Abstract
Background:
Hallucinogen use is rising in the US, yet little is known regarding the prevalence and psychosocial/behavioral correlates of driving under the influence of these drugs.
Methods:
This study examined data from 4,447 individuals ages 16-64 who reported past-year hallucinogen use in the 2016-2018 National Survey on Drug Use and Health. Prevalence estimates (with 95% confidence intervals [CIs]) were calculated for driving under the influence of hallucinogens (DUIH). Logistic regression examined psychosocial/behavioral correlates of DUIH, and latent class analysis (LCA) characterized subgroups of individuals reporting DUIH.
Results:
The prevalence of past-year hallucinogen use was 2.42% (CI = 2.30-2.54) and, in the general population, the prevalence of DUIH was 0.21%. Among past-year hallucinogen users, 8.94% (CI = 7.74-10.31) reported DUIH on at least one occasion over the previous 12 months. The probability of DUIH increased significantly with more frequent use. Compared to individuals who used hallucinogens and did not report DUIH, individuals reporting DUIH were significantly more likely to report mental health problems; use of other illicit drugs; selling drugs; a past-year arrest; or driving under the influence of alcohol, cannabis, or other illicit drugs. LCA identified three classes of individuals reporting DUIH, characterized by: use of and driving under the influence of cannabis; use of and driving under the influence of cannabis and other illicit drugs; and mental health concerns.
Conclusions:
Nearly one in ten individuals who report using hallucinogens also report driving under the influence of hallucinogens—drugs that affect perception and risk-taking, with alarming implications for driving safety.
Keywords: hallucinogens, driving under the influence, risk behavior, drugs
Hallucinogen use represents a growing public health problem in the United States (US). Recent epidemiological studies indicate that the lifetime prevalence of hallucinogen use among American adults is nearly 10 percent (Shalit et al., 2019) and that the annual prevalence of use has increased by more than 200 percent since the early 2000s (Killion et al., 2021; Johnson et al., 2019). We also know that several subgroups—such as young males, polysubstance users, individuals with psychiatric conditions, and those involved in illegal/antisocial behavior—tend to report higher rates of hallucinogen use (Degenhardt et al., 2006; Penning et al., 2010). Furthermore, there is currently increasing interest in the therapeutic use of hallucinogens, which may lead some to conclude that hallucinogen use is safe regardless of appropriate guidance or monitoring (Bogenschutz & Johnson, 2016).
The effects of hallucinogens vary by the individual user and the type and amount consumed, but generally their use results in an array of perceptual, cognitive, and psychomotor distortions (Frances et al., 2011). The perceptual and psychomotor distortions associated with hallucinogen use have alarming implications for driving safety, including impairment in attention, focus, memory, response time, motor abilities, and interpretation of visual and auditory stimuli (Giorgetti et al., 2015; Penning et al., 2010; Strand et al., 2016). Driving under the influence of hallucinogens is also associated with risk-taking and impulsive behaviors such as speeding or disregarding traffic signals (Penning et al., 2010). Indeed, in driving simulation studies, increased collisions have been observed in experimental groups under the influence of hallucinogens (Brookhuis et al., 2004).
Research on driving under the influence of substances in general shows that this behavior is often associated with psychosocial and behavioral problems (Donovan, 1993). For instance, recent research has shown that individuals driving under the influence of alcohol are more likely to report criminal justice contact (Oh et al., 2020) and that driving under the influence of cannabis is associated with psychiatric distress, comorbid drug use, and illegal behaviors such as theft and drug selling (Salas-Wright et al., 2021). Such findings are in line with an overall pattern in which drug use is connected with a panoply of behaviors influenced by high levels of sensation seeking and poor impulse control (Salas-Wright et al., 2016; Vaughn et al., 2021). While our understanding of driving under the influence of psychoactive drugs has advanced in recent years, research regarding the prevalence and psychosocial/behavioral correlates of driving under the influence of hallucinogens (DUIH) remains limited (Matthews et al., 2014) and DUIH often goes unmentioned by public health authorities (National Institute on Drug Abuse, 2019).
Cognizant of this gap, the aim of the present study is to systematically examine the prevalence and correlates of DUIH using up-to-date data from a national survey. Specifically, we examine the: annual prevalence of DUIH by gender and racial/ethnic group; links between hallucinogen use frequency and DUIH; mental health, substance misuse, and criminal justice correlates and latent subgroups, and; the likelihood of DUIH by specific hallucinogen use type (e.g., LSD, ketamine). An examination of these topics promises to address an increasingly important gap in drug use and risk behavior surveillance in the US.
Method
Data and Sample
This study examines public-use data collected between 2016 and 2018 as part of the National Survey on Drug Use and Health (NSDUH). The NSDUH provides population estimates for an array of substance use and health-related behaviors in the US general population using multistage area probability sampling methods. Each independent, cross-sectional NSDUH sample is considered representative of the non-institutionalized population ages 12 and older, including household residents, civilians residing on military bases, and shelter and group home residents.
Since 2002, nearly 1,000,000 respondents have completed the NSDUH survey; however, the present study’s analytic sample was limited to 130,916 participants, ages 16 to 64, interviewed between 2016 and 2018 with a primary emphasis on those reporting past-year hallucinogen use (n = 4447). We limited our analyses to the 2016-2018 surveys as these are the only years that include an assessment of DUIH. We limited our age range to 16-64 for several reasons. Age 16 is an appropriate lower limit, given that this is the most common age range for legal driving. Age 64 was determined to be the maximum age given that no instances of DUIH were observed among adults ages 65 and older. The design and methods are summarized briefly here, but a fuller description of NSDUH procedures is available elsewhere (see Substance Abuse and Mental Health Services Administration, 2020).
Measures
Hallucinogen Use
Hallucinogen use was determined by asking participants if they ever used hallucinogens, which are specified in the NSDUH survey as drugs that “often cause people to see or experience things that are not real.” Subsequently, a number of traditional (LSD/acid, psilocybin/mushrooms, mescaline/peyote, DMT/foxy) and dissociative (ecstasy/molly, PCP/ozone, ketamine, salvia divinorum) hallucinogenic substances are listed and participants can also select “other” hallucinogens besides the ones listed. Individuals who respond affirmatively to lifetime hallucinogen use were then asked about past year use and frequency.
Driving under the Influence of Hallucinogens
DUIH was assessed by asking respondents, “During the past 12 months, have you driven a vehicle while you were under the influence of hallucinogens?” (no, yes). Among hallucinogen users, we also examined past-month days of hallucinogen use (one, two, three to five, six or more).
Psychosocial and Behavioral Correlates
We examined a number of correlates in the domains of mental health, substance misuse, driving under the influence, and crime and justice. All variables were dichotomous (no, yes).
Mental health was measured in terms of past-year [a] major depressive episodes which is based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition or DSM-IV [American Psychiatric Association, 2000]) and [b] serious psychological distress as reflected by a score of 13 or higher on the widely-used K6 scale (Kessler et al., 2003).
Substance misuse was examined via three variables: [a] Heavy drinking was measured as five or more drinks on the same occasion for males or four or more drinks on the same occasion for females on five or more days over the past 30 days (National Institute on Alcohol Abuse and Alcoholism, n.d.). [b] Cannabis use refers to past-year use of marijuana/hashish. [c] Other illicit drug use refers to past-year use of cocaine, heroin, or methamphetamine.
Driving under the influence of substances other than hallucinogens focused on past-year driving under the influence of [a] alcohol, [b] cannabis, and [c] other illicit drugs (i.e., cocaine, heroin, methamphetamine).
Crime and justice involvement was measured in terms of one or more instances of self-reported [a] selling of illegal drugs and [b] being “arrested and booked” for breaking the law excluding minor traffic violations.
Demographic Factors
We examined key demographic factors commonly included as control variables in NSDUH-based studies, including age (16-17, 18-25, 26-34, 35-49, 50-64), sex (female, male), race/ethnicity (non-Hispanic [NH] White, NH Black/African American, NH Asian, Hispanic, other), and annual household income (less than $20,000, $20,000-$39,999, $40,000-$74,999, $75,000 or greater). We note that all of these variables were based on respondent self-report and acknowledge that, as is the case in most long-standing national surveys, the racial/ethnic categories lack the depth of nuance needed for classifying many individuals in the contemporary US (e.g., one cannot identify as both Hispanic and African American).
Statistical Analyses
Statistical analyses were carried out in several steps over three phases or “parts.” All statistical analyses were weighted to abide by the Substance Abuse and Mental Health Data Archive’s (SAMHDA) guidelines, accounting for the NSDUH’s stratified cluster sampling design (SAMHDA, 2014). Unless otherwise specified, all analyses were conducted using Stata 16MP.
In Part 1, we present the survey adjusted prevalence estimates with 95% confidence intervals (CIs)—using Stata 16’s svyset command and svy prefix—for hallucinogen use, and DUIH among the full adult sample and hallucinogen users only. Additionally, we assess the association between hallucinogen use frequency and the probability of DUIH (see Figure 2). The predicted probability was generated using logistic regression (and then the margins command) with DUIH specified as the dependent variable and days of hallucinogen use specified as an independent variable. We also examine the association between demographic factors and DUIH using logistic regression.
Figure 2.
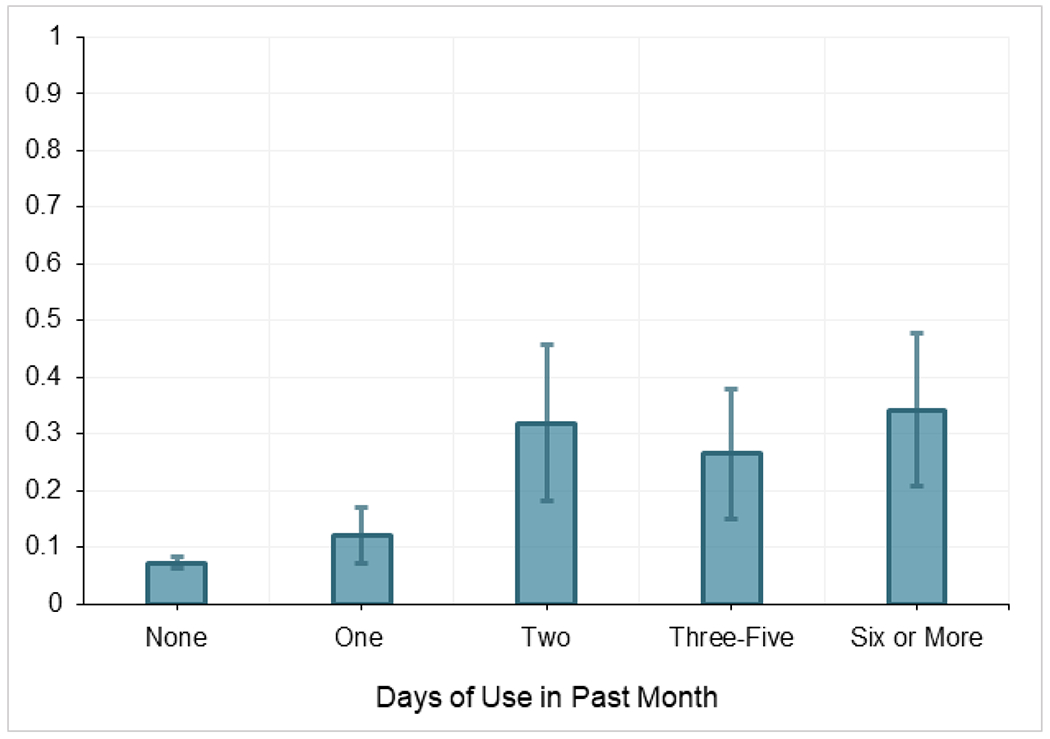
Predicted probabilities (with 95% CIs) of driving under the influence of hallucinogens, 2016-2018, by number of days of hallucinogen use in the past month among individuals reporting past-year hallucinogen use.
In Part 2, we examine the psychosocial and behavioral correlates of DUIH among hallucinogen users by means of logistic regression. DUIH was specified as the dependent variable using a multivariable approach (i.e., examining each psychosocial/behavioral variable independently while controlling for demographic factors) (Hidalgo and Goodman, 2013). We also conducted, among hallucinogen users, a similar analysis examining the prevalence of “classic” and dissociative hallucinogen use among those reporting no and any DUIH. We report adjusted odds ratios (AOR) that can be interpreted as small (1.68), medium (3.47), and large (6.71) per established guidelines regarding effect sizes with categorical data (Chen et al., 2010).
In Part 3, we conduct a latent class analysis (LCA) to identify psychosocial and behavioral subgroups of individuals reporting past year DUIH. LCA is a statistical procedure that assigns individual cases to their most likely latent subgroups on the basis of observed data (McLachlan and Peel, 2004). We began by identifying a sequence of latent profile models ranging from one to five classes by using Latent GOLD® 5.1 software (Vermunt and Magidson, 2016). Five statistical criteria were used to identify the best fitting model: Bayesian Information Criterion (BIC), Akaike’s Information Criterion (AIC), Consistent Akaike’s Information Criterion (CAIC), log likelihood (LL), and entropy. Higher entropy values—approaching .80—indicate clear class delineation (Celeux and Soromenho, 1996). In addition to quantitative criteria, the parsimony and substantive interpretability of the latent class solutions also function as model selection criteria. We present a visual of the latent classes (see Figure 3) in which the conditional item-response probabilities are displayed as dots or points for each class/item—for ease of interpretation, we color code and connect the dots for each class, consistent with other finite mixture modeling studies (Pilatti et al., 2020; Valente, Cogo-Moreira, & Sanchez, 2017). After modeling the latent classes, we examined the demographic characteristics of the latent classes using Stata 16 (StataCorp, 2019).
Figure 3.
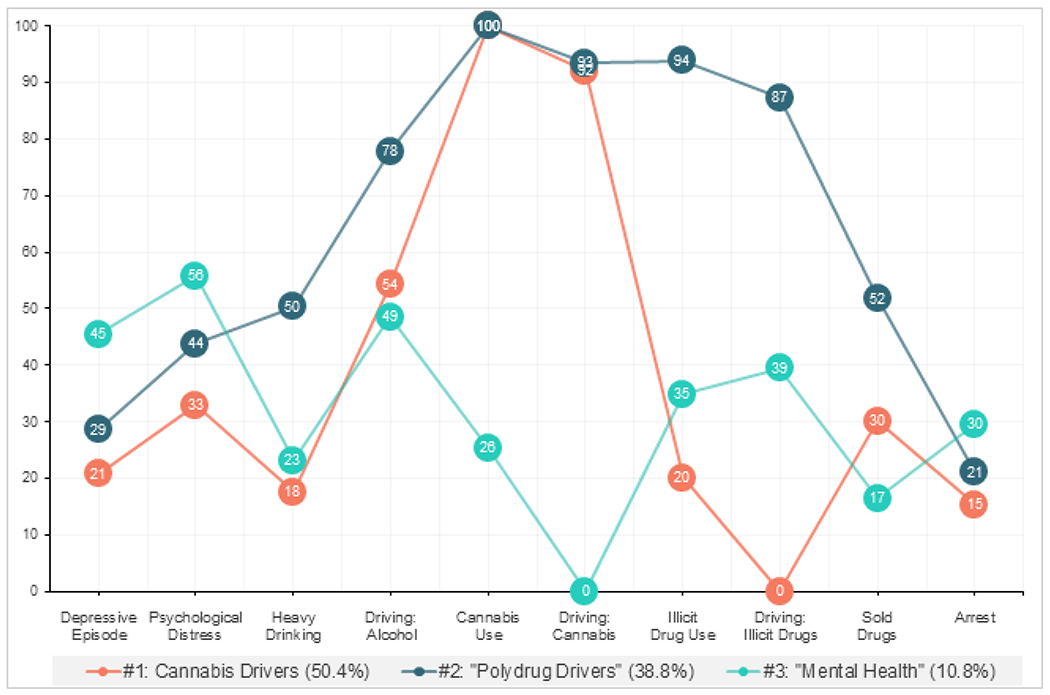
Conditional item-response probabilities for the selected three-class solution based on mental health, substance use, driving under the influence of drugs, and crime and justice involvement indicators, for individuals reporting past-year hallucinogen use, 2016-2018.
Results
Part 1: Prevalence and Probability of Driving under the Influence
Among individuals between the ages of 16 and 64, the prevalence of past year hallucinogen use was 2.42% (CI = 2.30-2.54) and, in the general population, the prevalence of DUIH was 0.21%). Among past-year hallucinogen users, 8.94% (CI = 7.74-10.31) reported DUIH on at least one occasion over the previous 12 months.
Table 1 displays the demographic characteristics of individuals DUIH. No significant variation in the prevalence of DUIH was observed in terms of age or household income. However, male hallucinogen users (10.10 %, CI = 8.3-12.2) were more likely than females (6.94%, CI = 5.5-8.6) to report DUIH (OR = 1.48, CI = 1.06-2.07). Also, NH Black/African American hallucinogen users (16.18%, CI = 12.00-21.47) were more likely to report DUIH compared to NH White (8.34%, CI = 6.89-10.07), Hispanic (8.67, CI = 6.20-11.98), NH Asian (7.18%, CI = 3.24-15.16), and “other race” (7.55%, CI = .90-11.46) users.
Table 1.
Demographic characteristics of individuals of driving under the influence of hallucinogens, 2016–2018
| During the past 12 months, have you driven a vehicle while you were under the influence of hallucinogens? | ||||
|---|---|---|---|---|
|
| ||||
| No (N = 3921) | Yes (N = 408) | |||
|
| ||||
| % (CI) | % (CI) | AOR | 95% CI | |
| Demographic Factors | ||||
|
| ||||
| Age | ||||
| 16-17 | 90.77 (86.9-93.6) | 9.23 (6.4-13.1) | 1.04 | (0.71-1.55) |
| 18-25 | 90.41 (88.5-92.1) | 9.58 (7.9-11.5) | 0.86 | (0.54-1.37) |
| 36-34 | 91.61 (88.9-93.7) | 8.39 (6.3-11.1) | 0.82 | (0.42-1.60) |
| 35-49 | 91.74 (87.4-94.7) | 8.26 (5.3-12.6) | 0.80 | (0.16-3.80) |
| 50-64 | 92.45 (73.9-98.1) | 7.55 (1.8-26.1) | 1.00 | -- |
| Sex | ||||
| Female | 93.06 (91.4-94.4) | 6.94 (5.5-8.6) | 1.00 | -- |
| Male | 89.90 (87.8-91.6) | 10.10 (8.3-12.2) | 1.50 | (1.08-2.09) |
| Race/Ethnicity | ||||
| NH White | 91.66 (89.9-93.1) | 8.34 (6.9-10.1) | 1.00 | -- |
| NH Black/African American | 83.82 (78.5-88.0) | 16.18 (12.0-21.5) | 2.22 | (1.44-3.42) |
| NH Asian | 92.82 (84.8-96.8) | 7.18 (3.2-15.2) | 0.87 | (0.37-2.06) |
| Hispanic | 91.33 (88.0-93.8) | 8.67 (6.2-12.0) | 1.02 | (0.69-1.50) |
| Other | 92.45 (88.5-95.1) | 7.55 (4.9-11.5) | 0.92 | (0.55-1.55) |
| Household Income | ||||
| Less than $20,000 | 91.28 (88.9-93.2) | 8.71 (6.8-11.1) | 1.00 | -- |
| $20,000-$39,999 | 91.33 (88.4-94.6) | 8.67 (6.4-11.6) | 1.06 | (0.70-1.59) |
| $40,000-$74,999 | 89.29 (85.2-92.4) | 10.71 (7.6-14.8) | 1.37 | (0.90-2.10) |
| $75,000 or greater | 91.42 (89.0-93.3) | 8.58 (6.7-11.0) | 1.09 | (0.74-1.60) |
Notes. Data from 2016-2018 are pooled. Adjusted odds ratios (AOR) adjusted for sex, age, race/ethnicity, and, annual household income. AORs and confidence intervals (CI) in bold are statistically significant at p < .05. Estimates are weighted to account for NSDUH’s complex sampling design.
Among hallucinogen users, the probability of DUIH increased significantly with more frequent use (see Figure 2). Nearly half of current/past-month hallucinogen users report only one (45%) day of use in the past month—among these individuals, the predicted probability of DUIH was 11.95%. In contrast, the predicted probability among those reporting two (22%), three to five (19%), or six or more days (14%) of past-month use was significantly greater (31.85%, 26.51%, and 34.23%, respectively). Among individuals reporting past-year use, but no past month use (87% of all hallucinogen users) the predicted probability of DUIH was 7.26% (CI = 6.18-8.34)
Part 2: Correlates of Driving under the Influence
As shown in Table 2, individuals reporting DUIH were significantly more likely to experience mental health problems as compared to hallucinogen users reporting no DUIH, including major depressive episodes (OR = 1.54, CI = 1.08-2.20) and significant psychological distress (OR = 1.48, CI = 1.03-2.12). Those DUIH were not more likely to report heavy drinking or cannabis use, but were more likely to report use of other illicit drugs (OR = 1.50, CI = 1.15-1.96). Notably, compared to non-hallucinogen users, rates of alcohol misuse (no DUIH: 29%, DUIH: 31%), cannabis use (no DUIH: 87%, DUIH: 92%), and illicit drug use (no DUIH: 42%, DUIH: 50%) were markedly elevated. In terms of driving under the influence, those reporting DUIH were also more likely to report driving under the influence of alcohol (OR = 4.44, CI = 3.12-6.32), cannabis (OR = 5.92, CI = 4.01-8.75), or other illicit drugs (OR = 5.65, CI = 4.16-7.67). Those DUIH were also more likely to report having sold drugs (OR = 3.18, CI = 2.31-4.38) and having been arrested and booked in the past year (OR = 2.28, CI = 1.57-3.32).
Table 2.
Correlates of driving under the influence of hallucinogens, 2016–2018
| Hallucinogen Users |
|||||
|---|---|---|---|---|---|
| During the past 12 months, Have you driven a vehicle while you were under the influence of hallucinogens? | |||||
|
|
|||||
| Point of Reference: | Percentage (95% Confidence Interval) | Logistic Regression |
|||
| (w/Demographic Controls) | |||||
|
|
|||||
| Non-Users (n = 153,450) | No (N = 3921) | Yes (N = 408) | AOR | 95% CI | |
| Mental Health | |||||
| Major Depressive Episode | |||||
| No | 92.28 (92.0-92.5) | 79.68 (78.0-81.3) | 73.38 (66.2-79.5) | 1.00 | - |
| Yes | 7.72 (7.5-7.9) | 20.32 (18.7-22.0) | 26.62 (20.5-33.8) | 1.54 | (1.08-2.20) |
| Psychological Distress | |||||
| No | 87.48 (87.2-87.7) | 67.47 (65.1-69.8) | 60.20 (52.1-67.8) | 1.00 | - |
| Yes | 12.53 (12.3-12.8) | 32.53 (30.2-34.9) | 39.80 (32.2-47.9) | 1.48 | (1.03-2.12) |
|
| |||||
| Substance Misuse | |||||
| Heavy Drinking | |||||
| No | 93.13 (92.9-93.4) | 70.93 (68.5-73.3) | 69.07 (62.9-74.6) | 1.00 | - |
| Yes | 6.87 (6.6-7.1) | 29.07 (26.7-31.5) | 30.93 (25.4-37.1) | 1.06 | (0.79-1.43) |
| Cannabis Use | |||||
| No | 83.35 (83.0-83.7) | 12.70 (10.8-14.9) | 8.01 (5.1-12.4) | 1.00 | - |
| Yes | 16.65 (16.3-17.0) | 87.30 (85.1-89.2) | 92.00 (87.6-94.9) | 1.71 | (0.96-3.05) |
| Other Illicit Drug Use | |||||
| No | 98.14 (98.0-98.2) | 58.43 (56.0-60.8) | 49.59 (43.6-55.6) | 1.00 | - |
| Yes | 1.86 (1.7-2.0) | 41.57 (39.2-44.0) | 50.41 (44.4-56.4) | 1.50 | (1.15-1.96) |
|
| |||||
| Driving under the Influence | |||||
| Alcohol | |||||
| No | 91.27 (91.0-91.5) | 70.42 (68.2-72.5) | 37.17 (29.9-45.1) | 1.00 | - |
| Yes | 8.73 (8.5-9.0) | 29.58 (27.5-31.7) | 62.83 (54.9-70.1) | 4.44 | (3.12-6.32) |
| Cannabis | |||||
| No | 95.59 (95.4-95.7) | 55.12 (52.6-57.6) | 17.32 (13.0-22.7) | 1.00 | - |
| Yes | 4.41 (4.3-4.5) | 44.88 (42.4-47.4 | 82.68 (77.3-87.0) | 5.92 | (4.01-8.75) |
| Other Illicit Drugs | |||||
| No | 99.32 (99.2-99.4) | 89.47 (88.2-90.6) | 61.74 (53.5-69.4) | 1.00 | - |
| Yes | 0.68 (0.6-0.7) | 10.53 (9.4-11.8) | 38.26 (30.6-46.5) | 5.65 | (4.16-7.67) |
|
| |||||
| Crime and Justice Involvement | |||||
| Sold Drugs | |||||
| No | 98.71 (98.6-98.8) | 84.25 (82.7-85.7) | 63.07 (55.8-69.8) | 1.00 | - |
| Yes | 1.29 (1.2-1.4) | 15.75 (14.3-17.3) | 36.93 (30.2-44.2) | 3.18 | (2.31-4.38) |
| Arrest | |||||
| No | 97.93 (97.8-98.0) | 91.59 (90.2-92.8) | 80.94 (75.3-85.5) | 1.00 | - |
| Yes | 2.07 (2.0-2.2) | 8.41 (7.2-9.8) | 19.06 (14.5-24.7) | 2.28 | (1.57-3.32) |
Notes. Data from years 2016-2018 are pooled. Demographic controls include sex, age, race/ethnicity, and annual household income. Adjusted odds ratios (AOR) and confidence intervals (95% CI) in bold are statistically significant at p < .05. All prevalence estimates are weighted to account for NSDUH’s complex sampling design.
As a point of reference, the rates of all mental health, substance misuse, driving under the influence, and crime and justice involvement variables among hallucinogen users (those reporting no and any DUIH) differed significantly—with “large effects” higher than that of non-users.
Table 3 displays the rates of use of specific classic and dissociative hallucinogens among those reporting no and any DUIH. Rates were largely comparable among both groups, but significantly higher rates were observed in terms of LSD (OR = 1.38, CI = 1.04-1.84), DMT (OR = 1.75, CI = 1.19-2.57), ecstasy (OR = 1.81, CI = 1.22-2.69), and ketamine (OR = 1.52, CI = 1.07-2.16). No differences were observed for psilocybin, mescaline, PCP, or Salvia Divinorum.
Table 3.
Specific hallucinogen use by driving under the influence of hallucinogens
| During the past 12 months, have you driven a vehicle while you were under the influence of hallucinogens? | ||||
|---|---|---|---|---|
|
| ||||
| No (N = 3921) | Yes (N = 408) | |||
|
| ||||
| % (CI) | % (CI) | AOR | 95% CI | |
| Classic Hallucinogen | ||||
|
| ||||
| LSD / Acid | ||||
| No | 32.92 (30.8-35.1) | 28.43 (22.9-34.6) | 1.00 | -- |
| Yes | 67.08 (64.9-69.2) | 71.57 (65.4-77.0) | 1.38 | (1.04-1.84) |
| Psilocybin / Mushrooms | ||||
| No | 34.56 (32.7-36.4) | 37.28 (30.8-44.2) | 1.00 | -- |
| Yes | 65.4 (63.6-67.3) | 62.72 (55.8-69.2) | 0.98 | (0.72-1.34) |
| Mescaline / Peyote | ||||
| No | 87.01 (85.2-88.6) | 85.19 (78.7-89.9) | 1.00 | -- |
| Yes | 12.99 (11.3-14.8) | 14.81 (10.1-21.3) | 1.32 | (0.81-2.15) |
| DMT / Foxy | ||||
| No | 82.07 (80.5-83.6) | 73.70 (66.2-80.0) | 1.00 | -- |
| Yes | 17.93 (16.4-19.5) | 26.30 (20.0-33.8) | 1.75 | (1.19-2.57) |
|
| ||||
| Dissociative | ||||
|
| ||||
| Ecstasy / Molly | ||||
| No | 28.10 (26.1-30.1) | 19.13 (14.4-24.9) | 1.00 | -- |
| Yes | 71.90 (69.8-73.9) | 80.87 (75.1-85.5) | 1.81 | (1.22-2.69) |
| PCP / Ozone | ||||
| No | 92.55 (91.0-93.9) | 90.41 (83.1-94.7) | 1.00 | -- |
| Yes | 7.45 (6.1-9.0) | 9.59 (5.2-16.9) | 1.44 | (0.79-2.62) |
| Ketamine | ||||
| No | 81.42 (79.7-83.0) | 76.07 (69.8-81.4) | 1.00 | -- |
| Yes | 18.58 (17.0-20.3) | 23.93 (18.6-30.2) | 1.52 | (1.07-2.16) |
| Salvia Divinorum | ||||
| No | 76.20 (74.0-78.2) | 73.41 (69.1-77.3) | 1.00 | -- |
| Yes | 23.80 (21.8-25.9) | 26.59 (22.7-30.9) | 1.24 | (0.97-1.59) |
Notes. Data from 2016-2018 are pooled. Adjusted odds ratios (AOR) adjusted for sex, age, race/ethnicity, and, annual household income. AORs and confidence intervals (CI) in bold are statistically significant at p < .05. Estimates are weighted to account for NSDUH’s complex sampling design.
Part 3: A Typology of Driving under the Influence
Analyzing the modeling of latent class solutions suggests a three-class solution as the statistically optimal and conceptually best-fitting model of the data (Table 4). Table 5 shows demographic characteristics by latent class. As shown in Figure 3, Class One (the “Cannabis Drivers” class) comprised 50% of the sample and was characterized by elevated levels of cannabis use and driving under the influence of cannabis in combination with relatively modest levels of all of the other variables. Notably, this class was characterized as having the highest proportion of respondents ages 25 and younger (69%). Class Two (the “Polydrug Drivers” class) comprised 39% of the sample and was characterized by very high levels of driving under the influence of cannabis and other illicit drugs as well as cannabis and illicit drug use. This class stood out as having the greatest number of male respondents (79%). The final class, Class Three (the “Mental Health” class) was the smallest of all classes comprising only 11% of the sample. This class had the highest rates of all depressive episodes and psychological distress, but was relatively low in terms of substance misuse, driving under the influence, and criminal behavior. In relative terms, members of this class tended to be older and were disproportionately female (47%).
Table 4.
Fit Indices for Latent Classes
| # Class Solution | Log Likelihood | LL | Bayesian Information Criterion | BIC | Akaike’s Information Criterion | AIC | Consistent Akaike’s Information Criterion | CAIC | Entropy R2 |
|---|---|---|---|---|---|
| 1-Class | −2312.84 | 4685.80 | 4645.69 | 4695.80 | n/a |
| 2-Class | −2170.70 | 4509.71 | 4397.40 | 4537.71 | 0.80 |
|
|
|||||
| 3-Class | −2097.21 | 4470.93 | 4286.41 | 4516.93 | 0.84 |
|
|
|||||
| 4-Class | −2041.07 | 4466.86 | 4210.13 | 4530.86 | 0.87 |
| 5-Class | −1999.34 | 4491.60 | 4162.68 | 4573.60 | 0.89 |
| 6-Class | −1952.87 | 4506.87 | 4105.74 | 4606.87 | 0.88 |
Table 5.
Demographic characteristics of latent classes
| All DUIH | #1: Cannabis Drivers (50.5%) | #2: Polydrug Drivers (38.8%) | #3: Mental Health (10.8%) | ||
|---|---|---|---|---|---|
|
| |||||
| % (N) | % (N) | % (N) | % (N) | χ2 | |
| Age | |||||
|
| |||||
| 16-17 | 5.79 (47) | 8.09 (32) | 3.27 (11) | 4.14 (4) | 55.19* |
| 18-25 | 50.18 (253) | 60.50 (142) | 42.29 (97) | 30.31 (14) | |
| 26-34 | 28.25 (76) | 22.27 (29) | 33.55 (36) | 37.20 (11) | |
| 35-49 | 11.92 (29) | 9.15 (12) | 10.96 (11) | 28.35 (6) | |
| 50-64 | 3.85 (3) | 0.00 (0) | 9.92 (3) | 0.00 (0) | |
|
| |||||
| Sex | |||||
|
| |||||
| Female | 28.45 (137) | 30.11 (74) | 21.30 (46) | 46.51 (17) | 11.29* |
| Male | 71.55 (271) | 69.89 (141) | 78.70 (112) | 53.49 (18) | |
|
| |||||
| Race/Ethnicity | |||||
|
| |||||
| NH White | 63.13 (230) | 57.75 (113) | 71.43 (101) | 58.37 (16) | ns |
| NH Black/African American | 14.97 (56) | 15.56 (34) | 12.05 (15) | 22.72 (7) | |
| NH Asian | 3.80 (12) | 6.03 (8) | 1.26 (3) | 2.47 (1) | |
| Hispanic | 13.98 (71) | 16.99 (42) | 12.06 (25) | 6.80 (4) | |
| Other | 4.12 (39) | 3.66 (18) | 3.20 (14) | 9.63 (7) | |
|
| |||||
| Household Income | |||||
|
| |||||
| Less than $20,000 | 23.57 (105) | 26.97 (58) | 15.68 (34) | 36.13 (13) | ns |
| $20,000-$39,999 | 30.51 (132) | 29.87 (69) | 33.65 (53) | 22.18 (10) | |
| $40,000-$74,999 | 16.95 (58) | 15.90 (29) | 16.18 (23) | 24.65 (6) | |
| $75,000 or greater | 28.97 (113) | 27.26 (59) | 34.49 (48) | 17.04 (6) | |
Notes. Data from 2016-2018 are pooled. % = Proportion of latent class. Estimates are weighted to account for NSDUH’s complex sampling design.
Discussion
The present study provides a number of important findings concerning DUIH in the US.
The first key finding is that a disconcerting number of hallucinogen users—nearly one in ten individuals reporting past-year use (9%)—in the US reports driving under the influence of substances we know distort one’s perception of reality, including visual and auditory hallucinations and the feeling of disconnection from one’s body and surroundings (National Institute of Drug Abuse, 2014). Fortunately, given that only 2.5% of the population reports past year hallucinogen use, DUIH remains a low prevalence phenomenon. Indeed, our estimates suggest that only one in every 5000 Americans (0.2%) takes part in this high-risk, illegal behavior. Nevertheless, this translates to several hundred thousand individuals driving automobiles over the course of the year while experiencing hallucinations and dissociative states. Moreover, this is all the more disconcerting in light of emerging evidence that hallucinogen use is rapidly increasing nationwide (Killion et al., 2021; Yockey et al., 2020).
The second key finding is that some hallucinogen users are more likely than are others to operate a vehicle while under the influence. As a case in point, we see that the likelihood of DUIH is substantially higher among more regular users than it is among the majority of users who consume hallucinogens sporadically. Most past-year hallucinogen users report no past month use (87%) and, among past month users, 45% report only one day of use—the probability of DUIH for these two lower-use groups is 7% and 12%, respectively. In contrast, the predicted probability of DUIH among those reporting multiple instances of hallucinogen use in the past month was greater than 30%. Additionally, we see that rates of DUIH are higher among men than among women (10% versus 7%) and two times higher among NH Black/African Americans than among all other racial/ethnic groups (16% versus 8%). The finding that there is higher risk behavior among male hallucinogen users is consistent with a large body of research showing that dangerous and problem behavior—including driving under the influence of alcohol—is consistently higher among both drug-using and abstinent men than among their female counterparts (Salas-Wright et al., 2016). The finding relating to NH Black/African Americans, however, is surprising in light of research indicating that rates of driving under the influence of alcohol and cannabis are comparable to or lower than other racial/ethnic groups (Oh et al., 2020; Salas-Wright et al., 2021). Future research should seek to test this finding using data from other national studies, and examine the situational and attitudinal factors that may be uniquely impacting NH Black/African Americans.
A third key finding is that, among hallucinogen users, those who report DUIH are more likely to experience behavioral problems. Perhaps unsurprisingly, hallucinogen users reporting DUIH are substantially more likely to report driving under the influence of alcohol, cannabis, and other illicit drugs. Indeed, among those reporting DUIH, more than 80% report also driving under the influence of cannabis compared to 45% of hallucinogen users reporting no DUIH and 9% of non-hallucinogen users. We also see that those DUIH are more likely to report involvement in other illegal substance related behaviors (i.e., drug selling) and being arrested in the past year. This finding is in keeping with prior evidence suggesting that illegal or problem behaviors tend to be highly co-occurring, especially among substance users (Vaughn et al., 2016, 2014). It is interesting to note that, although rates of substance misuse were high among all hallucinogen users (compared to non-users), substance misuse did not distinguish between those reporting no/any DUIH. Indeed, no significant differences in heavy drinking or cannabis use were observed between those reporting no versus any past-year DUIH, and only modest differences were observed for illicit drug use. This suggests that, while polydrug use is widespread among hallucinogen users, it is likely that other factors—perhaps those related to impulse control and deviant behavior in general—are more closely related to DUIH. Further research into the interplay between polysubstance use and DUIH, including key situational and decision-making processes, is warranted.
A fourth key finding is that there exists substantial mental health and behavioral heterogeneity among individuals reporting DUIH. For instance, latent class modeling revealed that half (50%) of those reporting DUIH also reported very high levels of cannabis use and driving under the influence of cannabis in combination with relatively lower levels of other mental health problems and problem behaviors (i.e., Class #1, “Cannabis Drivers”). Additionally, more than one third (39%) of those DUIH reported very high rates of driving under the influences of alcohol, cannabis, and other illicit drugs (i.e., Class #2, “Polydrug Drivers”). Roughly one in ten individuals (11%) reporting DUIH, however, reported elevated levels of mental health problems in combination with comparatively low levels of alcohol and other drug misuse, driving under the influence of other substances, and drug selling (i.e., Class #3, “Mental Health”). These findings underscore the fact that, while we can speak of general correlates among those DUIH, we should be careful not to lump together all individuals, as there exist distinct subtypes of those DUIH, which are identifiable based on mental health and behavioral characteristics.
Implications
Study findings have a number of implications for policy and public health practice. One is that our study findings make clear that a disconcerting number of hallucinogen users report DUIH. Not only is this behavior illegal, but it also likely—based on prior research on the effects of hallucinogen use and their impact on skills needed for safe driving—places others at risk. At a minimum, health and social service providers who screen for hallucinogen use should discuss the illegality and dangers of DUIH with individuals who report use. Additionally, as breathalyzer instruments have been developed for cannabis (Hwang et al., 2019), it may be worthwhile for scientists to consider the utility of such technologies for hallucinogen use as well. A second implication relates to the identification of very high annual rates of DUIH among specific behavioral subgroups (e.g., other illicit drug users, individuals driving under the influence of other drugs). This might take the form of incorporating content on DUIH in drug treatment center programming or in content designed specifically for individuals arrested for driving under the influence in general.
Limitations
Findings from the present study should be interpreted in light of several limitations. First, NSDUH data are entirely based on respondent self-report and not urine or blood analysis (for drug use). Although challenging in a large national study, future research would benefit from the use of other forms of reporting that obviate social desirability and recall biases. Second, despite pooling several survey years in order to increase our sample size and statistical power, data from the NSDUH are cross-sectional in nature. Third, although we are able to examine a number of key correlates, the NSDUH data do not allow us to examine precise situational or contextual factors that specifically contribute to DUIH. In future studies, it would be beneficial to move beyond self-report data (e.g., include multiple reporters and include biological samples analysis), utilize longitudinal data to examine within-person change and prospective associations, and use a mixed method approach to specifically examine the antecedents and decision-making processes among hallucinogen users who decide to operate a motor vehicle and those who elect not to drive under the influence.
Conclusion
Study findings indicate that nearly one in every ten (9%) hallucinogen users reports DUIH in the previous year, and that roughly one in three frequent hallucinogen users reports having driven under the influences of hallucinogens. These are a profoundly disconcerting findings, particularly in light of compelling evidence that hallucinogens lead to marked perceptual, cognitive, and psychomotor distortions that can serve to impair driving safety. Notably, our findings also indicate that individuals who drive under the influence of hallucinogens are at elevated risk of experiencing myriad behavioral problems, including co-occurring alcohol and drug misuse, driving under the influence of other psychoactive drugs, and criminal justice system involvement. As the use of hallucinogens in the U.S. increases, driving under the influence of hallucinogens represents an emerging public health concern.
Figure 1. Prevalence (with 95% CIs) of driving under the influence of hallucinogens, 2016-2018, by sex and race/ethnicity among individuals reporting past-year hallucinogen use.
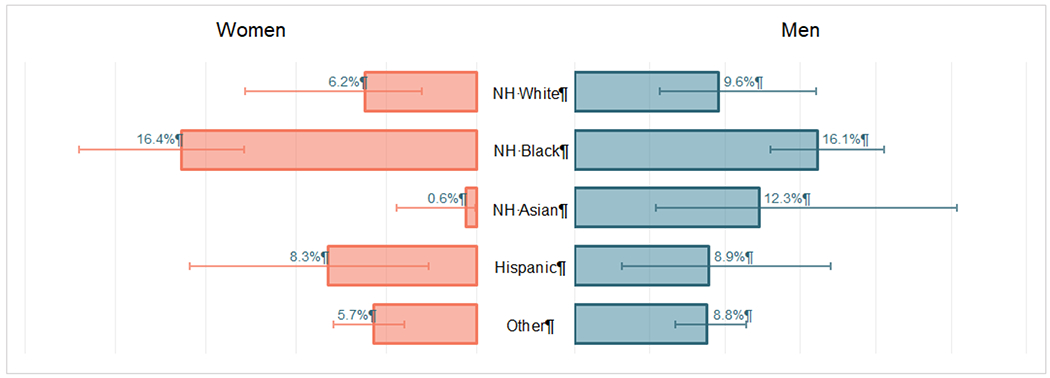
Notes. NH, Non-Hispanic. Data from the National Survey on Drug Use and Health.
Highlights.
Nearly 1/10 hallucinogen users drove under the influence of hallucinogens (DUIH)
Higher risk of DUIH was found among regular users, men, and Black/African Americans
Users who DUIH had higher likelihood for psychological and behavioral problems
Mental health and behavioral heterogeneity exists among individuals who DUIH
Role of Funding Source:
This work was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health [Award Number K01AA026645]. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIAAA or the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: No conflict declared.
References
- Bogenschutz MP, Johnson MW, 2016. Classic hallucinogens in the treatment of addictions. Prog. Neuro-Psychopharmacology Biol. Psychiatry 64, 250–258. 10.1016/j.pnpbp.2015.03.002 [DOI] [PubMed] [Google Scholar]
- Brookhuis KA, De Waard D, Samyn N, 2004. Effects of MDMA (ecstasy), and multiple drugs use on (simulated) driving performance and traffic safety. Psychopharmacology (Berl). 173, 440–445. 10.1007/s00213-003-1714-5 [DOI] [PubMed] [Google Scholar]
- Chen H, Cohen P, Chen S, 2010. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Commun. Stat. Simul. Comput 39, 860–864. 10.1080/03610911003650383 [DOI] [Google Scholar]
- Degenhardt L, Dillon P, Duff C, Ross J, 2006. Driving, drug use behaviour and risk perceptions of nightclub attendees in Victoria, Australia. Int. J. Drug Policy 17, 41–46. 10.1016/j.drugpo.2005.12.004 [DOI] [Google Scholar]
- Donovan JE, 1993. Young adult drinking-driving: Behavioral and psychosocial correlates. J. Stud. Alcohol 54, 600–613. 10.15288/jsa.1993.54.600 [DOI] [PubMed] [Google Scholar]
- Frances RJ, Miller SI, Mack AH, 2011. Clinical textbook of addictive disorders, 3rd ed. ed. Guilford Press, New York. [Google Scholar]
- Giorgetti R, Marcotulli D, Tagliabracci A, & Schifano F (2015). Effects of ketamine on psychomotor, sensory and cognitive functions relevant for driving ability. Forensic Science International, 252, 127–142. [DOI] [PubMed] [Google Scholar]
- Hidalgo B, Goodman M, 2013. Multivariate or multivariable regression? Am. J. Public Health 103, 39–40. 10.2105/AJPH.2012.300897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang SI, Franconi NG, Rothfuss MA, Bocan KN, Bian L, White DL, … & Star A (2019). Tetrahydrocannabinol detection using semiconductor-enriched single-walled carbon nanotube chemiresistors. ACS sensors, 4(8), 2084–2093. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Hendricks PS, Barrett FS, Griffiths RR, 2019. Classic psychedelics: An integrative review of epidemiology, therapeutics, mystical experience, and brain network function. Pharmacol. Ther 197, 83–102. 10.1016/j.pharmthera.2018.11.010 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SLT, Manderscheid RW, Walters EE, Zaslavsky AM, 2003. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 60, 184–189. 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- Killion B, Hai AH, Vaughn MG, Oh S, Oh S, Alsoami A, & Salas-Wright CP (2021). LSD use and in the United States: Trends, correlates, and a typology of use. Drug and Alcohol Dependence. [DOI] [PubMed] [Google Scholar]
- Matthews AJ, Bruno R, Dietze P, Butler K, & Burns L (2014). Driving under the influence among frequent ecstasy consumers in Australia: Trends over time and the role of risk perceptions. Drug and Alcohol Dependence, 144, 218–224. [DOI] [PubMed] [Google Scholar]
- McLachlan GJ, Peel D, 2004. Finite mixture models. John Wiley & Sons, New York. [Google Scholar]
- National Institute of Drug Abuse, 2014. Hallucinogens and dissociative drugs report [WWW Document]. URL https://www.drugabuse.gov/sites/default/files/hallucinogensrrs4.pdf (accessed 1.9.21).
- National Institute on Alcohol Abuse and Alcoholism, n.d. Drinking Levels Defined [WWW Document]. URL https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking (accessed 1.9.21).
- National Institute on Drug Abuse (2019). Drugged driving. https://www.drugabuse.gov/publications/drugfacts/drugged-driving (accessed 3.5.21)
- Oh S, Vaughn MG, Salas-Wright CP, AbiNader MA, Sanchez M, 2020. Driving under the influence of Alcohol: Findings from the NSDUH, 2002–2017. Addict. Behav 108, 106439. 10.1016/j.addbeh.2020.106439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penning R, Veldstra J, Daamen AP, Olivier B, Verster JC, 2010. Drugs of abuse and traffic safety. Curr. Drug Abuse Rev 3, 23–32. 10.1007/978-1-4614-3375-0_44 [DOI] [PubMed] [Google Scholar]
- Pilatti A, Bravo AJ, & Pautassi RM (2020). Contexts of alcohol use: a latent class analysis among Argentinean college students. Drug and Alcohol Dependence, 209, 107936. [DOI] [PubMed] [Google Scholar]
- Salas-Wright CP, Cano M, Hai AH, Oh S, Vaughn MG, 2021. Prevalence and correlates of driving under the influence of cannabis in the United States. Am. J. Prev. Med [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright Christopher P., Hai AH, Oh S, Alsolami A, Vaughn MG, 2021. Trends in cannabis views and use among american adults: Intersections with alcohol consumption, 2002-2018. Addict. Behav 106818. 10.1016/j.addbeh.2021.106818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG, Reingle Gonzalez JM, 2016. Drug Abuse and Antisocial Behavior: A Biosocial Life Course Approach. Palgrave Macmillan, New York. [Google Scholar]
- Shalit N, Rehm J, Lev-Ran S, 2019. Epidemiology of hallucinogen use in the U.S. results from the National epidemiologic survey on alcohol and related conditions III. Addict. Behav 89, 35–43. 10.1016/j.addbeh.2018.09.020 [DOI] [PubMed] [Google Scholar]
- StataCorp, L.P., 2019. Stata data analysis and statistical Software. [Google Scholar]
- Strand MC, Gjerde H, Mørland J, 2016. Driving Under the Influence of Non-Alcohol Drugs-An Update. Part II: Experimental Studies. Forensic Sci. Rev 28, 79–101. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Data Archive, 2014. SAMHDA FAQs: How do I account for effects of complex sampling design (design effects) when analyzing DAWN data?
- Substance Abuse and Mental Health Services Administration, 2020. What is NSDUH? [WWW Document]. URL https://nsduhweb.rti.org/respweb/homepage.cfm (accessed 7.1.20).
- Vaughn MG, Salas-Wright CP, Alsolami A, Oh S, Clark TC, 2021. Margin for error: Examining racial and ethnic trends in risk propensity. Soc. Psychiatry Psychiatr. Epidemiol [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Salas-Wright CP, DeLisi M, Maynard BR, 2014. Violence and Externalizing Behavior Among Youth in the United States: Is There a Severe 5%? Youth Violence Juv. Justice 12, 3–21. 10.1177/1541204013478973 [DOI] [Google Scholar]
- Valente JY, Cogo-Moreira H, & Sanchez ZM (2017). Gradient of association between parenting styles and patterns of drug use in adolescence: A latent class analysis. Drug and Alcohol Dependence, 180, 272–278. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Salas-Wright CP, Reingle-Gonzalez JM, 2016. Addiction and crime: The importance of asymmetry in offending and the life-course. J. Addict. Dis 35, 213–217. 10.1080/10550887.2016.1189658 [DOI] [PubMed] [Google Scholar]
- Vermunt JK, Magidson J, 2016. Upgrade manual for Latent GOLD 5.1. Statistical Innovations, Belmont, MA. [Google Scholar]
- Yockey RA, Vidourek RA, King KA, 2020. Trends in LSD use among US adults: 2015–2018. Drug Alcohol Depend. 212. 10.1016/j.drugalcdep.2020.108071 [DOI] [PubMed] [Google Scholar]


