Abstract
Background:
Social isolation and loneliness are critical to the health of older adults, but they have not been well-described at the end of life.
Objectives:
To determine the prevalence and correlates of social isolation and loneliness among older adults in the last years of life.
Design:
Nationally-representative, cross-sectional survey.
Setting:
Health and Retirement Study, 2006–2016 data.
Participants:
Adults age >50 interviewed once in the last four years of life (n=3,613).
Measurements:
We defined social isolation using a 15-item scale measuring household contacts, social network interaction, and community engagement, and frequent loneliness using the 3-item UCLA Loneliness Scale. We used multivariable logistic regression to determine their adjusted prevalence by time prior-to-death and by subgroups of interest.
Results:
Approximately 19% experienced social isolation, 18% loneliness, and 5% both in the last four years of life (correlation=0.11). The adjusted prevalence of social isolation was higher for individuals nearer to death (4 years: 18% vs 0–3 months: 27%, p=0.05) and there was no significant change in loneliness (4 years: 19% vs 0–3 months: 23%, p=0.13). Risk factors for both isolation and loneliness included (p<0.01): low net-worth (Isolation: 34% vs 14%; Loneliness: 29% vs 13%), hearing impairment (Isolation: 26% vs 20%; Loneliness: 26% vs 17%), and difficulty preparing meals (Isolation: 27% vs 19%; Loneliness: 29% vs 15%). Factors associated with loneliness, but not social isolation, included being female, pain, incontinence, and cognitive impairment.
Conclusions:
Social isolation and loneliness are common at the end of life, affecting 1 in 4 older adults, but few experience both. Rates were higher for older adults who were poor and experienced functional or sensory impairments. Results can inform clinical efforts to identify and address end-of-life psychosocial suffering and health policies which prioritize social needs at the end of life.
INTRODUCTION
In the last years of life clinicians have traditionally placed an intense focus on the diagnosis and treatment of disease and physical symptoms. Social well-being may be equally important to individuals and their families. A national survey found that up to 85% of older adults and caregivers prioritized social goals at the end of life, including sharing time with close friends, the presence of family, not dying alone, and being able to help others.1 Older adults who experience social isolation or loneliness, two distinct markers of social well-being, may be less likely to realize these end-of-life goals and are at risk for worsened symptoms and quality of care.2–4 A recent National Academy of Sciences report highlighted the need for clinicians to be aware of and actively address the health effects of social isolation and loneliness.5 Moreover, the 2018 National Consensus Project for Quality Palliative Care included social aspects of care as a core domain for the provision of high quality medical care to patients with serious illness.6 However, little is known regarding the epidemiology of these key markers of social well-being at the end of life.
Older adults may be uniquely vulnerable to experiencing social isolation and loneliness (defined in Figure 1) in the last years of life.3 Older adults may become more isolated due to widowhood, disability, and cognitive impairment. Those living in isolation may struggle at the end of life to access to sources of emotional, financial, and caregiver support to alleviate physical or psychological discomfort.7 Similarly, older adults may be less able to cope with loneliness in the last years of life, as compared with earlier in the lifespan when loneliness can be a transient feeling which motivates individuals to reconnect with relationships or the community.8–11 Left unaddressed, loneliness may cause significant emotional, physical and existential distress.12, 13 In national surveys, social isolation and loneliness have a low correlation (r<0.20), but it is unknown how related these experiences are to one another in the last years of life.14 A higher correlation between these two markers might indicate that an intervention could impact both through similar mechanisms. A low correlation might instead suggest a need for separate interventions to address each social need.
Figure 1.
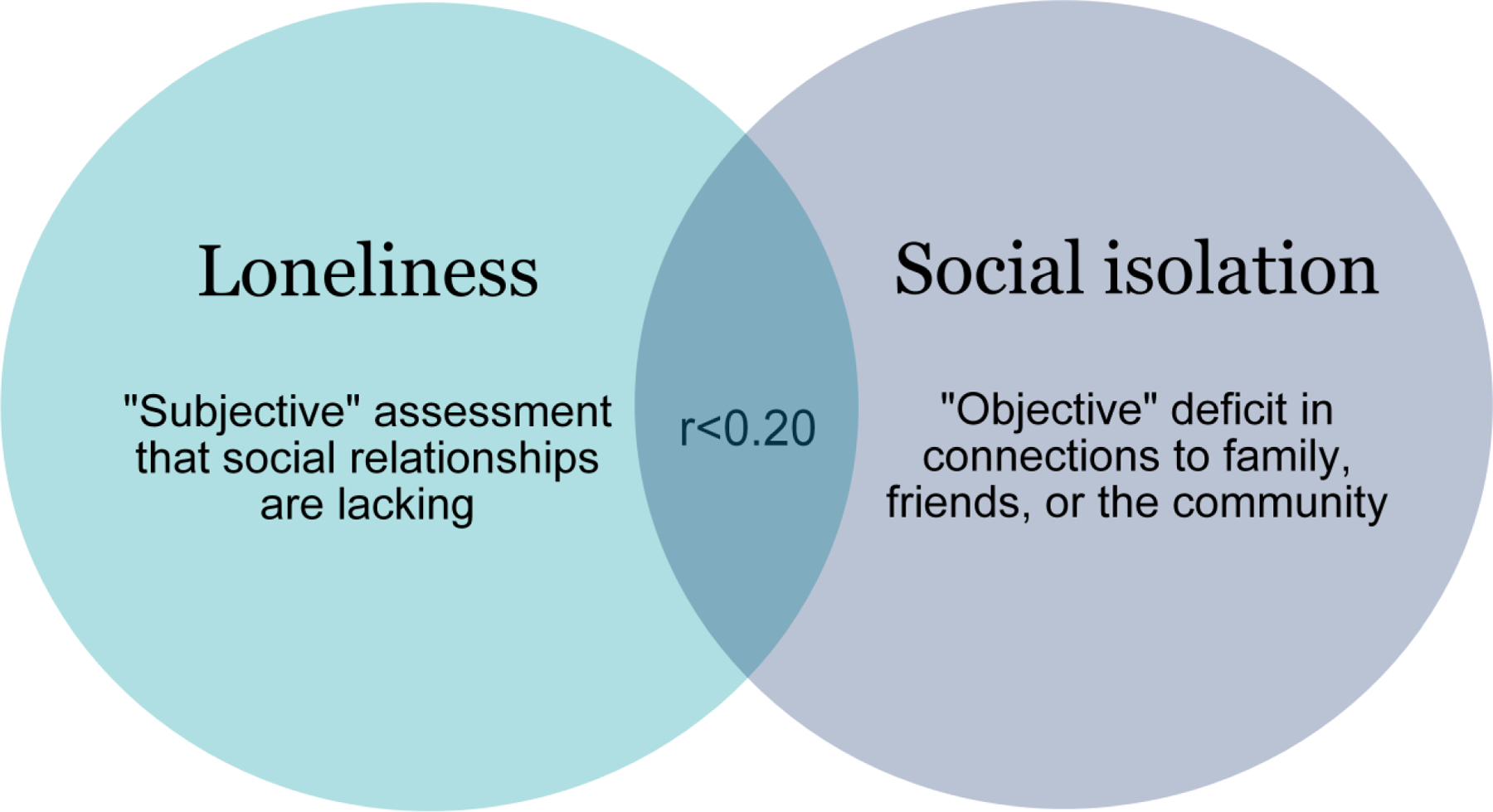
The Interrelationship of Loneliness and Social isolation.
*r<0.20 represents a low correlation between the two social markers which has been reported in prior national studies [3].
A better understanding of the magnitude of isolation and loneliness at the end of life, their relationship to one another, and subgroups at risk can highlight the potential for clinical and social interventions to reduce social suffering, an underappreciated focus of current approaches to medical care at the end of life. In this study, we therefore used a nationally-representative cohort of older adults, the Health and Retirement Study (HRS), to examine participants who responded to survey questions on social isolation and loneliness within four years of death. Our objectives were to determine: 1) the overall prevalence of social isolation and loneliness and their relationship to one another in the last years of life; 2) if the prevalence differs by time prior-to-death; and 3) the prevalence among sociodemographic and clinical subgroups.
METHODS
Study Sample
The HRS collects data on a nationally-representative cohort of adults ≥51 years old who are interviewed biennially until death.15 In 2006, the HRS began administering an extensive Psychosocial Leave-Behind Questionnaire (LBQ) which includes measures of social isolation and loneliness.16 Our study cohort included HRS participants who died by the year 2018 who completed the LBQ within four years of death. Overall, 5,976 primarily community-dwelling HRS participants over age 50 were invited to complete the LBQ in one of the two HRS waves before death, 3,822 (64%) of whom completed the interview. We excluded 209 participants with incomplete responses to the LBQ, resulting in a final sample of 3,613 decedent subjects who completed the LBQ within 4 years of death.
Social Measures
Social Isolation was defined based on three dimensions of social relationships as outlined by Shankar et al. (2011) and prior published social isolation scales,17–21 with cut-offs adapted to assess end-of-life isolation (extensive description in Supplementary Materials and Supplementary Figure 1). Each of the three dimensions was standardized to create a separate subscale ranging from 0–2 points with more points indicating more social connections. First, we measured household and core contacts including: marital status, household size, and having nearby children. Local or in-home contacts are important to the provision of end-of-life support. Second, we measured social network interaction, which assessed the frequency of contact with children, family, or friends through in-person, e-mail, or phone interactions.18 Third, we examined community engagement, including the frequency of participation in religious services, other community groups, or community volunteering.7, 22, 23 Community engagement can contribute to a sense of belongingness in the community or the ability to help others, which can improve quality of life among seriously ill older adults.1, 24 The three subscales were combined to create an overall social connectedness scale which ranged from 0–6 points, with 0–2 points representing social isolation.17
Loneliness was measured using the validated 3-item UCLA Loneliness Scale (Range 0–6 points),25 which includes three questions asking the frequency participants feel they lack companionship, are left out, or are isolated from others (Responses: “Hardly ever or never” (0 points), “Some of the time” (1 points), or “Often” (2 points); Range of 0–6 points). We categorized loneliness in two ways. First, as “any loneliness” if they scored 1+ points on the scale.26 Second, as “frequently lonely” if they scored 4+ points on the scale, requiring a response of “often” to at least one of the three questions.25 We focus primarily on frequent loneliness as this may represent a more significant source of emotional distress in the last years of life.
Time of Death
We used the HRS date-of-death and date-of-interview variables to determine how long prior to death the participant responded to survey questions.27 We focused on the last four years of life since serious illness might affect quality of life and social activities for multiple years prior to the last months or years immediately preceding death. In addition, a larger timeframe increased statistical power for subgroup comparisons.
Sociodemographic, Clinical, and Functional Subgroups
Sociodemographic factors included age, gender, marital status, race/ethnicity, education, and net worth.28, 29 Clinical factors included self-reported chronic conditions (diabetes, heart disease, lung disease, cancer, hypertension, and stroke),7, 30 pain, and recent hospitalizations.8 Functional status measures included vision impairment, hearing impairment, urinary incontinence, ognitive impairment (Cognitive Impairment Not Dementia (CIND) and Dementia),31 difficulty performing six Activities of Daily Living (ADLs) (bathing, dressing, transferring, toileting, eating, walking across a room), difficulty performing five Instrumental Activities of Daily Living (IADLs) (using a phone, managing finances, taking medications, shopping for groceries, and preparing hot meals),32 and difficulty walking one block.
Statistical Analysis
For objective 1, we determined the national prevalence of social isolation and loneliness in the last four years of life, and used logistic regression to describe the adjusted prevalence of loneliness by each dimension of social isolation. In addition, we used Chi-Square tests to compare the prevalence of social isolation and loneliness in our sample of decedents to a sample of non-decedents (n=3,156) who survived 4 years or longer after the HRS interview, matched on age, gender, and race/ethnicity.
For objective 2, we determined the unadjusted prevalence of social isolation and loneliness by time prior-to-death by dividing the sample into 3-month serial cross-sections prior to death. Evidence suggests the time between interview and death is random,8, 9, 33 and that observations at any time point are representative of the underlying sample of older adults at that time point. We then used separate multivariable logistic regression models to determine the prevalence of social isolation, social isolation sub-scales, and loneliness by time prior-to-death, adjusting for age at death, sex, race/ethnicity, and education. We did not adjust for comorbidities or functional status as we expected these factors to lie on the causal pathway between time prior to death and risk for each social factor. For each model, we tested different functional forms for the time covariate, including linear, quadratic, and restricted cubic spline to determine if the prevalence time trend changed at certain points prior to death. Based on comparisons using Wald tests, we present the results of linear models.
For objective 3, we determined the adjusted, model-based probabilities of social isolation and frequent loneliness by sociodemographic and clinical subgroups for the overall sample of decedents. Adjusted models included the following covariates: time before death, age at death, sex, race/ethnicity, education, comorbidities, and ADL impairments. We did not adjust for multiple comparisons as the goal of the analysis was exploratory in nature.34
We anticipated selection effects to occur over the four years prior to death, since respondents are likely to experience more physical or cognitive impairment closer to death, which might limit their participation in HRS interviews. To address this, we used inverse probability weighting, accounting for age, gender, marital status, race/ethnicity, net worth, cognitive status, functional status, and presence of chronic conditions, in all analyses to adjust for the lower response rates among certain subgroups closer to death.35 All analyses accounted for the complex sampling design, differential probability of selection, and differential probability of response to core and LBQ interviews. The analyses were performed using STATA 16.1 and SAS 9.4.36, 37
RESULTS
Demographic and health characteristics of our sample of decedents are summarized in Table 1. Overall, the mean age of our sample was 78 years at death and 50% were female, 11% African American/Black, and 21% had a net worth of <$6,000. Approximately 19% were socially isolated, 18% reported frequent loneliness, and 5% experienced both (r=0.11). The adjusted association between each social isolation item and frequent loneliness is summarized in Supplementary Table 1. Frequent loneliness occurred at higher rates (p<0.001) among those who were unmarried, lived alone, had low interaction with children or friends, and had less engagement with volunteer work, religious services, or community groups. In comparing our sample of decedents to a matched sample of those surviving longer than 4 years after the HRS interview, decedents were more likely to report social isolation (19% vs. 10%, p<0.001) and loneliness (18% vs. 11%, p<0.001).
Table 1.
Select characteristics in 2006–2016 HRS (N=3,613)
| Characteristics | N | % | |
|---|---|---|---|
| Sociodemographics | |||
| Age at death | 50–64 | 357 | 13.9% |
| 65–74 | 754 | 22.0% | |
| 75–84 | 1260 | 27.9% | |
| 85+ | 1242 | 36.1% | |
| Gender | Female | 1829 | 50.4% |
| Marital Status | Married/Partnered | 1833 | 47.0% |
| Race/Ethnicity | White/Caucasian | 2849 | 81.0% |
| Black/AA | 485 | 11.1% | |
| Hispanic | 221 | 6.1% | |
| Others | 58 | 1.8% | |
| Education | <HS or GED | 961 | 27.2% |
| Net Worth1 | <6,000 | 681 | 21.1% |
| 6,000-<81,000 | 807 | 22.7% | |
| 81,000-<239,000 | 856 | 22.8% | |
| >=239,000 | 1269 | 33.4% | |
| Health status | |||
| Cognition2 | Normal | 2133 | 55.9% |
| CIND | 1034 | 26.9% | |
| Dementia | 446 | 17.3% | |
| Comorbidities | Any condition | 2934 | 80.2% |
| Cancer | 1069 | 29.0% | |
| Diabetes mellitus | 1148 | 31.5% | |
| Lung disease | 840 | 23.3% | |
| Stroke | 686 | 19.7% | |
| Heart Disease | 1719 | 46.6% | |
| ADL Dependence | Any ADL dependence | 783 | 25.0% |
| Walking | 296 | 10.6% | |
| Dressing | 483 | 16.3% | |
| Eating | 187 | 7.3% | |
| Bathing | 500 | 17.2% | |
| Toilet | 158 | 6.3% | |
| In/Out of bed | 222 | 8.8% | |
| IADL Difficulty | Any IADL difficulty | 1612 | 48.9% |
| Cooking | 888 | 28.5% | |
| Shopping | 1091 | 35.0% | |
| Medications | 292 | 11.7% | |
| Telephone | 429 | 15.9% | |
| Finances | 743 | 25.5% | |
| Difficulty Walking a block | 1452 | 42.5% | |
| Sensory Impairment | Vision impairment | 1244 | 36.6% |
| Hearing impairment | 1187 | 33.8% | |
| Symptoms | Incontinence | 1169 | 34.3% |
| Pain | 1195 | 34.5% | |
| Hospitalizations | In last 2 years | 1759 | 48.6% |
| Loneliness 3 | Not lonely (0 points) | 1282 | 33.7% |
| Occasionally Lonely (1–3) | 1758 | 48.5% | |
| Frequently Lonely (4–6 points) | 573 | 17.8% | |
| Social Isolation and Subscales | |||
| Household and core contacts4 | None | 523 | 17.5% |
| Low | 810 | 24.5% | |
| Moderate/high participation | 2239 | 58.0% | |
| Community engagement5 | None | 956 | 29.7% |
| Low | 504 | 14.6% | |
| Moderate/high participation | 2037 | 55.7% | |
| Social Network Interaction6 | None | 649 | 20.9% |
| Low | 1186 | 36.4% | |
| Moderate/high participation | 1513 | 42.7% | |
| Overall Social Isolation7 | Not socially isolated | 2725 | 81.1% |
| Socially Isolated | 529 | 18.9% |
Abbreviations: CIND – Cognitive Impairment Not Dementia;
Net Worth was calculated as sum of all assets minus the sum of all debts.
Cognitive Impairment was defined using the Langa-Weir methods;
Loneliness was defined using the UCLA 3-item Loneliness Scale, “Any loneliness” reflects 1–6 points;
Household contact items included marital status, household size, and presence of children <10 miles away;
Community engagement items included frequency of volunteering, participating in community groups, and religious services;
Social Network Interaction items included the frequency of interaction with children, family, or friends through in-person, e-mail, or phone;
Overall Social Isolation was defined by combining the Household, Social Network Interaction, and Community Engagement subscales to create a 0–6 point scale with 0–2 points categorized as socially isolated.
We next examined the differences in prevalence for social isolation and loneliness by time prior-to-death. The adjusted population prevalence of social isolation was higher for individuals closer to death, increasing gradually (18% at 4 years to 27% at 0–3 months prior to death, p=0.050) (Figure 2A). As expected, this relationship was no longer significant after adjusting for ADL impairment and comorbidities. Examining social isolation subscales revealed a higher prevalence of low social network interaction (4 years: 57% versus 0–3 months: 68%, p=0.003) and low community engagement (4 years: 42% versus 0–3 months: 53%, p=0.01) by time prior to death, whereas household contacts were consistent over time (4 years: 45% versus 0–3 months: 47%, p=0.6) (Figure 2B and Supplementary Table 2). The prevalence of “frequent loneliness” (18% at 4 years to 23% at 0–3 months prior to death, p=0.13) or “any loneliness” (66% at 4 years to 72% at 0–3 months prior to death, p=0.09) did not differ significantly by time prior to death (Figure 3 and Supplementary Table 2).
Figure 2.
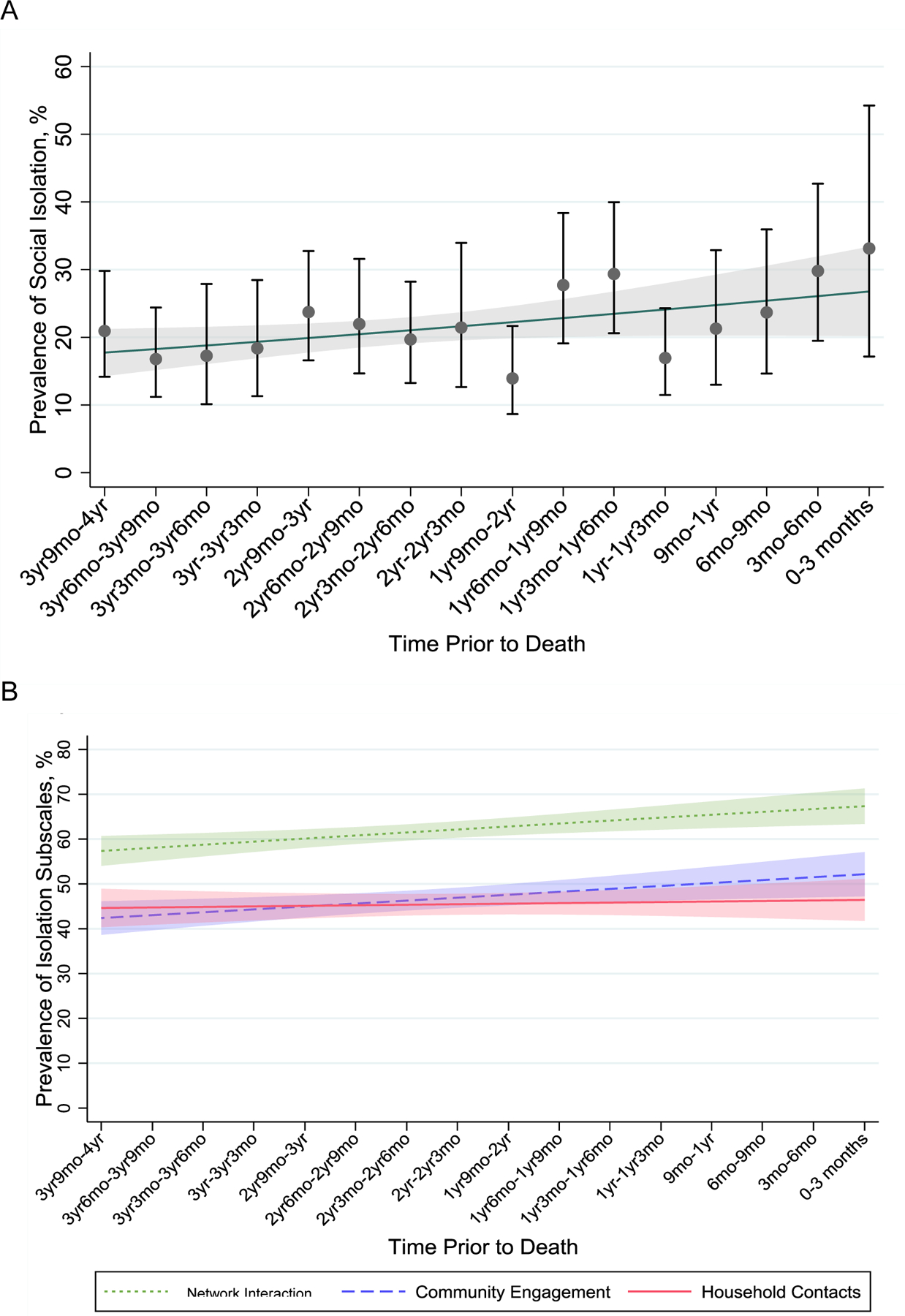
The Prevalence of (A) Social Isolation and (B) Social Isolation Subscales by Time Prior to Death.
Points in (A) represent the mean weighted prevalence of social isolation in 3 month time intervals prior to death. Bars represent 95% confidence intervals. In (A) and (B) lines represents social.
Figure 3.
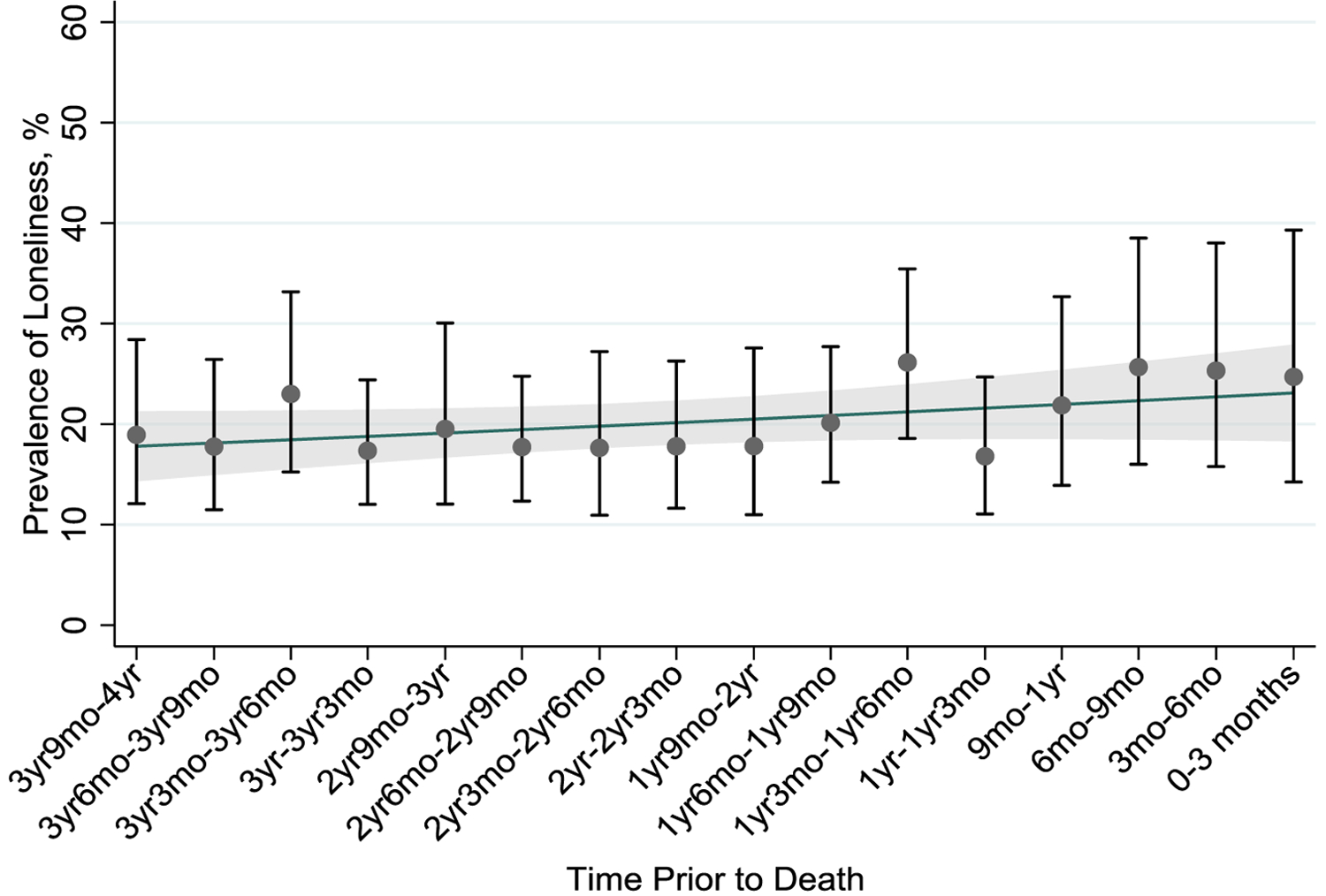
The Prevalence of Frequent Loneliness by Time Prior to Death.
Points represent the mean weighted prevalence of frequent loneliness in 3 month time intervals prior to death. Bars represent 95% confidence intervals. The line represents loneliness modeled by time prior to death, adjusted for age at death, sex, race/ethnicity, and education. Gray shading above and below the line represents modeled 95% confidence intervals.
We determined sociodemographic and clinical risk factors significantly associated with social isolation and loneliness in the full sample of decedents (p-value of <0.001 unless otherwise stated) (Figure 4 and Supplementary Table 3). Low net-worth was associated with isolation (<$6000: 34% vs >$239,000: 14%) and loneliness (<$6000: 29% vs >$239,000: 13%). Functional or sensory impairments associated with isolation and frequent loneliness included difficulty with preparing hot meals (Isolation: 27% vs 19%; Loneliness: 29% vs 15%), walking one block (Isolation: 25% 18%, p=0.04; Loneliness: 26% vs 15%), and hearing impairment (Isolation: 26% vs 20%, p=0.02; Loneliness: 26% vs 17%).
Figure 4.
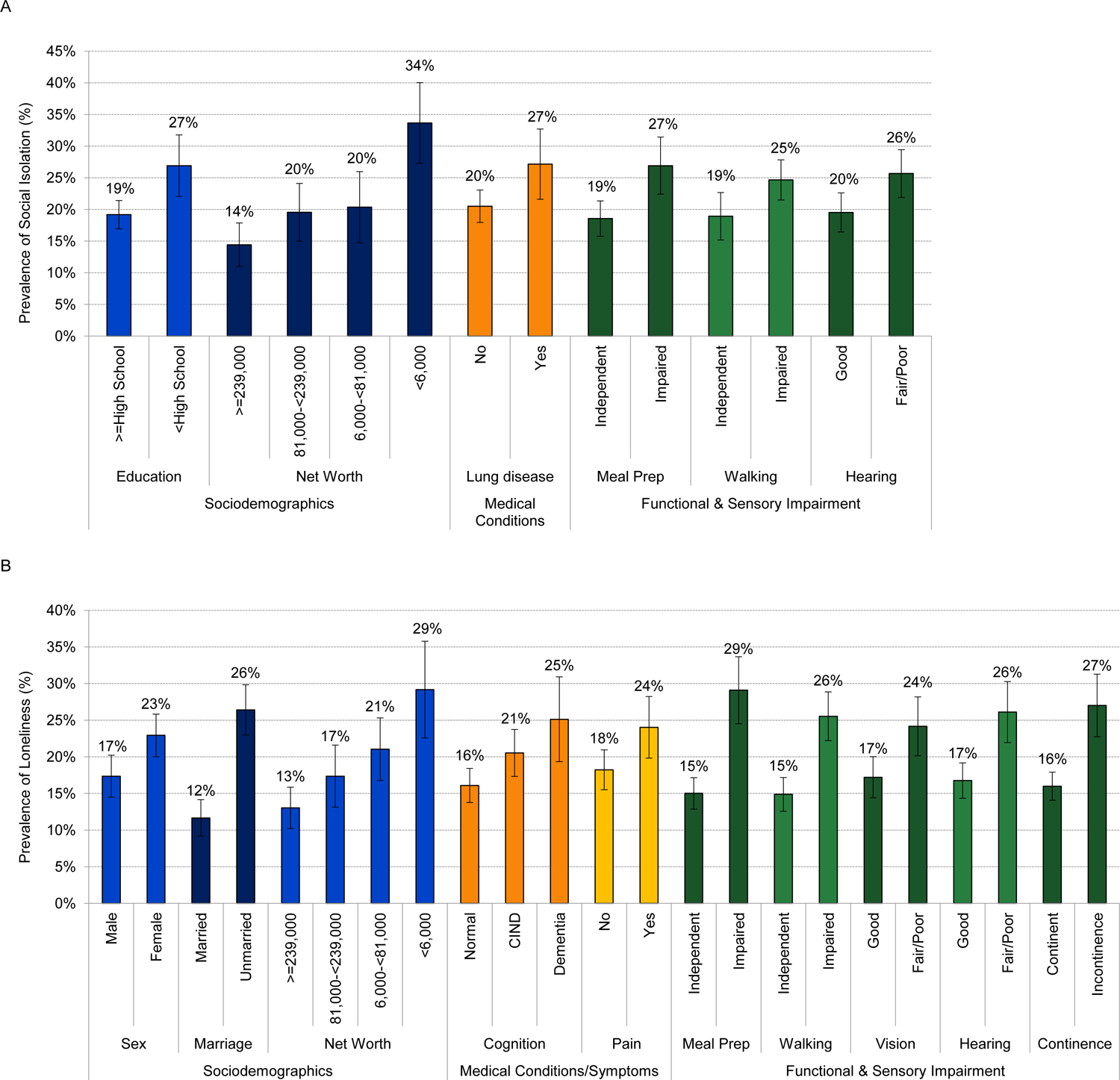
The Adjusted Prevalence of (A) Social Isolation and (B) Loneliness by Key Sociodemographic, Medical, and Functional Covariates.
Rates represent the model-based probabilities adjusted for age at death, sex, race/ethnicity, education, comorbidities, and number of ADL impairments. Error bars represent the 95% confidence intervals. All displayed comparisons reached a significance threshold of p<0.05 or less. Full model results are provided in Supplementary Materials.
Notably, several factors were associated with feelings of frequent loneliness, but not isolation, including sex (female: 23% vs male: 17%, p=0.004), current pain (24% vs 18%, p=0.02), vision impairment (24% vs 17%, p=0.006), and incontinence (27% vs 16%, p<0.001). With higher levels of cognitive impairment, individuals had frequent loneliness (Normal: 16%, CIND: 21%, Dementia: 25%, p=0.01), whereas this was not significant for social isolation (Normal: 19%, CIND: 22%, Dementia: 25%, p=0.07). Individuals with lung disease had higher rates of social isolation (27% vs 20%, p=0.03), but no significant difference in loneliness.
DISCUSSION
In a nationally-representative sample of older adults in the last four years of life, we found high rates of social isolation and loneliness, two key markers of social well-being, across the last four years of life. The prevalence of social isolation had a small, but significant increase to over 1 in 4 older adults in the last months of life, suggesting that isolation may intensify at the end of life as individuals experience worsening function or health as death approaches.9, 38 Nearly 1 in 5 older adults in our sample reported frequent loneliness, and over two in three reported any loneliness, substantially higher than the prevalence in the general US population of older adults.26 Loneliness is therefore a substantial, and potentially unrecognized, source of emotional distress in the last years of life. Notably, social isolation and loneliness were generally non-overlapping social experiences, with only 5% experiencing both. Study findings highlight the potential for clinicians to improve quality of life of older adults in their last years of life by asking about social needs and taking initial steps to improve social well-being.
Even with a relatively strict definition of social isolation, over 1 in 4 older adults were isolated in the last 3 months of life, substantially higher than the prevalence among matched non-decedents in HRS and rates among the general population of older adults.39 We hypothesize that those nearer to death may be selectively pruning their social relationships to focus on their closest relationships (socioemotional selectivity theory),40 or might experience co-occurring life events which lead to social losses (e.g. widowhood or death of friends). In addition, declines in functional status or health may contribute to social isolation, since the association between isolation and time prior-to-death was no longer significant after adjusting for ADL impairment and comorbidities. While some reduction in social activity is likely normal, the high prevalence of social isolation, as defined in our study, suggests older adults are commonly facing challenges associated with isolation at the end of life. Examples of such challenges might include a lack of access to end-of-life emotional support (e.g. for new onset anxiety or depression),4 instrumental support (e.g. transportation to medical appointments), caregiver support (e.g. to access services like home hospice), or a health care proxy.41 Future research might examine if socially isolated individuals in turn have higher symptom burden, lower hospice use at the end of life, and more ED or ICU visits.
Our study similarly suggests that loneliness may be more common in the last years of life compared to earlier in the lifespan. Prior national studies found that approximately 35–40% of older adults experienced “any” feelings of loneliness compared to 70% in our study,26 and 11% of non-decedents in HRS experienced “frequent” loneliness as compared with 18% in the last four years of life. Yet, the prevalence of loneliness did not increase for individuals closer to death when we examined separate time-intervals in the last 4 years of life. This is consistent with prior literature finding depression, anxiety, and other psychological states may not change substantially based on proximity to death.42 We hypothesize that individuals may change or downgrade their subjective perception of what constitutes an adequate level of social connectedness as they near death.43 In addition, end-of-life loneliness may occur through pathways unrelated to the frequency of social network interaction, including from existential distress, anticipatory grief, or a feeling of disconnection from one’s community;12, 44 these dimensions of loneliness may not have been fully captured by the 3-item UCLA scale. Further research including a qualitative component might examine how perceptions of loneliness differ among seriously ill older adults at high risk of death.
The high overall prevalence of social isolation and loneliness suggests clinicians should identify and screen for each marker as a first step to addressing psychosocial suffering at the end of life. Asking is particularly important as patients may not raise the issue on their own due to the stigma of self-identifying as lonely or isolated.3 Notably, each social condition should be identified separately as it is uncommon for individuals to experience both loneliness and isolation. Use of the 3-item UCLA loneliness scale or the Berkman-Syme social isolation scale can help clinicians track changes over time and be aware of clinically meaningful thresholds.3, 25
Once identified, clinicians may be unsure how to take steps to appropriately intervene, since evidence-based interventions specific to seriously ill older adults are lacking.5 We therefore suggest an individualized approach to addressing loneliness, social isolation, or both. For loneliness, clinical strategies can start by acknowledging the emotional distress patients experience from loneliness, asking whether the patient wishes for more social contact, and connecting patients with programs to enhance social connections and support. Psychological interventions to address end-of-life loneliness might include dignity therapy by chaplaincy,45 art therapy (e.g. the “UnLonely Project”),46 and therapies which address maladaptive cognition. Identifying loneliness may inform strategies to address associated end-of-life symptoms like pain,4 psychological distress,47 and prior life experiences of trauma, which can be amplified by the distress of loneliness.48 Notably, results suggested cognitive impairment was a significant risk factor for loneliness, possibly due to difficulty maintaining social networks and limited emotional coping.22 Further research is needed on how interventions might be adapted to the unique needs of older adults with cognitive impairment.
In contrast to loneliness, strategies to address end-of-life social isolation may center more on mobilizing external clinical or community support services and early advance care planning.41 Concerningly, most hospice agencies will not accept isolated patients who do not have a caregiver.49 Clinicians should work with social workers to identify alternatives such as so-called “bridge” programs that bill the Medicare Home Health benefit, residential hospice facilities, and for Veterans, a hospice contract with a skilled nursing facility.
Our results are suggestive of modifiable risk factors common to both end-of-life social isolation and loneliness which can be tested in future interventions. Difficulty preparing hot meals, for example, was strongly associated with both isolation and loneliness. Connecting patients with community centers or food programs which allow for shared experiences through cooking, communal dining, and the ability to eat favorite foods may therefore be helpful in building social connections and well-being.50, 51 Functional and sensory impairments such as difficulty walking, difficulty shopping, and hearing impairment were strongly associated with social isolation and loneliness and might be addressed by providing assistive devices. Finally, low net-worth, the strongest risk factor in our study for both isolation and loneliness, might be considered when making referrals and helping patients qualify for community programs.
When possible, it may be better to pursue upstream interventions (in the years rather than months prior to death) to maintain or enhance relationships and reduce the risk of end-of-life isolation and loneliness. In our study and others,26 social isolation and loneliness were highly prevalent in the years prior to death, long before the last months of life. Preventative interventions might start with primary care clinicians encouraging the maintenance of healthy social behaviors during annual or routine visits, or early referrals to community-based programs. Overall, clinical, policy, and public health experts should advocate for prioritizing social needs just as traditional medical needs are prioritized; the United Kingdom’s national Campaign to End Loneliness serves as a useful model for how an integrated national effort can meet this complex challenge.52
Our study has limitations. First, we anticipate a selection bias where respondents experiencing physical or cognitive impairment may be less likely to participate in HRS in interviews closer to death. We used inverse probability weighting, which might reasonably address this limitation.35 Nevertheless, results are primarily generalizable to older adults able to respond to survey questions at the end of life. Severely impaired individuals less likely to participate in the survey may experience more loneliness or social isolation, suggesting our prevalence estimates are conservative. Second, the study is cross-sectional with each interview occurring at different time points prior to death and roughly representative of the general population prevalence at that point before death. Longitudinal assessments at frequent time intervals are needed to fully understand the timing and risk factors for changes in social isolation and loneliness at the end of life. Third, there is a lack of consensus on how to best measure social isolation among seriously ill older adults. We defined social isolation based on prior measures and used strict thresholds more likely be associated with detrimental end-of-life clinical consequences (Supplementary Materials).21 Fourth, the HRS did not administer social measures to individuals living in nursing facilities or individuals with severe enough cognitive impairment to require proxy interviews,53 populations for whom the impacts of social isolation and loneliness may differ from the community-dwelling population studied here.
In conclusion, we found that social isolation and loneliness are common in the last years of life and identified sociodemographic and clinical subgroups at risk. Identifying and addressing these social needs in health care assessments represent an important clinical opportunity to reduce suffering in the last years of life.
Supplementary Material
Key points:
In a nationally-representative sample of older adults interviewed in their last 4 years of life (N=3,613), social isolation and loneliness were common at the end of life affecting 1 in 4 older adults, although few experience both.
Why does this matter?
Results can inform clinical and policy efforts to reduce psychosocial suffering in the last years of life.
ACKNOWLEDGMENTS
Author contributions: Conception and design: AK, IC, LW, KC, CP, JB, LH, WD, AS; Acquisition of the data: AK, IC, KC, AS; Analysis and interpretation: AK, IC, LW, KC, CP, JB, LH, WD, AS; Drafting and revising manuscript: AK, IC, LW, KC, CP, JB, LH, WD, AS; Approval of final manuscript: AK, IC, LW, KC, CP, JB, LH, WD, AS.
Funding:
Dr. Ashwin Kotwal’s effort on this project was supported by grants from the National Institute on Aging (K23AG065438; R03AG064323), the NIA Claude D. Pepper Older Americans Independence Center (P30AG044281), the National Palliative Care Research Center Kornfield Scholar’s Award, and the Hellman Foundation Award for Early-Career Faculty.
Footnotes
Conflicts of Interest: All authors report no conflicts of interest.
Sponsor’s Role: The sponsor had no role in the design, methods, data collection, analysis, or preparation of the paper.
SUPPLEMENTARY MATERIALS
- Supplementary Materials. Social Isolation Scale Adaptation
- Supplementary Figure 1. Social Isolation Scale.
- Supplementary Table 1. Association of Social Isolation and Social Isolation Items with Frequent Loneliness in the Last Years of Life
- Supplementary Table 2. Prevalence of Social Isolation, Social Isolation Subscales, and Loneliness by Time Prior to Death
- Supplementary Table 3. Adjusted Prevalence of Loneliness and Social Isolation During the Last 4 Years of Life Across Subgroups
REFERENCES
- [1].Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. Jama. 2000;284: 2476–2482. [DOI] [PubMed] [Google Scholar]
- [2].Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspectives on Psychological Science. 2015;10: 227–237. [DOI] [PubMed] [Google Scholar]
- [3].Perissinotto C, Holt-Lunstad J, Periyakoil VS, Covinsky K. A practical approach to assessing and mitigating loneliness and isolation in older adults. Journal of the American Geriatrics Society. 2019;67: 657–662. [DOI] [PubMed] [Google Scholar]
- [4].Abedini NC, Choi H, Wei MY, Langa KM, Chopra V. The Relationship of Loneliness to End-of-Life Experience in Older Americans: A Cohort Study. Journal of the American Geriatrics Society. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].NAS. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. In: Sciences NAo, ed., 2020. [PubMed] [Google Scholar]
- [6].Ferrell BR, Twaddle ML, Melnick A, Meier DE. National consensus project clinical practice guidelines for quality palliative care guidelines. Journal of palliative medicine. 2018;21: 1684–1689. [DOI] [PubMed] [Google Scholar]
- [7].Waite LJ. Social Well-Being and Health in the Older Population: Moving beyond Social Relationships. Future Directions for the Demography of Aging: Proceedings of a Workshop: National Academies Press, 2018. [PubMed] [Google Scholar]
- [8].Smith AK, Cenzer IS, Knight SJ, et al. The epidemiology of pain during the last 2 years of life. Annals of internal medicine. 2010;153: 563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Smith AK, Walter LC, Miao Y, Boscardin WJ, Covinsky KE. Disability during the last two years of life. JAMA internal medicine. 2013;173: 1506–1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Thoits PA, Hewitt LN. Volunteer work and well-being. Journal of health and social behavior. 2001: 115–131. [PubMed] [Google Scholar]
- [11].Cacioppo JT, Hawkley LC, Crawford LE, et al. Loneliness and health: Potential mechanisms. Psychosomatic medicine. 2002;64: 407–417. [DOI] [PubMed] [Google Scholar]
- [12].Ettema EJ, Derksen LD, van Leeuwen E. Existential loneliness and end-of-life care: A systematic review. Theoretical medicine and bioethics. 2010;31: 141–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sjöberg M, Beck I, Rasmussen BH, Edberg A-K. Being disconnected from life: meanings of existential loneliness as narrated by frail older people. Aging & mental health. 2017: 1–8. [DOI] [PubMed] [Google Scholar]
- [14].Cornwell EY, Waite LJ. Measuring social isolation among older adults using multiple indicators from the NSHAP study. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009;64: i38–i46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Health and Retirement Study. Volume 2018. Ann Arbor, MI: University of Michigan, pp. NIA U01AG009740. [Google Scholar]
- [16].Smith J, Fisher G, Ryan L, Clark P, House J, Weir D. Psychosocial and Lifestyle Questionnaire 2006–2010: Documentation report. Ann Arbor: Health and Retirement Study, University of Michigan, 2013. [Google Scholar]
- [17].Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proceedings of the National Academy of Sciences. 2013;110: 5797–5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Shaw JG, Farid M, Noel-Miller C, et al. Social isolation and Medicare spending: Among older adults, objective isolation increases expenditures while loneliness does not. Journal of aging and health. 2017;29: 1119–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Cornwell EY, Waite LJ. Measuring social isolation among older adults using multiple indicators from the NSHAP study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009;64: i38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Valtorta NK, Kanaan M, Gilbody S, Hanratty B. Loneliness, social isolation and social relationships: what are we measuring? A novel framework for classifying and comparing tools. BMJ open. 2016;6: e010799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Shankar A, McMunn A, Banks J, Steptoe A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychology. 2011;30: 377. [DOI] [PubMed] [Google Scholar]
- [22].Kotwal AA, Kim J, Waite L, Dale W. Social function and cognitive status: Results from a US nationally representative survey of older adults. Journal of general internal medicine. 2016;31: 854–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Idler E, Blevins J, Kiser M, Hogue C. Religion, a social determinant of mortality? A 10-year follow-up of the Health and Retirement Study. PloS one. 2017;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Koenig HG. A commentary: The role of religion and spirituality at the end of life. The Gerontologist. 2002;42: 20–23. [DOI] [PubMed] [Google Scholar]
- [25].Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on aging. 2004;26: 655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Perissinotto CM, Cenzer IS, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Archives of internal medicine. 2012;172: 1078–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Brown DC, Lariscy JT, Kalousová L. Comparability of mortality estimates from social surveys and vital statistics data in the United States. Population research and policy review. 2019;38: 371–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kim J, Waite L. Family Structure and Financial Well-Being:Evidence from the Great Recession. In: Couch K, Daly M, Zissimopolous J, eds. Unexpected Lifecycle Events and Economic Security: The Roles of Job Loss, Disability, and Changing Family Structure: Stanford University Press, 2013. [Google Scholar]
- [29].Smith JP. Wealth inequality among older Americans. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1997;52: 74–81. [DOI] [PubMed] [Google Scholar]
- [30].McClintock MK, Dale W, Laumann EO, Waite L. Empirical redefinition of comprehensive health and well-being in the older adults of the United States. Proceedings of the National Academy of Sciences. 2016;113: E3071–E3080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Langa KM, Weir DR, Kabeto M, Sonnega A. Langa-Weir Classification of Cognitive Function (1995 Onward). University of Michigan, 2018. [Google Scholar]
- [32].Katz S Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. Journal of the American Geriatrics Society. 1983;31: 721–727. [DOI] [PubMed] [Google Scholar]
- [33].Kozlov E, Dong X, Kelley AS, Ankuda CK. The Epidemiology of Depressive Symptoms in the Last Year of Life. Journal of the American Geriatrics Society. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Goodman SN. Multiple comparisons, explained. American journal of epidemiology. 1998;147: 807–812. [DOI] [PubMed] [Google Scholar]
- [35].Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Statistical methods in medical research. 2013;22: 278–295. [DOI] [PubMed] [Google Scholar]
- [36].StataCorp. Stata Statistical Software: Release 16. College Station, TX: StataCorp LP, 2019. [Google Scholar]
- [37].SAS. SAS/ACCESS® 9.4 Interface to ADABAS. Cary, NC: SAS Institute Inc, 2013. [Google Scholar]
- [38].Gill TM, Gahbauer EA, Han L, Allore HG. Trajectories of disability in the last year of life. New England Journal of Medicine. 2010;362: 1173–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Cudjoe TK, Roth DL, Szanton SL, Wolff JL, Boyd CM, Thorpe RJ Jr. The epidemiology of social isolation: National health and aging trends study. The Journals of Gerontology: Series B. 2020;75: 107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Carstensen LL. Social and emotional patterns in adulthood: support for socioemotional selectivity theory. Psychology and aging. 1992;7: 331. [DOI] [PubMed] [Google Scholar]
- [41].Cudjoe TK, Boyd CM, Wolff JL, Roth DL. Advance Care Planning: Social Isolation Matters. Journal of the American Geriatrics Society. 2020;68: 841–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Lichtenthal WG, Nilsson M, Zhang B, et al. Do rates of mental disorders and existential distress among advanced stage cancer patients increase as death approaches? Psycho-Oncology: Journal of the Psychological, Social and Behavioral Dimensions of Cancer. 2009;18: 50–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Shiovitz-Ezra S, Shemesh J, McDonnell M. Pathways from ageism to loneliness. Contemporary perspectives on ageism: Springer, 2018, pp. 131–147. [Google Scholar]
- [44].Levy LH. Anticipatory grief: Its measurement and proposed reconceptualization. The Hospice Journal. 1991;7: 1–28. [DOI] [PubMed] [Google Scholar]
- [45].Martínez M, Arantzamendi M, Belar A, et al. ‘Dignity therapy’, a promising intervention in palliative care: A comprehensive systematic literature review. Palliative medicine. 2017;31: 492–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Healing FfA. The UnLonely Project. 2021.
- [47].Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychology and aging. 2006;21: 140. [DOI] [PubMed] [Google Scholar]
- [48].Palgi Y, Shrira A, Ben-Ezra M, Shiovitz-Ezra S, Ayalon L. Self-and other-oriented potential lifetime traumatic events as predictors of loneliness in the second half of life. Aging & mental health. 2012;16: 423–430. [DOI] [PubMed] [Google Scholar]
- [49].Stajduhar K, Mollison A, Giesbrecht M, et al. “Just too busy living in the moment and surviving”: barriers to accessing health care for structurally vulnerable populations at end-of-life. BMC palliative care. 2019;18: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Kirk AB, Waldrop DP, Rittner BA. More than a meal: The relationship between social support and quality of life in daytime meal program participants. Journal of Gerontological Social Work. 2001;35: 3–20. [Google Scholar]
- [51].Locher JL, Burgio KL, Yoels WC, Ritchie CS. The social significance of food and eating in the lives of older recipients of meals on wheels. Journal of Nutrition for the Elderly. 1998;17: 15–33. [Google Scholar]
- [52].Goodman A, Symons M. Evidence-based campaigning on loneliness in older age: an update from the Campaign to End Loneliness. Working with Older People. 2013. [Google Scholar]
- [53].Staff H Proxy Selection in the Health and Retirement Study. Ann Arbor, MI: Survey Research Center, Institute for Social Research, University of Michigan, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


