Abstract
Background:
Accessible and quality care during the perinatal period is critical for optimal maternal and neonatal health. Using the socio-ecological model, the purpose of this study was to explore barriers and facilitators that shape the perinatal care experiences of people with intellectual and/or developmental disabilities (IDD).
Methods:
Semi-structured interviews were conducted with 10 individuals with IDD in Ontario, Canada, who had given birth within the last 5 years. Interviews focused on care experiences before, during, and after pregnancy. Data were analyzed using a directed content analysis approach, and the socio-ecological model guided analysis.
Results:
Barriers at the societal (e.g., cultural norms of motherhood), policy/institutional (e.g., child protection policies and practices), interpersonal (e.g., inadequate formal and informal support), and intrapersonal levels (e.g., internalized stigma) contributed to participants having negative perinatal care experiences. Conversely, we identified facilitators on the interpersonal level (e.g., positive interactions with perinatal care providers and familial and social service supports) as positively shaping participants’ perinatal care experiences.
Conclusions:
Findings reveal that the perinatal care experiences of people with IDD are shaped by several interrelated factors that largely stem from societal-level barriers, such as dominant (stigmatizing) discourses of disability. To improve the perinatal care experiences of people with IDD, there is a need for interventions at multiple levels. These include the development of policies to support perinatal care for diverse populations and training care providers to enact policies at the institutional and interpersonal levels.
Introduction
Access to health care that is free of attitudinal, communication, and physical barriers is a human right (United Nations, 2006). Perinatal care that is accessible and appropriate, based on individual social and medical needs, may mitigate risks of adverse perinatal outcomes (Laditka et al., 2005; Ronsmans et al., 2006). Yet, multiple intersecting factors make accessing appropriate care before, during, and after pregnancy challenging for women with disabilities (Davis et al., 2014; Gibson & Mykitiuk, 2012).
Among women with disabilities, those with intellectual and/or developmental disabilities (IDD) encounter pronounced barriers accessing health care and are at greater risk for perinatal complications than those without IDD (Abells et al., 2016; Sundelin et al., 2018; Tarasoff et al., 2020a). IDD encompasses a range of disabilities that manifest during the developmental period (e.g., autism spectrum disorder [ASD], Down syndrome, fetal alcohol spectrum disorder [FASD], intellectual disability) (Davis et al., 2014; Harris, 2006; Brown, Wehmeyer et al., 2017) and are characterized by cognitive challenges and limitations in practical, social, or conceptual skills. Individuals with IDD experience significant socioeconomic and health disparities, including high rates of poverty, unstable housing, low educational attainment, unemployment, violence, and mental illness (Fisher et al., 2016; Lunsky et al., 2014; Parish et al., 2009). These factors increase risks for perinatal complications among women with IDD (Brown, Cobigo et al., 2017; Kim & Saada, 2013; Luo et al., 2006; Mitra, Parish, et al., 2015). Given these risks, there is a need to understand the perinatal care experiences of women with IDD and how their care experiences may shape outcomes. This information can enable stakeholders at multiple levels to develop tailored interventions to support women with IDD in the perinatal period.
Several qualitative studies have explored perinatal care experiences of women with IDD, showing challenges in accessing and navigating care. These studies have found women with IDD experience barriers related to communication and involvement in decision-making (Potvin et al., 2016) and lack of adequate informational and emotional support (Llewellyn & McConnell, 2002; Potvin et al., 2016). They also highlighted experiences related to providers’ negative attitudes about childbearing (Walsh-Gallagher et al., 2012) and scrutiny about parenting abilities (Xie & Gemmill, 2018), and maternal anxiety about child custody (Höglund & Larsson, 2013). While this emerging literature identifies important factors that shape the ability of women with IDD to access equitable perinatal care, these studies are limited in several ways. Some only focused on specific aspects of perinatal care (e.g., social support; Potvin et al., 2016) or presented findings of women with IDD together with those with other disabilities, and thus did not highlight experiences specific to women with IDD (Walsh-Gallagher et al., 2012). One study was a thematic analysis of notes in patients’ medical records (Xie & Gemmill, 2018), rather than exploring the perspectives of women with IDD themselves. Two studies from women’s perspectives were based on small sample sizes (e.g., N=4, Potvin et al., 2016; N=1, Rogers et al., 2017). Therefore, there is limited information from the perspectives of women with IDD themselves about how different factors shape their overall perinatal care experiences.
Theoretical models inform explanations of behavioral, social, and structural influences on processes such as perinatal care experiences and can be a useful guide for research, practice, and policy development. The Socio-Ecological Model (SEM) is one such framework that describes how health inequity results from an interplay of factors beyond individual (intrapersonal) characteristics and behaviors (McLeroy et al., 1988). There are five levels of the SEM that shape health care access experiences, including intrapersonal factors (e.g., knowledge, attitudes, self-concept), interpersonal factors (e.g., formal and informal supports), institutional factors (e.g., health care systems), policy factors (e.g., laws and policies), and community factors (e.g., media). Newer iterations of this model also consider societal factors (e.g., social and cultural norms) (WHO, 2011). Although the SEM has been used as a framework to understand the perinatal care experiences of other marginalized groups, such as low-income women (Downe et al., 2009; Sword, 1999) and women living with HIV (Onono et al., 2015), to our knowledge, no qualitative study has used the SEM to examine factors that shape the perinatal care experiences of those with IDD.
The purpose of this study, therefore, was to use the SEM to examine factors that shape the perinatal care experiences of people with IDD in Ontario, Canada.
Methods
This study is part of a larger study examining the perinatal health care experiences of people with physical, sensory, and intellectual and/or developmental disabilities who had recently given birth in Ontario, Canada. The study received ethics approval from the University of Toronto Health Sciences Research Ethics Board. We use the language of “people,” as not all participants identified as cisgender women.
Sampling and Recruitment
Convenience sampling was used for recruitment, with practical purposeful sampling (Suri, 2011) to attain a range of information-rich experiences considering disability and other characteristics, notably race/ethnicity and geography. Study flyers were distributed electronically to over 100 organizations and groups that serve people with disabilities and/or pregnant and parenting people across Ontario. Participants were also recruited through networks of the research team and an Advisory Committee comprising over 30 individuals, including clinicians, staff from disability community organizations, provincial policy representatives, and women with disabilities, several of whom were parents. Interested individuals contacted the study coordinator and were screened by telephone to determine eligibility. To participate, individuals had to (a) identify as or be identified (e.g., by a service for adults with IDD or via enrollment in a disability-related government assistance program that requires an IDD diagnosis) as having an intellectual and/or developmental disability, (b) reside in Ontario, (c) be 18 years of age or older, (d) have given birth in the last five years, (e) be able to converse in English, and (f) be able to consent to participate in research. The criterion of birth within 5 years is consistent with related studies (e.g., Potvin et al., 2016); recall bias has been shown to not be a concern within 5 years postpartum (Takehara et al., 2014). To assess capacity to consent, participants were asked questions regarding understanding of voluntariness, the right to withdraw consent at any time without consequences, and the right to refuse to answer questions (Arscott et al., 1998).
Data Collection
Before the interview, participants provided written consent and completed a demographic questionnaire, which included items such as age, relationship status, racial/ethnic background, and level of education. Participants completed the questionnaire independently, though they had the option of completing the questionnaire with a support person or having the interviewers read the questionnaire aloud; for one of the participants who was interviewed via Zoom, the interviewers read the questionnaire aloud to the participant.
Using a semi-structured guide that was developed with input from the Advisory Committee, qualitative interviews were conducted with 10 individuals with IDD between July 2019 and February 2020. Six of the interviews were conducted in person and the remainder were conducted by telephone or Zoom. Interviews were conducted by a public health researcher and a peer researcher (woman with a disability), and averaged about 1 hour in duration (range 36–98 minutes). At their request, five participants had a support person (e.g., parent, caseworker) present during the interview. These individuals signed a confidentiality agreement before the interview. While some support persons actively participated in the interviews (e.g., clarifying or adding to participants’ responses), their responses are not included herein.
The interviews followed the chronology of the participants’ most recent perinatal care experience (if they had more than one pregnancy); participants were asked about the time before pregnancy, initiation of prenatal care, care during pregnancy, labour and delivery, and the early postpartum period. They were asked about what types of care or services they accessed at each stage, if services met their needs, and what they recommended to improve care. See Appendix A for a summary of the interview guide.
Participants were reminded throughout the interview that they could take breaks as needed and that they were not obligated to answer any question they did not want to answer. After the interview, participants received a $50 gift card (e.g., from a grocery store) and a list of resources regarding mental health, social services, and violence against women, in recognition that interviews might evoke upsetting experiences (e.g., child apprehension).
Data Analysis
Interviews were transcribed intelligent verbatim (e.g., false starts and utterances such as “um” were omitted) and were verified by the interviewers for accuracy. Identifying information was removed and names replaced by pseudonyms. Guided by a directed content analysis approach (Hsieh & Shannon, 2005), the SEM (McLeroy et al., 1988) was used to develop the initial coding framework. Two transcripts were first independently line-by-line coded by the first and last author to identify emergent codes and constructs associated with each level of the SEM that relate to perinatal care experiences. The second and third authors also reviewed these two transcripts. Through discussion and coding of two more transcripts, the first and last author modified the coding framework to reflect emergent codes, specifically collapsing the institutional and policy levels, and adding a societal level, consistent with recent iterations of the SEM (World Health Organization, 2020). The coding framework was then constructed in NVivo 10, wherein all data were coded. Theme memos were generated and discussed with the larger team.
Several steps were taken to ensure rigor and credibility of the data collection and analysis processes and, in turn, the study findings. After each interview, the interviewers wrote field notes to capture key points, to highlight similarities and differences in participants’ experiences, and to maintain reflexivity and awareness. The notes were reviewed after each interview to minimize personal and intellectual biases before interactions with future study participants, and reviewed again by the first and last author as part of the data analysis process. In addition to having two authors independently code all of the transcripts, analyst triangulation (Patton, 1999) was implemented through discussions with the larger research team. An overview of the findings was also shared with the study Advisory Committee.
Results
Participants
Participant characteristics are detailed in Table 1. Self-identified IDD included autism, cognitive delay, chromosomal abnormalities, and FASD. Four participants identified as also having a physical or sensory disability, and several reported experiencing other disabilities and health conditions (e.g., anxiety, attention-deficit/hyperactivity disorder, learning disability, and depression). Most participants were under the age of 35 years, and half were married or in a committed relationship. Most identified as heterosexual and as cisgender women. Seven identified as White and only one was born outside of Canada. Six resided in large urban centres in southern Ontario, and four in medium-sized and small towns in central and northern Ontario. Annual household incomes were low, with many participants indicating they received government assistance and lived in subsidized housing. Only one participant had completed education beyond high school, and one was working (part-time). All but one participant had experienced their most recent birth within 3.5 years of data collection; two participants were interviewed within 6 months of their most recent birth. All participants experienced their most recent birth in a hospital setting. Seven participants had two or more children, though at data collection, three did not have all their children living with them or in their custody. Four previously experienced a pregnancy loss or termination (Table 2).
Table 1.
Select Socio-demographic Characteristics of Study Participants
| Characteristic | N=10 |
|---|---|
| Disability | |
| Intellectual and/or developmental disability (IDD) | |
| Chromosomal abnormality (missing and extra) | 1 |
| Cognitive delay | 1 |
| Fetal alcohol spectrum disorder | 1 |
| IDD - not specified* | |
| Multiple mild intellectual disabilities | 1 |
| IDD + Physical Disability | |
| Autistic + Ehlers-Danlos syndrome | 1 |
| Chromosomal abnormality (missing) + scoliosis | 1 |
| IDD + Sensory Disability | |
| Developmental disability + severe hearing loss | 1 |
| Intellectual disability + legally blind in the right eye | 1 |
| Age | |
| 18–25 | 2 |
| 26–34 | 7 |
| 35–44 | 1 |
| Racial/Ethnic Background † | |
| White | 7 |
| Racialized (e.g., Black, Metis, Filipino) | 5 |
| Gender Identity | |
| Woman | 9 |
| Genderqueer or non-binary | 1 |
| Sexual Orientation | |
| Heterosexual | 8 |
| Bisexual or queer | 2 |
| Relationship Status | |
| Single | 4 |
| Married or common-law | 5 |
| Separated | 1 |
| Highest Level of Education | |
| Less than high school | 4 |
| High school | 5 |
| College | 1 |
| Annual Household Income (CAD) | |
| $0–$19,999 | 5 |
| $20,000–$39,999 | 3 |
| $40,000 or more‡ | 2 |
| Geographic Place of Residence | |
| Small town (population < 10,000) | 3 |
| Medium-sized city (population 10,000–100,000) | 1 |
| Large city (population > 100,000) | 6 |
Specific IDD or diagnosis not reported. We know these individuals met our study criteria based on where they were recruited from (e.g., program for parents with IDD) and/or because they indicated that they received disability-related government assistance (e.g., Ontario Disability Support Program, ODSP).
Total adds up to more than 10. Two participants identified themselves as White and another racial/ethnic background (e.g., Portuguese).
One participant indicated that their household income was between $36,000 and $48,000 and another indicated that it was between $60,000 and $79,999. The latter lived with their mother and received financial assistance through ODSP. Most participants received support from ODSP and lived in subsidized housing. Three participants lived in the same home as their parents, and one of these indicated that they pay rent to their parents.
Table 2.
Select perinatal health and parenting characteristics of study participants (most recent pregnancy unless otherwise specified)
| Characteristic | N=10 |
|---|---|
| Number of children birthed | |
| One | 3 |
| Two | 2 |
| Three | 2 |
| Four | 3 |
| Number of pregnancies | |
| One | 2 |
| Two | 1 |
| Three | 3 |
| Four or more | 3 |
| More than two but number not specified | 1 |
| Pregnancy was planned | |
| Yes | 2 |
| No | 8 |
| Prenatal education course participation (for at least one pregnancy) | |
| Yes | 7 |
| No | 3 |
| Primary perinatal care provider * | |
| Obstetrician | 9 |
| Nurse practitioner | 1 |
| Midwife | 2 |
| Had to travel or relocate to larger city to access specialist or higher level of care during pregnancy and/or for labor and delivery | |
| Yes | 3 |
| No | 7 |
| Involvement with child protection services (past or current) | |
| Yes | 5 |
| No | 5 |
Total adds up to more than 10. Some participants had more than one primary perinatal care provider or had their care transferred to a different provider (e.g., from nurse practitioner to obstetrician), in some cases to a different city, later in pregnancy.
Findings
We used the SEM to examine factors that shape the perinatal care experiences of people with IDD in Ontario (Figure 1). We identified factors that we understood as positively shaping participants’ perinatal care experiences (i.e., facilitators) and those that negatively shaped them (i.e., barriers) at various levels. We present our findings starting with the societal level to the intrapersonal level, as we posit that factors at higher levels influence factors at lower levels.
Figure 1.
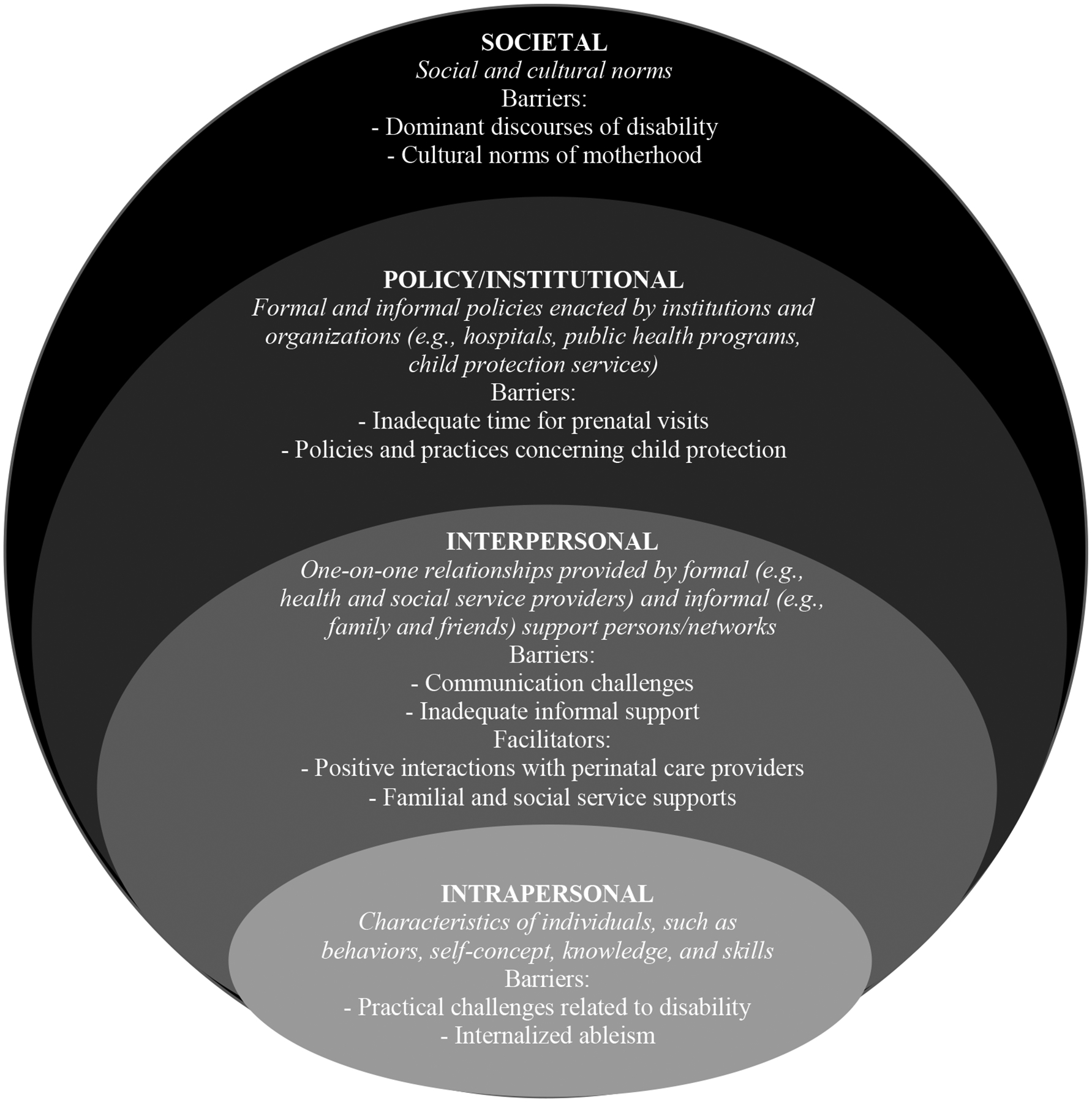
Adapted socio-ecological model of factors at four interconnected levels shaping the perinatal care experiences of people with intellectual and/or developmental disabilities.
Societal Level
We identified dominant discourses about disability and cultural norms of motherhood as two overlapping societal factors that shaped participants’ perinatal care experiences in negative ways.
Barrier: Dominant discourses of disability
Stigmatizing and pathologizing discourses of disability (e.g., disability as defective, an individual problem; Haegele & Hodge, 2016) were common. Some participants, like Maria, shared that they did not disclose their disability to their perinatal health care providers or people generally because they feared how others might perceive them or judge their parenting abilities:
“I just hide who I am. I just don’t want people judging. Not that it’s bad, right? But people think it’s bad … or people could say, ‘How does she take care of the kids if she has a disability?’”
Barrier: Cultural norms of motherhood
Coupled with perceived judgment about their “fitness” for motherhood because of disability, some participants experienced judgment from others, including health care providers, for not adhering to the cultural norms or expectations of motherhood because of their young age or single marital status. Jasmine, one of the younger participants, reported that “a lot of people wanted me to give him [baby] up for adoption.” Conversely, Corey, who was in their 30s, shared that while health care providers “didn’t express any concerns about [their] disability,” they did seem to judge them for pursuing parenthood alone:
“He [family physician] seemed a little judgey about the whole no there being a dad … The one [obstetrician] here in [my hometown] wasn’t necessarily great regarding the whole single thing.”
Policy/Institutional Level
Barriers identified at the policy/institutional level included inadequate time for prenatal visits and institutional and organizational policies that classified or “red flagged” participants as potentially unfit parents because of their disability.
Barrier: Inadequate time for prenatal visits
Some participants explained it was difficult to build a trusting relationship with their perinatal care provider due to the short length of prenatal appointments. When comparing their experiences with doctors and midwives, Crystal said:
“I like the midwife better than the doctors … with the doctor, I wasn’t able to really open up so much about too many things because it was more, ‘Okay, you got 15 minutes’ compared to ‘Okay, you have 45 minutes.’”
When later asked what providers could do to better to support people with disabilities who are pregnant, Crystal recommended that providers “Be more open. Listen to the client. … and [don’t be] so rushy-rushy.”
Barrier: Policies and practices concerning child protection
Five participants indicated they had involvement with child protection services during their most recent pregnancy and/or previous pregnancies, and in a few instances still had open case files. These participants were aware of formal and informal policies that might identify or “flag” them as a high-risk or at-risk parent (i.e., potentially unfit or incapable of parenting), and seemingly understood how the societal factors described above pervaded these policies:
“I was very quiet about my disability for a long time because back in the day I knew Children’s Aid judged people over that … I feel like they red flag you just because you might have a disability. They might be like, ‘Oh maybe she can’t take care of this kid.’”
(Garima)
Overwhelmingly, participants, particularly those who were working to regain custody of an older child while they were pregnant and/or anticipated having to contend with child protection services when their child was born, reported that this involvement had a detrimental impact on their care experience. Laura described the perinatal period as being a “very stressful time because I was also in the middle of getting my oldest home [from child protection services],” and that they “had to jump through every hoop you could think” to get their child back home.
A few participants described being caught off guard when child protection services became involved shortly after their child was born. When asked if child protections services explained why they apprehended their baby, Crystal said, “all they said was ‘previous history’” and “I was an instant red flag at any hospital in [large city]. It wasn’t even a matter of, ‘Hey, prove yourself. Show us that you can do it,’ until after they apprehended her.”
Interpersonal Level
Barriers identified at the interpersonal level included communication challenges with perinatal care providers and inadequate informal support. Facilitators included positive patient-provider interactions and familial and social service supports.
Barrier: Communication challenges
Several participants described poor communication with their perinatal care providers. Garima, who was unable to give birth at their preferred hospital with a midwife felt disrespected by the obstetrician at the hospital where they gave birth as he ignored their birth plan: “I know things can go wrong but it’s like they [obstetrician] weren’t explaining anything and they didn’t respect that I had a pregnancy plan…” Several other participants also shared that perinatal care providers failed to provide adequate explanations for pregnancy and delivery-related processes, which caused them to feel frustrated and anxious. Relatedly, some participants shared that their perinatal care providers used “doctor terms” or medical jargon that was difficult to understand.
As well, some participants reported an unwillingness to disclose their disability or health needs to their care providers as they felt they would not be supported appropriately. These participants perceived their care providers to have limited knowledge or training regarding disability. For instance, when asked why they did not share their disability with their doctor, Danielle said, “[they] probably wouldn’t understand it anyways so I don’t bother.”
Barrier: Inadequate informal support
When asked whom they typically relied on for support, several participants only mentioned a few immediate family members, and some indicated they had little to no support from the fathers of their children.
“My mom has always been involved. … [Son’s] dad has never met him. … I get money from him but I don’t get like the emotional support or anything. … He’s [father of other son] supposed to have, he can have access [to son] but it’s supposed to be supervised and he refuses to do it.”
(Laura)
Very few participants shared that they had close friends or other parents who they relied on for support; few participants had large support networks. Corey noted that while they connected with some peers online, their disability makes socializing in-person with other parents challenging:
“It could have been partly because being autistic too. … I feel okay socializing online but I’m not somebody who really has friends or likes going to social things or anything. … I do have a couple of like parents that I know who are also autistic and have kids, so we meet every now and then. But again, we’re not too social.”
Some participants cited lack of trust of others as the reason for having small social support networks. For example, Danielle stated, “I don’t have friends. I don’t trust people.” Similarly, Garima reported that they “don’t really trust people …. I don’t even invite my mom into my house.” Yet, Garima also shared that their mother was one of their only supports and did help with childcare occasionally. Most participants commented that having more social (family and friends) and informational support, particularly during pregnancy, would have made their perinatal care experience better.
Facilitator: Positive interactions with perinatal care providers
Several participants described positive interactions with perinatal care providers. Some described their providers as “extremely accommodating and caring,” exhibiting “a lot of respect,” “very understanding,” and taking the time to explain “everything to me in detail.” In terms of their disability, Corey explained how their doctor “was not concerned about me being autistic at all. He was like ‘well, I mean, a lot of people who are just a little different happen to be autistic,’ and he figured I would be good parenting that way.” Another participant was grateful that their doctor had taken time to build a trusting relationship with them. Similarly, Crystal, who had a doctor as their primary perinatal care provider for their previous pregnancies, had positive things to say about the midwife they worked with for their most recent pregnancy:
“She [midwife] was awesome. … She turned off every computer in her office, she didn’t write anything down, she was like, ‘Tell me anything you want to tell me, even if it’s about Children Aid, just let it loose,’ you know? And I was able to talk to her and I didn’t feel like she was writing anything down at the time. So I didn’t have to stress that, ‘Oh, no! What is she writing?’ kind of thing. So it kind of made me feel more at ease, to know that she was actually sitting there, listening to me.”
Facilitator: Familial and social service supports
Some participants shared that family members, notably their own mothers, and friends supported them with practical tasks during the perinatal period, including driving and/or accompanying them to appointments, communicating with care providers, and purchasing baby supplies. In a few cases, participants’ family members drove them many hours to another, often larger, city to give birth.
For some participants, public health nurses and disability-related caseworkers provided support, particularly during the postpartum period, such as budgeting, helping to establish routines, completing paperwork to access resources and birth certificates, creating a safe environment for infants, and supporting participants in regaining custody of their children.
“They [developmental disability support worker] were really helpful. Like, they would tell me things that I don’t even know, you know? They would guide me. For instance, if I don’t know how to go to [government agency] and do birth certificate, like a newborn baby, you know?”
(Maria)
“She [caseworker] helps me with all that and I think that’s kind of another reason why [child protection services] felt like they were okay with closing my case because they knew I had other support other than them to help me.”
(Garima)
“With my youngest, if I had the supports I do now [things would have been different with my older children]. … If I would have had all those supports right there in place, it would have probably been a different outcome. But it took me to get [the parenting program worker] and the [developmental disability support service] worker and every other support involved in order for my [youngest] child to be home.”
(Crystal)
Four participants were enrolled in a program for parents with IDD in a large city, wherein caseworkers or program therapists provided individualized, home-based parenting training and support.
Intrapersonal level
We identified disability and the various ways in which disability affected participants’ lives, including how they viewed themselves, as the overarching individual-level factors that shaped participants’ perinatal care experiences. As well, participants’ socio-demographic characteristics and perinatal health and parenting histories were important intrapersonal factors that shaped their perinatal care experiences.
Barrier: Practical challenges related to disability
Having an IDD shaped participants’ perinatal care experiences in several ways. For instance, having an IDD meant that some participants had difficulty with learning (e.g., “processing new information”) and routines, as well as experienced challenges accessing resources and doing other practical things on their own. For example, Maria shared: “It’s hard for me to learn something new and quick. … It’s hard for me to get around … I have trouble doing or finding out something. … I get so anxious doing something so it’s hard for me.” Conversely, for Corey, sensory sensitivities shaped their perinatal care experience: “Like with autism … I’ve had issues with noise sensitivity and with a lot of sensory issues. I haven’t necessarily liked people touching me…”
Barrier: Internalized ableism
Having a disability shaped how participants viewed themselves and how they believed others perceived them. When discussing their disability, it became evident that factors at the societal level shaped participants’ views of themselves, as their self-concept in relation to disability was predominantly negative. For instance, when asked what would have made their perinatal care experience better, Danielle responded, “not having the disability that I have.”
Participants seemed to internalize stigmatizing discourses of disability. As a result, several decided not to disclose their disability to their perinatal care provider:
“I never told the doctors that I had a disability. … [I] felt ashamed. Felt embarrassed. Didn’t want to admit to myself—well, I knew but I was still trying to hide it from myself too, at the same time, and I didn’t want people looking at me different because I had a disability.”
(Crystal)
Relatedly, some participants reported not asking for help or not asking their provider to clarify unclear instructions or simplify confusing terminology out of fear of how their provider might perceive them. Experiencing internalized ableism and in turn not disclosing their disability, however, seemed justified based on participants’ previous experiences:
“I never really thought it was important to share that with those doctors. You know, I was very quiet about my disability for a long time because back in the day I knew Children’s Aid judged people over that. But it’s like at the same time I think I was kind of in denial about my own disability until I was like, ‘Okay. Maybe they’re right. Maybe I can’t handle it.’”
(Garima)
Discussion
Using the SEM as a guiding framework for this qualitative study, we identified stigmatizing discourses of disability, policies and practices concerning child protection services, communication challenges with care providers, and internalized ableism as factors negatively influencing the perinatal care experiences of people with IDD. Although not as common, we also identified facilitators or factors that positively shaped participants’ perinatal care experiences, such as having familial and social service supports.
Our findings are consistent with prior studies on the perinatal care experiences of women with IDD in other high-income countries that focused on factors at specific SEM levels. At the societal level, a study in Australia showed that women with IDD experienced discrimination during pregnancy (Llewellyn & McConnell, 2002). Similarly, a study of mothers with Asperger syndrome in the U.S. found that formal and informal supports, including nurses, communicated expectations about how motherhood should be experienced and judged participants’ parenting skills (Gardner et al., 2016). At the policy/institutional level, mothers with IDD in Sweden reported feeling distressed about custody of their newborns; some moved to another municipality to avoid these challenges and expressed how they would not have had children if they knew the barriers they would face (Höglund & Larsson, 2013). At the interpersonal level, young mothers with disabilities, including those with IDD, in Ireland (Walsh-Gallagher et al., 2012) and mothers with Asperger syndrome in the U.S. (Gardner et al., 2016) similarly reported feeling they had limited say in their perinatal care and that care was not adapted to meet their needs. Like the case study presented by Rogers et al. (2017) and participants in Gardner et al.’s (2016) study, the autistic participant in our study also highlighted sensory modulation challenges as impacting their perinatal care experience.
The current study, guided by the SEM, contributes to the literature by highlighting barriers and facilitators at multiple levels that shape the perinatal care experiences of people with IDD. Notably, factors identified at each level do not necessarily stand on their own. Rather, participants’ experiences can be understood as an outcome of the interaction of factors at various levels, whereby those on the societal level, such as dominant discourses of disability and cultural notions of motherhood, inform factors at lower levels. In contrast to a biomedical model that emphasizes individual characteristics and in turn individual-level interventions (e.g., health behavior change), the SEM acknowledges higher-level factors that shape care experiences and outcomes (Sword, 1999). The SEM is also aligned with the social determinants of health framework, wherein instead of being understood as an individual problem, disability is one of many determinants of health (Krahn & Campbell, 2011). To understand the perinatal care experiences of people with IDD and ultimately improve them, there is a need to consider stigma and how other social determinants of health, systems of oppression, and identities, such as race/racism, gender identity, and geography may interact with or compound experiences of marginalization for people with IDD and shape their perinatal care experiences. Indeed, there is growing evidence that racialized women with IDD are at greater risk of adverse perinatal health outcomes (Rubenstein et al., 2020; Akobirshoev et al., 2020). A multi-level and intersectional focus is consistent with the perinatal health framework for women with disabilities, which suggests that pregnancy outcomes of people with disabilities are the result of factors that interact with one another across the life course (Mitra, Long-Bellil, et al., 2015; Long-Bellil et al., 2020).
This study has some limitations. Although several participants also had physical or sensory disability, our analyses did not address the nuances of having multiple disabilities. Further, while we had a sample of ten participants, a sample size larger than (e.g., Potvin et al., 2016; Rogers et al., 2017) or equivalent to related studies (e.g., Höglund & Larsson, 2013; Xie & Gemmill, 2018), we only had one autistic participant in our study. Recruitment of autistic people who had given birth within the last 5 years proved challenging and we hypothesize that this may be because of gender differences regarding autism presentation and diagnosis (Halladay et al., 2015), resulting in many mothers not receiving an autism diagnosis until later in life, often at the time of their child’s diagnosis or shortly thereafter. Of the eight participants with Asperger syndrome in Gardner et al.’s (2016) study, for instance, only two had a formal diagnosis before giving birth and two participants were unaware that they had an ASD at the time of their pregnancies. As such, future research exploring the perinatal care experiences of autistic people may need to include participants with pregnancies beyond the past 5 years. Also absent from our study were individuals with Down syndrome. More research is needed on the unique perinatal care experiences of individuals with Down syndrome and other IDD, notably those with more significant support needs, as their experiences are largely absent from the literature. While we identified societal and policy/institutional factors from participants’ responses, our interview guide did not specifically target these factors. Based on our findings, we suggest future research further explore these systemic issues. Finally, we highlighted the perinatal care experiences of people with IDD from their own perspectives, which are often overlooked. Missing, however, is an understanding of perinatal care from the perspective of other stakeholders such as physicians and midwives. A greater understanding of provider-identified barriers to care for people with IDD during the perinatal period may in turn shed light on policy/institutional level barriers and how to address barriers at multiple levels.
Implications for Practice and/or Policy
The application of the SEM in our study suggests multi-level intervention strategies. The experiences of study participants suggest that policies, including those that are informal or implicit, are often influenced by stigmatizing discourses of disability that unfairly penalize people with IDD. Policies created and administered by institutions such as hospitals and child protection services require revision so that they foster environments that respect the reproductive and parenting rights of people with IDD. These efforts should occur in tandem with appropriate training for providers who deliver care within these organizations so that people with IDD can be better supported during the perinatal period (Brown et al., 2019). Indeed, there is a growing body of research advocating for disability-related education and training of health and social service providers (Havercamp et al., 2021; Shakespeare & Kleine, 2013; Iezzoni & Long-Bellil, 2012). In addition to didactic lectures, researchers have found experiential learning through community-based centers and prompts for reflexivity enhanced the comfort level and ability of medical and dental students to work with patients with disabilities (Anderson et al., 2010; DeLucia & Davis, 2009). Researchers have also shown the importance of inter-professional education where providers such as social workers, nurses, and physicians benefit from each other’s experiences (Anderson et al., 2010). There are few tailored training resources related to the perinatal care of women with IDD (one example is a toolkit and maternity passport created by researchers in the UK; Cox et al., 2020), though there are some pertaining to reproductive health of women with IDD broadly, such as the Women Be Healthy 2 curriculum (Dickens et al., 2011; Lunsky, Straiko, & Armstrong, 2003). Providers may also benefit from clinical recommendations concerning perinatal care for women with IDD in the Primary Care of Adults with Intellectual and Developmental Disabilities: 2018 Canadian Consensus Guidelines (Sullivan et al., 2018).
People with IDD require holistic support networks that that incorporate formal and informal supports not only during the perinatal period but also before and between pregnancies (Tarasoff et al., 2020b). Preconception and interconception supports for women with IDD are particularly important as women with IDD have been found to experience preconception health disparities (Tarasoff et al., 2020b), to have high rates of mistimed and unintended pregnancy (Horner-Johnson et al., 2020), and to experience short inter-pregnancy intervals (Brown et al., 2018). While there are some existing postpartum and parenting support programs for parents with IDD (e.g., Connections, 2021; Tarleton & Turner, 2015), these programs are scant and tend to be limited to large urban centers and focus on parenting rather than pregnancy. To better support people with IDD and mitigate risks of negative care experiences and outcomes, it is recommended that perinatal care providers work proactively with other health and social service providers (e.g., social workers), IDD organizations, and informal supports to ensure there are supports in place for people with IDD early in, or even before, pregnancy (Xie & Gemmill, 2018).
Our research also suggests that perinatal health care providers should prioritize patient-centered care using a health equity lens; this includes paying attention to the ways in which a patient with IDD may be marginalized and identifying and tailoring care to their learning, communication, and sensory challenges and needs (e.g., demonstrate what is meant instead of just explaining, use of visual aids) (Abells, et al., 2016; Mitra, Parish et al., 2015; Gardner et al., 2016; Long-Bellil et al., 2020; Tint et al., 2021; Sullivan et al., 2018). Attending to the specific needs of people with IDD may require longer and more frequent appointments (Brown et al., 2019; Sullivan et al., 2018). Perinatal care providers should ask people with IDD, and their support persons as appropriate (Sullivan et al., 2018), what works for them and what (or who) they may need to feel informed, comfortable, and supported during the perinatal period. For autistic parents-to-be this may include a discussion of what features of the care setting (e.g., lighting) might trigger unpleasant sensory stimuli, strategizing ways to cope with sensory challenges, and, if possible, working to adjust these features to make care settings more comfortable (Gardner et al., 2016).
Addressing barriers at the policy/institutional and provider levels can help to alleviate barriers at the intrapersonal level such as internalized ableism, which may contribute to pregnant and parenting people with IDD avoiding or delaying accessing care for themselves and their children and in turn may exacerbate adverse health outcomes. People with IDD should feel safe to disclose their disability and disability-related needs, as well as concerns regarding their mental health, during the perinatal period without fear of judgement or mistreatment. Educating and encouraging perinatal care providers to reflect on and move beyond personal bias and assumptions concerning the intersection of pregnancy, parenthood, and disability is essential (Rogers et al., 2017) to better support people with IDD in the perinatal period. Disability-informed and supportive providers may in turn help pregnant and postpartum people with IDD feel empowered.
Conclusion
We identified several factors that may together contribute to negative and positive perinatal care experiences for people with IDD. Like a domino effect, many upstream barriers such as dominant discourses of disability and cultural norms of motherhood influence barriers identified at the policy/institutional, interpersonal, and intrapersonal levels. Although shared social and cultural norms may be difficult to address, interventions such as increased disability education for perinatal care providers and holistic support networks that take a life course approach can optimize perinatal care for people with IDD.
Supplementary Material
Acknowledgements:
The authors wish to acknowledge the study participants for their essential contributions to this research. The authors also wish to express thanks to the members of the Disability and Pregnancy Study Advisory Committee who assisted with recruitment, development of the data collection materials, and provided feedback on preliminary findings.
Funding Statement:
This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (Award 5R01HD092326 to Hilary K. Brown and Yona Lunsky). This research was undertaken, in part, thanks to funding from the Canada Research Chairs Program to Hilary K. Brown. Lesley A. Tarasoff is supported by a Canadian Institutes of Health Research Postdoctoral Fellowship. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Author Biographies
Momina Khan, BSc, is a Master of Public Health student at the Dalla Lana School of Public Health at the University of Toronto. Her research interests are diverse but focus largely on reproductive and child health.
Hilary K. Brown, PhD, is an Assistant Professor in the Department for Health and Society at the University of Toronto Scarborough. Her research interests lie at the intersection of maternal and child health and disability and chronic disease epidemiology.
Yona Lunsky, PhD, C.Psych., is the Director of the Azrieli Adult Neurodevelopmental Centre at the Centre for Addiction and Mental Health. Her research focuses on the mental health needs of individuals with intellectual and developmental disabilities and their families.
Kate Welsh, MEd, is a disability community activist, feminist artist, educator, and disabilityaffirming mental health counsellor. She is a Peer Research Assistant in the Department of Health and Society at the University of Toronto Scarborough.
Susan M. Havercamp, PhD, FAAIDD, is an Associate Professor in the Department of Psychiatry and Behavioral Health at the Ohio State University Nisonger Center. Her research explores health surveillance, health promotion, and health care training for people with disabilities.
Laurie Proulx, B.Com., has lived with a disability for much of her life, including the pregnancies of her two children. She is a Vice-President with the Canadian Arthritis Patient Alliance, and a Peer Research Assistant at the University of Toronto Scarborough.
Lesley A. Tarasoff, PhD, is a Postdoctoral Research Fellow at the University of Toronto Scarborough and the Centre for Addiction and Mental Health. Her research explores the reproductive and perinatal health of stigmatized women, notably women with disabilities and bisexual women.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interest: The authors have no conflicts to disclose.
References
- Abells D, Kirkham YA, & Ornstein MP (2016). Review of gynecologic and reproductive care for women with developmental disabilities. Current Opinion in Obstetrics & Gynecology, 28(5), 350–358. 10.1097/GCO.0000000000000299 [DOI] [PubMed] [Google Scholar]
- Akobirshoev I, Mitra M, Parish SL, Valentine A, & Simas T (2020). Racial and Ethnic Disparities in Birth Outcomes and Labor and Delivery Charges Among Massachusetts Women With Intellectual and Developmental Disabilities. Intellectual and Developmental Disabilities, 58(2), 126–138. 10.1352/1934-9556-58.2.126 [DOI] [PubMed] [Google Scholar]
- Anderson ES, Smith R, & Thorpe LN (2010). Learning from lives together: medical and social work students’ experiences of learning from people with disabilities in the community. Health & Social Care in the Community, 18(3), 229–240. 10.1111/j.1365-2524.2010.00921.x [DOI] [PubMed] [Google Scholar]
- Arscott K, Dagnan D, & Kroese BS (1998). Consent to psychological research by people with an intellectual disability. Journal of Applied Research in Intellectual Disabilities, 11(1), 77–83. 10.1111/j.1468-3148.1998.tb00035.x [DOI] [Google Scholar]
- Brown HK, Cobigo V, Lunsky Y, & Vigod SN (2017). Maternal and offspring outcomes in women with intellectual and developmental disabilities: a population- based cohort study. BJOG: An International Journal of Obstetrics & Gynaecology, 124(5), 757–765. 10.1111/1471-0528.14120 [DOI] [PubMed] [Google Scholar]
- Brown HK, Cobigo V, Lunsky Y, & Vigod S (2019). Reproductive health in women with intellectual and developmental disabilities in Ontario: Implications for policy and practice. Healthcare Quarterly, 21, 6–9. 10.12927/hcq.2019.2574 [DOI] [PubMed] [Google Scholar]
- Brown HK, Ray JG, Liu N, Lunsky Y, & Vigod SN (2018). Rapid repeat pregnancy among women with intellectual and developmental disabilities: a population-based cohort study. CMAJ, 190(32), E949–E956. 10.1503/cmaj.170932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown I, Wehmeyer ML, & Shogren KA (2017). What is meant by the terms intellectual disability and developmental disabilities? In Wehmeyer ML, Brown I, Percy M, Shogren KA, & Fung WLA (Eds.), A Comprehensive Guide to Intellectual and Developmental Disabilities (2nd ed., pp. 7–18). Baltimore, MD: Paul H. Brookes Publishing. [Google Scholar]
- Connections Counselling and Consulting Foundation. (2021). Connections. Calgary, Alberta, Canada Retrieved from http://www.connectionscounselling.ab.ca/
- Cox A, Gallagher A, Watkins S, & Parsons C (2020). The Together Project: Supporting the delivery of good practice in maternity services for parents with learning disabilities. University of Surrey, UK. Retrieved from https://www.surrey.ac.uk/research-projects/together-project-supporting-delivery-good-practice-maternity-services-parent-slearning-disabilities#more [Google Scholar]
- Davis R, Proulx R, & van Schrojenstein Lantman-de Valk H (2014). Health issues for people with intellectual disabilities: the evidence base. In Taggart L & Cousins W (Eds.), Health Promotion for People with Intellectual and Developmental Disabilities, (1st ed., pp. 7–16). Berkshire, England: Open University Press/McGraw-Hill Education. [Google Scholar]
- DeLucia LM, & Davis EL (2009). Dental students’ attitudes toward the care of individuals with intellectual disabilities: relationship between instruction and experience. Journal of Dental Education, 73(4), 445–453. 10.1002/j.0022-0337.2009.73.4.tb04715.x [DOI] [PubMed] [Google Scholar]
- Dickens P, Luken K, Parish SL, & Swaine JG (2011). Women Be Healthy 2: A curriculum to increase cervical and breast cancer screening rates of women with intellectual and developmental disabilities. Chapel Hill, NC: North Carolina Office on Disability and Health. Retrieved from https://fpg.unc.edu/publications/women-be-healthy-2-curriculum-increase-cervical-and-breast-cancer-screening-rates-women [Google Scholar]
- Downe S, Finlayson K, Walsh D, & Lavender T (2009). ‘Weighing up and balancing out’: a meta- synthesis of barriers to antenatal care for marginalised women in high- income countries. BJOG: An International Journal of Obstetrics & Gynaecology, 116(4), 518–529. 10.1111/j.1471-0528.2008.02067.x [DOI] [PubMed] [Google Scholar]
- Fisher MH, Baird JV, Currey AD, & Hodapp RM (2016). Victimisation and Social Vulnerability of Adults with Intellectual Disability: A Review of Research Extending beyond Wilson and Brewer. Australian Psychologist, 51(2), 114–127. 10.1111/ap.12180 [DOI] [Google Scholar]
- Gardner M, Suplee PD, Bloch J, & Lecks K (2016). Exploratory study of childbearing experiences of women with Asperger syndrome. Nursing for Women’s Health, 20(1), 28–37. 10.1016/j.nwh.2015.12.001 [DOI] [PubMed] [Google Scholar]
- Gibson BE, & Mykitiuk R (2012). Health care access and support for disabled women in Canada: falling short of the UN Convention on the Rights of Persons with Disabilities: a qualitative study. Women’s Health Issues, 22(1), e111–e118. 10.1016/j.whi.2011.07.011 [DOI] [PubMed] [Google Scholar]
- Haegele JA & Hodge S (2016). Disability Discourse: Overview and Critiques of the Medical and Social Models, Quest, 68(2), 193–206. 10.1080/00336297.2016.1143849 [DOI] [Google Scholar]
- Halladay AK, Bishop S, Constantino JN, Daniels AM, Koenig K, Palmer K, Messinger D, Pelphrey K, Sanders SJ, Singer AT, Taylor JL, & Szatmari P (2015). Sex and gender differences in autism spectrum disorder: summarizing evidence gaps and identifying emerging areas of priority. Molecular Autism, 6, 36. 10.1186/s13229-015-0019-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris JC (2006). Intellectual Disability: Understanding Its Development, Causes, Classification, Evaluation, and Treatment. New York, NY: Oxford University Press. [Google Scholar]
- Havercamp SM, Barnhart WR, Robinson AC, & Smith CNW (2021). What should we teach about disability? National consensus on disability competencies for health care education. Disability and Health Journal, 14(2), 100989. 10.1016/j.dhjo.2020.100989 [DOI] [PubMed] [Google Scholar]
- Horner-Johnson W, Dissanayake M, Wu JP, Caughey AB, & Darney BG (2020). Pregnancy intendedness by maternal disability status and type in the United States. Perspectives on Sexual and Reproductive Health, 52(1), 31–38. 10.1363/psrh.12130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Höglund B, & Larsson M (2013). Struggling for motherhood with an intellectual disability—a qualitative study of women’s experiences in Sweden. Midwifery, 29(6), 698–704. 10.1016/j.midw.2012.06.014 [DOI] [PubMed] [Google Scholar]
- Hsieh HF, & Shannon SE (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, & Long-Bellil LM (2012). Training physicians about caring for persons with disabilities: “Nothing about us without us!”. Disability and Health Journal, 5(3), 136–139. 10.1016/j.dhjo.2012.03.003 [DOI] [PubMed] [Google Scholar]
- Lunsky Y, Straiko A, & Armstrong S (2003). Women be healthy: Evaluation of a women’s health curriculum for women with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 16(4), 247–253. 10.1046/j.1468-3148.2003.00160.x [DOI] [Google Scholar]
- Kim D, & Saada A (2013). The social determinants of infant mortality and birth outcomes in Western developed nations: a cross-country systematic review. International Journal of Environmental Research and Public Health, 10(6), 2296–2335. 10.3390/ijerph10062296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krahn G, & Campbell VA (2011). Evolving views of disability and public health: the roles of advocacy and public health. Disability and Health Journal, 4(1), 12–18. 10.1016/j.dhjo.2010.05.005 [DOI] [PubMed] [Google Scholar]
- Laditka SB, Laditka JN, Mastanduno MP, Lauria MR, & Foster TC (2005). Potentially avoidable maternity complications: an indicator of access to prenatal and primary care during pregnancy. Women & Health, 41(3), 1–26. 10.1300/J013v41n03_01 [DOI] [PubMed] [Google Scholar]
- Llewellyn G, & McConnell D (2002). Mothers with learning difficulties and their support networks. Journal of Intellectual Disability Research, 46(1), 17–34. 10.1046/j.1365-2788.2002.00347.x [DOI] [PubMed] [Google Scholar]
- Long-Bellil L, Valentine A, Mitra M (2020). Achieving Equity: Including Women with Disabilities in Maternal and Child Health Policies and Programs. In Lollar DJ, Horner-Johnson W, W., & Froehlich-Grobe K (Eds.), Public Health Perspectives on Disability: Science, Social Justice, Ethics, and Beyond (2nd ed., pp. 207–224). New York, NY: Springer. 10.1007/978-1-0716-0888-3 [DOI] [Google Scholar]
- Lunsky Y, Balogh RS, Cobigo V, Isaacs B, Lin E, & Ouellette-Kuntz HMJ (2014). Primary Care of Adults with Developmental Disabilities in Ontario. Healthcare Quarterly, 17(3), 11–13. 10.12927/hcq.2014.24026 [DOI] [PubMed] [Google Scholar]
- Luo ZC, Wilkins R, & Kramer MS (2006). Effect of neighbourhood income and maternal education on birth outcomes: a population-based study. CMAJ, 174(10), 1415–1420. 10.1503/cmaj.051096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, & Glanz K (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4), 351–377. 10.1177/109019818801500401 [DOI] [PubMed] [Google Scholar]
- Mitra M, Long-Bellil LM, Smeltzer SC, & Iezzoni LI (2015). A perinatal health framework for women with physical disabilities. Disability and Health Journal, 8(4), 499–506. 10.1016/j.dhjo.2015.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitra M, Parish SL, Clements KM, Cui X, & Diop H (2015). Pregnancy outcomes among women with intellectual and developmental disabilities. American Journal of Preventive Medicine, 48(3), 300–308. 10.1016/j.amepre.2014.09.032 [DOI] [PubMed] [Google Scholar]
- Onono M, Kwena Z, Turan J, Bukusi EA, Cohen CR, & Gray GE (2015). “You know you are sick, why do you carry a pregnancy again?” Applying the socio-ecological model to understand barriers to PMTCT service utilization in Western Kenya. Journal of AIDS & Clinical Research, 6(6), 467. 10.4172/2155-6113.1000467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parish SL, Rose RA, & Andrews ME (2009). Income poverty and material hardship among US women with disabilities. Social Service Review, 83(1), 33–52. 10.1086/598755 [DOI] [Google Scholar]
- Patton MQ (1999). Enhancing the quality and credibility of qualitative analysis. Health Services Research, 34(5, Part II), 1189–1208. [PMC free article] [PubMed] [Google Scholar]
- Potvin LA, Brown HK, & Cobigo V (2016). Social support received by women with intellectual and developmental disabilities during pregnancy and childbirth: An exploratory qualitative study. Midwifery, 37, 57–64. 10.1016/j.midw.2016.04.005 [DOI] [PubMed] [Google Scholar]
- Rogers C, Lepherd L, Ganguly R, & Jacob-Rogers S (2017). Perinatal issues for women with high functioning autism spectrum disorder. Women and Birth, 30(2), e89–e95. 10.1016/j.wombi.2016.09.009 [DOI] [PubMed] [Google Scholar]
- Ronsmans C, Graham WJ, & Lancet Maternal Survival Series steering group. (2006). Maternal mortality: who, when, where, and why. The Lancet, 368(9542), 1189–1200. 10.1016/S0140-6736(06)69380-X [DOI] [PubMed] [Google Scholar]
- Rubenstein E, Ehrenthal DB, Mallinson DC, Bishop L, Kuo HH, et al. (2020). Pregnancy complications and maternal birth outcomes in women with intellectual and developmental disabilities in Wisconsin Medicaid. PLOS ONE, 15(10), e0241298. 10.1371/journal.pone.0241298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakespeare T, & Kleine I (2013). Educating health professionals about disability: a review of interventions. Health and Social Care Education, 2(2), 20–37. 10.11120/hsce.2013.00026 [DOI] [Google Scholar]
- Sundelin HE, Stephansson O, Hultman CM, & Ludvigsson JF (2018). Pregnancy outcomes in women with autism: a nationwide population-based cohort study. Clinical Epidemiology, 10, 1817–1826. 10.2147/CLEP.S176910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suri H (2011). Purposeful sampling in qualitative research synthesis. Qualitative Research Journal, 11(2), 63–75. 10.3316/QRJ1102063 [DOI] [Google Scholar]
- Sullivan WF, Diepstra H, Heng J, Ally S, Bradley E, Casson I, Hennen B, Kelly M, Korossy M, McNeil K, Abells D, Amaria K, Boyd K, Gemmill M, Grier E, Kennie-Kaulbach N, Ketchell M, Ladouceur J, Lepp A, Lunsky Y, McMillan S, Niel U, Sacks S, Shea S, Stringer K, Sue K, & Witherbee S (2018). Primary care of adults with intellectual and developmental disabilities: 2018 Canadian consensus guidelines. Canadian Family Physician, 64(4), 254–279. [PMC free article] [PubMed] [Google Scholar]
- Sword W (1999). A socio- ecological approach to understanding barriers to prenatal care for women of low income. Journal of Advanced Nursing, 29(5), 1170–1177. 10.1046/j.1365-2648.1999.00986.x [DOI] [PubMed] [Google Scholar]
- Takehara K, Noguchi M, Shimane T & Misago C (2014). A longitudinal study of women’s memories of their childbirth experiences at five years postpartum. BMC Pregnancy Childbirth, 14, 221. 10.1186/1471-2393-14-221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarasoff LA, Ravindran S, Malik H, Salaeva D, & Brown HK (2020a). Maternal disability and risk for pregnancy, delivery, and postpartum complications: A systematic review and meta-analysis. American Journal of Obstetrics and Gynecology, 222(1), 27.e1–27.e32. 10.1016/j.ajog.2019.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarasoff LA, Lunsky Y, Chen S, Guttmann A, Havercamp S, Parish S, Vigod S, Carty A, & Brown HK (2020b). Preconception Health Characteristics of Women with Disabilities in Ontario: A Population-Based, Cross-Sectional Study. Journal of Women’s Health, 29(12), 1564–1575. 10.1089/jwh.2019.8273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarleton B & Turner B (2015). Mellow Futures Parent Pioneers Pilot programme evaluation. University of Bristol, UK. Retrieved from https://www.mellowparenting.org/wp-content/uploads/2017/02/Parent-Pioneers-Final-Evaluation-Report-sept16.pdf [Google Scholar]
- Tint A, Brown HK, Chen S, Lai MC, Tarasoff LA, Vigod SN, Parish S, Havercamp SM, & Lunsky Y (2021). Health characteristics of reproductive-aged autistic women in Ontario: A population-based, cross-sectional study. Autism. 10.1177/1362361320982819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations. (2006). Convention on the Rights of Persons with Disabilities (CRPD). Retrieved from https://www.un.org/development/desa/disabilities/convention-on-the-rights-of-persons-with-disabilities.html [DOI] [PubMed]
- Walsh-Gallagher D, Sinclair M, & Mc Conkey R (2012). The ambiguity of disabled women’s experiences of pregnancy, childbirth and motherhood: a phenomenological understanding. Midwifery, 28(2), 156–162. 10.1016/j.midw.2011.01.003 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2020). The ecological framework. Violence Prevention Alliance. Retrieved from https://www.who.int/violenceprevention/approach/ecology/en/ [Google Scholar]
- Xie E, & Gemmill M (2018). Exploring the prenatal experience of women with intellectual and developmental disabilities: In a southeastern Ontario family health team. Canadian Family Physician, 64(Suppl 2), S70–S75. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


