Abstract
Behavioral theories inform the development of lifestyle interventions to address low participation in physical activity (PA); however, relatively little is known about the value of self-determination theory (SDT) for explaining screen time (ST) behaviors or in extending SDT into a dyadic context. Actor-partner (i.e., parent-adolescent) interdependence models (APIMs) allow for examination of these interpersonal relationships. The purpose of this study was to examine PA and ST among parent-adolescent dyads using the cross-sectional Family Life, Activity, Sun, Health, and Eating (FLASHE) Study. Parent-adolescent dyads provided responses to online surveys addressing PA (n=1177 dyads) and ST (n=1489 dyads) behaviors. We examined the influence of SDT-based constructs (perceived competence and motivation) on PA and ST behaviors. Structural equations were used to estimate APIMs in STATA 15.1. Full models provided a good fit to the data. For both PA and ST, perceived competence was more strongly associated with motivation among adolescents compared with parents (PA: β =0.72 vs. 0.58, ST: β =0.34 vs. 0.22, p’s <.001). Parental motivation was associated with parental PA and both adolescent motivation for PA and ST (p’s<.001). Parental motivation was not associated with adolescent ST-behavior. Adolescent motivation was only associated with parent motivation for PA. In the FLASHE study, SDT constructs extend acceptably to the dyadic setting, with PA models providing a slightly better fit to the data than ST models. Longitudinal studies that target perceived competence and the self-regulation of motivation in parents and their adolescents are a next logical step to understanding both PA and ST behaviors.
Keywords: Physical Activity, Screen Time, Lifestyle Behaviors, Perceived Competence, Motivation
Introduction
Physical activity (PA) and sedentary screen time (ST) behaviors established during adolescence may be important predictors of long-term health, due to the tendency of such behavioral patterns to track into adulthood.1 They are also independently associated with diseases such as type II diabetes, cardiovascular disease and cancer.2 It is thus important that researchers, educators, clinicians and public health professionals develop comprehensive strategies to identifying and addressing high risk behavioral profiles in youth.3, 4 In addition to individual-level factors, family, social and environmental interactions are important contexts in which behavioral patterns are established and reinforced. One limitation of prior behavioral research among adolescents, compared to children, has been the focus solely on individual level factors, without adequate consideration of social or environmental contexts such as family interactions, perhaps because they are perceived as having greater autonomy and independence than children.
The socio-ecological model may therefore be a useful conceptual framework for identifying both where and how interventions may be tailored to target important health behaviors.5 The first level considers individual level biological, psychological and socio-demographic factors that influence behaviors. The next level expands to include family, caregivers, friends and sociocultural context as influences on behavior. While the model also encompasses institutional, environmental and policy level factors, here we focus on the individual and interpersonal levels. A limitation of interventions guided solely by ecological frameworks is that they usually do not incorporate theory-driven behavioral models at the individual level.6 At the individual level, metanalytic data has provided some insight into the efficacy of randomized theory-based behavioral interventions targeting physical activity (PA) behaviors.7 Globally, theory-based interventions have been effective at changing PA (Cohen’s d=.31, interpreted as a small to medium effect). Interestingly, no empirical differences in efficacy were found between specific theory-based interventions; however, single theory-based interventions appeared more effective than combined theory approaches.
Both social cognitive theory (SCT)8–10 and self-determination theory (SDT)11, 12 are examples of extensively investigated individual level behavioral models, improving our understanding of how individuals motivate and self-regulate their engagement in PA and ST behaviors. A weakness of these theories is that they do not usually explain a high degree of variance in behavior, likely only working well for a subset of behavioral responders and partly or not at all for others.13 Expanding from the individual level to the interpersonal and family level (i.e., parent-adolescent), results from an older behavioral weight management intervention indicated that children in a parent-child intervention group had superior outcomes when compared with children in a non-specific control group.14 However, findings from one small 3-arm RCT conducted in an underserved rural setting found instead that a parent-only focused intervention was more effective at reducing weight gain in overweight children than a family-based intervention.15 Less evidence exists for the role of family or parent-level behavioral interventions in adolescents compared with those targeting children, or from behavioral interventions targeting ST behaviors in parents and adolescents.16 Multi-level approaches that can illuminate individual level factors as well as the interpersonal and organizational level factors may be one approach for augmenting behavioral interventions typically focused on the person as the unit of analysis.
For example, interventional strategies that can simultaneously be focused on contextual factors such as family/social/interpersonal interactions, and the home-, school or social environment4 might prove useful. Whether theories such as SDT, useful in explaining individual level behavior, can be successfully incorporated into more inclusive multi-level conceptualizations is yet to be fully explored. Furthermore, whether it adequately explains associations between constructs such as motivation and perceived competence for both positive behaviors (PA) and more negatively perceived ones (ST) is also unclear.
To provide an initial evaluation of how factors across both individual level behaviors and interpersonal and environmental interactions may be associated with the health behaviors of adolescents and their caregivers, the National Cancer Institute (NCI) conducted the Family, Life, Activity, Sun, Health and Eating Study (FLASHE), an internet-based survey of parent-adolescent dyads. This cross-sectional survey included assessments of physical activity (PA) and screen time (ST) as primary behavioral outcomes, and SDT-based evaluations of perceived competence (i.e., self-efficacy) and motivational self-regulation of those behaviors in parents and their adolescent teens. While SDT has been shown to explain individual level behaviors to some degree,11, 12 it has not been well-tested when conceptualized concurrently at the interpersonal level. Furthermore, there are limited examples of SDT as it pertains to limiting ST behaviors. Using a structural equation modelling (SEM) approach we examined the bi-directional relationships (actor-partner interdependence) between parent and adolescent perceived competence and motivational orientation (extrinsic vs. intrinsic self-regulation) for PA and ST behaviors. We hypothesized that SDT would extend well to the interpersonal context, with dyadic models (parent-adolescent) explaining significant variance in PA and ST behaviors. We also hypothesized that there would be differential effects of SDT constructs on PA and ST due to their different roles in social engagement, especially among adolescents.
Materials and Methods
Study Population
Data from the National Cancer Institute’s Family, Life, Activity, Sun, Health, and Eating (FLASHE) Study were utilized for the current analyses. FLASHE was a cross-sectional observation study conducted between April and October of 2014 designed to explore cancer-related behaviors in adolescents (aged 12–17) and one of their parents. To identify a representative sample matched on key demographic characteristics (sex, Census division, household income, household size, and race/ethnicity) FLASHE dyads were recruited through the Ipsos Consumer opinion panel, which includes over 700,000 active members.17 Parent participants were eligible if they were aged ≥18 years and lived with at least one child aged 12–17 years for a minimum of 50% of the time. If the parent had one eligible child, they were invited to the study. If two or more children were eligible, one was randomly selected for the study. A total of 5,027 parent–adolescent dyads were screened for eligibility, with 1,945 (38.7%) ultimately enrolled, of which 1,573 dyads returned all FLASHE surveys. FLASHE was reviewed and approved by the U.S. Government’s Office of Management and Budget, the National Cancer Institute Special Studies IRB, and the Westat IRB. Both parent consent and adolescent assent was required for dyads to be enrolled in the study. More information about the design and execution of the FLASHE study can be found elsewhere.17–19
Measures
Physical activity and screen time
The Youth Activity Profile (YAP) self-report survey was utilized to assess PA of the adolescent participants. The YAP is a 15-item questionnaire that assesses activity patterns both during and out of school the previous week20 and has been validated against accelerometry for these analyses.21 For the current study, PA was represented as a continuous variable derived as the total predicted (calibrated with accelerometry) minutes of physical activity (in school, out of school, and weekend). Time spent in sedentary ST pursuits was assessed from 4 items capturing the hours spent per day using a computer, cell phone, watching TV and or playing video games.22 The short form of the International Physical Activity Questionnaire (IPAQ) was utilized to assess PA in the adult participants.23, 24 The IPAQ assesses three specific types of activity undertaken in four domains. The specific types of activity assessed are walking, moderate-intensity activities and vigorous-intensity activities. The four domains are 1) leisure-time activities, 2) domestic activities, 3) work-related activities, and 4) transport-related activities. The IPAQ has previously been validated in adults and is a widely used measure of PA in epidemiological studies.23 For the current study, we expressed parental PA as a continuous score in MET-minutes/week. Both the YAP and IPAQ include questions that anchor behavior to different contexts (e.g., school, home, transport, leisure-time) providing a proxy for a multilevel assessment of activity patterns. For adult ST behaviors, questions were similar to those used in the YAP and assessed time (hours/day) using a computer, cell phone, watching TV, playing handheld video games or electronic readers. We did not expressly model environment or social context for either PA or ST.
Self-Determination Theory (SDT) constructs
Perceived competence (self-efficacy)
Perceived-competence for exercise or limiting screen time was assessed using a single item for each construct separately from the perceived competence scale (PCS),25 "I feel confident in my ability to exercise regularly (PA) or to limit use of electronic devices (ST)," which was assessed on a five-point Likert-type scale anchored with "1-strongly disagree" and "5-strongly agree " with higher scores representing greater perceived competence. The perceived competence construct was operationalized as self-efficacy in the FLASHE Study conceptual model.
Motivation
SDT constructs related to motivation for engaging in physical activity and for limiting screen time were assessed with four items representing self-regulatory orientation (external regulation, introjected regulation, identified regulation, intrinsic motivation) and adapted from the self-regulation for exercise questionnaire (SRQ-E) or the treatment-self regulation questionnaire (TSRQ).26 Each item was introduced with the stem, "I would exercise most days of the week/try to limit electronic device use because…" Responses were indicated using a five-point Likert-type scale anchored with "1-strongly disagree" and "5-strongly agree "The four items are, 1) "I would feel bad about myself if I didn’t", 2) "I have thought about it and decided that I want to…", 3) "Others would be upset with me if I didn’t", and 4) "It is an important thing for me to do."
Statistical Analyses
All candidate variables were screened for normality and collinearity. Parental PA and ST were positively skewed, so they were log transformed for structural equation modeling. Models for PA and ST were estimated separately, using an identical procedure. First, a theoretically derived measurement model was specified, which included adolescent and parent constructs separately (Figure 1). We then examined the correlations between theorized constructs of the actor-partner interdependence models (APIM’s) to support consideration of modification indices (>20, i.e., the amount by which the model chi-square would be reduced) automatically calculated by the software. Finally, theoretically supported paths and covariances were added in a stepwise fashion in descending order from highest to lowest until relevant candidates were exhausted. Structural equations were used to estimate in STATA 15.1. Model fit indices used were the Comparative Fit Index (CFI), an incremental fit measure with values below .90 considered to be a poor fitting model, between .90 and .95 considered marginal, and above .95 a good fit. Absolute fit measures included the Root Mean Square Error of Approximation (RMSEA), where values below .01, .05 and .08 represent an excellent, good and mediocre fit respectively, and the Standardized Root Mean Square Residual (SRMR) where values below .08 represent a good fit.
Figure 1. Measurement model of parent and adolescent motivational self-regulation of physical activity/screen time behaviors (color required).

Note: PA, Physical Activity; ST, Screen Time; e, Error variance; d, Disturbance
Results
Complete data were available for 1,177 dyads on the PA variables of interest. Missing data were most frequently observed for the PA variables (both the YAP and the IPAQ). For ST variables of interest, complete data were available for 1,489 dyads. Main reasons for exclusion were for missing data on screen time. For PA, the initial measurement model (Figure 1) provided a poor fit to the data (CFI=0.808, RMSEA=0.101; SRMR=0.103). Table 1 shows the resulting correlation coefficients for SDT constructs and both PA and ST behaviors (excluding a latent variable for motivation). Several modification indices met a-priori criteria (>20) for inclusion, were considered theoretically supported, and were thus added to the final model (Figure 2, PA). These indices included covariances between several motivational indicators, parent and adolescent perceived competence, and the parent and adolescent construct for "external regulation" indicated by "Others would be upset with me if I didn’t." Reciprocal paths were suggested between adolescent exercise motivation and parent exercise motivation, and from parent PA to adolescent PA. Once the paths were added, the model was a good fit for the data (CFI=0.932, RMSEA=0.071; SRMR=0.049). Similarly, the initial measurement model for ST (Figure 1) provided a poor fit to the data (CFI=0.810, RMSEA=0.101; SRMR=0.105). In a manner like the model for PA, several modification indices met the a priori criteria for inclusion, were theoretically supported and were added to the final model (Figure 2, ST) including covariances between several SDT indicators of motivational orientation, parent and adolescent perceived competence, and the parent and adolescent construct for "external regulation" indicated by "Others would be upset with me if I didn’t." The software modelling procedure suggested that paths between parent motivation for limiting ST and adolescent motivation for limiting ST, and from parent ST to adolescent ST would improve model fit. Once those paths were added, the model was also considered a good fit for the data (CFI=0.950, RMSEA=0.062; SRMR=0.044). In the final model, adolescents’ perceived competence for both PA and ST was more strongly associated with their motivation for PA and ST when compared to their parents (PA: β =0.72 vs. 0.58, ST: β =0.34 vs. 0.22, p’s <.001). Parental motivation was associated with parental PA (β =0.53) and both adolescent motivation for PA and ST (β =0.28 and β =0.38, p’s<.001). Parental motivation was not associated with adolescent ST-behavior. Adolescent’s motivation was only associated with their own motivation for PA and ST (β =0.39 and β = −0.12, p’s<.001) but only parent motivation for PA (β =0.24). Parental PA and ST behaviors were associated with their adolescents’ behaviors (β =− 0.10 and β = 0.39) but the reverse was not the case.
Table 1.
Correlations between parent-adolescent SDT constructs and physical activity (n=1177) /screen time (n=1489)
| Physical Activity | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|
| |||||||||||||
| 1 Parent: “I would feel bad about myself if I didn’t” | 3.45 | 1.18 | - | ||||||||||
| 2 Parent: “I have thought about it and decided that I want to exercise” | 4.08 | 0.93 | 0.48 | - | |||||||||
| 3 Parent: “Others would be upset with me if I didn’t” | 2.18 | 1.15 | 0.31 | 0.17 | - | ||||||||
| 4 Parent: “It is an important thing for me to do.” | 4.37 | 0.74 | 0.46 | 0.57 | 0.11 | - | |||||||
| 5 Parent self-efficacy for exercise | 3.65 | 1.29 | 0.35 | 0.40 | 0.08 | 0.33 | - | ||||||
| 6 Teen: “I would feel bad about myself if I didn’t” | 3.05 | 1.21 | 0.27 | 0.16 | 0.24 | 0.17 | 0.20 | - | |||||
| 7 Teen: “I have thought about it and decided that I want to exercise” | 3.81 | 1.03 | 0.14 | 0.26 | 0.10 | 0.24 | 0.18 | 0.51 | - | ||||
| 8 Teen: “Others would be upset with me if I didn’t” | 2.49 | 1.26 | 0.23 | 0.07 | 0.34 | 0.10 | 0.08 | 0.34 | 0.14 | - | |||
| 9 Teen: “It is an important thing for me to do.” | 4.13 | 0.93 | 0.15 | 0.16 | 0.08 | 0.28 | 0.11 | 0.44 | 0.54 | 0.17 | - | ||
| 10 Teen self-efficacy for exercise | 3.90 | 1.11 | 0.10 | 0.18 | 0.07 | 0.22 | 0.18 | 0.32 | 0.48 | 0.06 | 0.49 | - | |
| 11 Teen minutes of physical activity per week | 784.46 | 138.31 | 0.04 | 0.04 | 0.04 | 0.05 | 0.06 | 0.15 | 0.14 | 0.12 | 0.18 | 0.29 | - |
| 12 Parent MET minutes of physical activity per week | 3296.09 | 3088.34 | 0.20 | 0.21 | 0.13 | 0.18 | 0.27 | 0.12 | 0.15 | 0.08 | 0.07 | 0.15 | 0.13 |
|
| |||||||||||||
| Screen Time | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
| 1 Parent: “I would feel bad about myself if I didn’t” | 2.74 | 1.23 | - | ||||||||||
| 2 Parent: “I have thought about it and decided that I want to limit the amount of time I spend using electronic devices” | 3.01 | 1.25 | 0.63 | - | |||||||||
| 3 Parent: “Others would be upset with me if I didn’t limit the amount of time I spend using electronic devices” | 2.34 | 1.23 | 0.52 | 0.46 | - | ||||||||
| 4 Parent: “It is an important thing for me to do.” | 3.32 | 1.20 | 0.61 | 0.72 | 0.43 | - | |||||||
| 5 Parent self-efficacy to limit electronic device use. | 3.88 | 1.09 | 0.12 | 0.23 | 0.00 | 0.18 | - | ||||||
| 6 Teen: “I would feel bad about myself if I didn’t” | 2.44 | 1.18 | 0.29 | 0.24 | 0.24 | 0.22 | 0.10 | - | |||||
| 7 Teen: “I have thought about it and decided that I want to limit the amount of time I spend using electronic devices” | 2.69 | 1.22 | 0.25 | 0.28 | 0.20 | 0.24 | 0.15 | 0.61 | - | ||||
| 8 Teen: “Others would be upset with me if I didn’t limit the amount of time I spend using electronic devices” | 2.91 | 1.33 | 0.26 | 0.19 | 0.24 | 0.21 | 0.06 | 0.42 | 0.37 | ||||
| 9 Teen: “It is an important thing for me to do.” | 3.20 | 1.17 | 0.20 | 0.23 | 0.16 | 0.26 | 0.16 | 0.51 | 0.62 | 0.39 | |||
| 10 Teen self-efficacy to limit electronic device use. | 3.49 | 1.15 | 0.02 | 0.07 | 0.04 | 0.05 | 0.23 | 0.24 | 0.34 | 0.00 | 0.27 | - | |
| 11 Teen electronic device usage per week | 5.87 | 3.16 | 0.04 | 0.03 | 0.03 | 0.03 | 0.06 | 0.03 | 0.09 | 0.06 | 0.07 | 0.12 | |
| 12 Parent electronic device usage per week | 7.98 | 4.21 | 0.09 | 0.08 | 0.03 | 0.06 | 0.16 | 0.00 | 0.04 | 0.02 | 0.01 | 0.01 | 0.39 |
Figure 2. Full parent-adolescent APIM’s of physical activity/screen time behaviors (color required).
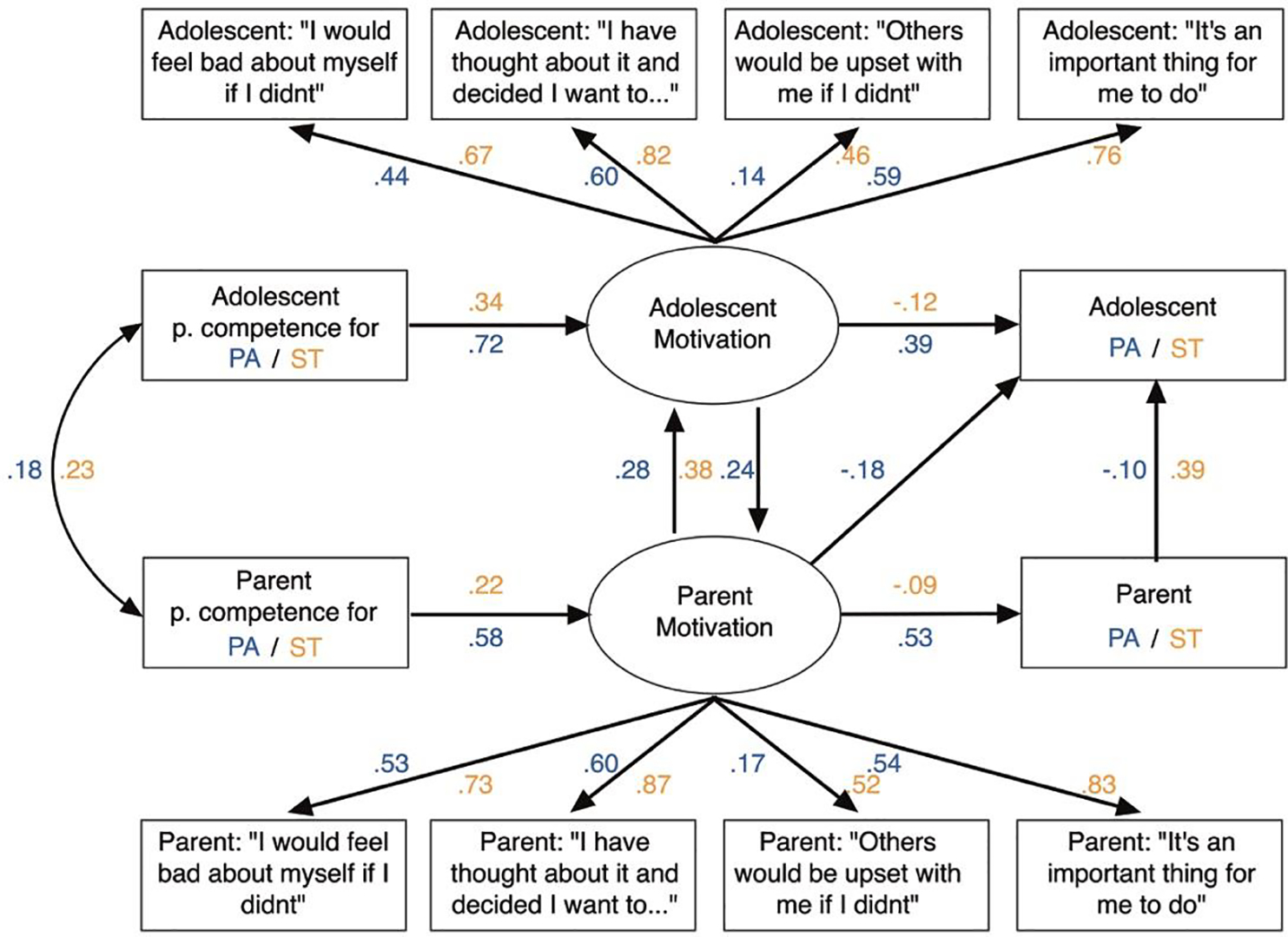
Note: Solid arrows = statistically significant paths (p=.05); Error variances and covariances have been omitted for clarity.
Abbreviations: PA, Physical Activity; ST, Screen Time
Discussion
Our primary finding was that SDT variables capturing the perceived competence and self-regulation of motivation were associated with both PA and ST behaviors among parents and their adolescent children. Interdependence of motivational self-regulation for PA differed between adolescents and their parents; notably, parent motivation was significantly associated with both adolescent motivation for PA and actual behavior. Overall, we found support for our hypotheses that SDT models would extend well to the dyadic context (interpersonal parent-adolescent) and would be useful for exploring relationships among SDT constructs and both PA and ST behaviors.
Similar to our study, other researchers using FLASHE data have found that PA-related enjoyment and self-efficacy are associated more strongly with actors’ own behaviors.27, 28 Joyal-Demarais and colleagues,28 using a similar approach to ours, tested an extension of the theory of planned behavior and found that attitudes, norms and perceived behavioral control consistently explained greater variance in intentions rather than behaviors for each lifestyle behavior examined. A different study, also using FLASHE data found that perceived weight status impacted perceived barriers to engaging in physical activity. Where at least one member of a parent-adolescent dyad was overweight or obese, their partner perceived greater barriers to PA, highlighting the importance of the family setting in promoting healthy behaviors.29 While these studies, and our own, lend support to the significance of interpersonal relationships, they are nonetheless correlational and future longitudinal studies are required to confirm these relationships.
A unique aspect of our own study is the examination of perceived competence and motivation for limiting ST, a negative rather than positive health behavior. While previous evidence suggests the treatment self-regulation questionnaire (TSRQ) is valid in explaining other negative behaviors (e.g., smoking)30 our evidence suggests SDT based motivational effects were smaller for ST vs. PA behaviors. While screen time among adolescents can involve social interactions or educational activities—it is unlikely to take up the majority of adolescents’ screen time. High levels of ST can lead to disruption of sleep patterns, negative impacts to cognitive development, and memory.31, 32 Furthermore, games and social media engagement activates the brains rewards system, which makes control of ST difficult for adolescents whose brains lack the capacity for self-regulation. This may be one reason we may have found smaller effects for ST outcomes than for PA outcomes. Counteracting these design features may require more thoughtful evidence based approaches.33 Taken as a whole, the evidence from multiple studies examining different individual level behavioral theories within FLASHE data, is consistent when expanded to the parent-adolescent dyad. This important development suggests further shifting the focus from the individual exclusively as the unit of analysis to the wider family and social setting.
A limitation is the cross-sectional observational design of the study, making it impossible to assess whether perceived competence or motivational self-regulation influences change in PA or ST over time. Other limitations are the use of single item scales for certain constructs (reducing the sensitivity of measure) and that only self-reported PA and ST measures were used (although adolescent PA data were calibrated with accelerometry). However, a strength of self-report and a reason why it should be used in conjunction with objective measures is that we can gain insight into the context (e.g. questionnaires specifically asked school vs. home or leisure-time vs. structured) in which adolescents engaged in PA behaviors.34 While not a focus of this study, such information may provide an opportunity to identify settings in which interventions would be likely to have the most impact, or perhaps point to a need to tailor the components of an intervention by setting.
Our findings support those of previous studies showing that theory-based behavioral models do explain both intrapersonal effects11, 12, 27, 28 and additionally, interpersonal effects.29 However, the finding that greater parental motivation for PA was associated with greater adolescent motivation for PA but lower PA behavior was unexpected. Likewise, parental motivation to reduce ST was associated with adolescent’s motivation to do the same but not the other way around. The direction of these associations may reflect different reasons for engaging in "health behavior" between parents and their adolescents. For example, in response to being pushed to be active by their parents, adolescents may feel less autonomy and therefore do less activity or parents may engage in ST for different reasons than their adolescents (i.e., work rather than play or social interaction). This may also highlight the importance of family engagement in activities, or for parents to support their adolescent’s autonomous motivation for exercise or limiting ST, which was most strongly associated with their behaviors in this study.
To effectively change health behaviors, multilevel strategies that consider both personal level factors as well as family, school and social contexts are critical.35 Nonetheless, improving our understanding of whether there are psychosocial factors that can be targeted by interventions to support the adoption and or maintenance of healthy lifestyle behaviors in adolescents and within the family unit is valuable for improving future health outcomes. Underpinning interventions with robust theory-based models that can support behavior change across multiple levels is paramount to their success. Further, while the degree to which SDT could be expanded to the dyadic context was relatively unknown, this study suggests further exploration may be worthwhile. Specifically, including more complete SDT-based assessments and using objective measures of behavioral outcomes may improve the degree to which theoretical models are useful for understanding behaviors across multiple settings. Models that more adequately include information about the environments in which behaviors are likely to take place are also important (i.e., home vs. school). Motivational self-regulation of parents and adolescents are surely related; however, longitudinal studies that can help to evaluate whether changes in SDT constructs are associated with improved positive behaviors like PA and limiting sedentary ST patterns over time are needed.
Highlights.
Physical activity and screen time are bi-directionally related in parent-adolescent dyads
Self-Determination Theory can be extended from intra- to inter-personal settings
Assessments of health behaviors should include family and social contexts
Acknowledgements:
We would like to extend our thanks to the participants of the FLASHE study for their willingness to participate in surveys and provide data on their behaviors and experiences.
Funding
This work is partially supported by the Cancer Center Support Grant from the National Cancer Institute to the Comprehensive Cancer Center of Wake Forest Baptist Medical Center (P30 CA012197).
Abbreviations
- FLASHE, Family
Life Activity Sun Health and Eating Study
- PA
Physical Activity
- ST
Screen Time
- SDT
Self-Determination Theory
- APIM
Actor-partner interdependence models
- CVD
cardiovascular disease
- SEM
structural equation modelling
Footnotes
Conflicts of Interest:
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lanoye A, Brown KL, LaRose JG. The Transition into Young Adulthood: a Critical Period for Weight Control. Curr Diabetes Rep Nov 2017;17(11):114. doi: 10.1007/s11892-017-0938-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daniels SR. Complications of obesity in children and adolescents. International journal of obesity. Apr 2009;33 Suppl 1(S1):S60–5. doi: 10.1038/ijo.2009.20 [DOI] [PubMed] [Google Scholar]
- 3.Foltz JL, Belay B, Dooyema CA, Williams N, Blanck HM. Childhood Obesity Research Demonstration (CORD): the cross-site overview and opportunities for interventions addressing obesity community-wide. Child Obes. Feb 2015;11(1):4–10. doi: 10.1089/chi.2014.0159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilson DK, Sweeney AM, Kitzman-Ulrich H, Gause H, St. George SM. Promoting Social Nurturance and Positive Social Environments to Reduce Obesity in High-Risk Youth. Clinical Child and Family Psychology Review. Mar 2017;20(1):64–77. doi: 10.1007/s10567-017-0230-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gordon-Larsen P, Nelson MC, Popkin BM. Longitudinal physical activity and sedentary behavior trends. American Journal of Preventive Medicine Nov 2004;27(4):277–283. doi: 10.1016/j.amepre.2004.07.006 [DOI] [PubMed] [Google Scholar]
- 6.Golden SD, Earp JA. Social ecological approaches to individuals and their contexts: twenty years of health education & behavior health promotion interventions. Health Educ Behav. Jun 2012;39(3):364–72. doi: 10.1177/1090198111418634 [DOI] [PubMed] [Google Scholar]
- 7.Gourlan M, Bernard P, Bortolon C, et al. Efficacy of theory-based interventions to promote physical activity. A meta-analysis of randomised controlled trials. Health psychology review. 2016;10(1):50–66. doi: 10.1080/17437199.2014.981777 [DOI] [PubMed] [Google Scholar]
- 8.Dishman RK, Motl RW, Saunders R, et al. Self-efficacy partially mediates the effect of a school-based physical-activity intervention among adolescent girls. Prev Med. May 2004;38(5):628–36. doi: 10.1016/j.ypmed.2003.12.007 [DOI] [PubMed] [Google Scholar]
- 9.Motl RW, Dishman RK, Saunders RP, et al. Examining social-cognitive determinants of intention and physical activity among Black and White adolescent girls using structural equation modeling. Health Psychology. Sep 2002;21(5):459–467. doi: 10.1037//0278-6133.21.5.459 [DOI] [PubMed] [Google Scholar]
- 10.Lampard AM, Jurkowski JM, Davison KK. Social-cognitive predictors of low-income parents' restriction of screen time among preschool-aged children. Heal Educ Behav Official Publ Soc Public Heal Educ. 2012;40(5):526–30. doi: 10.1177/1090198112467800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith JJ, Morgan PJ, Lonsdale C, Dally K, Plotnikoff RC, Lubans DR. Mediators of change in screen-time in a school-based intervention for adolescent boys: findings from the ATLAS cluster randomized controlled trial. Journal of Behavioral Medicine. Jun 2016;40(3):423–433. doi: 10.1007/s10865-016-9810-2 [DOI] [PubMed] [Google Scholar]
- 12.Patti Jean N. Screen Smart: Evaluation of a Brief School Facilitated and Family Focused Intervention to Encourage Children to Manage Their Screen-Time. Journal of Child and Adolescent Behaviour. 2014;02(01)doi: 10.4172/2375-4494.1000124 [DOI] [Google Scholar]
- 13.Fitzpatrick SL, Appel LJ, Bray B, Brooks N, Stevens VJ. Predictors of Long-Term Adherence to Multiple Health Behavior Recommendations for Weight Management. Health Education & Behavior. Dec 2018;45(6):997–1007. doi: 10.1177/1090198118757823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year follow-up of behavioral, family-based treatment for obese children. JAMA. Nov 21 1990;264(19):2519–23. doi: 10.1001/jama.1990.03450190051027 [DOI] [PubMed] [Google Scholar]
- 15.Janicke DM, Sallinen BJ, Perri MG, et al. Comparison of Parent-Only vs Family-Based Interventions for Overweight Children in Underserved Rural Settings. Archives of Pediatrics & Adolescent Medicine. Dec 2008;162(12):1119–25. doi: 10.1001/archpedi.162.12.1119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu L, Sun S, He Y, Jiang B. The effect of interventions targeting screen time reduction: A systematic review and meta-analysis. Medicine (Baltimore) Jul 2016;95(27):e4029. doi: 10.1097/MD.0000000000004029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oh AY, Davis T, Dwyer LA, et al. Recruitment, Enrollment, and Response of Parent–Adolescent Dyads in the FLASHE Study. American Journal of Preventive Medicine. Jun 2017;52(6):849–855. doi: 10.1016/j.amepre.2016.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nebeling LC, Dwyer L, Oh A, Hennessy E. The Family Life, Activity, Sun, Health and Eating Study: A public use data resource for individual and dyadic analyses of cancer preventive behaviors. Cancer Research. 2017;77(13 Supplement 1)doi: 10.1158/1538-7445.AM2017-4227 [DOI] [Google Scholar]
- 19.Nebeling LC, Hennessy E, Oh AY, et al. The FLASHE Study: Survey Development, Dyadic Perspectives, and Participant Characteristics. American Journal of Preventive Medicine. Jun 2017;52(6):839–848. doi: 10.1016/j.amepre.2017.01.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saint-Maurice PF, Welk GJ. Web-Based Assessments of Physical Activity in Youth: Considerations for Design and Scale Calibration. J Med Internet Res. Dec 1 2014;16(12):e269. doi: 10.2196/jmir.3626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saint-Maurice PF, Kim Y, Hibbing P, Oh AY, Perna FM, Welk GJ. Calibration and Validation of the Youth Activity Profile: The FLASHE Study. Am J Prev Med. Jun 2017;52(6):880–887. doi: 10.1016/j.amepre.2016.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taverno Ross SE, Larson N, Graham DJ, Neumark-Sztainer D. Longitudinal changes in physical activity and sedentary behavior from adolescence to adulthood: comparing U.S.-born and foreign-born populations. J Phys Act Health Mar 2014;11(3):519–27. doi: 10.1123/jpah.2011-0359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Validation Studies. Med Sci Sports Exerc. Aug 2003;35(8):1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 24.Fogelholm M, Malmberg J, Suni J, et al. International Physical Activity Questionnaire: Validity against fitness. Med Sci Sports Exerc. Apr 2006;38(4):753–60. doi: 10.1249/01.mss.0000194075.16960.20 [DOI] [PubMed] [Google Scholar]
- 25.Williams GC, Deci EL. Internalization of biopsychosocial values by medical students: a test of self-determination theory. J Pers Soc Psychol. Apr 1996;70(4):767–79. doi: 10.1037//0022-3514.70.4.767 [DOI] [PubMed] [Google Scholar]
- 26.Ryan RM, Connell JP. Perceived locus of causality and internalization: examining reasons for acting in two domains. J Pers Soc Psychol. Nov 1989;57(5):749–61. doi: 10.1037//0022-3514.57.5.749 [DOI] [PubMed] [Google Scholar]
- 27.Burns RD. Enjoyment, self-efficacy, and physical activity within parent-adolescent dyads: Application of the actor-partner interdependence model. Prev Med Sep 2019;126:105756. doi: 10.1016/j.ypmed.2019.105756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Joyal-Desmarais K, Lenne RL, Panos ME, et al. Interpersonal effects of parents and adolescents on each other’s health behaviours: a dyadic extension of the theory of planned behaviour. Psychology & Health. May 2019;34(5):569–589. doi: 10.1080/08870446.2018.1549733 [DOI] [PubMed] [Google Scholar]
- 29.Wiseman KP, Patel M, Dwyer LA, Nebeling LC. Perceived weight and barriers to physical activity in parent–adolescent dyads. Health Psychology. Aug 2018;37(8):767–774. doi: 10.1037/hea0000635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levesque CS, Williams GC, Elliot D, Pickering MA, Bodenhamer B, Finley PJ. Validating the theoretical structure of the Treatment Self-Regulation Questionnaire (TSRQ) across three different health behaviors. Health Education Research. Oct 2006;22(5):691–702. doi: 10.1093/her/cyl148 [DOI] [PubMed] [Google Scholar]
- 31.Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. Jun 2015;21:50–8. doi: 10.1016/j.smrv.2014.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stiglic N, Viner RM. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ open. Jan 3 2019;9(1):e023191. doi: 10.1136/bmjopen-2018-023191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rich M. Moving from child advocacy to evidence-based care for digital natives. JAMA Pediatr May 2014;168(5):404–6. doi: 10.1001/jamapediatrics.2014.55 [DOI] [PubMed] [Google Scholar]
- 34.Welk GJ, Saint-Maurice PF, Kim Y, et al. Understanding and Interpreting Error in Physical Activity Data: Insights from the FLASHE Study. American Journal of Preventive Medicine. Jun 2017;52(6):836–838. doi: 10.1016/j.amepre.2017.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Laverack G. The Challenge of Behaviour Change and Health Promotion. Challenges. 2017;8(2)doi: 10.3390/challe8020025 [DOI] [Google Scholar]


