant solution (0.2M 2-[(2-amino-2-oxoethyl)-(carboxymethyl) amino] acetic acid and 30% (w/v) PEG3350 at pH 6.5). Multilayer crystals grew within 1 week at 20°C. The cryoprotection solution was a 1:1 (v/v) mixture of precipitant solution and PEG300.
X-ray diffraction data were collected to a resolution of 2.65 Å at AMX Beamline 17-ID-1 at the National Synchrotron Light Source II at Brookhaven National Laboratory. Frames were processed with fast_dp.48 The crystals belonged to space group I222, with one molecule in the asymmetric unit. The structure was solved by molecular replacement by using ligand-free CYP3A5 (PDB: 6MJM; 100% sequence identity) as the search model with the program phaser.49 Initial model building was performed with COOT.50 Iterative cycles of building and refinement were conducted, and the final refinement was conducted with Phenix.51 The data collection and refinement statistics are shown in Table S1.
Plasmid Construction for Cell-Based Inhibition Assays.
The doxycycline-inducible pLVX-TRE3G-ZsGreen1 (Takara Bio USA) vectors containing ZsGreen1-IRES-CYP3A4 and ZsGreen1-IRES-CYP3A5 are previously described.30 All cloning primers are presented in Table S5. For this study, the ZsGreen1-IRES-CYP3A cassettes were subcloned into pcDNA3 (Thermo Fisher Scientific, Waltham, MA) to achieve constitutive gene expression, with ZsGreen1 serving as a transfection reporter. ZsGreen1-IRES-CYP3A4 was amplified with primers oAH522 and oAH523, and ZsGreen1-IRES-CYP3A5 was amplified with primers oAH522 and oAH524. The amplicons were cloned into HindIII-digested pcDNA3 with NEBuilder HiFi DNA Assembly Master Mix (New England Biolabs). Mutants were made with the QuikChange II Site-Directed Mutagenesis Kit (Agilent Technologies, Santa Clara, CA) with the primers listed in Table S5.
Cell-Based CYP3A Mutant Inhibition Assays.
We obtained 293T/17 cells (catalog no. CRL-11268) from the American Type Culture Collection (Manassas, VA) and authenticated the cell cultures by short tandem repeat DNA profiling. The cells were maintained in growth medium (Dulbecco Modified Eagle Medium with 10% fetal bovine serum) in a humidified atmosphere at 37°C with 5% CO2 and routinely verified to be mycoplasma free with the MycoProbe Mycoplasma Detection Kit (R&D Systems, Minneapolis, MN). Cell counts were obtained with a Countess II Automated Cell Counter (Thermo Fisher Scientific) and trypan blue exclusion staining.
Each CYP3A expression plasmid (10 μg) was mixed with 30 μL FuGENE HD transfection reagent (Promega, Madison, WI) in 1 mL Opti-MEM I Reduced Serum Medium (Thermo Fisher Scientific) and incubated for 30 min at room temperature. The transfection mixtures were added to 6 × 106 293T/17 cells in 10 mL growth medium, and the cells were plated in 10-cm tissue culture-treated dishes. After 24 h of transfection, the medium was removed and replaced with 10 mL fresh growth medium. After an additional 24 h, the medium was removed, and cells were washed with Dulbecco phosphate-buffered saline and trypsinized. Compound inhibition of WT and mutant CYP enzymes was quantified by using the P450-Glo assay kit with luciferin-IPA substrate (Promega, catalog no. V9002). We plated 5 × 104 cells in 25 μL growth media in white 384-well tissue culture-treated plates. Each well was added with 37.5 nL of DMSO or stock compounds with an Echo 555 Acoustic Liquid Handler (Labcyte), followed by 25 nL of 3 mM luciferin-IPA in DMSO. The final concentrations of the reaction components were 0.25% DMSO, 3 μM luciferin-IPA, and 0.0003–60 μM test compounds. Plates were shaken for 5 min at room temperature and incubated at 37°C with 5% CO2 for 1 h. Luciferin detection reagent (25 μL) was added to each well, and the plates were shaken for 5 min at room temperature and incubated for an additional 15 min at room temperature. Luminescence was then measured with an EnVision 2012 Multilabel Plate Reader (PerkinElmer Life Sciences, Waltham, MA). Experiments with each compound concentration were repeated three times on the same plate.
Light intensity signals for each mutant were normalized against the average of their DMSO negative controls (0% inhibition) and media-only positive controls (100% inhibition) within each plate to account for any differences in transfection efficiency, protein expression level, or enzymatic activity. The resulting percentage inhibition values were plotted against the log10 [Compound], and the data were fitted to Equation 1 in GraphPad Prism (GraphPad, San Diego, CA):
| (1) |
The bottom and top are the minimum and maximum percentage inhibition, and the hill slope is the factor for possible multiple-site binding events. The maximum percentage inhibition (top) was constrained to 100% if the fitted value was >120% of the positive control as it is not biologically possible.
Biochemical CYP3A Inhibition Assays.
The inhibitory effects of clobetasol and its analogs on CYP3A4 and CYP3A5 were measured by using the same P450-Glo assay as described in the cell-based approach (Promega, catalog no. V9002) with a few modifications. Instead of whole cells, protein mixtures containing purified human CYP3A4 (Corning, Corning, NY, catalog no. 456202) or CYP3A5 (Corning, catalog no. 456256) and their necessary cofactors were used as enzyme sources. The NADPH regenerating system (Promega, catalog no. V9510) was also required to initiate the reaction. All assays were performed in 384-well white assay plates. Each well was first administered 12.5 μL of 2× enzyme–substrate mixture solution followed by 37.5 nL of DMSO or stock compounds with an Echo 555 Acoustic Liquid Handler (Labcyte, San Jose, CA). The reactions were initiated by adding another 12.5 μL of 2× NADPH regenerating solution. For time-dependent inhibition assay, DMSO or stock compounds were pre-incubated with the substrate-free CYP3A5 enzyme mixture for 0 or 30 mins at room temperature, and the reaction was initiated by adding the NADPH regenerating solution containing the substrate. The final concentrations of the reaction components were 0.25% DMSO, 4 nM CYP3A4/5, 3 μM luciferin-IPA substrate, and 0.0003–300 μM of the test compounds. The plates were shaken for 5 min at room temperature and incubated for another 10 min at 37°C. The reactions were quenched by adding 25 μL/well luciferin detection reagent, and the plates were incubated for additional 20 min at room temperature. Luminescence signals were read with an EnVision 2012 Multilabel Plate Reader (PerkinElmer Life Sciences). Experiments for each compound concentration were repeated nine times, with three times in the same plate, and three times across different plates.
Light intensity signals were analyzed by using the same approach as the cell-based assay, with the exception that wells containing 30 μM ketoconazole were used as positive controls (100% inhibition).
UV-Vis Spectroscopy Assays.
UV-Vis–based binding assays were carried out in a plate-based format with Corning 384-well clear flat bottom plates (catalog no. 8807BC). Each well contained 50 μL solution at final concentrations of 4 μM protein and 0–100 μM test compounds in assay buffer (100mM HEPES, 100 mM NaOAc, 10 mM BME, and 20% glycerol, pH 7.4). Subsequently, 125 nL of DMSO or test compound were added from stock solutions with an Echo 555 liquid handler. The final DMSO concentration was maintained at 0.25% for all wells. Absorbance spectra ranging from 350–700 nm were recorded for each well, with a 2-nm step size, by using a SPECTRAmax PLUS384 spectrophotometer (Molecular Devices, San Jose, CA). Experiments for each compound concentration were repeated three times in the same plate.
The spectral dissociation constant (Ks) and maximum absorbance change (ΔAmax) were determined by monitoring spectral changes at different compound concentrations.52 For each set of measurements, the spectral differences were first calculated by subtracting the ligand-free spectrum from the ligand-bound spectra, and the peaks and troughs of the wavelengths were determined. To better represent the compound-induced spectral changes, the absorbance changes at the peaks and troughs of the wavelengths were summed and plotted against the compound concentrations and fitted to Equation 2 with GraphPad Prism (GraphPad):
| (2) |
Ks and ΔAmax are the values to be fitted, and [P]T and [L]T are the known total protein and ligand concentrations, respectively.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank ALSAC for support, Nisha Badders, PhD, ELS (St. Jude Department of Scientific Editing) for editing the manuscript, Lei Yang for performing high-resolution mass spectrometry and high-performance liquid chromatography analyses of compounds and analyzed data, Madison Rice for technical assistance in creating the supplementary cover art image, and other members of the Chen research laboratory for valuable discussions of the manuscript. This work utilized the FMX and AMX beamlines, which are primarily supported by the National Institutes of Health, National Institute of General Medical Sciences through a Center Core P30 Grant (P30GM133893), and by the U.S. Department of Energy Office of Biological and Environmental Research (KP1607011). As part of the National Synchrotron Light Source II, a national user facility at Brookhaven National Laboratory, work performed at the Center for BioMolecular Structures is supported in part by the U.S. Department of Energy, Office of Science, Office of Basic Energy Sciences Program under contract number DE-SC0012704.
Funding Sources
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under award number R35GM118041. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
ABBREVIATIONS
- BME
β-mercaptoethanol
- CBZ
clobetasol propionate
- CV
column volume
- CYP
cytochrome P450
- KPO4
potassium phosphate
- luciferin-IPA
luciferin isopropyl acetal
- PDB
Protein Data Bank
- WT
wild-type
Footnotes
The authors will release the atomic coordinates and experimental data for the structure of CYP3A5 in complex with CBZ (PDB: 7LAD) upon article publication.
REFERENCES
- (1).Danielson PB, The cytochrome P450 superfamily: biochemistry, evolution and drug metabolism in humans. Curr Drug Metab 2002, 3 (6), 561–97. [DOI] [PubMed] [Google Scholar]
- (2).Williams JA; Hyland R; Jones BC; Smith DA; Hurst S; Goosen TC; Peterkin V; Koup JR; Ball SE, Drug-drug interactions for UDP-glucuronosyltransferase substrates: a pharmacokinetic explanation for typically observed low exposure (AUCi/AUC) ratios. Drug Metab Dispos 2004, 32 (11), 1201–8. [DOI] [PubMed] [Google Scholar]
- (3).Wienkers LC; Heath TG, Predicting in vivo drug interactions from in vitro drug discovery data. Nat Rev Drug Discov 2005, 4 (10), 825–33. [DOI] [PubMed] [Google Scholar]
- (4).Wright WC; Chenge J; Chen T, Structural Perspectives of the CYP3A Family and Their Small Molecule Modulators in Drug Metabolism. Liver Res 2019, 3 (3–4), 132–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Hakkola J; Hukkanen J; Turpeinen M; Pelkonen O, Inhibition and induction of CYP enzymes in humans: an update. Arch Toxicol 2020, 94 (11), 3671–3722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (6).Shehu AI; Ma X; Venkataramanan R, Mechanisms of Drug-Induced Hepatotoxicity. Clin Liver Dis 2017, 21 (1), 35–54. [DOI] [PubMed] [Google Scholar]
- (7).Shehu AI; Ma X, Pregnane X receptor in drug-induced liver injury: Friend or foe? Liver Research 2018, 2 (4), 173–179. [Google Scholar]
- (8).Andrade RJ; Chalasani N; Bjornsson ES; Suzuki A; Kullak-Ublick GA; Watkins PB; Devarbhavi H; Merz M; Lucena MI; Kaplowitz N; Aithal GP, Drug-induced liver injury. Nat Rev Dis Primers 2019, 5 (1), 58. [DOI] [PubMed] [Google Scholar]
- (9).de Wildt SN; Kearns GL; Leeder JS; van den Anker JN, Cytochrome P450 3A: ontogeny and drug disposition. Clin Pharmacokinet 1999, 37 (6), 485–505. [DOI] [PubMed] [Google Scholar]
- (10).Diczfalusy U; Nylen H; Elander P; Bertilsson L, 4beta-Hydroxycholesterol, an endogenous marker of CYP3A4/5 activity in humans. Br J Clin Pharmacol 2011, 71 (2), 183–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Zhu Y; Wang F; Li Q; Zhu M; Du A; Tang W; Chen W, Amlodipine metabolism in human liver microsomes and roles of CYP3A4/5 in the dihydropyridine dehydrogenation. Drug Metab Dispos 2014, 42 (2), 245–9. [DOI] [PubMed] [Google Scholar]
- (12).Vermeer LM; Isringhausen CD; Ogilvie BW; Buckley DB, Evaluation of Ketoconazole and Its Alternative Clinical CYP3A4/5 Inhibitors as Inhibitors of Drug Transporters: The In Vitro Effects of Ketoconazole, Ritonavir, Clarithromycin, and Itraconazole on 13 Clinically-Relevant Drug Transporters. Drug Metab Dispos 2016, 44 (3), 453–9. [DOI] [PubMed] [Google Scholar]
- (13).Sudo M; Nishihara M; Takahashi J; Asahi S, Long-Term Stability of Cryopreserved Human Hepatocytes: Evaluation of Phase I and II Drug-Metabolizing Enzyme Activities and CYP3A4/5 Induction for More than a Decade. Drug Metab Dispos 2017, 45 (7), 734–736. [DOI] [PubMed] [Google Scholar]
- (14).Dennison JB; Kulanthaivel P; Barbuch RJ; Renbarger JL; Ehlhardt WJ; Hall SD, Selective metabolism of vincristine in vitro by CYP3A5. Drug Metab Dispos 2006, 34 (8), 1317–27. [DOI] [PubMed] [Google Scholar]
- (15).Lu Y; Hendrix CW; Bumpus NN, Cytochrome P450 3A5 plays a prominent role in the oxidative metabolism of the anti-human immunodeficiency virus drug maraviroc. Drug Metab Dispos 2012, 40 (12), 2221–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (16).Khan AR; Raza A; Firasat S; Abid A, CYP3A5 gene polymorphisms and their impact on dosage and trough concentration of tacrolimus among kidney transplant patients: a systematic review and meta-analysis. Pharmacogenomics J 2020, 20 (4), 553–562. [DOI] [PubMed] [Google Scholar]
- (17).Dai Y; Hebert MF; Isoherranen N; Davis CL; Marsh C; Shen DD; Thummel KE, Effect of CYP3A5 polymorphism on tacrolimus metabolic clearance in vitro. Drug Metab Dispos 2006, 34 (5), 836–47. [DOI] [PubMed] [Google Scholar]
- (18).Chen L; Prasad GVR, CYP3A5 polymorphisms in renal transplant recipients: influence on tacrolimus treatment. Pharmgenomics Pers Med 2018, 11, 23–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Werk AN; Cascorbi I, Functional gene variants of CYP3A4. Clin Pharmacol Ther 2014, 96 (3), 340–8. [DOI] [PubMed] [Google Scholar]
- (20).Williams JA; Cook J; Hurst SI, A significant drug-metabolizing role for CYP3A5? Drug Metab Dispos 2003, 31 (12), 1526–30. [DOI] [PubMed] [Google Scholar]
- (21).Noll EM; Eisen C; Stenzinger A; Espinet E; Muckenhuber A; Klein C; Vogel V; Klaus B; Nadler W; Rosli C; Lutz C; Kulke M; Engelhardt J; Zickgraf FM; Espinosa O; Schlesner M; Jiang X; Kopp-Schneider A; Neuhaus P; Bahra M; Sinn BV; Eils R; Giese NA; Hackert T; Strobel O; Werner J; Buchler MW; Weichert W; Trumpp A; Sprick MR, CYP3A5 mediates basal and acquired therapy resistance in different subtypes of pancreatic ductal adenocarcinoma. Nat Med 2016, 22 (3), 278–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Yano JK; Wester MR; Schoch GA; Griffin KJ; Stout CD; Johnson EF, The structure of human microsomal cytochrome P450 3A4 determined by X-ray crystallography to 2.05-A resolution. J Biol Chem 2004, 279 (37), 38091–4. [DOI] [PubMed] [Google Scholar]
- (23).Ekroos M; Sjogren T, Structural basis for ligand promiscuity in cytochrome P450 3A4. Proc Natl Acad Sci U S A 2006, 103 (37), 13682–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Hsu MH; Johnson EF, Active-site differences between substrate-free and ritonavir-bound cytochrome P450 (CYP) 3A5 reveal plasticity differences between CYP3A5 and CYP3A4. J Biol Chem 2019, 294 (20), 8015–8022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (25).Sevrioukova IF; Poulos TL, Structure and mechanism of the complex between cytochrome P4503A4 and ritonavir. Proc Natl Acad Sci U S A 2010, 107 (43), 18422–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (26).Hsu MH; Savas U; Johnson EF, The X-Ray Crystal Structure of the Human Mono-Oxygenase Cytochrome P450 3A5-Ritonavir Complex Reveals Active Site Differences between P450s 3A4 and 3A5. Mol Pharmacol 2018, 93 (1), 14–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (27).Wu J; Guan X; Dai Z; He R; Ding X; Yang L; Ge G, Molecular probes for human cytochrome P450 enzymes: Recent progress and future perspectives. Coordination Chemistry Reviews 2021, 427. [Google Scholar]
- (28).Li X; Jeso V; Heyward S; Walker GS; Sharma R; Micalizio GC; Cameron MD, Characterization of T-5 N-oxide formation as the first highly selective measure of CYP3A5 activity. Drug Metab Dispos 2014, 42 (3), 334–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Wu JJ; Cao YF; Feng L; He YQ; Hong JY; Dou TY; Wang P; Hao DC; Ge GB; Yang L, A Naturally Occurring Isoform-Specific Probe for Highly Selective and Sensitive Detection of Human Cytochrome P450 3A5. J Med Chem 2017, 60 (9), 3804–3813. [DOI] [PubMed] [Google Scholar]
- (30).Wright WC; Chenge J; Wang J; Girvan HM; Yang L; Chai SC; Huber AD; Wu J; Oladimeji PO; Munro AW; Chen T, Clobetasol Propionate Is a Heme-Mediated Selective Inhibitor of Human Cytochrome P450 3A5. J Med Chem 2020, 63 (3), 1415–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (31).Cali JJ; Sobol M; Ma D; Uyeda HT; Meisenheimer P, CYP3A4 P450-Glo® Assays with Luciferin-IPA: The Most Sensitive and Selective Bioluminescent CYP3A4 Assay. Promega Corporation. Available online at: http://www.promega.com/resources/pubhub/cellnotes/cyp3a4-p450-glo-assays-with-luciferin-ipa-the-most-sensitive-andselective-bioluminescent-cyp3a4/ Updated 2009. Accessed August 20th, 2021.
- (32).Wang H; Dick R; Yin H; Licad-Coles E; Kroetz DL; Szklarz G; Harlow G; Halpert JR; Correia MA, Structure-function relationships of human liver cytochromes P450 3A: aflatoxin B1 metabolism as a probe. Biochemistry 1998, 37 (36), 12536–45. [DOI] [PubMed] [Google Scholar]
- (33).Granfors MT; Wang JS; Kajosaari LI; Laitila J; Neuvonen PJ; Backman JT, Differential inhibition of cytochrome P450 3A4, 3A5 and 3A7 by five human immunodeficiency virus (HIV) protease inhibitors in vitro. Basic Clin Pharmacol Toxicol 2006, 98 (1), 79–85. [DOI] [PubMed] [Google Scholar]
- (34).Williams PA; Cosme J; Ward A; Angove HC; Matak Vinkovic D; Jhoti H, Crystal structure of human cytochrome P450 2C9 with bound warfarin. Nature 2003, 424 (6947), 464–8. [DOI] [PubMed] [Google Scholar]
- (35).Schoch GA; Yano JK; Wester MR; Griffin KJ; Stout CD; Johnson EF, Structure of human microsomal cytochrome P450 2C8. Evidence for a peripheral fatty acid binding site. J Biol Chem 2004, 279 (10), 9497–503. [DOI] [PubMed] [Google Scholar]
- (36).Rowland P; Blaney FE; Smyth MG; Jones JJ; Leydon VR; Oxbrow AK; Lewis CJ; Tennant MG; Modi S; Eggleston DS; Chenery RJ; Bridges AM, Crystal structure of human cytochrome P450 2D6. J Biol Chem 2006, 281 (11), 7614–22. [DOI] [PubMed] [Google Scholar]
- (37).Reynald RL; Sansen S; Stout CD; Johnson EF, Structural characterization of human cytochrome P450 2C19: active site differences between P450s 2C8, 2C9, and 2C19. J Biol Chem 2012, 287 (53), 44581–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (38).Shah MB; Wilderman PR; Liu J; Jang HH; Zhang Q; Stout CD; Halpert JR, Structural and biophysical characterization of human cytochromes P450 2B6 and 2A6 bound to volatile hydrocarbons: analysis and comparison. Mol Pharmacol 2015, 87 (4), 649–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (39).Sevrioukova IF; Poulos TL, Dissecting cytochrome P450 3A4-ligand interactions using ritonavir analogues. Biochemistry 2013, 52 (26), 4474–81. [DOI] [PubMed] [Google Scholar]
- (40).Kaur P; Chamberlin AR; Poulos TL; Sevrioukova IF, Structure-Based Inhibitor Design for Evaluation of a CYP3A4 Pharmacophore Model. J Med Chem 2016, 59 (9), 4210–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (41).Samuels ER; Sevrioukova I, Inhibition of Human CYP3A4 by Rationally Designed Ritonavir-Like Compounds: Impact and Interplay of the Side Group Functionalities. Mol Pharm 2018, 15 (1), 279–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (42).Samuels ER; Sevrioukova I, Structure-Activity Relationships of Rationally Designed Ritonavir Analogues: Impact of Side-Group Stereochemistry, Headgroup Spacing, and Backbone Composition on the Interaction with CYP3A4. Biochemistry 2019, 58 (15), 2077–2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (43).Samuels ER; Sevrioukova IF, An increase in side-group hydrophobicity largely improves the potency of ritonavir-like inhibitors of CYP3A4. Bioorg Med Chem 2020, 28 (6), 115349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (44).Paquin A; Oufqir Y; Sevrioukova IF; Reyes-Moreno C; Berube G, Innovative C2-symmetric testosterone and androstenedione dimers: Design, synthesis, biological evaluation on prostate cancer cell lines and binding study to recombinant CYP3A4. Eur J Med Chem 2021, 220, 113496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (45).Toupin N; Steinke SJ; Nadella S; Li A; Rohrabaugh TN Jr.; Samuels ER; Turro C; Sevrioukova IF; Kodanko JJ, Photosensitive Ru(II) Complexes as Inhibitors of the Major Human Drug Metabolizing Enzyme CYP3A4. J Am Chem Soc 2021, 143 (24), 9191–9205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (46).Guengerich FP; Martin MV; Sohl CD; Cheng Q, Measurement of cytochrome P450 and NADPH-cytochrome P450 reductase. Nat Protoc 2009, 4 (9), 1245–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (47).Omura T; Sato R, The Carbon Monoxide-Binding Pigment of Liver Microsomes. Ii. Solubilization, Purification, and Properties. J Biol Chem 1964, 239, 2379–85. [PubMed] [Google Scholar]
- (48).Winter G, xia2: an expert system for macromolecular crystallography data reduction. Journal of Applied Crystallography 2009, 43 (1), 186–190. [Google Scholar]
- (49).McCoy AJ; Grosse-Kunstleve RW; Adams PD; Winn MD; Storoni LC; Read RJ, Phaser crystallographic software. J Appl Crystallogr 2007, 40 (Pt 4), 658–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (50).Emsley P; Lohkamp B; Scott WG; Cowtan K, Features and development of Coot. Acta Crystallogr D Biol Crystallogr 2010, 66 (Pt 4), 486–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (51).Liebschner D; Afonine PV; Baker ML; Bunkoczi G; Chen VB; Croll TI; Hintze B; Hung LW; Jain S; McCoy AJ; Moriarty NW; Oeffner RD; Poon BK; Prisant MG; Read RJ; Richardson JS; Richardson DC; Sammito MD; Sobolev OV; Stockwell DH; Terwilliger TC; Urzhumtsev AG; Videau LL; Williams CJ; Adams PD, Macromolecular structure determination using X-rays, neutrons and electrons: recent developments in Phenix. Acta Crystallogr D Struct Biol 2019, 75 (Pt 10), 861–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (52).Jefcoate CR, Measurement of substrate and inhibitor binding to microsomal cytochrome P-450 by optical-difference spectroscopy. Methods Enzymol 1978, 52, 258–79. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


