Abstract
We describe the case of a 73-year-old woman with a high body mass index and a virgin abdomen who presented with a 5-day history of abdominal pain, emesis and confusion on admission. Inflammatory markers and renal function were significantly deranged. CT of the abdomen and pelvis demonstrated a clear transition point and faecalisation of the small bowel proximal to the obstruction. It was suggested that the patient may have ingested a foreign object. A collateral history was obtained, making this less likely and confirmed an acute cognitive impairment. She was optimised following multidisciplinary discussion preoperatively. Thereafter, the patient underwent a laparotomy, where a hard, mobile mass was identified in the jejunum. This was diagnosed as an enterolith of dimensions 62×38×32 mm secondary to a duodenal diverticulum. She improved postoperatively with complete resolution of her confusion and renal function. She was discharged on day 14 of admission.
Keywords: gastrointestinal surgery, general surgery
Background
Enteroliths are intestinal concretions and a relatively uncommon finding1, in the absence of previous intra-abdominal surgery, more so.1 2 Their aetiology and presentations are considerably varied, resulting in diagnostic challenges.3 They can be classified into two main categories, namely primary and secondary groups.4
Primary enteroliths tend to occur in areas of intestinal stasis,3 5 with concurrent pathology such as diverticular disease, surgical enteroanastomosis, intestinal kinking from intra-abdominal strictures and other causes.3 6 7 They can be further subdivided into ‘true’ and ‘false’ types based on composition.3 True primary enteroliths are formed from products of chyme whereas their false counterparts arise from substances in the bowel.3 5 8 Secondary enteroliths account for gallbladder or renal stones, which have migrated into the small bowel via fistula formation, ultimately resulting in obstruction.7 9
The reported prevalence of primary and secondary enterolithiasis in selected populations varies widely from 0.3% to 10% and is largely dependent on clinical presentation, aetiology and underlying risk factors.6
This is a case of a 73-year-old woman who presented with signs and symptoms of small bowel obstruction together with a new confusion, significant acute kidney injury and refractory hypotension. This was found to be secondary to the largest enterolith ileus due to a duodenal diverticulum in a patient with a virgin abdomen published. This case highlights the importance of establishing a collateral history in conjunction with confusion screening together with multidisciplinary team (MDT) discussion to improve patient outcomes.
Case presentation
We report the case of a 73-year-old woman who presented to the accident and emergency department with a 5-day history of progressive vomiting and abdominal pain.
On admission she was apyrexial at 36.4°C, her pulse rate was 81 beats/min and her blood pressure was 95/54 mm Hg. She was saturating at 93% on 2 L of oxygen delivered via nasal cannulae and had a respiratory rate of 16 breaths/min. Her lactate was 3.03 and her inflammatory markers and renal function demonstrated significant derangement (table 1).
Table 1.
Patient’s bloods throughout admission
| Bloods on admission | Bloods following 1 day ICU optimisation | Bloods post surgery | Reference values | |
| Haemoglobin | 155 | 117 | 95 | 110–147 g/L |
| Mean corpuscular volume | 83.4 | 82.1 | 87.9 | 80.0–98.1fl |
| Platelets | 333 | 230 | 190 | 150–400×109/L |
| White cell count | 14.0 | 11.9 | 9.1 | 3.5–9.5×109/L |
| Neutrophils | 12.04 | 9.61 | 5.71 | 1.7–6.5×109/L |
| Sodium | 137 | 138 | 141 | 133–146 mmol/L |
| Potassium | 4.2 | 3.8 | 4.2 | 3.5–5.3 mmol/L |
| Urea | 44.6 | 37.9 | 5.2 | 2.5–7.8 mmol/L |
| Creatinine | 547 | 313 | 45 | 44–80 mmol/L |
| Albumin | 48 | 33 | 29 | 35–50 g/L |
| Alkaline phosphatase | 146 | 97 | 63 | 30–130 IU/L |
| C reactive protein | 159 | 95 | 52 | 0.0–5 mg/L |
Values of interest are highlighted in bold for reference and comparative purposes.
ICU, intensive care unit.
Medical history of note included hypertension, osteoarthritis and previous breast cancer. Her drug history included Candesartan and analgesic agents. There was no history of abdominal surgery.
On examination, the patient had significant cognitive impairment and was considerably distressed by her vomiting. She had a body mass index of 42.3 kg/m2 and her abdomen was markedly distended with localised tenderness in the epigastric region, but with no evidence of peritonism. Auscultation of the precordium was unremarkable; heart sounds one and two present with no added sounds audible.
A formal cognitive assessment was performed in order to ascertain the extent of her confusion, which was concluded to be profound. A concomitant collateral history, provided by the patient’s daughter, confirmed that this was, indeed, a new derangement in cognitive function and far removed from the patient’s baseline.
Investigations
CT abdomen and pelvis with contrast (day 1)
The stomach is distended with an air fluid level, multiple distended fluid filled loops of small bowel down to an abrupt change in calibre in the mid pelvis with a ‘faecalisation’ of the mid small bowel contents proximal to the transition point. This area looks like it may represent something swallowed and now blocking small bowel (figure 1). Gallstones within a distended thin wall gallbladder with no air in the biliary tree. Lung bases are clear.
Figure 1.
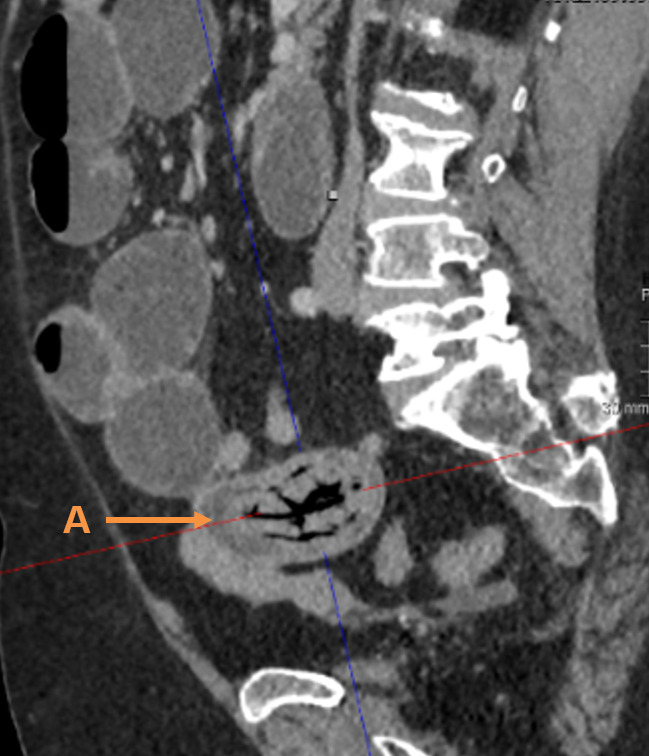
Computed tomography (CT) sagittal view showing the enterolith (A) causing obstruction.
Review addendum post surgery of CT (day 3)
A duodenal diverticulum is seen approximately the same size as the obstruction (figure 2).
Figure 2.
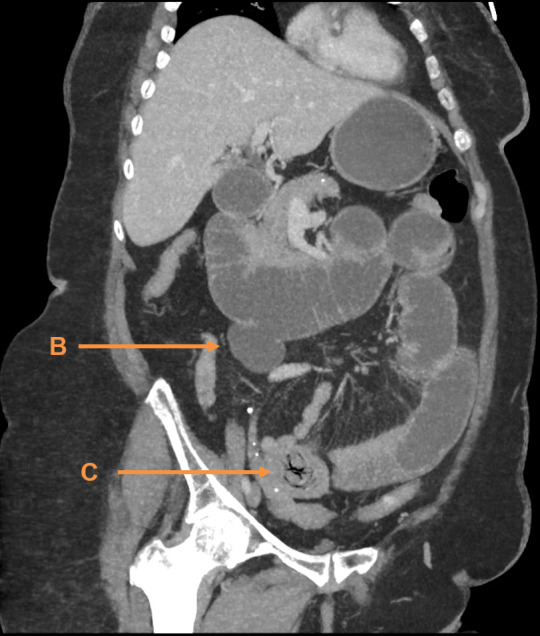
Computed tomography (CT) coronal view showing a duodenal diverticulum (B) and enterolith (C), the obstructing lesion.
The patient’s National Emergency Laparotomy Audit (NELA) mortality score was 29.7% with a morbidity of 95% on admission. Her NELA mortality score was 16.2% with a morbidity of 88% following 1 day of intensive care unit (ICU) optimisation.
Histology
Firm tan mass measuring 62×38×32 mm the composition in keeping with bile salt formation (figures 3 and 4).
Figure 3.

Enterolith specimen (D).
Figure 4.

Enterolith specimen post dissection (E).
Differential diagnosis
The patient’s presentation was that of a small bowel obstruction, likely secondary to adhesional obstruction as she had a virgin abdomen.
The CT scan findings suggested a small bowel obstruction due to an obstructing mass, which could have been due to a foreign object. The collateral history of confusion being recent made a swallowed foreign object less likely.
Gallstone ileus was considered; however, there was no air in the biliary tree. A tumour was also in the differential given the size of the mass.
Treatment
A nasogastric tube and urinary catheter were inserted, in order to facilitate a strict fluid balance, and the patient was given tazocin. Despite ongoing fluid resuscitation and having received 3 L of fluid, her systolic blood pressure remained at 92 mm Hg with a refractory hypotension.
An MDT discussion between anaesthetics, intensive care, general surgery and emergency medicine felt it was safer for the patient to remain in the resuscitation area in the emergency department, with an arterial line sited in order to facilitate the maintenance of her blood pressure. Due to delays in emergency theatres, the patient was admitted to the ICU for further optimisation of her blood pressure and renal function with fluids. The following day her renal function improved.
The patient underwent a laparotomy via a lower midline incision, approximately 24 hours following her initial presentation. A mass was found in the distal jejunum, later diagnosed as an enterolith secondary to a duodenal diverticulum. An enterotomy was performed to remove the structure with subsequent longitudinal enterotomy closure and mass abdominal closure.
Outcome and follow-up
Postoperatively, the patient had a brief stay in ICU. She recovered well and her confusion had resolved completely. The cause of this confusion was likely due to an acute kidney injury, secondary to small bowel obstruction and sepsis. This in turn was caused by the impacted enterolith.
The patient developed refeeding syndrome but this was managed by combined efforts from critical care and surgical teams alongside specialist input from the dieticians. She improved significantly and was discharged on day 14 of her admission.
Due to the patient’s physiology, this necessitated a shorter operating time, meaning that removal of the diverticulum itself at the time of surgery did not occur. Bearing in mind that formation of a further enterolith is feasible the patient will be followed up based on her symptoms.
Discussion
To this author’s knowledge, this is the largest enterolith ileus exclusively secondary to duodenal diverticulum in a patient with no previous abdominal surgery. The enterolith dimension in this case was considerable at 62×38×32 mm and occurred in the presence of a duodenal diverticulum of similar size. The few cases that were found ranged from 38 mm to 45 mm.10–12 There have been reports of the occurrence of larger enteroliths, a previous case report discussing the finding of an enterolith sized 80×70 mm.13 This manifested in a patient with previous hysterectomy for endometrial cancer and in the presence of an enterocolic fistula.13 Rare cases of recurrent enteroliths have been reported, but in concurrence with a significant intra-abdominal surgical history, such cases describe enteroliths measuring 50×50 mm.14 The majority of these cases all presented with symptoms of bowel obstruction similar to our case.
Prevalence of enteroliths in patients with Meckel’s diverticulum is best documented to date and is estimated at 3%–10%.15 There are cases describing such enteroliths occurring in the presence of a Meckel’s diverticulum. Meckel’s diverticula are infrequent in their occurrence with a prevalence of 2%–4% of the population16; however, they can be considered the most common congenital abnormality of the gastrointestinal system.16 A case documenting the presence of a 4 cm, giant Meckel’s diverticulum and a 40×30 mm enterolith liberated from it, resulting in small bowel obstruction is one such example.17 Our case was due to duodenal diverticulum as opposed to a Meckel’s diverticulum.
Clinical presentation of enterolith ileus is normally that of bowel obstruction and symptoms include abdominal pain, distension and vomiting.3 Symptoms tend to be sudden in onset but can fluctuate. This is accounted for by the enterolith ‘tumbling’ through the bowel lumen.3 Our patient presented similarly but it is worth noting that her progressive vomiting led to dehydration and resulted in a profound acute kidney injury. On CT of the abdomen and pelvis faecalisation of the small bowel was observed suggesting this presentation had been building up over a few days alongside a degree of sepsis. These factors likely contributed to her confusion and via obtaining a collateral history we were able to confirm this was a derangement from her baseline. This case demonstrates the importance of resuscitating a patient adequately as there can be a large amount of volume losses due to vomiting and sepsis.
Risk factors for enterolith ileus are diverse.3 Among most common are intraluminal stricturing or stenosis observed in inflammatory bowel disease, tuberculosis and radiation enteritis,.3 18 19 Surgical anastomoses, intestinal malignancy, extraluminal kinking or angulation found in the setting of intra-abdominal adhesions account for further causes.3 18 19 Our patient did not have any of these factors.
A diagnosis of enterolithiasis was previously made at laparotomy.3 Advances in imaging techniques have enabled us to establish the presence of single or multiple stones, potentiating arrival at a definitive diagnosis.3 In particular, CT scans with contrast enable the provision of two or three-dimensional orientation.3 20 This increases the yield of detection of radiolucent stones and associated pathology, such as anastomotic strictures, fistulas or the presence of diverticula as in our case.3 20 Our patient did fit this category.
A collateral history is a crucial core clinical skill.21 Patients who present with acute confusion are often unable to provide a thorough and comprehensive history.21 This could result in key aspects of the history being inaccurate or omitted entirely, potentially impacting negatively on the management.21 The patient had significant cognitive impairment, and this was initially thought to be chronic when the patient was seen in the emergency department. Subsequent cognitive testing confirmed the deterioration in cognition to be acute. Collateral history was sought, which further confirmed this was a new impairment. This highlights the importance of ascertaining the patient’s baseline, which in turn permitted us to rule out other differentials such as ingestion of a foreign object, as was suggested on the CT scan. Where elderly patients undergoing surgical procedures are concerned, utilisation of cognitive function screening tools in conjunction with reliable collateral is invaluable.22 It has been well documented in the literature that such measures facilitate collaborative efforts among surgeons and physicians in managing the ‘confused patient’.22
Evidence-based clinical decision making requires input from a multidisciplinary group of experts, rather than a ‘consensus of one’.23 Teamwork and care coordination are integrated into the DNA of the surgical MDT.23 High-risk patients are more likely to receive high quality care and less likely to experience complications or require rehospitalisation,.23 This case demonstrated the value of an MDT approach as the patient required multiorgan support in the form of vasopressors and goal-directed fluid therapy. The support of the emergency medicine team in conjunction with ICU was invaluable in optimising the patient prior to surgery, while waiting for emergency theatre availability.
NELA has helped improve the care of patients undergoing a laparotomy in the UK.24 It has highlighted areas which can standardise high quality care.25 The NELA risk prediction tool can help to identify patients that could benefit from preoperative optimisation.25 The patient had an estimated mortality score of 29.7% prior to optimisation and 16.2% thereafter, following 1 day of optimisation. The optimisation had a positive effect on our patient’s outcome and also delayed the surgical intervention to improve her current physiology. The shift towards the use of continuous variables in NELA has allowed for a more sensitive assessment tool to risk stratify patients and therefore facilitate better outcomes for patients.25 Removal of the enterolith is the primary focus in these cases; however, there should be an aim to correct the underlying pathology in an effort to prevent further enterolith recurrence.3 A complicated enterolith ileus could demonstrate signs such as bowel ischaemia, additional unborn enteroliths and potentially signs of a sealed perforation.26 Where there is intestinal obstruction expectant management including serial abdominal examinations, electrolyte correction, appropriate hydration, nasogastric tube suctioning and fluid balance is warranted.3 In our case it was clear that the obstruction would not resolve on its own but optimisation for surgery would make a significant difference to the patient’s outcome. Approaching a rare and relatively complex case such as this with a robust management strategy was essential in ensuring a positive outcome for our patient. This was achieved with the combination of conservative methods prior to surgery itself, while integrating multidisciplinary input throughout the patient’s admission. Ultimately, we attained the optimum outcome as our patient recovered well, with complete resolution of her confusion and was discharged home.
Patient’s perspective.
I found the whole experience to be very daunting. It all seemed to get worse very quickly. The pain I experienced was worse than giving birth—it was almost like having contractions. I was frightened because I didn’t know what was going on. When I went to hospital I didn’t really know what was going on at first, but the doctors were very kind and spoke to my family to help us all understand things without it getting overwhelming. I’m really happy with my care and grateful to the team. Thank you.
Learning points.
Enteroliths due to duodenal diverticula in patients with no surgical history are a rare cause of small bowel obstruction.
The instigation of preoperative optimisation significantly improved the patient’s outcome through a multidisciplinary approach.
Initial management of enterolith ileus should include intravenous fluids, correction of electrolytes, nasogastric aspirate, urinary catheter insertion and fluid balance monitoring.
The use of National Emergency Laparotomy Audit risk prediction scoring can help to identify the patient’s current physiology and measure how effective optimisation will be.
Cognitive screening in the elderly is essential in identifying acute cognitive impairment.
Acknowledgments
The authors would like to thank Dr David Bell - Registrar in radiology for annotating and editing the images. Dr Catherine Key - Consultant in radiology for annotating the images.
Footnotes
Correction notice: This article has been corrected since published online. Figures 1 & 2 are swapped and updated to match the captions and in-text citations.
Contributors: SJA: writing, drafting and proofing. JG: writing, drafting and editing. CJK: editing and article conception. NH: editing and article conception.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
References
- 1.Yadav G, Husain S, Shukla R, et al. A rare case of calcified enterolith presenting as subacute intestinal obstruction. Indian J Surg 2015;77:327–8. 10.1007/s12262-015-1289-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferrari-Light D, Shuchleib A, Ricci-Gorbea J. Bile salt enterolith: an unusual etiology mimicking gallstone ileus. Case Rep Surg 2018;2018:8965930 10.1155/2018/8965930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gurvits GE, Lan G. Enterolithiasis. World J Gastroenterol 2014;20:17819–29. 10.3748/wjg.v20.i47.17819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grettve S. A contribution to the knowledge of primary true concrements in the small bowel. Acta Chir Scand 1947;95:387–410. [PubMed] [Google Scholar]
- 5.Singleton JM. Calcific enterolith obstruction of the intestine. Br J Surg 1970;57:234–6. 10.1002/bjs.1800570322 [DOI] [PubMed] [Google Scholar]
- 6.Athey GN. Unusual demonstration of a Meckel’s diverticulum containing enteroliths. Br J Radiol 1980;53:365–8. 10.1259/0007-1285-53-628-365 [DOI] [PubMed] [Google Scholar]
- 7.Wilson I, Parampalli U, Butler C, et al. Multiple large enteroliths associated with an incisional hernia: a rare case. Ann R Coll Surg Engl 2012;94:e20–2. 10.1308/003588412X13373405385890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shocket E, Simon SA. Small bowel obstruction due to enterolith (bezoar) formed in a duodenal diverticulum: a case report and review of the literature. Am J Gastroenterol 1982;77:621–4. [PubMed] [Google Scholar]
- 9.Kia D, Dragstedt LR. Enterolithiasis associated with side-to-side intestinal anastomosis. Arch Surg 1967;95:898–901. 10.1001/archsurg.1967.01330180046008 [DOI] [PubMed] [Google Scholar]
- 10.Mora-Guzmán I, Muñoz de Nova JL, Rodríguez Sánchez A. An unusual enterolith ileus. Rev Esp Enferm Dig 2017;109:292. [PubMed] [Google Scholar]
- 11.Yang HK, Fondacaro PF. Enterolith ileus: a rare complication of duodenal diverticula. Am J Gastroenterol 1992;87:1846–8. [PubMed] [Google Scholar]
- 12.Kitagawa K, Ishizuka N, Komatsu E, et al. A case of enterolith ileus as a rare complication of duodenal diverticula. Nihon Rinsho Geka Gakkai Zasshi 2008;69:1935–40. 10.3919/jjsa.69.1935 [DOI] [Google Scholar]
- 13.Salelkar RS, Patil RT, Amonkar DP, et al. Enterolith with enterocolic fistula: the diagnostic approach. Saudi J Gastroenterol 2011;17:418–20. 10.4103/1319-3767.87186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shrestha AL, Shrestha P. Recurrent Enterolithiasis small bowel obstruction: a case seldom described. Case Rep Gastrointest Med 2017;2017:4684182 10.1155/2017/4684182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gadhia U, Raju D, Kapoor R. Large enterolith in a Meckels diverticulum causing perforation and bowel obstruction: an interesting case with review of literature. Indian J Surg 2013;75:177–9. 10.1007/s12262-012-0558-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore KL PT. The digestive system. In: Moore KL PT, ed. The developing human: clinically oriented embryology. 5th ed, 1993: 255–7. [Google Scholar]
- 17.Demetriou V, McKean D, Briggs J. Small bowel obstruction secondary to a liberated Meckel’s enterolith. Case Rep Child Meml Hosp Chic 2013;2013:bcr2013008868. 10.1136/bcr-2013-008868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chawla S, Bery K, Indra KJ. Enterolithiasis complicating intestinal tuberculosis. Clin Radiol 1966;17:274–9. 10.1016/S0009-9260(66)80035-1 [DOI] [PubMed] [Google Scholar]
- 19.Bery K, Chawla S, Gupta S. Enteroliths and intestinal tuberculosis. Ind J Radiol Imag 1985;39:225–30. [Google Scholar]
- 20.Singhal B, Kaval S, Kumar P, et al. Enterolithiasis: an unusual cause of small intestinal obstruction. Archives of International Surgery 2013;3:137–41. 10.4103/2278-9596.122936 [DOI] [Google Scholar]
- 21.Fitzpatrick D, Doyle K, Finn G, et al. The collateral history: an overlooked core clinical skill. Eur Geriatr Med 2020;11:1003–7. 10.1007/s41999-020-00367-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.George J, Haboubi H, Skinner P. Perforated Rectal Cancer Presenting as Fournier’s Gangrene in a Confused Older Patient. Reports 2018;1:17. 10.3390/reports1030017 [DOI] [Google Scholar]
- 23.Glance LG, Osler TM, Neuman MD. Redesigning surgical decision making for high-risk patients. N Engl J Med 2014;370:1379–81. 10.1056/NEJMp1315538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murray D. Improving outcomes following emergency laparotomy. Anaesthesia 2014;69:300–5. 10.1111/anae.12620 [DOI] [PubMed] [Google Scholar]
- 25.Eugene N, Oliver CM, Bassett MG, et al. Development and internal validation of a novel risk adjustment model for adult patients undergoing emergency laparotomy surgery: the National emergency laparotomy audit risk model. Br J Anaesth 2018;121:739–48. 10.1016/j.bja.2018.06.026 [DOI] [PubMed] [Google Scholar]
- 26.Steenvoorde P, Schaardenburgh P, Viersma JH. Enterolith ileus as a complication of jejunal diverticulosis: two case reports and a review of the literature. Dig Surg 2003;20:57–60. 10.1159/000068852 [DOI] [PubMed] [Google Scholar]


