Introduction
In the United States, approximately 19 million ambulatory oncology visits occur annually (Centers for Disease Control and Prevention, 2019). Evidence from the National Cancer Institute (2020) estimates that approximately 15.7 million people live with cancer in the US. Meanwhile, an increasing demand for oncology services is shown by growing trends in vertical practice consolidation (Alpert et al., 2017). The 2018 American Society for Clinical Oncology (ASCO) State of Oncology Practice in America report estimated that 25% of US oncology practices grew in size from 2016 to 2017, with half of those practices opening a new site. The ambulatory oncology market expansion presents a critical opportunity to advance our understanding of patient safety and clinician work processes, such as team communication during chemotherapy infusion and care planning.
In light of these developments, there is very little attention regarding how the physical space in which oncology clinicians deliver care uniquely structures safe chemotherapy delivery, particularly for urgent clinical needs. As opposed to operating rooms, or other high-risk clinical procedure areas, few standards exist to guide the design of ambulatory oncology practices (Jalalianhosseini et al., 2020), given the heterogeneity in clinic designs, patient volume, and clinician staffing models (de Matos et al., 2020; Huang et al., 2018). Within this context, a better understanding of the physical layout and utilization of space may help improve the patient experience, promote patient safety, and facilitate efficient cancer care delivery.
Previous research studies provide insight into how clinical oncology teams can achieve a high-value, patient-centered environment. Effective clinician communication, coordination, making the patient feel “known,” and flexible environments facilitate accessibility, engagement, and wayfinding (Blayney et al., 2018; Grover et al., 2018; Sadek & Willis, 2019). Oncology practice leaders may struggle with achieving a patient-centered, optimally safe clinical environment as treatment modalities evolve and the demand for oncology care increases. With these emerging challenges and knowledge gaps, the purpose of this study was to examine clinician perspectives on the influences of physical layouts and space as a facilitator or barrier to patient safety and clinician communication in ambulatory oncology practices. The research team aims to provide new insight to inform the design and allocation of space that aids in more successful patient safety and clinician communication in ambulatory oncology practices.
Methods
Study Design
This study employed a mixed methods design with sequential data collection: a quantitative survey phase followed by a qualitative phase (Creswell, 2018; Manojlovich et al., 2020), as shown in Figure 1. First, researchers aimed to understand the relationship between patient safety and clinician communication with quantitative data from oncology clinicians. Next, researchers aimed to understand how oncology clinicians engaged in safety organizing behaviors and communication practices across various practice layouts with qualitative data. Then, researchers integrated the data to compare patient safety and clinician communication findings at practices with various layouts. This study was one component of a multi-site, multi-aim investigation into the relationship between patient safety, electronic health record efficacy (EHRs), and communication technologies in ambulatory oncology practices (Lafferty et al., 2020; Patel et al., 2019).
Figure 1.
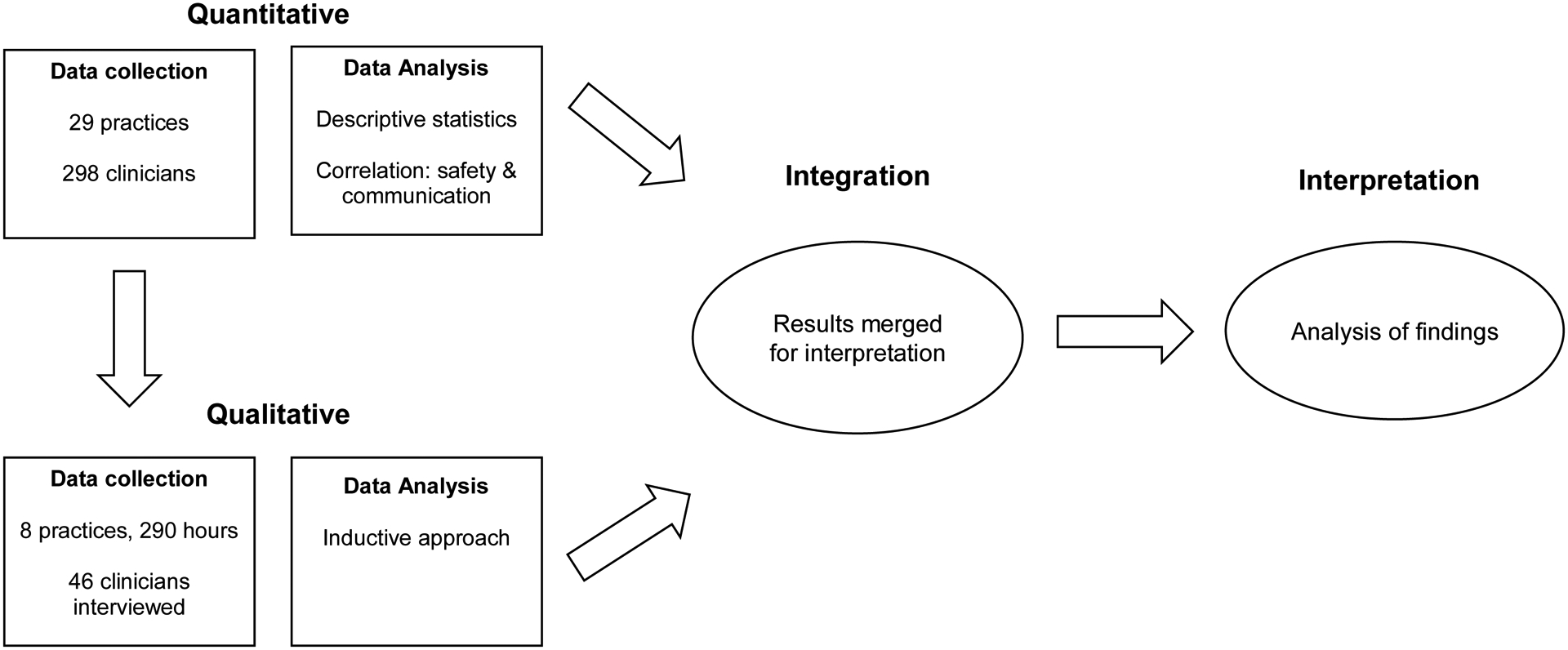
Mixed methods study design.
Few studies have examined the significance of physical layouts in ambulatory oncology practices; most literature has been published on inpatient settings (Bloom et al., 2015; Gharaveis et al., 2018; Høybye, 2013). The research team selected a mixed method design to investigate how physical layouts were barriers or facilitators to safe care practices, which consisted of clinician safety organizing behaviors and communication. The Institutional Review Board of the home institution deemed the quantitative phase exempt from review and approved the subsequent qualitative phase.
Setting, sampling, and recruitment
The study began by recruiting twenty-nine ambulatory oncology practices that participate in a statewide quality improvement program in the United States. Participating practices that provide outpatient chemotherapy were recruited at a regularly scheduled meeting of the quality improvement collaborative, followed by e-mail invitations to practice leaders. During this process, the research team identified and trained a volunteer at each practice to serve as a site study champion. This study champion was an on-site employee responsible for assisting the research team in distributing surveys, returning completed surveys, and handling any issues that may have arisen.
Out of the original twenty-nine study sites, eight were chosen for inclusion in the qualitative phase. Practices were selected using sequential sampling, informed by clinician survey responses, to maximize organizational context variation. Practices in this sample were a mix of privately-owned practices and practices embedded within integrated health care systems. Additionally, these practices were a mix of small, freestanding community oncology clinics and larger settings adjacent to community hospitals and academic medical centers. The number of chairs in the infusion centers ranged from seven to thirty-four. These diverse contextual factors as part of the original design of the selected ambulatory oncology practices affected chemotherapy delivery for clinicians as well as the research teams’ data collection processes.
The sample of participants consisted of clinicians employed at the ambulatory oncology practices, including registered nurses, physicians, and advanced practice providers (i.e., physician assistants, nurse practitioners). For interviews, the sample primarily consisted of chemotherapy-certified oncology nurses working in the ambulatory infusion center. Some prescribers (e.g., physicians and advanced practice providers [APPs]) were not available for interviews due to patient care responsibilities. For the quantitative and qualitative phases, clinicians’ inclusion criteria were: practiced at least a 0.5 full-time equivalent in the setting, currently licensed for their position, and completed their orientation. Exclusion criteria were: worked under contract for a travel or temporary staffing agency or expressed hesitation in study procedures.
Sample Characteristics
Across the entire project, 297 surveys from clinicians were available for analysis (68% response rate [76% for nurses, and 59% for physicians and APPs]). However, eight practices participated in both the clinician survey and qualitative phase. Therefore, 56 surveys from clinicians (18.9% of the entire study sample) were retained for this study’s analysis. In the qualitative phase, researchers spent 290 hours on site. They interviewed 46 clinicians: 40 individually and six during two separate small group interviews.
Quantitative Measures
The researchers operationalized patient safety and clinician communication with previously validated instruments as actions consistent with safety culture (i.e., safety organizing) and clinician communication satisfaction (i.e., clinician communication), respectively.
Safety organizing.
The Safety Organizing Scale (SOS) asked clinicians about the degree to which they engage in behaviors and practices consistent with a safety culture. This scale consisted of nine items scored on a Likert scale (1, “not at all” to 7, “to a very great extent”) (Vogus & Sutcliffe, 2007). Sample items included: the degree to which mistakes are discussed and learned from; discussion of how errors could be prevented in the future; time spent identifying potential problem areas; and the extent to which clinician expertise and unique skills are utilized. The SOS has good reliability and validity. The internal consistency reliability Cronbach alpha for this study was 0.88.
Clinician communication.
The clinician communication scale asked clinicians to report their satisfaction with relationships and communication between nurses, physicians, and APPs. With the permission of the developer (Shortell et al., 1991), the researchers adapted the scale for this study. The instrument measured four aspects of communication with separate subscales: timeliness, understanding, accuracy, openness. The four subscales were averaged and summed to yield a final score. The scale consisted of 21 items, scored on a Likert scale (1, “strongly disagree” to 5, “strongly agree”). Sample items on the survey included: the degree to which it is easy for nurses to talk with physicians; the openness of communication between nurses and physicians; and physicians having a good understanding of nursing objectives, among other items. The internal consistency reliability Cronbach alpha in our sample was 0.92.
Quantitative Data Collection
Quantitative data collection occurred in the first phase of the study, from May 2017 to October 2017, with methods previously published (Patel et al., 2019). Briefly, the trained, volunteer study champion for each site identified eligible nurse and prescriber (physician, APP) participants and provided them with questionnaires for completion. Two separate survey formats were distributed by study champions to nurses and prescribers, respectively, with the different surveys tailored to each role’s specific responsibilities. Each eligible clinician received a survey packet with a cover letter, the appropriate role-based survey, a $10 cash incentive, and a pre-addressed, stamped envelope to return the completed survey. The on-site champion used verbal and electronic reminders to assure that clinicians completed surveys in a manner consistent with the study protocol. Study champions mailed completed surveys back to the research team.
Qualitative Data Collection
Qualitative data were collected in the second phase of the study from March 2018 to November 2018 through on-site observations followed by shadowing of individual clinicians and interviews. The research team spent five days at each site selected for the qualitative phase. One researcher was present at every site, with one to two additional researchers assisting at three sites.
Qualitative data collection was an iterative process. Research team members met weekly to conduct a rapid assessment of data after each site visit concluded to determine if there were specific topics of interest that required additional focus. The effect that the site’s layout had on clinicians’ communication and safety behaviors was not identified a priori but became a focal point after field-testing research procedures at the study pilot site. After the pilot site visit, at each site the researchers performed initial observations paying close attention to the site’s physical layout and floorplan. Additionally, researchers included specific questions about layout and space in the interview guide.
Observations occurred throughout the ambulatory oncology practice (e.g., chemotherapy infusion areas, exam areas, and ancillary office spaces). Researchers met before beginning data collection to discuss data collection processes making a note to pay attention to each practice’s floorplan in the initial observations. Subsequent observations provided a closer examination of day-to-day patient care delivery and organizational processes offering an additional focus on clinicians’ communication behaviors. Conducting observations throughout the entire ambulatory oncology practice allowed research team members to gain insight into the specific ways in which infusion nurses interacted with one another as well as with providers (physicians and APPs) as well as understanding how these behaviors occurred in and were influenced by the physical space in which they took place. Researchers focused on observations during the earlier days of data collection to gain a holistic, nuanced understanding of the clinicians’ workflow and task-specific behaviors.
Researchers also shadowed individual clinicians (nurses, physicians, and APPs). Shadowing is a specific type of observation where the researcher follows a clinician closely for several hours to elicit a more nuanced understanding of each role’s individualized patient care responsibilities and workflow. Researchers shadowed clinicians to gain firsthand insight into how they navigated daily schedules, clinical duties, and physical space to communicate and interact with other clinicians to ensure safe and timely patient care. Shadowing notes captured researchers’ impressions of how clinicians functioned as a team as well as direct conversation with clinicians about their particular workflow and daily activity. Observation and shadowing (McDonald, 2005) data were recorded via hand-written field notes, which were subsequently transferred to electronic form.
Interviews were conducted later in the week. The interview guide was developed to elicit clinicians’ perspectives on barriers and facilitators towards patient safety and communication, to identify site-specific challenges, and to ask for recommendations to help improve patient safety and communication at each site. Data gathered from observations were used in the interviews, alongside the interview guide, to follow-up on site-specific issues allowing for more in-depth discussions with clinicians. Each interview was audio-recorded and subsequently transcribed verbatim by a third-party vendor.
Quantitative Data Analysis
The study coordinator supervised manual, double-entry survey data entry procedures into a secure database. The research team then compared data at the practice-level by calculating tertiles (high, medium, or low) on the safety organizing and clinician communication measures, including identifying outliers. Researchers used descriptive and parametric correlation statistics with continuous measures to examine the relationships between safety organizing and clinician communication. Stata version 15 (Stata Corp, College Station, TX) software was used for quantitative analyses.
Qualitative Analysis
Researchers utilized an inductive analytical approach to generate hypotheses within the data (Kyngäs et al., 2019). The research team first created a codebook based on the dominant patterns and abstract categories emerging from interview transcripts and field notes. This process included researchers independently identifying recurring topics within the data that would subsequently become codes. Researchers frequently met during codebook development to discuss any issues and reach a consensus on code definitions and application. Codes focused on various topics to capture the nuances within the data. Examples of codes include clinician tasks, communication, EHR, physical environment, and patient safety. Once the codebook was finalized, researchers applied line-by-line coding to categorize all field notes and interview data using the qualitative data software Atlas.ti version 8 (Atlas.ti Scientific Software Development GmbH, Berlin, Germany).
Data Integration
Following initial quantitative and qualitative analyses, the research team integrated the safety organizing and clinician communication outcomes at each site by triangulating findings of both datasets in tables for side-by-side comparisons of study variables to identify similarities and differences in the data (Guetterman et al., 2015). Researchers compared qualitative data that linked physical layouts to communication and safety behaviors to the site’s safety organizing and clinician communication scores. Once the research team had identified the factors within the qualitative data contributing to an association between physical layout and safety organizing and clinician communication, additional thematic content analysis was conducted to ensure that all representative data were identified.
Since physical layout was not a measure on the clinician survey, the aim of this integrated approach was to demonstrate how clinicians at sites with high and low quantitative scores discussed safety and communication in interviews and if they matched with the quantitative scores the sites received. It is important to note that not all qualitative data nor any particular layout design uniformly matched the quantitative scores. These findings are presented in a manner that aims to show the variation between how data are reported quantitatively and what factors may influence these scores in ways not illuminated solely by one method or the other. The aim was to add more detailed depth (i.e., the influence that layout has) on each site’s quantitative depiction (i.e., safety organizing and clinician communication scores).
Results
Table 1 lists information regarding the descriptive characteristics, clinician-reported performance in safety organizing behaviors, and clinician communication and qualitative observations of each site from the researchers’ perspectives of the clinics. The participant’s demographic characteristics from the larger, multi-site study were previously published (Patel et al., 2019).
Table 1.
Ambulatory oncology settings’ characteristics, performance of safety and communication, and selected observation findings.
| Descriptive Characteristics | Quantitative Measures | Qualitative Measures, Observation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Safety Organizing | Clinician Communication | |||||||||
| Site | Practice affiliation | No. Infusion Chairs | No. nurse personnel daily | Mean (SD) | Performance | Mean (SD) | Performance | Floorplan & nurses station description | Direct line of sight | Infusion center connected to clinic |
| 1 | Integrated network | 15 | 6 | 5.10 (0.83) | Low | 14.0 (1.69) | Low | 2 narrow rectangular rooms, 1 nurse station | No | No |
| 2 | Community collaborative | 34 | 11 | 5.66 (0.96) | High | 16.1 (1.91) | Medium | L-shape, 5 pods | Yes | Yes |
| 3 | Regional | 14 | 5 | 4.94 (1.19) | Low | 13.9 (1.95) | Low | L-shape, 1 nurse station | No | Yes |
| 4 | Private practice | 17 | 6 | 6.22 (0.83) | High | 17.0 (1.70) | High | Rectangular, 1 nurse station | Yes | Yes |
| 5 | Integrated network | 7 | 2–3 | 6.20 (0.68) | High | 16.6 (1.65) | High | Narrow rectangular, 1 nurse station | No | Yes |
| 6 | Regional | 16 | 4–5 | 5.69 (0.76) | High | 12.8 (3.31) | Low | L-shape, 1 nurse station | No | No |
| 7 | Regional | 10 | 2–3 | 6.17 (0.40) | High | 18.1 (1.14) | High | Wide rectangular, 1 nurse station | No | Yes |
| 8 | Academic health system | 10 | 6 | 4.35 (0.71) | Low | 13.4 (2.60) | Low | Wide rectangular, 1 nurse station | Yes | Yes |
As shown in Table 1, the infusion areas of each site were labeled as either L-shaped or rectangular. The infusion areas featured either a single workstation with computers for nurses in a central area of the room, with infusion chairs facing the workstation, or several smaller workstations spread between patients’ treatment chairs (see below for further detail). All of the infusion area clinicians could easily access the main entry/reception area, clinical exam rooms, utility rooms, and staff areas in the facilities. Several rectangular variations did occur most notably at Site 1, where the infusion area was divided into two separate, rectangular rooms.
Quantitative Findings
Safety Organizing.
Five practices (62.5%) reported high safety organizing behaviors, while three practices (37.5%) reported low behaviors. Sites 2, 4, and 6 had the highest number of infusion chairs in the study and were also higher performers of safety organizing behaviors. Researchers also observed differences in safety organizing behaviors from sites within the same health system indicating that other differences between infusion centers, such as layout and use of physical space, are an influencing factor in safety organizing.
Clinician Communication.
In three practices (37.5% of the sample), clinicians assessed their communication as high. One practice (12.5%) reported medium communication, and clinicians in four practices (50%) reported communication as low.
The research team found a positive correlation between safety organizing and clinician communication measures, r= .414, p=.002. Some sites performed similarly in both safety organizing and clinician communication (Sites 1, 3 and 8 were low-performers on both measures; Sites 4, 5 and 7 were high-performers). Sites 2 and 6 performed high in safety organizing but low or medium on clinician communication. No correlation between practice size (i.e. number of infusion chairs) and measures of safety organizing and communication (results not shown) was observed.
Qualitative Findings
Two major patterns were identified in the qualitative data regarding safety organizing and clinician communication: the practice’s physical layout may influence patient visibility and clinician proximity during chemotherapy treatment. Physical layout was also discussed as influencing perceptions of patient privacy.
Safety Organizing.
Infusion nurses reported that the layout of their practice either supported or hindered safe patient care. Nurses shared that they appreciated being close to patients to improve observation of patients for drug reactions, side effects, technical issues with infusion pumps, or other needs.
One nurse from Site 7, a high performer on the safety organizing scale, described how some patients are obscured from the nurses’ view,
“Well, let me say a negative first…I don’t like it because you can’t see everybody…you’re not right there to catch [reactions] right away…So that’s the one thing I don’t like about the setup.”
Conversely, a nurse from site 2 emphasized the positive effects of nurse to patient visibility and proximity during chemotherapy infusion,
“You can tell a lot by how a patient’s doing if you can actually see them or be close by to check on them more often. So I do like that fact that our patients sit near us.”
A nurse from Site 6 echoed this positive assessment of patient visibility to the nursing staff,
“And you know if [the patient is] having a reaction, because you’re right there…beside them almost or you know we’re hardly…ever out of the area… And then the patients know that their nurse is close by too.”
Although Sites 2 and 6 did not have an open infusion area layout but an L-shaped layout instead, both sites performed high on safety organizing. The sites used a geographically oriented nursing assignment, a model where nurses cared for whichever patients were placed in chairs or rooms physically nearest to a workstation. The geographically oriented assignment was used in Site 2 to counter the barriers presented by the physical layout. Further, Site 2 leaders stationed infusion nurses in teams of two or three at “pods” throughout the room with their assigned patients proximal to the pod. With this modification, the patients seated in each pod were highly visible to their infusion nurses (see Figure 3). For comparison, the infusion area at Site 3 was also L-shaped with two nurses assigned to patients on opposite sides of the room. However, despite the similarities in floorplan and nursing assignment to Sites 2 and 6, Site 3 performed poorly on the safety organizing scale. Unfortunately, while we requested floorplans from all eight sites, only one responded affirmatively to being included in publication.
Figure 3a.

Selected infusion center layout (site 2). The nursing pods are scattered throughout the infusion center (example of a pod is outlined in yellow). The clinic exam rooms and prescribers are near infusion nurses if an acute issue arises. The design of the pods allows for the infusion nurses to work closely to their assigned patients receiving chemotherapy.
Figure 3b. Photograph of clinical area highlighted in Figure 2a (blue border). Photo was taken in the direction of the light blue arrow. The nursing pod has patient chairs to the left and an open nurses’ station on the right, offering visibility of assigned patients within the pod. The photo was provided via the institution’s patient pamphlet.
Clinician communication.
The ability for clinicians’ to effectively communicate was often represented through the proximity between infusion nurses and between the infusion area and provider offices. Infusion nurse proximity to one another was a positive factor in facilitating effective communication. One nurse discussed the positive link between nurse proximity and communication practices to patient safety,
“Well, we’re always partnered up. We have a partner so that even though I have my set of patients, they have their set of patients, we are communicating back and forth all the time…Like if I’ve got a patient that’s getting a new drug for the first time, that there’s a reaction potential, I need to tell my partner about that…So we’re all then kind of watching that person, so we have to communicate a lot between us.”
Due to physical location of infusion areas in relationship to providers and clinical spaces, communication and interaction between infusion nurses and providers was more easily facilitated when the physical layout provided a direct link between the two. While it was not the only determining factor of poor communication, Site 1 and Site 6 both had infusion areas that were not connected to clinical spaces and both performed low on clinician communication measures.
Privacy.
Privacy was also a salient issue identified during our observations and interviews. While patient visibility is crucial for chemotherapy infusion, patients’ access to private space is also a concern. Many clinicians across the sites expressed concerns about patient privacy (i.e., discussing personal information or accessing central venous catheters and administering injections in sensitive body areas) in relation to the infusion area’s physical space. Most of the sites had small bedroom spaces in their infusion area if patients required or requested a bed. Several sites had infusion chairs divided by walls, curtains, or moveable partitions. Many of the clinicians relayed their perspectives on patient privacy in relation to the capacity for nurses to safely care for patients.
The nurse manager from Site 7 summarized this relationship,
“My ideal…we’d have a larger space and maybe more…divided for some privacy yet your nursing is going to be in front so you can still see and observe your patient, but the patient doesn’t need to be observed by the next patient. You know it’s taking away that communication with other patients, which over the past years has been very helpful.”
Data Integration
In Table 2, the research team integrated quantitative and qualitative findings, stratified by safety organizing and clinician communication categories, representing their positive and negative aspects on patient safety and clinician communication. Variations in layout contributed to differences in how clinicians discussed patient visibility and clinician proximity. Layout variations were both facilitators and barriers to safety organizing and clinician communication.
Table 2.
Data integration and quotes related to ambulatory oncology practices with high and low performance in safety organizing and clinician communication.
| Safety Organizing Behaviors | |
|---|---|
| The Safety Organizing Scale asked clinicians about the degree to which they engage in behaviors and practices consistent with a safety culture | |
| Low safety organizing practice |
|
| High safety organizing practice |
|
| Communication Satisfaction | |
| The communication satisfaction scale asked clinicians their satisfaction with relationships and communication between nurses and physicians. | |
| Low clinician communication practice |
|
| High clinician communication practice |
|
| Patient Privacy | |
| Amount of privacy afforded to patients generally in relation to physical layout and space of the infusion area (result represented in the qualitative findings but not measured in the quantitative phase). | |
| Clinician perspective on patient privacy |
|
Discussion
This mixed method study helps inform the clinical and health design community on how physical layouts and space influence safe cancer care delivery in ambulatory oncology practices. This study employs a novel approach to collect clinician- and practice-level data to understand how physical layout, when a barrier to care, affects safety and clinician communication behaviors with care delivery. To the researchers’ knowledge, this is the first study to use mixed quantitative and qualitative methods to examine the relationships between physical layouts, patient safety, and clinician communication in ambulatory oncology practices. Practices scoring highly in empirically validated safety organizing and clinician communication scales did not uniformly report on their ability to view patients directly during chemotherapy infusions nor on the proximity of infusion nurses and physical integration between infusion centers and other oncology office spaces. Additionally, clinicians were unsure and doubtful that their infusion centers were designed explicitly with chemotherapy safety elements in mind. The data suggested some design elements of infusion centers (e.g., ornamental walls blocking nurses’ views) were not appropriate for the delivery of chemotherapy, in terms of infusion nurses being able to safely administer treatments and to have clear access, both physical and visual, to their patients. Evidence from more practices is needed to validate this observation.
According to infusion nurses, patient visibility is a crucial aspect of infusion. Variations in visibility occur despite similarities in the physical shape of the infusion area. The importance of patient visibility to patient safety has been demonstrated in intensive care, but not in ambulatory oncology practices (Lu et al., 2014). How nurses are assigned and how space is utilized play a vital role in improving patient safety. As highlighted previously, one high-performing site with a rectangular shaped infusion area had poor patient visibility according to its nurses, while another high-performing site, this one with an L-shaped infusion center, reported positively on patient visibility.
Clinicians and patients repeatedly cite the importance of patient privacy in health care settings (Groff et al., 2008; Gulwadi et al., 2009; Olsen et al., 2008; Sadek & Willis, 2019). There is a need for balance between patients’ access to privacy, patients’ desire to socialize with other patients, and nurses’ ability to safely deliver care. Additional studies should investigate this finding and develop novel strategies to provide patient privacy in ways that optimize safety considerations.
Other recent studies have examined how clinical space and layout play an integral role in patient care and the patient experience. Notably, in ambulatory oncology, Wang & Pukszta (2017, 2018) have used surveys to better understand patient, family and clinician perspectives on how to provide various environments for ambulatory chemotherapy treatment. Other qualitative studies focusing on the intersection of the patient and the built environment analyze autobiographical patient accounts and patient narratives to centralize how patients experience the physical space of ambulatory oncology practices to aid in designing patient-centered spaces intended for cancer care (Carmel-Gilfilen & Portillo, 2016; Jellema et al., 2019).
A majority of the research to date, however, focuses on non-oncology ambulatory care (Wingler & Hector, 2015) or non-ambulatory care (Hadi & Zimring, 2016; Lu et al., 2017; Naccarella et al., 2019). Several of these studies have findings similar to ours linking visibility and communication to patient safety and satisfaction and have used a variety of methodological approaches, including GIS-mapping (Hadi & Zimring, 2016; Lu, 2010), survey-based (Lu et al., 2017), and qualitative methods (Gum et al., 2012). Yet, data demonstrating the clinician perspective on space and layout appears to be limited and additional knowledge is essential to ensuring that ambulatory care centers are designed with patient safety at the forefront.
Several studies also concluded that strengthened clinician communication is associated with improved patient safety (Gum et al., 2012; Naccarella et al., 2019). For example, Naccarella et al. (2019), highlighted that communication and safety were linked within the emergency department through a mixed methods approach. This study closely resembled our mixed methods approach with survey and interview data and reported similar findings in a different clinical context. Such similarities demonstrate the importance of highlighting these issues within ambulatory cancer care. In doing so, our study adds to the body of knowledge by reporting on these challenges and positing solutions within the high-risk context of ambulatory oncology practices. As one example, direct line of sight to patients may not be as vital to patient safety in other outpatient practices that are not administering highly toxic drugs daily, as happens in ambulatory oncology practices.
Our study presents relevant safety considerations as the demand for chemotherapy infusion services increases, vertical practice consolidation continues (Fauer & Friese, 2019), and financial pressures burden practices (Community Oncology Alliance, 2020). In these contexts, health systems may need to repurpose existing space instead of designing and building new chemotherapy infusion areas. Two health care sector studies have reported an increased need to adopt flexible design approaches and explore novel strategies to use pre-existing space in cost-effective ways (Joseph et al., 2018; Zeliotis, 2017). The findings from this study suggest there are nuanced opportunities for health system leaders to approach such projects to facilitate patient safety and clinician communication, primarily through enhancing patient visibility and integration of infusion spaces and clinical spaces within the broader ambulatory oncology practice.
Our study has several limitations. First, the investigators performed a secondary data analysis from an existing multi-site study in which floor plans were not a primary focus. Our patient safety and physical layout recommendations from clinicians may not be applicable for designers and health systems without greater spatial detail.
There are other study limitations to consider. The quantitative analyses were cross-sectional, limiting our inferences to associations. Researchers did not conduct the quantitative and qualitative phases concurrently. Although this is not a classical approach for convergent analysis, this analysis was feasible for the researchers to collect and analyze data at eight practices throughout the state without disrupting patient care activities. Additionally, the qualitative phase focused on nurses, potentially leading to conflicting practice-level outcomes in safety organizing and clinician communication. The qualitative findings may not be generalizable to all ambulatory oncology practices, despite successfully recruiting a mix of practices in terms of patient volume and organizational contexts. Combining insights from clinician perspectives with patient experience would create a more robust understanding of the influence physical layout has on care delivery. An explicit collection of physical layout data using specific quantitative measures coupled with a close examination of physical layout through qualitative data collection would strengthen future research endeavors. Additionally, including expertise from partners within other health and environmental design disciplines will provide pivotal insight for future research.
Conclusions
The physical layout, use of space, and assignment of personnel within ambulatory oncology practices contribute to safer cancer care delivery by affecting clinician-to-patient visibility during chemotherapy infusion and clinicians’ proximity to one another during routine care. Findings from this mixed methods study provide preliminary actions to enhance ambulatory oncology practices’ quality of care. Clinical leaders may discover new benefits from perceiving the physical layout and use of space through a safety lens with longitudinal methods to examine their impact on more successful patient safety and clinician communication practices.
Figure 2.

Interview guide topics with sample questions.
Acknowledgements:
The authors would like to thank the practices and staff involved in this project, the Michigan Oncology Quality Consortium (MOQC)—especially Dr. Jennifer Griggs and Louise Bedard, and our late colleague, Kari Mendelsohn-Victor, for her tireless contributions to our team.
Funding:
This work was supported by the Agency for Healthcare Research and Quality (R01HS024914) and the National Cancer Institute of the National Institutes of Health (P30CA046592). The findings and conclusions in this document are those of the authors, who are responsible for its content, and do not necessarily represent the views or positions of AHRQ, NIH, or the US Department of Health and Human Services.
Footnotes
Disclosures: The authors have no conflicts of interest to report
References
- Alpert A, Hsi H, & Jacobson M (2017). Evaluating The Role Of Payment Policy In Driving Vertical Integration In The Oncology Market. Health Affairs, 36(4), 680–688. 10.1377/hlthaff.2016.0830 [DOI] [PubMed] [Google Scholar]
- American Society for Clinical Oncology. (2019). State of Cancer Care in America. https://www.asco.org/research-guidelines/reports-studies/state-cancer-care
- Blayney DW, Simon MK, Podtschaske B, Ramsey S, Shyu M, Lindquist C, & Milstein A (2018). Critical Lessons From High-Value Oncology Practices. JAMA Oncology, 4(2), 164–171. 10.1001/jamaoncol.2017.3803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom M, Markovitz S, Silverman S, & Yost C (2015). Ten Trends Transforming Cancer Care and Their Effects on Space Planning for Academic Medical Centers. HERD: Health Environments Research & Design Journal, 8(2), 85–94. 10.1177/1937586714565598 [DOI] [PubMed] [Google Scholar]
- Carmel-Gilfilen C, & Portillo M (2016). Designing With Empathy: Humanizing Narratives for Inspired Healthcare Experiences. HERD: Health Environments Research & Design Journal, 9(2), 130–146. 10.1177/1937586715592633 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2019). Ambulatory Health Care Data. https://www.cdc.gov/nchs/ahcd/index.htm
- Community Oncology Alliance (2020). 2020 Community Oncology Alliance Practice Impact Report. https://communityoncology.org/2020-community-oncology-alliance-practice-impact-report/
- Creswell J (2018). Designing and Conducting Mixed Methods Research (3rd ed.). SAGE. [Google Scholar]
- de Matos LBN, Fumis RRL, Nassar Junior AP, Lacerda FH, & Caruso P (2020). Single-Bed or Multibed Room Designs Influence ICU Staff Stress and Family Satisfaction, But Do Not Influence ICU Staff Burnout. HERD: Health Environments Research & Design Journal, 13(2), 234–242. 10.1177/1937586719878445 [DOI] [PubMed] [Google Scholar]
- Fauer A, & Friese C (2019). 340B Drug Pricing Program: The Expansion and Its Effect on Cancer Care. Clinical Journal of Oncology Nursing. 10.1188/19.CJON.217-219 [DOI] [PubMed] [Google Scholar]
- Gharaveis A, Hamilton DK, & Pati D (2018). The Impact of Environmental Design on Teamwork and Communication in Healthcare Facilities: A Systematic Literature Review. HERD: Health Environments Research & Design Journal, 11(1), 119–137. 10.1177/1937586717730333 [DOI] [PubMed] [Google Scholar]
- Groff SL, Carlson LE, Tsang K, & Potter BJ (2008). Cancer Patientsʼ Satisfaction With Care in Traditional and Innovative Ambulatory Oncology Clinics. Journal of Nursing Care Quality, 23(3), 251–257. 10.1097/01.NCQ.0000324590.99460.f6 [DOI] [PubMed] [Google Scholar]
- Grover C, MacKasey E, Cook E, Tremblay L, & Loiselle CG (2018). Patient-reported care domains that enhance the experience of “being known” in an ambulatory cancer care centre. Canadian Oncology Nursing Journal, 28(3), 166–171. 10.5737/23688076283166171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guetterman TC, Fetters MD, & Creswell JW (2015). Integrating Quantitative and Qualitative Results in Health Science Mixed Methods Research Through Joint Displays. The Annals of Family Medicine, 13(6), 554–561. 10.1370/afm.1865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulwadi GB, Joseph A, & Keller AB (2009). Exploring the Impact of the Physical Environment on Patient Outcomes in Ambulatory Care Settings. HERD: Health Environments Research & Design Journal, 2(2), 21–41. 10.1177/193758670900200203 [DOI] [PubMed] [Google Scholar]
- Gum LF, Prideaux D, Sweet L, & Greenhill J (2012). From the nurses’ station to the health team hub: How can design promote interprofessional collaboration? Journal of Interprofessional Care, 26(1), 21–27. 10.3109/13561820.2011.636157 [DOI] [PubMed] [Google Scholar]
- Hadi K, & Zimring C (2016). Design to Improve Visibility: Impact of Corridor Width and Unit Shape. HERD: Health Environments Research & Design Journal, 9(4), 35–49. 10.1177/1937586715621643 [DOI] [PubMed] [Google Scholar]
- Høybye MT (2013). Healing environments in cancer treatment and care. Relations of space and practice in hematological cancer treatment. Acta Oncologica, 52(2), 440–446. 10.3109/0284186X.2012.741323 [DOI] [PubMed] [Google Scholar]
- Huang Y-L, Bryce AH, Culbertson T, Connor SL, Looker SA, Altman KM, Collins JG, Stellner W, McWilliams RR, Moreno-Aspitia A, Ailawadhi S, & Mesa RA (2018). Alternative Outpatient Chemotherapy Scheduling Method to Improve Patient Service Quality and Nurse Satisfaction. Journal of Oncology Practice, 14(2), e82–e91. 10.1200/JOP.2017.025510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalalianhosseini M, Freihoefer K, Doyle N, & Simpson A (2020). The Impact of Infusion Center Layout on Workflow and Satisfactions in Two Cancer Infusion Centers: A Case Study on Staff and Patients. HERD: Health Environments Research & Design Journal, 13(3), 70–83. 10.1177/1937586719888221 [DOI] [PubMed] [Google Scholar]
- Jellema P, Annemans M, & Heylighen A (2019). Foregrounding the built environment in the experience of cancer care: A qualitative study of autobiographical cancer narratives. European Journal of Cancer Care, 28(6). 10.1111/ecc.13156 [DOI] [PubMed] [Google Scholar]
- Joseph A, Henriksen K, & Malone E (2018). The Architecture of Safety: An Emerging Priority For Improving Patient Safety. Health Affairs, 37(11), 1884–1891. [DOI] [PubMed] [Google Scholar]
- Kyngäs H, Mikkonen K, & Kääriäinen M (Eds.). (2019). The Application of Content Analysis in Nursing Science Research. Springer Nature. [Google Scholar]
- Lafferty M, Fauer A, Wright N, Manojlovich M, & Friese C (2020). Causes and Consequences of Chemotherapy Delays in Ambulatory Oncology Practices: A Multisite Qualitative Study. Oncology Nursing Forum, 47(4), 417–427. 10.1188/20.ONF.417-427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Y (2010). Measuring the Structure of Visual Fields in Nursing Units. HERD: Health Environments Research & Design Journal, 3(2), 48–59. 10.1177/193758671000300205 [DOI] [PubMed] [Google Scholar]
- Lu Y, Cai H, & Bosch SJ (2017). Key Spatial Factors Influencing the Perceived Privacy in Nursing Units: An Exploration Study With Eight Nursing Units in Hong Kong. HERD: Health Environments Research & Design Journal, 10(4), 37–48. 10.1177/1937586716672857 [DOI] [PubMed] [Google Scholar]
- Lu Y, Ossmann MM, Leaf DE, & Factor PH (2014). Patient Visibility and ICU Mortality: A Conceptual Replication. HERD: Health Environments Research & Design Journal, 7(2), 92–103. 10.1177/193758671400700206 [DOI] [PubMed] [Google Scholar]
- Manojlovich M, Bedard L, Griggs JJ, McBratnie M, Mendelsohn-Victor K, & Friese CR (2020). Facilitators and Barriers to Recruiting Ambulatory Oncology Practices Into a Large Multisite Study: Mixed Methods Study. JMIR Cancer, 6(1), e14476. 10.2196/14476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald S (2005). Studying actions in context: a qualitative shadowing method for organizational research. Qualitative Research, 5(4), 455–473. 10.1177/1468794105056923 [DOI] [Google Scholar]
- Naccarella L, Raggatt M, & Redley B (2019). The Influence of Spatial Design on Team Communication in Hospital Emergency Departments. HERD: Health Environments Research & Design Journal, 12(2), 100–115. 10.1177/1937586718800481 [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. (2020). Cancer Stat Facts: Cancer of Any Site. https://seer.cancer.gov/statfacts/html/all.html
- Olsen JC, Cutcliffe B, & O’Brien BC (2008). Emergency Department Design and Patient Perceptions of Privacy and Confidentiality. The Journal of Emergency Medicine, 35(3), 317–320. 10.1016/j.jemermed.2007.10.029 [DOI] [PubMed] [Google Scholar]
- Patel MR, Friese CR, Mendelsohn-Victor K, Fauer AJ, Ghosh B, Bedard L, Griggs JJ, & Manojlovich M (2019). Clinician Perspectives on Electronic Health Records, Communication, and Patient Safety Across Diverse Medical Oncology Practices. Journal of Oncology Practice, 15(6), e529–e536. 10.1200/JOP.18.00507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadek AH, & Willis J (2019). Ways to harness the built environment of ambulatory cancer facilities for comprehensive patient support: A review of the literature. International Journal of Nursing Studies. 10.1016/j.ijnurstu.2019.05.004 [DOI] [PubMed] [Google Scholar]
- Shortell SM, Rousseau DM, Gillies RR, Devers KJ, & Simons TL (1991). Organizational Assessment in Intensive Care Units (ICUs): Construct Development, Reliability, and Validity of the ICU Nurse-Physician Questionnaire. Medical Care, 29(8), 709–726. 10.1097/00005650-199108000-00004 [DOI] [PubMed] [Google Scholar]
- Vogus TJ, & Sutcliffe KM (2007). The Safety Organizing Scale: Development and Validation of a Behavioral Measure of Safety Culture in Hospital Nursing Units. Medical Care, 45(1), 46–54. 10.1097/01.mlr.0000244635.61178.7a [DOI] [PubMed] [Google Scholar]
- Wang Z, & Pukszta M (2017). Patient Needs and Environments for Cancer Infusion Treatment. Journal of Interior Design, 42(2), 13–25. 10.1111/joid.12096 [DOI] [Google Scholar]
- Wang Z, & Pukszta M (2018). Private Rooms, Semi-Open Areas, or Open Areas for Chemotherapy Care: Perspectives of Cancer Patients, Families, and Nursing Staff. HERD: Health Environments Research & Design Journal, 11(3), 94–108. 10.1177/1937586718758445 [DOI] [PubMed] [Google Scholar]
- Wingler D, & Hector R (2015). Demonstrating the Effect of the Built Environment on Staff Health-Related Quality of Life in Ambulatory Care Environments. HERD: Health Environments Research & Design Journal, 8(4), 25–40. 10.1177/1937586715573745 [DOI] [PubMed] [Google Scholar]
- Zeliotis C (2017). Where to next for cancer centre design? Future Hospital Journal, 4(2), 142–145. 10.7861/futurehosp.4-2-142 [DOI] [PMC free article] [PubMed] [Google Scholar]


