Abstract
Introduction:
The aim of the present study is to examine gender identity disparities in different kinds of weight-related health behaviors, including physical activity, participation in physical education at school, and healthy and unhealthy eating habits, and to investigate the relationship between school safety and such behaviors in a sample of transgender and non-transgender students.
Method:
We analyzed a statewide sample of 31,609 students (Mage = 14.04, SD = 1.70; 1.1% transgender). We used multilevel regression models to examine the interactive effects of gender identity and perceptions of school safety on the 4 different outcome variables (physical activity, physical education, healthy and unhealthy eating habits). All models included student- and school-level characteristics as controls.
Results:
Findings indicated that transgender students, when compared to non-transgender students, reported (a) feeling less safe at school; (b) more physical activity, but less participation in physical education at school; and (c) both more healthy as well as unhealthy eating behaviors. Adjusted regression models showed a significant interaction between gender identity and perceived school safety on healthy eating behaviors; simple slopes indicated that transgender students have healthier eating behaviors when the school context is perceived as safe compared to those who perceived the school as less safe.
Conclusions:
School interventions are needed to improve school safety for transgender youth and to reduce gender identity-related disparities in healthy eating and physical activity. Research implications and limitations are discussed.
Keywords: transgender students, school safety, healthy eating behaviors, physical activity, gender identity
Adverse weight-related behaviors, such as poor dietary intake and physical inactivity, are a serious public health concern (Allison, Adlaf, Dwyer, Lysy, & Irving, 2007; Cooper et al., 2000; Pilkington, Powell, & Davis, 2016). A growing number of studies highlight the importance of understanding the development of such behaviors during adolescence in order to reduce their adverse effects on growth, psychosocial development, and physical health (Haines & Neumark-Sztainer, 2006; Nelson, Neumark-Stzainer, Hannan, Sirard, & Story, 2006; Suisman et al. 2014). Lesbian, gay, bisexual and transgender (LGBT) youth are particularly at risk for unhealthy weight-related behaviors due to stressors and challenges related to sexual and gender identity development (Miller & Luk, 2018; Watson, Adjei, Saewyc, Homma, & Goodenow, 2017). Several studies report that LGBT people are less likely to engage in healthy behaviors, such as physical activity (Calzo et al., 2013; Mereish & Poteat, 2015; Shankle, 2013) or healthy eating habits (Cohen & Cribbs, 2017; Rainey, Furman, & Gearhardt, 2018) and more likely to report disordered eating than their non-LGBT counterparts (IOM, 2011; Jones, Haycraft, Murjan, & Arcelus, 2016).
Such findings represent an important step in understanding disparities in health behaviors based on sexual and gender identity. Yet, the research to date has tended to focus on LGBT as a combined group; there is a dearth of research reporting on distinctive weight-related health behaviors among transgender people. Specifically, most studies assessing weight-related health behaviors among LGBT people only include measures related to sexual orientation (i.e. Baiocco, Pistella, Salvati, Ioverno, & Lucidi, 2018; Cohen & Cribbs, 2017; Miller & Luk, 2018; Calzo et al., 2013) or monolithic measures of sexual orientation combined with gender identity (i.e. Brackenridge, Rivers, Gough, & Llewellyn, 2007; Jones et al., 2016; Toomey, McGuire, & Russell, 2012). Only a small number of recent studies separate measures of sexual orientation and gender identity (i.e. Brittain & Dinger, 2017; Kosciw, Greytak, Zongrone, Clark, & Truong, 2018) or use measures specifically related to gender identity (i.e. Jones, Arcelus, Bouman, & Haycraft, 2017; Muchicko, Lepp, & Barkley, 2014; VanKim et al., 2014; see references list for more details).
This paucity of studies is especially concerning given evidence that transgender youth may have greater consciousness regarding their bodies compared to non-transgender youth, including experiencing dissatisfaction with their bodies (Jones et al., 2016; McGuire, Doty, Catalpa, & Ola, 2016; Witcomb et al., 2015). Further, negative school experiences and feeling unsafe are common among transgender students (McGuire, Anderson, Toomey, & Russell, 2010), and may be risk factors for unhealthy weight-related behaviors (Halvarsson-Edlund, Sjödén, & Lunner, 2008; Libbey, Story, Neumark-Sztainer, & Boutelle, 2008).
In the following sections, we review the small body of existing literature on weight-related health behaviors among transgender people. We also include an overview of the research on the school experiences of transgender youth in an effort to understand the potential risk factors for disparities in weight-related behaviors based on gender identity. We then provide results from a multilevel study on the effects of negative school experiences on indicators of weight-related health behaviors among transgender students.
Weight-Related Health Behaviors among Transgender People
Physical activity is an important indicator of weight-related health behaviors and most adolescents are physically active at school (i.e., physical education) as well as outside of school (Gorczynski & Brittain, 2016; Nelson, Lust, Story, & Ehlinger, 2008; Zapata, Bryant, McDermott, & Hefelfinger, 2008). The National Association for Sport and Physical Education & American Heart Association (2010) recommends that schools provide 225 minutes per week for middle and high school students throughout the school year, but individual school districts may choose to exceed the required standards. Physical education classes focus on physical activity, such as running or dancing, as well as health, nutrition, and the value of physical activity throughout one’s life. Physical activity beyond school-mandated physical education includes personal exercise, but could also involve other group activities such as extracurricular sports in community-based clubs and organizations.
Overall, there is evidence that lower levels of physical activity are associated with higher risk for adverse health outcomes, such as coronary heart disease and cancer (Cooper et al., 2000; de Souto Barreto, Cesari, Andrieu, Vellas, & Rolland, 2017; Kubota et al., 2017), as well as poor mental health among youth (Nelson et al., 2008). Despite the crucial health implications, little research has investigated disparities in physical activity based on gender identity (Jones et al., 2017). One study (VanKim et al., 2014) showed that transgender college students (n = 53) engaged in less strenuous forms of physical activity and muscle strengthening exercise than non-transgender counterparts. Another study (Muchicko et al., 2014) found that transgender adults (n = 33) reported significantly less physical activity compared to non-transgender people.
Dietary intake is another indicator of weight-related behaviors. Dietary quality has received considerable attention and is a continuing concern within the field of public health. There is evidence that poor dietary quality across childhood and adolescence is associated with obesity, disordered eating, and diet-related chronic diseases in adulthood (Banfield, Liu, Davis, Chang, & Frazier-Wood, 2016; Brown & Roberts, 2012), including diabetes and cardiovascular disease. However, to our knowledge, only one study has investigated weight-related eating habits among transgender people (VanKim et al., 2014); findings showed no significant differences in healthy and unhealthy food consumption between transgender and non-transgender college students.
School Safety and Weight-related Health Behaviors: The Experience of Transgender Students
Extensive research has shown the negative impact of unsafe school contexts on students in the United States. Students who feel less safe at school are at higher risk of psychological adjustment problems (Farrow & Fox, 2011; Hawker & Boulton, 2000; Lunde, Frisén, & Hwang, 2006). Moreover, existing research finds a strong association between emotional symptoms caused by feeling unsafe and unhealthy eating or even eating disorders (Halvarsson-Edlund et al., 2008; Libbey et al., 2008).
To date, there has been little discussion about how the school context may influence transgender students’ weight-related behaviors. Existing evidence mostly focuses on LGBT students, with most LGBT youth (Brackenridge et al., 2007), especially males (Baiocco et al., 2018) leaving or avoiding sports because of harassment or when they feel unsafe at school, and a tendency to avoid locker rooms, gyms, or physical education classes. The rates of such avoidance behaviors tend to be higher among transgender students compared to sexual minorities (Kosciw et al., 2018).
The influence of school safety on students’ weight-related behaviors may be a crucial aspect for understanding the differences in health behaviors between transgender and non-transgender youth. In fact, there is evidence that transgender students are less likely to feel safe at school compared to non-transgender students. In a national sample of LGBT students, Kosciw and colleagues (Kosciw et al., 2018) reported that of 5,099 transgender youth from the United States, more than half felt unsafe at school because of their gender identity (83%) or gender expression (61%). Likewise, Toomey and colleagues (2012) estimated that 40% of all students in their study (n = 1,415) perceived schools as unsafe for gender nonconforming youth. A qualitative study in Philadelphia reported that 18 out of 24 transgender students (ages ranged from 16–21) did not feel safe at school (Sausa, 2005).
Addressing the lack of knowledge on how school context may influence transgender students’ weight-related behaviors is especially important given that school attendance is mandatory for youth. The school context is a key setting for public health strategies for youth to improve healthy behaviors including encouraging physical activity through physical education and healthy diets (Haines & Neumark-Sztainer, 2006; Levine & Smolak, 2005; Story, Nanney, & Schwartz, 2009). Moreover, existing literature on weight-related health behaviors among transgender people is mostly based upon data from adults (Conron, Scott, Stowell, & Landers, 2012; Fredriksen-Goldsen et al., 2013; Muchicko et al., 2014), college students (VanKim et al., 2014), or clinical samples (Bandini et al., 2013; Holt, Skagerberg, & Dunsford, 2016; Vocks, Stahn, Loenser, & Legenbauer, 2009). Further, most studies of transgender people have relied on convenience samples; have been based on small sample of transgender people; and are limited by the lack of comparison groups of non-transgender people. To our knowledge, there are no existing studies based on data from non-clinical, school-wide samples of transgender adolescents in comparison with non-transgender counterparts on weight-related health behaviors.
The Present Study
To our knowledge, there has been no research that has considered the role of school safety on weight-related health behaviors among transgender and non-transgender students using a large school-based sample. The current study aimed to address this gap in the literature by focusing on potential correlates of students’ weight-related health behaviors including physical activity, participation in physical education at school, and healthy and unhealthy eating habits.
Based on existing studies, we proposed the following hypotheses: 1) transgender students have lower levels of physical activity, and lower levels of physical education at school, compared to non-transgender students (Jones et al., 2017); 2) Transgender youth are more likely to report unhealthy eating behaviors compared to their non-transgender counterparts. Prior studies have found no differences for transgender adults in healthy or unhealthy eating behaviors; however, it is well-known that adolescence is a critical period for gender identity development (Di Ceglie, 1998). Consequently, stressors associated with exploring one’s gender identity during adolescence may increase the risk of negative health behaviors among transgender youth (Vocks et al., 2009). For instance, transgender youth may consume beverages and foods in an unhealthy manner as a way to cope with stressful events (VanKim et al., 2014) or as a strategy to change their body (Vocks et al., 2009).
Finally, our third hypothesis builds on previous findings on the role of school environment and its influence on student weight-related behaviors (Halvarsson-Edlund et al., 2008; Libbey et al., 2008) as well as the findings that transgender students tend to experience their school climate as more hostile compared to non-transgender students (Kosciw et al., 2018). Specifically, we expected greater disparities between transgender and non-transgender students on weight-related health behaviors when schools are perceived as unsafe.
Method
Procedures and Participants
We analyzed data from the 2013–2015 California Healthy Kids Survey (CHKS), a survey designed to explore youth health and risk behaviors among middle and high school students in California schools. The CHKS was developed by WestEd for the California Department of Education (Austin, Bates, & Duerr, 2015a), and the survey was administered by school staff following detailed instructions provided by them. Written informed consent was obtained from the parents of the participating students. Participants were assured of anonymity and confidentiality and were also given the option not to participate.
The initial sample included a total of 910,885 students from 2,641 middle and high schools; data is collected in 7th, 9th, and 11th grade classrooms. The CHKS is comprised of a Core Module administered to all schools that contains questions about demographic characteristics and school safety, as well as several optional modules. In the present study, we used a supplemental “Physical Health and Nutrition Module” (PHMN) that includes information on physical activity and healthy and unhealthy eating habits. The PHMN was administered in 6.4% of schools. Based on the recommendation of WestEd, this study excludes respondents who are systematically identified as having questionable responses (1.10% of the sample). Exclusion is based on meeting two or more criteria related to inconsistent responses (e.g., responding that they never used a drug, but reporting drug use in the past 30 days), exaggerated drug use, using a fake drug, and indicating that they answered dishonestly to all or most of the questions on the survey (i.e., “how many questions in this survey did you answer honestly”) (Austin, Bates, & Duerr, 2015b).
Thus, the analytic sample consisted of 31,609 students in 168 schools (females: n = 15, 750, 49.8%; students did not reveal their sex: n = 309, 1%). The number of students per school ranged from 1 to 1,306 participants. They self-identified as heterosexual (n = 30,185, 95.5%), lesbian, gay, or bisexual (n = 1,424, 4.5%), and transgender (n = 358, 1.1%), and questioning/declined (n = 5,022, 16.3%). Given that participants were only asked about their sex (male or female) and not about their sex assigned at birth, we were unable to make comparisons between female-to-male and male-to-female transgender youth. Ages ranged from 10 or younger to 18 or older (Mage = 14.04, SD = 1.70). The sample included students enrolled in Grades 6 to 12 and students in undefined grades (the majority in grades 7, 9 and 11). Racial identity was diverse: 28.6% of the students reported they were White, 21.2% Asian, 4.2% Black/African American, 2.2% Native Hawaiian or Pacific Islander, 2.3% American Indian/Alaskan Native, and 31.0% multi-racial; 10% did not identify their race. Almost 63% of the total sample self-identified as non-Hispanic/Latino (n = 19,237).
Measures
Student and school indicators.
Participants reported personal characteristics including sex (male or female), race (White, Asian, Black/African American, Native Hawaiian or Pacific Islander, American Indian/Alaskan Native, multi-racial) and ethnicity (Hispanic/Latino or non-Hispanic/Latino). Based on the percentage of students in each grade we created four dichotomous variables: 1) Grades 6th –7th and 8th; 2) Grades 9th and 10th, 3) Grades 11th and 12th, 4) Ungraded students or other grades. A single question included responses for sexual orientation and gender identity with the following response categories: “Heterosexual”, “gay, lesbian, bisexual”, “transgender”, “unsure”, “decline to respond”; participants were asked to mark all the categories that apply. Four non-mutually exclusive dichotomous variables were created: one for “gay, lesbian, bisexual”; one for “heterosexual”; one for “transgender”; and one for questioning/declined (coded for students who marked “unsure” or “decline to respond”). Students who selected both “heterosexual” and “gay, lesbian, bisexual” identities (0.9%) were coded as “gay, lesbian, bisexual”. Students who did not select “transgender” identities were coded as “non-transgender”.
School-level indicators were collected from publicly-available data from the California Department of Education, including school enrollment, school socioeconomic status, and the proportion of students eligible for a free or reduced-price meal (FRPM). School urbanicity status, based on the 2010 U.S. census, was categorized as: 1) Urbanized Area of 50,000 or more people (UA), 2) Urban Clusters of at least 2,500 and less than 50,000 people (UC), and 3) Rural.
Feeling safe.
Consistent with prior research (Moore, Benbenishty, Astor, & Rice, 2017) we calculated school safety as the mean of two items: “I feel safe in my school” (ranging from 1 = totally disagree to 5 = totally agree) and “how safe do you feel when you are at school?” (ranging from 1 = very safe to 5 = very unsafe). The second item was reverse coded so that a high score indicated feeling very safe at school. The correlation between these two items was high, r = .72.
Physical activity.
A measure of physical activity was developed for the CHKS by WestEd (Austin, Polik, Hanson, & Zheng, 2016) and comprised of three items assessing the number of days in the past week a student engaged in vigorous and moderate physical activity, or muscle strengthening and toning exercise. Students were asked how often they: 1) “exercise or do a physical activity for at least 20 minutes that made you sweat and breathe hard? (For example, basketball, soccer, running, swimming laps, fast bicycling, fast dancing, or similar aerobic activities)”; 2) “participate in a physical activity for at least 30 minutes that did not make you sweat and breathe hard? (e.g., fast walking, slow bicycling, shooting baskets, skating, raking leaves, or mopping floors)”; and 3) “do exercises to strengthen or tone your muscles?” (e.g. push-ups, sit-ups, or weightlifting)”. Response options range from 0 (0 days) to 7 (7 days). Consistent with other studies (Hanson, Austin, & Lee-Bayha, 2003), the three items were averaged to form a composite scale of physical activity, with higher values corresponding to greater levels of exercise (Cronbach’s α = .79).
Physical education.
Questions related to physical education included the following: “in an average week, on how many days do you have physical activity in your physical education class?” (ranging from 0 = 0 days to 5 = 5 days) and “during an average physical education class, how many minutes do you spend actually exercising or playing sports?” (ranging from 0 = I do not take physical education to 4 = more than 30 minutes). Consistent with previous studies using identical measures of physical education (Cawley, Meyerhoefer, & Newhouse, 2007; Sabia, Nguyen, & Rosenberg, 2017), we multiplied the two items in order to reflect the total active time in physical education class per week. The second item asks students to report minutes in one of several intervals; we multiplied the number of days per week the student has physical education class by the midpoint of the interval. For example, for “less than 10 minutes”, we assume active time was 5 minutes; for “10–20 minutes” we assume active time was 15 minutes. The top category is “more than 30 minutes”. In this case we scored the top interval at 35 minutes. By multiplying the two items, if students reported “0 days” of physical education on the first item or “I do not take physical education” on the second item, their physical education score was 0.
Healthy and unhealthy eating habits.
Foods and beverages were classified as either unhealthy or healthy using the UK Ofcom Nutrient Profiling model (De Cock et al., 2017; Department of Public Health, 2011). The healthy eating habits scale included four items assessing the healthy eating behaviors of the students. Participants were asked “during the past 24 hours (yesterday), how many times did you...”: “eat vegetables (including salads and nonfried potatoes)”; “eat fruit (do not count fruit juice)”; “drink milk or eat yogurt (in any form, including in cereal)”; and “drink 100% fruit juice, such as orange, apple, or grape (do not count punch, Kool–Aid, sports drinks, and fruit–flavored drinks)”. Response options range from 0 (0) to 5 (5 or more); a higher mean score indicated more healthy eating habits (Cronbach’s α = .79). The unhealthy eating habits scale is a two-item measure. Using the same question stem for healthy eating, participants were asked: “drink soda pop” and “eat French fries, potato chips, or other fried potatoes”. Higher mean scores indicate more unhealthy eating habits. The correlation between these two scales was moderate (r = .40).
Statistical Analysis
Descriptive statistics with differences by gender identity are presented in Table 1. We used the Stata statistical software package (StataCorp, 2017; version 15) to conduct multivariate analyses. Gender identity differences (transgender vs. non-transgender students) were analyzed using the chi-squared test for categorical variables and analysis of variance (ANOVA) for continuous variables. Bivariate correlations were performed to test the relationships between variables. Multilevel regression models were conducted for each of the 4 dependent variables (physical activity, physical education, healthy and unhealthy eating habits) using the mixed command, accounting for within-school associations. All models control for student- and school-level characteristics.
Table 1.
Descriptive (means, standard deviations, and percentages) of the sample’s characteristics
|
|
|||
|---|---|---|---|
| Transgender (n = 358) | Non-transgender (n = 31,251) | ||
|
| |||
| F/χ2 | |||
|
| |||
| Sexual orientation, n (%) | |||
| LGB | 217 (60.6%) | 1,207 (3.9%) | 2600.00*** |
| Questioning | 176 (49.2%) | 182 (15.9%) | 286.81*** |
| Race, n (%) | 22.89*** | ||
| White | 106 (31.4%) | 8,939 (32.0%) | – |
| Asian | 67 (19.8%) | 6,634 (23.7%) | – |
| Black | 30 (8.9%) | 1,283 (4.6%) | – |
| Hawaiian | 11 (3.2%) | 684 (2.4%) | – |
| American Indian | 16 (4.7%) | 723 (2.6%) | – |
| Multi-racial | 108 (31.9%) | 9,685 (34.6%) | – |
| Ethnicity, n (%) | 0.23 | ||
| Hispanic/Latino | 129 (37.8%) | 11,381 (37.4%) | – |
| Non-Hispanic/Latino | 212 (62.2%) | 19,025 (62.6%) | – |
| Grades, n(%) | 62.07*** | ||
| 6th-7th-8th grades | 87 (24.6%) | 11,612 (37.4%) | – |
| 9th-10th grades | 145 (41.0%) | 10,869 (35.0%) | – |
| 11th-12th grades | 117 (33.1%) | 8,545 (27.5%) | – |
| Other grade/ungraded | 5 (1.4%) | 41 (0.1%) | – |
| School safety, M (SD) | 3.32 (1.10) | 3.81 (.84) | 112.91*** |
| Physical activity, M (SD) | 3.80 (2.58) | 3.70 (2.10) | 0.66 |
| Physical education, M (SD) | 69.19 (70.54) | 100.01 (68.02) | 57.60*** |
| Healthy eating habits, M (SD) | 3.12 (1.55) | 2.94 (1.27) | 6.08* |
| Unhealthy eating habits, M (SD) | 2.58 (1.73) | 1.99 (1.21) | 78.09*** |
Note.
p < .05
p < .01
p < .01.
The column F/χ2 refers to the gender identity difference (transgender vs. non-transgender). Totals for each variable vary because of missing data.
Dependent variables and continuous covariates were standardized prior to analysis. The only continuous variable at the student-level was school safety, thus it was group-mean centered. School-level variables (percentage of students with free & reduced-priced meals, and school enrollment) were grand mean centered. Finally, we tested the interaction between gender identity and perceptions of school safety on the 4 different outcome variables. For the models with significant interaction terms, simple slope analyses were performed using the margins command. Only significant interaction terms are reported. Complete case analyses resulted in a loss of 21.6% to 28.5% of the sample. Data were determined to be missing at random. We therefore used multiple imputations using chained equations (10 iterations) to account for missing data, seeded at 12,345 for replicability (Enders, 2010).
Results
Gender Identity Differences and Correlations Among Variables
Table 1 shows mean and frequency differences between transgender and non-transgender students on all key variables. The majority of the transgender youth self-identified as lesbian, gay, bisexual or questioning/declined, while most of the non-transgender students reported being heterosexual. Moreover, compared to non-transgender students, transgender students were less likely to be in 6th-8th grades. Oneway ANOVA analyses showed that transgender students reported feeling less safe at school, less physical education in school, and more healthy and unhealthy eating behaviors when compared to non-transgender students. No significant difference was found for physical activity.
Correlations in Table 2 show that perceptions of school safety were positively associated with physical activity and physical education, and negatively associated with unhealthy eating habits, but only among transgender students. However, school safety was positively associated with healthy eating habits among both transgender and non-transgender students. Among all youth, healthy eating behaviors were moderately associated with unhealthy eating behaviors and more physical activity; more general physical activity was moderately associated with more physical activity in physical education class.
Table 2.
Pearson’s r between school safety and other variables for transgender (n = 358, below the diagonal) and non-transgender people (n = 31,251, above the diagonal)
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
|
|
|||||
| 1. School safety | 1.00 | .03** | .03** | .03** | −.11** |
| 2. Physical activity | .01 | 1.00 | .28** | .32** | .08** |
| 3. Physical education class | −.01 | .44** | 1.00 | .13** | .01 |
| 4. Healthy eating habits | .14* | .44* | .12* | 1.00 | .40** |
| 5. Unhealthy eating habits | −.10 | .14* | −.09 | .51** | 1.00 |
Note.
p < .01
p < .05.
Physical Activity and Physical Education
Regarding physical activity, adjusted regression models (Table 3) indicate that transgender students reported more general physical activity compared to their non-transgender peers, and students who reported feeling more safe at school report more general physical activity. Female, LGB, and questioning/declined students reported significantly lower levels of physical activity. Asian and Hispanic students reported less physical activity compared to White students, and 11th –12th grade students reported less physical activity compared to 6th – 8th graders. Students in schools with larger enrollments reported more physical activity, whereas those in schools with higher proportions of students who received free or reduced price meals reported significantly less physical activity.
Table 3.
Multilevel regression analyses for gender identity and perception of school safety predicting weight-related health behaviors
| Physical Activity | Physical Education | Healthy Eatinga | Unhealthy Eating | |
|---|---|---|---|---|
|
| ||||
| Final Models: | B (SE) | B (SE) | B (SE) | B (SE) |
|
|
||||
| Fixed Effects | ||||
| Intercept | .40(.03)*** | .42(.04)*** | .16(.03)*** | .06(.03)* |
| Transgender Identity | .16(.06)** | −.26(.05)*** | .17(.06)** | .32(.06)*** |
| School safety | .03(.01)*** | .05(.01)*** | .03(.01)*** | −.09(.01)*** |
| Transgender identity X School safety | .10(.05)* | |||
| Covariates (student-level characteristics) | ||||
| Grades (Grades 6th-7th-8th as reference category) | ||||
| 9th-10th grades | −.02(.03) | −.17(.04)*** | −.13(.03)*** | .01(.03) |
| 11th-12th grades | −.32(.03)*** | −1.16(.04)*** | −.25(.03)*** | −.05(.03) |
| Other grade/ungraded | −.01(.16) | −.44(.14)** | .25(.17) | .31(.16) |
| Female | −.27(.01)*** | −.07(.01)*** | −.22(.01)*** | −.22(.01)*** |
| LGB sexual orientation | −.16(.03)*** | −.03(.03) | −.01(.03) | .13(.03)*** |
| Questioning | −.16(.02)*** | −.08(.01)*** | .04(.02)* | .01(.02) |
| Race (White as reference category) | ||||
| American Indian/Alaskan Native | −.03(.04) | −.07(.04) | .11(.04)** | .14(.04)*** |
| Asian | −.15(.02)*** | .01(.02) | .15(.02)*** | −.08(.02)*** |
| Black/African American | −.03(.03) | −.05(.03) | .18(.03)*** | .39(.03)*** |
| Native Hawaiian/Pacific Islander | .06(.04) | .05(.04) | .11(.04)** | .08(.04) |
| Multi racial | −.01(.02) | .03(.01)* | .06(.02)** | .08(.02)*** |
| Hispanic/Latino | −.09(.01)*** | .01(.01) | .01(.02) | .03(.02) |
| Covariates (school-level characteristics) | ||||
| Free / reduced price meals | −.06(.01)*** | .05(.02)** | −.03(.01)** | .12(.01)*** |
| Urbanicity | .04(.05) | −.05(.06) | .01(.03) | .03(.03) |
| Enrollment | .05(.02)* | .05(.02)* | .02(.01) | .01(.01) |
|
| ||||
| Random Effects | ||||
| Intercept (School) | .16(.01)*** | .23(.02)*** | .08(.01)*** | .10(.01)*** |
| Residual (Student) | .97(.01)*** | .83(.01)*** | .98(.01)*** | .96(.01)*** |
Note.
p<.05
p<.01
p<.001.
All continuous variables were standardized to z-scores prior to analysis, results are presented as standardized estimates and standard errors.
model includes a fixed effect level-2 interaction between gender identity & school safety.
Regarding physical education, students who feel more safe at school reported more physical activity in physical education class, whereas transgender student report less physical activity in physical education. Females and questioning/declined students reported less physical education, but there were no differences for LGB students. There were few differences based on race or ethnicity; the only difference was for multi-racial students who reported slightly more physical education. Students in grades 6th – 8th reported more physical education than all other grades. Schools with larger enrollments, and with more students who received free and reduce priced meals, reported more physical education.
Healthy and Unhealthy Eating
Adjusted regression models for eating habits (Table 3) showed that transgender students and students who felt more safe at schools reported more healthy eating habits. Female students reported less healthy eating, whereas questioning/declined youth reported more healthy eating habits. Students in 6th – 8th grades reported more healthy eating. There were no ethnic group differences in healthy eating, but every non-White group reported more healthy eating that White students. Healthy eating habits were less common in schools with more students who received free or reduced-priced meals.
Regarding unhealthy eating, transgender students reported more unhealthy eating habits, and lack of safety predicted unhealthy eating. Male and LGB students reported more unhealthy eating scores. Compared to White students, Black, American Indian/Alaska Native, and Multiracial identity students reported more unhealthy eating habits, whereas Asian students reported less unhealthy eating.
Interaction Effects between Transgender Identity and Perceived Safety at School
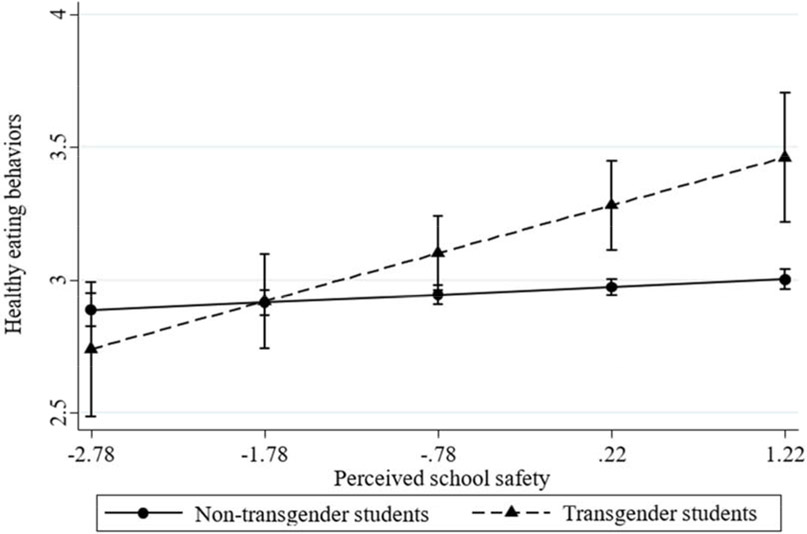
We tested a series of moderating effects between transgender identity and perceived school safety on the four weight-related behaviors. The only significant interaction was on healthy eating behaviors (see Table 3, third column). The simple slopes for transgender (B = .13, p = .010) and non-transgender students (B = .03, p < = .001) were both positive and significantly differed from zero. Results indicate that the strength of the association between perceived school safety and healthy eating behaviors is stronger for transgender compared to non-transgender adolescents. Specifically, transgender youth have significantly healthier eating behaviors in schools perceived as more safe when compared to those in schools perceived as less safe (Figure 1).
Figure 1.
Moderation effect between gender identity and perceived school safety on healthy eating behaviors
General Discussion
The primary aim of this study was to investigate gender identity disparities in multiple weight-related health behaviors (physical activity, phsyical education, and eating habits) and analyze the relationship between school safety and such behaviors in a sample of transgender and non-transgender students. Our first hypothesis was that transgender students would be less likely to engage in physical activity and physical education compared to non-transgender students. Our findings partially confirmed our expectations showing that transgender students engage less in physical education at school, yet report significantly more physical activity.
The disparity in physical education is consistent with previous findings showing that transgender youth avoid gym or physical education classes more frequently compared to their non-transgender counterparts (Kosciw et al., 2018). Transgender students may be more likely to perceive school physical activity as hostile: sports activities at school tend to be sex segregated, and often transgender students are not allowed to use bathrooms or locker rooms aligned with their perceived gender identity (Kosciw et al., 2018). Transgender students were more likely to be in later grades, and it is possible that the difference in physical education could be because some of the older students had already completed physical education requirements. Participants were not asked whether or not they had completed physical education requirements; this possibility could be explored in future studies of transgender students and their experiences in physical education at school.
Yet transgender students reported more general physical activity in our study, a finding that is not consistent with the existing literature (Gorczynski & Brittain, 2016; Muchicko et al., 2014; Shankle, 2013; VanKim et al., 2014). This may be due to the age difference between our sample and those used in the previous studies; in fact, prior research on physical activity disparities for transgender people has been based on adult samples. Given that transgender youth may be more conscious of or attuned to their bodies, the finding of no difference for physical activity may indicate that transgender youth are more likely to seek opportunities outside of school to engage in regular physical activity, without fear of being teased or bullied (Elling, De Knop, & Knoppers, 2003; Pronger, 1990; van Ingen, 2011), which is common in schools.
Our second hypothesis was that transgender students would be likely to engage in less healthy eating habits (both less healthy as well as more unhealthy eating). However, transgender students in our sample reported higher levels of both healthy and unhealthy eating. These findings are not consistent with the results reported by VanKim and colleagues (2014), which found no disparities. However, their study was based on a small sample of transgender college students (n = 53), and should be considered preliminary until replicated with a larger transgender sample. There are no other studies on this topic in transgender adolescents. Body dissatisfaction could explain the higher prevalence of both healthy and unhealthy food/drinks consumption among transgender youth in this sample. Transgender people are more likely to be dissatisfied with their bodies (Jones et al., 2016; Witcomb et al., 2015), a factor that is linked to high prevalence of eating difficulties (Ålgars, Alanko, Santtila, & Sandnabba, 2012; Becker et al., 2016), and high rates of underweight or overweight status. Transgender people might use healthy eating behaviors as a strategy to control their body and unhealthy eating behaviors as a strategy to modify it (Vocks et al., 2009). Another explanation could be that transgender adolescents engage in unhealthy eating behaviors as way to cope with stressful events (VanKim et al., 2014). However, these explanations are only speculative and are not supported by data from our study.
Our third hypothesis was that the perception of school safety would have a stronger effect on healthy weight-related behaviors in transgender compared to non-transgender students. Notably, our results showed that, regardless of gender identity, school safety is associated with all healthy weight-related behaviors. Students in unsafe schools may be exposed to added stressors that can influence their health behaviors. Consistent with these findings, there is evidence that stress may impair efforts to be physically active (Stults-Kolehmainen & Sinha, 2014), and unhealthy eating behaviors are often used as a strategy to mitigate the adverse effects of stress (Dallman et al., 2003).
Consistent with several prior studies (Coulter, Bersamin, Russell, & Mair, 2017; Grossman et al., 2009; Toomey, Ryan, Diaz, Card, & Russell, 2010; Toomey et al., 2012), our descriptive analyses showed that transgender students reported feeling less safe at school compared to non-transgender students, suggesting that school climate is a crucial aspect to consider for understanding transgender youth’s disparities on weight-related behaviors. In a series of moderation tests of the associations between perceived school safety and gender identity on weight-related behaviors, we found a significant interaction only for healthy eating habits. We found that transgender students have healthier eating habits when the school context is perceived as a safe place compared to transgender students in less safe schools.
Although this finding is not consistent with our expectations, it is consistent with the argument that transgender students are generally more self-conscious about their bodies (Jones et al., 2016; Vocks et al., 2009; Witcomb et al., 2015), and thus about weight-related behaviors. In safer schools, transgender students may be more likely to attend to their health and their bodies. Our third hypothesis was guided by a risk-focused frame on the health of transgender youth; we acknowledge that we were predisposed to consider their vulnerability, rather than their unique strengths. Instead, our finding suggests that, consistent with the notion that they may be more conscious about their bodies, in safe school settings transgender youth appear to make healthier choices about their diets.
Limitations of the Study and Future Research
There are several limitations. First, the data in this study is cross-sectional, thus, it is not possible to provide evidence for causal associations. Future research should examine these relationships longitudinally. Second, this study was geographically restricted to the state of California and this may limit the generalizability of the results. Third, sexual and gender identity were not assessed independently and students could mark multiple categories which makes the measurements susceptible to misclassification. In fact, respondents were not provided with a cisgender option and some youth only indicated a transgender identity (n = 3). Fourth, since the survey did not include a separate measure of sex assigned at birth, this research does not lead to inferences concerning whether there are significant differences between female-to-male and male-to-female transgender youth. Further research should assess gender identity with a method to cross-classify sex assigned at birth and gender identity status.
In addition, further investigation could also examine sexual orientation of either group (i.e. transgender and non-transgender people) and analyze possible differences in weight-related health behaviors based on sexual orientation, sex assigned at birth, and gender identity, including various categories, such as gender-queer, gender-nonconforming, and other contemporary gender identities. Future investigations should examine gender identity variations between different sporting disciplines (i.e., soccer, basket, swimming, etc.) or competitive level groups (amateur vs. sub-elite vs. elite) and analyze whether transgender students specifically avoid some types of athletic contexts. Finally, future studies are needed to test the role of other moderators in order to more fully understand associations between minority stressors such as perceptions of school safety, gender identity, and weight-related health behaviors, such as body dissatisfaction, body weight, stressful events, or negative sport/school climate.
Conclusions
This research addresses a gap in the literature about weight-related behaviors among transgender adolescents. It is now well known that disparities exist between transgender and non-transgender students’ experiences (Brittain & Dinger, 2017; Cohen & Cribbs, 2017; Gorczynski & Brittain, 2016; Miller & Luk, 2018), and that the school environment has an important role in influencing healthy weight-related behaviors (Haines & Neumark-Sztainer, 2006; Levine & Smolak, 2005; Story et al., 2009). However, as far as we know, no previous work has investigated transgender adolescents’ engagement in weight-related behaviors and the influence of school-level factors. Overall, our results show that interventions are still needed at the school level to reduce weight-related health behaviors disparities between transgender and non-transgender youth, especially with regards to physical activity at school and healthy and unhealthy eating.
Interventions on weight-related health behaviors should include strategies that affirm and support the complexity of gender identities and expressions. For example, the implementation of gender-inclusive restrooms or the creation of individual showers or private changing rooms could make locker rooms and bathrooms safe for transgender students, and could facilitate transgender students to maintain healthy weight-related behavior. Finally, the implementation of policies and practices focused on gender identity issues at school, such as teacher training, enumerated policies, and gender-sexuality (or gay-straight) alliance student-led clubs, may improve the perception of safety for gender minorities and all students (Ioverno, Belser, Baiocco, Grossman, & Russell, 2016; Russell, Day, Ioverno, & Toomey, 2015). As our results suggest, safety at school is especially important to supports transgender and all students to acquire skills for healthy weight-related behaviors, including healthy eating and regular physical activity.
Acknowledgments.
This research was supported by grant, P2CHD042849, Population Research Center, awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors acknowledge generous support from the Communities for Just Schools Fund, and support for Russell from the Priscilla Pond Flawn Endowment at the University of Texas at Austin. In addition, the research reported in this publication was supported by Sapienza University of Rome (Mobility Projects Call for Research Doctorates) under award number 2682/2017 (0051266). All authors who contributed significantly to the work have been identified.
Footnotes
Author Disclosure Statement. The authors declare that there are no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ålgars M, Alanko K, Santtila P, & Sandnabba NK (2012). Disordered eating and gender identity disorder: A qualitative study. Eating Disorders, 20(4), 300–311. [DOI] [PubMed] [Google Scholar]
- Allison KR, Adlaf EM, Dwyer JJ, Lysy DC, & Irving HM (2007). The decline in physical activity among adolescent students: A cross-national comparison. Canadian Journal of Public Health, 98(2), 97–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin G, Bates S, & Duerr M (2015a). Guidebook for the California Healthy Kids Survey part II: Data use and dissemination (2013–14 Edition). San Francisco, CA: WestEd. Retrieved from http://eric.ed.gov/?id=ED486326 [Google Scholar]
- Austin G, Bates S, & Duerr M (2015b). Guidebook to the California Healthy Kids Survey part II: Survey content core module (2013–14 edition). San Francisco, CA: WestEd. Retrieved from http://surveydata.wested.org/resources/chks_guidebook_2_coremodules.pdf [Google Scholar]
- Austin G, Polik J, Hanson T, & Zheng C (2016). School climate, substance use, and student well-being in California, 2013–2015. Results of the fifteenth Biennial Statewide Student Survey, Grades 7, 9, and 11. San Francisco: WestEd Health & Human Development Program [Google Scholar]
- Baiocco R, Pistella J, Salvati M, Ioverno S, & Lucidi F (2018). Sports as a risk environment: homophobia and bullying in a sample of gay and heterosexual men. Journal of Gay & Lesbian Mental Health, 22(4), 385–411. [Google Scholar]
- Bandini E, Fisher AD, Castellini G, Lo Sauro C, Lelli L, Meriggiola MC, ... & Dettore D (2013). Gender identity disorder and eating disorders: Similarities and differences in terms of body uneasiness. The Journal of Sexual Medicine, 10(4), 1012–1023. [DOI] [PubMed] [Google Scholar]
- Banfield EC, Liu Y, Davis JS, Chang S, & Frazier-Wood AC (2016). Poor adherence to US dietary guidelines for children and adolescents in the national health and nutrition examination survey population. Journal of the Academy of Nutrition and Dietetics, 116(1), 21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker I, Nieder TO, Cerwenka S, Briken P, Kreukels BP, Cohen-Kettenis PT, ... & Richter-Appelt H (2016). Body image in young gender dysphoric adults: A European multi-center study. Archives of Sexual Behavior, 45(3), 559–574. [DOI] [PubMed] [Google Scholar]
- Brackenridge C, Rivers I, Gough B, & Llewellyn K (2007). Driving down participation: Homophobic bullying as a deterrent to doing sport. In Aitchison CC, (Ed.), Sport and Gender Identities: Masculinities, Femininities and Sexualities (pp.122–139). London: Routledge. [Google Scholar]
- Brittain DR, & Dinger MK (2017). Physical activity in diverse populations: Evidence and practice. In Bopp M (Ed.), Physical activity among lesbian, gay, bisexual and transgender populations (pp.180–199). New York, NY: Routledge. [Google Scholar]
- Brown HW, & Roberts J (2012). Exploring the factors contributing to sibling correlations in BMI: A study using the panel study of income dynamics. Obesity, 20(5), 978–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calzo JP, Roberts AL, Corliss HL, Blood EA, Kroshus E, & Austin SB (2013). Physical activity disparities in heterosexual and sexual minority youth ages 12–22 years old: Roles of childhood gender nonconformity and athletic self-esteem. Annals of Behavioral Medicine, 47(1), 17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawley J, Meyerhoefer C, & Newhouse D (2007). The impact of state physical education requirements on youth physical activity and overweight. Health Economics, 16(12), 1287–1301. [DOI] [PubMed] [Google Scholar]
- Cohen N, & Cribbs K (2017). The everyday food practices of community-dwelling lesbian, gay, bisexual, and transgender (LGBT) older adults. Journal of Aging Studies, 41, 75–83. doi: 10.1016/j.jaging.2017.05.002 [DOI] [PubMed] [Google Scholar]
- Conron KJ, Scott G, Stowell GS, & Landers SJ (2012). Transgender health in Massachusetts: Results from a household probability sample of adults. American Journal of Public Health, 102(1), 118–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper R, Cutler J, Desvigne-Nickens P, Fortmann SP, Friedman L, Havlik R, ... & Mosca L (2000). Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: Findings of the national conference on cardiovascular disease prevention. Circulation, 102(25), 3137–3147. [DOI] [PubMed] [Google Scholar]
- Coulter RW, Bersamin M, Russell ST, & Mair C (2017). The effects of gender-and sexuality-based harassment on lesbian, gay, bisexual, and transgender substance use disparities. Journal of Adolescent Health, 62(6), 688–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallman MF, Pecoraro N, Akana SF, La Fleur SE, Gomez F, Houshyar H, ... & Manalo S (2003). Chronic stress and obesity: A new view of “comfort food”. Proceedings of the National Academy of Sciences, 100(20), 11696–11701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Cock N, Vangeel J, Lachat C, Beullens K, Vervoort L, Goossens L, ... & Eggermont S (2017). Use of fitness and nutrition apps: associations with body mass index, snacking, and drinking habits in adolescents. JMIR mHealth and uHealth, 5(4), e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Souto Barreto P, Cesari M, Andrieu S, Vellas B, & Rolland Y (2017). Physical activity and incident chronic diseases: A longitudinal observational study in 16 European countries. American Journal of Preventive Medicine, 52(3), 373–378. [DOI] [PubMed] [Google Scholar]
- Department of Public Health (2011). Nutrient Profiling Technical Guidance. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216094/dh_123492.pdf
- Di Ceglie D (1998). Stranger in my own body: Atypical gender identity and mental health. London: Karnac Books. [Google Scholar]
- Elling A, De Knop P, & Knoppers A (2003). Gay/lesbian sport clubs and events: places of homo-social bonding and cultural resistance?. International Review for the Sociology of Sport, 38(4), 441–456. [Google Scholar]
- Enders CK (2010). Applied missing data analysis. New York: The Guildford Press. [Google Scholar]
- Farrow CV, & Fox CL (2011). Gender differences in the relationships between bullying at school and unhealthy eating and shape-related attitudes and behaviours. British Journal of Educational Psychology, 81(3), 409–420. [DOI] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Cook-Daniels L, Kim HJ, Erosheva EA, Emlet CA, Hoy-Ellis CP, ... & Muraco A (2013). Physical and mental health of transgender older adults: An at-risk and underserved population. The Gerontologist, 54(3), 488–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorczynski PF, & Brittain DR (2016). Call to action: The need for an LGBT-focused physical activity research strategy. American Journal of Preventive Medicine, 51(4), 527–530. [DOI] [PubMed] [Google Scholar]
- Grossman AH, Haney AP, Edwards P, Alessi EJ, Ardon M, & Howell TJ (2009). Lesbian, gay, bisexual and transgender youth talk about experiencing and coping with school violence: A qualitative study. Journal of LGBT Youth, 6(1), 24–46. [Google Scholar]
- Haines J, & Neumark-Sztainer D (2006). Prevention of obesity and eating disorders: A consideration of shared risk factors. Health Education Research, 21(6), 770–782. [DOI] [PubMed] [Google Scholar]
- Halvarsson-Edlund K, Sjödén PO, & Lunner K (2008). Prediction of disturbed eating attitudes in adolescent girls: A 3-year longitudinal study of eating patterns, self-esteem and coping. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 13(2), 87–94. [DOI] [PubMed] [Google Scholar]
- Hanson TL, Austin G & Lee-Bayha J (2003). Student health risks, resilience, and academic performance: Year 1 Report. Los Alamitos, CA: WestEd. [Google Scholar]
- Hawker DS, & Boulton MJ (2000). Twenty years’ research on peer victimization and psychosocial maladjustment: A meta-analytic review of cross-sectional studies. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 41(4), 441–455. [PubMed] [Google Scholar]
- Holt V, Skagerberg E, & Dunsford M (2016). Young people with features of gender dysphoria: Demographics and associated difficulties. Clinical Child Psychology and Psychiatry, 21(1), 108–118. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (2011). The health of lesbian, gay, bisexual, and transgendered people: Building a foundation for better understanding. Washington, DC, The National Academies Press. [PubMed] [Google Scholar]
- Ioverno S, Belser AB, Baiocco R, Grossman AH, & Russell ST (2016). The protective role of gay–straight alliances for lesbian, gay, bisexual, and questioning students: A prospective analysis. Psychology of Sexual Orientation and Gender Diversity, 3(4), 397–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BA, Arcelus J, Bouman WP, & Haycraft E (2017). Sport and transgender people: A systematic review of the literature relating to sport participation and competitive sport policies. Sports Medicine, 47(4), 701–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BA, Haycraft E, Murjan S, & Arcelus J (2016). Body dissatisfaction and disordered eating in trans people: A systematic review of the literature. International Review of Psychiatry, 28(1), 81–94. [DOI] [PubMed] [Google Scholar]
- Kosciw JG, Greytak EA, Zongrone AD, Clark CM, & Truong NL (2018). The 2017 National School Climate Survey: The experiences of lesbian, gay, bisexual, transgender, and queer youth in our nation’s schools. New York: GLSEN. [Google Scholar]
- Kubota Y, Evenson KR, MacLehose RF, Roetker NS, Joshu CE, & Folsom AR (2017). Physical activity and lifetime risk of cardiovascular disease and cancer. Medicine and Science in Sports and Exercise, 49(8), 1599–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine M, & Smolak L (2005). The prevention of eating problems and eating disorders: Theory, research, and practice. Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Libbey HP, Story MT, Neumark-Sztainer DR, & Boutelle KN (2008). Teasing, disordered eating behaviors, and psychological morbidities among overweight adolescents. Obesity, 16(S2), S24–S29. [DOI] [PubMed] [Google Scholar]
- Lunde C, Frisén A, & Hwang CP (2006). Is peer victimization related to body esteem in 10-year-old girls and boys?. Body Image, 3(1), 25–33. [DOI] [PubMed] [Google Scholar]
- McGuire JK, Anderson CR, Toomey RB, & Russell ST (2010). School climate for transgender youth: A mixed method investigation of student experiences and school responses. Journal of Youth and Adolescence, 39(10), 1175–1188. [DOI] [PubMed] [Google Scholar]
- McGuire JK, Doty JL, Catalpa JM, & Ola C (2016). Body image in transgender young people: Findings from a qualitative, community based study. Body Image, 18, 96–107. doi: 10.1016/j.bodyim.2016.06.004 [DOI] [PubMed] [Google Scholar]
- Mereish EH, & Poteat VP (2015). Let’s get physical: Sexual orientation disparities in physical activity, sports involvement, and obesity among a population-based sample of adolescents. American Journal of Public Health, 105(9), 1842–1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JM, & Luk JW (2018). A Systematic review of sexual orientation disparities in disordered eating and weight-related behaviors among adolescents and young adults: Toward a developmental model. Adolescent Research Review, 4(2), 187–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore H, Benbenishty R, Astor RA, & Rice E (2017). The positive role of school climate on school victimization, depression, and suicidal ideation among school-attending homeless youth. Journal of School Violence, 17(3), 298–310. [Google Scholar]
- Muchicko MM, Lepp A, & Barkley JE (2014). Peer victimization, social support and leisure-time physical activity in transgender and cisgender individuals. Leisure/Loisir, 38(3–4), 295–308. [Google Scholar]
- National Association for Sport and Physical Education & American Heart Association. (2010). Shape of the nation report: Status of physical education in the USA. Reston, VA: National Association for Sport and Physical Education. [Google Scholar]
- Nelson MC, Lust K, Story M, & Ehlinger E (2008). Credit card debt, stress and key health risk behaviors among college students. American Journal of Health Promotion, 22(6), 400–406. [DOI] [PubMed] [Google Scholar]
- Nelson MC, Neumark-Stzainer D, Hannan PJ, Sirard JR, & Story M (2006). Longitudinal and secular trends in physical activity and sedentary behavior during adolescence, Pediatrics, 118(6), 1627–1634. [DOI] [PubMed] [Google Scholar]
- Pilkington P, Powell J, & Davis A (2016). Evidence-based decision making when designing environments for physical activity: The role of public health. Sports Medicine, 46(7), 997–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronger B (1990) The Arena of Masculinity. Sports, Homosexuality and the Meaning of Sex. New York: St Martin’s Press. [Google Scholar]
- Rainey JC, Furman CR, & Gearhardt AN (2018). Food addiction among sexual minorities. Appetite, 120, 16–22. doi: 10.1016/j.appet.2017.08.019 [DOI] [PubMed] [Google Scholar]
- Russell ST, Day JK, Ioverno S, & Toomey RB (2015). Are school policies focused on sexual orientation and gender identity associated with less bullying? Teachers’ perspectives. Journal of School Psychology, 54, 29–38. 10.1016/j.jsp.2015.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabia JJ, Nguyen TT, & Rosenberg O (2017). High School Physical Education Requirements and Youth Body Weight: New Evidence from the YRBS. Heal Econ (United Kingdom), 26(10), 1291–1306. [DOI] [PubMed] [Google Scholar]
- Sausa LA (2005). Translating research into practice: Trans youth recommendations for improving school systems. Journal of Gay & Lesbian Issues in Education, 3(1), 15–28. [Google Scholar]
- Shankle M (2013). The handbook of lesbian gay bisexual and transgender public health: A practitioner’s guide to service. New York, NY: Routledge. [Google Scholar]
- StataCorp. 2017. Stata Statistical Software: Release 15. College Stations, TX: StataCorp LLC. [Google Scholar]
- Story M, Nanney MS, & Schwartz MB (2009). Schools and obesity prevention: Creating school environments and policies to promote healthy eating and physical activity. The Milbank Quarterly, 87(1), 71–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stults-Kolehmainen MA, & Sinha R (2014). The effects of stress on physical activity and exercise. Sports Medicine, 44(1), 81–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suisman JL, Thompson JK, Keel PK, Burt SA, Neale M, Boker S, ... & Klump KL (2014). Genetic and environmental influences on thin-ideal internalization across puberty and preadolescent, adolescent, and young adult development. International Journal of Eating Disorders, 47(7), 773–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toomey RB, McGuire JK, & Russell ST (2012). Heteronormativity, school climates, and perceived safety for gender nonconforming peers. Journal of Adolescence, 35(1), 187–196. [DOI] [PubMed] [Google Scholar]
- Toomey RB, Ryan C, Diaz RM, Card NA, & Russell ST (2010). Gender nonconforming lesbian, gay, bisexual, and transgender youth: School victimization and young adult psychosocial adjustment. Developmental Psychology, 46(6), 1580–1589. [DOI] [PubMed] [Google Scholar]
- VanKim NA, Erickson DJ, Eisenberg ME, Lust K, Rosser BR, & Laska MN (2014). Weight-related disparities for transgender college students. Health Behavior and Policy Review, 1(2), 161–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ingen C (2011). Shape your life and embrace your aggression: a boxing project for female and trans survivors of violence. Women in Sport and Physical Activity Journal, 20(1), 66–77. [Google Scholar]
- Vocks S, Stahn C, Loenser K, & Legenbauer T (2009). Eating and body image disturbances in male-to-female and female-to-male transsexuals. Archives of Sexual Behavior, 38(3), 364–377. [DOI] [PubMed] [Google Scholar]
- Watson RJ, Adjei J, Saewyc E, Homma Y, & Goodenow C (2017). Trends and disparities in disordered eating among heterosexual and sexual minority adolescents. International Journal of Eating Disorders, 50(1), 22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witcomb GL, Bouman WP, Brewin N, Richards C, Fernandez-Aranda F, & Arcelus J (2015). Body image dissatisfaction and eating-related psychopathology in trans individuals: A matched control study. European Eating Disorders Review, 23(4), 287–293. [DOI] [PubMed] [Google Scholar]
- Zapata LB, Bryant CA, McDermott RJ, & Hefelfinger JA (2008). Dietary and physical activity behaviors of middle school youth: the youth physical activity and nutrition survey. Journal of School Health, 78(1), 9–18. [DOI] [PubMed] [Google Scholar]