Abstract
Background
Effective, evidence-based treatments for opioid use disorder are not equally accessible to Americans. Recent studies have found urban/rural disparities in the driving times to the nearest opioid treatment providers. These disparities may be even worse than currently reported in the literature because patients may not be able to obtain appointments with their nearest provider. We examine the robustness of the opioid treatment infrastructure by estimating how driving times to treatment change as provider availability decreases.
Methods
We used public data from the federal government to estimate the driving time from each census tract centroid to the nearest 15 treatment providers. We summarized the median and interquartile range of driving times to increasingly distant providers (i.e., nearest, second nearest, etc.), stratified by urban/rural classification.
Results
The median driving time to the nearest provider was greater in rural areas than urban areas for both opioid treatment programs (12 minutes vs 61 minutes) and buprenorphine-waivered prescribers (5 minutes vs 21 minutes). Importantly, driving times in rural areas increased more steeply as nearer providers became unavailable. For example, the increase in driving time between the nearest provider and the fifth nearest provider was much greater in rural areas than in urban areas for both buprenorphine-waivered prescribers (23 minutes vs 4 minutes) and for opioid treatment programs (54 minutes vs 22 minutes).
Conclusions
Access to treatment for opioid use disorder is more robust in urban areas compared with rural areas. This disparity must be eliminated if the opioid overdose crisis is to be resolved.
Keywords: opioids, substance use, treatment, urban-rural inequality
Introduction
While fatal opioid-related overdoses continue to rise in both urban and rural areas of the U.S. (Hedegaard et al., 2019; Hedegaard and Spencer, 2021), access to evidence-based treatment remains unequally distributed, with people in rural areas needing to drive greater distances to access fewer, more geographically-dispersed opioid agonist treatment providers (Ghertner, 2019; Joudrey et al., 2020; Kleinman, 2020; Langabeer et al., 2020). Opioid agonist treatment remains highly stigmatized (Tsai et al., 2019), and this stigma contributes to disparities in access to evidence-based treatment (Stone et al., 2021). These geographical disparities in access have important clinical consequences given that greater distance to treatment is associated with lower retention in care (Amiri et al., 2018). “Nearest provider” estimates may underestimate real-world rural/urban inequalities in access to opioid agonist treatment because the nearest provider may not be accepting new patients or may not accept the patient’s insurance and because rural patients are more likely to be uninsured (Day, 2019; Joudrey et al., 2020; Kleinman, 2020). For example, a recent audit study found that only one-fifth of simulated Medicaid enrollees seeking treatment could obtain an appointment for buprenorphine induction in rural areas (Beetham et al., 2019). The robustness of physical access to opioid treatment providers, measured as changes in driving time to successively farther providers, is not known. We estimated the extent to which driving time to the nearest opioid treatment providers increased as the capacity or availability of nearer opioid treatment providers decreased.
Methods
We used publicly available data from the U.S. Substance Abuse and Mental Health Services Administration Buprenorphine Practitioner Locator (BPL) (SAMHSA, 2020a) and Opioid Treatment Program Directory (OTP) (SAMHSA, 2020b) to identify opioid agonist treatment providers (buprenorphine-waivered prescribers and opioid treatment programs) on July 5, 2020. The raw data include 51,211 observations from the BPL database and 1,767 observations from the OTP directory. We pre-processed the files by excluding exact duplicates (BPL, N=133; OTP, N=14), locations outside the 50 United States and Washington, D.C. (BPL, N=413; OTP, N=0), and P.O. Boxes (BPL, N=159; OTP, N=6). Using the pre-processed street address, city, and state, we created queries for the Google Maps Geocoding Application Programming Interface (API) (Google, 2020). Because multiple providers can be located at the same address, we further excluded duplicate Google Maps API queries (BTP, N=9,597; OTP, N=6). After querying the Google Maps Geocoding API, we excluded duplicate locations that mapped to the same standardized address (e.g., “1000 4th Street” and “1000 Fourth St” would both map to the standardized address “1000 4th St” through the Google Maps API) or queries that yielded approximate locations (e.g., locations not classified as a building in the Google Maps API). The final sample included 31,053 unique locations for all opioid treatment providers. The BPL files yielded 30,009 locations. The OTP files yielded 1,691 locations. There were 647 locations in both datasets.
We used the 2017 U.S. Census Bureau TIGER/Line shapefiles (Bureau, 2020) to estimate the driving distance from each census tract centroid to the 15 nearest opioid treatment providers using the Open Source Routing Machine (http://project-osrm.org) (Luxen and Vetter, 2011), which takes into account the speed limits of roads. We ranked providers by driving time, and assumed patients prefer to seek treatment at the nearest available provider, such that if the nearest provider was unavailable, they would seek treatment at the second closest, and so on. For each county in the U.S., we estimated the tract-level population-weighted mean, median, standard deviation, and interquartile range in driving time and driving distance to increasingly distant providers (i.e., the nearest, second nearest, etc.), stratifying the results by urban (large central metro, large fringe metro, medium metro, small metro) and rural (micropolitan, non-core) classification code. Each county (and tract within that county) was classified as either “urban” (i.e., large central metro, large fringe metro, medium metro, small metro) or “rural” (i.e., micropolitan, non-core) according to the 2013 Urban-Rural Classification Scheme for Counties developed by the U.S. National Center for Health Statistics (Ingram and Franco, 2014). In this classification scheme, large central metro counties (the most urban) are those with metropolitan statistical areas (MSAs) of 1 million or more population that also contain the entire population of the largest city or have the entire population within the largest city or have at least 250,000 inhabitants in a principal MSA city. Large fringe metro counties are in MSAs of 1 million or more population that are not large central metro counties. Medium metro counties are those with MSAs of populations between 250,000 and 999,999. Small metro counties are counties in MSAs with populations of less than 250,000. Micropolitan (rural) counties are those in micropolitan statistical areas and lastly noncore (most rural) counties are those that did not quality as urban or micropolitan. We used the 2017 5-year ACS for tract-level population estimates.
All analyses were stratified by treatment type (buprenorphine-waivered prescribers vs opioid treatment programs) because regulations on access to buprenorphine and methadone differ. In the context of our analysis, the most notable difference is that buprenorphine is typically prescribed in an office setting, whereas opioid treatment programs which dispense methadone generally require patients to be physically present for daily dosing. We conducted two sensitivity analyses, repeating the same analysis (1) allowing for multiple providers at a single address (assuming any duplicate is a different provider at the same location) and (2) using the US Census Bureau’s census tract-level center of population instead of geographic centroid of the tract. The raw data and replication code are available online at: https://github.com/mkiang/opioid_treatment_distance/.
Results
Median driving times to the nearest opioid treatment provider were both greater and more variable in rural areas compared with urban areas, particularly for opioid treatment programs compared with buprenorphine-waivered prescribers. In rural areas, median driving times were highly sensitive to provider availability in the local treatment infrastructure (Figure 1). For example, if a person seeking treatment in a rural area could not access the four nearest buprenorphine-waivered prescribers, s/he would face 44 minutes (interquartile range [IQR], 28–64 minutes) of driving time to the 5th nearest provider -- an increase of 23 more minutes of driving time (compared with 4 more minutes for someone living in an urban area). For opioid treatment programs, which require patients to be physically present for daily dosing of methadone, the driving time to the nearest and 5th nearest providers were higher (compared with access to buprenorphine-waivered prescribers). Specifically, if a person seeking treatment in a rural area could not access the four nearest opioid treatment programs, s/he would face 116 total minutes of driving time (IQR, 85–67) or an increase of 55 minutes, compared with a person seeking treatment in an urban area, who would face a total driving time of 33 minutes (IQR, 19–65) or an increase of 21 minutes.
Figure 1.
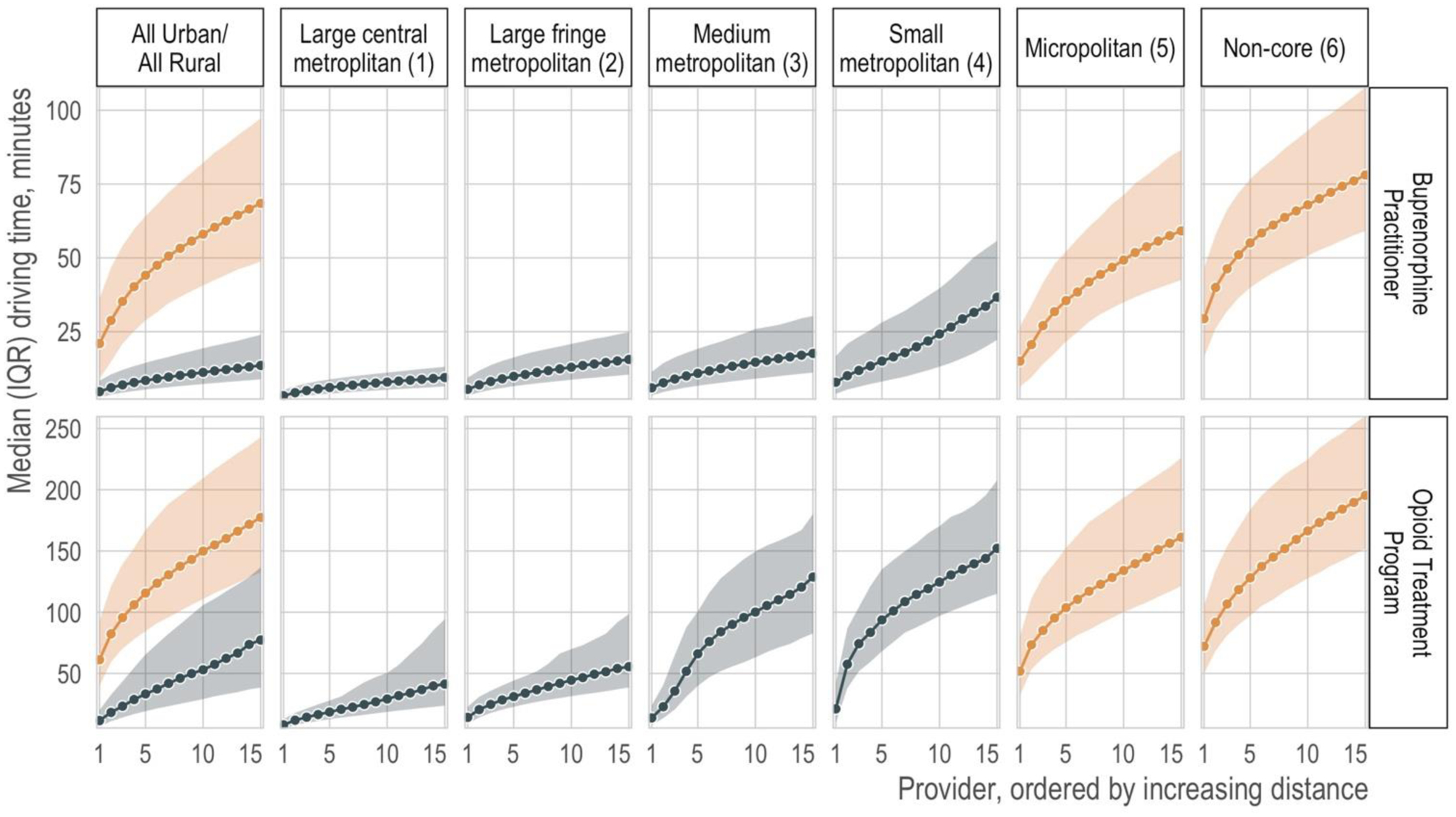
Median (points) and interquartile range (IQR; shaded regions) of driving time from census tract centroids to the 15 nearest opioid treatment providers, by urban (blue) vs. rural (orange) classification code. Note: The magnitude of the y-axis differs between the top and bottom rows. Numerical representations of these data are available in the Supplement.
There was substantial geographic dispersion in opioid treatment programs. People living in large regions of the U.S., particularly the upper Midwest and Southwest, would need to drive an additional hour to obtain treatment from the 5th nearest, rather than the nearest, opioid treatment program and over two hours for people living in many counties (Figure 2). In contrast, in urban counties, median driving times changed little from the 1st to 5th nearest opioid treatment program (Figure 1). Our results remained consistent in sensitivity analyses allowing for multiple providers at a single address and using centers of population instead of geographic centers (Supplement).
Figure 2.
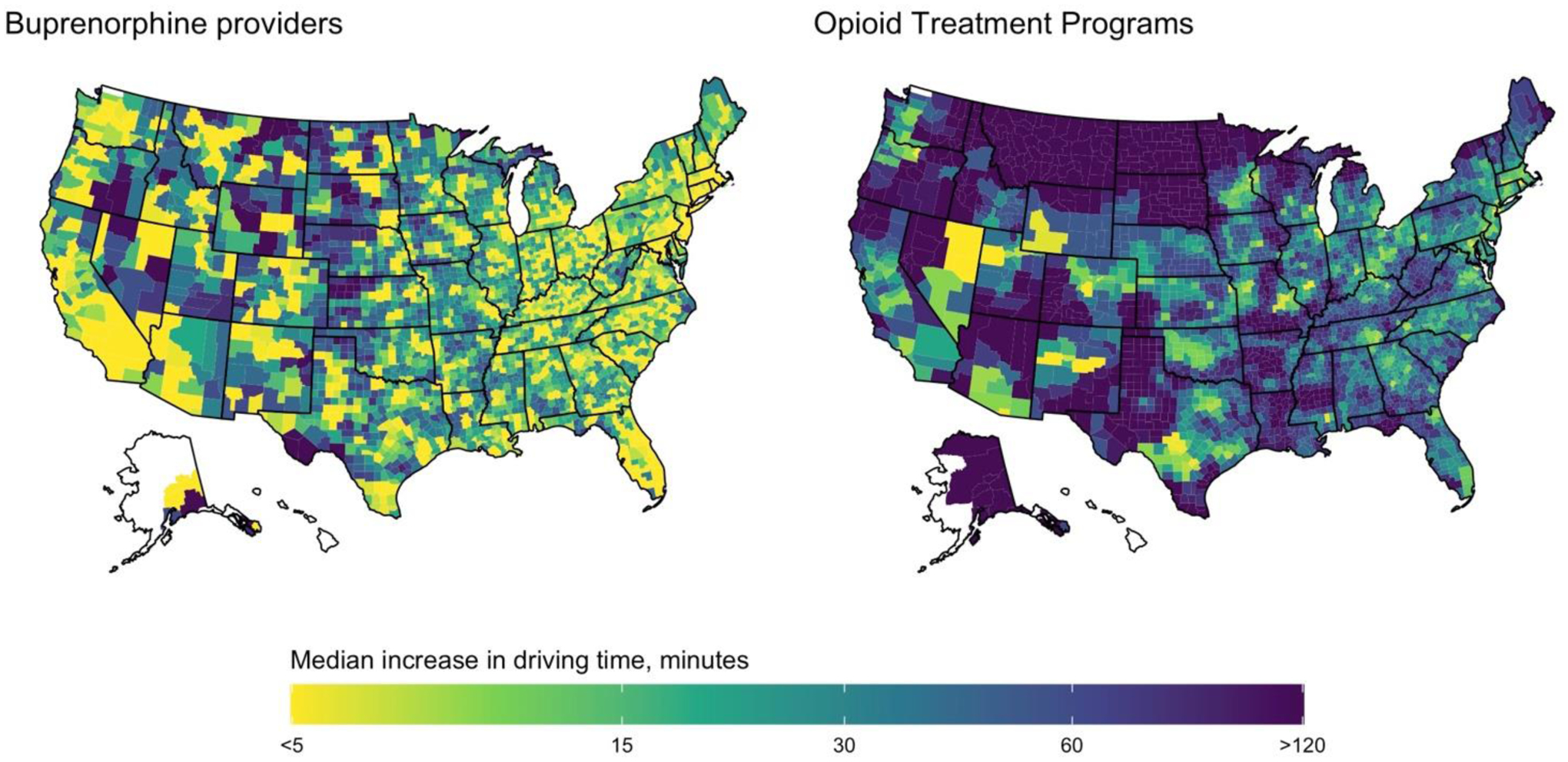
Median increase in driving time between the nearest opioid treatment provider and the 5th nearest opioid treatment provider.
Discussion
In this nationwide study of geographic access to opioid agonist treatment in the US, we found that median driving times were highly sensitive to availability of treatment providers in the local treatment infrastructure, particularly in rural areas (Figure 1). The increases in median driving times to next-nearest opioid treatment providers are relevant when nearest providers, when contacted, either do not offer appointments (Beetham et al., 2019; Huhn and Dunn, 2017; Tsai et al., 2019), do not accept the patient’s insurance (or do not accept uninsured patients), or offer non-evidence based treatment (Beetham et al., 2020), thereby requiring prospective patients -- especially those living in rural areas -- to seek evidence-based treatment from providers located even farther away. Patients can also be forced elsewhere if a hospital closes, a disproportionately common occurrence in rural areas (Seigel, 2019). The increase in driving time from the nearest to the 5th nearest provider is especially stark for opioid treatment programs, with large swaths of the country facing a hypothetical increase in 2 hours of driving time (Figure 2).
Research consistently finds that lowering barriers to access and treatment results in better outcomes (Deering et al., 2011; Kourounis et al., 2016; Nolan et al., 2015; Truong et al., 2019). Thus, our analysis highlights a worrisome finding: patients in rural areas must travel farther, and are more likely to experience substantial increases in driving time, due to limited provider availability. One national study found that patients living in rural areas, compared with patients living in urban areas, reported greater concerns about travel costs (Henning-Smith et al., 2018). The low availability of public transportation in rural areas (APTA, 2013) makes car ownership, and driving for medical care, even more of a necessity (Syed et al., 2013). In addition, patients in rural areas face other substantial barriers. Rural patients, on average, tend to be older, sicker, and poorer than urban patients (Jensen et al., 2020; Rhubart et al., 2020). Rural residents are less likely to have health insurance (Day, 2019), often relying on strong social relationships; however, rural residents may still face challenges when accessing assistance from their social networks (Cohen and Bennett, 2016; Leider et al., 2020). Relative to urban areas, rural areas lack an adequate supply of mental health providers (Summers-Gabr, 2020). Recently, there has been a push to leverage telehealth for treatment of substance use disorders (Oesterle et al., 2020), but rural areas have limited broadband internet (Busby et al., 2021), making such interventions difficult to implement. As a result of all these factors, the lack of a robust treatment infrastructure in rural areas is likely to exacerbate urban-rural inequities (Leider et al., 2020).
This study has important limitations. The Buprenorphine Provider List and Opioid Treatment Program list may not represent all providers and may be out of date. However, they reflect the information publicly available to a treatment-seeking patient. We assume prospective patients have access to a car or form of public transit that uses the road network (e.g., buses but not trains); however, the rate of car ownership among patients is not known. In the US, only 8.6% of households do not own a vehicle, and the rate of car ownership is higher in rural areas (where only 6.5% of households do not own a vehicle) (Bureau, 2021). Similarly, outside of a handful of dense urban mass areas with rail systems, US public transit consists primarily of buses, which must adhere to speed limits and road infrastructure. For example, only 5% of the US population commutes by public transportation (Burrows et al., 2021). Therefore, our estimates likely represent the lower bound of travel time for most Americans. Our results are unlikely to be applicable to other countries where rates of private car ownership are lower.
Despite these limitations, our study demonstrates that “nearest provider” metrics (Joudrey et al., 2020; Kleinman, 2020) likely overestimate the robustness of access to opioid treatment providers for people with opioid use disorders living in rural areas. Policies designed to increase access to treatment of opioid use disorder, such as increasing reimbursement to providers for opioid agonist therapy, mandating coverage of all evidence-based substance use disorder treatments in Medicaid (Andrews and Humphreys, 2019), pharmacy-based methadone dispensing (Joudrey et al., 2020) regulatory changes lowering barriers to obtaining a buprenorphine prescribing waiver (Fiscella et al., 2019; SAMHSA, 2021) will not only improve “nearest provider” metrics of access but also improve the robustness of the local treatment infrastructure, thereby reducing inequities in access to treatment.
Supplementary Material
Highlights.
Patients in rural areas face greater burden to physical access for treatment of opioid use disorder
Rural patients experience higher driving times as provider availability decreases
Provider availability only slightly affect driving times in urban areas
Funding:
MVK is supported in part by the U.S. National Institutes of Health (K99DA051534 and T32DA035165). KH is supported by the Esther Ting Memorial Professorship and a career research scientist grant from the Veterans Affairs Health Services Research and Development Service (RCS 04-141-3). ACT is supported in part by the Sullivan Family Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Role of Funding Source
The funders had no role in the design, data collection, writing, or decision to publish this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
Dr. Barnett reports being retained as an expert witness by plaintiffs in lawsuits against opioid manufacturers. All other authors have no conflicts to declare.
References
- Amiri S, Lutz R, Socías E, McDonell MG, Roll JM, Amram O, 2018. Increased distance was associated with lower daily attendance to an opioid treatment program in Spokane County Washington. J Subst Abuse Treat 93, 26–30. 10.1016/j.jsat.2018.07.006 [DOI] [PubMed] [Google Scholar]
- Andrews CM, Humphreys K, 2019. Investing in Medicaid to End the Opioid Epidemic. Psychiatr Serv 70, 537–537. 10.1176/appi.ps.70705 [DOI] [PubMed] [Google Scholar]
- APTA, 2013. American Public Transportation Association 2013 Public Transportation Fact Book.
- Beetham T, Saloner B, Gaye M, Wakeman SE, Frank RG, Barnett ML, 2020. Therapies Offered at Residential Addiction Treatment Programs in the United States. Jama 324, 804–806. 10.1001/jama.2020.8969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beetham T, Saloner B, Wakeman SE, Gaye M, Barnett ML, 2019. Access to Office-Based Buprenorphine Treatment in Areas With High Rates of Opioid-Related Mortality. Ann Intern Med 171, 1. 10.7326/m18-3457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau UC, 2021. Table DP04 Selected Housing Characteristics (5-year ACS) [WWW Document]. URL https://data.census.gov/cedsci/table?tid=ACSDP5Y2019.DP04&hidePreview=true (accessed 7.9.21).
- Bureau UC, 2020. TIGER/Line Shapefiles [WWW Document]. URL https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-line-file.html (accessed 7.10.20).
- Burrows M, Burd C, McKenzie B, 2021. Commuting by Public Transportation in the United States: 2019, American Community Survey Reports. US Census Bureau. [Google Scholar]
- Busby J, Tanberk J, Cooper T, 2021. BroadbandNow Estimates Availability for all 50 States; Confirms that More than 42 Million Americans Do Not Have Access to Broadband [WWW Document]. URL https://broadbandnow.com/research/fcc-broadband-overreporting-by-state (accessed 7.9.21).
- Cohen AL, Bennett CR, 2016. Support Network Connectedness in the Lives of Community-Dwelling Rural Elders and Their Families. Marriage Fam Rev 53, 576–588. 10.1080/01494929.2016.1247763 [DOI] [Google Scholar]
- Day JC, 2019. Health Insurance in Rural America [WWW Document]. URL https://www.census.gov/library/stories/2019/04/health-insurance-rural-america.html (accessed 7.9.21).
- Deering DEA, Sheridan J, Sellman JD, Adamson SJ, Pooley S, Robertson R, Henderson C, 2011. Consumer and treatment provider perspectives on reducing barriers to opioid substitution treatment and improving treatment attractiveness. Addict Behav 36, 636–642. 10.1016/j.addbeh.2011.01.004 [DOI] [PubMed] [Google Scholar]
- Fiscella K, Wakeman SE, Beletsky L, 2019. Buprenorphine Deregulation and Mainstreaming Treatment for Opioid Use Disorder. Jama Psychiat 76, 229–230. 10.1001/jamapsychiatry.2018.3685 [DOI] [PubMed] [Google Scholar]
- Ghertner R, 2019. U.S. trends in the supply of providers with a waiver to prescribe buprenorphine for opioid use disorder in 2016 and 2018. Drug Alcohol Depen 204, 107527. 10.1016/j.drugalcdep.2019.06.029 [DOI] [PubMed] [Google Scholar]
- Google, 2020. Google Developers Geocoding API [WWW Document]. URL https://developers.google.com/maps/documentation/geocoding/overview (accessed 7.20.21).
- Hedegaard H, Miniño AM, Warner M, 2019. Urban-rural Differences in Drug Overdose Death Rates, by Sex, Age, and Type of Drugs Involved, 2017. Nchs Data Brief 1–8. [PubMed] [Google Scholar]
- Hedegaard H, Spencer MR, 2021. Urban-Rural Differences in Drug Overdose Death Rates, 1999–2019. Nchs Data Brief 1–8. [PubMed] [Google Scholar]
- Henning-Smith C, Evenson A, Kozhimannil K, Moscovice I, 2018. Geographic variation in transportation concerns and adaptations to travel-limiting health conditions in the United States. J Transp Health 8, 137–145. 10.1016/j.jth.2017.11.146 [DOI] [Google Scholar]
- Huhn AS, Dunn KE, 2017. Why aren’t physicians prescribing more buprenorphine? Journal of Substance Abuse Treatment 78, 1–7. 10.1016/j.jsat.2017.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram DD, Franco SJ, 2014. 2013 NCHS Urban-Rural Classification Scheme for Counties. Vital Heal Statistics Ser 2 Data Evaluation Methods Res 1–73. [PubMed] [Google Scholar]
- Jensen L, Monnat SM, Green JJ, Hunter LM, Sliwinski MJ, 2020. Rural Population Health and Aging: Toward a Multilevel and Multidimensional Research Agenda for the 2020s. Am J Public Health 110, 1328–1331. 10.2105/ajph.2020.305782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joudrey PJ, Chadi N, Roy P, Morford KL, Bach P, Kimmel S, Wang EA, Calcaterra SL, 2020. Pharmacy-based methadone dispensing and drive time to methadone treatment in five states within the United States: A cross-sectional study. Drug Alcohol Depen 211, 107968. 10.1016/j.drugalcdep.2020.107968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman RA, 2020. Comparison of Driving Times to Opioid Treatment Programs and Pharmacies in the US. Jama Psychiat 77, 1163–1171. 10.1001/jamapsychiatry.2020.1624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kourounis G, Richards BDW, Kyprianou E, Symeonidou E, Malliori M-M, Samartzis L, 2016. Opioid substitution therapy: Lowering the treatment thresholds. Drug Alcohol Depen 161, 1–8. 10.1016/j.drugalcdep.2015.12.021 [DOI] [PubMed] [Google Scholar]
- Langabeer J, Stotts AL, Cortez A, Tortolero G, Champagne-Langabeer T, 2020. Geographic Proximity to Buprenorphine Treatment Providers in the U.S. Drug Alcohol Depen 213, 108131. 10.1016/j.drugalcdep.2020.108131 [DOI] [PubMed] [Google Scholar]
- Leider JP, Meit M, McCullough JM, Resnick B, Dekker D, Alfonso YN, Bishai D, 2020. The State of Rural Public Health: Enduring Needs in a New Decade. Am J Public Health 110, 1283–1290. 10.2105/ajph.2020.305728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luxen D, Vetter C, 2011. Real-time routing with OpenStreetMap data. Proceedings of the 19th ACM SIGSPATIAL International Conference on Advances in Geographic Information Systems. 10.1145/2093973.2094062 [DOI] [Google Scholar]
- Nolan S, Hayashi K, Milloy M-J, Kerr T, Dong H, Lima VD, Lappalainen L, Montaner J, Wood E, 2015. The impact of low-threshold methadone maintenance treatment on mortality in a Canadian setting. Drug Alcohol Depen 156, 57–61. 10.1016/j.drugalcdep.2015.08.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oesterle TS, Kolla B, Risma CJ, Breitinger SA, Rakocevic DB, Loukianova LL, Hall-Flavin DK, Gentry MT, Rummans TA, Chauhan M, Gold MS, 2020. Substance Use Disorders and Telehealth in the COVID-19 Pandemic Era: A New Outlook. Mayo Clin Proc 95, 2709–2718. 10.1016/j.mayocp.2020.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhubart DC, Monnat SM, Jensen L, Pendergrast C, 2020. The Unique Impacts of U.S. Social and Health Policies on Rural Population Health and Aging. Public Policy Aging Rep 31, 24–29. 10.1093/ppar/praa034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA, 2021. FAQs About the New Buprenorphine Practice Guidelines [WWW Document]. URL https://www.samhsa.gov/medication-assisted-treatment/practitioner-resources/faqs (accessed 7.20.21).
- SAMHSA, 2020a. Buprenorphine Treatment Practitioner Locator [WWW Document]. URL https://www.samhsa.gov/medication-assisted-treatment/practitioner-program-data/treatment-practitioner-locator (accessed 7.10.20).
- SAMHSA, 2020b. OTP Directory [WWW Document]. URL https://dpt2.samhsa.gov/treatment/directory.aspx (accessed 7.10.20).
- Seigel J, 2019. Rural Hospital Closures Rise to Ninety-Eight [WWW Document]. URL https://www.ruralhealthweb.org/blogs/ruralhealthvoices/february-2019/rural-hospital-closures-rise-to-ninety-seven (accessed 7.9.21).
- Stone EM, Kennedy-Hendricks A, Barry CL, Bachhuber MA, McGinty EE, 2021. The role of stigma in U.S. primary care physicians’ treatment of opioid use disorder. Drug Alcohol Depen 221, 108627. 10.1016/j.drugalcdep.2021.108627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summers-Gabr NM, 2020. Rural–urban mental health disparities in the United States during COVID-19. Psychological Trauma Theory Res Pract Policy 12, S222–S224. 10.1037/tra0000871 [DOI] [PubMed] [Google Scholar]
- Syed ST, Gerber BS, Sharp LK, 2013. Traveling Towards Disease: Transportation Barriers to Health Care Access. J Commun Health 38, 976–993. 10.1007/s10900-013-9681-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truong C, Krawczyk N, Dejman M, Marshall-Shah S, Tormohlen K, Agus D, Bass J, 2019. Challenges on the road to recovery: Exploring attitudes and experiences of clients in a community-based buprenorphine program in Baltimore City. Addict Behav 93, 14–19. 10.1016/j.addbeh.2019.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Kiang MV, Barnett ML, Beletsky L, Keyes KM, McGinty EE, Smith LR, Strathdee SA, Wakeman SE, Venkataramani AS, 2019. Stigma as a fundamental hindrance to the United States opioid overdose crisis response. Plos Med 16, e1002969. 10.1371/journal.pmed.1002969 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


