Summary:
Dorsal nasal augmentation is a common injection associated with ocular complications. Digital compressions on both sides of the nose are recommended during injection. Considering the reported incidences of visual complications, this preventive technique may need an adjustment for more effectiveness to prevent blindness. Therefore, the dorsal nasal arteries (DNAs) were studied by conventional dissections in the subcutaneous and fibromuscular tissues of the nasal dorsum in 60 embalmed cadavers. The results showed that among the 60 faces, 32 faces had bilateral DNAs (53.3%), 23 had dorsal nasal plexus with minute arteries (38.3%), and five had a single dominant DNA (8.3%). The DNA originated from one of the four arterial sources, which influenced the location and course of the artery. These sources included the ophthalmic angular arteries in 21 faces (56.8%), terminal ophthalmic arteries in two faces (5.4%), lateral nasal arteries in 11 faces (29.7%) and facial angular arteries in three faces (8.1%). Consequently, the dominant dorsal nasal artery running close to the midline found in 8% of the cases could make side compressions during nasal dorsum augmentation less effective from preventing ocular complications. However, an adjustment of digital compressions which combines pinching and side compressions is suggested to improve the safety.
INTRODUCTION
Nasal augmentation inherits a great risk of severe ocular complications and fatal cerebral infarction.1–3 These include sudden painful and irreversible vision loss, ophthalmoplegia, and blepharoptosis. Side compressions are usually performed to temporarily occlude both dorsal nasal arteries (DNAs) to prevent ocular complications.1,4,5 Some authors recommended pinching up to prevent filler displacement.5 This recommendation does not emphasize on occlusion of the DNA traveling near the midline. To understand how ocular complications still occur regardless of this preventive maneuver, recognition of the arterial anatomy is needed.
The ophthalmic arteries could be the main nasal blood supply, while the facial artery would supplement blood to one side of the lower nose by 46%.6 Previous studies described the course of the ophthalmic DNA, but variation of the source was not described.7–9 Thus, the origin of the DNA could influence the arterial location and risk of blindness.
MATERIALS AND METHODS
Sixty embalmed cadavers with red latex arterial perfusion were studied for the arterial pattern at the radix. The age of the cadavers ranged between 58 and 84 years. The DNAs in the subcutaneous and fibromuscular tissues of the nasal dorsum8 were observed by conventional layer dissections.
RESULTS
The DNA is the main blood supply of the nasal dorsum traveling in the subcutaneous tissue on the fibromuscular superficial musculoaponeurotic system layer. Among the 60 faces, the DNA was found bilaterally in 32 faces (53.3%), the dorsal nasal plexus with minute arteries in 23 faces (38.3%), and a single dominant DNA in five faces (8.3%) (See figure 1, Supplemental Digital Content 1, which demonstrates two types of the single dominant DNA. http://links.lww.com/PRSGO/B833.) The artery originated from one of the four sources (Table 1). These sources included the ophthalmic angular arteries in 21 faces (56.8%), terminal ophthalmic arteries in two faces (5.4%), lateral nasal arteries in 11 faces (29.7%) and facial angular arteries in three faces (8.1%).
Table 1.
Classification of the DNA in Each Face According to the Origin
| Pattern | No. Faces | Origin (type) | No. Faces | No. Arteries |
|---|---|---|---|---|
| DNA plexus | 23 (38.3%) | |||
| Bilateral DNA | 32 (53.3%) | Ophthalmic angular a (type I) | 18 (48.6%) | 36 (52.2%) |
| Lateral nasal a (type III) | 11 (29.7%) | 22 (31.9%) | ||
| Facial angular a (type IV) | 3 (8.1%) | 6 (8.7%) | ||
| Single dominant DNA | 5 (8.3%) | Ophthalmic angular a (type I) | 3 (8.1%) | 3 (4.3%) |
| Terminal ophthalmic a (type II) | 2 (5.4%) | 2 (2.9%) | ||
| Total | 60 (100%) | 37 (100%) | 69 (100%) |
Different Origins of the DNAs
The DNA type I from the ophthalmic angular artery was the most common type (57%). (See Figure 1A, Supplemental Digital Content 1, http://links.lww.com/PRSGO/B833.) Among these, three faces had a single DNA near the midline. The radix artery rose transversely at the level of the intercanthal line from the ophthalmic angular artery. The radix artery in this typical level of origin ended as a rectangular bifurcation. The artery would bifurcate into the DNA and paracentral artery in the opposite directions. Then, the DNA descended on the side of the nose to anastomose with the lateral nasal artery (LNA). The single dominant DNA usually deviated and crossed the midline at the level of upper lateral cartilage to anastomose with the contralateral LNA.
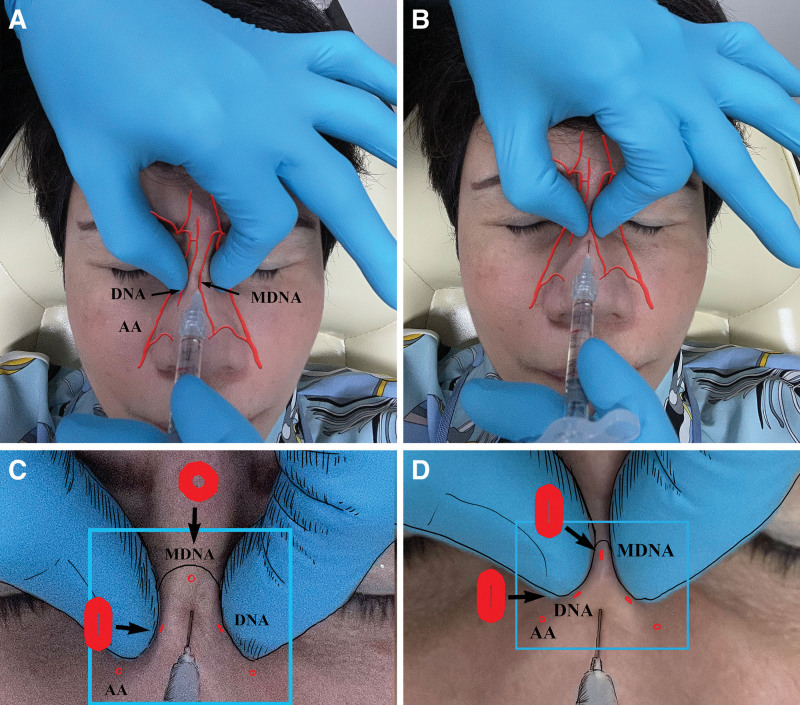
Fig. 1.
Comparison between the common practice of side compressions and the pinching and riding technique. A, Compressions on both sides of the injection can avoid lateral filler displacement and simultaneously compress the DNAs running along the sides of the nasal dorsum (DNA), but do not occlude the DNA traveling near the midline (MDNA). C, Magnification of the cross sections of the DNAs. Side compressions or pinching nasal tissue up cannot compress the dominant DNA traveling near the midline (MDNA). B, pinching and riding technique emphasizes on pinching the nasal dorsum and simultaneously compressing the nasal bone which can occlude all types of DNAs, both the DNAs at the sides of the nose and the one near the midline. D, The injection is not between, but caudal to the compressions. Large red circle illustrates patent DNA near the midline. Large red ellipses demonstrate collapsed DNAs. AA, patent angular artery; MDNA, dorsal nasal artery near the midline.
The DNA type II was a direct branch from the ophthalmic artery above the medial canthus as the “high level of origin” when the angular artery continued from the facial artery (2, 5.4%). (See Figure 1B, Supplemental Digital Content 1, http://links.lww.com/PRSGO/B833.) The dominant DNA could deviate medially or cross the midline.
The ascending or reverse DNA type III could retrogradely ascend from the LNA on one side or both (11, 29.7%).6 The supratip arterial arcade formed by both LNAs could be the low level of origin of the DNA.
The DNA type IV could be divided from the facial angular artery when the ipsilateral ophthalmic artery provided only the frontal branches to the forehead (3, 8.1%). This low level of origin of the DNA could thus be inferior to the medial canthus. Hence, the low levels of origins of the DNA would have a low risk of blindness complications due to the indirect or secondary cannulation.10
DISCUSSION
The dominant DNA was rarely found in one of 12 people (8.3%). However, a direct injection of the DNA can cause severe ocular complications. Compressions should occlude all direct paths connecting the DNA to the ophthalmic artery to prevent direct or primary cannulation.10 Although side compressions could occlude the DNA from typical level of origin (Fig. 1A, C), they leave the potential for injection into the single dominant DNA that passes between the compression points from the ophthalmic artery. The possibility of encountering an aberrant dorsal nasal artery implies that an adjustment is needed to occlude the artery near the midline.
Although this technique is not clinically verified, we suggest an adjustment of pinching the skin and riding the nasal bone rostral to the injection point instead of side compressions (Fig. 1B, D). Pinching can occlude the dominant DNA and riding the bone can occlude the normal DNA.
Compression Techniques to Prevent Ocular Complications
For a fronto-glabellar injection, bilateral orbito-glabellar compressions at the nasal corners of the supraorbital rims can block all ophthalmic branches, preventing filler emboli to the eyes. Side compressions during radix augmentation are sufficient to improve safety and prevent filler emboli through the radix arteries. Pinching the nasal skin and pressing it against the nasal bone would occlude both the lateral and dorsal lying DNAs during dorsal nasal augmentation. (See Figure 2, Supplemental Digital Content 2, which demonstrates ultrasound imaging to monitor the dorsal nasal artery during pinching and riding technique. http://links.lww.com/PRSGO/B834.) The skin puncture is on the caudal side of the skinfold created by pinching. A needle angle of 45 degrees would facilitate accurate injection and mitigate the chance of sharp tip bending. Nasal tip refinement needs pinching after the needle is verified at the superficial subcutaneous tissue, and a small aliquot is needed for blanching the nasal tip skin. Previous known techniques that are essential and might minimize the risk of intra-arterial injection are use of vasoconstrictive agents, topical cooling, use of blunt injection cannulas, and delivery of filler agent at low pressure on withdrawal of the needle.
CONCLUSION
A dominant dorsal nasal artery close to the midline would make side compressions during nasal dorsum augmentation ineffective to prevent ocular complications.
ACKNOWLEDGMENT
This research was supported by the Ratchadapiseksompotch Fund, Faculty of Medicine, Chulalongkorn University, grant number RA63/038. The authors express their sincere gratitude to Mr. Pattarapol Rajitvanit, Scientist, Faculty of Medicine, Siam University for preparing the earlier draft of this article.
PATIENT CONSENT
The patient provided written consent for the use of her image.
Supplementary Material
Footnotes
Published online 16 November 2021.
Disclosure: The authors have no financial interest in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Lee W, Koh IS, Oh W, et al. Ocular complications of soft tissue filler injections: a review of literature. J Cosmet Dermatol. 2020;19:772–781. [DOI] [PubMed] [Google Scholar]
- 2.Thanasarnaksorn W, Cotofana S, Rudolph C, et al. Severe vision loss caused by cosmetic filler augmentation: case series with review of cause and therapy. J Cosmet Dermatol. 2018;17:712–718. [DOI] [PubMed] [Google Scholar]
- 3.Yang Q, Lu B, Guo N, et al. Fatal cerebral infarction and ophthalmic artery occlusion after nasal augmentation with hyaluronic acid—A case report and review of literature. Aesthetic Plast Surg. 2020;44:543–548. [DOI] [PubMed] [Google Scholar]
- 4.Scheuer JF, III, Sieber DA, Pezeshk RA, et al. Facial danger zones: techniques to maximize safety during soft-tissue filler injections. Plast Reconstr Surg. 2017;139:1103–1108. [DOI] [PubMed] [Google Scholar]
- 5.Bertossi D, Lanaro L, Dorelan S, et al. Nonsurgical rhinoplasty: nasal grid analysis and nasal injecting protocol. Plast Reconstr Surg. 2019;143:428–439. [DOI] [PubMed] [Google Scholar]
- 6.Cai B, Yuan R, Zhu GZ, et al. Deployment of the ophthalmic and facial angiosomes in the upper nose overlaying the nasal bones. Aesthet Surg J. 2021. [E-pub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 7.Tansatit T, Apinuntrum P, Phetudom T. Facing the worst risk: confronting the dorsal nasal artery, implication for non-surgical procedures of nasal augmentation. Aesthetic Plast Surg. 2017;41:191–198. [DOI] [PubMed] [Google Scholar]
- 8.Choi DY, Bae JH, Youn KH, et al. Topography of the dorsal nasal artery and its clinical implications for augmentation of the dorsum of the nose. J Cosmet Dermatol. 2018;17:637–642. [DOI] [PubMed] [Google Scholar]
- 9.Tansatit T, Phumyoo T, Jitaree B, et al. Anatomical and ultrasound-based injections for sunken upper eyelid correction. J Cosmet Dermatol. 2020;19:346–352. [DOI] [PubMed] [Google Scholar]
- 10.Tansatit T, Phumyoo T, Jitaree B, et al. Commentary on: Deployment of the ophthalmic and facial angiosomes in the upper nose overlaying the nasal bones. Aesthet Surg J. 2021. [E-pub ahead of print.] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.