Abstract
Background and Aims
The alcohol harm paradox (AHP) posits that disadvantaged groups suffer from higher rates of alcohol-related harm compared with advantaged groups, despite reporting similar or lower levels of consumption on average. The causes of this relationship remain unclear. This study aimed to identify explanations proposed for the AHP. Secondary aims were to review the existing evidence for those explanations and investigate whether authors linked explanations to one another.
Methods
This was a systematic review. We searched MEDLINE (1946–January 2021), EMBASE (1974–January 2021) and PsycINFO (1967–January 2021), supplemented with manual searching of grey literature. Included papers either explored the causes of the AHP or investigated the relationship between alcohol consumption, alcohol-related harm and socio-economic position. Papers were set in Organization for Economic Cooperation and Development high-income countries. Explanations extracted for analysis could be evidenced in the empirical results or suggested by researchers in their narrative. Inductive thematic analysis was applied to group explanations.
Results
Seventy-nine papers met the inclusion criteria and initial coding revealed that these papers contained 41 distinct explanations for the AHP. Following inductive thematic analysis, these explanations were grouped into 16 themes within six broad domains: individual, life-style, contextual, disadvantage, upstream and artefactual. Explanations related to risk behaviours, which fitted within the life-style domain, were the most frequently proposed (n = 51) and analysed (n = 21).
Conclusions
While there are many potential explanations for the alcohol harm paradox, most research focuses on risk behaviours while other explanations lack empirical testing.
Keywords: Alcohol consumption, alcohol-related harm, causal mechanisms, disadvantage, health inequalities, morbidity, mortality, socio-economic position
INTRODUCTION
Alcohol accounts for 5.3% of deaths and 5.1% of the burden of disease and injury globally [1]. However, alcohol-related harms (e.g. deaths, illnesses and hospitalizations due partly or wholly to alcohol) are not equally distributed across socio-economic positions (SEP)—the social and economic factors that determine an individual’s position in society [2].
Disadvantaged groups suffer from higher rates of alcohol-related hospital admissions and deaths compared with advantaged groups, despite reporting similar or lower average levels of consumption [3,4]. For example, in the United Kingdom, the proportion of people in the highest SEP group drinking more than 4/3 (45%) or 8/6 (23%) units per day is almost double compared to the lowest SEP (22 and 10%, respectively) [5]. Despite this, the alcohol-specific mortality rate among the most deprived is 5.5 times higher [6]. This relationship, termed the alcohol harm paradox (AHP), is found internationally, including in the United Kingdom [4], Australia [7], the Netherlands [8] and Finland [9] and across measures of SEP (e.g. social grade, income, education, car ownership, employment and housing tenure) [10]. Prior to 1980, findings suggest a clear dose–response relationship between alcohol consumption and alcohol-related hospitalization and mortality, irrespective of SEP [11–13]. However, in the last 40 years the AHP has become a consistent and long-standing finding [14]. Despite this, there is a paucity of research attempting to understand the underlying causes of the AHP.
Several reviews and meta-analyses have described socio-economic differences in alcohol-related harms based on existing evidence or available survey data [3,15–19]. However, only a subset also focused upon the contribution of alcohol consumption to this relationship, measured as average consumption (e.g. grams or units weekly, monthly or yearly) or drinking patterns (how often and how much people drink) [3,17,18]. This evidence highlights that neither average alcohol consumption nor heavy drinking patterns can explain differences in alcohol-attributable outcomes between SEP groups. At best, heavy drinking occasions partially attenuate the link between SEP and hospitalizations or mortality by 15–30% [3]. Put simply, the most disadvantaged consistently suffer disproportionate risks of harm from their alcohol consumption when compared to their advantaged counterparts, which is not only a health burden on society but contributes to increasingly widening health inequalities [20].
Empirical studies of the AHP have largely focused upon proximal individual-level factors as potential explanations. The role of unrecorded alcohol consumption has, to an extent, been investigated, and results suggest that under-reporting is similar across socio-economic groups [21]. Cross-sectional studies have also tested differences in drinking patterns, behavioural clustering and drinking histories [21,22]. Although there is evidence that low SEP groups tend to have heavier drinking patterns [21,22] and engage in multiple risky health-related behaviours [21], fewer studies go on to test the degree to which life-style risk factors explain differences in alcohol-related harm. One study highlighted that the rate of alcohol-attributable mortality and hospital admissions was three times higher for the most disadvantaged compared with the most advantaged; this association remained after adjusting for weekly consumption and heavy drinking occasions, and it was only slightly attenuated after further adjusting for body mass index (BMI) and smoking [4]. While investigation of life-style factors is prominent, other potentially fruitful avenues of explanation, such as social and economic causes (e.g. social support, housing and employment), have been neglected.
Substantial socio-economic gradients in health exist across countries and contexts [23,24]. There is a critical need for evidence to support public health policies that tackle not only behaviour, but also the broader social determinants of health to mitigate the AHP. This study aimed to review explanations for the paradox put forward in relevant scientific literature. Secondary aims were to review the existing evidence for or against these explanations, and to explore how authors combine different explanations to shed light upon potential relationships between different causal factors. To our knowledge, this is the first review to collate explanations for the AHP.
METHODS
Search strategy
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA) [25]. The protocol for this study can be found at: http://doi.org/10.13140/RG.2.2.25606.60489. MEDLINE (1946 – January 2021), EMBASE (1974–January 2021) and PsycINFO (1967–January 2021) were searched to identify peer-reviewed literature on the topic of the AHP or studies that investigated the relationship between alcohol-related harm, socio-economic position and alcohol consumption. An extensive list of search terms was used (see Supporting information, Table S1) to capture the themes of alcohol (e.g. alcohol adj3 drink*) and socioeconomic factors (e.g. disadvantage*). Given the large number of results returned during test searches, further specifications were made by focusing upon papers with alcohol in the title, and some exclusory terms were included (e.g. NOT therapeutics). Terms were tailored dependent upon database requirements. For grey literature, Google and Google Scholar were searched, and this was supplemented via expert identification of relevant reports (C.A.).
Inclusion and exclusion criteria
The population, exposures, comparisons, outcome and study designs (PECOS) criteria for inclusion are listed in Table 1. Studies were included if they: (i) were full papers published in English and (ii) explicitly explored the AHP OR investigated the relationship between: alcohol-related harm, socio-economic position and alcohol consumption (Table 1). We focused upon high-income Office for Economic Cooperation and Development (OECD) countries as classified by the World Bank [26], primarily due to differences in alcohol environments between high- and low–middle-income countries, e.g. greater availability of informally produced alcohol in low–middle-income countries [27]. A range of study designs were eligible for inclusion. Systematic reviews and meta-analyses were included, as it is equally possible to extract ‘explanations’ for the paradox from these studies. However, intervention and treatment studies were outside the scope of this review. Additionally, empirical studies which analysed data exclusively collected pre-1980s were excluded.
Table 1.
Population, exposures, comparisons, outcomes and study design criteria for study inclusion.
| Criteria | Definition |
|---|---|
|
| |
| Population | OECD high-income countries only |
| Exposures | Alcohol consumption (any measure including both self-report (e.g. quantity/frequency, heavy drinking occasions), biological indicators (e.g. blood alcohol concentration) and aggregate sales data (e.g. per-capita consumption) |
| Comparisons | Socio-economic position [any measure including area-level deprivation and individual measures (e.g. educational attainment, occupation and income level)] |
| Outcomes | Alcohol-related harm [any measure which relates to health harms (e.g. morbidity and mortality), clinical diagnosis of alcohol use disorder using ICD codes or DSM-IV manual or negative alcohol-related consequences (e.g. had an accident)] |
| Study designs | All designs were considered both quantitative and qualitative—including secondary research, intervention studies were excluded |
OECD = Office for Economic Cooperation and Development.
Screening
All records were imported to EndNote Online and duplicates were removed. Titles and abstracts were screened to identify papers matching the inclusion criteria. Full-text versions of the papers were then screened to determine inclusion. Initial screening was carried out by one reviewer (J.B.). A second reviewer (O.S.) then randomly screened a sample of the included studies (n = 20) to validate that papers were correctly included. There was no disagreement between reviewers regarding inclusion.
Data extraction
Data from the papers were extracted by one reviewer (J.B.). A second reviewer (O.S.) independently assessed the accuracy of data extraction for a sample of the included studies (n = 20). In the case of disagreement both reviewers referred to the paper in question, and a consensus was reached. A data extraction matrix was developed, which included characteristics of the studies (design, year of data collection and location), participants (age, target population and sample size), measures (unit of analyses, SEP, alcohol consumption and alcohol harm measures) and outcomes (main findings and explanations for the AHP). Both tested and hypothetical explanations were extracted. ‘Explanations’ were any reasons identified from the empirical results or proposed by the authors which explain why alcohol-related harm outcomes were worse for those of a low SEP. Explanations were commonly taken from the results and discussion sections of empirical papers or the main body of other types of included paper. Hypothetical explanations were extracted verbatim. The evidence for these explanations was also extracted from included primary research or from authors citing other research findings when proposing an explanation.
Quality assessment
Quality appraisal of the included studies was conducted by one researcher (J.B.) to assess risk of bias. The AXIS critical appraisal tool [28], CASP qualitative, CASP systematic review, CASP cohort study and CASP case–control study checklists [29] were used depending upon the study design. Commentaries, author replies, discussion papers and reports were not critically appraised. Overall, the quality of included papers was assessed as good. More information on critical appraisal can be found in the Supporting information, Table S2.
Analysis
Descriptive summary statistics were used to describe search results and study characteristics. An inductive thematic approach was taken to analyse the explanations provided by included papers. This aimed to group explanations within broader themes. Explanations were coded and initially analysed by one researcher (J.B.) in consultation with co-authors (R.P. and J.H.). In the instance where an author meaningfully linked multiple explanations in the text, this was recorded as a connection. A narrative synthesis of the findings providing evidence for or against the extracted explanations was also conducted.
RESULTS
Descriptive analysis
A search of electronic databases returned 20 828 records. A further 13 records were identified from the grey literature. Total records reduced to 18 790 following de-duplication. Of the 18 790 records, following title and abstract screening, 195 were selected for full-text screening and 79 of these met the inclusion criteria for data synthesis (Fig. 1). Attempts to retrieve inaccessible papers were made through the search databases, University Library services and Google Scholar. Study characteristics are displayed in Table 2.
Figure 1.
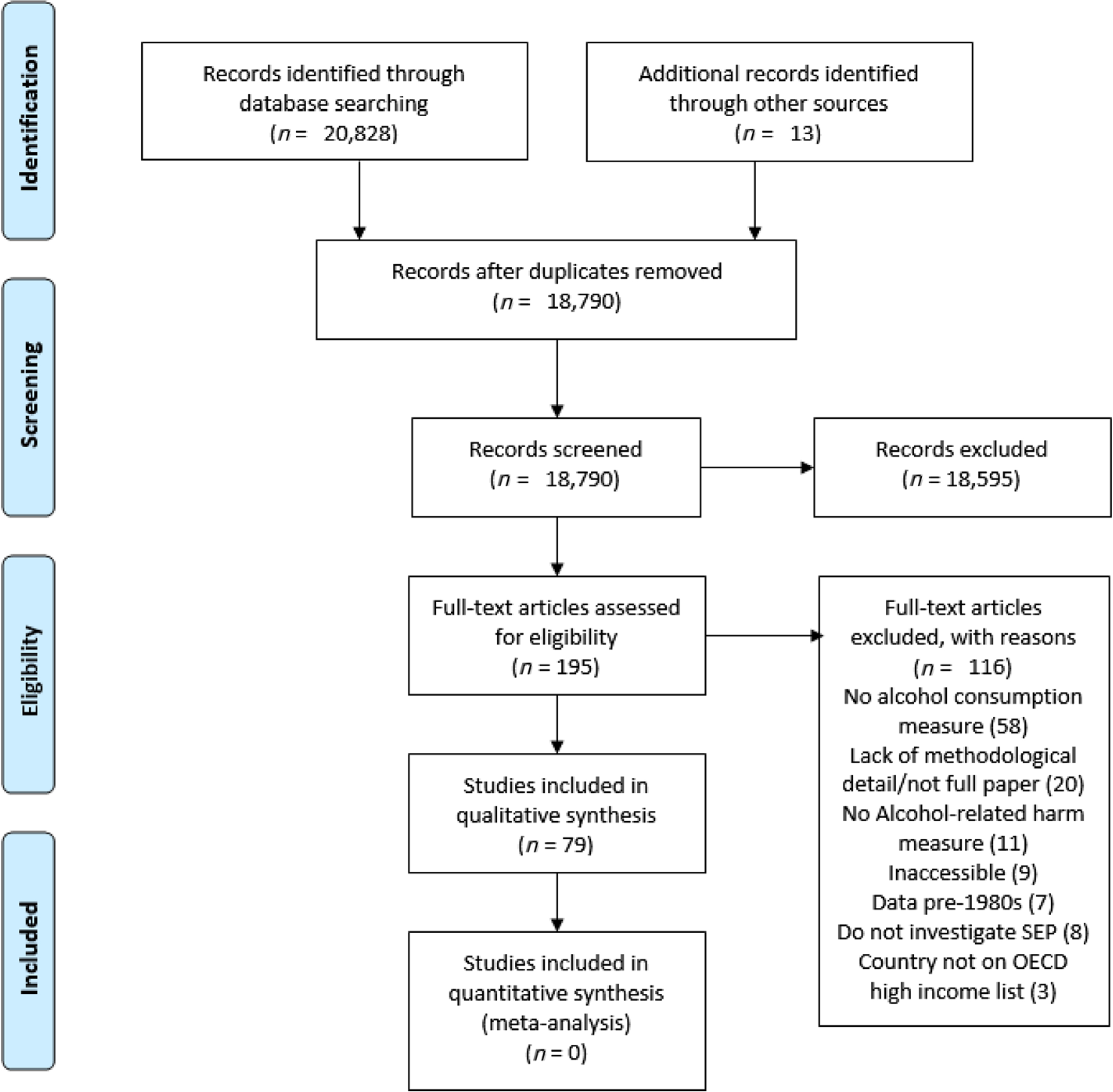
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram
Table 2.
Characteristics of included papers.
| Author, year | Country | Study design | Study year | Population | Sample size | Age | Measurement level | Harm measure | SEP measure | Consumption measure | Evidence of the AHP |
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Alcohol Research UK, 2015 [53] | UK | Report | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Backhans et al. 2016 [57] | Sweden | Cohort | 2002–11 | G | 15 841 | 18–84 | I | AR hospital, death | ES, E | Last 12 months; drinks/week; binge drinking | Yes |
| Beard et al. 2016 [10] | UK | Cross-sectional | 2014–15 | G | 1700 | 16+ | I | AUDIT-H, AUDIT-D | O, I, E, ES, H | AUDIT-C | Yes |
| Beilis & Hughes, 2009 [39] | UK | Report | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Beilis et al. 2016 [21] | UK | Cross-sectional | 2013–14 | G | 6015 | 18+ | I, AG | NA | A | Last 12 months, units/week | NA |
| Bloomfield, 2020 [71] | Denmark | Commentary | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Boyle et al. 2014 [72] | Australia | Case–control | 2005–07 | G | 918 (cases), 1021 (controls) | 40–79 | I, AG | Colorectal cancer | A | g/week | NA |
| Breakwell et al. 2007 [73] | UK | Cross-sectional | 1991–2004 | G | NA | 15+ | AG | AR death | A | Units/week | Yes |
| Brown et al. 2014 [33] | USA | Cross-sectional | 2010–11 | G | 663 | 19–91 | I | Somatic complaints | E | Drinks/month | NA |
| Chick, 1998 [34] | UK | Review | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Collins, 2016 [16] | USA | Review | NA | NA | 28 studies | NA | NA | NA | NA | NA | NA |
| Connor et al. 2010 [54] | New Zealand | Cross-sectional | 2006–07 | G | 1770 | 18–70 | I, AG | Negative AR consequences | E, A | Drinking days last 12 months, drinks/occasion, binge drinking | NA |
| Conway et al. 2015 [74] | EU, Americas | Case–control | 1988–2007 | G | 23 964 cases, 31, 954 controls | NR | I | Head and neck cancer | E, I | Drinker status, drinks/day | Yes |
| Degerud et al. 2018 [40] | Norway | Cohort | 1960–2011 | G | 207 394 | NR | I | Cardiovascular disease, ischaemic heart disease, cerebrovascular and all-cause mortality | H, I, E | g/day, heavy drinking episodes | Yes |
| Evans-Polce et al. 2016 [35] | UK | Cohort | 1958–2006 | G | 11 469 | 7–55 | I | All-cause mortality | PI, H, O | Units/week | NA |
| Fair Foundation, 2015 [75] | Australia | Report | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Fillmore et al. 1998 [76] | USA, Sweden | Meta-analysis | 1964–82 | NA | 31 studies | 16+ | I | All-cause mortality | E, ES, I | Drinks/occasion, occasions/month, drinks/month | Yes |
| Gartner et al. 2019 [47] | Wales | Record-linkage | 2013–16 | G | 11 038 | 16+ | I | AR hospital | A, SC, E, ES, H | Units/heaviest drinking day, last 12 months | Yes |
| Hall, 2017 [77] | UK | Commentary | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Hart, 2015 [78] | Australia | Qualitative | NA | Young adults | NA | 18–24 | I | NA | NA | NA | NA |
| Herttua et al. 2007 [56] | Finland | Cohort | 1985–2003 | G | 70.1 million | 15+ | I, AG | AR death | E | Litres/capita | NA |
| Huckle et al. 2010 [49] | New Zealand | Cross-sectional | 1995, 2000, 2004 | G | 3848, 4295, 5477 | 18–65 | I | Negative AR consequences | E, I, O | Litres/year | Yes |
| Jonas et al. 1999 [79] | Australia | Cross-sectional | 1995–96 | G | NR | NA | AG | AR hospital | ES, O, H, I, MV | Litres/capita | NA |
| Jones et al. 2015 [18] | EU, Americas | Systematic review | 2012 | NA | 31 studies | NA | I, AG | AR morbidity, death | E, O, I, A, ES, H, OM | g/year, g/day, drinks/week, units/week, drinks/day, drinking status, ml/day, days drank/week, glasses/day, binge drinking, years vodka consumption, drinks/last 12 months | Yes |
| Karriker-Jaffe et al. 2012 [80] | USA | Cross-sectional | 2000, 2005 | G | 7613, 6919 | 18+ | I, AG | Negative AR consequences, AD | A | Drinks/last 12 months, Heavy drinking | Yes |
| Karriker-Jaffe et al. 2013 [81] | USA | Cross-sectional | 2000, 2005 | G | 7613, 6919 | 18+ | I, AG | Negative AR consequences | A | Drinks/last 12 months, Heavy drinking | Yes |
| Katikireddi et al. 2017 (a) [4] | UK | Record-linkage | 1995–2012 | G | 50 236 | M = 48 | I, AG | AR hospital, death and prescription | E, A, O, I | Units/week, binge drinking | Yes |
| Katikireddi et al. 2017 (b) [82] | UK | Commentary | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Kuendig et al. 2008 [83] | EU | Cross-sectional | 1997–2002 | G | NA | 25–60 | I | Negative AR consequences | E, ES | g/day, binge drinking | Yes |
| Lawder et al. 2011 [63] | UK | Cohort | 1998–2008 | G | 8305 | M = 47 | I, AG | AR hospital | ES, B, A | Units/week | Yes |
| Lewer et al. 2016 [22] | UK | Cross-sectional | 2008–13 | G | 51 498 | 18+ | I, AG | NA | I, E, ES, A | Heavy episodic drinking, Heavy weekly drinking | NA |
| Livingston, 2014 [38] | Australia | Cross-sectional | 2010 | G | 21 452 | 12+ | I, AG | NA | A, I | Drinks/year, risky drinking | NA |
| Lundin et al. 2012 [58] | Sweden | Cohort | 1969–91 | MC | 37 798 | 18+ | I | AR hospital | PI, O, E, I | Risky alcohol use | Yes |
| Major et al. 2014 [59] | USA | Cohort | 1995–2006 | G | 4 814 247 | M = 63 | I, AG | Hepatocellular carcinoma incidence, chronic liver disease mortality | A | Drinks/day | Yes |
| Makela & Paljarvi, 2007 [9] | Finland | Cohort | 1969–2000 | G | 6406 | 25–69 | I | AR hospital, death | O | Cl/year | Yes |
| Makela, 2008 [84] | Finland | Commentary | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Marmot, 2001 [85] | UK | Commentary | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Mayor, 2016 [86] | UK | Commentary | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| McDonald et al. 2008 [60] | UK | Record-linkage | 1995–2005 | G | 23 183 | 30+ | I, AG | AR discharge diagnosis | A | Units/week | Yes |
| Meier et al. 2017 [36] | UK | Discussion | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Menvielle et al. 2004 [43] | France | Case–control | 1989, 1991 | MP | 504 cases, 242 controls | < 50–70 | I | Laryngeal or hypopharyngeal cancer | E, O, OM | Glasses/day | Yes |
| MESAS, 2016 [87] | UK | Report | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Moller et al. 2019 [48] | Denmark | Cross-sectional | 2014 | Young adults | 70 566 | M = 17.9 | I | Negative alcohol consequences | PI | Standard drinks/week | Yes |
| Mulia & Karriker-Jaffe, 2012 [88] | USA | Record-linkage | 2000, 05 | G | 13 231 | 24+ | I, AG | Negative alcohol consequences, AD | E, A | Drinking status, risky drinking, monthly drunkenness | NA |
| Mulia & Zemore, 2012 [89] | USA | Cross-sectional | 2005 | G | 4080 | 18+ | I | AD | Poverty status | Frequency of drunkenness in the last year | NA |
| Nielsen et al. 2004 [90] | Denmark | Cohort | 1976–2001 | G | 14 223 | 20+ | I | All-cause mortality | E, I | Frequency of types | NA |
| Norstrom & Landberg, 2020 [91] | Sweden | Cohort | 1994–2017 | G | NA | NA | AG | Alcohol-specific mortality, violent deaths | E | Per-capita consumption | Yes |
| Norstrom & Romelsjo, 1999 [30] | Sweden | Cross-sectional | 1990, 1991–95 | M | 2817 | 20–64 | I | AR death | O | Litres/year | No |
| Nweze et al. 2016 [92] | USA | Cross-sectional | 2013 | P | 738 | 15–70 | I | AR hospital | ES, IN | BAC | NA |
| Parkman et al. 2017 [93] | UK | Qualitative | 2015 | P | 30 | 16+ | I | AR hospital | E, H, ES | Current and previous use | NA |
| Pena et al. (2020) [64] | Finland | Eight cohort studies | 1978–2016 | G | 52 164 | 25+ | I | AR death | I, E | g/week, alcohol biomarkers | Yes |
| Pena et al. (2021) [46] | Finland | Eight cohort studies | 1978–2016 | G | 53 632 | 25+ | I | AR death | I, E | g/week | Yes |
| Probst et al. 2020 [3] | Canada | Systematic review/meta-analysis | 2020 | NA | 10 studies | NA | NA | NA | NA | NA | Yes |
| Public Health Wales, 2014 [94] | UK | Report | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Rehm & Probst, 2018 [95] | Canada | Discussion | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Rhew et al. 2020 [51] | USA | Cohort | NA | Young adults | 746 | 18–23 | I | Negative alcohol consequences | PI | Standard drinks/week | NA |
| Roberts et al. 2008 [32] | UK | Record-linkage | 1998–2003 | P | 52 096 | < 35–> 75 | I, AG | Pancreatitis incidence, death | A | Binge drinking | No |
| Roberts et al. 2013 [31] | UK | Record-linkage | 1999–2010 | P | 19 196 | < 35–> 75 | I, AG | Pancreatitis incidence, death | A | Units/day in the previous week | No |
| Roche et al. 2015 [96] | Australia | Review | NA | NA | 138 studies | NA | NA | NA | NA | NA | NA |
| Romelsjo & Lundberg, 1996 [97] | Sweden | Cross-sectional | 1967–93 | G | NR | 25–64 | I | AR hospital, deaths | O | g/day | Yes |
| Sadler et al. 2016 [98] | UK | Cross-sectional | 2010–13 | P | 9.6 million HES alcohol admissions | 18+ | AG | AR hospital | A | NA | NA |
| Salom et al. 2014 [55] | Australia | Cohort | 1981–2002 | Young adults | 2399 | 0–21 | I | Mental health, AD | ES, PI, PES | Drinks/occasion | Yes |
| Sargent, 1989 [61] | Australia | Discussion | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Shaper et al. 1988 [62] | UK | Cohort | 1978–87 | M | 7735 | 40–59 | I | All-cause mortality | O | Units/week | Yes |
| Singh & Hoyert, 2000 [52] | USA | Cohort | 1979–89, 1990–92 | G | 370 500 | 25+ | I, AG | Cirrhosis and chronic liver disease mortality | ES, E, PI, O | Per-capita consumption | Yes |
| Skogen et al. 2019 [99] | Norway | Cross-sectional | NA | G | 4311 | 16–72 | I | AUDIT | O, I, ES | AUDIT-C | NA |
| Smith & Foster, 2014 [14] | UK | Report | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Stanford-Moore et al. 2018 [44] | USA | Case–control | 2002–06 | P | 1153 cases, 1267 controls | 20–80 | I | Squamous cell carcinoma of the head and neck | I, E, IN | Drinking status, years drank, g/lifetime | Yes |
| Stewart et al. 2017 [41] | UK | Cohort | 2000–14 | Adults with LTC | 95 991 | 18+ | I, AG | All-cause mortality | A | Drinking status, units/week | Yes |
| Syden et al. 2017 [45] | Sweden | Cohort | 2002–11 | G | 17 440 | 25–64 | I | AR hospital, death | O | g/week, Heavy drinking | Yes |
| Thern et al. 2019 [42] | Sweden | Cohort | 2013–14 | Young adults | 1005 | 17–29 | I | AUD | ES | Weekly binge drinking | Yes |
| Thor et al. 2019 [50] | Sweden | Cross-sectional | 2015–16 | Young adults | 6153 | 17–18 | I | Negative alcohol consequences | PI, A, academic orientation | Binge drinking | Yes, for 2/3 SEP measures |
| Trias-Llimos et al. 2020 [100] | Europe | Cross-sectional, cohort | 2011–15 | G | 159 132 person – years at risk | 50–85 | I | All-cause mortality | E | AUDIT-C | Yes |
| Van Oers et al. 1999 [8] | the Netherlands | Cross-sectional | 1994 | G | 3537 | 16–69 | I | Negative alcohol consequences | E | Type, days/month, glasses/occasion | Yes |
| Whitley et al. 2014 [37] | UK | Cohort | 1990–2008 | G | C1 = 1444, C2 = 1550 | 35+ | I | All-cause mortality | O, I, E | Units/week | Yes |
| WHO, 2014 (a) [101] | Global | Report | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| WHO, 2014 (b) [1] | Global | Report | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| WHO, 2018 [102] | Global | Report | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Wood & Beilis, 2015 [103] | EU | Report | NA | NA | NA | NA | NA | NA | NA | NA | NA |
AUDIT = Alcohol Use Disorders Identification Test; NR = not reported; NA = not applicable; G = general population; MC = military conscripts; P = patient; MP = male patients; M = males; LTC = long-term conditions; I = individual; AG = aggregate; AR = alcohol-related; AD = alcohol dependence; AUD = alcohol use disorder; ES = employment status; E = education; O = occupational social grade; I = income; H = home ownership; A = measure of area-level deprivation; OM = occupational mobility; IN = insurance; PI = parental indicators; PES = partner employment status; MV = motor vehicles; B = benefits; SC = social class; SEP = socio-economic position; G = grams; CL = centilitres; BAC = blood alcohol content.
The largest number of papers came from the United Kingdom (n = 27). Other countries providing several papers included the United states, Sweden, Australia, New Zealand, Finland, France, Denmark, Canada, the Netherlands and Norway. Some studies were set at a continental (e.g. Europe) or global level. Of the included empirical studies, cohort (n = 26), cross-sectional (n = 21), case–control (n = 4) and qualitative (n = 2) designs were employed. One used both cross-sectional and longitudinal data. The included reviews and meta-analyses (n = 5) contained a total of 238 studies. Commentaries (n = 6), debate/discussion papers (n = 4) and reports (n = 10) were also included.
Empirical studies covered the general population (n = 37), patients only (n = 7), young adults (n = 6), men only (n = 2), adults with long-term health conditions (n = 1) and military conscripts (n = 1). The existence of the alcohol harm paradox was explicitly explored in 39 of the empirical studies. Of the identified papers, only seven included explicit theoretical discussion.
Of the empirical studies, the majority used at least one quantity/frequency measure of alcohol use (n = 36). Other measures included hazardous consumption, heavy drinking episodes, per-capita consumption, alcohol biomarkers and blood alcohol concentration (Table 2). Measures of SEP included individual-level (e.g. education) and area-level deprivation measures (Table 2). Most studies used physical health harm outcomes, including deaths, hospitalizations or disease states wholly and/or partially attributable to alcohol (n = 36). Other harm outcomes included negative alcohol-related consequences and alcohol use disorder or dependence (Table 2).
Evidence of the AHP
Only three of the included empirical studies found that those of a lower SEP had higher alcohol consumption which then led to increased harm, two of which were specifically focused upon pancreatitis [30–32]. Therefore, the evidence base generally supported the existence of the AHP (n = 36, including three meta-analyses of a total of 72 studies); excess harm among those of lower SEP could not be explained by the volume of alcohol consumed.
Thematic analysis
Initial coding revealed 41 explanations for the AHP. The explanations were often presented in discussion sections, did not draw upon existing theory and often appeared to be post-hoc explanations for findings. Following inductive thematic analysis of the 41 explanations, we identified 16 themes and then grouped these themes into six domains: individual, life-style, contextual, disadvantage, upstream and artefactual. Domains, themes and explanation definitions are shown in Table 3. The number of papers suggesting each theme as an explanation is presented; however, it should be noted that this is a metric of popularity rather than merit. There was no obvious connection between study design or population and the type of explanation given (Table 3). Themes were not mutually exclusive, and authors often combined or indicated interactions between explanations. These relationships are highlighted in a network diagram (Fig. 2).
Table 3.
Thematic table of explanations for the AHP extracted from included papers with information on type of study design and population.
| Domain | Theme | Explanation | Definition | Study design | Population |
|---|---|---|---|---|---|
|
| |||||
| Individual | Biological | Biological characteristics [3,34,40] | SEP groups have a different biological or genetic make-up related to ethnicity or due to experiencing inequality which leaves them more susceptible to harm | Systematic review, discussion paper, cohort | General population |
| Behavioural-related alterations [21,40,46,85,102] | Engaging in multiple risk behaviours has a biological impact: (i) nutritional deficiencies and metabolic consequences which alter protein and vitamin absorption, (ii) an adverse effect on the immune system and (iii) they interact with live enzymes, all leading to greater risk of disease (e.g. liver disease) and harm | Cross-sectional, cohort, commentary, report | General population | ||
| Psychological | Stress [3,4,34,46,52,76,81] | Low SEP groups experience more psychological stress and a greater number of stressful events: (e.g. marital breakdown, dangerous environment, immigrant status, unemployment and living in poverty). This is thought to reduce resilience to disease | Systematic review, cohort, discussion paper, meta-analysis, cross-sectional | General population | |
| Coping [8,30,33,34,42,52,56,58,78,80,88,89,93,98] | Differences in coping strategies: low SEP groups use alcohol as a coping strategy which can lead to alcohol dependence. They are also more likely to use resigned acceptance as a coping strategy and are less likely to use cognitive avoidance and emotional discharge which independently negatively impact wellbeing | Cross-sectional, discussion paper, cohort, qualitative | General population, men, young people, military conscripts, patient | ||
| Stereotypes/stigma [61,80,81,88,89,96] | Lower SEP groups experience more labelling and discrediting which leads to social rejection and exclusion. This could result in a self-fulfilling prophecy, whereby members of that group enact the behaviours they are expected to possess. This could also increase group and individual tensions which find an outlet via harmful drinking. This may also lead to fewer social resources, increasing psychological vulnerability | Discussion paper, cross-sectional, cohort, review | General population | ||
| Attribution [8,83] | There are a higher number of abstainers in low SEP groups, therefore the alcohol problems faced by those who do drink in this group may seem worse by comparison. This only holds true for subjective measures of alcohol-related harm | Cross-sectional | General population | ||
| Health and wellbeing | Physical health [8,9,32,34,35,41,47,62,63,74,76,93,94,96,98] | There is a higher prevalence of pre-existing physical health conditions, poorer general health, multi-morbidities or being overweight/obese in low SEP groups which could explain disproportionate effects of alcohol | Cross-sectional, cohort, review, case–control, meta-analysis, qualitative, report | General population, patient, men, adults with long-term conditions | |
| Mental health [8,22,34,41,47,48,50,53,63,76,93,96,98] | Low SEP individuals tend to be more psychologically vulnerable and have a greater prevalence of pre-existing mental health conditions, mental distress, or psychological symptoms (e.g. nervousness, irritability, helplessness, loneliness) which could exacerbate the effects of alcohol. There is also an independent association between poor wellbeing and worse health outcomes | Cross-sectional, review, cohort, report, meta-analysis, qualitative | General population, patient, adults with long-term conditions, young adults | ||
| Life-style | Risk behaviour | Drinking patterns [1,3,4,8,10,14,18,21,22,30,32,34,39,41,45–47,49,51–54,59,60,62–64,71,73,79,81,83,85,86,91,94,95,98–100,103] | Although overall or average alcohol consumption may be similar, or lower for low SEP groups, they consume greater quantities of alcohol per drinking occasion | report, systematic review, meta-analysis, cross-sectional, cohort, review, commentary, discussion paper | General population, men, patient, young adults |
| Clustering of health behaviours [3,4,10,18,21,22,37,40–44,46,47,53,59,63,64,72,74,76,81,90,95,103] | Those in low SEP groups engage in multiple health risk behaviours for example smoking, poor diet, a lack of exercise and concurrent drug use which exacerbate the impact of alcohol | Systematic review, meta-analysis, cross-sectional, cohort, case–control, report, discussion paper | General population, adults with long-term conditions, young adults, male patients, patient | ||
| Type of beverage [4,10,18,21,32,47,86,90,93,102] | Beers, ciders and spirits are more commonly consumed by low SEP, while wine is often associated with higher SEP. The quality and price of alcohol consumed may impact harm outcomes | Cohort, systematic review, meta-analysis, cross-sectional, commentary, qualitative, report | General population, patient | ||
| Drinking history/future drinking [4,21,22,60,62,77,103] | Drinking is temporal and may change throughout the life-course. Although those of low SEP may have reduced consumption upon measurement, increased susceptibility to harm could be due to previous drinking. There are several reasons why people may reduce consumption (e.g. developing an illness). This explanation was extended to an increase in consumption in the future, as some studies only measure consumption at baseline and outcomes in following years | Cohort, cross-sectional, commentary, report | General population, men | ||
| Drinking practices | Norms [51,53,75,78,85,87,92,96,101] | Group and neighbourhood norms including drinking pattern, expected volume, how to drink certain beverages (e.g. shot a spirit) and norms around the permissibility of excessive alcohol use differs by SEP | Cohort, report, qualitative, review | Young adults, patient | |
| Culture [75,78,88,96] | Drinking culture attached to certain places of employment or neighbourhoods may lead to poorer health and difficulties maintaining employment, which could then exacerbate stress and increase consumption | Report, qualitative, cohort, review | Young adults, general population | ||
| Health-consciousness | Health literacy [21,37,77,93,94,97] | Engagement with health promotion campaigns and preventative services. It was proposed that low SEP may not make use of available services or are slower to access these services | Cross-sectional, cohort, commentary, qualitative, report | General population, patient, men | |
| Healthy behaviours [9,34,37,76,85] | Those of a high SEP adopt healthy behaviours (e.g. good diet and exercise) which may protect against negative impacts of drinking | Cohort, review, meta-analysis, commentary | General population | ||
| Contextual | Social | Social support [9,18,34,35,45,51–53,55,73,75,76,89,93,96,101–103] | Social support may buffer the negative impacts of alcohol consumption. Those of high SEP have a wider ‘social margin’ which insulates them from the negative consequences of their actions while low SEP lack social support and are often socially isolated | Systematic review, meta-analysis, report, cross-sectional, review, cohort | General population, young adults |
| Social exclusion [1,75,76,88,96] | The marginalization of low SEP groups is greater due to several factors including a higher number of abstainers, stigmatization that comes with having an alcohol use disorder and intersections between multiple minority status (e.g. ethnic, refugee, homeless and LGBT+) | Report, meta-analysis, cohort, review | General population | ||
| Peer influence [9,53,75,96,101,102] | Negative influence from peers and family in low SEP groups may impact harm outcomes. There is evidence that men of high SEP are more likely to be married and therefore long-term partners may be an important agent of social control for excessive drinking. Not only would a partner provide social control but also additional financial support via combined income and this influence was extended to others in their social network | Cohort, report, review | General population | ||
| Drinking context | Dangerous environment [1,9,18,36,48–50,78,84,98,102] | Low SEP are more likely to drink in dangerous environments with a lack of policing and safety, which may lead to a higher risk of violence, police encounters and unintentional injury | Report, systematic review, meta-analysis, cohort, discussion paper, cross-sectional, qualitative, commentary | General population, young adults, patient | |
| Exposure [102] | Drinking in public places is common among the most deprived groups (e.g. the homeless). This leaves them exposed to certain infectious diseases (e.g. TB and HIV) which may compound harm | Report | NA | ||
| Place | Neighbourhood deprivation [10,18,44,46,50,53,79,81,84,89,102] | A lack of resources, treatment facilities or preventative/educational programs, an increased police presence, neighbourhood disorder, low educational ethos and a lack of community institution negatively impact harm outcomes | Systematic review, meta-analysis, cross-sectional, report, case–control, cohort, commentary | General population, patient, young adults | |
| Alcohol outlet/advertising density [3,53,54,59,71,75,81,87,89,96,102] | Increased outlet density has an impact on patterns of drinking and harmful consequences. The density of alcohol advertising in deprived areas was also considered to potentially influence the excess harm experienced by those of a low SEP | Systematic review, report, cross-sectional, cohort, commentary, review | General population | ||
| Disadvantage | Intersectionality | Multiple minorities [44,52,76,80,81,92,96,101] | The impact of belonging to multiple minority groups (e.g. SEP, race, gender, and sexuality), and how experiencing multiple aspects of disadvantage may amplify inequalities in alcohol-related harm | Case–control, cohort, meta-analysis, cross-sectional, review, report | Patient, general population |
| Life-course | Cumulative effects [9,37,44,52,55,58,74,84,96,102] | The accumulation of negative/stressful life events over time or additive effects of prolonged risky health behaviours which negatively impacts health and potentially employment itself | Cohort, case–control, commentary, review, report | General population, patient, military conscripts | |
| Early risk factors [9,50,55,58,75,96,103] | The experience of ACE’s in childhood, childhood household dysfunction and a disadvantaged start in life (including prenatal factors) perpetuates a vicious cycle of poverty and poor health which impacts on social participation, wellbeing, their ability to cope and access to available support or treatment | Cohort, cross-sectional, report, review | General population, young adults, military conscripts | ||
| Family influence [55,81,102] | Limited family income restricts material resources and creates stress given the inability to meet basic needs. Family history of alcohol problems could impact alcohol consumption and health in later life. Parental education is shown to negatively impact on health literacy and children’s employment aspirations, opportunities, and adulthood income | Cohort, cross-sectional, report | General population | ||
| Material | Material resources [1,4,14,49,51,55,73,74,93,96] | A lack of resources could negatively impact on harm due to the inability to protect themselves from the experience of a problem or stressful life event and could exacerbate poor health through poor housing conditions, homelessness, and unemployment | Report, cohort, cross-sectional, case–control, qualitative, review | General population, young adults, patient | |
| Neo-materialist | Access, quality and barriers [1,3,10,14,18,21,38,44,46,52,53,55,64,75,76,87,93,96,98,102,103] | Depending on geographical distribution, services in disadvantaged areas may be fewer and more difficult to access or of a lower quality. Low SEP groups face several potential barriers when attempting to access health-care including cost, transport, availability (in terms of opening hours), mobility issues and stigma which may deter them from using services. Dependent on country there were additional considerations for example the cost of health insurance | Report, systematic review, cohort, meta-analysis, qualitative, review, cross-sectional, case–control | General population, patient | |
| Upstream | Structural | Economic [1,16,33,45,53,56,75,87,96,97,102] | Trickle-down effects of the economy were thought to contribute to excess harm. Economic stressors (e.g. economic downturns or recession) are more closely associated with morality in the lowest SEP groups. Gross national income and changes in minimum or disposable income has increased the buying power of low SEP groups, which has led to an equalization of alcohol consumption | Report, review, cross-sectional, cohort | General population |
| Socio-political [38,44,46,75,80,84,96] | The attitudes and decision making of residents and policymakers. Politicians focusing on individual behaviours rather than tackling the social determinants of health which increases inequalities. Political context is extremely important, as countries with poor minimum living standards, limited public investment in social goods (particularly in deprived areas) and worse social system responses are likely to worsen health outcomes for low SEP groups | Cross-sectional, case–control, cohort, report, commentary, review | General population, patient | ||
| Alcohol policy [41,61,75,87,96] | The mutually beneficial economic relationship between the state and the alcohol industry shapes policy decisions. Although it is hoped that this is counterbalanced by ‘helping professions’ it is also in their interest to continue the expansion of treatment and this is deflected by each entity casting blame on the another. Additionally, a lack of policy that aims to reduce harmful consumption, alcohol availability, pricing and promotion, and global market liberalization (changes in affordability), production, importation, distribution, and pricing of alcohol were hypothesized to contribute to the AHP | Cohort, discussion paper, report, review | Adults with long-term conditions | ||
| Corporate influence [61] | The alcohol industry funds alcohol research which may misinform policy decision-making. Privately owned media was also argued to play a role via diffusing true or false information | Discussion paper | NA | ||
| Employment [9,14,43,52,74,75,81,96] | There were several mechanisms through which employment could worsen alcohol-related harms for low SEP groups. This included the working conditions or occupational exposures faced by low SEP individuals. Job type, low wages and inflexible employment, and job alienation, stress and low satisfaction are all thought to negatively impact harm outcomes. Those from more deprived backgrounds with insecure employment may also be less able to take time off work when they become ill, compounding the problem. This contrasts with the idea that high SEP individuals may get more support from their employers, whereby employers are more willing to invest energy in solving their alcohol problems. Relatedly issues of unemployment were also discussed including the issue of receiving additional help of benefits related to a long-term condition or disability which may discourage some people from getting better as they would lose this additional help as a result | Cohort, report, case–control, cross-sectional, review | General population, male patients | ||
| Power [61] | Dominant groups in society may suppress subordinate groups via different means (e.g. variable wages, segmented social status), therefore fragmenting groups. These subgroups would then experience greater discrimination and stigma, while the status quo is maintained by the dominant groups having individualistic beliefs. This coupled with social control: the idea that the most powerful individuals have an interest in subordinate groups adopting deviant or socially problematic behaviour which in turn is defined by the powerful, facilitates a ‘revolving door’ system by which the same individuals pass through a multitude of institutions including hospitals, jails, and clinics | Discussion paper | NA | ||
| Broad determinants [45,46,85,90] | Other broad factors, such as social and commercial determinants of health, are the causal factors associated with low SEP which may explain the AHP | Cohort, commentary | General population | ||
| Artefact | Downward drift | Reverse causation [1,4,21,45,53,57,74,81,85] | Heavier drinkers are more likely to lose their job or move to deprived areas due to their heavy drinking. The existence of an alcohol problem is the driving force behind low SEP, rather than low SEP having an independent association with increased harm | Report, cross-sectional, cohort, report, case–control, commentary | General population |
| Methodological | Under-reporting/measurement error [3,14,42,44,47,59,60,64,71,74,90,94,103] | The use of self-report measures allows the opportunity for response bias and memory limitation to impact the results. Measures which rely on binge drinking beyond a threshold instead of individual units is not accurate at capturing differences in the proportions of non-drinkers between SEP groups | Systematic review, meta-analysis, report, cohort, case–control, cross-sectional, commentary | Young adults, patient, general population | |
| Unmeasured factors [44] | Not all confounders are measured. For example, the way cigarette smoke is inhaled or the type of cigarette could have an impact on harm | Case–control | Patient | ||
| Study Design [46] | Need to use more longitudinal data when investigating the AHP particularly to account for time-dependent effects | Cohort | General population | ||
| Under-representation [3,14,21,85,94] | The heaviest drinkers in deprived areas are often under-represented in studies. This is a potential confounder for cross-sectional studies using aggregate data, as once the heaviest drinkers are accounted for higher rates of harm are no longer paradoxical | Systematic review, meta-analysis, report, commentary | NA | ||
SEP = socio-economic position; LGBT = lesbian, gay, bisexual, transgender; NA = not applicable; TB = tuberculosis.
Figure 2.
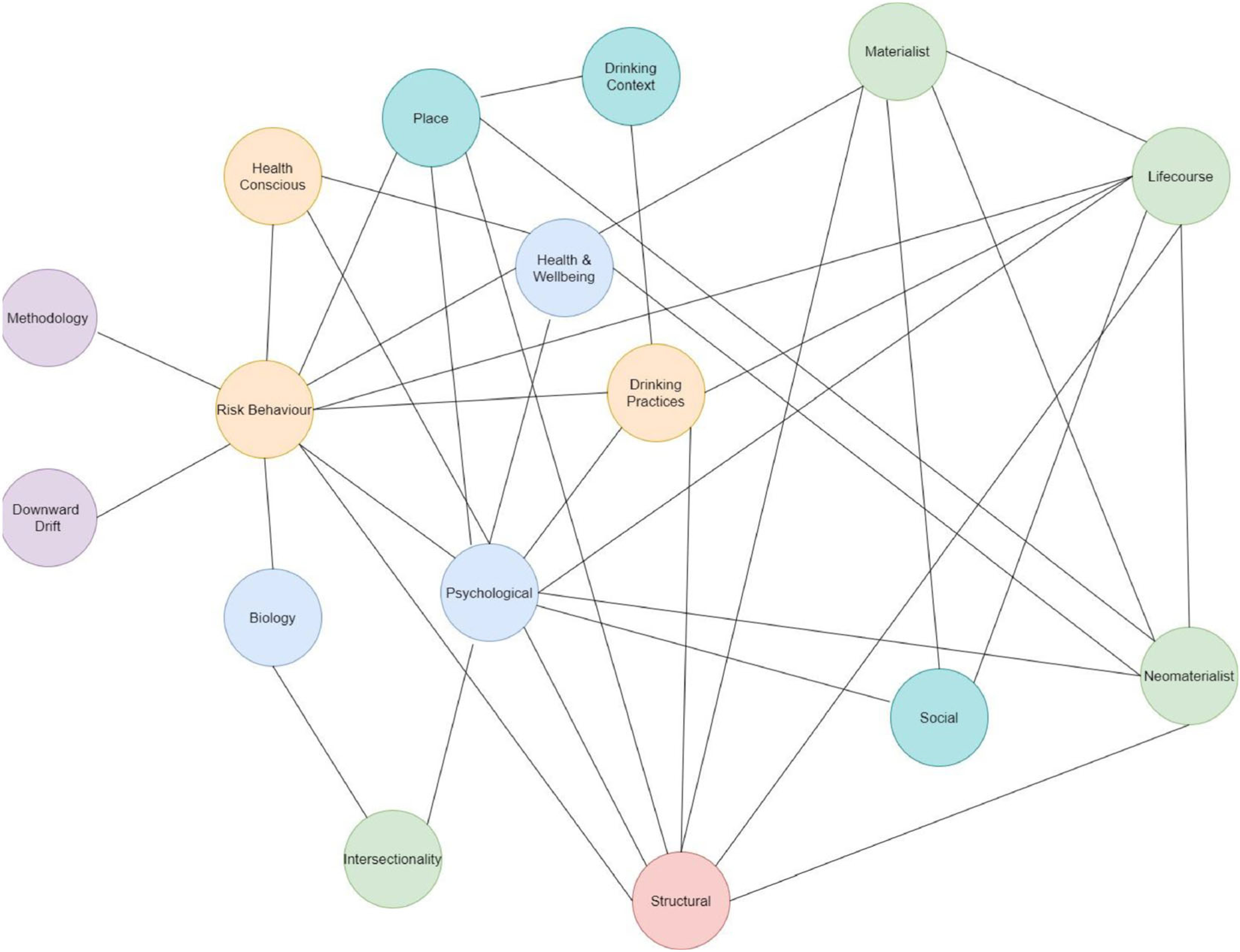
Network diagram illustrating the connections between themes. Domain key: purple = artefactual; orange = life-style; blue = individual; green = disadvantage; turquoise = contextual; red = upstream
Individual
Individual explanations consisted of processes which take place within individuals that could increase their susceptibility to alcohol-related harm. Themes within this domain included biological (n = 7), psychological (n = 22) and health and wellbeing (n = 19) (Table 3). Explanations within the individual domain were often not amenable to human intervention (e.g. genetic make-up or a pre-existing physical health condition).
Individual explanations for the AHP were only hypothesized and had not been tested within any causal or correlational analyses. In related areas, one author has used the tension reduction model to explain alcohol consumption (the idea that alcohol is consumed as a coping strategy to achieve tension reduction) [33]. There was also some evidence to suggest coping strategies more broadly [8,34], and abstention due to pre-existing health conditions [34,35] differed by SEP. Another paper highlighted that the biological effects of social inequality which leads to higher mortality of lower social classes has been observed in primates [34]. However, given the lack of evidence it is unclear whether these explanations contribute to the AHP.
Life-style
The life-style domain focused upon health behaviour of individuals and groups. These were distinct from individual explanations, as they involved an element of choice. Themes were risk behaviour (n = 51), drinking practices (n = 11) and health-consciousness (n = 10) (Table 3). One paper explicitly referred to theories of social practice (the context, how and why of drinking) when discussing how drinking practices at the group level could contribute to the paradox [36]. Another discussed diffusion of innovation theory: the idea that higher SEP groups are faster to adopt new and healthier behaviours [37].
Several papers (n = 21) investigated the role of risk behaviour in explaining the AHP. One study highlighted higher rates of hazardous behaviour (e.g. creating a public disturbance or physically abusing someone) among the socio-economically advantaged rather than the disadvantaged [38]. Another study also highlighted that, for young adults, risky alcohol consumption and heavy drinking was more prevalent in the employed compared to the unemployed, while alcohol-related problems were greater for the unemployed [42]. Otherwise, there was evidence to suggest that drinking patterns and clustering of health behaviours may play some role, as several cross-sectional studies highlighted that those of a low SEP tend to engage in heavier drinking patterns and multiple unhealthy behaviours [8,21,22,30,39–41]. Those testing the causal role of risk behaviour (n = 13) found that these factors partially attenuate the AHP but could not fully explain excess harm experienced by lower SEP groups [3,4,9,18,43–48]. For example, one record linkage study revealed that when adjusting for alcohol consumption, heavy drinking, BMI and smoking, the hazard ratio for the most deprived group compared to the least deprived was 2.71 [95% confidence interval (CI) = 2.01–3.64] [4]. However, two studies found that controlling for drinking pattern completely accounted for differences in alcohol-related problems in an adult and young adult population [49,50]. In contrast, there was no evidence on the impact of drinking practices or the protective effects of health-consciousness.
Contextual
Contextual factors were those in the individual’s immediate environment which may contribute to the AHP. Themes included social (n = 20), drinking context (n = 11) and place (n = 18) (Table 3).
Although widely discussed, contextual explanations lacked empirical testing. One study, using a within- and between-subjects design, found that when individuals live in neighbourhoods with higher levels of poverty they report 5% more negative alcohol consequences compared to when they lived in a wealthier area [credible interval (CR) = 1.05; 95% CI = 1.00, 1.11; P = 0.045] and those who, on average, reside in more impoverished areas also report more negative alcohol consequences (CR = 1.27; 95% CI = 1.10, 1.46; P = 0.001) [51]. Some studies provided evidence that social factors (e.g. marital status) provide a protective effect [9,52]. However, the limited evidence on other contextual factors, including the relationship between outlet density, consumption and harm, was mixed [53,54].
Disadvantage
Explanations in the disadvantage domain tended to focus upon the lived experience of those in poverty and how different facets of this may contribute to the AHP. Themes included intersectionality (n = 8), life-course (n = 14), material (n = 10) and neo-materialist (n = 21) (Table 3).
Despite repeatedly appearing in the discussion sections of included papers, only a few explanations associated with disadvantage were empirically tested. Adjusting for material and behavioural factors [45] or cumulative behaviours during the life-course [37] attenuated the relationship between SEP and harm by 18–31% and 38–77%, respectively. There was also evidence that early SEP, disadvantage during adulthood and negative prenatal factors (e.g. maternal heavy drinking) all increased the risk of developing a comorbid mental health and alcohol use disorder, which was not attenuated when controlling for own adolescent drinking [55].
Upstream
The upstream domain captured explanations at the macro-level which were hypothesized to have effects on alcohol-related harm. Themes included economic (n = 11), socio-political (n = 7), alcohol policy (n = 5), corporate influence (n = 1), employment (n = 8), power (n = 1) and broad determinants (n = 4) (Table 3). These explanations focused upon the structure of society rather than factors associated with belonging to SEP groups. However, the pathways between these societal structures and alcohol harm were not well explained.
None of the included papers attempted to empirically assess whether structural factors can account for the AHP. There was evidence to suggest that economic stressors are more closely associated with mortality in the lowest SEP groups [33,56]. There is also mixed evidence that negative health effects associated with job loss are concentrated in those already at risk due to pre-existing alcohol problems [57], and that SEP overlaps with harmful occupational exposures [43]. However, the extent to which these contribute to the AHP is unknown.
Artefactual
Artefactual explanations claimed the AHP was found due to error. Themes included downward drift (n = 9) and methodological (n = 16) (Table 3).
There was evidence which opposed artefactual explanations for the AHP. Although downward drift was commonly discussed, the only study to test it found that it could not account for the AHP [4]. Record linkage and longitudinal studies also support the existence of the paradox [4,9,37,40,41,45,52,55,57–63], and therefore diminished concerns of under-representation of low-income heavy drinkers in the alcohol consumption data. Another study highlighted that adjusting for alcohol biomarkers only slightly attenuated socio-economic differences in alcohol mortality (1.0–12.1%), suggesting that measurement error is not a probable explanation for the AHP [64]. There was a lack of evidence investigating the impact of often unmeasured factors (e.g. type of cigarette).
Relationships between the thematic explanations
The relationships between all themes (colour-coded for domain) are shown in Fig. 2. The connections represent where authors have combined themes within a single explanation. For example, the methodology theme is connected to risk behaviour, as one explanation argues that lower SEP groups drink more than they self-report and their heavy consumption leads to greater harm [60].
It is clear that risk behaviour is central to explanations for the AHP, with the greatest number of connections to other themes (n = 10) and links with every other domain (Fig. 2). This is unsurprising, given that health risk behaviours have been the focus of empirical efforts to understand the causes of the AHP.
Other themes, specifically within the upstream and disadvantage domains, were also well connected, possessing connections to four of the five domains. Despite this, they lacked empirical testing.
However, some themes—biological, intersectionality, drinking context and those in the artefactual domain—only had one or two connections. This could reflect the characteristics of the explanation; for example, one of the methodological explanations suggests that, due to the use of self-report measures, research has failed to capture accurate levels of alcohol consumption for low SEP groups: they consume more than they report. Alternatively, the lack of connectivity could reflect value in terms of what researchers think are important explanations for the paradox.
DISCUSSION
This review examined explanations for the AHP to identify potential pathways and mechanisms which result in differential risk of harm between SEP groups. This is a new approach, and goes beyond previous systematic reviews and meta-analyses which have so far established the existence of the AHP and the contribution of alcohol to this relationship [3,18]. We identified 16 themes within six domains used to explain the AHP. Risk behaviours were the most prevalent explanations. This finding, paired with the dominance of the behavioural paradigm in empirical work, suggests that there has been a reliance upon using risk behaviour to understand the AHP. Evidence found in this review opposed the idea that the AHP was an artefact. There were many other, mainly hypothetical, explanations for the AHP proposed in the literature. This included individual-level mechanisms (e.g. biological or psychological), contextual factors (e.g. place-based factors), the lived experience of disadvantage and upstream structural factors (e.g. the economy and politics). In part, this reflects an awareness that the AHP is complex; there is no simple explanation, and researchers do not view causes in isolation. However, it remains unclear why other re-occurring explanations (e.g. social support or access to health care) have been neglected, while researchers frequently return to risk behaviours. This is particularly puzzling, given that quantitative evidence suggests that risk behaviours only play a partial role [4,47].
There are two potential reasons for this: theoretical and methodological. Study of the AHP is rooted in alcohol epidemiology, which singularly focuses upon the causes and effects of alcohol consumption [65]. More broadly, the field of epidemiology has faced criticism regarding its approach to understand population health. One of the earliest critiques by Krieger points to fundamental errors in developing epidemiological methods rather than theory, with greater weight given to proximal risk factors and a focus upon causes without context [66]. These limitations have led to an emphasis upon individual disease susceptibility and individual-level interventions. Instead, Krieger argues that the eco-social perspective (the idea that biology and biological changes are shaped by the social environment) should be used to understand health [66]. Concerns regarding how causation is viewed in epidemiology have persisted in contemporary public health, with similar criticisms raised more recently [67]. These concerns continue, despite efforts to raise the profile of theories such as the eco-social perspective and calls to adopt pluralist approaches to causality in epidemiology, which stipulate that causation is not a single connection between two things, but the context in which a causal relationship is observed plays a role [67]. Adopting such an approach would change the way alcohol researchers conceptualize and investigate the AHP.
The lack of clear theoretical structuring in epidemiology, which is argued to have led to a focus upon proximal risk factors (e.g. risk behaviours), could also be a symptom of a lack of methods to carry out more complex analyses of distal factors. Possible solutions to this include the use of complex system modelling methods, which have gained traction within public health and are now being implemented in a UK-based project to gain insight into the causal relationships between policy and health-related outcomes [68]. Software architecture has also recently been devised to address how theory can be systematically incorporated into individual-level and agent-based computer simulations to understand health and health behaviours [69]. Applying these computer simulation methods to the AHP could provide the opportunity to shift the empirical focus from risk behaviours to wider determinants, as they can capture complexity and are mechanism-based rather than focused upon testing relationships between variables.
Strengths and limitations
This is the first review, to our knowledge, to catalogue explanations provided for the AHP across a breadth of literature. In taking a broad approach to literature searching and inclusion criteria it was possible to review work from multiple disciplines employing varied methodologies. This led to the identification of a varied set of explanations. However, it is possible that some explanations are more appropriate, depending upon the study design, population and measure of harm. As the primary aim of this review was to collate and review explanations more generally, we did not conduct an in-depth exploration of this issue. However, upon examination there was no evidence that study design or population influenced which explanations were presented. In terms of measures, we found one clear example of an explanation only applicable when using a subjective measure of alcohol harm—those in low SEP groups who drink may feel their outcomes are worse because their peers are more likely to be abstainers [8]. This issue awaits further examination.
This review was restricted to high-income countries. The results and conclusions are therefore only applicable to this context. Furthermore, most papers focused upon the United Kingdom, which may limit generalizability. This was justified, given substantial differences in alcohol environments. However, given that alcohol is a global issue [1], future research should gain insight into how alcohol affects the disadvantaged in low–middle-income countries to help address the deepening of local and global health inequalities.
Another limitation is that only one reviewer screened and extracted data from the papers. We recruited an independent researcher to re-assess a sample of papers for inclusion and extraction. Cross-checking between the two reviewers demonstrated good reliability.
Research and policy implications
The lack of explicit theory used to present explanations is a barrier to understanding the causes of the AHP. The development or application of theory may be fundamental to identify the true causal mechanisms which create and sustain the AHP. Several explanations have been proposed which align with the vast literature detailing theories of health inequality more generally. The eco-social perspective, among those more commonly discussed [e.g. the materialist (the link between wealth and resources and health) or political economy perspective (the idea that risk factors for health inequalities are rooted in structures)] [70], are just some examples of health inequality theory which could be applied to understand the AHP.
The AHP is well-evidenced, and behavioural-related explanations play a partial role. However, these explanations fall short in understanding the complex causes of inequalities in alcohol-related harm. There is a current lack of evidence investigating other explanations found in this review, which makes it difficult to suggest potential interventions to mitigate the AHP. Future research should empirically investigate these alternative explanations for the AHP. Computer simulations models offer one potential way of achieving this aim in the short term and for relatively low cost.
Based on the evidence from this review, the key policy implication is that tackling drinking alone will not reduce inequalities in alcohol-related harm. While there is some evidence that improving multiple health behaviours may attenuate the risk of alcohol-related harm, it is critical that policymakers look to policies outside the scope of public health to mitigate the inequality produced by the paradox.
Conclusions
There are many proposed explanations for the AHP; however, efforts thus far have revolved around risk behaviours as the main cause. Other potentially promising explanations associated within the individual, contextual, disadvantage and upstream domains have remained hypothetical and understudied. Implementation of health inequality theory and complex modelling techniques could provide the opportunity to explore the role of wider determinants in creating and sustaining the AHP.
Additional supporting information may be found online in the Supporting Information section at the end of the article.
Supplementary Material
Table S1 Systematic Search Strategy
Table S2.1 AXIS Critical Appraisal for included cross-sectional studies.
Table S2.2 CASP Critical Appraisal for included case–control studies.
Table S2.3 CASP Critical Appraisal for included cohort studies.
Table S2.4 CASP Quality Appraisal for included qualitative studies
Table S2.5 CASP Quality Appraisal for included systematic reviews.
Acknowledgements
This work was supported by funding from The Wellcome Trust (Award number 108903/B/15/Z). Research reported in this publication was also supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health (Award number R01AA024443)].
Footnotes
Declaration of interests
None.
References
- 1.World Health Organization. Global Status Report on Alcohol and Health 2014. 2014; 1–392. Last Accessed [16/05/21]. Available at: http://www.who.int/substance_abuse/publications/global_alcohol_report/msbgsruprofiles.pdf.
- 2.Krieger N, Williams DR, Moss NE Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health 1997; 18: 341–78 [cited 2020 May 26]. www.annualreviews.org. [DOI] [PubMed] [Google Scholar]
- 3.Probst C, Kilian C, Sanchez S, Lange S, Rehm J The role of alcohol use and drinking patterns in socioeconomic inequalities in mortality: a systematic review. Lancet Public Health 2020; 5(6): e324–e332. 10.1016/S2468-2667(20)30052-9. [DOI] [PubMed] [Google Scholar]
- 4.Katikireddi SV, Whitley E, Lewsey J, Gray L, Leyland AH Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data. Lancet Public Health. 2017; 2(6):e267–e276. Available at: 10.1016/S2468-2667(17)30078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Information Centre for Health and Social Care. Statistics on Alcohol: England. Table 2.12. 2011. Leeds, UK: Information Centre for Health and Social Care; 2011. Last Accessed [16/05/21]. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-alcohol/2011. [Google Scholar]
- 6.Department of Health (DoH). Written Evidence from the Department of Health for the Health Select Committee. London, UK: 2012. Last Accessed [16/05/21]. Available at: https://www.parliament.uk/globalassets/documents/commons-committees/Health/Writtenevidencebyoralwitnesses.pdf. [Google Scholar]
- 7.Giskes K, Turrell G, Bentley R, Kavanagh A Individual and household-level socioeconomic position is associated with harmful alcohol consumption behaviours among adults. Aust NZ J Public Health 2011; 35(3): 270–71 [cited 2020 Apr 8]; 10.1111/j.1753-6405.2011.00683.x. [DOI] [PubMed] [Google Scholar]
- 8.Van Oers JAM, Bongers IMB, Van De Goor LAM, Garretsen HFL Alcohol consumption, alcohol-related problems, problem drinking, and socioeconomic status. Alcohol Alcohol 1999; 34(1): 78–88. [DOI] [PubMed] [Google Scholar]
- 9.Mäkelä P, Paljärvi T Do consequences of a given pattern of drinking vary by socioeconomic status? A mortality and hospitalisation follow-up for alcohol-related causes of the Finnish drinking habits surveys. J Epidemiol Community Health 2008; 62(8): 728–33. [DOI] [PubMed] [Google Scholar]
- 10.Beard E, Brown J, West R, Angus C, Brennan A, Holmes J, et al. Deconstructing the alcohol harm paradox: a population based survey of adults in England. PLOS ONE 2016; 11(9): e0160666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edwards G, Kyle E, Nicholls P, Taylor C Alcoholism and correlates of mortality. Implications for epidemiology. J Stud Alcohol 1978; 39(9): 1607–17. [DOI] [PubMed] [Google Scholar]
- 12.Lindberg S, Agren G Mortality among male and female hospitalized alcoholics in Stockholm 1962–1983. Br J Addict 1988; 83(10): 1193–200. [DOI] [PubMed] [Google Scholar]
- 13.Rossow I, Amundsen A The disadvantage of being advantaged?—on a social gradient in excess mortality among alcohol abusers. Addiction 1996; 91(12): 1821–9. [PubMed] [Google Scholar]
- 14.Smith K, Foster J Alcohol, Health Inequalities and the Harm Paradox: Why some groups face greater problems despite consuming less alcohol. A summary of the available evidence. London, UK: Institute of Alcohol Studies; 2014. Last Accessed [16/05/21]. Available at: https://iogt.org/wp-content/uploads/2015/03/IAS-report-Alcohol-and-health-inequalities-FULL.pdf. [Google Scholar]
- 15.Probst C, Roerecke M, Behrendt S, Rehm J Socioeconomic differences in alcohol-attributable mortality compared with all-cause mortality: a systematic review and meta-analysis. Int J Epidemiol 2014; 43: 1314–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collins SE Associations between socioeconomic factors and alcohol outcomes. Alcohol Res Curr Rev 2016; 38(1): 83–94. [PMC free article] [PubMed] [Google Scholar]
- 17.Grittner U, Kuntsche S, Graham K, Bloomfield K Social inequalities and gender differences in the experience of alcohol-related problems. Alcohol Alcohol 2012; 47(5): 597–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones L, Bates G, McCoy E, Bellis MA Relationship between alcohol-attributable disease and socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis. BMC Public Health 2015; 15(1): 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Probst C, Roerecke M, Behrendt S, Rehm J Gender differences in socioeconomic inequality of alcohol-attributable mortality: a systematic review and meta-analysis. Drug Alcohol Rev 2015; 34(3): 267–77. [DOI] [PubMed] [Google Scholar]
- 20.Angus C, Pryce R, Holmes J, de Vocht F, Hickman M, Meier P, et al. Assessing the contribution of alcohol-specific causes to socio-economic inequalities in mortality in England and Wales 2001–16. Addiction 2020. [cited 2020 Jun 1]; 10.1111/add.15037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bellis MA, Hughes K, Nicholls J, Sheron N, Gilmore I, Jones L The alcohol harm paradox: using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health 2016; 16 (1): 1–10. Available at: 10.1186/s12889-016-2766-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lewer D, Meier P, Beard E, Boniface S, Kaner E Unravelling the alcohol harm paradox: a population-based study of social gradients across very heavy drinking thresholds. BMC Public Health 2016; 16(1): 1–11. Available at: 10.1186/s12889-016-3265-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J Health equity in England: the Marmot review 10 years on. BMJ 2020; 368. https://discovery.ucl.ac.uk/id/eprint/10106434/3/Bockenhauer_BMJ%20Ten%20years%20essay2pg3.pdf. [DOI] [PubMed] [Google Scholar]
- 24.Mackenbach JP, Stirbu I, Roskam A-JR, Schaap MM, Menvielle G, Leinsalu M, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med 2008; 358(23): 2468–81 [cited 2021 Feb 10]. Available at: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman D Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLOS medicine 2009; 6(7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Bank Group. Fact Sheet: OECD High-Income. Doing Business. 2019. Last Accessed [16/05/21] Available at: https://www.doingbusiness.org/content/dam/doingBusiness/media/Fact-Sheets/DB19/FactSheet_DoingBusiness2019_OECD_Eng.pdf. [Google Scholar]
- 27.Walls H, Cook S, Matzopoulos R, Advancing alcohol research in low-income and middle-income countries: a global alcohol environment framework analysis. BMJ Glob Heal. 2020; 5(4): e001958 [cited 2021 Feb 11]. Available at: https://gh.bmj.com/content/bmjgh/5/4/e001958.full.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Downes M, Brennan M, Williams H, Open RD-B Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 2016; 6(12) [cited 2020 May 22]. Available at: https://bmjopen.bmj.com/content/6/12/e011458.short. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Critical Appraisal Skills Programme. CASP Qualitative, Systematic Review, Cohort Study and Case Control Study Checklists 2018. Last Accessed [16/05/21]. Available at: https://casp-uk.net/casp-tools-checklists/. [Google Scholar]
- 30.Norström T, Romelsjö A Social class, drinking and alcohol-related mortality. J Subst Abuse 1998; 10(4): 385–95. [DOI] [PubMed] [Google Scholar]
- 31.Roberts SE, Akbari A, Thorne K, Atkinson M, Evans PA The incidence of acute pancreatitis: impact of social deprivation, alcohol consumption, seasonal and demographic factors. Aliment Pharmacol Ther 2013; 38: 539–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roberts SE, Williams JG, Meddings D, Goldacre MJ Incidence and case fatality for acute pancreatitis in England_geographical variation, social deprivation, alcohol consumption and aetiology—a record linkage study. Aliment Pharmacol Ther 2008; 28: 931–41. [DOI] [PubMed] [Google Scholar]
- 33.Brown RL, Richman JA, Rospenda KM Economic stressors and alcohol-related outcomes: exploring gender differences in the mediating role of somatic complaints. J Addict Dis 2014; 33: 303–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alcohol Chick J., health, and the heart: implications for clinicians. Alcohol Alcohol 1998; 33: 576–91. [DOI] [PubMed] [Google Scholar]
- 35.Evans-Polce RJ, Staff J, Maggs JL Alcohol abstention in early adulthood and premature mortality: do early life factors, social support, and health explain this association? Soc Sci Med [internet] 2016; 163: 71–9. Available at: 10.1016/j.socscimed.2016.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meier PS, Warde A, Holmes J All drinking is not equal: how a social practice theory lens could enhance public health research on alcohol and other health behaviours. Addiction 2018; 113: 206–13. [DOI] [PubMed] [Google Scholar]
- 37.Whitley E, Batty GD, Hunt K, Popham F, Benzeval M The role of health behaviours across the life course in the socioeconomic patterning of all-cause mortality: the West of Scotland Twenty-07 prospective cohort study. Ann Behav Med 2014; 47: 148–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Livingston M Socioeconomic differences in alcohol-related risk-taking behaviours. Drug Alcohol Rev 2014; 33: 588–95. [DOI] [PubMed] [Google Scholar]
- 39.Bellis MA, Hughes S Chapter 3: Alcohol in Bambra C, Joyce KE, & Mayron-Davies. Strategic Review of Health Inequalities in England post 2010 (Marmot Review). 2009. Last Accessed [16/05/21]. Available at: https://dro.dur.ac.uk/6396/2/6396R.pdf. [Google Scholar]
- 40.Degerud E, Ariansen I, Ystrom E, Graff-Iversen S, Høiseth G, Mørland J, et al. Life course socioeconomic position, alcohol drinking patterns in midlife, and cardiovascular mortality: analysis of Norwegian population-based health surveys. PLOS Med 2018; 15: 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stewart D, Han L, Doran T, McCambridge J Alcohol consumption and all-cause mortality an analysis of general practice database records for patients with long-term conditions. J Epidemiol Community Health 2017; 71: 729–35. [DOI] [PubMed] [Google Scholar]
- 42.Thern E, Ramstedt M, Svensson J The associations between unemployment at a young age and binge drinking and alcohol-related problems. Eur J Public Health 2019; 30: 368–73. [DOI] [PubMed] [Google Scholar]
- 43.Menvielle G, Luce D, Goldberg P, Leclerc A Smoking, alcohol drinking, occupational exposures and social inequalities in hypopharyngeal and laryngeal cancer. Int J Epidemiol 2004; 33: 799–806. [DOI] [PubMed] [Google Scholar]
- 44.Stanford-Moore G, Bradshaw PT, Weissler MC, Zevallos JP, Brennan P, Anantharaman D, et al. Interaction between known risk factors for head and neck cancer and socioeconomic status: the Carolina head and neck cancer study. Cancer Causes Control [internet] 2018; 29: 863–73. Available at: 10.1007/s10552-018-1062-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sydén L, Sidorchuk A, Mäkelä P, Landberg J The contribution of alcohol use and other behavioural, material and social factors to socio-economic differences in alcohol-related disorders in a Swedish cohort. Addiction 2017; 112: 1920–30. [DOI] [PubMed] [Google Scholar]
- 46.Peña S, Mäkelä P, Laatikainen T, Härkänen T, Männistö S, Heliövaara M, et al. Joint effects of alcohol use, smoking and body mass index as an explanation for the alcohol harm paradox: causal mediation analysis of eight cohort studies. Addiction 2021; 1–11. 10.1111/add.15395. [DOI] [PubMed] [Google Scholar]
- 47.Gartner A, Trefan L, Moore S, Akbari A, Paranjothy S, Farewell D Drinking beer, wine or spirits—does it matter for inequalities in alcohol-related hospital admission? A record-linked longitudinal study in Wales. BMC Public Health 2019; 19: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Møller SP, Pisinger VSC, Christensen AI, Tolstrup JS Socioeconomic position and alcohol-related harm in Danish adolescents. J Epidemiol Community Health 2019; 73: 839–45. [DOI] [PubMed] [Google Scholar]
- 49.Huckle T, You RQ, Casswell S Socio-economic status predicts drinking patterns but not alcohol-related consequences independently. Addiction 2010; 105: 1192–202. [DOI] [PubMed] [Google Scholar]
- 50.Thor S, Karlsson P, Landberg J Social inequalities in harmful drinking and alcohol-related problems among Swedish adolescents. Alcohol Alcohol 2019; 54: 532–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rhew IC, Duckworth JC, Hurvitz PM, Lee CM Within- and between-person associations of neighborhood poverty with alcohol use and consequences: a monthly study of young adults. Drug Alcohol Depend 2020; 212: 108068; 10.1016/j.drugalcdep.2020.108068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Singh GK, Hoyert DL. Social epidemiology of chronic liver disease and cirrhosis mortality in the United States, 1935–1997: trends and differentials by ethnicity, socioeconomic status, and alcohol consumption. Human biology. 2000. October 1:801–20. [PubMed] [Google Scholar]
- 53.Jones L, McCoy E, Bates G, Bellis MA, Sumnall H Understanding the Alcohol Harm Paradox in Order to Focus the Development of Interventions. London, UK: Alcohol Research UK; 2015. Last Accessed [16/05/21]. Available at: https://alcoholchange.org.uk/publication/understanding-the-alcohol-harm-paradox. [Google Scholar]
- 54.Connor JL, Kypri K, Bell ML, Cousins K Alcohol outlet density, levels of drinking and alcohol-related harm in New Zealand: a national study. J Epidemiol Community Health 2010; 65: 841–6. [DOI] [PubMed] [Google Scholar]
- 55.Salom CL, Williams GM, Najman JM, Alati R Does early socio-economic disadvantage predict comorbid alcohol and mental health disorders? Drug Alcohol Depend 2014; 142: 146–53. Available at: 10.1016/j.drugalcdep.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 56.Herttua K, Mäkelä P, Martikainen P Differential trends in alcohol-related mortality: a register-based follow-up study in Finland in 1987–2003. Alcohol Alcohol 2007; 42: 456–64. [DOI] [PubMed] [Google Scholar]
- 57.Backhans MC, Balliu N, Lundin A, Hemmingsson T Unemployment is a risk factor for hospitalization due to alcohol problems: a longitudinal study based on the Stockholm public health cohort (SPHC). J Stud Alcohol Drugs 2016; 77: 936–42. [DOI] [PubMed] [Google Scholar]
- 58.Lundin A, Backhans M, Hemmingsson T Unemployment and hospitalization owing to an alcohol-related diagnosis among middle-aged men in Sweden. Alcohol Clin Exp Res 2012; 36: 663–9. [DOI] [PubMed] [Google Scholar]
- 59.Major JM, Sargent JD, Graubard BI, Carlos HA, Hollenbeck AR, Altekruse SF, et al. Local geographic variation in chronic liver disease and hepatocellular carcinoma: contributions of socioeconomic deprivation, alcohol retail outlets, and lifestyle. Ann Epidemiol 2014; 24: 104–10. Available at: 10.1016/j.annepidem.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McDonald SA, Hutchinson SJ, Bird SM, Graham L, Robertson C, Mills PR, et al. Association of self-reported alcohol use and hospitalization for an alcohol-related cause in Scotland: a record-linkage study of 23 183 individuals. Addiction 2009; 104: 593–602. [DOI] [PubMed] [Google Scholar]
- 61.Sargent M Drinking and the perpetuation of social inequality in Australia. Med Law 1989; 8: 507–16. [PubMed] [Google Scholar]
- 62.Shaper AG, Wannamethee G, Walker M Alcohol and mortality in British men: explaining the U-shaped curve. Lancet 1988; 332: 1267–73. [DOI] [PubMed] [Google Scholar]
- 63.Lawder R, Grant I, Storey C, Walsh D, Whyte B, Hanlon P Epidemiology of hospitalization due to alcohol-related harm: evidence from a Scottish cohort study. Public Health 2011; 125: 533–9. Available at: 10.1016/j.puhe.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 64.Peña S, Mäkelä P, Härkänen T, Heliövaara M, Gunnar T, Männistö S, et al. Alcohol-related harm measurement error as an explanation for the alcohol harm paradox: analysis of eight cohort studies. Int J Epidemiol 202049:1836–1846. https://academic.oup.com/ije/article/49/6/1836/5913111. [DOI] [PubMed] [Google Scholar]
- 65.Rossow I, Norström T The use of epidemiology in alcohol research. Addiction 2013; 108: 20–5 [cited 2020 Jul 17]. Available at: 10.1111/j.1360-0443.2012.04031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Krieger N Epidemiology and the web of causation has anyone seen the spider? Soc Sci Med 1994; 39: 887–903 [cited 2020 Jul 17]. Available at: https://reader.elsevier.com/reader/sd/pii/027795369490202X?token=8B4BB2D36238D22301AE3A78054F3DB56B20C4A19EED15BCAFE507A1D2DA57A35EDEEC3CD206F5B4FB42631E28973517. [DOI] [PubMed] [Google Scholar]
- 67.Vandenbroucke JP, Broadbent A, Pearce N Causality and causal inference in epidemiology: the need for a pluralistic approach. Int J Epidemiol 201645(6):1776–86 [cited 2020 Jul 17]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Meier P, Purshouse R, Bain M, Bambra C, Bentall R, Birkin M et al. The SIPHER Consortium: Introducing the new UK hub for systems science in public health and health economic research [version 1; peer review: 2 approved] [internet], vol. 4. Wellcome Open Research, F1000 Research Ltd; 2019, p. 174. Last Accessed [16/05/21]. Available at: 10.12688/wellcomeopenres.15534.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vu TM, Probst C, Nielsen A, Bai H, Buckley C, Meier PS, et al. A software architecture for mechanism-based social systems modelling in agent-based simulation models. JASSS 2020; 23(3):1–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Smith KE, Bambra C, Hill SE Health Inequalities: Critical Perspectives. Oxford, UK: Oxford University Press; 2016. [Google Scholar]
- 71.Bloomfield K Understanding the alcohol-harm paradox: what next? Lancet Public Health [internet] 2020; 5: e300–e301. Available at: 10.1016/S2468-2667(20)30119-5. [DOI] [PubMed] [Google Scholar]
- 72.Boyle T, Fritschi L, Tabatabaei SM, Ringwald K, Heyworth JS Smoking, alcohol, diabetes, obesity, socioeconomic status and the risk of colorectal cancer in a population-based case–control study. Cancer Causes Control 2014; 25: 1659–68. [DOI] [PubMed] [Google Scholar]
- 73.Breakwell C, Baker A, Griffiths C, Jackson G, Fegan G, Marshall D Trends and geographical variations in alcohol-related deaths in the United Kingdom, 1991–2004. Health Stat Q 2007; 33: 6–24. [PubMed] [Google Scholar]
- 74.Conway DI, Brenner DR, McMahon AD, Macpherson LMD, Agudo A, Ahrens W, et al. Estimating and explaining the effect of education and income on head and neck cancer risk: INHANCE consortium pooled analysis of 31 case–control studies from 27 countries. Int J Cancer 2015; 136: 1125–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.VicHealth. Reducing Alcohol-related Health Inequities. An Evidence Summary. Melbourne, Australia: VicHealth; 2015. Last Accessed [16/05/21]. Available at: https://www.vichealth.vic.gov.au/-/media/ResourceCentre/PublicationsandResources/Health-Inequalities/Fair-Foundations/Summary/Health-Equity_Summary-Report_Acohol.pdf?la=en&hash=9A176F33C7D55ABFC1A1F50B7BB654530EBC1786. [Google Scholar]
- 76.Fillmore K, Golding JM, Graves KL, Kniep S, Leino EV, Romelsjö A, et al. Alcohol consumption and mortality. I. Characteristics of drinking groups. Addiction 1998; 93: 183–203. [DOI] [PubMed] [Google Scholar]
- 77.Hall W Socioeconomic status and susceptibility to alcohol-related harm. Lancet Public Health [internet] 2017; 2: e250–e251. Available at: 10.1016/S2468-2667(17)30089-0. [DOI] [PubMed] [Google Scholar]
- 78.Hart A Assembling interrelations between low socioeconomic status and acute alcohol-related harms among young adult drinkers. Contemp Drug Probl 2015; 42: 148–67. [Google Scholar]
- 79.Jonas H, Dietze P, Rumbold G, Hanlin K, Cvetkovski S, Laslett AM Associations between alcohol related hospital admissions and alcohol consumption in Victoria: influence of socio-demographic factors. Aust NZ J Public Health 1999; 23: 272–9. [DOI] [PubMed] [Google Scholar]
- 80.Karriker-Jaffe KJ, Zemore SE, Mulia N, Jones-Webb R, Bond J, Greenfield TK Neighborhood disadvantage and adult alcohol outcomes: differential risk by race and gender. J Stud Alcohol Drugs 2012; 73: 865–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Karriker-Jaffe KJ, Roberts SCM, Bond J Income inequality, alcohol use, and alcohol-related problems. Am J Public Health 2013; 103: 649–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Katikireddi SV, Whitley E, Lewsey J, Leyland AH Alcohol consumption, wealth, and health – Authors’ reply. Lancet Public Health 2017; 2: e354. Available at: 10.1016/S2468-2667(17)30142-1. [DOI] [PubMed] [Google Scholar]
- 83.Kuendig H, Plant ML, Plant MA, Kuntsche S, Miller P, Gmel G, et al. Beyond drinking: differential effects of demographic and socioeconomic factors on alcohol-related adverse consequences across European countries. Eur Addict Res 2008; 14: 150–60. [DOI] [PubMed] [Google Scholar]
- 84.Makela P Commentary: Addressing inequalities in alcohol problems: the Marathon has only just begun. Addiction 2008; 103: 1294–5. [DOI] [PubMed] [Google Scholar]
- 85.Marmot MG Commentary: Reflections on alcohol and coronary heart disease. Int J Epidemiol 2001; 30: 729–34. [DOI] [PubMed] [Google Scholar]
- 86.Mayor S Greater adverse effects of alcohol consumption in deprived communities are explained in study. BMJ 2016; 352: i992. 10.1136/bmj.i992. [DOI] [PubMed] [Google Scholar]
- 87.Beeston C, Mcauley A, Robinson M, Craig N, Graham L Monitoring and Evaluating Scotland’s Alcohol Strategy. Edinburgh, UK: NHS Scotland; 2016. Last Accessed [16/05/21]. Available at: http://www.healthscotland.scot/media/1100/mesas-final-annual-report_5780_mar-2016.pdf. [Google Scholar]
- 88.Mulia N, Karriker-Jaffe KJ Interactive influences of neighborhood and individual socioeconomic status on alcohol consumption and problems. Alcohol Alcohol 2012; 47: 178–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mulia N, Zemore SE Social adversity, stress, and alcohol problems: are racial/ethnic minorities and the poor more vulnerable? J Stud Alcohol Drugs 2012; 73: 570–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nielsen NR, Schnohr P, Jensen G, Grønbæk M Is the relationship between type of alcohol and mortality influenced by socio-economic status? J Intern Med 2004; 255: 280–8. [DOI] [PubMed] [Google Scholar]
- 91.Norström T, Landberg J The link between per capita alcohol consumption and alcohol-related harm in educational groups. Drug Alcohol Rev 2020; 39: 656–63. [DOI] [PubMed] [Google Scholar]
- 92.Nweze IC, DiGiacomo JC, Shin SS, Gupta C, Ramakrishnan R, Angus LDG Demographic and socioeconomic factors influencing disparities in prevalence of alcohol-related injury among underserved trauma patients in a safety-net hospital. Injury 2016; 47: 2635–41. Available at: 10.1016/j.injury.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 93.Parkman T, Neale J, Day E, Drummond C Qualitative exploration of why people repeatedly attend emergency departments for alcohol-related reasons. BMC Health Serv Res 2017; 17: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gartner A, Francis I, Hickey D, Hughes R, May L, Cosh H et al. Alcohol and Health in Wales 2014. Cardiff, UK: NHS Wales; 2014. Last Accessed [16/05/21]. Available at: http://www2.nphs.wales.nhs.uk:8080/PubHObservatoryProjDocs.nsf/85c50756737f79ac80256f2700534ea3/d7ead329fc08591480257d7200326f03/$FILE/AlcoholAndHealthInWales2014_v2a.pdf. [Google Scholar]
- 95.Rehm J, Probst C What about drinking is associated with shorter life in poorer people? PLOS Med 2018; 15: 10–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Roche A, Kostadinov V, Fischer J, Nicholas R, O’Rourke K, Pidd K, et al. Addressing inequities in alcohol consumption and related harms. Health Promot Int 2015; 30: ii20–ii35. [DOI] [PubMed] [Google Scholar]
- 97.Romelsjö A, Lundberg M The changes in the social class distribution of moderate and high alcohol consumption and of alcohol-related disabilities over time in Stockholm County and in Sweden. Addiction 1996; 91: 1307–24. [DOI] [PubMed] [Google Scholar]
- 98.Sadler S, Angus C, Gavens L, Gillespie D, Holmes J, Hamilton J, et al. Understanding the alcohol harm paradox: an analysis of sex- and condition-specific hospital admissions by socio-economic group for alcohol-associated conditions in England. Addiction 2017; 112: 808–17. [DOI] [PubMed] [Google Scholar]
- 99.Skogen JC, Bøe T, Thørrisen MM, Riper H, Aas RW Sociodemographic characteristics associated with alcohol consumption and alcohol-related consequences, a latent class analysis of the Norwegian WIRUS screening study. BMC Public Health 2019; 19: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Trias-Llimós S, Bosque-Prous M, Obradors-Rial N, Teixidó-Compañó E, Belza MJ, Janssen F, et al. Alcohol and educational inequalities: hazardous drinking prevalence and all-cause mortality by hazardous drinking group in people aged 50 and older in Europe. Subst Abuse 20201–9. Available at: 10.1080/08897077.2020.1773597. [DOI] [PubMed] [Google Scholar]
- 101.World Health Organization. Alcohol and inequities. 2014; iv–23. Last Accessed [16/05/21]. Available at: http://www.euro.who.int/_data/assets/pdf_file/0003/247629/Alcohol-and-Inequities.pdf.
- 102.Schmidt L, Makela P, Rehm J, Room R Chapter 2: Alcohol: equity and social determinants. In: Blas E, Kuru AS, editors. Equity, Social Determinants and Public Health Programmes. Geneva, Switzerland: WHO Press; 2010, pp. 11–30. [Google Scholar]
- 103.Wood S, Bellis M Socio-economic inequalities in alcohol consumption and harm: Evidence for effective interventions and policy across EU countries. Cardiff, UK: Public Health Wales; 2015, pp. 1–29. https://ec.europa.eu/health/sites/default/files/social_determinants/docs/hepp_screport_alcohol_en.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Systematic Search Strategy
Table S2.1 AXIS Critical Appraisal for included cross-sectional studies.
Table S2.2 CASP Critical Appraisal for included case–control studies.
Table S2.3 CASP Critical Appraisal for included cohort studies.
Table S2.4 CASP Quality Appraisal for included qualitative studies
Table S2.5 CASP Quality Appraisal for included systematic reviews.


