Introduction
Cardiopulmonary exercise testing (CPET) is the gold standard measure of aerobic fitness (VO2peak), a powerful indicator of an older adults’ capacity to perform daily and recreational activities (VO2peak >18 mL/kg/min indicative of functional independence).1 However, maximal effort during CPET performance may be limited by functional status and is not always feasible in epidemiologic studies due to rigorous staff training, equipment requirements, participant burden, and potential inconsistency across clinical centers. Subsequently, a fast-paced overground long-distance corridor walk (LDCW), a safer and less-expensive alternative for older adults, was validated against treadmill CPET.2 However, many clinical and epidemiologic studies include a usual-paced 400m LDCW in lieu of a fast-paced walk.3 With increasing frailty and age, even a usual-paced 400m LDCW may be challenging and elicit ones’ maximal capacity, as evidenced by comparable performance on fast-paced and usual-paced 400m LDCW tests for those older and lower functioning.4 Therefore, the usual-paced LDCW may estimate CPET performance, though this has not been previously shown.
This report examined whether a usual-paced 400m LDCW was related to VO2peak measured from treadmill CPET.
Methods
Community-dwelling older adults (N=36) aged 70-89 years were enrolled in the cross-sectional Study of Energy and Aging - Pilot (SEA-P), the pilot to the Study of Muscle, Mobility, and Aging (SOMMA).5 Institutional Review Boards at the University of Pittsburgh and California Pacific Medical Center approved SEA-P, and written informed consent was obtained.
Participants were instructed to complete the 400m LDCW at their “usual or normal walking pace” down a long hallway marked with traffic cones spaced 20m apart with time to completion (seconds) recorded. VO2peak was determined using a modified Balke protocol following American College of Sports Medicine criteria,6 with strong encouragement to reach a respiratory exchange ratio >1.05 and Borg RPE >16.5 Treadmill speed was held constant at the participants’ fastest of two usual-paced gait speed 6m walks. Treadmill grade began at 0% and increased by 2% every 2 minutes until volitional exhaustion.5 Covariates examined: age, sex, and physical fatigue (Situational Fatigue Scale7).
Two participants completed the usual-paced 400m LDCW, but were unable to finish CPET; final analytic sample N=34. We generated Pearson correlations between VO2peak and covariates. Linear regression analysis estimated VO2peak (outcome) and usual-paced 400m LDCW time (independent variable), adjusted for covariates. Statistical analyses were conducted using SAS v9.4 (SAS Institute, Inc., Cary, NC).
Results
SEA-P participants were mean age 78.2±5.1 years, largely male (59%) and white (94%), with physical fatigue score=6.4±4.2 (scale range: 0-20), and Short Physical Performance Battery score=10.9±1.3 (test range: 0-12), indicating higher function. Participants had a VO2peak of 22.1±5.6 mL/kg/min (range: 7.8-33.4 mL/kg/min). Time to complete the usual-paced 400m LDCW was 339.6±60.4s (range: 252.5s-536.0s). VO2peak was strongly inversely correlated (r=−0.64, p<.0001, Figure 1) with usual-paced 400m LDCW time and moderately inversely correlated with age (r=−0.41) and physical fatigue score (r=−0.42), both p<.02.
Figure 1.
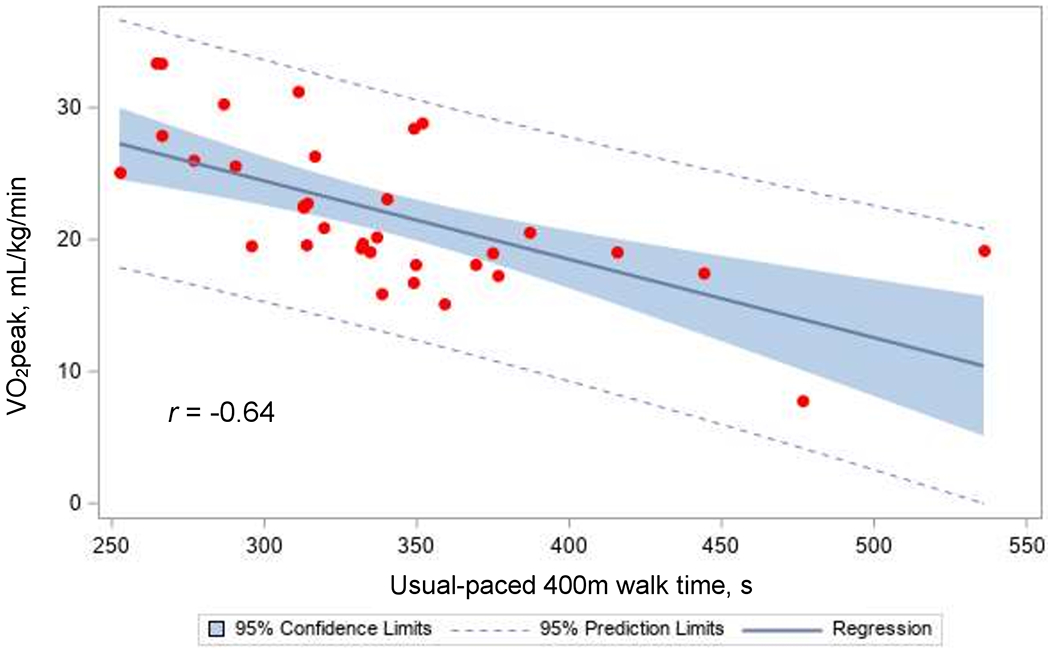
Correlation between time to complete a usual-paced 400m long-distance corridor walk and cardiorespiratory fitness (VO2peak) measured by treadmill cardiopulmonary exercise testing with a modified Balke protocol.
Every 30 seconds longer (i.e., slower) time to complete the usual-paced 400m LDCW was associated with a 1.5 mL/kg/min lower measured VO2peak adjusted for age and physical fatigue score (p=.0002), explaining 41% of the 57% total model variance in VO2peak (Supplemental Table 1). Age (8%) and fatigue (8%) also contributed to the explained variance in VO2peak (both p=.03). Adding sex did not improve the estimation of VO2peak, p=.27.
Discussion
We established that usual-paced 400m LDCW time strongly estimated cardiorespiratory fitness in older adults after age and physical fatigue adjustment. As expected, age was associated with VO2peak, but usual-paced 400m LDCW time explained >5-fold more of the model variance than age. Physical fatigue score also explained some variance in VO2peak, supporting existing evidence that higher fatigue relates to poorer exercise capacity8,9 All participants completed the LDCW, but two were unable to finish the CPET, highlighting the utility for an alternative measurement of VO2peak.
Limitations include small sample size and using a less sensitive measure of one’s perception of fatigue.9,10 Furthermore, the SEA-P sample was relatively high functioning, hence more research is needed to confirm our findings in lower functioning older adults. A strength was measuring VO2peak with the well-established, standardized modified Balke protocol.
Our findings demonstrate initial support for using a usual-paced 400m LDCW as a viable alternative for measuring cardiorespiratory fitness in older adults, thus providing another low-cost, safer option for research and clinical settings. The ability to identify at-risk older adults with poor walking endurance indicative of prevalent or impending mobility limitations is important for early interventions. Future research in SOMMA may confirm and extend this work, as its large sample will allow for subgroup analyses by age, sex, physical function, and fatigability severity.
Supplementary Material
Supplemental Table 1. Final model for estimating cardiorespiratory fitness (VO2peak, mL/kg/min) using a usual-paced 400m long distance corridor walk: Study of Energy and Aging – Pilot (N=34)
Financial Disclosure:
This work was supported by the National Institutes of Health, National Institute on Aging, American Recovery and Reinvestment Act grant RC2 AG036594, the University of Pittsburgh Claude D. Pepper Older Americans Independence Center Research Registry P30 AG024827. Additionally, the National Institute on Aging Epidemiology of Aging training grant T32 AG000181 at the University of Pittsburgh supported KJM and BSL. AJS was supported by National Institute on Aging grant K01 AG057726.
Footnotes
Preliminary findings were presented at the 2014 American College of Sports Medicine Annual Meeting, Orlando, FL, May, 2014.
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Sponsor’s Role: None
References
- 1.Huggett DL, Connelly DM, Overend TJ. Maximal aerobic capacity testing of older adults: a critical review. J Gerontol A, Biol Sci Med Sci. 2005;60(1):57–66. doi: 10.1093/gerona/60.1.57 [DOI] [PubMed] [Google Scholar]
- 2.Simonsick EM, Fan E, Fleg JL. Estimating cardiorespiratory fitness in well-functioning older adults: treadmill validation of the long distance corridor walk. J Am Geriatr Soc. 2006;54(1):127–132. doi: 10.1111/j.1532-5415.2005.00530.x [DOI] [PubMed] [Google Scholar]
- 3.Rolland YM, Cesari M, Miller ME, Penninx BW, Atkinson HH, Pahor M. Reliability of the 400-m usual-pace walk test as an assessment of mobility limitation in older adults. J Am Geriatr Soc. 2004;52(6):972–976. doi: 10.1111/j.1532-5415.2004.52267.x [DOI] [PubMed] [Google Scholar]
- 4.Lange-Maia BS, Newman AB, Strotmeyer ES, Harris TB, Caserotti P, Glynn NW. Performance on fast- and usual-paced 400-m walk tests in older adults: are they comparable? Aging Clin Exp Res. 2015;27(3):309–314. doi: 10.1007/s40520-014-0287-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richardson CA, Glynn NW, Ferrucci LG, Mackey DC. Walking energetics, fatigability, and fatigue in older adults: the study of energy and aging pilot. J Gerontol A, Biol Sci Med Sci. 2015;70(4):487–494. doi: 10.1093/gerona/glu146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ACSM’s Guidelines For Exercise Testing And Prescription. 9th ed. Lippincott Williams & Wilkins; 2013. [Google Scholar]
- 7.Yang C-M, Wu C-H. The situational fatigue scale: a different approach to measuring fatigue. Qual Life Res. 2005;14(5):1357–1362. doi: 10.1007/s11136-004-5680-0 [DOI] [PubMed] [Google Scholar]
- 8.Alexander NB, Taffet GE, Horne FM, et al. Bedside-to-Bench conference: research agenda for idiopathic fatigue and aging. J Am Geriatr Soc. 2010;58(5):967–975. doi: 10.1111/j.1532-5415.2010.02811.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schrack JA, Simonsick EM, Glynn NW. Fatigability: A prognostic indicator of phenotypic aging. J Gerontol A, Biol Sci Med Sci. 2020;75(9):e63–e66. doi: 10.1093/gerona/glaa185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glynn NW, Santanasto AJ, Simonsick EM, et al. The Pittsburgh Fatigability Scale for older adults: development and validation. J Am Geriatr Soc. 2015;63(1):130–135. doi: 10.1111/jgs.13191 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. Final model for estimating cardiorespiratory fitness (VO2peak, mL/kg/min) using a usual-paced 400m long distance corridor walk: Study of Energy and Aging – Pilot (N=34)


