Abstract
Purpose
The aim of this study was to analyze the outcomes of anatomical repair and ligament bracing for Schenck III and IV knee dislocation (KD).
Methods
The results of 27 patients (15 and 12 cases of Schenck III and IV KD, respectively) after a mean follow-up of 18.1 ± 12.1 months (range 6–45 months) were retrospectively reviewed. Twenty-two patients suffered high-kinetic-energy accidents, whereas five patients suffered ultralow-velocity (ULV) trauma due to obesity. The outcome measures were the Lysholm score, Hospital for Special Surgery (HSS) knee score, Knee Society Score (KSS), Knee Injury and Osteoarthritis Outcome Score (KOOS) and Short Form 36 (SF-36) score. A kinematic 3D gait analysis with five walking trials was performed to compare the patients and healthy controls.
Results
The mean KSS, HSS score, Lysholm score, and KOOS were 77.4 ± 14.4, 84.6 ± 11.2, 81.5 ± 10.4, and 67.3 ± 16.8, respectively. No intra- or postoperative complications occurred. The mean range of motion deficiency compared to the healthy side was 24.4 ± 18.5°. Ten patients had first-degree residual laxity of the anterior cruciate ligament; 12 and 2 patients had first- and second-degree residual laxity of the collateral ligament, respectively. Five patients underwent additional arthroscopic arthrolysis due to arthrofibrosis at an average of 6.2 ± 1.9 months (range 4–9 months) after the initial surgery. The 3D gait analysis showed no major differences in joint stability or movement between the patients and healthy controls. Only the ULV trauma patients had significantly lower outcome scores and showed larger kinematic deviations in joint movement during the gait analysis.
Conclusion
Anatomical repair with ligament bracing is a suitable surgical procedure in the treatment of KD and provides evidence in clinical practice with the benefit of early, definitive repair and preservation of the native ligaments. Patients reach acceptable subjective and objective functional outcomes, including mainly normalized gait patterns during short-term follow-up, with only minor changes in kinematics and spatial–temporal characteristics. Obese patients who suffered ULV trauma showed significantly inferior outcomes with larger deviations in joint kinematics.
Level of evidence
Level III.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00167-021-06501-2.
Keywords: Knee dislocation, Multiligament injuries, Anatomical repair, Gait analysis
Introduction
Knee dislocation (KD) with multiligament lesions is one of the most severe injuries of the knee joint, not least due to the high rate of accompanying injuries, such as peroneal nerve, vascular, chondral and meniscal lesions, injury to the posterolateral capsule and/or popliteus complex or disruption of the m. biceps femoris [3, 8, 10, 16, 17, 25, 37, 40, 51] and complications like the need for blood transfusion or pulmonary embolism [27]. The occurrence of KD has been reported to account for between 0.02% and 0.1% of all musculoskeletal injuries [40]. The injury mechanism of KD is quite inconsistent and is mainly divided into high-and low kinetic-energy trauma [11], for example, sports or work accidents, and ultralow-velocity (ULV) trauma (activities of daily living) with high energy related to obesity [16]. Since nonsurgical therapy in the case of acute KD yields unsatisfactory results [14, 29, 35, 38], various surgical procedures have been developed. These strategies range from early to late surgery [18] and repair to reconstruction and one- to two-stage procedures, with comparably satisfactory results [1, 4, 9, 15, 19, 24, 30, 34, 43, 54], even if most authors recommend a staged procedure for the repair of peripheral structures and reconstruction of cruciate ligaments [5, 14, 16, 22]. Furthermore, both open and arthroscopic treatment strategies in the early and late stages have been described as practicable [12, 20, 46]. However, due to the inhomogeneity of the patient characteristics, small case numbers and different associated injuries, no standards of treatment currently exist [32]. Therefore, Heitmann et al. presented the first results of a multicenter study of anatomical repair and ligament bracing as a new treatment option for acute KD [16]. The obtained results and revision rate show that early primary suture repair is a promising option [16], even if ULV KD seems to be a particular problem, with an increasing incidence over recent years, higher rates of concomitant injuries and complications and poorer outcomes [16, 23, 39, 50]. However, only a few studies are available regarding the outcome of anatomical repair with suture augmentation after acute KD. Furthermore, to the best of our knowledge, 3D gait analysis following the surgical repair of acute KD has not yet been performed. Gait analysis allows objective kinematic measurements to be obtained and has been used for the evaluation of different knee surgeries, including total knee arthroplasty [2, 53] and anterior cruciate ligament (ACL) reconstruction [44]. Therefore, the aim of this study was to analyze the subjective and functional outcomes of anatomical repair and ligament bracing for Schenck III and IV acute KD to evaluate the clinical suitability and thereby improve the management of this severe injury. It was hypothesized that anatomical repair and ligament bracing yield good functional results, including widely restored physiological gait kinematics.
Materials and methods
The study was reviewed and approved by the local ethics committee of the medical faculty of Ruhr University Bochum, Germany (registered number: 18-6508_1-BR). All procedures were performed in accordance with the ethical standards of the institutional research committee and with the 1964 Declaration of Helsinki and its later amendments.
Patients with acute KD undergoing anatomical repair and bracing of the ruptured ligaments between 01/2015 and 01/2019 were retrospectively reviewed. KD was categorized according to the classification reported by Schenck et al. [42], which subdivides the severity of the injury based on the ruptured ligaments. Only patients presenting with clinical and radiological evidence of type III or IV KD were included in this study. The other inclusion criteria were clinical examination and gait analysis data with a minimum follow-up of 6 months. Patients with polytrauma, with type I or II KD, treated with a hybrid technique (ligament reconstruction and/or suture or two-stage procedures) or with incomplete data were excluded from further analysis. In total, 27 of 33 (81.8%) patients (15 and 12 cases of Schenck III and IV KD, respectively) with a mean follow-up of 18.1 ± 12.1 months (range 6–45 months) fulfilled the inclusion criteria and were considered for further analysis. Twenty-two of these patients suffered high- or low-velocity accidents, whereas five patients underwent ULV trauma due to obesity (mean BMI, 44.1 ± 11.6 kg/m2). Table 1 shows data regarding the demographics, allocation and concomitant injuries in the study group.
Table 1.
Study group
| Study group | |
|---|---|
| Age (years) | 38.3 ± 14.4 (range 15–61) |
| Sex | |
| Male | 18 (66.7%) |
| Female | 9 (33.3%) |
| ASA-score | |
| I | 15 (55.6%) |
| II | 10 (37.0%) |
| III | 2 (7.4%) |
| Comorbidities | |
| Smokers | 9 (33.3%) |
| Arterial hypertension | 3 (11.1%) |
| Diabetes mellitus | 1 (3.7%) |
| Asthma | 1 (3.7%) |
| Epilepsy | 1 (3.7%) |
| BMI (kg/m2) | 29.0 ± 9.3 (range 15.6–60.1) |
| Type of injury | |
| KD 3 medial | 6 (22.2%) |
| KD 3 lateral | 9 (33.3%) |
| KD 4 | 12 (44.4%) |
| Concomitant injuries | |
| Disruption of posterolateral capsule and/or popliteus complex | 15 (55.6%) |
| Peroneal nerve lesion | 5 (18.5%) |
| Meniscal lesion | 8 (29.6%) |
| Chondral lesion | 1 (3.7%) |
| Disruption of m. biceps femoris | 3 (11.1%) |
| Disruption of m. vastus medialis | 1 (3.7%) |
| Fracture of fibula head and/or tibial plateau and/or distal femur | 2 (7.4%) |
Surgical management and postoperative procedure
Anatomical repair with ligament bracing was performed based on plain radiographs, MRI scans and intraoperative findings in combination with a physical examination of ligamentous instability. Prior to open reconstruction, diagnostic arthroscopy was performed to identify possible meniscal tears or chondral lesions. An augmented primary suture repair of all torn ligaments was then performed using the surgical technique previously described by Heitmann et al. [16]. In brief, an anteromedial parapatellar arthrotomy was used to address type III medial KD. In the case of type III lateral KD, injury of the posterolateral corner or type IV KD, an additional lateral incision was performed. ACL and posterior cruciate ligament (PCL) tunnels were drilled in standard positions with the assistance of arthroscopic ACL and PCL drill guides. The ligament stumps were reinforced with FiberWire 2 (Arthrex, Naples, USA), and FiberWire 5 was used in placing augmentation sutures. After extracortical diversion through the drill tunnels, the sutures were knotted using metal suture buttons (Arthrex, Naples, USA). First, the augmentation sutures were knotted, followed by tension-free knotting of the pull-out sutures of the ligaments [16]. After reconstruction of the cruciate ligaments, all torn collateral ligaments were repaired using transosseous pull-out sutures that were fixed extracortically with suture buttons. In cases of posterolateral corner injuries with avulsion of the popliteus tendon, the tendon was also fixed with a transosseous pull-out suture. In all cases of a meniscal tear, open repair was performed; in one case, debridement and microfracture were performed for a grade 4 chondral lesion.
Physical therapy started 48 h after the operation with passive motion of the joint in the prone position with limited range of motion (ex./flex. 0°/0°/90°). In some cases, peripheral nerve block anesthesia was applied. Patients had a limited weight-bearing of 20 kg and limited range of motion (ex./flex. 0°/0°/90°) for 6 weeks. Flexible stabilization braces were recommended for 12 weeks (e.g., a DonJoy Armor® brace).
Follow-up examination
The patient assessment and clinical examination were scheduled at a minimum of six months after the primary surgery. Subjective and functional outcomes after ligament bracing were determined using the Lysholm score [47], Knee Injury and Osteoarthritis Outcome Score (KOOS) [41], Hospital for Special Surgery (HSS) knee score [21], Knee Society score (KSS) [33] and Short Form 36 (SF-36) score [49]. Time to return to work and return to sport with regard to cycling, swimming and walking were recorded. Additionally, to quantify the kinematics (e.g., side-by-side differences, stability and movement) of the joints of the lower extremities, a 3D gait analysis (3D myoMOTION, Noraxon, Scottsdale, USA) using inertial sensor technology was performed.
Gait analysis
The 3D biomechanical gait analysis was conducted while the participant performed five trials of level walking over 10 m at a self-selected pace. Therefore, the 3D myoMOTION system (Noraxon, Scottsdale, AZ, USA) was used. The system consists of seven sensors and is based on inertial sensor technology. The sensors have a maximum sampling rate of 200 Hz. The accuracy of anatomical angles in the static setup is ± 1°, and that in the dynamic setup is ± 2°. The accuracy of the orientation angles for the pitch and heading is 0.25° and 1.25°, respectively. The sensors were mounted in the designated positions at the pelvis, thighs, shanks and feet. Based on a so-called fusion algorithm, the information from a 3D accelerometer, gyroscope and magnetometer is used to measure the anatomical angles of the pelvis, hips, knees and ankles. MR 3.14 software (Noraxon, Scottsdale, AZ, USA) was used to calculate the values of the joint angles from the inertial sensor data. The sensors were calibrated before each walking trial separately. The validity and reliability of wearable inertial measurement units have received particular attention in the area of analyzing spatiotemporal characteristics and gait parameters [26]. The mean and peak angles of the joints during the stance and swing phases of walking, the walking speed and the time of double limb support were analyzed. Gait data were evaluated side by side. The kinematic curves normalized to a gait cycle in the patients were compared to those of an age-, sex- and BMI-matched control group of 20 healthy participants without injuries or a history of surgery in the lower extremities (excluding morbidly obese patients).
Statistical analysis
Descriptive data are described by the mean, standard deviation, minimum and maximum. After the normality of the data was tested using the Shapiro–Wilk test, normally distributed variables were assessed using the two-tailed t-test, a parametric test. Nonnormally distributed variables were analyzed with the Wilcoxon/Mann–Whitney test. Nominally scaled variables were compared using cross tables and Fischer’s exact test. To assess the level of similarity between the different kinematic curves normalized to the gait cycle, cross-correlation analysis was performed. The sample size calculation using G*Power (version 3.1.9.6 for Mac, University of Dusseldorf, Germany) resulted in a minimum sample size of 19 persons for both the study and control group. The gait data were processed in MATLAB, MathWorks, Inc. The level of statistical significance was set to α = 0.05.
Results
The subjective and functional outcome scores are shown in Tables 2 and 3. Patients with ultra-low velocity (ULV) trauma had a significantly lower KSS, HSS knee score and SF-36 Physical Functioning, Energy/Fatigue, Emotional Well-Being and Social Functioning score (Table 4). All patients reached full weight-bearing without the use of canes, crutches or external braces.
Table 2.
Overall outcome scores in the study group
| KSS | KSS functional | HSS Knee Score | Lysholm Score | KOOS | |
|---|---|---|---|---|---|
| Mean | 77.4 | 80.2 | 84.6 | 81.5 | 67.3 |
| Standard deviation | 14.4 | 20.3 | 11.2 | 10.4 | 16.8 |
| Minimum | 41 | 20 | 55 | 67 | 38.7 |
| Maximum | 100 | 100 | 100 | 96 | 95.2 |
KSS Knee Society Score, KOOS Knee Injury and Osteoarthritis Outcome Score
Table 3.
SF-36 scores
| SF 36% | Physical functioning | Role limitations (physical health) | Role limitations (emotional problems) | Energy/fatigue | Emotional well-being | Social functioning | Pain | General health | Health change |
|---|---|---|---|---|---|---|---|---|---|
| Mean | 67.3 | 52.8 | 67.9 | 60 | 74.1 | 83.4 | 71.5 | 70.9 | 67.6 |
| SD | 21.5 | 42.1 | 41.1 | 20.6 | 20.3 | 24.6 | 26.4 | 16.0 | 26.2 |
| Minimum | 20 | 0 | 0 | 15 | 16 | 0 | 22.5 | 45 | 0 |
| Maximum | 100 | 100 | 100 | 95 | 96 | 100 | 100 | 95 | 100 |
Table 4.
Significant differences in outcome scores between ULV and HV + LV trauma patients
| HV + LV | ULV | ||
|---|---|---|---|
| Mean ± SD | Mean ± SD | P value | |
| Knee Society Score | 80.7 ± 13.7 | 62.6 ± 8.9 | 0.010 |
| Knee Society Score funct | 86.6 ± 13.4 | 52.0 ± 24.9 | 0.000 |
| HSS Knee Score | 88.0 ± 8.8 | 69.4 ± 8.8 | 0.000 |
| SF 36 physical functioning % | 73.3 ± 17.6 | 41.0 ± 20.7 | 0.001 |
| SF 36 energy/fatigue % | 64.3 ± 18.4 | 41.0 ± 23.0 | 0.022 |
| SF 36 emotional well-being % | 79.7 ± 13.9 | 49.6 ± 29.2 | 0.002 |
| SF 36 Social functioning % | 88.2 ± 22.0 | 62.5 ± 29.3 | 0.035 |
HV high-velocity trauma, LV low-velocity trauma, ULV ultra-low velocity trauma
In total, 24 patients returned to work at an average of 7.8 ± 4.0 months (range 1–18 months), and 21 patients returned to sports (cycling, walking, swimming) at an average of 8.7 ± 4.4 months (range, 4–24 months) after the operation. However, the activity level of sports was lower after the accident in 17 patients. The mean range of motion deficiency compared to the healthy side was 24 ± 19°, but only five patients had an extension deficit of 5°. The thigh and shank circumference as a measure of muscle atrophy was reduced on the operative side compared to the healthy side by an average of 1.9 ± 1.5 cm and 1.1 ± 1.0 cm, respectively. Table 5 demonstrates the residual laxity after ligament bracing of the knee joint. No intra- or postoperative complications occurred during the study period. In five patients, additional arthroscopic arthrolysis due to arthrofibrosis was performed an average of 6.2 ± 1.9 months (range 4–9 months) after the initial surgical treatment.
Table 5.
Remaining postoperative functional deficits and laxity of the ligaments
| Residual deficit | |
|---|---|
| ROM deficit | 24 ± 19° (range 0–75°) |
| ACL laxity | 10 patients (1°) |
| PCL laxity | 0 Patients |
| Collateral laxity | |
|
Lateral Medial Medial + lateral |
9 Patients (8 patients 1°, one patient 2°) 3 Patients (1°) 1 Patient (2°) |
Gait analysis
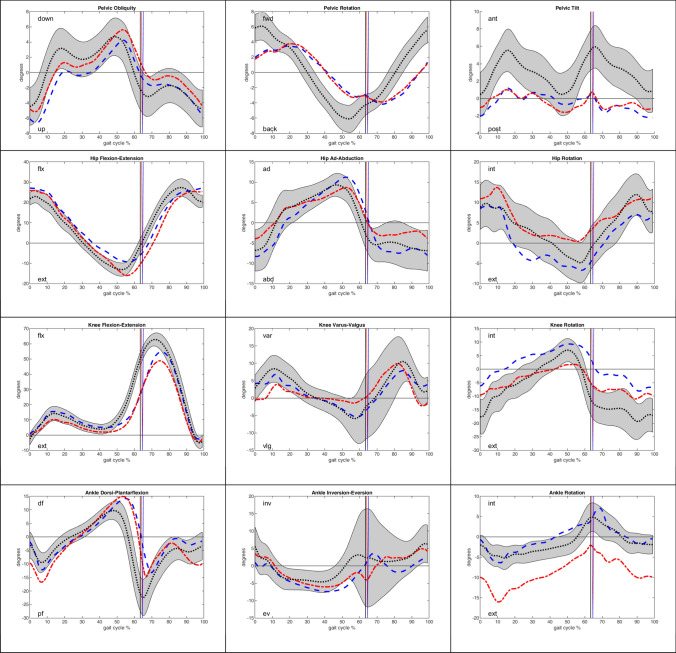
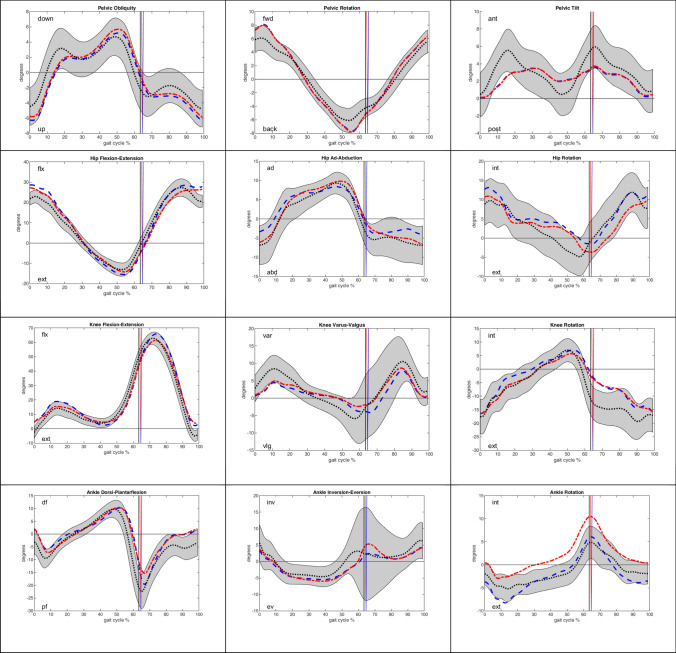
Spatial–temporal characteristics and differences between the control and patient groups determined by gait analysis are shown in Table 6. In particular, the patients had a significantly longer stance phase and shorter swing phase than did the controls, although the velocity of the patients was significantly slower. Kinematic curves of the different patient groups in relation to the control group are demonstrated in Figs. 1 and 2. The kinematic curves of the patient group without ULV trauma deviated only slightly from the mean kinematic curve and standard deviation of the control group (Fig. 2). The morbidity obese patients with ULV trauma showed larger deviations in gait kinematics than the controls (Fig. 1). The additionally calculated cross-correlation of the gait curves demonstrated a high similarity of the kinematic curves of the patients and controls.
Table 6.
Spatial–temporal characteristics
| ULV (n = 5) | HV + LV (n = 22) | Control (n = 20) | |
|---|---|---|---|
| Stance % |
67.6 ± 2.3 H* (p < 0.001) 66.4 ± 2.6 I* (p < 0.001) |
64.3 ± 1.7 H* (p < 0.001) 63.5 ± 1.9 I (p = 0.246) |
63.3 ± 1.4 |
| Pre-swing % |
17.2 ± 3.5 H* (p < 0.001) 16.8 ± 1.4 I* (p < 0.001) |
14.6 ± 2.6 H* (p < 0.001) 13.3 ± 2.4 I (p = 0.794) |
13.2 ± 1.5 |
| Swing % |
32.4 ± 2.3 H* (p < 0.001) 33.6 ± 2.6 I* (p < 0.001) |
35.7 ± 1.7 H* (p < 0.001) 36.5 ± 1.9 I (p = 0.246) |
36.7 ± 1.4 |
| Double Stance % | 33.9 ± 4.8* (p < 0.001) | 27.7 ± 3.4* (p = 0.002) | 26.3 ± 2.7 |
| Step length cm |
53.5 ± 7.3 H* (p < 0.001) 54.7 ± 9.7 I* (p < 0.001) |
65.6 ± 8.4 H* (p = 0.009) 65.0 ± 8.8 I* (p = 0.002) |
68.2 ± 7.6 |
| Step time ms |
611.7 ± 141.1 H* (p < 0.001) 616.8 ± 100.0 I* (p < 0.001) |
574.2 ± 56.0 H* (p < 0.001) 568.6 ± 51.4 I* (p < 0.001) |
539.2 ± 46.7 |
| Velocity km/h | 3.3 ± 0.8* (p < 0.001) | 4.2 ± 0.7* (p < 0.001) | 4.6 ± 0.6 |
*Indicates significant difference (p < 0.02) to control group
H healthy side, I injured side
Fig. 1.
Kinematic curves for peak joint angles on the healthy side (blue) and injured side (red) of ULV trauma patients in contrast to the mean curve in the healthy control group (black). The gray area demonstrates the range of the standard deviation in the control group. The vertical lines mark the transition from stance to swing phase
Fig. 2.
Kinematic curves for peak joint angles on the healthy side (blue) and injured side (red) in the study group without ULV trauma patients in contrast to the mean curve in the healthy control group (black). The gray area demonstrates the range of the standard deviation in the control group. The vertical lines mark the transition from stance to swing phase
Discussion
The most important finding of the present study was the demonstration of the adequate suitability of anatomical repair and ligament bracing as a rarely described surgical procedure for treating high-grade KD with a low complication rate. Considering the severity of this injury, our study demonstrates satisfactory subjective and functional outcomes and largely physiological gait after the operative treatment of high-grade KD using the method of anatomical repair and ligament bracing published by Heitmann et al. [17] and Frosch et al. [14]. Most of the patients reported acceptable to good knee function, with sufficient stability and low pain. Furthermore, our short-term results show low complication and revision rates, additionally supporting anatomical repair and ligament bracing as a procedure for the successful treatment of these serious injuries. The overall health status (SF-36 score) was also mostly characterized as good. The mean postoperative stiffness of the knee with flexion deficits, muscle atrophy of the thigh and shank muscles and minor changes in gait were restrictive; however, they were considered acceptable considering the severity of the injury and current literature [1]. Nevertheless, these limitations resulted in an extended rehabilitation time and time to return to sports and work in most of the patients, who did not reach their preinjury activity level during the follow-up period. Patients with ULV trauma were particularly affected by poorer outcomes (Tables 4, 6).
These results are in agreement with the results reported by Heitmann et al. [16], who demonstrated the first results of anatomical repair and ligament bracing for KD in their prospective, multicenter study. Sixty-nine cases of KD (Schenck III and IV) were evaluated. The average International Knee Documentation Committee (IKDC) score was 75.5 ± 14.5, the average Lysholm score was 81.0 ± 15.5, and the median loss of activity according to the Tegner score was 1 (range 0–3) point; these outcomes are nearly the same as our results (Tables 2, 3). Stress radiographs showed a mean side-to-side difference of 3.2 ± 1.3 mm for the ACL and 2.9 ± 2.1 mm for the PCL. The surgical revision rate (early and late) was 17.4%. In the later stage, four patients with knee stiffness and six patients with symptomatic knee instability needed reoperation. The rate of arthrofibrosis requiring surgical intervention was 23.2% [16] (vs. 18.5% in our study). Indeed, the patients with ULV trauma, in accordance with our results, had significantly inferior outcome scores [16], probably due to the high overweight of these patients.
Moreover, as an additional outcome measure, a 3D biomechanical gait analysis was performed to analyze the kinematics of the lower extremity joints during full weight-bearing while performing a complex movement sequence. To date, no data regarding gait in KD have been reported in the literature. This gait analysis showed a largely physiological gait cycle in the short- to midterm follow-up period, with no major differences in joint kinematics between the injured and healthy sides or between the patients and healthy controls (Fig. 2). However, the spatiotemporal characteristics showed significant differences between the patients and controls, and the changes in gait speed, smaller step length and longer stance phase were certainly related to the injury (Table 6). Taking a differentiated view of the knee kinematics, slightly lower knee varus/valgus and lower external rotation while transitioning from the stance to the swing phase of the gait cycle were observed (Fig. 2). These observations are comparable to known gait data from patients treated with ACL reconstruction, which also describe changes in the frontal- and sagittal-plane walking kinematics of the knee in the early- to midterm follow-up period [44]. Looking at the subgroup of patients with ULV trauma, in accordance with the subjective and clinical results, the larger deviations in joint movement during the gait cycle are striking. For example, reduced knee rotation and knee flexion indicated increased stiffness of the operated knee joint (Fig. 1), which was in accordance with the results of the clinical examination. When considering the gait analysis, it must be mentioned restrictively that obesity has an influence on joint movement during gait [28]. Therefore, the deviations in the gait of the patients with ULV trauma could partly be due to the high overweight of these patients and the low number of patients investigated.
Considering the major advantages of this surgical procedure for anatomical repair and ligament bracing, early, timely, definitive surgical treatment after trauma [18] (in contrast to late reconstruction with a longer period of limited movement and disease progression for the patient) and preservation of the native ligaments with the possibility of subsequent reconstruction in case of remaining laxity [36, 52] must be emphasized. However, two difficulties in our patient cohort were also noticed: (1) residual laxity, especially regarding the ACL and collateral ligaments; and (2) postoperative stiffness due to arthrofibrosis requiring arthroscopic arthrolysis during the follow-up period. In that regard, whether ligament reconstruction or repair provides greater stability, reduces arthrofibrosis and consequently improves the outcomes remains a matter of debate [7, 14, 32, 48]. Regarding the residual laxity of the ACL, Heitmann et al. mentioned a hybrid technique involving ACL reconstruction and bracing of the other ruptured ligaments as a promising option [16]. Focusing on postoperative arthrofibrosis, it is unclear whether early surgical repair via arthrotomy leads to increased postoperative stiffness, whereas it is known that early reconstruction leads to a higher rate of postoperative stiffness [16]. In conclusion, it must be stated that comparative data regarding complications and outcomes between surgical repair and reconstruction after KD are missing, which is why such studies would be desirable [6, 14].
Despite trying to ensure reliability, there are certain limitations to our study. An inhomogeneous follow-up period among the patients is based on the retrospective study design. Furthermore, only short-term results with a mean follow-up of 18.1 ± 12.1 months are provided by the study. Gait analysis using inertial sensors does not provide any information about kinetics, which prevents a deeper understanding of rehabilitation mechanisms. Moreover, the small study group with varied results and distinctly pronounced differences in the gait pattern between the individual subgroups (e.g., patients with ULV trauma) led to large standard deviations, which might have led to underpowered statistical results. However, the small group size is due to the rarity of the injury and the single-center study design. Therefore, because of the high relevance of this topic, larger, longer-term investigations of this surgical procedure are required, especially since nearly about 25% of patients with KD suffer from osteoarthritis in the long-term [13, 31, 45]. Despite these limitations, anatomical repair and ligament bracing can be evaluated as a promising option for the treatment of KD based on the results of our study. This approach offers orthopedic surgeons a working treatment concept in daily clinical practice, with acceptable short- term objective outcomes, low complication rates and the advantages of early, definitive repair and preservation of the native ligaments, since the treatment of KD is still debated in the literature [32]. Moreover, in the day-by day work, the results of our study help inform patients, who suffered from KD, about first clinical results and benefits of ligament bracing.
Conclusion
The treatment of Schenck III and IV KD by anatomical repair and ligament bracing leads to acceptable subjective and functional outcomes. Furthermore, patients who suffered from high- or low-velocity accidents showed a widely restored physiological gait pattern in the short-term follow-up. Obese patients who suffered ULV trauma showed significantly inferior outcomes and larger deviations in joint kinematics.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviations
- KD
Knee dislocation
- ULV
Ultralow-velocity
- KOOS
Knee Injury and Osteoarthritis Outcome Score
- HSS
Hospital for Special Surgery
- KSS
Knee Society Score
- SF 36
Short Form 36
- IKDC
International Knee Documentation Committee
Authors contribution
JG, DS and TAS carried out the study design. TR, SL, MK and VR participated in the acquisition of data, while TR and BJ performed the analysis and interpretation of the data. TR, JG drafted the manuscript. All author’s read, revised and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Compliance with ethical standards
Conflict of interest
All authors confirm that there is no conflict of interest.
Ethical approval
The study was reviewed and approved by the local ethics committee of the medical faculty of Ruhr University Bochum, Germany (registered number: 18-6508_1-BR).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alentorn-Geli E, Lazarides AL, Utturkar GM, Myers HS, Samuelsson K, Choi JHJ, et al. Factors predictive of poorer outcomes in the surgical repair of multiligament knee injuries. Knee Surg Sports Traumatol Arthrosc. 2019;27:445–459. doi: 10.1007/s00167-018-5053-9. [DOI] [PubMed] [Google Scholar]
- 2.Baczkowicz D, Skiba G, Czerner M, Majorczyk E. Gait and functional status analysis before and after total knee arthroplasty. Knee. 2018;25:888–896. doi: 10.1016/j.knee.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Bernhoff K, Michaelsson K, Bjorck M. Incidence and outcome of popliteal artery injury associated with knee dislocations, ligamentous injuries, and close to knee fractures: a Nationwide Population Based Cohort Study. Eur J Vasc Endovasc Surg. 2020 doi: 10.1016/j.ejvs.2020.10.017. [DOI] [PubMed] [Google Scholar]
- 4.Billieres J, Labruyere C, Steltzlen C, Gonzalez A, Boisrenoult P, Beaufils P, et al. Multiligament knee injuries treated by one-stage reconstruction using allograft: postoperative laxity assessment using stress radiography and clinical outcomes. Orthop Traumatol Surg Res. 2020;106:937–944. doi: 10.1016/j.otsr.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Bin SI, Nam TS. Surgical outcome of 2-stage management of multiple knee ligament injuries after knee dislocation. Arthroscopy. 2007;23:1066–1072. doi: 10.1016/j.arthro.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Burton HL, Philips AJR, Badhe NP, Olliverre BJ, Moran CG. Proprioception after multiligament knee injury: does ligament repair lead to better proprioceptive acuity than ligament reconstruction? Cureus. 2020;12:e11380. doi: 10.7759/cureus.11380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chahla J, Nelson T, Dallo I, Yalamanchili D, Eberlein S, Limpisvasti O, et al. Anterior cruciate ligament repair versus reconstruction: a kinematic analysis. Knee. 2019 doi: 10.1016/j.knee.2019.10.020. [DOI] [PubMed] [Google Scholar]
- 8.Chowdhry M, Burchette D, Whelan D, Nathens A, Marks P, Wasserstein D. Knee dislocation and associated injuries: an analysis of the American College of Surgeons National Trauma Data Bank. Knee Surg Sports Traumatol Arthrosc. 2020;28:568–575. doi: 10.1007/s00167-019-05712-y. [DOI] [PubMed] [Google Scholar]
- 9.Cook S, Ridley TJ, McCarthy MA, Gao Y, Wolf BR, Amendola A, et al. Surgical treatment of multiligament knee injuries. Knee Surg Sports Traumatol Arthrosc. 2015;23:2983–2991. doi: 10.1007/s00167-014-3451-1. [DOI] [PubMed] [Google Scholar]
- 10.Darcy G, Edwards E, Hau R. Epidemiology and outcomes of traumatic knee dislocations: isolated vs multi-trauma injuries. Injury. 2018;49:1183–1187. doi: 10.1016/j.injury.2018.02.016. [DOI] [PubMed] [Google Scholar]
- 11.Dean RS, DePhillipo NN, Kahat DH, Graden NR, Larson CM, LaPrade RF. Low-energy multiligament knee injuries are associated with higher postoperative activity scores compared with high-energy multiligament knee injuries: a systematic review and meta-analysis of the literature. Am J Sports Med. 2020 doi: 10.1177/0363546520962088363546520962088. [DOI] [PubMed] [Google Scholar]
- 12.Fanelli GC, Edson CJ. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthroscopy. 2002;18:703–714. doi: 10.1053/jars.2002.35142. [DOI] [PubMed] [Google Scholar]
- 13.Fanelli GC, Sousa PL, Edson CJ. Long-term followup of surgically treated knee dislocations: stability restored, but arthritis is common. Clin Orthop Relat Res. 2014;472:2712–2717. doi: 10.1007/s11999-014-3707-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frosch KH, Preiss A, Heider S, Stengel D, Wohlmuth P, Hoffmann MF, et al. Primary ligament sutures as a treatment option of knee dislocations: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1502–1509. doi: 10.1007/s00167-012-2154-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goyal T, Paul S, Banerjee S, Das L. Outcomes of one-stage reconstruction for chronic multiligament injuries of knee. Knee Surg Relat Res. 2021;33:3. doi: 10.1186/s43019-020-00083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heitmann M, Akoto R, Krause M, Hepp P, Schopp C, Gensior TJ, et al. Management of acute knee dislocations: anatomic repair and ligament bracing as a new treatment option-results of a multicentre study. Knee Surg Sports Traumatol Arthrosc. 2019;27:2710–2718. doi: 10.1007/s00167-018-5317-4. [DOI] [PubMed] [Google Scholar]
- 17.Heitmann M, Gerau M, Hotzel J, Giannakos A, Frosch KH, Preiss A. Ligament bracing–augmented primary suture repair in multiligamentous knee injuries. Oper Orthop Traumatol. 2014;26:19–29. doi: 10.1007/s00064-013-0263-2. [DOI] [PubMed] [Google Scholar]
- 18.Hohmann E, Glatt V, Tetsworth K. Early or delayed reconstruction in multi-ligament knee injuries: a systematic review and meta-analysis. Knee. 2017;24:909–916. doi: 10.1016/j.knee.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 19.Ibrahim SA. Primary repair of the cruciate and collateral ligaments after traumatic dislocation of the knee. J Bone Joint Surg Br. 1999;81:987–990. doi: 10.1302/0301-620x.81b6.9516. [DOI] [PubMed] [Google Scholar]
- 20.Ibrahim SA, Ahmad FH, Salah M, Al Misfer AR, Ghaffer SA, Khirat S. Surgical management of traumatic knee dislocation. Arthroscopy. 2008;24:178–187. doi: 10.1016/j.arthro.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 21.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–765. [PubMed] [Google Scholar]
- 22.Jiang W, Yao J, He Y, Sun W, Huang Y, Kong D. The timing of surgical treatment of knee dislocations: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:3108–3113. doi: 10.1007/s00167-014-3435-1. [DOI] [PubMed] [Google Scholar]
- 23.Johnson JP, Kleiner J, Klinge SA, McClure PK, Hayda RA, Born CT. Increased incidence of vascular injury in obese patients with knee dislocations. J Orthop Trauma. 2018;32:82–87. doi: 10.1097/BOT.0000000000001027. [DOI] [PubMed] [Google Scholar]
- 24.Jokela MA, Makinen TJ, Koivikko MP, Lindahl JM, Halinen J, Lindahl J. Treatment of medial-sided injuries in patients with early bicruciate ligament reconstruction for knee dislocation. Knee Surg Sports Traumatol Arthrosc. 2020 doi: 10.1007/s00167-020-06207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kahan JB, Li D, Schneble CA, Huang P, Bullock J, Porrino J, et al. The pathoanatomy of posterolateral corner ligamentous disruption in multiligament knee injuries is predictive of peroneal nerve injury. Am J Sports Med. 2020;48:3541–3548. doi: 10.1177/0363546520962503. [DOI] [PubMed] [Google Scholar]
- 26.Kobsar D, Charlton JM, Tse CTF, Esculier JF, Graffos A, Krowchuk NM, et al. Validity and reliability of wearable inertial sensors in healthy adult walking: a systematic review and meta-analysis. J Neuroeng Rehabil. 2020;17:62. doi: 10.1186/s12984-020-00685-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kyhos J, Johnson D, Alvandi B, Terry M, Tjong V. Multi-ligament reconstructions as a risk factor for adverse outcomes in arthroscopic surgery. Knee Surg Sports Traumatol Arthrosc. 2020 doi: 10.1007/s00167-020-06252-6. [DOI] [PubMed] [Google Scholar]
- 28.Lai PP, Leung AK, Li AN, Zhang M. Three-dimensional gait analysis of obese adults. Clin Biomech (Bristol, Avon) 2008;23(Suppl 1):S2–6. doi: 10.1016/j.clinbiomech.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 29.Levy BA, Dajani KA, Whelan DB, Stannard JP, Fanelli GC, Stuart MJ, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25:430–438. doi: 10.1016/j.arthro.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 30.Liow RY, McNicholas MJ, Keating JF, Nutton RW. Ligament repair and reconstruction in traumatic dislocation of the knee. J Bone Joint Surg Br. 2003;85:845–851. [PubMed] [Google Scholar]
- 31.Moatshe G, Dornan GJ, Ludvigsen T, Loken S, LaPrade RF, Engebretsen L. High prevalence of knee osteoarthritis at a minimum 10-year follow-up after knee dislocation surgery. Knee Surg Sports Traumatol Arthrosc. 2017;25:3914–3922. doi: 10.1007/s00167-017-4443-8. [DOI] [PubMed] [Google Scholar]
- 32.Mosquera MF, Jaramillo A, Gil R, Gonzalez Y. Controversies in acute multiligamentary knee injuries (MLKI) J Exp Orthop. 2020;7:56. doi: 10.1186/s40634-020-00260-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Noble PC, Scuderi GR, Brekke AC, Sikorskii A, Benjamin JB, Lonner JH, et al. Development of a new Knee Society scoring system. Clin Orthop Relat Res. 2012;470:20–32. doi: 10.1007/s11999-011-2152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Noyes FR, Barber-Westin SD. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Use of early protected postoperative motion to decrease arthrofibrosis. Am J Sports Med. 1997;25:769–778. doi: 10.1177/036354659702500608. [DOI] [PubMed] [Google Scholar]
- 35.Plancher KD, Siliski J. Long-term functional results and complications in patients with knee dislocations. J Knee Surg. 2008;21:261–268. doi: 10.1055/s-0030-1247829. [DOI] [PubMed] [Google Scholar]
- 36.Qin C, Roth C, Lee C, Athiviraham A. National trends, 90-day readmission and subsequent knee surgery following multi-ligament knee reconstruction. J Orthop. 2020;21:49–52. doi: 10.1016/j.jor.2020.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ramirez-Bermejo E, Gelber PE, Pujol N. Management of acute knee dislocation with vascular injury: the use of the external fixator. A systematic review. Arch Orthop Trauma Surg. 2020 doi: 10.1007/s00402-020-03684-0. [DOI] [PubMed] [Google Scholar]
- 38.Richter M, Bosch U, Wippermann B, Hofmann A, Krettek C. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med. 2002;30:718–727. doi: 10.1177/03635465020300051601. [DOI] [PubMed] [Google Scholar]
- 39.Ridley TJ, Cook S, Bollier M, McCarthy M, Gao Y, Wolf B, et al. Effect of body mass index on patients with multiligamentous knee injuries. Arthroscopy. 2014;30:1447–1452. doi: 10.1016/j.arthro.2014.05.035. [DOI] [PubMed] [Google Scholar]
- 40.Rihn JA, Groff YJ, Harner CD, Cha PS. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg. 2004;12:334–346. doi: 10.5435/00124635-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 41.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)-development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 42.Schenck RC., Jr The dislocated knee. Instr Course Lect. 1994;43:127–136. [PubMed] [Google Scholar]
- 43.Shapiro MS, Freedman EL. Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation. Am J Sports Med. 1995;23:580–587. doi: 10.1177/036354659502300511. [DOI] [PubMed] [Google Scholar]
- 44.Slater LV, Hart JM, Kelly AR, Kuenze CM. Progressive changes in walking kinematics and kinetics after anterior cruciate ligament injury and reconstruction: a review and meta-analysis. J Athl Train. 2017;52:847–860. doi: 10.4085/1062-6050-52.6.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sobrado MF, Giglio PN, Bonadio MB, Pecora JR, Gobbi RG, Angelini FJ, et al. High incidence of osteoarthritis observed in patients at short- to midterm follow-up after delayed multiligament knee reconstruction. J Knee Surg. 2021 doi: 10.1055/s-0040-1722348. [DOI] [PubMed] [Google Scholar]
- 46.Strobel MJ, Schulz MS, Petersen WJ, Eichhorn HJ. Combined anterior cruciate ligament, posterior cruciate ligament, and posterolateral corner reconstruction with autogenous hamstring grafts in chronic instabilities. Arthroscopy. 2006;22:182–192. doi: 10.1016/j.arthro.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 47.Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 43–49 [PubMed]
- 48.Trasolini NA, Lindsay A, Gipsman A, Rick Hatch GF. The biomechanics of multiligament knee injuries: from trauma to treatment. Clin Sports Med. 2019;38:215–234. doi: 10.1016/j.csm.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 49.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 50.Werner BC, Gwathmey FW, Jr, Higgins ST, Hart JM, Miller MD. Ultra-low velocity knee dislocations: patient characteristics, complications, and outcomes. Am J Sports Med. 2014;42:358–363. doi: 10.1177/0363546513508375. [DOI] [PubMed] [Google Scholar]
- 51.Woodmass JM, Johnson NR, Mohan R, Krych AJ, Levy BA, Stuart MJ. Poly-traumatic multi-ligament knee injuries: is the knee the limiting factor? Knee Surg Sports Traumatol Arthrosc. 2018;26:2865–2871. doi: 10.1007/s00167-017-4784-3. [DOI] [PubMed] [Google Scholar]
- 52.Woodmass JM, O'Malley MP, Krych AJ, Reardon PJ, Johnson NR, Stuart MJ, et al. Revision multiligament knee reconstruction: clinical outcomes and proposed treatment algorithm. Arthroscopy. 2018;34(736–744):e733. doi: 10.1016/j.arthro.2017.09.022. [DOI] [PubMed] [Google Scholar]
- 53.Yeo JH, Seon JK, Lee DH, Song EK. No difference in outcomes and gait analysis between mechanical and kinematic knee alignment methods using robotic total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27:1142–1147. doi: 10.1007/s00167-018-5133-x. [DOI] [PubMed] [Google Scholar]
- 54.Zhao D, Yang Z, Wu C, Zhong J, Zhou X, Li J, et al. The outcomes of one-stage treatment for multiple knee ligament injuries combined with extensor apparatus rupture. BMC Musculoskelet Disord. 2020;21:450. doi: 10.1186/s12891-020-03470-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.