Abstract
Climatic variability affects many underlying determinants of child malnutrition, including food availability, access, and utilization. Evidence of the effects of changing temperatures and precipitation on children’s nutritional status nonetheless remains limited. Research addressing this knowledge gap is merited given the short- and long-run consequences of malnutrition. We address this issue by estimating the effects of temperature and precipitation anomalies on the weight and wasting status of children ages 0–59 months across 16 countries in sub-Saharan Africa. Linear regression models show that high temperatures and low precipitation are associated with reductions in child weight, and that high temperatures also lead to increased risk of wasting. We find little evidence of substantively meaningful differences in these effects across sub-populations of interest. Our results underscore the vulnerability of young children to climatic variability and its second-order economic and epidemiological effects. The study also highlights the corresponding need to design and assess interventions to effectively mitigate these impacts.
Keywords: climate variability, wasting, weight-for-height, child malnutrition, Sub-Saharan Africa, vulnerability
1. Introduction
Changing temperature and precipitation patterns associated with climate change are expected to disrupt food systems across the world through impacts on agricultural production, as well as on the health and socioeconomic status of agricultural laborers and consumers (Bosello et al. 2006; Dell et al. 2012; McMichael et al. 2006; Myers et al. 2017; Nelson et al. 2014). Such impacts have clear implications for food security, as they will affect the availability of food and households’ ability to access and fully utilize food for adequate nutrition (Barrett 2010; Wheeler & Von Braun 2013). One relatively understudied implication is that climatic variability and its second-order effects are likely to affect levels and patterns of malnutrition (Phalkey et al. 2015). These impacts are anticipated to be concentrated among children, who are especially vulnerable to food and nutritional insecurity. Malnutrition may increase children’s risk of other morbidities and mortality (Pelletier et al. 1995), and malnutrition during early childhood can permanently diminish individuals’ health and socioeconomic attainment over the life course (Alderman et al. 2006; Currie & Vogl 2013; Maccini & Yang 2009; Van den Berg et al. 2009). Unmitigated exposure to climate variability among children may have residual health and social costs decades into the future.
We contribute to the emerging climate-nutrition literature by analyzing the respective effects of temperature and precipitation anomalies on child weight-for-height (WHZ) and wasting (WHZ < −2) across a sample from 16 countries in sub-Saharan Africa. Using data from the Demographic and Health Surveys (DHS), combined with historical climate records from the University of East Anglia’s Climate Research Unit Time Series (Boyle et al. 2018; Harris et al. 2014), we estimate a series of multivariate regression models to address two overarching objectives. First, we estimate the association between recent exposure to climatic variability and children’s weight, measured both continuously and as a binary indicator of low weight (i.e., wasting). Second, we test for systematic variation in these effects across socioeconomic groups that we expect to be differentially vulnerable to changing environmental conditions. We focus this second set of analyses on wasting since the health and social costs of such acute malnutrition are high. Our analyses reveal that exposure to high temperatures is associated with reductions in WHZ and corresponding increases in the prevalence of wasting. The overall direction of temperature effects on wasting are remarkably similar across multiple sub-populations of interest, with only modest differences between rural and urban populations. Precipitation deficits are associated with reduced WHZ, but these changes do not translate into increased wasting risk. Together, our findings underline the need to develop evidence-based interventions to protect children from the health effects of environmental change.
2. Climatic Variability and Nutritional Security
Changes in temperatures, precipitation, and the second-order effects of such environmental changes are expected to affect child malnutrition through multiple pathways. All three of the major determinants of food and nutritional security—availability, access, and utilization—are plausibly affected by climatic variability. Climate impacts on the production, and thus availability, of food have been posited to be particularly important and have received the most attention to date (Grace et al. 2012; Myers et al. 2017). Shifts in both temperatures and precipitation can affect crop yields and production. High temperatures and low precipitation are associated with reductions in the output of many crops and corresponding changes in local and regional food supplies (Nelson et al. 2014; Schlenker & Roberts 2009). These impacts may occur directly (e.g., via heat stress) or indirectly (e.g., via changing the prevalence and distribution of pests and crop diseases) (Thornton et al. 2014). There is also evidence that climatic change may affect the quality and number of crops planted by smallholders, thereby changing the nutritional value and diversity of available food (Call et al. 2019; Headey et al. 2019; Myers et al. 2014; Smith & Myers 2018; Tobin et al. 2019). Even if the local availability of food remains sufficient in terms of caloric requirements, the nutrient content of the food supply may not be adequate to maintain a healthy, well-nourished population (e.g., leading to micronutrient deficiencies). The consequences of such changes for food availability are likely to be especially noticeable in low-income agrarian contexts where households are disproportionately dependent on on-farm or local agricultural production for the food they consume (Cohn et al. 2017; Jones and Thornton 2003; Morton 2007).
Even when shifts in agricultural output do not reduce local and regional food availability to critical levels, such changes may affect households’ access to food. Fluctuations in agricultural production due to temperature and precipitation shocks may affect income among food producers and others employed in the agricultural sector; and they may also result in changing food prices for consumers (Brown & Kshirsagar 2015; Kumar et al. 2016; Mueller et al. 2014; Tiwari et al. 2017). As such, these perturbations have the potential to affect households’ ability to access food through market mechanisms, namely changes in food prices and purchasing power. Climatic variability may also affect households’ ability to access food through changes in income that are separate from impacts on crop yields or prices. For example, anomalous temperatures and precipitation may affect employment opportunities outside of the agricultural sector (Mueller et al. 2020). They may also change the capacity or productivity of non-agricultural labor through physiological responses to environmental conditions (Dunne et al. 2013; Dell et al. 2012), with the resulting changes in earnings affecting households’ food access.
Additionally, shifting temperatures and precipitation may affect children’s biological ability to fully utilize the food they consume via impacts on health (Aberman & Tirado 2014; Wheeler & Von Braun 2013). Morbidities including diarrheal illnesses and vector-borne diseases (e.g., malaria, dengue fever, chikungunya) are all major causes of child malnutrition, and have also been shown to be sensitive to changing environmental conditions (Bandyopadhyay et al. 2012; Caminade & Jones 2016; Kolstad & Johansson 2010; Mordecai et al. 2020). Environment-induced changes in adult health may also filter down to affect the well-being of younger household members by reducing the resources and time allocated to childcare (Lohmann & Lechtenfeld 2015; Mueller & Gray 2018; Pailler & Tsaneva 2018). These scenarios demonstrate that climatic variability may affect the incidence of child malnutrition even in the absence of changes to food availability and access—and even among populations with only tenuous ties to agricultural production. Such dynamics underline the potential pitfalls of assuming that children in rural, agriculturally-dependent households are necessarily most vulnerable to environmental change.
Given these hypothesized pathways—and corresponding evidence regarding the direction of temperature and precipitation effects on crop yields (Challinor et al. 2014; Schlenker & Roberts 2009), agricultural income (Dunne et al. 2013; Mueller et al. 2014), and disease prevalence (Bandyopadhyay et al. 2012; Caminade & Jones 2016; Singh et al. 2001)—we expect that a warmer and drier climate will generally lead to increased child malnutrition. This expectation is also, in part, supported by prior research that has examined the overall relationship between climatic variability and child nutrition. For example, Hoddinott and Kinsey (2001) find that young children exposed to the 1994–1995 drought in Zimbabwe experienced stunted growth (i.e., low height-for-age). Reductions in precipitation or composite measures of drought (e.g., the standardized precipitation-evapotranspiration index) have been found to be associated with low child height in a number of other contexts, including Ethiopia (Randell et al 2020), Kenya (Grace et al. 2012), Mali (Jankowska et al. 2012), across multiple African countries (Davenport et al. 2017), and across the developing world more broadly (Cooper et al. 2019a). A similar health-reducing effect of precipitation deficits has been observed in studies of alternative nutritional outcomes, including weight-for-age, weight-for-height, and infant mortality (Kumar et al. 2016). Many of these same studies also document adverse impacts of high temperatures on child health and nutrition (Davenport et al. 2017; Grace et al. 2012; Randell et al. 2020), which is consistent with other evidence of strong temperature effects on agriculture and human populations (Bohra-Mishra et al. 2014; Mueller et al. 2014; Mueller & Gray 2018).
Although existing evidence generally supports the expectation that hotter and drier conditions will increase child malnutrition, there are reasons to question this assumption. The aforementioned pathways may operate in an offsetting manner. Consider the hypothetical scenario in which a period of above-average precipitation contributes to improvements in nutrition by raising crop yields (thus increasing food availability) and agricultural income (increasing food access), while concurrently leading to increased localized flooding (reducing food availability and access) and the transmission of malnutrition-increasing diseases (reducing food utilization). In this case, the overall change in malnutrition cannot be predicted without a strong prior reason to expect one pathway to dominate another. Indeed, other empirical evidence suggests the opposite of our above-mentioned hypotheses and highlights the complexity of climate-nutrition links (Cooper et al. 2019b; Louis & Hess 2008; Singh et al. 2001; Tiwari et al. 2017). For example, contrary to our expectation that precipitation deficits are associated with poor nutritional outcomes, Cornwell and Inder (2015) find that high precipitation reduces child height in urban Indonesia, likely due to increases in waterborne illnesses. Similarly, Skoufias and Vinha (2012) show that below-average temperatures are associated with reductions in child height in parts of rural Mexico, which runs contrary to expected adverse effects of heat. Tiwari et al. (2017) explicitly underline the complexity of these relationships by showing that an overall positive association between rainfall and child weight in Nepal masks offsetting processes: spells of above-average rainfall are associated with increases in both disease transmission (reducing child health) and crop production (improving child health via increased food availability and agricultural income). The latter effect outweighs the former in this case, resulting in a net weight gain during spells of high precipitation.
Given these considerations, we qualify our expectation that children’s health will suffer most under above-average temperatures and below-average precipitation, and we ultimately consider the strength and direction of climate effects an empirical question. We contribute to the emerging climate-nutrition literature (Andalón et al. 2016; Bandyopadhyay et al. 2012; Davenport et al. 2018; Kumar et al. 2012; Grace et al. 2012; Groppo & Kraehnert 2016; Randell et al. 2020; Thiede & Gray 2020) by analyzing the links between temperature and precipitation variability and child weight across a large population in sub-Saharan Africa. Our study draws new attention to the links between climatic variability and acute malnutrition, employing an analytic framework that accounts for spatial and temporal confounders more rigorously than other multi-national analyses of climate-nutrition linkages in the region. Robust evidence of this relationship is particularly important in sub-Saharan Africa, which is characterized by persistently high levels of food and nutritional insecurity and faces unique vulnerabilities to climate change (FAO 2018).
Our study addresses three specific objectives. First, we estimate the overall relationships between temperature and precipitation exposures and WHZ among children ages 0–59 months. We focus on children’s weight to complement existing evidence on climate and child height in the region (Davenport et al. 2017). Weight is sensitive to recent conditions that can be measured precisely and is often correlated with children’s survival prospects and broader health, including their risk of subsequently experiencing stunted growth (Tiwari et al. 2017; Wells et al. 2019). Second and relatedly, we assess whether temperature and precipitation are significant predictors of acute malnutrition by estimating models of wasting (WHZ < −2). A comparison of these first two analyses allows us to assess where climate effects are concentrated along the weight distribution. These models account for the complex forms the hypothesized relationships may take by testing for non-linearities and interactions between temperature and precipitation variability. Our third objective is to assess whether the association (or lack thereof) between climatic variability and children’s weight varies systematically across sub-populations in our sample defined by sex, number of young coresident children, maternal education, and residence in rural and urban communities. As discussed below, we expect these groups to vary in terms of their vulnerability to climate variability, variously reflecting differences in households’ exposure to the impacts of environmental change and their means of coping with shocks (Watts & Bohle 1993).
3. Data and Methods
3.1. Data
We analyze child anthropometric and socioeconomic data from the Demographic and Health Surveys (DHS), which we access using the Integrated Public Use Microdata Series database (IPUMS-DHS) (Boyle et al. 2018). The DHS program has implemented over 400 nationally-representative household surveys across nearly 100 low- and middle-income countries since the 1980s (DHS Program 2019). DHS data have been used extensively in demographic and public health research on sub-Saharan Africa (Eissler et al. 2019; Eloundou-Enyegue et al. 2017; Miedema et al. 2018) and are considered among the highest-quality population health surveys in the developing world. Importantly for our purposes, the data are collected using a standardized core questionnaire that facilitates harmonization and pooling of samples (Headey 2013; Rieger & Trommlerová 2016). The DHS samples that we use here also include high-resolution geographic identifiers, which are rarely available for such a large population.
We restrict our analytic sample to observations from the available IPUMS-DHS samples from sub-Saharan Africa, and for which (a) anthropometric measures of children ages 0–36 or 0–59 months were collected, (b) the latitude and longitude of DHS clusters (i.e., communities) were made publicly available, and (c) data on mothers’ length of residence in their cluster of enumeration were collected. Cluster-level geocodes allow us to link individual records to high-resolution temperature and precipitation data (see below). Note that the DHS program randomly displaces cluster geocoordinates (0–2 km for urban clusters; and 0–5 km for rural clusters, with 1% of rural clusters displaced 0–10 km) before public release to protect respondent confidentiality. This procedure has the potential to introduce minor and non-systematic noise into our climate measures as described below.
We use information on duration of residence to exclude individuals who were not present in the cluster of enumeration during the entire period that we measure climate anomalies, and who therefore may have been exposed to other unobserved climatic conditions. We limit our sample to children born to mothers who had resided in their cluster of enumeration for at least two years, which corresponds to the length of the maximum period (24 months) used to measure temperature and precipitation exposures in our analyses. By default, our sample also excludes individuals who left the DHS clusters during the period that we measure climate exposure but before the DHS survey was fielded. Although whole-household migration in response to environmental change is relatively rare (Bohra-Mishra et al. 2014; Gray & Mueller 2012), this is nonetheless an unavoidable source of potential bias in our sample. Finally, we exclude observations with biologically implausible WHZ values (> |5|). After these restrictions, our analytic sample includes a total of 182,272 child records from 39 DHS surveys implemented in 16 African countries between 1990 and 2015. Sampling weights are applied to all analyses as recommended by the DHS program. The characteristics of our sample are described in Table 1 and the geographic distribution of the clusters included in the sample is illustrated in Figure 1.
Table 1.
Summary of variables
| Variable | Mean | SD | Min | Max |
|---|---|---|---|---|
| Outcome | ||||
| Weight-for-height z-score | −0.275 | 1.446 | −5 | 5 |
| Wasting (WHZ < −2) | 0.110 | 0.312 | 0 | 1 |
| Climate anomalies, 12 months before survey | ||||
| Temperature | 0.511 | 0.882 | −2.765 | 3.424 |
| Precipitation | −0.189 | 0.814 | −3.192 | 3.181 |
| Control variables | ||||
| Child’s age (months) | 27.185 | 17.001 | 0 | 59 |
| Child’s sex = female | 0.498 | - | 0 | 1 |
| Child’s birth order | 3.971 | 2.486 | 1 | 10 |
| Coresident under-5 children | 0.907 | 1.000 | 0 | 10 |
| Mother’s age (years) | 29.085 | 6.997 | 15 | 49 |
| Mother’s education = primary+ | 0.281 | - | 0 | 1 |
| Residence = urban | 0.215 | - | 0 | 1 |
| Historical monthly temperature, mean | 22.389 | 3.410 | 11.287 | 27.585 |
| Historical monthly temperature, SD | 0.487 | 0.133 | 0.267 | 2.112 |
| Historical monthly precipitation, mean | 969.302 | 384.764 | 48.453 | 2783.602 |
| Historical monthly precipitation, SD | 190.279 | 57.796 | 18.120 | 799.865 |
| Country of residence | ||||
| Benin | 0.030 | - | 0 | 1 |
| Burkina Faso | 0.083 | - | 0 | 1 |
| Cameroon | 0.026 | - | 0 | 1 |
| Cote d’Ivoire | 0.016 | - | 0 | 1 |
| Ethiopia | 0.074 | - | 0 | 1 |
| Ghana | 0.047 | - | 0 | 1 |
| Guinea | 0.013 | - | 0 | 1 |
| Kenya | 0.047 | - | 0 | 1 |
| Madagascar | 0.015 | - | 0 | 1 |
| Malawi | 0.103 | - | 0 | 1 |
| Mali | 0.128 | - | 0 | 1 |
| Niger | 0.042 | - | 0 | 1 |
| Nigeria | 0.143 | - | 0 | 1 |
| Rwanda | 0.018 | - | 0 | 1 |
| Tanzania | 0.055 | - | 0 | 1 |
| Uganda | 0.032 | - | 0 | 1 |
| Zambia | 0.074 | - | 0 | 1 |
| Zimbabwe | 0.055 | - | 0 | 1 |
| Decade of interview | ||||
| 1990s | 0.234 | - | 0 | 1 |
| 2000s | 0.626 | - | 0 | 1 |
| 2010s | 0.140 | - | 0 | 1 |
| Sample size | 182,272 | |||
Weighted descriptive statistics. Historical climate variables measured at the cluster level. Distribution by country shown for illustrative purposes only. Multivariate models also control for interview month (ranked by mean precipitation) and province (subnational level-1 unit) of residence.
Figure 1.
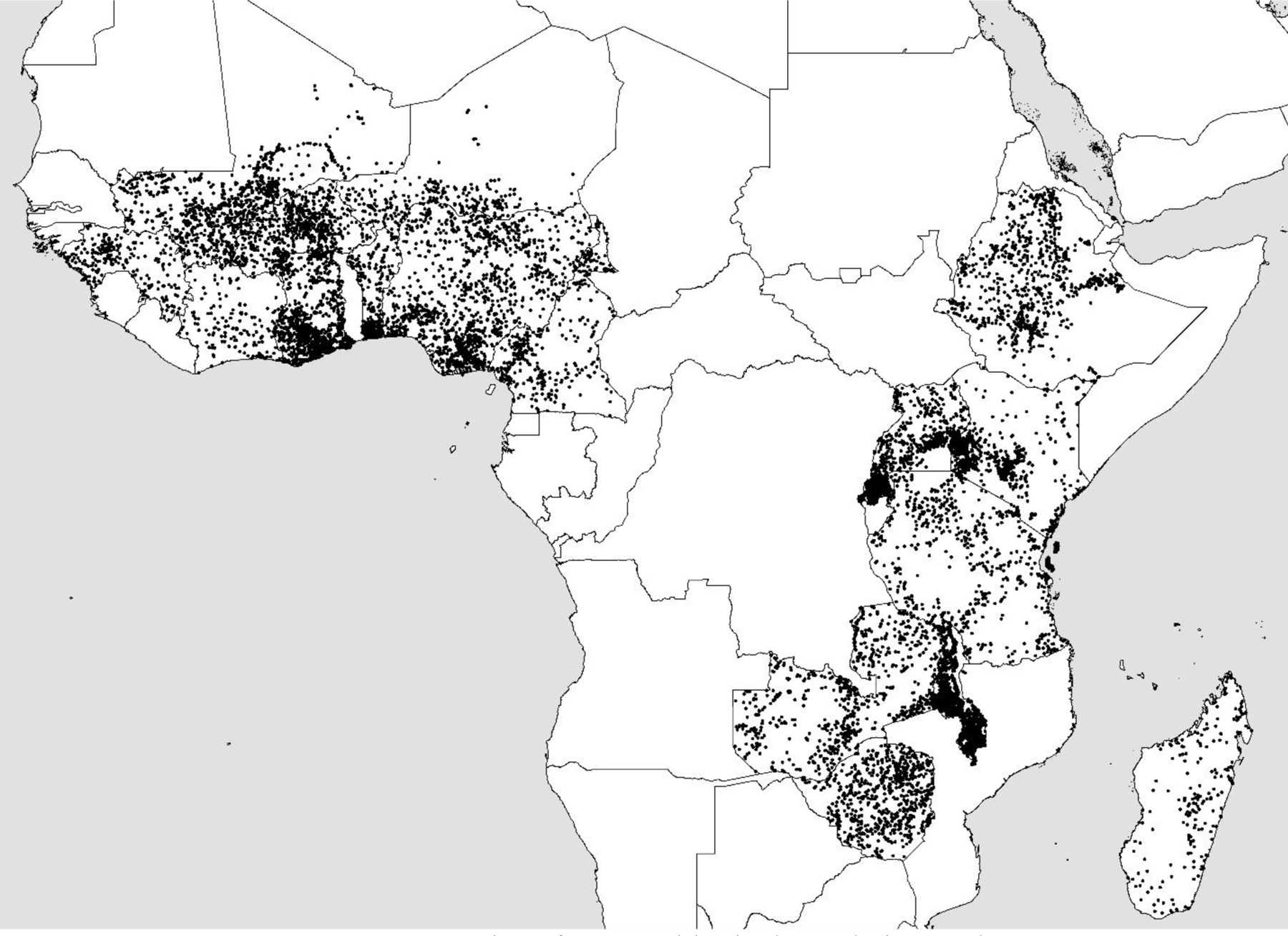
Location of communities in the analytic sample
We measure climate variability using data from the University of East Anglia Climate Research Unit’s Time Series (CRU TS). CRU TS is a global dataset of monthly weather conditions (Harris et al. 2014) and has been used widely in population-environment research (Call et al. 2019; Eissler et al. 2019; Gray & Wise 2016; Randell & Gray 2019). The CRU TS data are constructed at 0.5° resolution and are based on statistical interpolations of data from over 4,000 weather stations. We extract temperature and precipitation records from 1951 through 2015 for the grid cell that each DHS cluster falls in and calculate temperature and precipitation anomalies as described below. Measurement error associated with the random displacement of DHS geocodes (described above) should not be systematic.
3.2. Measures
The dependent variables are WHZ and wasting (WHZ < −2), with z-scores calculated using World Health Organization (WHO) standards (Boyle et al. 2018; World Health Organization 2006). A child’s standardized weight reflects their recent health and nutritional status. Low average WHZ across a population is often associated with increased prevalence of wasting, or acute malnutrition. Wasting is associated with a range of negative outcomes, including increased risk of chronic undernutrition, other morbidities, and mortality (Pelletier et al. 1995; Richard et al. 2012; Schoenbuchner et al. 2019; Wells et al. 2019). Children who experience repeated acute malnutrition early in life may also face developmental deficits and correlated socioeconomic disadvantages that persist into and through adulthood (Alderman et al. 2006; Martorell et al. 2009). As such, the prevalence of wasting has implications for human development both immediately and over the long run as exposed children progress through the life course.
Our independent variables of interest are temperature and precipitation anomalies, which capture deviations from the long-term average conditions within each community in the sample. These variables are respectively measured as the mean temperature and total precipitation observed for a given cluster during the 12 months prior to each DHS survey, standardized over all consecutive 12-month periods in our entire climate history for that location. For instance, our precipitation variable can be interpreted as the standardized deviation (z-score) of precipitation in community c during the 12-month period t and in reference to the long-term mean and standard deviation of precipitation in that community for all 12-month periods from 1951–2015. The temperature variable can be interpreted in an analogous manner. This approach is consistent with prior work on the demographic impacts of short-term climatic variability (Gray & Wise 2016; Mueller et al. 2014; Nawrotzski et al. 2017). Like our study, this prior research assesses the impacts of historical climatic variability to inform expectations about the consequences of ongoing and future anthropogenic climate change.
We illustrate the temporal sequence over which the outcome and predictor variables are measured in Figure 2. This figure illustrates a highly-stylized example in which we assume the DHS interview occurred at the midpoint of year t—the average survey date assuming a uniform intra-year distribution—and in a location with a single agricultural season that runs across the second half of the calendar year (which is not always the case, see e.g., Randell et al. 2020). Consistent with other studies of climate and WHZ (e.g., Thiede & Gray 2020; Tiwari et al. 2016), we focus on environmental conditions within the past year. Such a 12-month window is appropriate given the acute nature of thinness (low WHZ), which is generated by short-term processes relative to chronic malnutrition. We acknowledge that an exposure window of this length may exclude lagged impacts. For example, temperature-induced declines in crop yields may not result in food insecurity until many months after harvests, when households face declining food supplies earlier in the year than usual (i.e., a lengthened “hungry season”, Anderson et al. 2018; Miller 2017). On the other hand, a longer exposure window (e.g., 24+ months) would not allow us to detect cases in which environmental conditions early in the period lead to immediate but temporary reductions in weight. For example, a child may recover from non-lagged impacts of a shock during year t-2 before the interview occurred in calendar year t. Given reasonable arguments for slightly shorter or longer exposure intervals, we compare our main findings with the results of supplemental models using 18- and 24-month intervals (reported below and in the Supplemental Information, SI).
Figure 2.
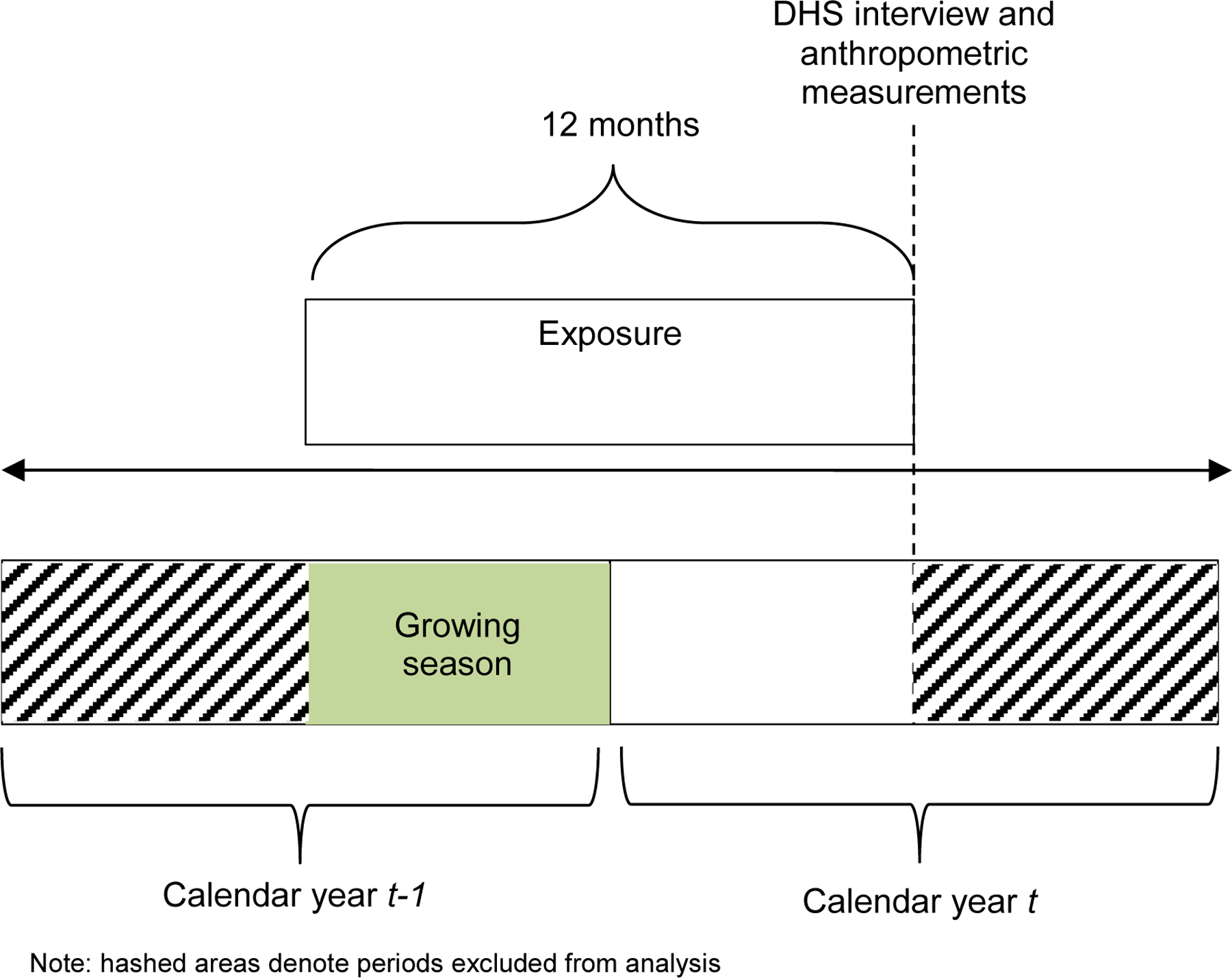
Stylized timeline of data collection, measurement, and climate exposures under hypothetical assumption of a mid-year interview date and July-December growing season
3.3. Statistical Models
We evaluate the effects of temperature and precipitation variability on children’s weight and wasting status by estimating a series of linear regression models in which the WHZ or wasting status of child i is a function of temperature and precipitation anomalies in cluster c during the 12 months prior to the survey, exogenous child and maternal characteristics measured at the time of the survey, and the historical climate in cluster c. We also control for the season of the survey month (see below) and include both province and decade fixed effects. The set of control variables includes child age (in months and allowing for non-linearities), sex, birth order, and number of coresident under-five children; maternal age and primary school attainment; the rural (urban) status of the household’s cluster of residence; and the historical climate of the cluster of residence as measured by the respective means and standard deviations of temperature and precipitation across our entire climate history. These variables may be correlated with child malnutrition (Behrman & Skoufias 2004; Fotso 2007; Rieger & Trommlerová 2016), and their inclusion in the models increases the precision of our estimates since climate exposures cannot be assumed to be truly randomized. Among possible controls, we include only child and maternal characteristics that are fixed prior to child i’s birth or independent of recent climate (e.g., age) to ensure these variables are not themselves affected by the temperature and precipitation anomalies of interest.
In addition to the control variables described above, we include a series of fixed effects to control for spatial and temporal confounders. We control for the season of the survey month by including a set of indicator variables capturing that month’s rank within the historical rainfall distribution of the cluster of enumeration (1 = historically-driest month in cluster c, 12 = historically-wettest month in cluster c). This approach allows us to control for baseline seasonality while allowing for spatial variation in such patterns. Survey decade fixed effects control for all decade-on-decade changes across the entire sample and thereby help to reduce the risk that the analysis is confounded by unobserved factors correlated with the secular changes in temperature, precipitation, and WHZ over the study period. Finally, province fixed effects control for all unobserved province-level factors so long as they are time invariant. Standard errors are clustered on the DHS enumeration areas (n=14,934) since this is the level at which our exposure variables are measured (Abadie et al. 2017).
In addition to estimating the average effects of temperature and precipitation anomalies on WHZ and wasting across the sample, we test for variation in climate effects on wasting across select sub-populations. We estimate a sequence of four models that include interactions between the primary measures of climate exposure and group identifiers. These models respectively include interactions with measures of child sex (male versus female), number of coresident under-five children, maternal educational attainment (< primary versus ≥ primary), and rural (versus urban) residence. The models take the same general form as described above but are inclusive of these interaction terms.
4. Results
4.1. Overall Estimates
We begin by estimating the average effects of climatic variability on children’s weight and wasting status across our target population. Given the possibility that the most significant impacts will occur at the extremes of the temperature and precipitation distributions, we conduct a series of preliminary analyses to test for non-linearities in, and interactions between, temperature and precipitation. We estimate models that include only linear temperature and precipitation terms (Model S1 and S2, Table S1 in the SI), models that include quadratic temperature and precipitation terms (Models 1 and 2, Table 2), and models that include quadratic climate terms and a temperature-by-precipitation interaction (Models S3 and S4, Table S2). After evaluating these models, our preferred specification allows the effects of temperature and precipitation to operate non-linearly but excludes the temperature-by-precipitation interaction, which is not statistically or substantively significant.
Table 2.
Coefficient estimates, linear regression model predicting weight-for-height z-score (Model 1) and wasting (Model 2)
| Variable | Model 1 (WHZ) |
Model 2 (Wasting) |
||
|---|---|---|---|---|
| Climate anomalies, 12 months before survey | ||||
| Temperature | −0.0226 | ** | 0.0105 | *** |
| Temperature2 | 0.0070 | −0.0031 | ** | |
| Precipitation | 0.0328 | *** | 0.0035 | ** |
| Precipitation2 | −0.0188 | ** | 0.0016 | |
| Control variables | ||||
| Child’s age (months) | 0.0078 | *** | −0.0039 | *** |
| Child’s age2 (months) | 0.0000 | 0.0000 | *** | |
| Child’s sex = female | 0.0356 | *** | −0.0147 | *** |
| Child’s birth order | −0.0088 | ** | 0.0011 | † |
| Coresident under-5 children | 0.0057 | −0.0010 | ||
| Mother’s age (years) | 0.0002 | 0.0002 | ||
| Mother’s education = primary+ | 0.1023 | *** | −0.0178 | *** |
| Residence = urban | 0.0725 | *** | −0.0181 | *** |
| Historical monthly temperature, mean | −0.0516 | *** | 0.0053 | *** |
| Historical monthly temperature, SD | −0.4675 | *** | 0.0900 | ** |
| Historical monthly precipitation, mean | 0.0002 | *** | 0.0000 | ** |
| Historical monthly precipitation, SD | 0.0002 | 0.0000 | ||
| Season of interview month fixed effects | Yes | Yes | ||
| Interview decade fixed effects | Yes | Yes | ||
| Province fixed effects | Yes | Yes | ||
| R2 | 0.0944 | 0.0612 | ||
| Joint test, temperature | † | *** | ||
| Joint test, precipitation | *** | ** | ||
| Joint test, all climate variables | *** | *** | ||
| Sample size | 182,272 | 182,272 | ||
p<0.10
p<0.05
p<0.001
Standard errors clustered at the community level. Historical climate variables measured at the cluster level. Interview month (ordinal) ranked by historical monthly precipitation within cluster. WHZ = weight-for-height z-score.
We begin with the overall model of child weight (Model 1) and find that both temperature and precipitation exposures are statistically significant predictors of WHZ. These relationships are complex given the presence of non-linearities, but in general reveal that both hot and dry spells are associated with reduced WHZ. To understand these patterns, we plot the predicted child weight across a plausible range of temperature (Panel a) and precipitation (Panel b) anomalies, holding all other variables at their means (Figure 3). According to our estimates, an increase in temperatures from average to two standard deviations above average is associated with a reduction in predicted WHZ of 6.7 percent, from −0.252 to −0.269. An equivalent two standard deviation decline in precipitation is associated with an even larger 35.6 percent reduction in predicted weight, which falls to −0.396 when precipitation is z = −2.
Figure 3.
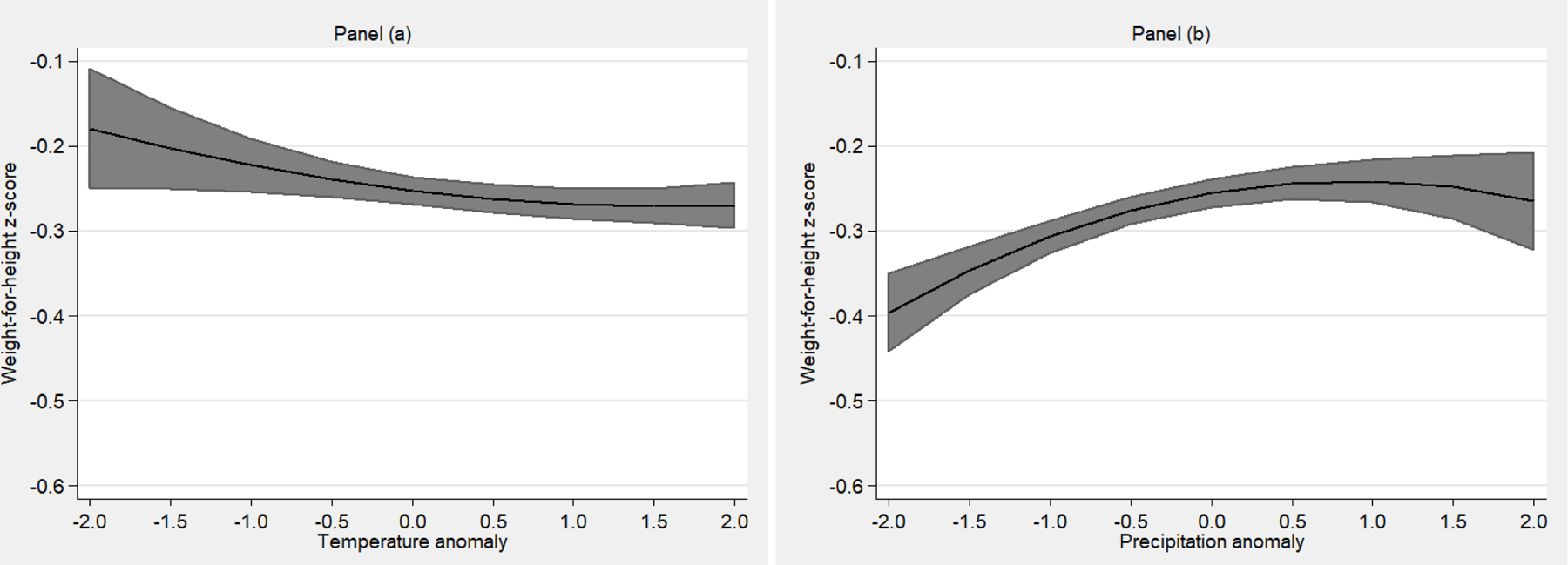
Predicted weight-for-height z-score by (a) temperature and (b) precipitation exposure
We next estimate a similarly specified model of wasting (Model 2) to assess whether climate-induced reductions in WHZ correspond to increases in the prevalence of acute malnutrition. Alternatively, climate effects may be concentrated away from the lower end of the weight distribution, such that declines in average weight do not manifest in additional wasting. Such dynamics may differ for precipitation and temperature if each influences child weight through a unique mechanism(s). Our results suggest that the observed temperature-induced declines in WHZ do indeed lead to higher wasting probabilities (illustrated in Figure 4). For instance, the predicted probability of wasting increases by approximately 8.1 percent (from 9.9 to 10.7%) as temperatures increase two standard deviations over the baseline average. Surprisingly, we do not find evidence of a similar pattern with respect to precipitation effects. While the first model of WHZ showed large reductions in child weight during spells of low precipitation, the results of the second model suggest that wasting is most common during spells of excess rainfall. The magnitude of estimated precipitation effects on wasting is modest and substantively less meaningful than comparable temperature effects. These conclusions are confirmed by a supplemental model in which wasting is estimated using logistic regression (Model S5, Table S2). The results reveal substantively similar temperature effects, but we do not detect a statistically significant association between precipitation and wasting in this model.
Figure 4.
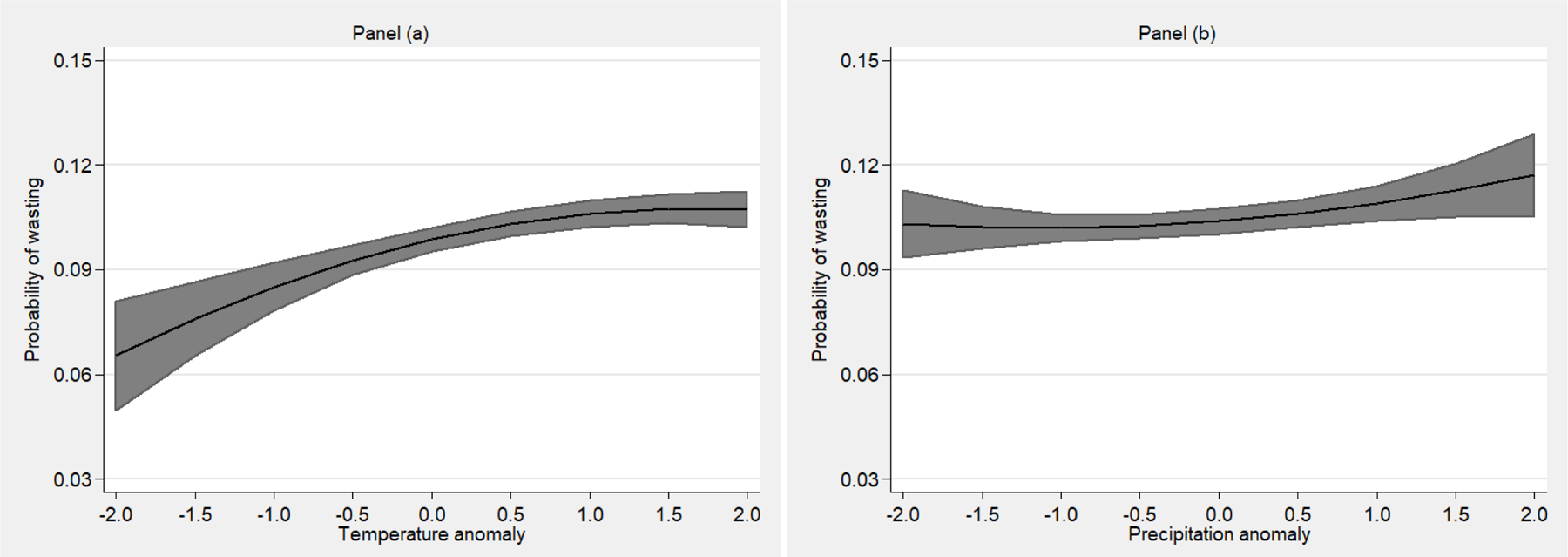
Predicted probability of wasting by (a) temperature and (b) precipitation exposure
4.2. Variation in Climate Effects
We next test for variation in climate effects across major demographic groups (Table 3), which we expect to differ in their vulnerability to climate shocks (Bohle et al. 1994; Deressa et al. 2009; Morton 2007). Given the health and social costs of acute malnutrition, we focus this set of analyses on wasting rather than WHZ in general. The first two interaction models respectively compare climate effects between male and female children (Model 3) and according to the number of coresident under-five children (Model 4). The associations between temperature, precipitation, and wasting may vary by children’s sex or the number of other young children in the household if gender discrimination or resource constraints influence the measures parents take to protect children from the adverse effects of climatic variability (e.g., allocation of food, clean water, healthcare) (Block et al. 2004; Lloyd & Desai 1992; Tiwari et al. 2017). We find no evidence of sex differentiation in climate effects on wasting (Model 3), and the effects of temperature do not vary significantly according to the number of coresident young children (Model 4). We do observe statistically significant differences in the association between precipitation exposures and wasting according to the number of young children in the household. However, the substantive significance of this finding is limited. The effects of precipitation remain non-significant across the range of plausible precipitation anomalies for all but the most crowded households in our sample. For the latter, the marginal effect of precipitation is only non-zero within a narrow range of precipitation anomalies (i.e., between −1 and 0).
Table 3.
Coefficient estimates, linear regression models predicting wasting
| Variable | Model 3 | Model 4 | Model 5 | Model 6 | ||||
|---|---|---|---|---|---|---|---|---|
| Climate anomalies, 12 months before survey | ||||||||
| Temperature | 0.0116 | *** | 0.0099 | *** | 0.0113 | *** | 0.0093 | *** |
| Temperature2 | −0.0035 | ** | −0.0035 | ** | −0.0032 | ** | −0.0025 | ** |
| Precipitation | 0.0031 | 0.0001 | 0.0022 | 0.0033 | † | |||
| Precipitation2 | 0.0024 | 0.0025 | 0.0016 | 0.0022 | ||||
| Group × climate anomaly interactions | ||||||||
| Female × temperature | −0.0022 | |||||||
| Female × temperature2 | 0.0009 | |||||||
| Female × precipitation | 0.0008 | |||||||
| Female × precipitation2 | −0.0017 | |||||||
| Coresident under-5 children × temperature | 0.0005 | |||||||
| Coresident under-5 children × temperature2 | 0.0006 | |||||||
| Coresident under-5 children × precipitation | 0.0039 | ** | ||||||
| Coresident under-5 children × precipitation2 | −0.0009 | |||||||
| Mother education (primary+) × temperature | −0.0046 | |||||||
| Mother education (primary+) × temperature2 | 0.0012 | |||||||
| Mother education (primary+) × precipitation | 0.0036 | |||||||
| Mother education (primary+) × precipitation2 | −0.0012 | |||||||
| Residence (urban) × temperature | 0.0076 | ** | ||||||
| Residence (urban) × temperature2 | −0.0041 | ** | ||||||
| Residence (urban) × precipitation | 0.0023 | |||||||
| Residence (urban) × precipitation2 | −0.0025 | |||||||
| Controls | Yes | Yes | Yes | Yes | ||||
| Season of interview month fixed effects | Yes | Yes | Yes | Yes | ||||
| Interview decade fixed effects | Yes | Yes | Yes | Yes | ||||
| Province fixed effects | Yes | Yes | Yes | Yes | ||||
| R2 | 0.0612 | 0.0613 | 0.0612 | 0.0612 | ||||
| Joint test, group × temperature interaction | † | |||||||
| Joint test, group × precipitation interaction | *** | |||||||
| Joint test, group × all climate variables interaction | *** | |||||||
| Joint test, temperature | *** | *** | *** | *** | ||||
| Joint test, precipitation | ||||||||
| Joint test, all climate variables | *** | *** | *** | *** | ||||
| Sample size | 182,272 | 182,272 | 182,272 | 182,272 | ||||
p<0.10
p<0.05
p<0.001
Standard errors clustered at the community level. Interview month (ordinal) ranked by historical monthly precipitation within cluster.
We next test for differences in the relationship between climatic variability and the probability of wasting by maternal education (Model 5), distinguishing between children of mothers with and without a primary school education. Maternal education is a broad proxy for socioeconomic status and childcare knowledge (Smith-Greenaway et al. 2012; Ukwauani & Suchindran 2003). As such, we expect better-educated women to reside in households that are less exposed to the effects of climatic variability, both physically and with respect to the impacts of climate on household members’ employment. We also expect such women to be better equipped to care for their children in the face of adverse conditions. Despite these expectations, our results reveal no statistically significant differences in temperature or precipitation effects according to maternal education.
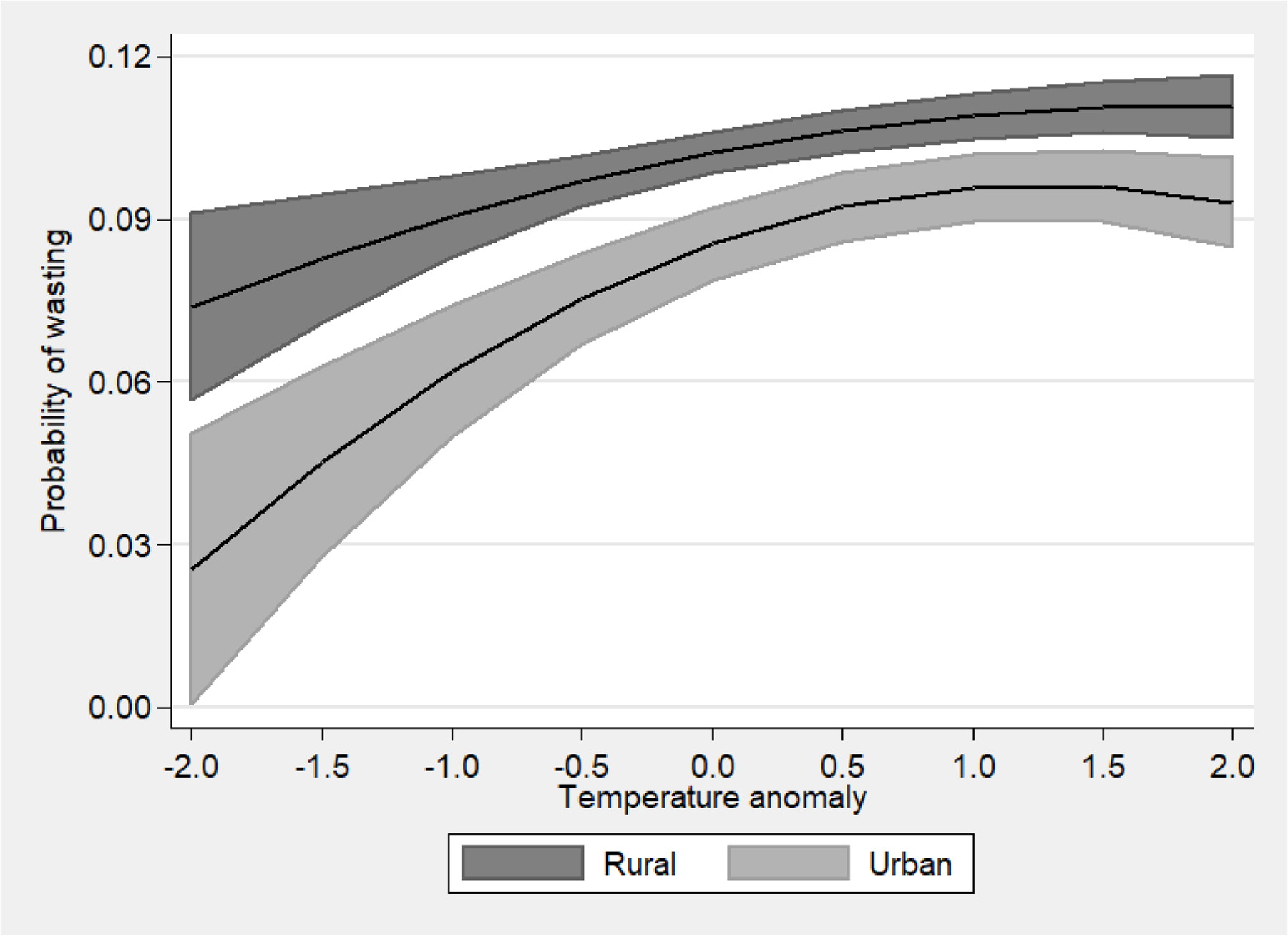
The final interaction model tests for rural-urban differences in the association between climatic variability and wasting (Model 6). Rural populations are commonly assumed to be more vulnerable to the effects of climatic variability given their disproportionate reliance on rainfed agriculture and lower levels of wealth to protect against climate impacts (Nawrotzki et al. 2017; Sahn & Stifel 2003). However, such hypothesized differences may be overstated given urban populations’ vulnerability to climate-induced changes in food prices, in the prevalence of malnutrition-increasing illnesses, and to heat island effects (Desbureaux & Rodella 2019; Headey & Martin 2016). Many urban households in Africa also retain close ties to rural areas through migration and other exchanges of resources and persons, thereby blurring rural-urban boundaries (Eloundou-Enyegue & Stokes 2002). The estimates from Model 6 show statistically significant differences in the magnitude of temperature (but not precipitation) effects between rural and urban populations. To assist with the interpretation of these estimates, we plot the predicted probability of wasting for each group across a range of temperatures, holding all other values at their means (Figure 5). This figure—and additional analysis of corresponding marginal temperature effects—demonstrates that urban children experience greater reductions in wasting risk than their rural peers as temperatures fall below average. Temperature effects are largely indistinguishable as temperatures move above average and lead to an increased probability of wasting. The implication is that rural and urban children face quantitatively similar health risks from rising temperatures, but urban children benefit from lower-than-average temperatures more than their rural counterparts.
Figure 5.
Predicted probability of wasting by temperature exposure and rural (urban) residence
4.3. Sensitivity Analyses
As a final objective, we estimate a series of models to ensure our main findings are not driven by key methodological decisions. We summarize the results of these sensitivity analyses here and include the full results in the SI. First, we estimate an additional model that includes categorical indicators of climate shocks to confirm that our conclusions about the respective effects of high and low temperatures and precipitation are not driven by the structure we impose on the model via quadratic climate terms. Shocks are defined as when temperature and precipitation are one standard deviation above or below the long-term mean. The results (Model MS6, Table S3) confirm that above-average temperatures and precipitation are each associated with increased risk of wasting, below-average temperatures are associated with lower wasting risk, and low precipitation is not a significant predictor of wasting.
Next, we re-estimate three alternative versions of our main model (all results in Table S3). First, we flexibly control for child age by including a series of age-in-month indicator variables (Model S7). Second, we restrict the analytic sample to children ages 0–35 months (Model S8). We thereby exclude the 36- to 59-month-old children who are observed in only some of the DHS samples that we include in the main analysis and focus on the ages at which most wasting occurs (Alderman & Headey 2018). Third, we restrict the sample to observations from 2009 and earlier since a declining number of weather stations over the study period may affect the quality of the most recent CRU TS data (Model S9). All three of these alternative models support our substantive conclusions about temperature effects on wasting. The joint effect of the precipitation variables is only statistically significant in the last of these models, which provides further reason to interpret the precipitation effects detected in Model 2 with caution.
For the final sensitivity analysis of note (Table S4), we re-estimate the main model using slightly longer windows of 18 months (Model S10) and 24 months (Model S11) to measure climate exposures. The results of both alternative models reveal substantively similar temperature and precipitation effects as the main model, demonstrating that our overall conclusions are not influenced by the choice among these three defensible exposure periods.
5. Discussion and Conclusion
Our analysis of the links between climatic variability and child weight in 16 African countries suggests that concerns about the nutritional impacts of climate change are well founded. Over the past three decades, temperature and precipitation variability has had substantively important effects on young children’s nutritional status, as indicated by WHZ measurements and the probability of wasting. The first objective of this study was to estimate the overall association between climatic variability and children’s weight, accounting for potential non-linearities in these relationships. Our findings reveal that recent temperate and precipitation exposures are both significant predictors of WHZ, with above-average temperatures and below-average precipitation each associated with reduced weight. These findings are consistent with multiple prior studies of climate variability and child nutrition, including evidence that higher temperatures are associated with reduced height and weight (Blom et al. 2019; Randell et al. 2020) and that precipitation is positively associated with these outcomes (Grace et al. 2012; Kumar et al. 2016; Randell et al. 2012; Tiwari et al. 2017). However, our results are less consistent with other studies that document more complex relationships between climate and health. For example, Cooper et al. (2019a) show that the relationship between precipitation and stunting follows an inverted-U-shaped pattern across a large sample from more than 50 counties; Skoufias and Vinha (2012) show that excess precipitation reduces child height; and Thiede and Gray (2020) find that changes in precipitation timing, rather than precipitation levels, influences child weight and height. Some prior studies also find null or inconsistent temperature and precipitation effects (Cooper et al. 2019b; Thiede & Gray 2020).
Our second objective was to assess whether climate-induced shifts in WHZ translated into changes in the risk of acute malnutrition, operationalized as wasting status (WHZ < −2). The negative effects of high temperatures on WHZ lead to statistically significant increases in the risk of wasting but precipitation-induced declines in WHZ do not. These differences are particularly notable given that the effects of precipitation deficits on WHZ are larger in magnitude than temperature effects. The implication is that temperature-related declines in WHZ were likely concentrated among children at the lower end of the weight distribution, who were most likely to fall below the WHZ threshold used to define wasting. In contrast, precipitation-induced declines in weight were likely distributed more widely, including among children for whom large declines in weight did not lead to wasting (e.g., from WHZ = 0 to WHZ = −1.5). Such differences imply that precipitation and temperature anomalies may affect weight through different mechanisms. This analysis underlines the need to differentiate changes in average weight from changes in wasting—a principle that should also be applied to studies of child height (stunting). Randell and colleagues’ (2020) study of stunting in Ethiopia provides an excellent example, with explicit comparisons of climate effects on HAZ, stunting, and severe stunting; and Kumar and colleagues (2016) do the same for underweight. Our finding also suggests the need to test for differences in climate effects according to children’s baseline weight (when appropriate panel data are available).
Our final objective was to assess whether these associations varied systematically across sub-populations that we expected to be differentially vulnerable to climate variability and its second-order effects. Despite expectations, we found very little in the way of substantively meaningful differences in climate effects by child sex, number of coresident young children, or maternal education. Our analysis of rural-urban differences revealed that urban children experience significantly larger reductions in wasting risk as temperatures fall below average than their rural peers. However, both groups of children face similar increases in wasting risk during high-temperature spells, which climate change will make increasingly common. The similarity of heat effects among rural and urban children is important given the widespread assumption that rural populations are most vulnerable to environmental change. Our study adds to other recent evidence that this assumption is flawed (Desbureaux & Rodella 2019; Mueller et al. 2020), and that serious attention should be paid to the demographic and health effects of climate variability among urban populations. Rural and urban populations may differ more in the ways they are vulnerable to environmental change than in the magnitude of that vulnerability.
Our findings point to a number of broad conclusions and implications for research and development policy. Foremost, child malnutrition and related health burdens are likely to increase under the hotter climate regimes that will take hold over coming decades as anthropogenic climate change continues. These climatic changes are expected to be particularly dramatic in parts of sub-Saharan Africa where, for example, increases in the global average temperature of 2ºC or 3ºC may translate into disproportionately large increases of 3ºC to 5ºC (James & Washington 2013). Governments, donors, and other development actors will therefore need to meet growing demand for programs to protect against such changes or, if left unprotected, will face increasing health burdens among affected populations. Robust and nuanced understandings of climate-nutrition linkages are needed to develop appropriate interventions to protect against the child health effects of climatic variability and change.
The need for such evidence raises three additional conclusions that stem from this study and its limitations. First, our findings underline the need for continued attention to climate impacts on agriculture, livelihoods, and health, which together determine children’s nutritional status (Wheeler et al. 2013). Rather than assume that climate affects nutrition solely through changes in agricultural production and food availability, research must account for the multiple pathways through which this relationship operates. While some empirical attention to mechanisms has been given in studies of malnutrition outside of the sub-Saharan African context (e.g., Tiwari et al. 2017), much of the existing climate-nutrition literature in the region has used data that are relatively unconducive to identifying causal pathways. Future work should draw on the rich, longitudinal datasets that are available in many countries within the region to assess the mechanisms that have been hypothesized but largely untested. At minimum, future studies of the nutritional impacts of climate should include parallel analyses of outcomes that correspond to hypothesized pathways (e.g., health and income), as has been common in other population-environment research (e.g., Mueller et al. 2014; Mueller et al. 2020; Sellers & Gray 2019).
Second and relatedly, more work is needed to understand the temporal dimensions of climate effects on child health. For one, more attention to the timing of environmental shocks vis-à-vis key agricultural seasons can provide further insight into whether and how climate impacts on agriculture are influencing child health. Additional analysis of the lag (or lack thereof) between climate exposures and outcomes can likewise provide indirect evidence about mechanisms. It may also inform the development or improvement of index-based forecasts of the demand for nutritional interventions. Given the significant spatial variation between and even within countries, such analyses are better suited to geographically limited studies (e.g., Grace et al. 2012; Kumar et al. 2016; Randell et al. 2020; Thiede & Gray 2020) than the multi-national focus of this paper.
Third, more evidence is needed to design and evaluate interventions that can enhance resilience to climatic variability as it relates to children’s health and nutrition. There has been some attention to the ways in which development interventions (e.g., cash transfers) may moderate the effects of climatic variability on population processes in Africa (Mueller et al. 2019), but overall very little evidence is available to design interventions that mitigate the demographic and health impacts of climatic change. The large number of governmental (e.g., Ethiopia’s Productive Safety Net Program) and non-governmental (e.g., GiveDirectly cash transfers) social protection programs being implemented across sub-Saharan Africa provide ample opportunity to conduct such assessments. This line of future research must also give significant attention to the causal pathways through which climate effects operate, since policy interventions must be tailored accordingly.
Given both the short- and long-run consequences of child malnutrition, continued efforts are needed to refine our understanding of whether, how, and why such outcomes are influenced by environmental change. With further attention to the complex set of causal mechanisms that may underlie this relationship, and assessments of whether ongoing interventions mitigate (or amplify) these effects, research can better inform policies and programs that improve nutritional outcomes in the face of ongoing climatic variability.
Supplementary Material
Acknowledgments
A previous version of this paper was presented at the 2017 annual meeting of the Population Association of America (PAA) in Chicago, IL. The authors thank Mark Montgomery for his constructive feedback as a discussant for the PAA session in which the initial version of this paper was presented. The authors acknowledge Matthew Hancock’s helpful editorial assistance and Yosef Bodovski’s programming assistance. Thiede also acknowledges assistance provided by the Population Research Institute at the Pennsylvania State University, which is partly funded through the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2CHD041025). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Thiede’s work was also supported by the USDA National Institute of Food and Agriculture and Multistate Research Project #PEN04623 (Accession #1013257).
Contributor Information
Brian C. Thiede, The Pennsylvania State University.
Johann Strube, The Pennsylvania State University.
References
- Abadie A, Athey S, Imbens GW, & Wooldridge J (2017). “When Should You Adjust Standard Errors for Clustering?” Working Paper No. w24003. National Bureau of Economic Research. [Google Scholar]
- Aberman NL, & Tirado C (2014). Impacts of climate change on food utilization. Pp. 717–724 in Global Environmental Change. Springer Netherlands. [Google Scholar]
- Alderman H, & Headey D (2018). The timing of growth faltering has important implications for observational analyses of the underlying determinants of nutrition outcomes. PloS One, 13(4), e0195904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderman H, Hoddinott J, & Kinsey B (2006). Long term consequences of early childhood malnutrition. Oxford Economic Papers, 58(3), 450–474. [Google Scholar]
- Andalón M, Azevedo JP, Rodríguez-Castelán C, Sanfelice V, & Valderrama-González D (2016). Weather shocks and health at birth in Colombia. World Development, 82, 69–82. [Google Scholar]
- Anderson CL, Reynolds T, Merfeld JD, & Biscaye P (2018). Relating seasonal hunger and prevention and coping strategies: A panel analysis of Malawian farm households. The Journal of Development Studies, 54(10), 1737–1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandyopadhyay S, Kanji S, & Wang L (2012). The impact of rainfall and temperature variation on diarrheal prevalence in Sub-Saharan Africa. Applied Geography, 33, 63–72. [Google Scholar]
- Barrett CB (2010). Measuring food insecurity. Science, 327(5967), 825–828. [DOI] [PubMed] [Google Scholar]
- Behrman JR, & Skoufias E (2004). Correlates and determinants of child anthropometrics in Latin America: background and overview of the symposium. Economics and Human Biology, 2(3), 335–351. [DOI] [PubMed] [Google Scholar]
- Block SA, Kiess L, Webb P, Kosen S, Moench-Pfanner R, Bloem MW, & Timmer CP (2004). Macro shocks and micro outcomes: child nutrition during Indonesia’s crisis. Economics & Human Biology, 2(1), 21–44. [DOI] [PubMed] [Google Scholar]
- Blom S, Ortiz-Bobea A, & Hoddinott J (2019). Temperature & children’s nutrition: Evidence from West Africa. Paper presented at the 2019 Agricultural & Applied Economics Association Annual Meeting, Atlanta, GA, July 21–23. [Google Scholar]
- Bohle HG, Downing TE, & Watts MJ (1994). Climate change and social vulnerability: toward a sociology and geography of food insecurity. Global Environmental Change, 4(1), 37–48. [Google Scholar]
- Bohra-Mishra P, Oppenheimer M, & Hsiang SM (2014). Nonlinear permanent migration response to climatic variations but minimal response to disasters. Proceedings of the National Academy of Sciences, 111(27), 9780–9785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosello F, Roson R, & Tol RS (2006). Economy-wide estimates of the implications of climate change: Human health. Ecological Economics, 58(3), 579–591. [Google Scholar]
- Boyle EH, King M, and Sobek M (2018). IPUMS-Demographic and Health Surveys: Version 5 [dataset]. IPUMS and ICF International. [Google Scholar]
- Brown ME, & Kshirsagar V (2015). Weather and international price shocks on food prices in the developing world. Global Environmental Change, 35, 31–40. [Google Scholar]
- Call M, Gray C, & Jagger P (2019). Smallholder responses to climate anomalies in rural Uganda. World Development, 115, 132–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caminade C, & Jones AE (2016). Epidemiology: Malaria in a warmer West Africa. Nature Climate Change, 6(11), 984. [Google Scholar]
- Carlton EJ, Eisenberg JN, Goldstick J, Cevallos W, Trostle J, & Levy K (2013). Heavy rainfall events and diarrhea incidence: the role of social and environmental factors. American Journal of Epidemiology, 179(3), 344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Challinor AJ, Watson J, Lobell DB, Howden SM, Smith DR, & Chhetri N (2014). A meta-analysis of crop yield under climate change and adaptation. Nature Climate Change, 4(4), 287. [Google Scholar]
- Cohn AS, Newton P, Gil JD, Kuhl L, Samberg L, Ricciardi V, … & Northrop S (2017). Smallholder agriculture and climate change. Annual Review of Environment and Resources, 42, 347–375. [Google Scholar]
- Cooper MW, Brown ME, Hochrainer-Stigler S, Pflug G, McCallum I, Fritz S, … & Zvoleff A (2019a). Mapping the effects of drought on child stunting. Proceedings of the National Academy of Sciences, 116(35), 17219–17224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper M, Brown ME, Azzarri C, & Meinzen-Dick R (2019b). Hunger, nutrition, and precipitation: evidence from Ghana and Bangladesh. Population and Environment, 41(2), 151–208. [Google Scholar]
- Cornwell K, & Inder B (2015). Child health and rainfall in early life. The Journal of Development Studies, 51(7), 865–880. [Google Scholar]
- Currie J, & Vogl T (2013). Early-life health and adult circumstance in developing countries. Annual Review of Economics, 5(1), 1–36. [Google Scholar]
- Davenport F, Grace K, Funk C, & Shukla S (2017). Child health outcomes in sub-Saharan Africa: A comparison of changes in climate and socio-economic factors. Global Environmental Change, 46, 72–87. [Google Scholar]
- Dell M, Jones BF, & Olken BA (2012). Temperature shocks and economic growth: Evidence from the last half century. American Economic Journal: Macroeconomics, 4(3), 66–95. [Google Scholar]
- Deressa TT, Hassan RM, Ringler C, Alemu T, & Yesuf M (2009). Determinants of farmers’ choice of adaptation methods to climate change in the Nile Basin of Ethiopia. Global Environmental Change, 19(2), 248–255. [Google Scholar]
- Desbureaux S, & Rodella AS (2019). Drought in the city: The economic impact of water scarcity in Latin American metropolitan areas. World Development, 114, 13–27. [Google Scholar]
- DHS Program. (2019). The DHS Program: Demographic and Health Surveys. Available at: https://dhsprogram.com/.
- Dunne JP, Stouffer RJ, & John JG (2013). Reductions in labour capacity from heat stress under climate warming. Nature Climate Change, 3(6), 563. [Google Scholar]
- Eissler S, Thiede BC, & Strube J (2019). Climatic variability and changing reproductive goals in Sub-Saharan Africa. Global Environmental Change, 57, 101912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eloundou‐Enyegue PM, & Stokes CS (2002). Will economic crises in Africa weaken rural‐urban ties? Insights from child fosterage trends in Cameroon. Rural Sociology, 67(2), 278–298. [Google Scholar]
- Fotso JC (2007). Urban–rural differentials in child malnutrition: trends and socioeconomic correlates in sub-Saharan Africa. Health & Place, 13(1), 205–223. [DOI] [PubMed] [Google Scholar]
- Grace K, Davenport F, Funk C, & Lerner AM (2012). Child malnutrition and climate in Sub-Saharan Africa: An analysis of recent trends in Kenya. Applied Geography, 35(1–2), 405–413. [Google Scholar]
- Gray C, & Mueller V (2012). Drought and population mobility in rural Ethiopia. World Development, 40(1), 134–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray C, & Wise E (2016). Country-specific effects of climate variability on human migration. Climatic Change, 135(3–4), 555–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groppo V, & Kraehnert K (2016). Extreme weather events and child height: evidence from Mongolia. World Development, 86, 59–78. [Google Scholar]
- Harris IPDJ, Jones PD, Osborn TJ, & Lister DH (2014). Updated high‐resolution grids of monthly climatic observations–the CRU TS3. 10 Dataset. International Journal of Climatology, 34(3), 623–642. [Google Scholar]
- Headey DD (2013). Developmental drivers of nutritional change: a cross-country analysis. World Development, 42, 76–88. [Google Scholar]
- Headey DD, & Martin WJ (2016). The impact of food prices on poverty and food security. Annual Review of Sesource Economics, 8, 329–351. [Google Scholar]
- Headey DD, Hirvonen K, Hoddinott J, & Stifel D (2019). Rural food markets and child nutrition. American Journal of Agricultural Economics, 101(5), 1311–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoddinott J, & Kinsey B (2001). Child growth in the time of drought. Oxford Bulletin of Economics and statistics, 63(4), 409–436. [Google Scholar]
- James R, & Washington R (2013). Changes in African temperature and precipitation associated with degrees of global warming. Climatic Change, 117(4), 859–872. [Google Scholar]
- Jankowska MM, Lopez-Carr D, Funk C, Husak GJ, & Chafe ZA (2012). Climate change and human health: Spatial modeling of water availability, malnutrition, and livelihoods in Mali, Africa. Applied Geography, 33, 4–15. [Google Scholar]
- Jones PG, & Thornton PK (2003). The potential impacts of climate change on maize production in Africa and Latin America in 2055. Global Environmental Change, 13(1), 51–59. [Google Scholar]
- Kolstad EW, & Johansson KA (2010). Uncertainties associated with quantifying climate change impacts on human health: a case study for diarrhea. Environmental Health Perspectives, 119(3), 299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S, Molitor R, & Vollmer S (2016). Drought and early child health in rural India. Population and Development Review, 42(1), 53–68. [Google Scholar]
- Lloyd CB, & Desai S (1992). Children’s living arrangements in developing countries. Population Research and Policy Review, 11(3), 193–216. [Google Scholar]
- Lohmann S, & Lechtenfeld T (2015). The effect of drought on health outcomes and health expenditures in rural Vietnam. World Development, 72, 432–448. [Google Scholar]
- Louis MES, & Hess JJ (2008). Climate change: impacts on and implications for global health. American Journal of Preventive Medicine, 35(5), 527–538. [DOI] [PubMed] [Google Scholar]
- Maccini S, & Yang D (2009). Under the weather: Health, schooling, and economic consequences of early-life rainfall. American Economic Review, 99(3), 1006–26. [DOI] [PubMed] [Google Scholar]
- Martorell R, Melgar P, Maluccio JA, Stein AD, & Rivera JA (2009). The nutrition intervention improved adult human capital and economic productivity. The Journal of Nutrition, 140(2), 411–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael AJ, Woodruff RE, & Hales S (2006). Climate change and human health: present and future risks. The Lancet, 367(9513), 859–869. [DOI] [PubMed] [Google Scholar]
- Miedema SS, Haardörfer R, Girard AW, & Yount KM (2018). Women’s empowerment in East Africa: Development of a cross-country comparable measure. World Development, 110, 453–464. [Google Scholar]
- Miller R (2017). Childhood health and prenatal exposure to seasonal food scarcity in Ethiopia. World Development, 99, 350–376. [Google Scholar]
- Mordecai EA, Ryan SJ, Caldwell JM, Shah MM, & LaBeaud AD (2020). Climate change could shift disease burden from malaria to arboviruses in Africa. The Lancet Planetary Health, 4(9), e416–e423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton JF (2007). The impact of climate change on smallholder and subsistence agriculture. Proceedings of the National Academy of Sciences, 104(50), 19680–19685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller V, & Gray C (2018). Heat and adult health in China. Population and Environment, 40(1), 1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller V, Gray C, & Kosec K (2014). Heat stress increases long-term human migration in rural Pakistan. Nature Climate Change, 4(3), 182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller V, Sheriff G, Dou X, & Gray C (2020). Temporary migration and climate variation in eastern Africa. World Development, 126, 104704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller V, Gray C, Handa S, & Seidenfeld D (2019). Do social protection programs foster short-term and long-term migration adaptation strategies?. Environment and Development Economics, forthcoming. [DOI] [PMC free article] [PubMed]
- Myers SS, Zanobetti A, Kloog I, Huybers P, Leakey AD, Bloom AJ, … & Holbrook NM (2014). Increasing CO2 threatens human nutrition. Nature, 510(7503), 139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nawrotzki RJ, DeWaard J, Bakhtsiyarava M, & Ha JT (2017). Climate shocks and rural-urban migration in Mexico: exploring nonlinearities and thresholds. Climatic Change, 140(2), 243–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson GC, Valin H, Sands RD, Havlík P, Ahammad H, Deryng D, … & Kyle P (2014). Climate change effects on agriculture: Economic responses to biophysical shocks. Proceedings of the National Academy of Sciences, 111(9), 3274–3279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pailler S, & Tsaneva M (2018). The effects of climate variability on psychological well-being in India. World Development, 106, 15–26. [Google Scholar]
- Pelletier DL, Frongillo EA Jr, Schroeder DG, & Habicht JP (1995). The effects of malnutrition on child mortality in developing countries. Bulletin of the World Health Organization, 73(4), 443. [PMC free article] [PubMed] [Google Scholar]
- Phalkey RK, Aranda-Jan C, Marx S, Höfle B, & Sauerborn R (2015). Systematic review of current efforts to quantify the impacts of climate change on undernutrition. Proceedings of the National Academy of Sciences, 112(33), E4522–E4529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randell H, & Gray C (2019). Climate change and educational attainment in the global tropics. Proceedings of the National Academy of Sciences, 116(18), 8840–8845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randell H, Gray C, & Grace K (2020). Stunted from the start: Early life weather conditions and child undernutrition in Ethiopia. Social Science & Medicine, 113234. [DOI] [PMC free article] [PubMed]
- Richard SA, Black RE, Gilman RH, Guerrant RL, Kang G, Lanata CF, … & Checkley W (2012). Wasting is associated with stunting in early childhood. Journal of Nutrition, 142(7), 1291–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rieger M, & Trommlerová SK (2016). Age-specific correlates of child growth. Demography, 53(1), 241–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahn DE, & Stifel DC (2003). Urban–rural inequality in living standards in Africa. Journal of African Economies, 12(4), 564–597. [Google Scholar]
- Schlenker W, & Roberts MJ (2009). Nonlinear temperature effects indicate severe damages to US crop yields under climate change. Proceedings of the National Academy of Sciences, 106(37), 15594–15598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenbuchner SM, Dolan C, Mwangome M, Hall A, Richard SA, Wells JC, … & Moore SE(2019). The relationship between wasting and stunting: a retrospective cohort analysis of longitudinal data in Gambian children from 1976 to 2016. The American Journal of Clinical Nutrition. [DOI] [PMC free article] [PubMed]
- Sellers S, & Gray C (2019). Climate shocks constrain human fertility in Indonesia. World Development, 117, 357–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh RB, Hales S, De Wet N, Raj R, Hearnden M, & Weinstein P (2001). The influence of climate variation and change on diarrheal disease in the Pacific Islands. Environmental Health Perspectives, 109(2), 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skoufias E, & Vinha K (2012). Climate variability and child height in rural Mexico. Economics & Human Biology, 10(1), 54–73. [DOI] [PubMed] [Google Scholar]
- Smith MR, & Myers SS (2018). Impact of anthropogenic CO2 emissions on global human nutrition. Nature Climate Change, 8(9), 834. [Google Scholar]
- Smith-Greenaway E, Leon J, & Baker DP (2012). Understanding the association between maternal education and use of health services in Ghana: exploring the role of health knowledge. Journal of Biosocial Science, 44(6), 733–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiede BC, & Gray C (2020). Climate Exposures and Child Undernutrition: Evidence from Indonesia. Social Science & Medicine, 113298. [DOI] [PMC free article] [PubMed]
- Thornton PK, Ericksen PJ, Herrero M, & Challinor AJ (2014). Climate variability and vulnerability to climate change: a review. Global Change Biology, 20(11), 3313–3328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari S, Jacoby HG, & Skoufias E (2017). Monsoon babies: rainfall shocks and child nutrition in Nepal. Economic Development and Cultural Change, 65(2), 167–188. [Google Scholar]
- Tobin D, Jones K, & Thiede BC (2019). Does crop diversity at the village level influence child nutrition security? Evidence from 11 sub-Saharan African countries. Population and Environment, 41(2), 74–97. [Google Scholar]
- Ukwuani FA, & Suchindran CM (2003). Implications of women’s work for child nutritional status in sub-Saharan Africa: a case study of Nigeria. Social Science & Medicine, 56(10), 2109–2121. [DOI] [PubMed] [Google Scholar]
- Van den Berg GJ, Doblhammer G, & Christensen K (2009). Exogenous determinants of early-life conditions, and mortality later in life. Social Science & Medicine, 68(9), 1591–1598. [DOI] [PubMed] [Google Scholar]
- Watts MJ, & Bohle HG (1993). The space of vulnerability: the causal structure of hunger and famine. Progress in Human Geography, 17(1), 43–67. [Google Scholar]
- Wells JC, Briend A, Boyd EM, Berkely JA, Hall A, Isanaka S, … & Dolan C (2019). Beyond wasted and stunted—a major shift to fight child undernutrition. The Lancet Child & Adolescent Health. [DOI] [PubMed]
- Wheeler T, & Von Braun J (2013). Climate change impacts on global food security. Science, 341(6145), 508–513. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2006). WHO child growth standards: length/height for age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age, methods and development. World Health Organization. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


