Abstract
It is well known that human crystalline lens shape, dimensions and optical properties change throughout life and influence whole eye refraction. However, it is not clear if lens properties are associated with other ocular parameters. The purpose of the present study was to investigate the relationship of corneal and external globe dimensions with adult lens diameter (LD), lens thickness (LT) and lens power (LP) in order to determine if external factors influence lens properties. Postmortem human eyes (n = 66, age = 20-78 years) were obtained from the Ramayamma International Eye Bank, Hyderabad, India. Globe antero-posterior length (GAPL) and mean (average of horizontal and vertical) diameters of cornea (MCD) and globe (MGD) were measured using digital calipers. Eyes were dissected to produce ocular structures that contain the lens maintained in its accommodating framework, including intact zonules, ciliary body and sections of sclera. Specimens were mounted in a mechanical lens stretching system. LD, LT and LP were measured using high magnification retro-illumination photography, slit illumination photography and Scheiner principle-based optical system respectively in the unstretched (accommodated) state. Relationships between external globe and corneal dimensions and LD, LT or LP were assessed by multiple regression analysis. Age (0.012 ± 0.003 mm/year; p<0.001) and GAPL (0.185 ± 0.045 mm/mm; p<0.001) were significant (p<0.0001) predictors of LD. After adjusting for age-related increases, LD appears to be positively correlated with GAPL. Age (0.010 ± 0.004 mm/year; p = 0. 009) and GAPL (−0.143 ± 0.060 mm/mm; p = 0.02) were significant (p = 0.001) predictors of LT. After adjusting for the age-related increase, LT appears to be negatively correlated with GAPL. Only age was a significant predictor of LP (−0.26 ± 0.04 D/year; p<0.001). The results suggest that, apart from aging, lens diameter and thickness are dependent on the anteroposterior length of the eye globe. Lens power is not influenced by globe dimensions.
Keywords: cornea, crystalline lens, diameter, globe, length, multiple regression, power, thickness
1. Introduction
Unlike other ocular structures, the human crystalline lens continuously grows throughout life (Augusteyn, 2010; Mohamed and Augusteyn, 2018; Mohamed et al., 2012). During this time, it is subject to a variety of stresses, both external and internal, which may alter its structure and function. A thorough understanding of the factors affecting lens growth is necessary for understanding the emmetropization process and for the effective treatment and management of age-related vision changes. It could also be of value, for example, to ophthalmologists wanting to predict the correct size of a capsular tension ring prior to cataract surgery (Dong and Joo, 2001; Khng and Osher, 2008; Lim et al., 1998). Previous in vitro studies on lens weights, geometrical shape and size or functional properties such as refractive power, spherical aberrations and stiffness have provided some insights (Augusteyn et al., 2011; Heys et al., 2004). In particular, lens diameter (LD) and adult lens thickness (LT) have been shown to increase with age as evaluated in vitro by techniques such as high magnification photography, optical coherence tomography and shadow photogrammetry (Augusteyn et al., 2011; Manns et al., 2007; Martinez-Enriquez et al., 2020; Mohamed et al., 2020; Urs et al., 2009; Urs et al., 2010). However, it is not clear if factors other than age contribute. Similarly, lens power (LP) has been shown to decrease with age in vitro and it is not known if it is affected by other factors (Borja et al., 2008).
There is a need for studies to understand the relationship between lens properties and those of other ocular structures. A few studies in the past have evaluated the relationship between various ocular parameters and LD in cadaveric eyes. Some found a correlation between corneal diameter and LD, while others yielded contradictory results, possibly due to either a small sample size or the low precision of instruments used for the measurements (Dong and Joo, 2001; Khng and Osher, 2008; Lim et al., 1998). Although in vivo studies have shown a relationship between eye axial length and LP (Garner et al., 1992; He et al., 2017), LP measured in vivo is under the influence of surrounding optical media and the state of eye accommodation. The purpose of the present study was to investigate the relationship of corneal and external globe dimensions with adult LD, LT and LP in order to understand if external factors influence lens size and power.
2. Material and methods
Human donor eye globes were collected from the Ramayamma International Eye Bank, L V Prasad Eye Institute, Hyderabad, India. The study protocol was approved by the Institutional Ethics Committee. Consent to enucleate eyes for the purpose of transplantation, therapy, medical research, or education was obtained by the eye bank in accordance with its practices and procedures. All tissues were obtained and used in compliance with the guidelines of the Declaration of Helsinki.
Measurements were made on 66 post-mortem eyes from 66 human donors. The unique eye bank identification number for each tissue was noted along with details such as donor age, gender, time and cause of death, time of enucleation and time of experimental usage. Median donor age was 40 years (inter-quartile range IQR, 26-47 years and range, 20-78 years) and 47 (71.2%) donors were males. The duration between time of death and time of usage was noted as post-mortem time (PMT). Median PMT was 41.5 hours (IQR, 27-58.5 hours and range, 15-114 hours). In a study by Augusteyn et al. (2006), it was shown that storing lenses for a long time can cause swelling and capsular detachment, which can be detected from changes in the lens thickness to diameter ratio. Therefore, during the experimental procedures, tissues were monitored to ensure that there was no damage and lenses were evaluated for any postmortem swelling.
The eyes were dissected according to the protocol described earlier (Augusteyn et al., 2011; Manns et al., 2007). In brief, external tissues of the globe, including tenons, extra ocular muscle insertions and conjunctiva, were excised. Balanced salt solution (Alcon Laboratories Inc., Fort Worth, TX, USA) was injected through the optic nerve into the globe to maintain globe tonicity during tissue dissection and measurements.
Globe antero-posterior length (GAPL), globe horizontal diameter, globe vertical diameter, cornea horizontal diameter and cornea vertical diameter were measured using digital calipers (INOX IP54 calipers; Micro Precision Calibration Inc, Calif., Grass Valley, California) as described previously (Augusteyn et al., 2012; Mohamed et al., 2013). The average of horizontal and vertical dimensions provided mean globe diameter (MGD) and mean cornea diameter (MCD).
After the external measurements were taken, the anterior scleral surface was bonded with eight custom-made scleral shoes that help in avoiding globe deformation during dissection. The posterior segment and vitreous were cut off circumferentially to expose the lens posterior surface leaving behind a rim of anterior vitreous. The cornea and iris were then carefully excised leaving tissue containing the accommodating framework, including the lens, intact zonules, ciliary body and sections of the sclera.
The scleral-shoe-plus-tissue assembly was placed in a chamber filled with Dulbecco’s Modified Eagle’s Medium (DMEM/F-12, D8437, Sigma, St Louis, MO, USA) and was connected to the Ex Vivo Accommodation System (EVAS) through pulleys and strings as described elsewhere (Augusteyn et al., 2011; Manns et al., 2007). An advantage of using the lens stretcher is that the zonule attachment to the lens capsule remains intact and the only force acting on the lens is gravity which is also partially counteracted by the lens buoyancy. To further control the effect of potential distorting forces, measurement of stretching force was used to determine the stretch state. Tension was applied to the stretcher until resistance was observed by an increase in the measured force, at which point measurements were taken.
LD, LT and LP were measured as described previously (Augusteyn et al., 2011). Briefly, the lens was imaged in the unstretched (accommodated) state using high magnification retro-illumination photography. LD was measured in pixels from the image in vertical and horizontal meridians using graphical software Canvas 9.0 (ACD Systems, Miami, FL, USA). Pixels were converted into mm using the calibration obtained with a precision ruler. The average of the vertical and horizontal measurements was taken as the LD. LT was measured on images with the lens illuminated obliquely with a slit. A fixed proportionality factor was derived to convert oblique thickness to true axial thickness as described earlier (Augusteyn et al., 2011). LP was measured using a custom designed optical system based on the principle of Scheiner (Augusteyn et al., 2011).
Statistical analysis was performed using software STATA v14.2 (StataCorp, College Station, TX, USA). Continuous data were checked for the normality of distribution by the Shapiro-Wilk test. The mean ± standard deviation or median with IQR were used to describe the continuous data if the distribution was normal or non-normal, respectively. The relationships between age and corneal or globe dimensions were evaluated by linear regression. Bivariate analyses between age, globe dimensions and cornea dimensions as independent variables and LD, LT or LP as dependent variable were also performed by linear regression. Relationships between explanatory variables (age, GAPL, MGD and MCD) and response variables (LD, LT or LP) were assessed by multivariate stepwise regression analysis (backward elimination). A p-value of <0.05 was considered statistically significant.
3. Results
3.1. Ocular dimensions and age
It has been shown that globe dimensions change rapidly in the first 2 post-natal years while lens remodeling continues until the late teens before dimension changes become linear with age (Augusteyn, 2010; Mohamed et al., 2020). Since all lenses and globes were from donor aged 20 years and above, where dimensions vary linearly with age, multivariate linear regression analysis was performed. The relationships of LD, LT, GAPL, MGD and MCD with age are presented in Figure 1.
Figure 1: Ocular dimensions and age.

Changes with age in (A) globe antero-posterior length (GAPL), mean globe diameter (MGD) and mean corneal diameter (MCD) and (B) lens diameter (LD) and lens thickness (LT).
Linear regression analysis (Figure 1B) indicated that LD increases with age [LD (mm) = 8.748 (mm) + 0.012(mm/year)*Age(year); p = 0.0001; R2 = 0.22] as does LT [LT (mm) = 3.511 (mm) + 0.012(mm/year)*Age(year); p = 0.004; R2 = 0.22]. There was no significant correlation between age and lens aspect ratio (LT/LD; p = 0.12), age and GAPL (p = 0.77), age and MGD (p = 0.49) or age and MCD (p = 0.33). Mean aspect ratio was 0.43 ± 0.03. Mean GAPL was 24.66 ± 0.70 mm (range, 22.90-26.03 mm). Mean MGD was 24.44 ± 0.67 mm (range, 22.85-26.44 mm). Mean MCD was 11.68 ± 0.50 mm (range, 10.18-12.61 mm). No significant gender differences were found for any of the parameters examined in the present study.
3.2. Interrelationships of ocular dimensions
Regression analysis of all combinations of the dimensions indicated that GAPL and LD are significantly correlated [Figure 2A; LD (mm) = 4.481 (mm) + 0.192(mm/mm)*GAPL(mm); p = 0.0004; R2 = 0.18] as were MCD and LD [Figure 2C; LD (mm) = 7.196 (mm) + 0.173(mm/mm)*MCD(mm); p = 0.03; R2 = 0.07], There is no relationship between MGD and LD (Figure 2B; p = 0.053). GAPL and LT are also significantly correlated [Figure 2D; LT (mm) = 8.253 (mm) - 0.175(mm/mm)*GAPL(mm); p = 0.01; R2 = 0.18] but there is no relationship between LT and any of the other parameters examined (MGD vs LT: p = 0.37; MCD vs LT: p = 0.25, Figures 2E and 2F, LD vs LT: p = 0.44). The aspect ratio (LT/LD) also significantly correlated with GAPL [LT/LD = 1.013 – 0.024(mm−1)*GAPL(mm); p = 0.002; R2 = 0.25] and not with MGD (p = 0.20) or MCD (p = 0.16).
Figure 2: Interrelationships of ocular dimensions.

Regression analysis of lens diameter on globe antero-posterior length (A), on mean globe diameter (B) and on mean corneal diameter (C) and regression analysis of lens thickness on globe antero-posterior length (D), on mean globe diameter (E) and on mean corneal diameter (F).
As age, GAPL and MCD are significant predictors of LD in the bivariate analyses, a multiple regression analysis was performed. A backward elimination exploratory approach (Table 1) showed MGD (p = 0.70) and MCD (p = 0.22) to be insignificant variables. The analysis showed that both age (co-efficient: 0.012 ± 0.003 mm/year; p<0.001) and GAPL (co-efficient: 0.185 ± 0.045 mm/mm; p<0.001) are significant predictors of LD in the model (p<0.0001, R2 = 0.38 and constant term 4.212 ±1.119 mm with p<0.001) containing these two variables. A backward elimination exploratory approach in multiple regression analysis of LT (Table 1) also showed that both age (co-efficient: 0.010 ± 0.004 mm/year; p = 0.009) and GAPL (co-efficient: −0.143 ± 0.060 mm/mm; p = 0.02) are significant predictors of LT in the model (p = 0.001, R2 = 0.33 and constant term 7.088 ±1.511 mm with p<0.001) containing these two variables, and not MGD (p = 0.23), MCD (p = 0.92) or LD (p = 0.83). Multiple regression analysis of the aspect ratio indicated that only GAPL is a significant predictor (co-efficient: −0.027 ± 0.011 ratio/mm; p = 0.02).
Table 1:
Regression summary table for lens diameter, lens thickness and lens power listing the steps of backward elimination indicating which variable was eliminated at each step (with the statistical significance and coefficient) and then the final model.
| Dependent variable: Lens diameter | |||
|---|---|---|---|
| Step | Variable Eliminated | Co-efficient ± standard error | p-value |
| 1 | Mean globe diameter | 0.027 ± 0.071 | 0.70 |
| 2 | Mean cornea diameter | 0.082 ± 0.065 | 0.22 |
| Final Model | Predictor Variables | Co-efficient ± standard error | p-value |
| p<0.0001 | Age | 0.012 ± 0.003 | <0.001 |
| R2 = 0.38 | Globe antero-posterior length | 0.185 ± 0.045 | <0.001 |
| Constant term | 4.212 ± 1.119 | <0.001 | |
| Dependent variable: Lens thickness | |||
| Step | Variable Eliminated | Co-efficient ± standard error | p-value |
| 1 | Mean cornea diameter | −0.009 ± 0.091 | 0.92 |
| 2 | Lens diameter | 0.033 ± 0.150 | 0.83 |
| 3 | Mean globe diameter | 0.092 ± 0.075 | 0.23 |
| Final Model | Predictor Variables | Co-efficient ± standard error | p-value |
| p = 0.001 | Age | 0.010 ± 0.004 | 0.009 |
| R2 = 0.33 | Globe antero-posterior length | −0.143 ± 0.060 | 0.02 |
| Constant term | 7.088 ± 1.511 | <0.001 | |
| Dependent variable: Lens power | |||
| Step | Variable Eliminated | Co-efficient ± standard error | p-value |
| 1 | Lens thickness | -0.755 ± 2.134 | 0.73 |
| 2 | Lens diameter | −0.712 ± 1.549 | 0.65 |
| 3 | Globe antero-posterior length | −0.685 ± 0.822 | 0.41 |
| 4 | Mean globe diameter | 0.208 ± 0.562 | 0.71 |
| 5 | Mean cornea diameter | 0.873 ± 0.740 | 0.24 |
| Final Model | Predictor Variables | Co-efficient ± standard error | p-value |
| p<0.0001 | Age | −0.260 ± 0.037 | <0.001 |
| R2 = 0.49 | Constant term | −33.137 ± 1.451 | <0.001 |
To further explore the relationship between the lens and GAPL, all dimensions were corrected for age, leaving only the residual variations in each globe and its lens. All residuals were randomly distributed about their mean (GAPL, −0.011 ± 0.65 mm and range −1.5 to +1.5 mm; LD, 0.029 ± 0.26 mm and range −0.64 to +0.73 mm; LT, −0.024 ± 0.24 mm and range +0.59 to −0.56 mm). The GAPL residuals range indicates that the globe can be up to 1.5 mm shorter or longer than the adult average of 24.66 mm. Approximately one-third are shorter.
3.3. Lens power
The relationship of LP with age is presented in Figure 3. Reliable data on LP for ages >60 years could not be obtained because of early cataract development in the Indian population. Linear regression analysis indicated that lens power decreases with age [LP (D) = 33.14 (D) - 0.26(D/year)*Age(year); p<0.0001; R2 = 0.49] and lens diameter [LP (D) = 57.03 (D) – 3.66(D/mm)*LD(mm); p = 0.03; R2 = 0.09], Regression analyses also indicated that there was no relationship between LT and LP (p = 0.07), GAPL and LP (p = 0.87), MGD and LP (p = 0.66), and MCD and LP (p = 0.33). A backward elimination exploratory approach in multiple regression analysis (Table 1) showed only age to be a significant predictor of LP and not GAPL (p = 0.41), MGD (p = 0.71), MCD (p = 0.24), LD (p = 0.65) or LT (p = 0.73).
Figure 3: Lens power and age.
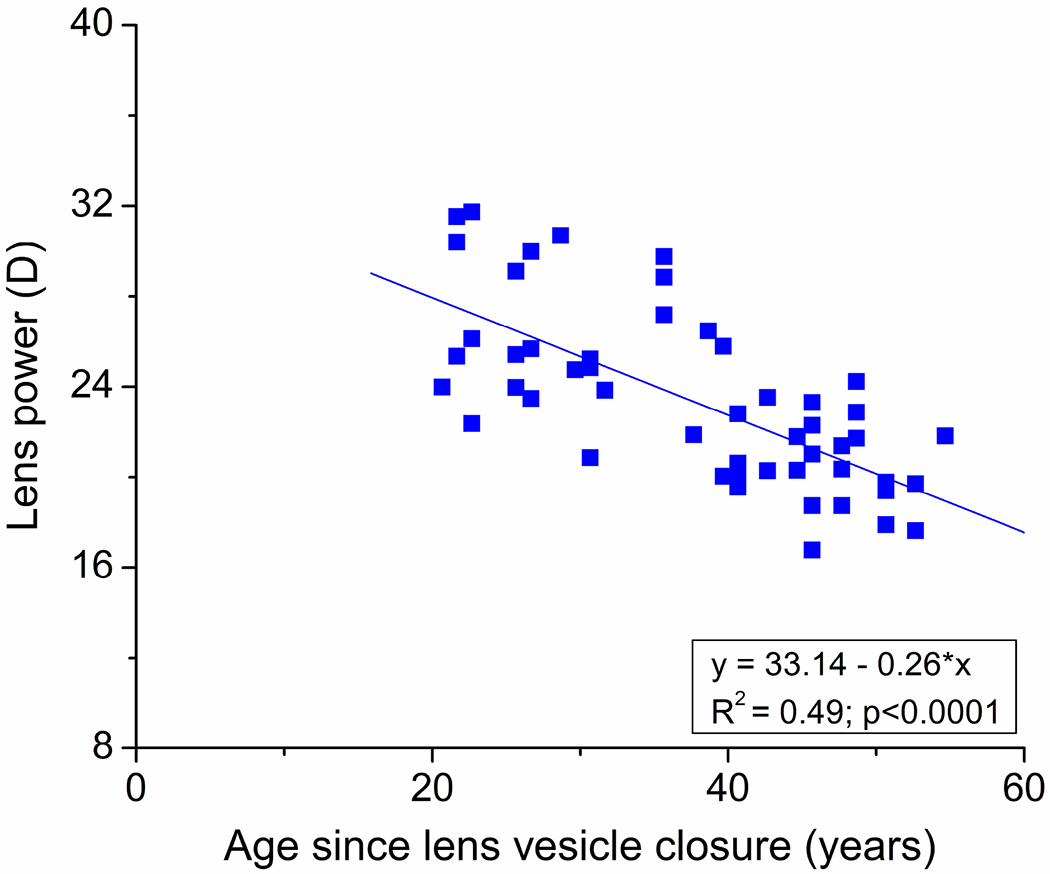
Changes with age in lens power (−0.26 D/year).
4. Discussion
The human lens is a unique tissue; it does not discard cells despite growing continuously. Its growth pattern is complex with differences between the diameter and thickness (Augusteyn, 2010). Diameter growth is biphasic: rapid and asymptotic in the prenatal to late teen years period followed by slow apparently linear growth thereafter (Augusteyn, 2010). Thickness also increases rapidly in prenatal life but decreases from around 2 years to the late teens before increasing again (Augusteyn, 2010; Martinez-Enriquez et al., 2020; Mohamed et al., 2020). Understanding the relationship of the complex growth patterns with other ocular dimensions would provide better cognizance of the age-related changes in various lens properties. In this study, we have evaluated the effect of external ocular factors, cornea and globe dimensions, on lens diameter, thickness and power. Dimension comparisons were made only with tissues from the available donors over 20 years old when lens remodeling is complete. The measurements were acquired on lenses mounted in a lens stretcher in the unstretched state, corresponding to maximal accommodation.
Our observations have revealed that, apart from age, lens diameter and thickness are also significantly correlated with the globe’s antero-posterior length. However, the relationships are not just for longer eyes but also include shorter eyes. Thus for eyes longer than the adult mean of 24.66 mm, the equatorial diameter is larger and the axial thickness is smaller. For shorter eyes, the equatorial diameter is smaller and the thickness is greater. Based on the observations of Bekerman et al. (2014) on globe dimensions, it would appear that the longer eyes may be associated with myopia and the shorter eyes with hypermetropia. These relationships are reflected in the aspect ratio which decreases with increasing eye length. These responses in LD and LT do not appear to be accompanied by a change in MGD implying that the lens changes are not simply passive responses to changes in overall globe size.
It is unlikely that lens growth determines eye length since GAPL reaches its maximum before age 2 while the lens keeps growing thereafter. What actually determines globe length remains to be established. It seems that the dimensions of the growing lens are adjusted to maintain emmetropia for the different globe lengths. It is not possible from the current data to determine whether this occurs during the prenatal growth phase which finishes around age 2 or during the remodeling phase which terminates in the late teens (Augusteyn, 2010). Such information could be of value in understanding myopia development. Significant numbers of lenses aged under 20 years were not available in the present study to examine this in detail.
Lens power correlation with age is evident in the literature both in vivo and in vitro (Borja et al., 2008; Jongenelen et al., 2015; Moffat et al., 2002). In agreement with previous observations, we also found that lens power decreases with age. Some in vivo studies have found a strong correlation between lens power and refractive error and axial length (Meng et al., 2011; Muralidharan et al., 2019). It was not possible to compare these findings with ours since we did not measure axial length and refractive status of the post-mortem donor globes and GAPL was not reported in the previous in vivo studies. The effect of GAPL on LP has not been examined in the past. Our results suggest that, in the adult, lens power is not influenced by globe length. An analysis of lens thickness and curvature by Martinez-Enriquez et al. (2020) shows that in adult lenses (age 20 and older), there is no obvious relationship between thickness and radius or thickness and power in adult lenses. So the fact that we find an effect for thickness but not for power in adult lenses is not a contradiction.
After about the age of 2, refractive development is a balance between changes in lens shape and changes in the eye length and retinal shape. The changes in eye length are expected to be correlated with changes in GAPL. As the eye grows in the lateral direction during childhood, it stretches the lens and causes a reduction in lens thickness and power (Mutti et al., 1998). During this equatorial growth phase, there is a relationship between eye growth and lens thickness and power (Xiong et al., 2017). Assuming similar lens diameters, thinner lenses would expectedly be flatter and have less power. For emmetropisation to be successful, this decrease in lens power should correlate with longer eyes. When the lens transitions to the axial growth phase in the late teens, it begins with a flatter lens in the longer eye. Our finding that lens thickness and eye length but not lens power and eye length are correlated in adult lenses suggests that, during the axial growth phase, additional changes in lens thickness and lens curvature beyond those that occurred during the equatorial growth phase are independent of each other. This could explain why lens thickness and diameter are not correlated. At this stage, a correlation between the additional changes in lens thickness and any additional elongation of the eye is not expected, since lens thickness changes are now uncorrelated with curvature changes which determine lens power. Together these findings suggest a reduced role of lens growth on refractive development after the transition from equatorial to axial growth.
Our ex vivo study is the first of its kind to perform multiple regression analyses to evaluate the effect of external factors on LD and LT. Although relationships between age, corneal diameter or globe dimensions and LD were evaluated independently in various past studies (Dong and Joo, 2001; Khng and Osher, 2008; Lim et al., 1998), none of them analyzed the effect on LD after adjustments for the other variables. Lim et al. (1998) found that LD exhibited a significant positive correlation with age and GAPL independently, similar to our present observations. However, multiple regression analysis was not performed by the authors to evaluate the age-adjusted effect of GAPL on LD. Khng and Osher (2008) found a weak (R2 = 0.10) but significant (p = 0.005) relationship between cornea and lens diameters but concluded that lens dimensions cannot be predicted from corneal dimensions. A study of post-mortem eyes by Dong and Joo (2001) also revealed a significant positive correlation between corneal diameter and LD (R2 = 0.71, p<0.001). The range of values measured appeared comparable to our study; however, age was not provided (Dong and Joo, 2001). We also detected a positive relationship between average corneal and lens diameters in bivariate analysis but this became insignificant in a multiple regression analysis.
In the present study, multiple regression modelling was performed with age, corneal and globe dimensions (significant factors in bivariate analyses) as independent variables and LD or LT as dependent variables. Only age and GAPL turned out to be significant factors affecting LD and LT in the models and not cornea or globe diameter. The results established the following equations that can be used to predict isolated lens diameter and thickness after age 20 years for globe lengths between 23 mm and 26 mm:
and
A possible limitation of the current study was the difficulty in obtaining clear axial images of the lens. This resulted in fewer LT measurements and greater scatter in the data than for LD. This may be responsible for the apparently low growth rate of 0.01 mm/year compared to the 0.012-0.024 mm/year reported previously (Atchison et al., 2008; Augusteyn, 2010; Dubbelman et al., 2003; Mohamed et al., 2012; Rosen et al., 2006; Schachar, 2005). However, this does not affect the overall conclusions of this study. Another limitation was that the relationships between corneal asymmetry and lens asymmetry (e.g. whether horizontal diameter of the cornea correlated with horizontal diameter of the lens) were not examined.
5. Conclusions
Our study results suggest that, apart from aging, lens diameter and thickness are related to the anteroposterior length of the eye globe. Lens power is not influenced by globe dimensions.
Highlights.
Little is known about factors other than age that contribute to lens properties.
Lens diameter and thickness are dependent on antero-posterior globe length
Globes with large lengths have long lens diameters and short thicknesses.
Adult human crystalline lens power is not dependent on any globe dimension
First ex vivo study to reveal the effect of globe on lens in a multiple regression.
Funding:
This study has been supported by National Eye Institute Grants R01EY021834, P30EY14801 (Center Grant); the Australian Federal Government CRC Scheme through the Vision Cooperative Research Centre; the Hyderabad Eye Research Foundation; Florida Lions Eye Bank and the Beauty of Sight Foundation; Dr Harry W Flynn Jr; Drs Karl R Olsen and Martha E Hildebrandt; Drs Raksha Urs and Aaron Furtado; an unrestricted grant from Research to Prevent Blindness to the Department of Ophthalmology, University of Miami and the Henri and Flore Lesieur Foundation (J-M. Parel).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: None for all authors.
References
- Atchison DA, Markwell EL, Kasthurirangan S, Pope JM, Smith G, Swann PG, 2008. Age-related changes in optical and biometric characteristics of emmetropic eyes. J. Vis. 8, 29.1–20. 10.1167/8.4.29. [DOI] [PubMed] [Google Scholar]
- Augusteyn RC, 2010. On the growth and internal structure of the human lens. Exp. Eye. Res. 90, 643–654. 10.1016/j.exer.2010.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augusteyn RC, Mohamed A, Nankivil D, Veerendranath P, Arrieta E, Taneja M, Manns F, Ho A, Parel JM, 2011. Age-dependence of the optomechanical responses of ex vivo human lenses from India and the USA, and the force required to produce these in a lens stretcher: the similarity to in vivo disaccommodation. Vision. Res. 51, 1667–1678. 10.1016/j.visres.2011.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augusteyn RC, Nankivil D, Mohamed A, Maceo B, Pierre F, Parel JM, 2012. Human ocular biometry. Exp. Eye. Res. 102, 70–75. 10.1016/j.exer.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augusteyn RC, Rosen AM, Borja D, Ziebarth NM, Parel JM, 2006. Biometry of primate lenses during immersion in preservation media. Mol. Vis. 12, 740–747. [PubMed] [Google Scholar]
- Bekerman I, Gottlieb P, Vaiman M, 2014. Variations in eyeball diameters of the healthy adults. J. Ophthalmol. 2014, 503645. 10.1155/2014/503645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borja D, Manns F, Ho A, Ziebarth N, Rosen AM, Jain R, Amelinckx A, Arrieta E, Augusteyn RC, Parel JM, 2008. Optical power of the isolated human crystalline lens. Invest. Ophthalmol. Vis. Sci. 49, 2541–2548. 10.1167/iovs.07-1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong EY, Joo CK, 2001. Predictability for proper capsular tension ring size and intraocular lens size. Kor. J. Ophthalmol. 15, 22–26. 10.3341/kjo.2001.15.1.22. [DOI] [PubMed] [Google Scholar]
- Dubbelman M, van der Heijde GL., Weeber HA, Vrensen GFJM, 2003. Changes in the internal structure of the human crystalline lens with age and accommodation. Vision. Res. 43, 2363–2375. 10.1016/s0042-6989(03)00428-0. [DOI] [PubMed] [Google Scholar]
- Garner LF, Yap M, Scott R, 1992. Crystalline lens power in myopia. Optom. Vis. Sci. 69, 863–865. 10.1097/00006324-199211000-00005. [DOI] [PubMed] [Google Scholar]
- He J, Lu L, He X, Xu X, Du X, Zhang B, Zhao H, Sha J, Zhu J, Zou H, Xu X, 2017. The Relationship between Crystalline Lens Power and Refractive Error in Older Chinese Adults: The Shanghai Eye Study. PLoS. One. 12, e0170030. 10.1371/journal.pone.0170030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heys KR, Cram SL, Truscott RJ, 2004. Massive increase in the stiffness of the human lens nucleus with age: the basis for presbyopia? Mol. Vis. 10, 956–963. [PubMed] [Google Scholar]
- Jongenelen S, Rozema JJ, Tassignon MJ, EVICR.net., Project Gullstrand Study Group., 2015. Distribution of the Crystalline Lens Power In Vivo as a Function of Age. Invest. Ophthalmol. Vis. Sci. 56, 7029–7035. 10.1167/iovs.15-18047. [DOI] [PubMed] [Google Scholar]
- Khng C, Osher RH, 2008. Evaluation of the relationship between corneal diameter and lens diameter. J. Cataract. Refract. Surg. 34, 475–479. 10.1016/j.jcrs.2007.10.043. [DOI] [PubMed] [Google Scholar]
- Lim SJ, Kang SJ, Kim HB, Kurata Y, Sakabe I, Apple DJ, 1998. Analysis of zonular-free zone and lens size in relation to axial length of eye with age. J. Cataract. Refract. Surg. 24, 390–396. 10.1016/s0886-3350(98)80329-5. [DOI] [PubMed] [Google Scholar]
- Manns F, Parel JM, Denham D, Billotte C, Ziebarth N, Borja D, Fernandez V, Aly M, Arrieta E, Ho A, Holden B, 2007. Optomechanical response of human and monkey lenses in a lens stretcher. Invest. Ophthalmol. Vis. Sci. 48, 3260–3268. 10.1167/iovs.06-1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Enriquez E, de Castro A, Mohamed A, Sravani NG, Ruggeri M, Manns F, Marcos S, 2020. Age-Related Changes to the Three-Dimensional Full Shape of the Isolated Human Crystalline Lens. Invest. Ophthalmol. Vis. Sci. 61, 11. 10.1167/iovs.61.4.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng W, Butterworth J, Malecaze F, Calvas P, 2011. Axial length of myopia: a review of current research. Ophthalmologica. 225, 127–134. 10.1159/000317072. [DOI] [PubMed] [Google Scholar]
- Moffat BA, Atchison DA, Pope JM, 2002. Age-related changes in refractive index distribution and power of the human lens as measured by magnetic resonance micro-imaging in vitro. Vision. Res. 42, 1683–1693. 10.1016/s0042-6989(02)00078-0. [DOI] [PubMed] [Google Scholar]
- Mohamed A, Augusteyn RC, 2018. Human lens weights with increasing age. Mol. Vis. 24, 867–874. [PMC free article] [PubMed] [Google Scholar]
- Mohamed A, Durkee HA, Williams S, Manns F, Ho A, Parel JMA, Augusteyn RC, 2021. Morphometric analysis of in vitro human crystalline lenses using digital shadow photogrammetry. Exp. Eye. Res. 202, 108334. 10.1016/j.exer.2020.108334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamed A, Nankivil D, Pesala V, Taneja M, 2013. The precision of ophthalmic biometry using calipers. Can. J. Ophthalmol. 48, 506–511. 10.1016/j.jcjo.2013.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamed A, Sangwan VS, Augusteyn RC, 2012. Growth of the human lens in the Indian adult population: preliminary observations. Indian. J. Ophthalmol. 60, 511–515. 10.4103/0301-4738.103775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muralidharan G, Martínez-Enríquez E, Birkenfeld J, Velasco-Ocana M, Pérez-Merino P, Marcos S, 2019. Morphological changes of human crystalline lens in myopia. Biomed. Opt. Express. 10, 6084–6095. 10.1364/BOE.10.006084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutti DO, Zadnik K, Fusaro RE, Friedman NE, Sholtz RI, Adams AJ, 1998. Optical and structural development of the crystalline lens in childhood. Invest. Ophthalmol. Vis. Sci. 39, 120–133. [PubMed] [Google Scholar]
- Rosen AM, Denham DB, Fernandez V, Borja D, Ho A, Manns F, Parel JM, Augusteyn RC, 2006. In vitro dimensions and curvatures of human lenses. Vision. Res. 46, 1002–1009. 10.1016/j.visres.2005.10.019. [DOI] [PubMed] [Google Scholar]
- Schachar RA, 2005. Growth patterns of fresh human crystalline lenses measured by in vitro photographic biometry. J. Anat. 206, 575–580. 10.1111/j.1469-7580.2005.00422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urs R, Ho A, Manns F, Parel JM, 2010. Age-dependent Fourier model of the shape of the isolated ex vivo human crystalline lens. Vision. Res. 50, 1041–1047. 10.1016/j.visres.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urs R, Manns F, Ho A, Borja D, Amelinckx A, Smith J, Jain R, Augusteyn R, Parel JM, 2009. Shape of the isolated ex-vivo human crystalline lens. Vision. Res. 49, 74–83. 10.1016/j.visres.2008.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong S, Zhang B, Hong Y, He X, Zhu J, Zou H, Xu X, 2017. The Associations of Lens Power With Age and Axial Length in Healthy Chinese Children and Adolescents Aged 6 to 18 Years. Invest. Ophthalmol. Vis. Sci. 58, 5849–5855. 10.1167/iovs.17-22639. [DOI] [PubMed] [Google Scholar]


