Abstract
Objective
The current study examined trajectories of anxiety and depression symptoms at three-time points during the COVID-19 pandemic and examined correlates of those trajectories.
Design
Data were collected at three time points during the COVID-19 pandemic.
Participants
The sample in the current study consisted of 804 respondents who had completed the online questionnaire at all three time points designed for the study.
Results
Using Latent Growth Mixture Modeling (LGMM) we identified four trajectories: (a) A resilient group reported consistently low levels of symptoms (62% anxiety and 72% depression), (b) a chronic group reported consistently high levels of symptoms (12% anxiety and 14% depression), (c) an emerging group reported low initial symptoms that increased steadily across time (20% anxiety and 13% depression), and (d) an improving group reported high initial symptoms that decreased across time (6% anxiety and 3% depression).
Conclusions
The salient conclusion that emerged from these results is that even in a severe and prolonged crisis, such as the COVID-19 pandemic, the most common outcome in the population is that of resilience. Moreover, examining predictors of these trajectories, we found that the resilience trajectory was associated with fewer economic difficulties due to the COVID-19, greater income, and self-identification as religious.
Keywords: Anxiety, Depression, Trajectories, COVID-19, Longitudinal study
1. Introduction
The COVID-19 pandemic originated in China towards the end of 2019 and in a short time spread to 213 countries and territories (WHO, 2019). This pandemic is a clear and tangible threat to all humans. Research suggests that the COVID-19 pandemic has affected and will continue to exert enduring effects on mental health (Kontoangelos et al., 2020), economic (Fernandes, 2020), physical health (Saltzman et al., 2020), and social interactions (Fancourt et al., 2020; Settersten et al., 2020).
1.1. Anxiety and depression during COVID-19
Distress symptoms have been one of the most salient responses to the pandemic (Cullen et al., 2020). These include continuous emotional and behavioral difficulties such as depression and anxiety symptoms (Ettman et al., 2020; Islam et al., 2020). Earlier studies that explored these symptoms during the COVID-19 pandemic reported mixed results across varied times of measurement, countries, and cultures. For example, Kimhi et al. (2020) found an increased level of anxiety and depression symptoms during the COVID-19 pandemic in Israel. Tan et al. (2020) identified various three-class trajectories of “panic” in China based on a single, self-report question. O'Connor et al. (2020) examined changes in anxiety and depressive symptoms across three waves of the pandemic and reported that women, young people (between 18 and 29 years), individuals from lower socioeconomic levels, or previous mental health problems were more severely affected.
LGMM is ideal for tracking patterns of change over time because it does not assume data homogeneity but, rather, allows for the parsing of distinct subgroups of individuals who share similar patterns of change across time (Jung and Wickrama, 2008; Muthén, 2004; Nagin and Odgers, 2010). Previous studies using LGMM, following a wide range of aversive or potentially traumatic stressor events, have consistently documented a common set of prototypical outcome trajectories (Bonanno et al., 2010, Bonanno et al., 2015; Chen and Bonanno, 2020). These include: (a) a trajectory of consistently low symptom levels or resilience, (b) a chronic trajectory of consistently elevated symptoms, (c) an emerging trajectory of increasing symptoms over time, and (d) an improving trajectory of initially elevated symptoms that gradually decrease over time (Bonanno, 2004; Galatzer-Levy et al., 2018). In the current study, we examined whether these same prototypical trajectories would also effectively capture a longitudinal change in anxiety and depression among a Jewish population of Israelis during the COVID-19 crisis.
The rationale for the present study is based on an effort to better understand, based on repeated measurements throughout the COVID-19 crisis in Israel, two main issues: (a) how patterns of anxiety and depressive symptoms change over time and (b) the demographic factors, income, economic difficulties, and religious identity, associated with these trajectory patterns. To our knowledge, no study has yet systematically examined depression and anxiety trajectories using an unsupervised computational approach, such as Latent Growth Mixture Modeling (LGMM), during the COVID-19 pandemic.
1.2. COVID-19 in Israel
The COVID-19 outbreak in Israel was initially recognized on February 27, 2020. As of February 7, 2021, there were 5074 dead and 615,178 COVID-19 cases in Israel attributed to the pandemic (Worldometer, 2020). Israel was ranked (as of November 30, 2020) 48th in the world in the number of death from COVID-19, per million people (311 deaths per million inhabitants). Four waves of the COVID-19 pandemic were experienced in Israel; the first three waves (March–April 2020, August–October 2020, and December 2020–February 2021; Muhsen and Cohen, 2021) resulted in the initiation of national lockdowns (Ram et al., 2021). At the peak of the first wave, 500–700 newly daily confirmed cases were identified, compared to 4000–6000 in the peak of the second wave, and8000 cases in the peak of the third wave (Birenbaum-Carmeli and Chassida, 2021; Ram & al., 2021). In the midst of the third wave, the national vaccination campaign was launched. The fourth wave of the COVID-19 pandemic started in July 2021.
Two additional stressful events occurred in Israel during the course of the pandemic that likely further compounded the stress from COVID-19: First, the pandemic materialized in parallel to an ongoing political crisis (e.g., three elections that took place in the past two years and another election campaign that was in its midst). Second, an economic crisis which is partly a byproduct of the political crisis (e.g., failure to approve the state budget for 2020) and partly a consequence of the pandemic management itself (mass unemployment rates resulting from partial or full lockdowns). The result is a "multidimensional crisis" that encompasses the health, economic, and political systems (Gesser-Edelsburg et al., 2020). It has been claimed that the current crisis constitutes the most severe adversity since the establishment of the State of Israel (Maor et al., 2020).
1.3. Demographic and personal characteristics
The impact of the COVID-19 crisis on different populations within Israel was found to vary markedly according to the affiliation to unique subpopulations, such as religious Ultra-Orthodox Jewish populations or Arab minority groups (Shadmi et al., 2020). Previous studies in Israel have shown significant associations between population demographics as well as personal attributes and distress symptoms: economic difficulties, due to the pandemic crisis, positively correlated with distress symptoms, while levels of income and age negatively correlated with distress (Kimhi, Marciano, Eshel, & Adini, 2020, 2020a; Sharabi and Kay, 2021). Gender differences were also found regarding distress symptoms, with women displaying a higher level of distress, compared with men (Kimhi et al., 2020a, Kimhi et al., 2020b, Kimhi et al., 2020c, Kimhi et al., 2020d). Furthermore, a recent meta-analysis presented a moderate positive association between resilience and religiosity (Schwalm et al., 2021). However, no study has examined the associations between these demographic variables and longitudinal trajectories of anxiety and depressive symptoms.
To summarize, in the current study we examined trajectories of anxiety and depression symptoms, development and modification of these symptoms over time. Based on previous findings (Bonanno et al., 2010, 2015), we anticipated that the majority of individuals in our study would show a resilience trajectory, while less frequent outcomes would be characterized by either a chronic symptom trajectory, an emerging symptom trajectory, or an improving symptom trajectory. The second aim of our study was to explore associations between these trajectories and several demographic and personal variables that have shown associations with distress in previous studies and, in particular, levels of religiosity, income, and economic difficulties. We explored these associates as an open research question. To the best of our knowledge, this issue has not yet been investigated.
2. Method
2.1. Participants
Data were garnered with the aid of an internet panel company, that utilizes a database of approximately 65,000 people, representing all demographic groups and geographic locations in Israel (https://sekernet.co.il/). A stratified sampling method was employed, aligned with the data published by the Israeli Central Bureau of Statistics, to appropriately include the varied groups of the Israeli population in terms of gender, age, and geographic dispersal. The exclusion criteria included individuals aged less than 18.
Data were available at three-time points during the COVID-19 pandemic: in May 2020 (n = 1100), July 2020 (n = 906), and October 2020 (n = 804). All three measurements pre-dated the development of an approved vaccine for the COVID-19. Due to the loss of respondents across the three measurements, we compared the demographic and personal characteristics, to examine whether there were any significant differences in age, religiosity, family income, political attitudes, economic difficulties, and the number of children across the three samples. Only one significant difference emerged: participants of the reduced sample at the third measurement were slightly older (M = 44.63, sd = 15.40) compared with age in the first (M = 42.81, sd = 15.47) and second (M = 44.08, sd = 15.53) measurements (F(2,2807) = 3.53, p < 0.05, small effect size).
The sample for the current study included respondents who had completed the online questionnaire at each of the three time points designed for the study (N = 804). The sample size was determined before any data analysis. The questionnaire was approved by the Ethics Committee of Tel Aviv University, number 0001150-1 from April 7th, 2020, and an informed consent form was signed by all participants (Table 1 ).
Table 1.
Demographic characteristics of the respondents (N = 804).
| Variable | Group | No. of respondents | % | Average (S.D) |
|---|---|---|---|---|
| Age | 18–30 | 171 | 21 | 44.65 (15.40) |
| 31–40 | 191 | 24 | ||
| 41–60 | 151 | 19 | ||
| 51–60 | 141 | 17 | ||
| 61–82 | 150 | 19 | ||
| Gender | Male | 416 | 52 | |
| Female | 388 | 48 | ||
| Level of religiosity | Secular | 398 | 49 | |
| Traditional | 231 | 29 | ||
| Religious | 107 | 13 | ||
| Very religious (ultra-orthodox) | 68 | 8 | ||
| Family income relative to average in Israel | 1. Much lower | 206 | 26 | 2.54 (1.21) |
| 2. Lower | 198 | 25 | ||
| 3. About average | 204 | 25 | ||
| 4. Above | 153 | 19 | ||
| 5. Much above | 43 | 5 | ||
| Political attitudes | 1. Strong left | 7 | 1 | 3.45 (.83) |
| 2. Left | 94 | 12 | ||
| 3. Center | 272 | 34 | ||
| 4. Right | 360 | 45 | ||
| 5. Strong right | 71 | 9 | ||
| Education | 1. Elementary | 5 | .6 | |
| 2. High school | 192 | 24 | ||
| 3. Above high school, no B.A | 277 | 34 | ||
| 4. B.A. | 208 | 26 | ||
| 5. M.A. and above | 122 | 15 | ||
| Family status | 1. Bachelor | 177 | 22 | |
| 2. Married | 507 | 63 | ||
| 3. Divorce | 68 | 8 | ||
| 4. Widowed | 8 | 1 | ||
| 5. living in partnership | 44 | 5 | ||
| Number of children | 1. No children | 253 | 31 | |
| 2. One child | 84 | 10 | ||
| 3. 2–3 children | 338 | 42 | ||
| 4. 4–5 children | 98 | 12 | ||
| 5. 6 and above | 31 | 2 | ||
| Economic difficulties due to the pandemic (during third measurement) | 1. Not at all | 178 | 22 | |
| 2. To a small extent | 209 | 26 | 2.61 | |
| 3. To a moderate extent | 237 | 29 | (1.22) | |
| 4. To a great extent | 105 | 13 | ||
| 5. To a very great extent | 75 | 9 |
2.2. Measures
2.2.1. Depression and anxiety symptoms
Two subscales of the Brief Symptom Inventory (BSI) scale (Derogatis and Savitz, 2000) were employed in the current study: depression (5 items) and anxiety (3 items). Due to ethical reasons, the item regarding suicidal thoughts was removed from the scale. Respondents were asked to report the extent to which they are currently suffering from any of the problems presented. The response scale ranged from 1 = not at all to 5 = to a very large extent, and the internal reliabilities were high: Depression: T1, α=.88; T2, α=.89, and T3, α=.88; Anxiety: T1, α=.77, T2, α=.78, and T3, α=.77.
2.2.2. Demographic characteristics
Respondents reported nine demographic variables: age (18–30, 31–40, 41–60. 60 + ), gender (1 = male, 2 = female), level of religiosity (1 = non-religious to 4 = very religious), family income relative to the average income in Israel (1 = much lower than the national average to 5 = much higher than the national average), political attitudes (1 = extreme left to 5 = extreme right), level of education (1 = elementary to 5 = graduate degree and higher), number of children (no children to 4 children or more), and economic difficulties (experiencing financial hardship such as unemployment, reduced business activity, etc.) due to the COVID-19 pandemic (1 = not at all, to 5 = to a very much degree) (see Table 1).
2.3. Statistical analysis
As a preliminary analysis, we examined correlations between the variables and used analysis of variance to examine differences of anxiety and depression averages, across the three repeated measurements. Next, we employed Latent Growth Mixture Modeling (LGMM) using Mplus (Version 8.1; Muthén and Muthén, 2017) to identify the best-fitting trajectories of anxiety and depression symptoms across the three-time points. Best-fitting class solutions were determined by testing successive models of increasing complexity with variations in the estimation of intercept, slope, and quadratic parameters. Models with increasing numbers of classes were compared against Akaike (AIC), Bayesian (BIC), and sample-size-adjusted Bayesian (SSBIC) information criteria, entropy values, and, for comparing k vs. k-1 model-fit, the adjusted Lo-Mendell-Rubin test (A-LRT). Interpretability, model parsimony, and theoretical coherence were also considered in the selection of the optimal unconditional model (Bonanno, 2004; Muthén, 2004). Following identification of the final unconditional models for both anxiety and depression symptoms, we examined overall concordance in trajectory membership across symptom types and compared the frequency of membership in each trajectory relative to chance using Haberman's (1978) standardized, adjusted residual (HAR). Next, we examined a set of baseline covariates for inclusion in conditional trajectory models of each trajectory. Finally, we examined economic difficulties due to COVID at each time point concerning the conditional trajectories using repeated measures ANOVAs.
In these studies, we report all measures, manipulations, and exclusions.
3. Results
3.1. Correlations and long-term change among the study variables
Correlations among the variables are presented in Table 2 . Differences in average-level anxiety and depression symptoms across the three repeated measurements are presented in Table 3 . Anxiety increased significantly between T1 and T2 (small effect size) but did not change significantly at T3. Depression increased significantly between all three measurements (small effect sizes).
Table 2.
Correlations between anxiety and depression ant the demographic variables, and economic difficulties, across 3 repeated measures.
| Depression | Gender | Age | Religiosity | Income | children | Political attitudes | Education | Economic difficulties | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety | T1 | .76*** | .14*** | -.16*** | .06 | -.12*** | -.13*** | .01 | -.04 | .29*** |
| T2 | .79*** | .15*** | -.10** | .10** | -.12*** | -.11** | .00 | .00 | .32*** | |
| T3 | .78*** | .13*** | -.06 | -.18*** | -.15*** | -.09** | -.05 | .04 | .35*** | |
| Depression | T1 | – | .10** | -.18*** | -.12*** | -.19*** | -.22*** | -.02 | -.09** | .29*** |
| T2 | – | .10 | -.12*** | -.16*** | -.18*** | -.18*** | -.05 | -.04 | .31*** | |
| T3 | – | .12*** | -.14*** | -.20*** | -.16*** | -.18*** | -.10* | -.03 | .36*** | |
*p < 0.05, **p < 0.01, ***p < 0.001.
Table 3.
General Linear Model – Repeated three measures of anxiety and depressive symptoms (N = 804).
| Symptoms | T1 |
T2 |
T3 |
F(1,803) | Partial Eta Squared | |||
|---|---|---|---|---|---|---|---|---|
| M | S.D | M | S.D | M | S.D | |||
| Anxiety | 2.46a | .90 | 2.60b | .94 | 2.59b | .93 | 24.22*** | .03 |
| Depression | 2.08a | .95 | 2.16b | 1.00 | 2.26c | 1.00 | 19.55*** | .02 |
***p < 0.001, a,b,c = Pairwise comparison.
3.2. Trajectories of anxiety symptoms
3.2.1. Unconditional models
We tested 1–5 class solutions of anxiety symptoms, allowing the variance of the intercept to be freely estimated across classes while fixing the slope parameter to facilitate model convergence. These analyses indicated a good model convergence, continued improvement model fit, and adequate entropy through 4 classes (see Table 4 ). The 5-class solution yielded an increased BIC and slightly increased entropy but decreased fit in other indices, most notably a non-significant comparison value on the A-LRT. These statistics, in conjunction with considerations of model coherence and interpretability (Bonanno, 2004; Nagin and Odgers, 2010), clearly indicated that the 4-class model was optimal.
Table 4.
Fit Indices for latent growth mixture models of anxiety and depression symptoms (n = 804).
| Models for anxiety symptoms | ||||||||
|---|---|---|---|---|---|---|---|---|
| Statistic | One class | Two class | Three class | Four class | Five class | |||
| AIC | 5287.21 | 5335.95 | 5304.14 | 5277.89 | 5269.19 | |||
| BIC | 5415.35 | 5378.16 | 5360.57 | 5348.26 | 5353.62 | |||
| SSBIC | 5396.30 | 5349.59 | 5322.47 | 5300.62 | 5296.46 | |||
| Entropy | – | .50 | .70 | .70 | .72 | |||
| A-LRT | – | 54.54 | 35.87 | 30.85 | 14.00 | |||
| A-LRT p-value |
(<.01) |
(<.05) |
(<.05) |
(.42) |
||||
| Models for depression symptoms | ||||||||
| Statistic | One class | Two class | Three class | Four class | Five class | Six class | ||
| AIC | 5707.33 | 5590.60 | 5533.62 | 5474.98 | 5423.98 | 5407.72 | ||
| BIC | 5735.48 | 5632.82 | 5589.91 | 5535.35 | 5507.92 | 5506.22 | ||
| SSBIC | 5716.42 | 5604.24 | 5551.80 | 5497.71 | 5450.76 | 5439.53 | ||
| Entropy | – | .73 | .77 | .82 | .81 | .79 | ||
| A-LRT | – | 116.90 | 60.00 | 61.56 | 54.77 | 20.73 | ||
| A-LRT p-value | (<.001) | (<.05) | (<.05) | (<.05) | (p = 0.49) | |||
Note: AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion; SSBIC = Sample Size Adjusted Bayesian Information Criterion; A-LRT = Adjusted Lo-Mendell-Rubin Likelihood Ratio Test.
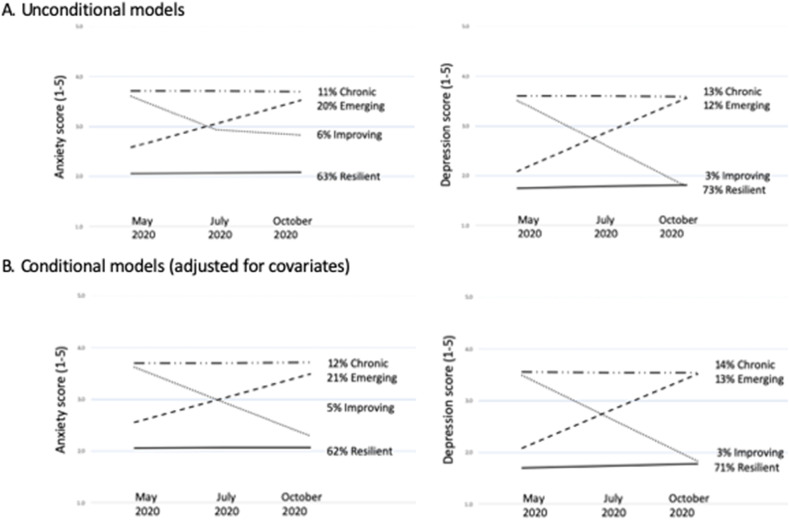
Trajectories of anxiety symptoms for the 4-class model are depicted in Fig. 1 a. The largest class was a Resilience trajectory (63%) characterized by low levels of anxiety throughout the 6 months. The resilient class was characterized by a low intercept (b = 2.06, SE = 0.05, p < 0.001) and a non-significant slope (b = 0.01, SE = 0.02, p = 0.51). The next largest was an Emerging Anxiety trajectory (20%), with relatively low initial anxiety that increased markedly across the 6-month study. This class was characterized by a relatively low intercept (b = 2.58, SE = 0.12, p < 0.001), and a significant positive slope (b = 0.47, SE = 0.07, p < 0.001). The third-largest class was a trajectory of Chronic Anxiety (11%), characterized by consistently high anxiety scores at each time point. This class had a significant intercept (b = 3.71, SE = 0.19, p < 0.001) and a non-significant slope (b = −0.01, SE = 0.08, p = 0.95). Finally, we observed an Improving class (6%) with high initial anxiety that improved by T2 and then improved slightly again by the third time point. This trajectory was characterized by a high intercept (b = 3.60 SE = 0.14, p < 0.001) and a significant negative slope (b = −0.66, SE = 0.11, p < 0.001).
Fig. 1.
Unconditional and conditional models of anxiety trajectories.
3.2.2. Conditional anxiety trajectories adjusted for covariates
We tested the following variables as possible covariates in a condition model for the anxiety trajectories: age, sex, family income, education, number of children, religious identity, family status, and political attitudes. Only two variables successfully distinguished anxiety trajectory membership: family income and religious identity. Logistic regressions conducted within the conditional analysis (see Annex 1) indicated that individuals in the resilience trajectory were more religious and had greater income than both the chronic and emerging anxiety classes but did not significantly differ from the improving class. However, improving individuals were also more religious than chronic and emerging anxiety classes.
Inclusion of covariates in the conditional model resulted in anxiety trajectories that were highly similar to those from the unconditional model (see Fig. 1b).The Resilience trajectory (62%) was again characterized by a low intercept (b = 2.06, SE = 0.05, p < 0.001) and a non-significant slope (b = 0.01, SE = 0.02, p = 0.68); the Emerging Anxiety trajectory (21%) again by a relatively low intercept (b = 2.55, SE = 0.12, p < 0.001), and significant positive slope (b = 0.47, SE = 0.08, p < 0.001), the Chronic Anxiety trajectory (12%) again by high intercept (b = 3.70, SE = 0.22, p < 0.001) and a non-significant slope (b = −0.01, SE = 0.10, p = 0.94), and the Improving trajectory (5%) again by a high intercept (b = 3.61 SE = 0.17, p < 0.001) and a significant negative slope (b = −0.66, SE = 0.11, p < 0.001).
3.3. Trajectories of depression symptoms
3.3.1. Unconditional models
We repeated the same analyses for depression symptoms, testing 1–6 class solutions and again allowing the variance of the intercept to be freely estimated across classes while fixing the slope parameter to facilitate model convergence. We observed good model convergence, continued improvement model fit, and adequate entropy through 5 classes (see Table 2). The 6-class solution yielded increased fit on the AIC, BID, and SSBIC but had a slightly smaller intercept and, critically, a non-significant comparison value on the A-LRT. Although the 5-class solution showed improved fit over the 4-class solution, it produced several small classes and thus suggested an unstable and relatively less interpretable model. Based on these considerations, we chose the 4-class model as optimal. The 4-class solution also had the added benefit of theoretical continuity and interpretability concerning the 4-class solution for anxiety symptoms.
Trajectories of depression symptoms for the 4-class model are depicted in Fig. 1a. The largest class was again a Resilience trajectory (73%) characterized by low levels of depression throughout the 6 months. The resilient class was characterized by a low intercept (b = 1.74, SE = 0.05, p < 0.001) and a non-significant slope (b = 0.37, SE = 0.20, p = 0.07). The Emerging Anxiety trajectory (12%) was characterized by a relatively low intercept (b = 2.08, SE = 0.11, p < 0.001), and a significant positive slope (b = 0.74, SE = 0.10, p < 0.001). The Chronic Anxiety (12%) was characterized by a high intercept (b = 3.60, SE = 0.17, p < 0.001) and a flat, non-significant slope (b = −0.01, SE = 0.06, p = 0.97). Finally, we observed a relatively small Improving class (3%) with a high intercept (b = 3.51, SE = 0.28, p < 0.001) and a steep negative slope (b = −0.86, SE = 0.19, p < 0.001).
3.3.2. Conditional depression trajectories adjusted for covariates
We tested the same candidate covariates for inclusion in a conditional model for the depression trajectories. Income and religious identity again distinguished the trajectories, as did an additional covariate, sex. Logistic regressions conducted within the conditional analysis (see Annex 1) indicated that individuals in the resilience trajectory were more likely to be female than the emerging anxiety class, more religious than both the chronic and emerging anxiety classes, and had greater income than all other classes. No other significant class differences emerged.
Inclusion of covariates in the conditional model also resulted in depression trajectories that were highly similar to those of the unconditional model (see Fig. 1b). The Resilience trajectory (71%) was again characterized by a low intercept (b = 1.71, SE = 0.05, p < 0.001) and a non-significant slope (b = 0.35, SE = 0.20, p = 0.07). The Emerging Anxiety trajectory (13%) was characterized by a relatively low intercept (b = 2.09, SE = 0.12, p < 0.001), and a significant positive slope (b = 0.71, SE = 0.12, p < 0.001). The Chronic Anxiety (12%) was characterized by a high intercept (b = 3.55, SE = 0.22, p < 0.001) and a flat, non-significant slope (b = −0.01, SE = 0.07, p = 0.95). Finally, we observed a relatively small Improving class (3%) with a high intercept (b = 3.48, SE = 0.28, p < 0.001) and a steep negative slope (b = −0.82, SE = 0.19, p < 0.001).
3.4. Convergence across conditional anxiety and depression trajectories
We next examined the overlap in trajectory membership for conditional anxiety and depression. This analysis revealed a significant, non-random distribution across the four outcome patterns, χ2(9, N = 803) = 536.90, p < 0.001. Concordance was very high for resilience, with the vast majority in the resilience trajectory for anxiety (92.3%) also in the resilience trajectory for depression, HAR = 17.3, p < 0.001. Concordance was reduced but still observed in a majority of individuals (60.2%) for the chronic anxiety trajectory and chronic depression trajectory, HAR = 14.2, p < 0.001. However, concordance was lesser, observed in only slightly more than one-third of individuals, for emerging anxiety and emerging depression (39.2%), HAR = 11.6, p < 0.001, and for improving anxiety and improving depression (34.9%), HAR = 11.8, p < 0.001. These latter findings suggest that change in anxiety and depression differs across individuals.
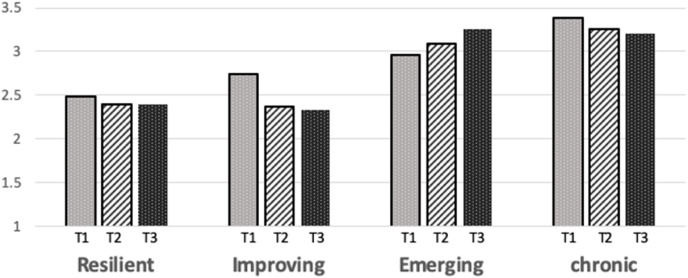
3.5. Trajectories and COVID-19-related economic difficulties over time
In a final set of analyses, we examined the conditional anxiety and depression trajectories about self-reported economic difficulties attributed to the COVID-19 pandemic at each time point. A repeated-measures ANOVA using the anxiety trajectories as the between-subjects factor revealed significant main effects of time [F(2, 799) = 3.28, p < 0.05], and trajectory [F(3, 799) = 38.57, p < 0.001], but a non-significant interaction of time and trajectory [F(6,799) = 1.24, p = 0.281] (see Table 5 ). Post-hoc pair-wise comparisons, with significance set at p < 0.05, indicated that COVID-related economic difficulties decreased from T1 to T2 but did not differ from T2 to T3. Besides, individual resilience reported fewer COVID-19-related economic difficulties overall than improving individuals, and improving individuals, in turn, reported fewer COVID-19-related economic difficulties than emerging and chronic anxiety individuals.
Table 5.
Economic difficulties at each time point in relation to the conditional (adjusted) trajectories for anxiety and depression.
| Conditional anxiety trajectories | T1 econ difficulties | T2 econ difficulties | T3 econ difficulties | Time | Trajectory | Time X Trajectory | |
|---|---|---|---|---|---|---|---|
| Resilient | 2.40 (1.16) | 2.31 (1.08) | 2.32 (1.13) | 2.34 (1.27)a | 3.28* | 38.57*** | 1.24 |
| Improving | 2.81 (1.30) | 2.60 (1.42) | 2.53 (1.33) | 2.65 (4.33)b | |||
| Emerge | 3.08 (1.14) | 3.06 (1.16) | 3.17 (1.12) | 3.11 (2.18)c | |||
| Chronic | 3.37 (1.22) | 3.24 (1.17) | 3.19 (1.30) | 3.27 (2.94)c | |||
|
|
2.91(1.70)a |
2.80(1.64)b |
2.81(1.67)b |
||||
| Conditional depression trajectories | |||||||
| T1 econ difficulties | T2 econ difficulties | T3 econ difficulties | Time | Trajectory | Time X Trajectory | ||
| Resilient | 2.49 (1.18) | 2.39 (1.14) | 2.40 (1.17) | 2.43 (1.21)a | 2.51 | 29.83*** | 3.24** |
| Improve | 2.74 (1.23) | 2.37 (1.08) | 2.33 (1.30) | 2.48 (5.55)a | |||
| Emerge | 2.96 (1.15) | 3.09 (1.10) | 3.25 (1.61) | 3.10 (2.86)b | |||
| Chronic | 3.38 (1.26) | 3.26 (1.21) | 3.21 (1.18) | 3.29 (2.80)b | |||
| 2.89 (2.02)a | 2.78 (1.96)b | 2.80 (1.98)ab | |||||
A similar repeated-measures ANOVA using depression trajectories revealed a marginal time effect [F(2, 799) = 2.41, p = 0.10], a significant effect of trajectory [F(3, 799) = 29.83, p < 0.001], and a qualifying interaction of time and trajectory interaction [F(6, 799) = 3.24, p < 0.005] (see Table 3). Post-hoc pair-wise comparisons (p < 0.05), again showed a decrease in economic difficulties from T1 to T2. Post-hoc comparisons also indicated that resilient and improving individuals did not differ from each other but also that both groups reported fewer COVID-19-related economic difficulties than emerging and chronic anxiety individuals who, in turn, did not differ from each other. Visual inspection of the cell means comprising the trajectory × time interaction (see Fig. 2 ) suggested that: a) the chronic group reported high and relatively stable economic difficulties; b) the resilient group reported low and relatively stable economic difficulties; c) the improved group reported lessening economic difficulties over time, and d) the emerging group reported worsening economic difficulties over time. Thus, at each time point, levels of mental distress appear to correspond with the economic situation. Pair-wise comparisons (p < 0.05) confirmed this impression. At T1, the chronic trajectory had significantly greater economic difficulties than all other groups but by T2 both the chronic and emerging trajectories had similarly high levels of economic difficulties and were significantly higher in economic difficulties than the improving and resilient group.
Fig. 2.
Economic difficulties due to the COVID in relation to conditional anxiety and depression trajectories.
4. Discussion
The present study examined trajectories of anxiety and depression during the COVID-19 pandemic across three time points in a representative sample of the adult Jewish population in Israel. LGMM revealed four patterns of depression and anxiety symptoms: (a) a resilience trajectory of stable low symptoms (62% anxiety and 72% depression), (b) a chronic symptom trajectory (12% anxiety and 24% depression), (c) an emerging symptoms trajectory (20% anxiety and 13% and depression), and (d) an improving symptom trajectory (6% anxiety and 3% depression). Overall, our results were highly consistent with the prototypical patterns of trajectories observed in previous studies of highly aversive life events (Galatzer-Levy et al., 2018).
Identification of these trajectories in the context of the COVID-19 pandemic highlights the need for follow-up research on these groups, in particular, to establish the duration of the pandemic's impact and to further probe its association with the demographic variables identified in this study. In past research, a resilient pattern of the duration observed in the current study has not varied tended to change. However, delayed elevations in symptoms may occur in some individuals. When delayed symptoms do occur, people showing this pattern typically had earlier experienced moderate to sub-threshold symptom levels and then gradually worse (Andrews and Brewing, 2007; Bryant and Harvey, 2002; Bonanno et al., 2010). However, the pandemic has presented an especially long period of chronic stress and, as noted earlier for Israel, often has been laid with other imposing stressor events. It would be informative as well to further explore why some people recover from elevated symptoms and some do not. This distinction could suggest implications for potentially effective intervention programs (Barzilay et al., 2020, Sheerin et al., 2018).
We found that family income and level of religiosity significantly differentiated between the resilience, chronic and emerging trajectory groups: lower family income and lower levels of religiosity were linked to a higher level of symptoms. However, these relationships differed to some extent depending on the type of symptom the trajectories were based on. Family income and level of religiosity significantly distinguished between resilience trajectory and improving trajectories for depression but not for anxiety. Conversely, the level of religiosity distinguished the improving and emerging trajectories for anxiety but not for depression. Overall, however, our results are consistent with previous studies that point to the positive role of religion in dealing with the COVID pandemic among Jewish samples (Pirutinsky et al., 2020).
The predictive relations of gender and COVID-related economic difficulties also varied by symptom trajectory. Gender significantly distinguished between resilience trajectory and emerging trajectory for depression, but not for anxiety. Although economic difficulties due to the COVID-19 showed generally similar patterns across symptom types, the resilience trajectory for anxiety had the fewest economic difficulties compared to all other groups, while the resilience trajectory for depression did not differ in economic difficulties from the improving trajectory for depression.
When considered in the context of the study's limitations delineated below, our findings nonetheless demonstrate the importance of mapping longitudinal patterns of outcome during the COVID pandemic. Our findings, as well as those from previous studies, indicated that most people will show resilience in the face of the pandemic but also that subgroups of individuals will require longer periods to return to pre-adversity levels. Additionally, these patterns of change may vary by the type of difficulties people experience as well as characteristics and resources they might have at their disposal (Bonanno, 2004). The differing patterns we observed for the anxiety and depression trajectories are compatible with other research indicating the differences between anxiety and depression during the COVID-19 pandemic (Hyland et al., 2020) and in other adversities as well (Choi, Kim and Jeon, 2010). Our findings indicated significant associations of anxiety and depression with three demographic characteristics that are likewise compatible with previous research. The role of religiosity has, for example, been observed to inversely correlate with the level of distress (Kimhi et al., 2020b; Galiatsatos et al., 2020; Lucchetti et al., 2020). Difficulties due to the COVID-19 crisis have also been linked in other studies that highlight the importance of economic harm (Kimhi et al., 2020a; Nicola et al., 2020). Finally, income has also been shown to predict reduced stress (Biddle et al., 2020). To our knowledge, the current data is the first to link these demographic factors specifically to trajectories of mental health during the COVID crisis. Moreover, this study is the first we know of to link religiosity specifically to a trajectory of resilience in any study (Bonanno, 2021).
4.1. Limitations
It is important to point out several limitations of our study. First, although the sample we used was representative of the broader Israeli population, this sample was obtained from a web survey provider and thus was not a truly random sample, as it requires digital literacy. Second, all data were derived from self-report measures, which may introduce response biases. Third, although the data were longitudinal, these data were exclusively correlational and thus restrict inferences that might suggest causal relationships. Fourth, the health status of the respondents before COVID-19 was not available and thus could not be accounted for in the interpretation of the trajectory patterns. Fifth, the use of an Internet panel does not allow to know the response rate.
5. Conclusions
Three possible conclusions emerge from the present study: First, like previous studies, our results show that a large part of the population exhibited individual resilience across all three measurements. The levels of anxiety and depression were measured during three different periods of the pandemic; in the first and third measurements, there were increased levels of infectivity while during the second measurement, the number of daily confirmed cases was much lower. The findings that the trajectories were stable across the varied times, despite the varied fluctuations in confirmed cases of COVID-19, support the assumption that more people are resilient in varied adversities. Second, our observation of chronic and emerging trajectories of anxiety and depression are consistent with other studies indicating subgroups who reported high levels of these symptoms. Third, our study indicates the positive role of religion in coping with adversity, such as the COVID-19.
Funding information
The study was supported by the Israeli Ministry of Science. The funder was not involved in any part of the study itself (the design, the data collection, the analysis nor writing the manuscript).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Suggested running head
Anxiety and depression trajectories during COVID-19.
CRediT authorship contribution statement
Shaul Kimhi: Conceptualization, constructed some of the study tools used, designed specific components of the study, Formal analysis, Writing – original draft. Yohanan Eshel: constructed some of the study tools used. Hadas Marciano: designed specific components of the study. Bruria Adini: Conceptualization. George A. Bonanno: Formal analysis, Writing – original draft, all authors reviewed the varied versions of the manuscript, commented and achieved consensus as to the final version.
Declaration of competing interest
There are no conflicts of interest to any of the authors.
Acknowledgments
N/A.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2021.10.043.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Andrews B., Brewin C.R., Philpott R., Stewart L. Delayed-Onset posttraumatic stress disorder: a systematic review of the evidence. American Journal of Psychiatry. 2007;164(9):1319–1326. doi: 10.1176/appi.ajp.2007.06091491. [DOI] [PubMed] [Google Scholar]
- Barzilay R., Moore T.M., Greenberg D.M., DiDomenico G.E., Brown L.A., White L.K., Gur R.E. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Translational psychiatry. 2020;10(1):1–8. doi: 10.1038/s41398-020-00982-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biddle N., Edwards B., Gray M., Sollis K. Hardship, distress, and resilience: the initial impacts of COVID-19 in Australia. . 2020 [Google Scholar]
- Birenbaum-Carmeli D., Chassida J. Health and socio-demographic implications of the Covid-19 second pandemic wave in Israel, compared with the first wave. International. Journal for Equity in Health. 2021;20(1):1–12. doi: 10.1186/s12939-021-01445-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno G.A. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? American psychologist. 2004;59(1):20. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A. Basic Books; New York: 2021. The End of Trauma: How the New Science of Resilience Is Changing How We Think about PTSD. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A., Brewin C.R., Kaniasty K., La Greca A.M. Weighing the costs of disaster: consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest. 2010;11(1):1–49. doi: 10.1177/1529100610387086. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A., Romero S.S., Klein S.I. The temporal elements of psychological resilience: an integrative framework for the study of individuals, families, and communities. Psychological Inquiry. 2015;26(2):139–169. [Google Scholar]
- Bryant R.A., Harvey A.G. Delayed-onset posttraumatic stress disorder: a prospective evaluation. Australian and New Zealand Journal of Psychiatry. 2002;36(2):205–209. doi: 10.1046/j.1440-1614.2002.01009.x. Retrieved from. [DOI] [PubMed] [Google Scholar]
- Chen S., Bonanno G.A. Psychological adjustment during the global outbreak of COVID-19: a resilience perspective. Psychological Trauma. 2020;12(S1):S51–S54. doi: 10.1037/tra0000685. [DOI] [PubMed] [Google Scholar]
- Choi K.W., Kim Y.K., Jeon H.J. Anxiety Disorders. . Springer; Singapore: 2020. Comorbid anxiety and depression: clinical and conceptual consideration and transdiagnostic treatment; pp. 219–235. [DOI] [PubMed] [Google Scholar]
- Cullen W., Gulati G., Kelly B.D. Mental health in the Covid-19 pandemic. QJM: An International Journal of Medicine. 2020;113(5):311–312. doi: 10.1093/qjmed/hcaa110. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L.R., Savitz K.L. In: Handbook of Psychological Assessment in Primary Care Settings. Maruish M.E., editor. Lawrence Erlbaum Associates; Mahwah, NJ: 2000. The SCL-90-R and Brief symptom inventory (BSI) in primary care; pp. 297–334. [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA network open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D., Bu F., Mak H.W., Steptoe A. Vol. 15. Results release; 2020. (COVID-19 Social Study). [Google Scholar]
- Fernandes N. Economic effects of coronavirus outbreak (COVID-19) on the world economy. . 2020 Available at SSRN 3557504. [Google Scholar]
- Galatzer-Levy I.R., Huang S.H., Bonanno G.A. Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clinical Psychology Review. 2018;63:41–55. doi: 10.1016/j.cpr.2018.05.008. . [DOI] [PubMed] [Google Scholar]
- Galiatsatos P., Monson K., Oluyinka M., Negro D., Hughes N., Maydan D., Hale W.D. Community calls: lessons and insights gained from a medical–religious community engagement during the COVID-19 pandemic. Journal of religion and health. 2020;59(5):2256–2262. doi: 10.1007/s10943-020-01057-w. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gesser-Edelsburg A., Cohen R., Hijazi R., Shahbari N.A.E. Analysis of public perception of the Israeli government's early emergency instructions regarding COVID-19: online survey study. Journal of Medical Internet Research. 2020;22(5) doi: 10.2196/19370. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland P., Shevlin M., McBride O., Murphy J., Karatzias T., Bentall R.P., Vallières F. Anxiety and depression in the Republic of Ireland during the COVID‐19 pandemic. Acta Psychiatrica Scandinavica. 2020;142(3):249–256. doi: 10.1111/acps.13219. . [DOI] [PubMed] [Google Scholar]
- Islam M.A., Barna S.D., Raihan H., Khan M.N.A., Hossain M.T. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. PloS One. 2020;15(8) doi: 10.1371/journal.pone.0238162. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung T., Wickrama K.A. An introduction to latent class growth analysis and growth mixture modeling. Social and personality psychology compass. 2008;2(1):302–317. . [Google Scholar]
- Kimhi S., Eshel Y., Marciano H., Adini B. Online first). A renewed outbreak of the COVID-19 pandemic: a longitudinal study of distress, resilience and subjective well-being. International Journal of Environmental Research and Public Health. 2020;17:7743. doi: 10.3390/ijerph17217743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhi S., Marciano H., Eshel Y., Adini B. Community and national resilience and their predictors in face of terror. International Journal of Disaster Risk Reduction. 2020:101746. . [Google Scholar]
- Kimhi S., Marciano H., Eshel Y., Adini B. Resilience and demographic characteristics predicting distress during the COVID-19 crisis. Social Science & Medicine. 2020;265:113389. doi: 10.1016/j.socscimed.2020.113389. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhi S., Marciano H., Eshel Y., Adini B. Community and national resilience and their predictors in face of terror. International Journal of Disaster Risk Reduction. 2020:101746. . [Google Scholar]
- Kontoangelos K., Economou M., Papageorgiou C. Mental health effects of COVID-19 pandemia: a review of clinical and psychological traits. Psychiatry Investigation. 2020;17(6):491. doi: 10.30773/pi.2020.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucchetti G., Góes L.G., Amaral S.G., Ganadjian G.T., Andrade I., de Araújo Almeida P.O., Manso M.E.G. Spirituality, religiosity and the mental health consequences of social isolation during Covid-19 pandemic. The International Journal of Social Psychiatry. 2020 doi: 10.1177/0020764020970996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maor M., Sulitzeanu-Kenan R., Chinitz D. When COVID-19, constitutional crisis, and political deadlock meet: the Israeli case from a disproportionate policy perspective. Policy and Society. 2020;39(3):442–457. doi: 10.1080/14494035.2020.1783792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhsen K., Cohen D. Clinical Microbiology and Infection. 2021. COVID-19 vaccination in Israel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B. Latent variable analysis. The Sage handbook of quantitative methodology for the social sciences. 2004;345(368):106–109. . [Google Scholar]
- Muthén B.O., Muthén L.K., Asparouhov T. . Muthén & Muthén; Los Angeles, CA: 2017. Regression and Mediation Analysis Using Mplus. [Google Scholar]
- Nagin D.S., Odgers C.L. Group-based trajectory modeling in clinical research. Annual Review of Clinical Psychology. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. . [DOI] [PubMed] [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. International Journal of Surgery. 2020 doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor R.C., Wetherall K., Cleare S., McClelland H., Melson A.J., Niedzwiedz C.L., Robb K.A. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. The British Journal of Psychiatry. 2020:1–8. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirutinsky S., Cherniak A.D., Rosmarin D.H. COVID-19, mental health, and religious coping among American Orthodox Jews. Journal of religion and health. 2020;59(5):2288–2301. doi: 10.1007/s10943-020-01070-z. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram Y., Collins-Kreiner N., Gozansky E., Moscona G., Okon-Singer H. Is there a COVID-19 vaccination effect? A three-wave cross-sectional study. Current Issues in Tourism. 2021;31:1–8. [Google Scholar]
- Saltzman L.Y., Hansel T.C., Bordnick P.S. Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12:s55–s57. doi: 10.1037/tra0000703. [DOI] [PubMed] [Google Scholar]
- Sharabi M., Kay A. The relative centrality of life domains among secular, traditionalist, and Ultra-Orthodox (Haredi) men in Israel. Community, Work & Family. 2021;24(1):60–76. . [Google Scholar]
- Settersten R.A., Jr., Bernardi L., Härkönen J., Antonucci T.C., Dykstra P.A., Heckhausen J., Mulder C.H. Understanding the effects of Covid-19 through a life course lens. . 2020 doi: 10.1016/j.alcr.2020.100360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shadmi E., Chen Y., Dourado I., Faran-Perach I., Furler J., Hangoma P., Willems S. Health equity and COVID-19: global perspectives. International Journal for Equity in Health. 2020;19(1):1–16. doi: 10.1186/s12939-020-01218-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheerin C.M., Lind M.J., Brown E.A., Gardner C.O., Kendler K.S., Amstadter A.B. The impact of resilience and subsequent stressful life events on MDD and GAD. Depression and Anxiety. 2018;35(2):140–147. doi: 10.1002/da.22700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwalm F.D., Zandavalli R.B., de Castro Filho E.D., Lucchetti G. Is there a relationship between spirituality/religiosity and resilience? A systematic review and meta-analysis of observational studies. Journal of Health Psychology. 2021 doi: 10.1177/1359105320984537. 1359105320984537. [DOI] [PubMed] [Google Scholar]
- Tan Y., Lin X., Wu D., Chen H., Jiang Y., He T., Tang Y. Different trajectories of panic and the associated factors among unmarried Chinese during the COVID‐19 pandemic. Applied Psychology: Health and Well‐Being. 2020;12(4):967–982. doi: 10.1111/aphw.12238. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worldometer 2020. https://www.worldometers.info/coronavirus Retrieved (20-12-20) from:
- WHO World Health Organization 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Retrieved (1, August) retrieved from.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.