Abstract
There is consensus that social needs influence health outcomes, but less is known about the relationships between certain needs and chronic health conditions in large, diverse populations. This study sought to understand the association between social needs and specific chronic conditions using social needs screening and clinical data from Electronic Health Records. Between April 2018-December 2019, 33,550 adult (≥18y) patients completed a 10-item social needs screener during primary care visits in Bronx and Westchester counties, NY. Generalized linear models were used to estimate prevalence ratios for eight outcomes by number and type of needs with analyses completed in Summer 2020. There was a positive, cumulative association between social needs and each of the outcomes. The relationship was strongest for elevated PHQ-2, depression, alcohol/drug use disorder, and smoking. Those with ≥3 social needs were 3.90 times more likely to have an elevated PHQ-2 than those without needs (95% CI: 3.66, 4.16). Challenges with healthcare transportation was associated with each condition and was the most strongly associated need with half of conditions in the fully-adjusted models. For example, those with transportation needs were 84% more likely to have an alcohol/drug use disorder diagnosis (95% CI: 1.59, 2.13) and 41% more likely to smoke (95% CI: 1.25, 1.58). Specific social needs may influence clinical issues in distinct ways. These findings suggest that health systems need to develop strategies that address unmet social need in order to optimize health outcomes, particularly in communities with a dual burden of poverty and chronic disease.
Introduction
Chronic diseases are the leading cause of death and disability in the United States, as well as the leading contributor of healthcare costs.1 There is growing recognition that social determinants of health are important factors that influence health outcomes, including chronic diseases and related health behaviors.2 There are multiple pathways through which unmet social needs influence health outcomes. First, specific needs, such as food insecurity or poor housing quality, increase exposure to risk factors for specific diseases such as asthma and diabetes.3,4,5 Second, unmet needs lead to chronic stress, which reduces adherence to healthy behaviors and clinical care. Third, chronic stress has been shown to lead to ‘wear and tear’ on the body’s stress response system, which worsens health outcomes and may accumulate over the life course. Finally, unmet social needs and health outcomes may be bi-directional and feed into each other, preventing individuals from accessing resources for other needs and resulting in an additive effect for multiple needs.6,7
However, few studies have focused on how the burden and types of needs influence specific chronic risk factors and diseases for a large, diverse population.8 Instead, most studies have focused on singular needs,5,9,10,11 specific populations,12,13,14 overall health status15,16 or a limited number of health conditions.17,18
With the shift towards value-based the care, the influence of unmet social needs on health outcomes has become a priority for health systems. Several health systems are routinely integrating standardized social need screening into clinical care to connect patients to resources.19,20,21,22,23,24,25 As health systems implement large-scale screenings and associated data become available, there is an opportunity to leverage both screener and clinical data to understand how the overall burden of social needs, as well as how individual social needs, are associated with common chronic conditions. Analytic models that take social needs and chronic conditions into account may be able to identify types of patients who are more impacted by multiple or specific needs as well as specific needs that require prioritization. These insights could drive decisions at the practice and intervention-level regarding referrals, support services, interventions and allocation of resources. Health systems may also find it advantageous to invest in upstream factors (i.e. housing vouchers, food pantries, etc.) based on such data to optimize outcomes and decrease costs.
The objective of this study was to examine the relationship between overall social needs burden, as well as types of social needs, and specific chronic conditions to better inform quality improvement strategies.
Methods
Study population and social risk screening
Beginning in April 2018, Montefiore Medical Center began implementing a social needs screener at primary care sites in the Bronx and Westchester County, NY. The ten-item screener was based on the Health Leads screener but supplemented with questions from other tools addressing community-specific priority issues (see Table 1).26,27 These needs were selected because they are specific, actionable, and common concerns for households based on the expert opinion of the committee developing the screener. Clinics had discretion to determine the frequency and target population for screening. These decisions were influenced by numerous factors such as perceived social needs, existing workflows, staff availability and alignment with concurrent projects. Patients were provided with a paper screener, available in nine languages, to complete in the waiting or exam room. Providers reviewed the results with patients in the exam room and offered to connect patients to community health workers or social workers. Parents/guardians completed the screener for minors. (for additional detail on screening practices and workflow, see Heller et al 2020).
Table 1.
SDH screening questions and variable names
| SDH Screening Question | Variable name | % Positive |
|---|---|---|
| Are you worried that the place you are living now is making you sick? (has mold, bugs/rodents, water leaks, not enough heat) | Housing quality | 5.4 |
| Are you worried that in the next 2 months, you may not have a safe or stable place to live? (eviction, being kicked out, homelessness) | Housing instability | 5.0 |
| In the last 12 months, did you worry that your food could run out before you got money to buy more? | Food insecurity | 6.1 |
| In the last 12 months, has lack of transportation kept you from medical appointments or getting your medications? | Healthcare transportation | 5.1 |
| In the last 12 months, did you have to skip buying medications or going to doctor’s appointments to save money? | Healthcare cost | 4.8 |
| In the past 12 months, has the electric, gas, oil or water company threated to shut off services to your home? | Utilities cost | 2.7 |
| Are you finding it hard to get along with a partner, spouse, or family members? | Getting along | 4.1 |
| Do you need help getting child care or care for an elderly or sick adult? | Care need | 2.2 |
| Do you need legal help? (child/family services, immigration, housing discrimination, domestic issues, etc.)? | Legal | 2.7 |
| Does anyone in your life hurt you, threaten you, frighten you or make you feel unsafe? | Interpersonal Violence | 1.4 |
Between April 2018-December 2019, 35,084 unique adult patients (≥18y) completed social need screeners at one of the sites. After limiting the sample to those who answered all ten questions, the final sample size was 33,550. For reference, during the same time period, about 175,000 adults were seen at these clinics, though it is important to note that not all of these patients were offered a screen.
Outcome variables
The outcomes of interest were selected a priori based on a combination of factors including: known associations with social needs,5,16,17,28,29,30 importance as priority health issues to the community,31 and ability to be assessed and treated in primary care where the screener was implemented. The primary outcome variables fall into three categories: (1) risk factors for chronic disease, including smoking, alcohol/drug use disorder, and obesity, (2) prevalent chronic diseases including hypertension, diabetes, and asthma, and (3) mental/behavioral health measures, including depression and an elevated Patient Health Questionnaire-2 (PHQ-2) score.32 All conditions except for obesity, smoking and PHQ-2, were defined using International Classification of Diseases, 10th edition (ICD-10) diagnosis codes with codes for depression, alcohol/drug use disorder, diabetes and asthma derived from the Elixhauser comorbidity index.33 Obesity was defined as BMI≥30 kg/m2 based on the latest body mass index (BMI) documented in the health record. A positive PHQ-2 score was defined as a score ≥2 based on latest PHQ-2 score in the year prior to the screener. Patients were defined as smokers if they reported being a current smoker in the year prior to the screener. All outcomes were calculated using data extracted from the Electronic Health Record (EHR) using Looking Glass Clinical Analytics and Microsoft SQL Server to query data from the Epic Electronic Health Record Data Warehouse.34
Independent variables and covariates
Independent variables of interest included individual needs as well as the overall number of social needs, categorized as none, 1, 2, or ≥3 with categories selected based on the distribution of social needs to ensure adequate statistical power. Covariates included age (18–39;40–49;50–59;60–69;≥70y), sex (male, female), race/ethnicity (Hispanic, non-Hispanic Black, non-Hispanic white, non-Hispanic Asian/Pacific Islander, non-Hispanic other and a “missing” indicator), preferred language (English, Spanish, other and a “missing” indicator), health insurance at the visit (Medicaid, Medicare, commercial and a “missing” indicator), whether the patient lived in public housing (with a “missing” indicator for non-geocoded and non-NYC addresses), and block-group poverty quintile with a “missing” indicator.
To obtain block-group poverty and public housing status, patient addresses were extracted. After excluding those with PO Box addresses (n=411) and those living outside of NY, CT, PA, NJ (n=56), the remaining addresses were geocoded using either the New York State Street and Address Composite for NY addresses or the US Census Bureau geocoder for non-NY addresses. Overall, 97.7% of included patients were successfully geocoded.
New York City patients were identified as residing in public housing if their addresses geocoded to tax lots associated with public housing. Block-group poverty data was obtained from the 2014–2018 American Community Survey, the most recent year for which poverty data was available at the block-group level.35
Statistical Analysis
To determine the relationship between the number of social needs and health outcomes, unadjusted (Model 1) and adjusted (Model 2) generalized linear models, with a Poisson distribution and log-link function, were used to estimate ratios of prevalence proportions for each outcome. Robust standard errors were used in each model to address potential heteroscedasticity. Adjusted models accounted for age, sex, race/ethnicity, preferred language, health insurance type, public housing status, and block-group poverty. These covariates were included based on their known relationship with both social needs and the outcomes of interest. In a few cases, some of these variables (e.g., insurance) may be on the causal pathway between social needs and the outcomes of interest but were adjusted for in order to provide our best estimate of the direct effect/association. The direct effect/association estimates most closely address our study objective of identifying opportunities for novel interventions. Clustering of individuals by Census block group was accounted for in variance estimation for all models that adjusted for area-based poverty. Tests for trend used the number of social needs as a grouped linear variable. For analyses of each individual social need, a third model (Model 3) was also fit that adjusted for all covariates included in Model 2 as well as all social needs simultaneously to account for correlations, but not strong collinearity between social needs (Variance Inflation Factor [VIF]<1.50 for all). Effect-modification by age (18–39;40–59;≥60y) was also evaluated. Given the number of tests an interaction p-value <0.001 was considered statistically significant. Statistical analyses used Stata 16.0 (StataCorp, College Station, TX) and mapping used ArcGIS 10.3.1 (ESRI, Redlands, CA). The study was approved by the Albert Einstein College of Medicine IRB. Data were analyzed in the winter/spring of 2019.
Results
Table 1 includes the wording of the screening questions and the percent of adults answering affirmatively to each question. Characteristics of the screened population are presented in Table 2. Two-thirds of respondents were female (64.7%) and the median age was 51.9 years. Half (52.8%) of the sample was Hispanic and over one-third (37.2%) was non-Hispanic Black. Most respondents (80.6%) preferred English, while 17.2% preferred Spanish. One-third of respondents were insured through Medicaid and commercial insurance (35.1% and 36.0%, respectively) while a smaller proportion was insured through Medicare (28.9%). Nearly 11% percent of NYC respondents lived in public housing.
Table 2.
Patient characteristics among screened Montefiore Patients, April 2018-December 2019
| n | % (95% CI) | |
|---|---|---|
| Total | 33,550 | - |
| Age group | ||
| 18–39 | 11,076 | 33.0 (32.5, 0.3) |
| 40–49 | 4,656 | 13.9 (13.5, 0.1) |
| 50–59 | 5,961 | 17.8 (17.4, 0.2) |
| 60–69 | 5,814 | 17.3 (16.9, 0.2) |
| ≥70 | 6,043 | 18.0 (17.6, 0.2) |
| Sex | ||
| Male | 11,827 | 35.3 (34.7, 0.4) |
| Female | 21,723 | 64.7 (64.2, 0.7) |
| Race/ethnicity | ||
| Hispanic | 13,784 | 52.8 (52.2, 0.5) |
| Non-Hispanic black | 9,692 | 37.2 (36.6, 0.4) |
| Non-Hispanic white | 1,753 | 6.7 (6.4, 0.1) |
| Non-Hispanic Asian/Pacific | ||
| Islander | 784 | 3.0 (2.8, 0.0) |
| Other | 73 | 0.3 (0.2, 0.0) |
| Missing | 7,464 | - |
| Preferred Language | ||
| English | 26,871 | 80.6 (80.2, 0.8) |
| Spanish | 5,739 | 17.2 (16.8, 0.2) |
| Other | 712 | 2.1 (2.0, 0.0) |
| Missing | 228 | - |
| Health Insurance | ||
| Medicaid | 11,126 | 35.1 (34.6, 0.4) |
| Medicare | 9,145 | 28.9 (28.4, 0.3) |
| Commercial | 11,413 | 36.0 (35.5, 0.4) |
| Missing | 1,866 | - |
| Block-group poverty, % | ||
| Q1: 0–8.2% | 6,517 | 20.2 (19.7, 0.2) |
| Q2: 8.2%−17.2% | 6,408 | 19.8 (19.4, 0.2) |
| Q3: 17.2%−28.1% | 6,456 | 20.0 (19.6, 0.2) |
| Q4: 28.1%−39.8% | 6,458 | 20.0 (19.6, 0.2) |
| Q5: 39.8%−88.4% | 6,459 | 20.0 (19.6, 0.2) |
| Missing | 1,252 | - |
| Public housing | ||
| No | 26,958 | 89.4 (89.0, 0.9) |
| Yes | 3,207 | 10.6 (10.3, 0.1) |
| Outside of NYC/Missing | 3,385 | - |
Across health conditions examined, 45.2% had hypertension, 43.7% were obese, 11.4% were current smokers, and 6.9% had a diagnosis related to drug/alcohol use disorder. Over one quarter (26.0%) of patients had diabetes and 18.2% had asthma. One-quarter of patients (25.5%) had depression and 18.4% had a positive PHQ-2 score.
Number of Risks and Health Outcomes
Figure 1 shows the unadjusted and adjusted association between number of social needs and each outcome. There was a significant, positive relationship between the number of needs and each outcome, although the strength of the relationship varied by outcome. Adjustment for covariates resulted in some attenuation of associations. For example, the prevalence ratio comparing ≥3 needs to no needs for elevated PHQ-2 decreased from 4.50 to 3.90 and for alcohol/drug use disorder from 2.85 to 2.15. In fully-adjusted analyses, the dose-response relationship was strongest for elevated PHQ-2, depression, alcohol/drug use disorder, and smoking status, in that order. Those with ≥3 needs were almost 4 times as likely (prevalence ratio [PR]: 3.90, 95% Confidence Interval [CI]: 3.66, 4.16) to have a positive PHQ-2 result than those without needs. The dose-response relationship was weakest for obesity and hypertension (hypertension PR: 1.15, 95% CI: 1.09, 1.21; obesity PR: 1.06, 95% CI: 1.00, 1.12).
Figure 1.
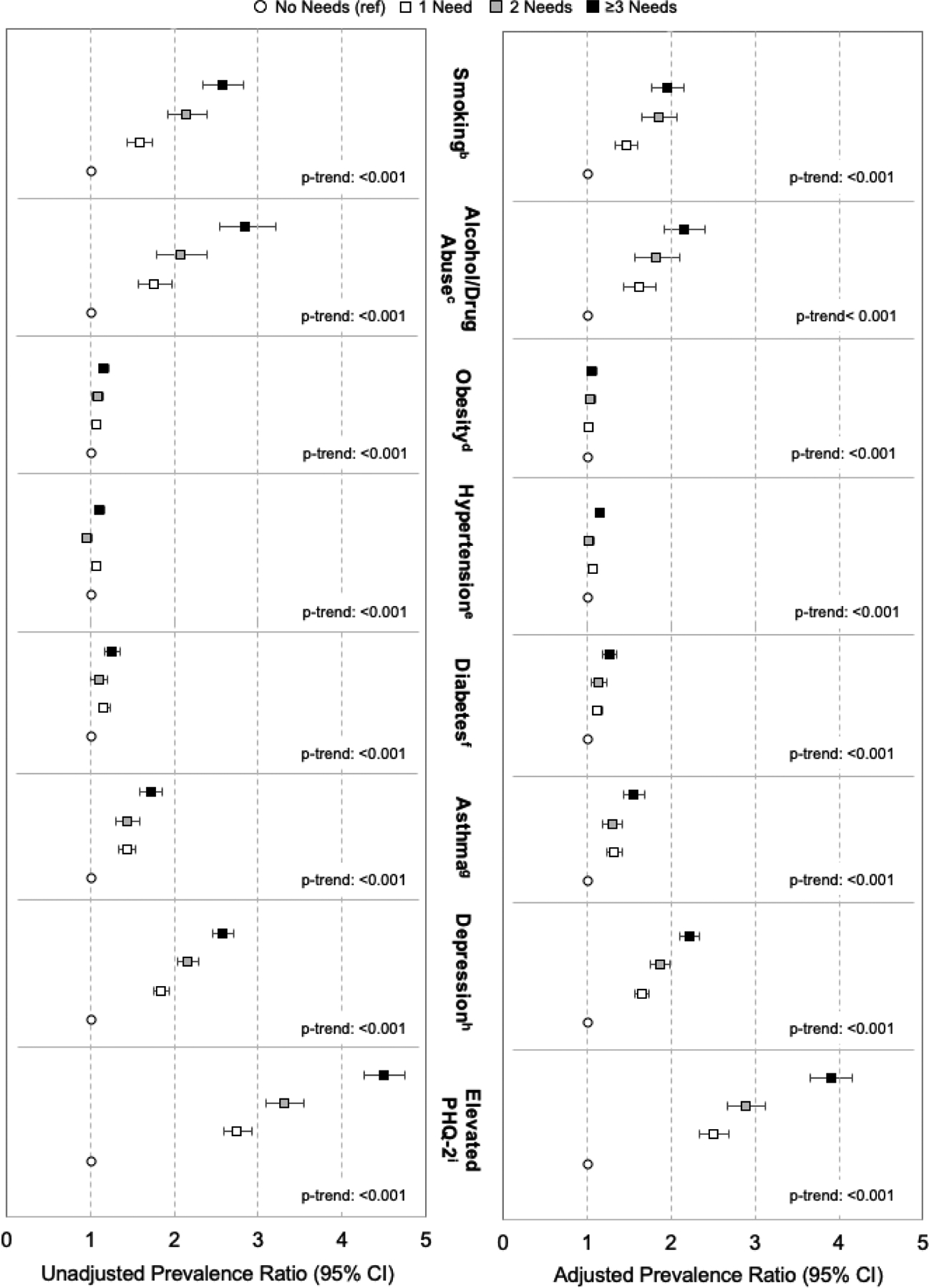
Unadjusted and adjusteda prevalence ratio of outcomes by number of unmet needs among screened Montefiore patients, April 2018-December 2019
Figure reflects the unadjusted and adjusted prevalence ratios of selected chronic conditions by number of needs (no needs (referent; white circle); 1 need (white square); 2 needs (gray square); ≥3 needs (black square). Tests for trend used number of needs as a grouped linear variable.
aAdjusted for age, sex, race/ethnicity, preferred language, health insurance, block-group poverty and public housing status; bDefined as those reporting being a current smoker in latest smoking survey in 1 year prior to the screener; excludes 7.5% not surveyed; cDefined as those with a diagnosis for the following: F11.x–F16.x, F18.x, F19.x, Z71.5, Z72.2, F10, E52, G62.1, I42.6, K29.2, K70.0, K70.3, K70.9, T51.x, Z50.2, Z71.4, Z72.1 in two years prior to screener; dDefined as those with BMI≥30 kg/m2, based on latest BMI value in 1 year prior to screener; excludes 2.1% without BMI measurement; eDefined as those with I10.x diagnosis in two years prior to screener; fDefined as those with E10.X, E11.X, E12.X, E13.X, E14.X diagnosis codes in two years prior to screener; gDefined as those with J45.X diagnosis codes in two years prior to screener; hDefined as those with F20.4, F31.3–F31.5, F32.x, F33.x, F34.1, F41.X, F43.2 diagnosis codes in two years prior to screener; iDefined as those with a score ≥2, based on latest PHQ-2 score in 1 year prior to screener; excludes 7.5% of sample not screened
Types of Risks and Health Outcomes
Table 2 shows the relationship between each need and outcome in unadjusted, adjusted and fully-adjusted analyses (e.g., those mutually adjusting for all needs). To complement the table, Figure 2 shows the social need with the strongest fully-adjusted association with each outcome. For half of the health outcomes/risk factors, healthcare transportation had the strongest association of the needs. Those reporting healthcare transportation as a need were 84% (95% CI: 1.59, 2.13) more likely to have an alcohol/drug use disorder-related diagnosis and 41% (95% CI: 1.25, 1.58) more likely to smoke than those without a healthcare transportation need. The mental/behavioral health outcomes had the strongest associations with any social need; those with issues getting along with others were 98% and 82% more likely to an elevated PHQ-2 or have depression, respectively. Those who had a housing quality issue were 37% more likely to have asthma than those without a housing quality issue.
Figure 2:
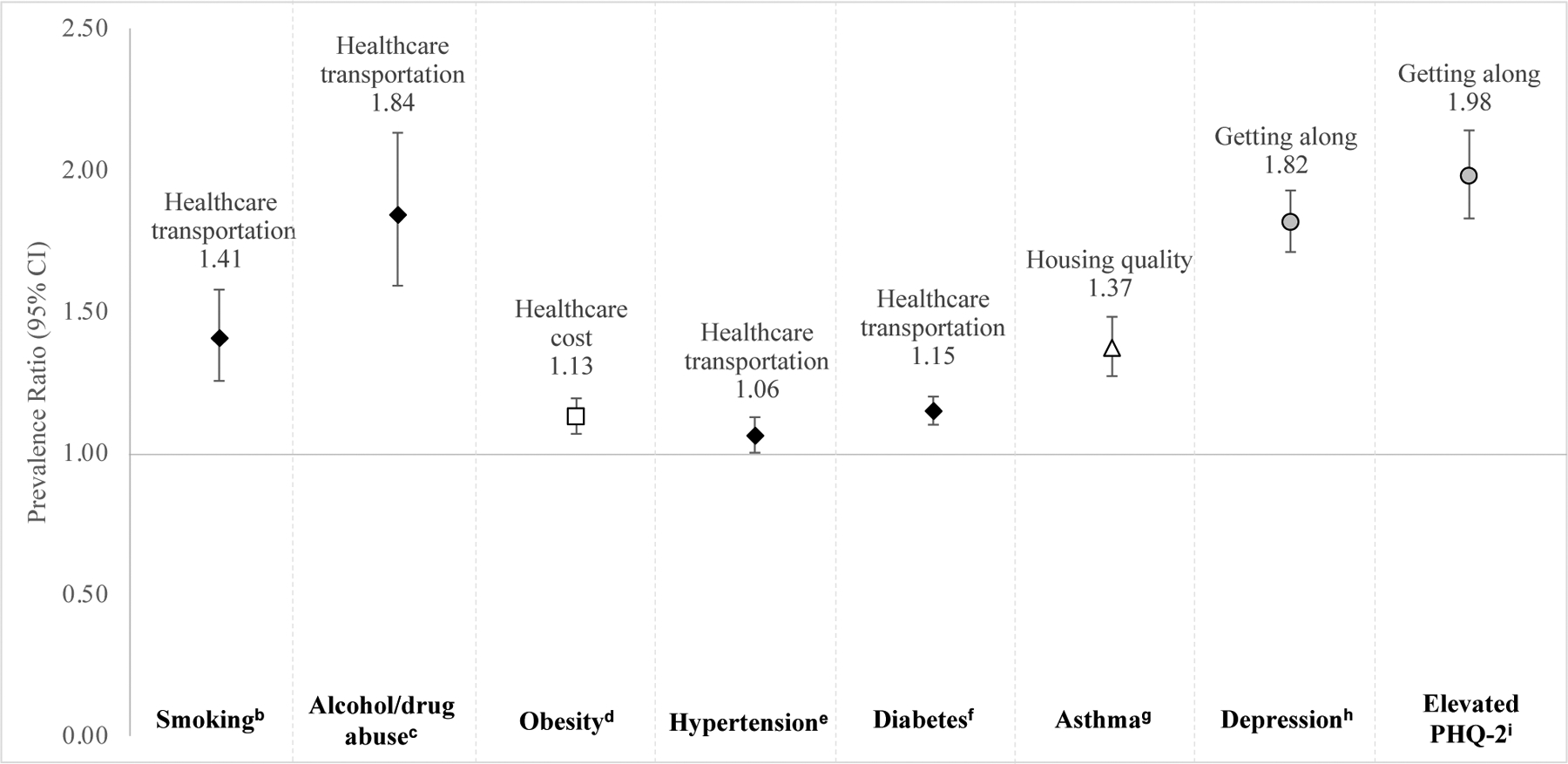
Adjusted prevalence ratio of outcomes by strongest social needs among screened Montefiore patients, April 2018-December 2019
Figure identifies the specific unmet that has the strongest fully-adjusted association with the identified chronic condition. Symbols in the figure indicate need type (healthcare transportation (black diamond); healthcare cost (white square); housing quality (white triangle); getting along (gray circle).
aAdjusted for age, sex, race/ethnicity, preferred language, health insurance, block-group poverty and public housing status; bDefined as any patient reporting being a current smoker in latest smoking survey in 1 year prior to the screener; excludes 7.5% not surveyed; cDefined as any patient with a diagnosis for the following: F11.x–F16.x, F18.x, F19.x, Z71.5, Z72.2, F10, E52, G62.1, I42.6, K29.2, K70.0, K70.3, K70.9, T51.x, Z50.2, Z71.4, Z72.1 in two years prior to screener; dDefined as BMI≥30 kg/m2, based on latest BMI value in 1 year prior to screener; excludes 2.1% without BMI measurement; eDefined as any patient with I10.x diagnosis in two years prior to screener; fDefined as any patient with E10.X, E11.X, E12.X, E13.X, E14.X diagnosis codes in two years prior to screener; gDefined as any patient with J45.X diagnosis codes in two years prior to screener; hDefined as any patient with F20.4, F31.3–F31.5, F32.x, F33.x, F34.1, F41.X, F43.2 diagnosis codes in two years prior to screener; iDefined as those with a score ≥2, based on latest PHQ-2 score in 1 year prior to screener; excludes 7.5% of sample not screened
Interactions by age
For number of social needs and interaction by age, potential interactions were observed for diabetes and hypertension, with the strongest, positive trend observed among younger adults (18–39y). For individual needs and age, associations were observed for hypertension and half of the needs (housing instability, healthcare transportation, healthcare costs, care need, legal issues), with stronger relationships observed among younger adults. For diabetes, age modified the association with healthcare transportation and housing stability, with stronger, positive trends observed among younger adults. For asthma, age modified the association with healthcare transportation, with a stronger association for younger and middle-aged adults than those ≥60y. To further understand the effect of age on the association between social needs and both hypertension and diabetes, the average number of needs and comorbidities were estimated by age strata and hypertension/diabetes status. The ratio of the mean number of needs for young adults with hypertension versus those without hypertension was 1.79, in comparison to 1.05 for older adults, with a similar pattern for diabetes. The ratio of the mean Elixhauser score was 3.05 for younger adults with hypertension versus those without, in comparison to 1.89 for older adults.
Discussion
This study examines the relationship between self-reported social needs and selected chronic conditions measured during clinical visits. The study adds to current social determinants of health literature by examining multiple needs and chronic conditions for a large, diverse population, which provides insight into how the relationship between outcomes and individual and multiple social needs may vary. Overall, we find that there is a significant relationship between the number and types of needs and common chronic outcomes, although the strength of the association varies by outcome and need. Importantly, this suggests that targeted approaches to addressing individual needs and multipronged interventions addressing multiple needs will be needed to improve health outcomes. Finally, this study underscores the utility of collecting patient-level social needs data, including that it can be used to better understand and serve patients at both the individual- and population-level. While health systems may be reluctant to screen patients because of concerns about the additional burden, obtaining patient-level data is critical to understanding the unique challenges faced by systems’ specific patient populations, whose needs may vary by context and demographics. While patient-level data may at times affirm anecdotal experiences of providers, it is also important to identify when it does not and for whom it does not, particularly in low-resource settings.
Number of Needs
Similar to previous research,12,18,36 this study finds a cumulative relationship between the number of needs and each outcome and may provide support for interventions to identify and mitigate needs in clinical care. For example, one study found a graded association between the number of social and behavioral risk factors and the risk of hypertension and diabetes for adult healthcare plan members. More specifically, those with ≥3 risk factors had 1.41 and 1.53 times the risk of developing hypertension and diabetes, respectively, although results are not comparable given the focus on incidence rather than prevalence.18 Similarly, another study found a positive association between the number of needs and the number of chronic conditions amongst a sample of 1,214 Medicaid beneficiaries.12
The strength of the relationship is not consistent across chronic conditions. Among the outcomes investigated here, social needs are most strongly associated with elevated PHQ-2, depression, alcohol/drug use disorder and smoking status and weakest for hypertension and obesity, aligning with findings from previous research.12,17 A previous study amongst adults in primary care found a significant relationship between having any needs and depression, hypertension and diabetes, with the strongest association for depression.17 Another study found that amongst Medicaid beneficiaries, the strongest association between needs and outcomes was for perceived stress, which the authors hypothesize is the short-term outcome from unmet social needs.12 This theory is supported by a framework that argues unmet needs lead to chronic stress, which worsen the body’s physiological stress-response systems and influence health outcomes as well as reduce adherence to clinical care and self-care behaviors.7 Thus, the prevalence of stress-related outcomes for patients with unmet social needs in this study may be elevated in comparison to other chronic conditions because these risk factors and conditions are the first indications of chronic stress and most sensitive to unmet needs.
Types of Needs
Identifying the needs most strongly associated with chronic diseases and the most frequently significant needs across these conditions can also identify patients at higher risk for specific outcomes and direct referrals to interventions. As Figure 2 depicts, in the fully-adjusted models, healthcare transportation most frequently had the strongest association with the selected outcomes. Similarly, healthcare transportation was the need most frequently associated with the outcomes in the fully-adjusted model, significant for seven of eight outcomes. These results identify challenges with healthcare transportation as a priority social need in improving chronic disease. Previous literature has identified transportation as a key barrier to the timely access of medical care and medications, particularly for those who are chronically ill.37,38 Additionally, previous analyses using social needs data from the same health system identified healthcare transportation as the need most strongly associated with no show visits and thus, an important barrier in access to care.39
This study also adds to the literature by adjusting for multiple social needs in the same models, which allows us to identify which need has the strongest independent association with each outcome. For example, after adjusting for other needs, only healthcare transportation remained associated with diabetes, despite the fact that over half of the measured needs were associated with diabetes in models not accounting for other social needs. This suggests that healthcare transportation has the strongest independent relationship with diabetes and may be important to consider in addressing diabetes at the population-level.
Interactions by Age
Finally, the analysis identified significant interactions by age for the burden and types of social needs for selected conditions. There was a stronger association between the number of needs and specific needs and having diabetes and hypertension for younger adults. Multiple factors are possible explanations for the smaller effect size, including that social needs may play a larger role in hypertension and diabetes for younger adults than older adults or older adults may have access to more social programs and support than their younger counterparts. Additionally, this difference could be attributed to the fact that individuals in lower socioeconomic groups often have a lower life expectancy.40 Additional estimates found that younger adults with hypertension or diabetes may be of higher need or medically more complex than their counterparts without hypertension or diabetes than older adults, although additional research is needed. These findings may be used to inform care and interventions.
Limitations
This study is not without its limitations. First, the cross-sectional nature of the data prevents us from attributing causality though the stated goal of the project was not to elucidate causal relationships. While the study examines the relationship between social needs and chronic disease, it does not examine the specific mechanisms for the observed relationships. However, a previous analysis of screening data and no-show visits from the same health system identified challenges with healthcare transportation as the social need most strongly associated with no-shows.39 More specifically, patients that reported challenges with healthcare transportation had a 24.4% higher no-show proportion than those without. Future research should focus on exploring possible mechanisms for these associations, such as assessing how care and treatment varies by the presence of various social needs. Second, these data only include primary care patients, so findings may not be generalizable to those who do not seek care or receive care outside of primary care. However, the objective was to understand the association between needs and health outcomes for the clinical population as this is the population on which the health system would intervene. Similarly, these data only include patients who completed a screener, which may not be generalizable to the general patient population as clinics selected their target population. However, a previous analysis found similar patterns of social needs after accounting for predictors of completing the screener.27 Additionally, the screener relies on self-reporting, so results may be biased or underestimated if patients are unable or hesitant to answer accurately. However, from a pragmatic perspective, if interventions will be based on the results of such screening, this is the very data that should be used. In a previous analysis using screening data from the same health care system, the authors found that living in public housing and in higher poverty areas were significantly associated with the presence of social needs. Additionally, in weighted analyses that accounted for predictors of being screened, the proportion of patients with social needs, the ranking of individual social needs and the patterns for specific subgroups remained similar to the unweighted analyses.27 Finally, the study uses clinical data, which is prone to data entry errors and other forms of systematic and random measurement error.
Conclusions
Screening for social needs in the primary care setting provides data that can be used to improve our understanding of how social needs impact health, which can inform mitigation strategies. Results indicate there is a positive and graded association between the burden of social needs and specific chronic conditions, although the association varies by condition and is strongest for behavioral risk factors and mental health. This finding suggests that mental health-related outcomes may be the most sensitive to the presence of needs, at least in the short term. Results also suggest that healthcare transportation challenges are more strongly associated with chronic conditions than others, highlighting the role of addressing healthcare transportation to prevent and manage chronic conditions. These findings suggest that health systems should consider the disparate impact that social needs have on managing chronic conditions and the practical implications for health care delivery, the design of interventions and the allocation of social service resources. Finally, while the findings of this study can be used to inform interventions and care delivery more broadly, they also support the utility of health systems collecting patient-level social needs data to understand their own patients’ needs.
Table 3.
Unadjusted and adjusted prevalence ratio for each outcome by individual social need among screened Montefiore patients, April 2018-December 2019
| Housing | Access to Healthcare | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Food Insecurity | Quality | Instability | Health Transportation | Health Cost | Getting Along | Utilities Cost | Legal | Care Need | Interpersonal Violence | |
| Risk Factors | ||||||||||
| Smokinga | ||||||||||
| Model 1b | 2.18 (1.97, 2.41) | 1.66 (1.48, 1.87) | 2.18 (1.95, 2.43) | 2.34 (2.11, 2.60) | 1.91 (1.70, 2.15) | 1.99 (1.76, 2.25) | 1.97 (1.70, 2.29) | 2.24 (1.94, 2.58) | 1.31 (1.07, 1.59) | 2.02 (1.65, 2.46) |
| Model 2c | 1.74 (1.58, 1.91) | 1.39 (1.25, 1.54) | 1.70 (1.53, 1.88) | 1.82 (1.66, 1.99) | 1.58 (1.42, 1.75) | 1.63 (1.47, 1.82) | 1.58 (1.39, 1.79) | 1.70 (1.51, 1.92) | 1.26 (1.04, 1.52) | 1.59 (1.34, 1.90) |
| Model 3d | 1.28 (1.14, 1.45) | 1.01 (0.89, 1.15) | 1.21 (1.06, 1.38) | 1.41 (1.25, 1.58) | 1.04 (0.91, 1.18) | 1.23 (1.09, 1.39) | 1.13 (0.98, 1.30) | 1.15 (0.99, 1.33) | 0.85 (0.69, 1.04) | 1.00 (0.82, 1.20) |
| Alcohol/drug use disorder:e | ||||||||||
| Model 1b | 2.24 (1.98, 2.53) | 1.96 (1.72, 2.25) | 2.20 (1.92, 2.51) | 2.94 (2.62, 3.31) | 1.96 (1.70, 2.26) | 1.88 (1.61, 2.20) | 1.90 (1.57, 2.28) | 2.63 (2.23, 3.09) | 1.57 (1.25, 1.96) | 2.08 (1.63, 2.65) |
| Model 2c | 1.79 (1.60, 1.99) | 1.66 (1.47, 1.88) | 1.65 (1.46, 1.87) | 2.22 (2.00, 2.47) | 1.63 (1.43, 1.86) | 1.60 (1.39, 1.86) | 1.51 (1.26, 1.81) | 1.92 (1.65, 2.24) | 1.50 (1.20, 1.88) | 1.65 (1.33, 2.03) |
| Model 3d | 1.22 (1.05, 1.42) | 1.20 (1.04, 1.39) | 1.05 (0.89, 1.24) | 1.84 (1.59, 2.13) | 0.94 (0.79, 1.11) | 1.12 (0.93, 1.34) | 1.03 (0.85, 1.25) | 1.25 (1.05, 1.50) | 0.95 (0.75, 1.21) | 0.97 (0.76, 1.24) |
| Obesityf | ||||||||||
| Model 1b | 1.07 (1.00, 1.14) | 1.11 (1.04, 1.19) | 1.04 (0.96, 1.12) | 1.12 (1.04, 1.20) | 1.19 (1.11, 1.28) | 1.13 (1.04, 1.22) | 1.20 (1.10, 1.32) | 1.06 (0.96, 1.17) | 1.09 (0.98, 1.21) | 1.08 (0.95, 1.24) |
| Model 2c | 1.02 (0.97, 1.07) | 1.03 (0.98, 1.09) | 1.00 (0.95, 1.06) | 1.07 (1.02, 1.12) | 1.14 (1.08, 1.19) | 1.07 (1.02, 1.13) | 1.13 (1.06, 1.21) | 1.01 (0.94, 1.09) | 1.09 (1.01, 1.18) | 1.03 (0.94, 1.13) |
| Model 3d | 0.96 (0.90, 1.02) | 1.01 (0.96, 1.07) | 0.95 (0.89, 1.02) | 1.02 (0.97, 1.08) | 1.13 (1.07, 1.19) | 1.05 (0.99, 1.11) | 1.12 (1.04, 1.20) | 0.96 (0.89, 1.05) | 1.06 (0.98, 1.15) | 0.99 (0.89, 1.09) |
| Chronic Disease | ||||||||||
| Hypertensiong | ||||||||||
| Model 1b | 1.06 (1.00, 1.13) | 1.13 (1.06, 1.21) | 1.07 (0.99, 1.15) | 1.17 (1.09, 1.25) | 1.07 (0.99, 1.15) | 0.86 (0.79, 0.94) | 1.03 (0.93, 1.13) | 1.10 (1.00, 1.21) | 1.09 (0.98, 1.21) | 0.99 (0.87, 1.13) |
| Model 2c | 1.08 (1.04, 1.13) | 1.09 (1.05, 1.14) | 1.08 (1.03, 1.13) | 1.12 (1.07, 1.16) | 1.12 (1.07, 1.17) | 1.06 (1.01, 1.12) | 1.08 (1.02, 1.15) | 1.08 (1.02, 1.14) | 1.08 (1.01, 1.15) | 1.07 (0.99, 1.16) |
| Model 3d | 1.02 (0.97, 1.06) | 1.05 (1.01, 1.10) | 1.01 (0.96, 1.07) | 1.06 (1.01, 1.11) | 1.06 (1.00, 1.11) | 1.01 (0.95, 1.07) | 1.02 (0.96, 1.09) | 1.00 (0.94, 1.07) | 1.02 (0.96, 1.09) | 0.99 (0.91, 1.09) |
| Diabetesh | ||||||||||
| Model 1b | 1.18 (1.09, 1.28) | 1.24 (1.14, 1.35) | 1.12 (1.03, 1.23) | 1.35 (1.24, 1.47) | 1.19 (1.08, 1.30) | 0.91 (0.81, 1.01) | 1.12 (0.99, 1.26) | 1.22 (1.08, 1.37) | 1.18 (1.03, 1.34) | 1.09 (0.92, 1.29) |
| Model 2c | 1.17 (1.10, 1.25) | 1.16 (1.09, 1.23) | 1.10 (1.02, 1.18) | 1.24 (1.16, 1.32) | 1.21 (1.12, 1.31) | 1.12 (1.02, 1.22) | 1.17 (1.07, 1.28) | 1.15 (1.05, 1.26) | 1.11 (1.01, 1.23) | 1.15 (1.01, 1.31) |
| Model 3d | 1.05 (0.97, 1.14) | 1.08 (1.01, 1.16) | 0.96 (0.88, 1.05) | 1.15 (1.06, 1.24) | 1.08 (0.99, 1.19) | 1.02 (0.92, 1.12) | 1.06 (0.96, 1.17) | 1.03 (0.92, 1.14) | 1.00 (0.90, 1.12) | 1.01 (0.87, 1.10) |
| Asthmai | ||||||||||
| Model 1b | 1.37 (1.25, 1.50) | 1.79 (1.64, 1.96) | 1.36 (1.22, 1.50) | 1.70 (1.55, 1.86) | 1.63 (1.48, 1.80) | 1.38 (1.24, 1.54) | 1.53 (1.35, 1.74) | 1.53 (1.35, 1.74) | 1.33 (1.15, 1.55) | 1.42 (1.19, 1.70) |
| Model 2c | 1.26 (1.16, 1.36) | 1.54 (1.43, 1.65) | 1.29 (1.18, 1.41) | 1.51 (1.40, 1.63) | 1.50 (1.39, 1.62) | 1.25 (1.14, 1.38) | 1.43 (1.28, 1.59) | 1.43 (1.29, 1.58) | 1.24 (1.09, 1.39) | 1.26 (1.08, 1.47) |
| Model 3d | 0.95 (0.86, 1.05) | 1.37 (1.27, 1.48) | 0.98 (0.88, 1.09) | 1.25 (1.14, 1.37) | 1.24 (1.12, 1.36) | 1.03 (0.93, 1.15) | 1.18 (1.05, 1.33) | 1.11 (0.98, 1.25) | 0.98 (0.86, 1.11) | 0.94 (0.80, 0.00) |
| Mental/behavioral | ||||||||||
| Depressionj | ||||||||||
| Model 1b | 1.99 (1.86, 2.12) | 1.88 (1.75, 2.02) | 2.01 (1.87, 2.16) | 2.10 (1.96, 2.25) | 1.85 (1.71, 1.99) | 2.62 (2.44, 2.82) | 1.85 (1.68, 2.04) | 2.07 (1.89, 2.28) | 1.83 (1.64, 2.04) | 2.58 (2.30, 2.89) |
| Model 2c | 1.70 (1.62, 1.79) | 1.56 (1.47, 1.65) | 1.79 (1.69, 1.88) | 1.75 (1.66, 1.84) | 1.65 (1.56, 1.75) | 2.34 (2.23, 2.45) | 1.64 (1.52, 1.76) | 1.86 (1.74, 1.98) | 1.63 (1.51, 1.77) | 2.16 (2.00, 2.34) |
| Model 3d | 1.17 (1.10, 1.25) | 1.11 (1.04, 1.19) | 1.16 (1.09, 1.24) | 1.22 (1.14, 1.30) | 1.07 (1.00, 1.15) | 1.82 (1.71, 1.93) | 1.11 (1.02, 1.20) | 1.09 (1.01, 1.19) | 1.08 (0.99, 1.18) | 1.16 (1.05, 1.27) |
| Elevated PHQ2k | ||||||||||
| Model 1b | 3.02 (2.81, 3.24) | 2.66 (2.46, 2.87) | 3.03 (2.81, 3.27) | 3.04 (2.82, 3.27) | 2.80 (2.59, 3.03) | 3.66 (3.38, 3.95) | 2.64 (2.38, 2.92) | 2.94 (2.66, 3.24) | 2.69 (2.41, 3.01) | 3.61 (3.20, 4.07) |
| Model 2c | 2.56 (2.42, 2.72) | 2.22 (2.09, 2.36) | 2.63 (2.47, 2.79) | 2.51 (2.36, 2.67) | 2.48 (2.32, 2.64) | 3.21 (3.03, 3.40) | 2.31 (2.13, 2.50) | 2.56 (2.38, 2.75) | 2.39 (2.18, 2.61) | 3.04 (2.80, 3.30) |
| Model 3d | 1.40 (1.30, 1.51) | 1.28 (1.18, 1.39) | 1.31 (1.21, 1.43) | 1.31 (1.21, 1.42) | 1.25 (1.15, 1.36) | 1.98 (1.83, 2.14) | 1.18 (1.08, 1.30) | 1.05 (0.96, 1.16) | 1.22 (1.10, 1.35) | 1.14 (1.01, 1.20) |
Defined as those reporting being a current smoker in latest smoking survey in 1 year prior to the screener; excludes 7.5% not surveyed;
Unadjusted;
Adjusted for age, sex, race/ethnicity, preferred language, health insurance, block-group poverty and public housing status;
Adjusted for each individual social need, age, sex, race/ethnicity, preferred language, health insurance, block-group poverty and public housing status;
Defined as those with a diagnosis for the following: F11.x–F16.x, F18.x, F19.x, Z71.5, Z72.2, F10, E52, G62.1, I42.6, K29.2, K70.0, K70.3, K70.9, T51.x, Z50.2, Z71.4, Z72.1 in two years prior to screener;
Defined as those with BMI≥30 kg/m2, based on latest BMI value in 1 year prior to screener; excludes 2.1% without BMI measurement;
Defined as those with I10.x diagnosis in two years prior to screener;
Defined as those with E10.X, E11.X, E12.X, E13.X, E14.X diagnosis codes in two years prior to screener;
Defined as those with J45.X diagnosis codes in two years prior to screener;
Defined as those with F20.4, F31.3–F31.5, F32.x, F33.x, F34.1, F41.X, F43.2 diagnosis codes in two years prior to screener;
Defined as those with a score ≥2, based on latest PHQ-2 score in 1 year prior to screener; excludes 7.5% of sample not screened in year prior
Highlights.
This study uses patient-level social needs screener data and clinical data.
This study includes screener results from 33,550 adult primary care patients.
We find a positive, graded association between social needs and chronic conditions.
This association varies by condition but is strongest for mental health.
Healthcare transportation needs are most strongly related to chronic conditions.
Acknowledgements
The authors are grateful to those from Montefiore Medical Group who helped develop and implement the screening tool. Dr. Chambers is supported by grants from the National Heart, Lung, and Blood Institute (K01HL125466 and 1R03HL140265) and by a grant from the National Institutes of Diabetes and Digestive and Kidney Diseases (P30 DK111022 and R01 DK121896). Dr. Fiori is supported by grants from the Doris Duke Charitable Foundation (2018169) and the Agency for Health Care Research and Quality, HHS (K12HS026396). Colin Rehm was with Montefiore Medical Center and the Albert Einstein College of Medicine at the time this study was conducted. He is currently an employee of PepsiCo, Inc.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No other financial disclosures were reported by the authors of this paper and the authors declare no conflicts of interest.
References
- 1.National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP). About Chronic Diseases. Published 2019. Accessed July 7, 2020. https://www.cdc.gov/chronicdisease/about/index.htm
- 2.National Academies of Sciences, Engineering and M. Integrating Social Care into the Delivery of Health Care. National Academies Press; 2019. doi: 10.17226/25467 [DOI] [PubMed] [Google Scholar]
- 3.Cockerham WC, Hamby BW, Oates GR. The Social Determinants of Chronic Disease. Am J Prev Med. 2017;52(1S1):S5–S12. doi: 10.1016/j.amepre.2016.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaw M. Housing and public health. Annu Rev Public Health. 2004;25:397–418. 10.1146/annurev.publhealth.25.101802.123036 [DOI] [PubMed] [Google Scholar]
- 5.Seligman HK, Laraia BA, Kushel MB. Food Insecurity Is Associated with Chronic Disease among Low-Income NHANES Participants. J Nutr. 2010;140(2):304–310. doi: 10.3945/jn.109.112573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berkowitz SA, Hulberg AC, Placzek H, et al. Mechanisms Associated with Clinical Improvement in Interventions That Address Health-Related Social Needs: A Mixed-Methods Analysis. Popul Health Manag. 2019;22(5):399–405. doi: 10.1089/pop.2018.0162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gurewich D, Garg A, Kressin NR. Addressing Social Determinants of Health Within Healthcare Delivery Systems: a Framework to Ground and Inform Health Outcomes. J Gen Intern Med. 2020;35(5):1571–1575. doi: 10.1007/s11606-020-05720-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gottlieb LM, Wing H, Adler NE. A Systematic Review of Interventions on Patients’ Social and Economic Needs. Am J Prev Med. 2017;53(5):719–729. doi: 10.1016/j.amepre.2017.05.011 [DOI] [PubMed] [Google Scholar]
- 9.Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: A longitudinal cohort study. Am J Manag Care. 2018;24(9):399–404. [PMC free article] [PubMed] [Google Scholar]
- 10.Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: A predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. 2013;103(11):2056–2062. doi: 10.2105/AJPH.2013.301261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burgard SA, Seefeldt KS, Zelner S. Housing instability and health: Findings from the Michigan recession and recovery study. Soc Sci Med. 2012;75(12):2215–2224. doi: 10.1016/j.socscimed.2012.08.020 [DOI] [PubMed] [Google Scholar]
- 12.Thompson T, McQueen A, Croston M, et al. Social Needs and Health-Related Outcomes Among Medicaid Beneficiaries. Heal Educ Behav. 2019;46(3):436–444. doi: 10.1177/1090198118822724 [DOI] [PubMed] [Google Scholar]
- 13.Blazer DG, Sachs-Ericsson N, Hybels CF. Perception of unmet basic needs as a predictor of depressive symptoms among community-dwelling older adults. Journals Gerontol - Ser A Biol Sci Med Sci. 2007;62(2):191–195. doi: 10.1093/gerona/62.2.191 [DOI] [PubMed] [Google Scholar]
- 14.Blosnich JR, Marsiglio MC, Dichter ME, et al. Impact of Social Determinants of Health on Medical Conditions Among Transgender Veterans. Am J Prev Med. 2017;52(4):491–498. doi: 10.1016/j.amepre.2016.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prather AA, Gottlieb LM, Giuse NB, et al. National Academy of Medicine Social and Behavioral Measures: Associations With Self-Reported Health. Am J Prev Med. 2017;53(4):449–456. doi: 10.1016/j.amepre.2017.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blazer DG, Sachs-Ericsson N, Hybels CF. Perception of unmet basic needs as a predictor of depressive symptoms among community-dwelling older adults. Journals Gerontol - Ser A Biol Sci Med Sci. 2007;62(2):191–195. doi: 10.1093/gerona/62.2.191 [DOI] [PubMed] [Google Scholar]
- 17.Berkowitz SA, Catherine Hulberg A, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177(2):244–252. doi: 10.1001/jamainternmed.2016.7691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pantell MS, Prather AA, Downing JM, Gordon NP, Adler NE. Association of Social and Behavioral Risk Factors With Earlier Onset of Adult Hypertension and Diabetes. JAMA Netw open. 2019;2(5):e193933. doi: 10.1001/jamanetworkopen.2019.3933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fraze T, Lewis VA, Rodriguez HP, Fisher ES. Housing, transportation, and food: How ACOs seek to improve population health by addressing nonmedical needs of patients. Health Aff. 2016;35(11):2109–2115. doi: 10.1377/hlthaff.2016.0727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee Josh; Korba C. Social Determinants of Health: How Are Hospitals and Health Systems Investing in and Addressing Social Needs? New York; 2017. https://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-lshc-addressing-social-determinants-of-health.pdf. [Google Scholar]
- 21.Bachrach D, Pfister H, Wallis K, Lipson M, Manatt Health Solutions. Addressing Patients’ Social Needs: An Emerging Business Case for Provider Investment. https://www.commonwealthfund.org/publications/fund-reports/2014/may/addressing-patients-social-needs-emerging-business-case-provider. Published January 8, 2014. Accessed April 27, 2019.
- 22.Krieger N Health equity and the fallacy of treating causes of population health as if they sum to 100%. Am J Public Health. 2017;107(4):541–549. doi: 10.2105/AJPH.2017.303655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adler NE, Cutler DM, Fielding JE, et al. Addressing Social Determinants of Health and Health Disparities: A Vital Direction for Health and Health Care. NAM Perspect. 2016;6(9). doi: 10.31478/201609t [DOI] [Google Scholar]
- 24.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable Health Communities — Addressing Social Needs through Medicare and Medicaid. N Engl J Med [DOI] [PubMed] [Google Scholar]
- 25.Braveman P, Gottlieb L. The Social Determinants of Health: It’s Time to Consider the Causes of the Causes. Public Health Rep. 2014;129(1_suppl2):19–31. doi: 10.1177/00333549141291S206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Health Leads. Social Needs Screening Toolkit. https://nopren.org/wp-content/uploads/2016/12/Health-Leads-Screening-Toolkit-July-2016.pdf. Published 2016.
- 27.Heller CG, Parsons AS, Chambers EC, Fiori KP, Rehm CD. Social Risks Among Primary Care Patients in a Large Urban Health System. Am J Prev Med. 2020;58(4):514–525. doi: 10.1016/j.amepre.2019.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gregory CA, Coleman-Jensen A. Economic Research Service Economic Research Report Number 235 Food Insecurity, Chronic Disease, and Health Among Working-Age Adults. 2017;(235). www.ers.usda.gov [Google Scholar]
- 29.Waitzkin H, Getrich C, Heying S, et al. Promotoras as mental health practitioners in primary care: A multi-method study of an intervention to address contextual sources of depression. J Community Health. 2011;36(2):316–331. doi: 10.1007/s10900-010-9313-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miller-Archie SA, Walters SC, Singh TP, Lim S. Impact of supportive housing on substance use–related health care utilization among homeless persons who are active substance users. Ann Epidemiol. 2019;32:1–6.e1. doi: 10.1016/j.annepidem.2019.02.002 [DOI] [PubMed] [Google Scholar]
- 31.Montefiore Medical Center. Community Health Needs and Implementation Strategy 2019–2021. Published 2019. Accessed June 17, 2020. https://www.montefiore.org/documents/communityservices/MMC-Community-Health-Needs-Report-2019-2021.pdf
- 32.Arroll B, Goodyear-Smith F, Crengle S, et al. Validation of PHQ-2 and PHQ-9 to Screen for Major Depression in the Primary Care Population. Ann Fam Med. 2010;8(4):348–353. doi: 10.1370/afm.1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Quan H, Sundararajan V, Halfon P, et al. Coding Algorithms for Defining Comorbidities in ICD-9-CM and ICD-10 Administrative Data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83 [DOI] [PubMed] [Google Scholar]
- 34.Bellin E, Fletcher DD, Geberer N, Islam S, Srivastava N. Democratizing Information Creation From Health Care Data for Quality Improvement, Research, and Education—The Montefiore Medical Center Experience. Acad Med. 2010;85(8):1362–1368. doi: 10.1097/ACM.0b013e3181df0f3b [DOI] [PubMed] [Google Scholar]
- 35.U.S. Census Bureau. American Community Survey: Areas Published. https://www.census.gov/programs-surveys/acs/geography-acs/areas-published.html. Published 2018.
- 36.Caleyachetty R, Echouffo-Tcheugui JB, Muennig P, Zhu W, Muntner P, Shimbo D. Association between cumulative social risk and ideal cardiovascular health in US adults: NHANES 1999–2006. Int J Cardiol. 2015;191:296–300. doi: 10.1016/j.ijcard.2015.05.007 [DOI] [PubMed] [Google Scholar]
- 37.Syed ST, Gerber BS, Sharp LK. Traveling Towards Disease. J Community Health. 2013;38(5):976–993. doi: 10.1007/s10900-013-9681-1.Traveling [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wallace R, Hughes-Cromwick P, Mull H, Khasnabis S. Access to Health Care and Nonemergency Medical Transportation. Transp Res Rec J Transp Res Board. 2005;1924(1):76–84. doi: 10.1177/0361198105192400110 [DOI] [Google Scholar]
- 39.Fiori KP, Heller CG, Rehm CD, et al. Unmet Social Needs and No-Show Visits in Primary Care in a US Northeastern Urban Health System, 2018–2019. Am J Public Health. 2020;110(S2):S242–S250. doi: 10.2105/AJPH.2020.305717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buajitti E, Frank J, Watson T, Kornas K, Rosella LC. Changing relative and absolute socioeconomic health inequalities in Ontario, Canada: A population-based cohort study of adult premature mortality, 1992 to 2017. PLoS One. 2020;15(4):e0230684. Published 2020 Apr 2. doi: 10.1371/journal.pone.0230684 [DOI] [PMC free article] [PubMed] [Google Scholar]


