Abstract
Objective:
To compare the presence of migraine features between patients with isolated aural fullness (AF) who meet the diagnostic criteria for migraine headache and those who do not, and to propose diagnostic criteria for migraine-related AF based on our results.
Methods:
We performed a retrospective study of patients presenting to a tertiary-care neurotology clinic between 2014-2020 with migraine-related AF. This was defined as isolated, prolonged aural fullness concurrent with migraine features once other etiologies were ruled out via exam, audiometry, and imaging. Migraine features were compared between patients meeting the diagnostic criteria for migraine headache and those not meeting the criteria.
Results:
Seventy-seven patients with migraine-related AF were included. The mean age was 56±15 years and 55 (71%) patients were female. Eleven (14%) patients fulfilled the criteria for migraine headache (migraine group). Of the 66 patients who did not meet the criteria (non-migraine group), 17 (26%) met 4/5 criteria, and 32 (48%) met 3/5 criteria, for a total of 49 (74%) patients. The migraine and non-migraine groups were only different in 5 out of 20 features, including family history of migraine (P=0.007), sound sensitivity (P<0.001), mental fogginess (P=0.008), visual motion sensitivity (P=0.008), and light sensitivity (P<0.001).
Conclusion:
There are minimal differences in the overall prevalence of migraine features between patients with migraine-related AF who meet and do not meet the diagnostic criteria for migraine. Our findings suggest that the criteria may be too stringent and exclude many patients from potentially benefitting from treatment with migraine prophylaxis.
Keywords: Aural fullness, Ear pressure, Otologic migraine, Migraine headache
INTRODUCTION
Aural fullness (AF) is a broadly defined otologic complaint, often described as ear fullness or a clogging sensation that can cause considerable discomfort (1). The most frequently identifiable causes of AF include Eustachian tube dysfunction (ETD) and otitis media. However, it has also been reported as a common symptom in patients with temporomandibular joint (TMJ) disorder, sudden sensorineural hearing loss, Meniere’s disease, and third window syndrome (e.g., canal dehiscence, perilymphatic fistula) (2-6). In the context of migraine, AF has been previously studied in its association with vestibular migraine (VM), with reports showing a prevalence ranging from 19-51% in VM patients as well as improvement in AF symptoms with VM treatment (7-12). In our experience, a subset of patients with migraine features have reported AF, but do not suffer from concurrent vertiginous episodes necessary to fulfill a diagnosis of VM. Given the otherwise normal exam of these patients, the presence of AF appears to suggest an alternative etiology.
The clinical entity of isolated, prolonged AF has been only recently described as a potential symptom of migraine disorder. In a study by Moshtaghi et al. (13), 11 patients with isolated, prolonged AF were found to have a high prevalence of migraine features and experienced symptom and quality of life improvement following treatment with migraine diet and lifestyle modifications and migraine medications. These findings therefore signal a possible link between migraine headache and isolated AF. Many patients who present to our clinic are believed to suffer from migraine-related AF based on the same study criteria used by Moshtaghi et al. and response to migraine therapy. Additionally, a minority of these patients concurrently suffer from migraine headache as defined by the International Classification of Headache Disorders 3rd edition (ICHD-3) criteria (14). However, the majority who do not fulfill the diagnostic criteria nonetheless frequently present with migraine features and report improvement following treatment with migraine therapy. The objective of our study was (1) to compare the prevalence of migraine features in a larger cohort of patients with migraine-related AF who either meet or do not meet the ICHD-3 guidelines for migraine headache and (2) to propose a set of criteria for the diagnosis of migraine-related AF based on our findings.
METHODS
Following Institutional Review Board approval, we performed a retrospective chart review of all adult (age ≥18 years) patients with complete data who were determined to have migraine-related AF at our tertiary care neurotology clinic from 2014-2020. At the initial visit, each patient was instructed to complete a custom-designed, 28-item questionnaire used to identify their migraine-related symptoms and evaluate the presence of migraine. Survey responses were retrospectively analyzed to determine which patients met the ICHD-3 migraine criteria (Table 1). Migraine-related AF (isolated, prolonged AF with concurrent migraine features) was diagnosed according to the inclusion criteria set by Moshtaghi et al. in their original study: (1) persistent AF ≥ 6 months; (2) normal physical examination, no conductive or low-frequency sensorineural hearing loss, and normal tympanogram; (3) lack of improvement with manual nasal Valsalva or myringotomy; and (4) negative findings on either computed tomography (CT) scan or magnetic resonance imaging (MRI) to rule out canal dehiscence or tumor. If the MRI did not rule out canal dehiscence due to a close semicircular canal to the dura, a CT scan of temporal bones with 0.6 mm cuts was obtained to rule out a third window syndrome. Additionally, patients who fulfilled the criteria for Meniere’s Disease (according to the American Academy of Otolaryngology—Head and Neck Surgery) or VM (according to the International Headache Society), or those who reported autophony, were grouped separately (13-15). Patients who were initially believed to suffer from ETD were included if they failed a trial of daily auto-insufflation, antihistamines, reflux medications, or intranasal corticosteroids, and no improvement with myringotomy. The entire cohort was then divided into patients who fulfilled the ICHD-3 criteria for migraine headache (migraine group) and patients not meeting the full ICHD-3 criteria (non-migraine group). Statistical analysis was performed using SPSS 26.0 (SPSS Inc., IBM Company, Chicago, Illinois). A P value <0.01 was considered to be statistically significant, due to multiple comparisons. Chi-square or Fisher’s exact test were used to compare categorical variables between the cohorts.
Table 1.
Diagnostic criteria for migraine headache without aura as defined by the International Classification of Headache Disorders, 3rd edition (ICHD-3) (14).
Migraine headache without aura
|
RESULTS
A total of 77 patients were included. The mean age of all patients was 56.2 years (range, 20-83 years). Fifty-five (71%) patients were female and 22 (29%) were male. The mean onset of AF symptoms prior to the initial clinic visit was 25.2±30.5 months (range, 0-144 months). Nineteen (25%) patients had a history of headache. Seven (9%) patients had a family history of migraine. Eleven (14%) patients fulfilled the ICHD-3 criteria for migraine headache (migraine group). Of the 66 patients who did not meet the full criteria (non-migraine group), 17 (26%) met 4 out of 5 migraine criteria, and 32 (48%) met 3 out of 5 criteria, for a total of 49 (74%) patients (Figure 1). In patients who met 4/5 criteria, 8 patients had experienced 4 headache attacks (of the required 5 attacks necessary to diagnose migraine) at the time of the survey. The migraine and non-migraine groups were only different in 5 out of 20 total migraine features examined, including family history of migraine (P=0.007), sound sensitivity (P<0.001), mental fogginess (P=0.008), visual motion sensitivity (P=0.008), and light sensitivity (P<0.001). Table 2 summarizes the prevalence of individual migraine features in patients who met the ICHD-3 migraine headache criteria and those who did not meet the full criteria.
Figure 1.
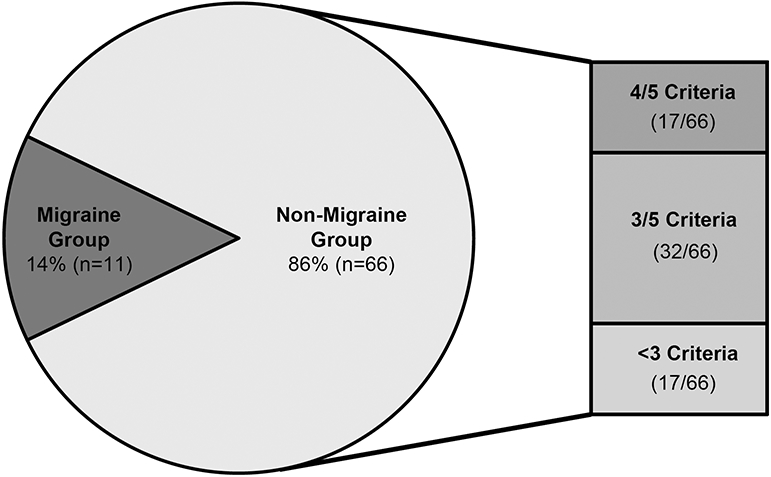
Percentage of patients with aural fullness who met ICHD-3 criteria for migraine headache (migraine group).
Table 2.
Migraine features in patients meeting ICHD-3 criteria for migraine (migraine group) vs. patients not meeting ICHD-3 criteria for migraine (non-migraine group)
| Migraine Feature | Non-Migraine (n=66) No. (%) |
Migraine (n=11) No. (%) |
P-value |
|---|---|---|---|
| History of migraine headaches | 13 (19.7) | 6 (54.5) | 0.22 |
| Family history of migraine headaches | 3 (4.5) | 4 (36.4) | 0.007* |
| Unilateral head pain | 4 (6.1) | 2 (18.2) | 0.202 |
| Allodynia | 3 (4.5) | 0 (0.0) | 1.000 |
| Visual symptoms | 2 (3.0) | 2 (18.2) | 0.095 |
| Difficulty speaking | 0 (0.0) | 1 (9.1) | 0.143 |
| Nausea | 1 (1.5) | 2 (18.2) | 0.052 |
| Sound sensitivity | 2 (3.0) | 5 (45.5) | <0.001* |
| Symptoms exacerbated by | |||
| Menstruation | 0 (0.0) | 1 (9.1) | 0.143 |
| Certain foods | 1 (1.5) | 0 (0.0) | 1.000 |
| Physical activity | 4 (6.1) | 1 (9.1) | 0.548 |
| Mental fog | 1 (1.5) | 3 (27.3) | 0.008* |
| Visual motion sensitivity | 1 (1.5) | 3 (27.3) | 0.008* |
| Head motion sensitivity | 1 (1.5) | 2 (18.2) | 0.052 |
| Sinus pain, facial pressure, or headache when exposed to wind or air conditioning | 2 (3.0) | 0 (0.0) | 1.000 |
| Light sensitivity | 0 (0.0) | 5 (45.5) | <0.001* |
| Motion sickness | 8 (12.1) | 4 (36.4) | 0.063 |
| Neck stiffness | 4 (6.1) | 1 (9.1) | 0.548 |
| History of chronic sinus headaches | 1 (1.5) | 0 (0.0) | 1.000 |
denotes statistically significant values (alpha = 0.01)
DISCUSSION
Our study is the first to compare the prevalence of migraine features between patients with migraine-related AF who meet the ICHD-3 criteria for migraine and those who do not meet the diagnostic criteria. In our cohort, 14% of patients met the migraine criteria, but of the 20 migraine features examined, only 5 features were significantly more prevalent in the migraine cohort. It is also important to note that of the 17 patients who met 4/5 migraine criteria, nearly half (8/17) were only missing one additional migraine episode necessary to make a migraine diagnosis. Although these patients may not have fulfilled the migraine criteria at the time of their initial survey, this does not preclude the presence of migraine as these patients may eventually experience a subsequent attack and thus meet criteria at a later time point. Combined with the results from the original study by Moshtaghi et al., our findings suggest that the current migraine criteria might be too stringent, and unfortunately exclude many patients with migraine-related AF from receiving and possibly benefitting from migraine treatment. We believe that expansion of ICHD-3 criteria to include aural fullness would result in a larger pool of patients receiving treatment. Based on our results, we propose the following diagnostic criteria for migraine-related AF: (A) aural fullness with a normal otologic exam, tympanometry, and audiometry, not meeting the criteria for other disease processes with negative imaging (major features); and (B) at least one of the following (1-3): (1) personal or family history of migraine headaches (2) chronic headaches or unilateral neck stiffness, (3) sound sensitivity, visual or head motion sensitivity, or light sensitivity (minor features) (Table 3).
Table 3.
Proposed diagnostic criteria for migraine-related aural fullness.
|
Migraine-related aural fullness
Major Features
Minor Features
|
The pathophysiology of migraine is complex and remains poorly understood. However, several studies investigating the potential underlying mechanisms may serve to explain the presence of otologic symptoms linked to migraine. One prevailing hypothesis of migraine pathophysiology is cortical spreading depression, in which a wave of depolarization causes release of neuropeptides from the trigeminal nerve leading to migraine aura and pain, as well as auditory and balance symptoms (16-18). Trigeminal nerve fibers have been shown to innervate the spiral modiolar artery and stria vascularis, important structures within the cochlear vascular network (19). It has been theorized that trigeminal innervation therefore serves as the link between migraine and concurrent cochleovestibular symptoms including tinnitus, vertigo, and hearing loss (19). Experiments conducted in animal models have demonstrated the presence of plasma extravasation in the cochlea due to alterations in vascular permeability following trigeminal nerve stimulation (20). This phenomenon is believed to contribute to the otologic manifestations of migraine, and we theorize that these central processes may also contribute to migraine-related AF.
It has been previously hypothesized that AF may originate specifically from a somatotopic relationship between the tympanic membrane and trigeminal nerve (21). This link is evidenced by studies demonstrating sensory innervation of the tympanic membrane by the trigeminal nerve fibers and also through rodent anatomic studies showing divisions of the trigeminal ganglion projecting into the cochlear nucleus and superior olivary complex (22,23). Another major theory regarding the presence of aural fullness with headache and migraine symptoms involves the tonic tensor tympani syndrome (TTTS), which was first described by Klockhoff in the early 1970s (24). In TTTS, there is a decrease in the contraction threshold of the tensor tympani muscle, which results in symptoms of chronic ear pain, headache, and aural fullness in the affected ear. These patients have been described to have tinnitus and hyperacusis as well. The trigeminal nerve is thought to play a significant role in this syndrome, as contractions of the tensor tympani muscle are elicited to a greater degree by trigeminal nerve stimuli compared to acoustic stimuli (25). While the exact mechanisms of isolated aural fullness remain to be elucidated, we believe that the trigeminal nerve serves as a critical link between this symptom and migraine.
The results of the present study add further support to the hypothesis that prolonged aural fullness represents a symptom of “otologic migraine”, a term recently introduced to the literature to characterize a spectrum of disorders in which migraine manifests primarily with cochleovestibular complaints (26-31). We believe that proper identification and treatment of these otologic symptoms with migraine therapies may avoid unnecessary surgical interventions and excess diagnostic work-up. For example, we have seen a number of patients with migraine-related aural pressure/fullness undergo Eustachian tube balloon dilation procedures, which did not improve their symptoms. Many of these patients were later successfully treated at our institution as “probable migraine without aura” after meeting our proposed criteria for migraine-related AF and were offered migraine lifestyle/diet optimization, and if necessary, migraine prophylactic medication.
This study has certain limitations as a retrospective review, including the accuracy and availability of patient information, and selection bias with respect to patients determined to have migraine-related AF by the neurotologists at our institution. Additionally, the survey-based nature of our data introduces the possibility of recall bias, which may influence statistical outcomes and warrant cautious interpretation of the study results. As there is currently no objective diagnostic test for migraine-related AF, the number of false positives cannot be accurately determined, and it is possible that other etiologies of aural fullness may have been missed. Future prospective studies should examine larger cohorts of patients presenting with migraine-related AF to further define the clinical features that may guide treatment and response to migraine therapy.
CONCLUSION
This study reveals minimal meaningful differences in migraine features between patients in our cohort with migraine-related AF who meet the ICHD-3 migraine headache criteria and those who do not. Our findings further support the association between isolated, prolonged aural fullness and migraine, and suggest that the current diagnostic criteria for migraine may unnecessarily exclude many patients from receiving beneficial migraine treatment.
Financial Disclosure:
Mehdi Abouzari is supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant TL1TR001415.
Footnotes
Conflicts of Interest: Hamid R. Djalilian holds equity in MindSet Technologies and Cactus Medical LLC, and is a consultant to NXT Biomedical.
Portion of this work has been presented as a poster at the COSM-ANS 2021 Virtual Annual Spring Meeting on April 7, 2021.
REFERENCES
- 1.Park MS, Lee HY, Kang HM, et al. Clinical manifestations of aural fullness. Yonsei Med J 2012;53:985–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levo H, Kentala E, Rasku J, et al. Aural fullness in Ménière's disease. Audiol Neurootol 2014;19:395–9. [DOI] [PubMed] [Google Scholar]
- 3.Riga M, Xenellis J, Peraki E, et al. Aural symptoms in patients with temporomandibular joint disorders: multiple frequency tympanometry provides objective evidence of changes in middle ear impedance. Otol Neurotol 2010;31:1359–64. [DOI] [PubMed] [Google Scholar]
- 4.Sakata T, Kato T. Feeling of ear fullness in acute sensorineural hearing loss. Acta Otolaryngol 2006;126:828–33. [DOI] [PubMed] [Google Scholar]
- 5.Sarna B, Abouzari M, Merna C, et al. Perilymphatic Fistula: A Review of Classification, Etiology, Diagnosis, and Treatment. Front Neurol 2020;11:1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bi WL, Brewster R, Poe D, et al. Superior semicircular canal dehiscence syndrome. J Neurosurg 2017;127:1268–76. [DOI] [PubMed] [Google Scholar]
- 7.Lopez-Escamez JA, Dlugaiczyk J, Jacobs J, et al. Accompanying Symptoms Overlap during Attacks in Menière's Disease and Vestibular Migraine. Front Neurol 2014;5:265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neff BA, Staab JP, Eggers SD, et al. Auditory and vestibular symptoms and chronic subjective dizziness in patients with Ménière's disease, vestibular migraine, and Ménière's disease with concomitant vestibular migraine. Otol Neurotol 2012;33:1235–44. [DOI] [PubMed] [Google Scholar]
- 9.Sabra O, Muhammad Ali M, Al Zayer M, et al. Frequency of migraine as a chief complaint in otolaryngology outpatient practice. Biomed Res Int 2015;2015:173165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martinez E, Ruiz-Pinero M, de Lera M, et al. [Clinical characteristics of vestibular migraine: considerations in a series of 41 patients]. Rev Neurol 2017;64:1–6. [PubMed] [Google Scholar]
- 11.Chen J, Gong D, Cai S, et al. [Clinical characteristics of 100 vestibular migraine cases]. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2016;30:399–401. [PubMed] [Google Scholar]
- 12.Battista RA. Audiometric findings of patients with migraine-associated dizziness. Otol Neurotol 2004;25:987–92. [DOI] [PubMed] [Google Scholar]
- 13.Moshtaghi O, Ghavami Y, Mahboubi H, et al. Migraine-Related Aural Fullness: A Potential Clinical Entity. Otolaryngol Head Neck Surg 2018;158:100–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia; 2018;38. [DOI] [PubMed] [Google Scholar]
- 15.Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Menière's disease. American Academy of Otolaryngology-Head and Neck Foundation, Inc. Otolaryngol Head Neck Surg 1995;113:181–5. [DOI] [PubMed] [Google Scholar]
- 16.Charles AC, Baca SM. Cortical spreading depression and migraine. Nat Rev Neurol 2013;9:637–44. [DOI] [PubMed] [Google Scholar]
- 17.Abouzari M, Goshtasbi K, Sarna B, et al. Proposal for a new diagnosis for U.S. diplomats in Havana, Cuba, experiencing vestibular and neurological symptoms. Med Hypotheses 2020;136:109499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Malhotra R. Understanding migraine: Potential role of neurogenic inflammation. Ann Indian Acad Neurol 2016;19:175–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vass Z, Shore SE, Nuttall AL, et al. Direct evidence of trigeminal innervation of the cochlear blood vessels. Neuroscience 1998;84:559–67. [DOI] [PubMed] [Google Scholar]
- 20.Vass Z, Steyger PS, Hordichok AJ, et al. Capsaicin stimulation of the cochlea and electric stimulation of the trigeminal ganglion mediate vascular permeability in cochlear and vertebro-basilar arteries: a potential cause of inner ear dysfunction in headache. Neuroscience 2001;103:189–201. [DOI] [PubMed] [Google Scholar]
- 21.Sakata T, Higuchi H, Ueno T, et al. Modulation of somatosensory abilities and the feeling of ear fullness in patients with acute sensorineural hearing loss. Auris Nasus Larynx 2012;39:265–9. [DOI] [PubMed] [Google Scholar]
- 22.Saunders RL, Weider D. Tympanic membrane sensation. Brain 1985;108 ( Pt 2):387–404. [DOI] [PubMed] [Google Scholar]
- 23.Shore SE, Vass Z, Wys NL, et al. Trigeminal ganglion innervates the auditory brainstem. J Comp Neurol 2000;419:271–85. [DOI] [PubMed] [Google Scholar]
- 24.Klockhoff I, Lindholm L, Westerberg CE. [Spontaneous impedance fluctuation--a "tensor tympani syndrome" with special reference to tension headache]. Nord Med 1971;85:577. [PubMed] [Google Scholar]
- 25.Rauchfuss A, Hiller E, Leitner H, et al. [Reaction of the tympanic tensor muscle--elicited by nasally applied trigeminal stimulants]. Laryngol Rhinol Otol (Stuttg) 1987;66:131–2. [PubMed] [Google Scholar]
- 26.Bruss D, Abouzari M, Sarna B, et al. Migraine Features in Patients With Recurrent Benign Paroxysmal Positional Vertigo. Otol Neurotol 2021;42:461–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Teixido M, Seymour P, Kung B, et al. Otalgia associated with migraine. Otol Neurotol 2011;32:322–5. [DOI] [PubMed] [Google Scholar]
- 28.Paparella MM, Djalilian HR. Etiology, pathophysiology of symptoms, and pathogenesis of Meniere's disease. Otolaryngol Clin North Am 2002;35:529–45, vi. [DOI] [PubMed] [Google Scholar]
- 29.Abouzari M, Cheung D, Pham T, et al. The Relationship Between Vestibular Migraine and Motion Sickness Susceptibility. Otol Neurotol 2020;41:1116–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sarna B, Risbud A, Lee A, et al. Migraine Features in Patients with Persistent Postural-Perceptual Dizziness. Ann Otol Rhinol Laryngol 2021;34894211007233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goshtasbi K, Chua JT, Risbud A, et al. Treatment of Long-term Sudden Sensorineural Hearing Loss as an Otologic Migraine Phenomenon. Otol Neurotol 2021;42:1001–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


