Abstract
Introduction
Given the widespread use of clinical reasoning (CR) in the healthcare practice, it is essential to inculcate the CR practice in undergraduate pharmacy education which can not only facilitate their clinical education and clinical rotations but can also help them become better clinical pharmacists. There is very limited CR employed in the pharmacy curriculum and practice in the Middle East countries. This study aimed to develop and evaluate CR practice in pharmacy undergraduates in one college of pharmacy in Saudi Arabia.
Methods
We employed a mixed-methods methodology that included two phases. In Phase I, students were introduced to CR practice (‘think aloud’ method) and given geriatric clinical cases which they used in two sessions together with a tutor. This was followed by the writing of SOAP notes using the tutor feedback and completion of a survey that included a self-reflection about their experience of using the CR method. Phase II included face-to-face semi-structured interviews involving selected students that were recruited via convenience sampling to further explore the issues identified in Phase I of the study.
Results
Of the 155 students who completed the survey (response rate 94%), the majority of them agreed that CR using the ‘think aloud’ method was useful in gathering (92%) and interpreting (95%) relevant patient information, identifying medication-related problems (95%), exploring therapeutic options for the problem(s) (93%) and formulating a treatment plan for the patient (90%). Qualitative data analysis of the 12 interviews was consistent with these findings. Furthermore, it provided an insight into the challenges faced by the students in applying this CR method.
Conclusions
Students found the practice of CR using the ‘think aloud’ method helpful in working through given cases and taking clinical decisions. This method can be widely employed in pharmacy education and practice.
Keywords: Clinical reasoning, Think-aloud, Mixed-methods, Clinical decision-making, SOAP
1. Introduction
Clinical reasoning has been defined as, ‘the set of reasoning strategies that permit us to combine and synthesize diverse data into one or more diagnostic hypotheses, make the complex trade‐offs between the benefits and risks of tests and treatments, and formulate plans for patient management (Kassirer and Kopelman 1991). It is generally based on the individual’s existing knowledge to construct explanations and reach conclusions (Cooper and Frain 2017). Knowledge of basic and clinical sciences provides the foundation for its core elements which include: clinical skills (including communication skills); use and interpretation of patient data; understanding cognitive biases and human factors; critical thinking (metacognition); patient-centered evidence-based medicine and shared decision making (Cooper and Frain 2017). Clinical reasoning can also be defined as ‘the cognitive process involved in arriving at a diagnosis or treatment plan’ (Durning et al., 2013, Pinnock et al., 2015). It is a higher-order thinking in which the healthcare provider, guided by the best evidence or theory, observes and relates concepts and phenomena to develop an understanding of their significance. It is now increasingly becoming a core skill in nursing and medical practice, yet remains a challenging concept to grasp for learners (Hughes 2008).
The term clinical reasoning has been associated with critical thinking and clinical judgment in the literature. Victor-Chmil has outlined the association between these two in the context of nursing practice as (a) analyze collected data (critical thinking), (b) apply reasoning to the data obtained (clinical reasoning), and (c) appropriately act based on the specific situation (clinical judgment) (Victor-Chmil 2013), which can be translated to the competencies required by other healthcare professionals including pharmacy. More precisely, critical thinking is defined as thought with the purpose of interpreting, analyzing, explaining, and evaluating a given idea or situation (Facione 2006). Knowledge, skills, and behaviors that are produced through critical thinking then constitute the concepts of clinical judgment (Barnes 2019). Clinical judgment is the process used by the healthcare professionals to obtain and interpret data about a patient and use this data to determine appropriate actions and interventions to implement (Lasater 2007). Clinical reasoning encompasses both these elements and is the process of applying knowledge to the clinical settings that guides responses and the development of a solution (Banning 2008).
‘Think aloud’ is one method that facilitates clinical reasoning. It is the approach in which the individuals verbalize their thoughts out loud to ease their cognitive process. It may start with random reasoning but helps in organizing the thinking by generating the links between existing knowledge and available data, and can even identify the gaps in knowledge and available data. It is particularly helpful when clinical reasoning is performed by a team of students or by learners together with the teachers or expert clinicians who can identify whether the individual is thinking in the right direction.3 It can not only serve as a method to learn clinical reasoning but also used as a means to assess individuals’ clinical reasoning by teachers or expert clinicians (Pinnock et al. 2016).
The pharmacy profession has evolved significantly worldwide over the last two decades with pharmacists moving from the traditional role of dispensing towards a more patient-oriented role (Ali et al. 2012). The pharmacists are now expected to collaborate with the medical staff regarding medication-related problems as well as developing effective treatment plans. With the changing roles of pharmacists, the need to introduce and practice clinical reasoning in the pharmacy profession is becoming more obvious. Moreover, the Accreditation Council for Pharmacy Education (ACPE) requires this skill to be applied across the pharmacy curriculum (ACPE, 2015). The cognitive ability of pharmacists to recall and synthesize information is a critical aspect of safe and optimal medication use. Given the widespread use of clinical reasoning in the healthcare practice, it is essential to inculcate the clinical reasoning practice in undergraduate pharmacy education which can not only facilitate their clinical education and clinical rotations but can also help them become better clinical pharmacists.
The influence of culture on individuals’ learning cannot be denied as it also affects their critical thinking, clinical reasoning, and/or clinical judgment (Sommers 2018). It is, therefore, imperative to explore clinical reasoning in the cultural context appropriately (Hwang et al., 2010, Shin et al., 2014, Shin et al., 2015, Yu et al., 2013). However, there is very limited conscious clinical reasoning employed in the pharmacy curriculum and practice in the Middle East countries. Likewise, there is limited research regarding the practice and effectiveness of clinical reasoning in the field of pharmacy education and practice in this region. This study aims to develop and evaluate clinical reasoning practice in pharmacy undergraduate students in Saudi Arabia.
2. Methods
2.1. Study design
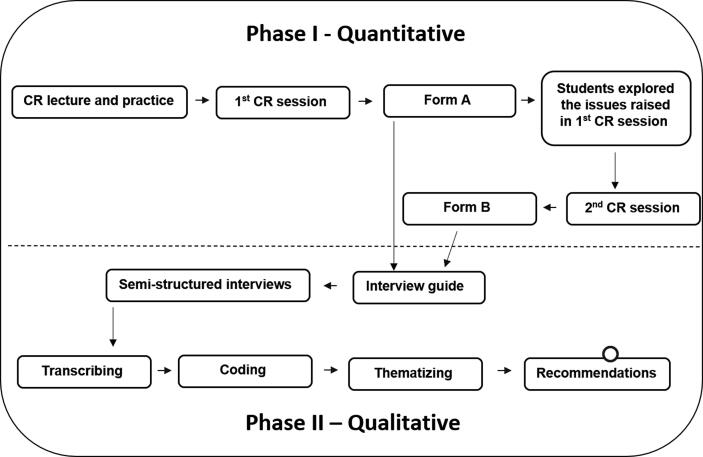
We employed a mixed-methods methodology for this study that comprised of two phases: Phase I used a quantitative survey approach, while, Phase II involved qualitative semi-structured interviews. The quantitative data was analyzed and used to help guide the semi-structured interviews with selected students for triangulation and further exploration of the issues related to the development of clinical reasoning in undergraduate students. Fig. 1 illustrates the study plan and the link between the two phases of the study.
Fig. 1.
The study was conducted in the semester I of the academic year of 2019–2020 (September 2019 through February 2020). This study was reviewed and approved by the Intuitional Review Board (IRB) of Umm Al-Qura University (KSA) (Approval number: HAPO-02-K-012–2020-06–406).
2.2. Sample and setting
The study involved Fifth-year Pharm D students enrolled in the College of Pharmacy, Umm Al-Qura University, Saudi Arabia
2.3. Phase I – Quantitative
2.3.1. Introduction to clinical topics and clinical reasoning
In a Therapeutics course (which encompassed geriatric pharmacotherapy), students of 5th-year PharmD, which is a didactic year before the experiential year in the six-year PharmD program, students were given a 2-hour lecture on two geriatric disease areas (urinary incontinence and erectile dysfunction). Following this, the students were introduced to the concept of clinical reasoning, underpinning theory, and method of clinical reasoning using the ‘think aloud’ approach. A tutor then performed the clinical reasoning using the ‘think aloud’ approach as a practice with the students using two clinical cases related to these disease areas. The students were then given an additional geriatric clinical case for self-directed learning in order to practice clinical reasoning using the ‘think aloud’ method on their own. Furthermore, the students were provided with a written model SOAP (Subjective, Objective, Assessment, Plan) notes related to this additional clinical case to help guide their thought process.
2.3.2. First clinical reasoning session
A week later, in the Therapeutics session, students were given new unseen geriatric cases. They practiced clinical reasoning in small groups on these cases with the tutor. The aim of this session was to identify any clinical issues, and not necessarily answer them. This was due to the limited clinical knowledge and experience of the students at this stage. Students explored the clinical issues in this session with the tutor and made note of all the unanswered questions for further self-directed learning.
2.3.3. Self-study
After the first clinical reasoning session, the students were asked to complete and submit a survey form (Form A) about their experience of using the ‘think aloud’ method for clinical reasoning and feedback on the support provided thus far. The students then had one week to find out the answers to all the unanswered questions on their own and address the clinical issues which were raised in the first session. During this period, drop-in sessions were arranged by the tutor to help students who needed further support.
2.3.4. Second clinical reasoning session
In the second session, the students (in the same groups) were expected to come prepared with answers and resolve any clinical issues which were raised in the first clinical reasoning session. During this session, the students performed the clinical reasoning using the ‘think aloud’ method on the same clinical cases with the tutor. The students were also encouraged to take the lead while performing clinical reasoning while the tutor only facilitated the session. At the end of the session, the students received immediate feedback from the tutor on their performance.
2.3.5. Post-second clinical reasoning session
The students completed SOAP notes on their clinical cases, based on their performance and the tutor feedback from the second session. The students had prior experience of writing SOAP notes in the 4th-year. These SOAP notes were then submitted to the tutor as part of a summative assignment that was graded as per the assessment rubric provided to the students. Besides, the students were also asked to complete another survey form (Form B) with self-reflection about their experience of applying clinical reasoning and the whole process. General feedback on students’ performance during the second session and their SOAP notes was provided by the tutor a week later.
2.3.6. Description of the survey forms
Form A: Students were asked to complete this form after the first clinical reasoning session. This form was comprised of the following sections with most of the questions having a 5-point Likert scale:
-
-
Pre-assignment task: Student knowledge about clinical reasoning using the ‘think aloud’ approach after the introductory lecture on clinical reasoning.
-
-
Knowledge gap: Students were asked whether the clinical reasoning approach helped identify clinical issues during the first session for further exploration.
-
-
General feedback: Students were asked whether the first session was helpful in the application of the concept and the development of their clinical reasoning skills for taking better clinical decisions.
-
-
Self-reflection: Students’ opinions about what they liked or disliked, what they found easy or difficult, and what they learned thus far. Students also commented on how they would approach differently if they had to do this session again and what next steps they would take after this session.
Form B: Students were asked to complete this form after the second clinical reasoning session. This form was comprised of the following sections with most of the questions having a 5-point Likert scale:
-
-
Knowledge gap: Students were asked how they addressed the clinical issues which were raised in the first session, which resources they used, and which issues were still left unanswered.
-
-
Clinical reasoning process: Students were asked whether clinical reasoning is a useful method of gathering and processing patient information, identifying medication-related problems, exploring therapeutic options, and formulating a treatment plan for the patient in a given case; and whether the whole process helped develop their clinical reasoning skills.
-
-
Value of clinical reasoning method: Students were asked how helpful clinical reasoning was in writing a SOAP notes, whether any other method could be better in reaching clinical decisions and whether clinical reasoning skills can make them better pharmacists in the future.
-
-
Self-reflection: Students’ opinions about what they liked or disliked, what they found easy or difficult, and what they learned in the whole process. Students also commented on how they would approach differently if they had to do this again and how they would use clinical reasoning skills in the future.
2.3.7. Data analysis
Descriptive results from Form A and Form B were presented as frequencies and percentages.
2.4. Phase II – Qualitative
2.4.1. Sampling
This phase involved face-to-face semi-structured interviews with the students from the same cohort, recruited on a convenience sampling basis. It was planned to recruit the students and conduct the interviews with subsequent qualitative data analysis until the data saturation was achieved.
2.4.2. Development of interview guide
An interview guide was developed to help the authors to explore students’ views and experiences about the clinical reasoning approach. The interview guide was aimed to explore the challenges that students faced in the whole process, their development of clinical decision-making ability, comparison of clinical reasoning with other methods of learning, future use of clinical reasoning, and suggestions to improve learning about clinical reasoning. The interview guide was developed in the English language and validated by two academics with experience in qualitative research from different universities. This was followed by a forward and backward translation of the interview guide to the Arabic language by two bilingual staff members. The interview guide was then piloted with a small number of students (n = 2). No changes in the interview guide were required after piloting.
2.4.3. Interviews
Two authors (research students) (FA and ZM) had a briefing session with the research supervisor (MA) regarding how to conduct face-to-face semi-structured interviews followed by a practice interview with the research supervisor by them separately. Both interviewers were provided with appropriate feedback by the research supervisor followed by discussion/reflection until the research supervisor was satisfied with their interviewing skills. The interviewers then conducted the interviews with the recruited students in the Arabic language since it is the first language of our students and we expected that they can more conveniently express themselves in the Arabic language. Students who agreed to be interviewed were also asked to sign a consent form before being interviewed. All interviews were audio-recorded and transcribed verbatim later. The accuracy of the transcriptions was checked alternatively by the authors.
2.4.4. Data analysis
We employed an inductive approach of thematic analysis to analyze the qualitative data from the interviews. The analysis started with familiarizing the data through reading the transcripts, followed by the generation of initial codes from the data independently by two teams of researchers. The codes generated by the two teams were further verified by the research supervisor. Any discrepancies in the coding process were resolved through discussion. These codes were then categorized into broad themes independently by the same two teams of researchers and then verified again by the research supervisor. A few themes were excluded due to the limited codes related to them. Any further discrepancies, at this stage, were again resolved through discussion. The final themes were then defined and renamed by the authors.
3. Results
3.1. Phase I – Quantitative results from Form a and Form B
For the convenience of data interpretation and presentation, we condensed the responses of a 5-point Likert scale by combining the response numbers of ‘Strongly agree’ and ‘Agree’ into one category, ‘Agree’. Similarly, we combined the response numbers of ‘Strongly disagree’ and ‘Disagree’ into one category, ‘Disagree’. Out of 165 students in the cohort, 157 students (response rate 95%) completed Form A. Responses are presented in Table 1. Overall, the majority of the students agreed that the support provided for elaborating the concept of clinical reasoning with the example cases was useful and helped in writing SOAP notes. Notably, at this stage of the process, 86% of the respondents agreed that the ‘think aloud’ method of clinical reasoning helped identify the issues they needed to explore or find out the answers for after the first clinical reasoning session and 90% believed that this method of clinical reasoning can help them take better clinical decisions as pharmacists in the future.
Table 1.
Number (Percentage) of Responses for Each Item in Form A (n = 157).
| Item | Agree (%) | Neutral (%) | Disagree (%) |
|---|---|---|---|
| I found the clinical reasoning lecture useful to understand what clinical reasoning is. | 135 (86%) | 19 (12%) | 3 (2%) |
| I found the clinical reasoning lecture (& examples in it) useful to apply clinical reasoning using the ‘think aloud method. | 136 (86%) | 20 (13%) | 1 (1%) |
| The practical case given was helpful for practicing clinical reasoning using the ‘think aloud method. | 141 (90%) | 13 (8%) | 3 (2%) |
| The practical case given was helpful for practicing the SOAP note. | 128 (81%) | 25 (16%) | 4 (3%) |
| ‘Think aloud’ method of clinical reasoning was helpful in identifying the issue/points which I need to explore or find out after the session. | 135 (86%) | 18 (11%) | 4 (3%) |
| Overall, the above process, so far, was helpful in understanding the concept of clinical reasoning. | 132 (84%) | 24 (15%) | 1 (1%) |
| Overall, the above process, so far, was helpful in developing my clinical reasoning skill. | 141 (90%) | 15 (9%) | 1 (1%) |
| The method of clinical reasoning can help me take better clinical decisions in the future as a pharmacist. | 141 (90%) | 15 (9%) | 1 (1%) |
Of the 165 students in the class, 155 students (response rate 94%) completed Form B. Responses are presented in Table 2. The majority of the respondents agreed that this method of clinical reasoning was useful in gathering relevant patient information, processing/interpreting the patient information, identifying the medication-related problem(s), exploring therapeutic options for the identified problem(s), and formulating a treatment plan for the patient. A list of the resources used by the respondents for exploring the issues and finding out the answers for unanswered questions was developed (not presented in this manuscript). The majority of the respondents mentioned that no issues were left unaddressed or unanswered after the second session. At this stage of the process, 94% of the respondents agreed that the whole process was helpful in developing their clinical reasoning skills and 65% agreed that they learned more from this method, in comparison with other learning and assessment methods (such as presentations). Similar to the results of Form A, 90% believed that this method of clinical reasoning can help them take better clinical decisions as a pharmacist in the future.
Table 2.
Number (Percentage) of Responses for Each Item in Form B (n = 155).
| Item | Agree (%) | Neutral (%) | Disagree (%) |
|---|---|---|---|
| I/we managed to find out answers for all issues/points/questions from the 1st clinical reasoning session. | 132 (85%) | 20 (13%) | 3 (2%) |
| I found the method of clinical reasoning useful in gathering relevant patient information. | 143 (92%) | 12 (8%) | 0 (0%) |
| I found the method of clinical reasoning useful in processing/interpreting the patient information. | 147 (95%) | 8 (5%) | 0 (0%) |
| I found the method of clinical reasoning useful in identifying the medication-related problem(s). | 147 (95%) | 7 (4%) | 1 (1%) |
| I found the method of clinical reasoning useful in exploring therapeutic options for the identified problem(s). | 144 (93%) | 11 (7%) | 0 (0%) |
| I found the method of clinical reasoning useful in formulating a treatment plan for the patient. | 139 (90%) | 13 (8%) | 3 (2%) |
| Overall, the process was helpful in developing my clinical reasoning skill. | 146 (94%) | 8 (5%) | 1 (1%) |
| As compared to this clinical reasoning method, I would have learned more with any other method of assignment e.g. written case study, case study presentation, topic presentation, etc. | 14 (9%) | 41 (26%) | 100 (65%) |
| The method of clinical reasoning can help me take better clinical decisions in the future as a pharmacist. | 139 (90%) | 14 (9%) | 2 (1%) |
As for the self-refection by the respondents in Form A and Form B, we attempted to categorize them into positive, suggestions, and negative. Their numbers are presented in Table 3 whereas the detailed reflections are not presented in this manuscript. However, based on these reflections, recommendations have been developed for the curriculum committee and academic staff in our college to restructure the learning and assessment methods and roll this approach out to other years of study.
Table 3.
Number of Categories of Self-reflections by the Respondents.
| Form | Positive | Suggestions | Negative |
|---|---|---|---|
| Form A | 54 | 5 | 9 |
| Form B | 56 | 9 | 7 |
3.2. Phase II – Thematic analysis of semi-structured interviews
Twelve interviews were conducted with the students recruited on a convenience sampling basis, with the aim of conducting more interviews should the data saturation was not achieved. However, following the thematic analysis of the 12 interviews (six male and six female students), the authors believed that the data saturation was achieved, and no further interviews were required. The average duration of the interviews was 15 min (range: 10–23 min). The thematic analysis generated 210 codes which were categorized into seven overarching themes as shown in Table 4 with specific student comments supporting each of the themes.
Table 4.
Themes with Number of Associated Codes and Student Quotes Supporting the Themes.
| Theme 1 – Participants’ background knowledge about clinical reasoning (codes: 21) |
|---|
|
| Theme 2 – Use of 'think aloud' method for clinical reasoning (codes: 25) |
|
| Theme 3 – Application of clinical reasoning (codes: 17) |
|
| Theme 4 – Challenges of applying clinical reasoning (codes: 6) |
|
| Theme 5 – Advantages of clinical reasoning (codes: 95) |
|
| Theme 6 – Clinical reasoning versus other learning and assessment methods (codes: 12) |
|
| Theme 7 – Suggestions for future use of clinical reasoning (codes: 29) |
|
CR: Clinical reasoning
3.2.1. Theme 1 – Participants’ background knowledge about clinical reasoning
This theme is related to the basic information regarding clinical reasoning which the participants had before the first session. The participants mentioned clinical reasoning definitions, their perceptions, or previous clinical reasoning experiences. The majority of the participants did not know what the clinical reasoning was before the first session or even before the course. Others, though failed to provide the correct definition of clinical reasoning, had heard about clinical reasoning before and were able to provide some information about the clinical reasoning process.
3.2.2. Theme 2 – Use of 'think aloud' method for clinical reasoning
A wide range of opinions was obtained from the participants regarding the use of the ‘think aloud’ method in the process of clinical reasoning. The majority of the participants found this method useful to “connect the thoughts together”, “organize the priorities”, and “make yourself think more”. Some participants also commented on performing clinical reasoning in a group as compared to performing it alone and found the former a helpful means of knowledge sharing. One participant envisaged the method with a broader perspective of personal development.
3.2.3. Theme 3 – Application of clinical reasoning
The participants identified how to maximize the use and benefit of clinical reasoning by applying it to different fields of healthcare. They also mentioned that the clinical reasoning process will benefit them even more in their internship year (APPE) and on the job as a pharmacist when they would have the opportunity of discussing real-life cases. Some participants recognized that clinical reasoning makes the writing of SOAP notes much easier. However, the majority of the participants were of the opinion that clinical reasoning is a skill that can be developed and further improved by practice.
3.2.4. Theme 4 – Challenges of applying clinical reasoning
The participants highlighted several difficulties and the challenges that they faced while performing clinical reasoning. Some participants did not face any difficulties while performing clinical reasoning except that they found it time-consuming. One participant commented on the challenge of performing clinical reasoning in a group based on his/her experience of working in a “non-cooperative” team. The majority of the participants recognized that “the struggle is in the beginning” when they “do not know what to do”. Some participants recognized that one of the main challenges is not having sufficient clinical information.
3.2.5. Theme 5 – Advantages of clinical reasoning
All the participants acknowledged that clinical reasoning helps in working through the given clinical cases. The participants highlighted several advantages of clinical reasoning. One participant recognized the holistic approach that clinical reasoning offers in viewing the case, “the most beneficial thing in CR is taking different opinions from different sides” and “CR helps to see the bigger picture”. Some participants mentioned that the main advantage of clinical reasoning is that it helps in “gathering relevant information” which then leads to the identification of the alternative approaches to the clinical problem and exclude “irrelevant options”. Several participants found it extremely helpful in “deprescribing harmful” or “deprescribing unnecessary drugs” and reach “appropriate therapeutic plan” for the patient. Some participants viewed the benefits of clinical reasoning in writing SOAP notes. A few participants envisaged the long-term benefits of clinical reasoning, “clinical reasoning improves the self-confidence” and “increases communication skills”.
3.2.6. Theme 6 – Clinical reasoning versus other learning and assessment methods
The participants described clinical reasoning in comparison with other methods of learning and assessment. All the participants were of the view that clinical reasoning is “better than the other learning and assessment methods”. Some of them compared it with oral presentations, “even presentation come after it” and “more important than presentations”. The participants also described the clinical reasoning as an important element in the curriculum to support their educational journey. Some participants found “clinical reasoning more organized and engaging when compared to other methods of assessment”. One participant reflected on how clinical reasoning is different from other methods of learning and assessment, “the presentations only provide ideas from you, but with clinical reasoning … it creates a discussion that produces other perspectives”. One participant, however, commented that “CR cannot be compared with other assessments as it is different”.
3.2.7. Theme 7 – Suggestions for future use of clinical reasoning
We received several suggestions and views from the participants regarding how the benefits of the clinical reasoning process can be leveraged as well as improving the process for the future use. The majority of the participants opinionated that clinical reasoning must be used in the earlier years of the pharmacy degree program. One participant suggested to include clinical reasoning in OSCE stations. The majority of the participants would also like to “practice CR more frequently”.
4. Discussion
Widespread successful application of clinical reasoning in healthcare education programs such as medicine and nursing spurred us on to exploring its application in pharmacy education as the reasoning process differs among various healthcare professions (Banning, 2008, Page et al., 2016). The students who are exposed to this method of approach towards the clinical problems during their education and should they find it helpful are inclined to continue clinical reasoning in their professional practice. Furthermore, we know that applying clinical reasoning by practicing pharmacists leads to correct and appropriate clinical decisions (Croft et al. 2017). Although the ACPE standards recognize the importance of the development of clinical reasoning in pharmacy students (ACPE, 2015), the pharmacy curriculum, especially in the Middle East countries does not include the development and evaluation of this skill. This may be attributed to the fact that it is currently not the requirement for colleges of pharmacy in this region to be accredited by ACPE or any other local accreditation body. In this study, we attempted to introduce clinical reasoning and its application in approaching clinical problems using the ‘think aloud’ method as this is one of the most convenient models to apply clinical reasoning to novice learners developing this skill (Weitzel et al. 2012). We evaluated its value through the student feedback survey and then conducted face-to-face semi-structured interviews for triangulation and in-depth exploration of some of the issues raised in the feedback survey (Graham 2005; Turner et al., 2017).
Abuzour and colleagues conducted a qualitative study to explore the process and influences of clinical reasoning using the ‘think aloud’ method in secondary care pharmacists and nurses in the UK. They concluded that clinical reasoning is a very complex and dynamic process and suggested that healthcare professionals develop these skills to provide better patient care (Abuzour et al., 2018). Our students opinionated that developing this skill will help them make better clinical decisions in the future. Atayee and colleagues evaluated clinical reasoning in palliative care among pharmacy students and concluded that it increased the students’ confidence in palliative care competencies. This can be extrapolated to the application of clinical reasoning in the development of other competencies in pharmacy students (Atayee et al. 2018).
The role of the tutor or preceptor in developing or guiding clinical reasoning in the students is crucial (Sylvia, 2019, Weitzel et al., 2012). We ensured that the two tutors involved in clinical reasoning sessions with the students had an adequate clinical experience and held several meetings at the start of the semester to ensure consistent execution of these sessions. This contributed to the encouraging feedback received from the students regarding the overall process.
Tietze has described the development and implementation of a structured clinical reasoning course for pharmacy students to guide pharmacy students through the clinical reasoning processes for making patient-specific therapeutic recommendations and integrating standard SOAP writing (Tietze 2018). Our study reiterates this facilitation of SOAP writing using the clinical reasoning process as students recognized that clinical reasoning makes the writing of SOAP notes much easier. Similarly, Nolt and colleagues also described the design and delivery of a similar course and concluded that clinical reasoning can help students evolve their learning strategies and better engage them in the learning process (Nolt et al. 2018). Our students iterated this notion by reflecting that clinical reasoning is more organized and engaging when compared to other learning and assessment methods.
A multifaceted approach is required to teach and assess clinical reasoning (Daniel et al., 2019, Gonzalez, 2018). Since there is limited evidence that short courses alone improve clinical reasoning Daniel et al. 2019, we recommend that clinical reasoning should be integrated within the entire curriculum with a variety of other active learning activities such as problem-based learning. Linn and colleagues suggested that clinical reasoning is best taught as a skill and should be included in the skill-teaching framework (Linn et al. 2012). Moreover, our students also reflected in their responses that their limited knowledge and experience was one of the hindrances in executing clinical reasoning effectively. To address this issue, Linn and colleagues suggested that the novice learners such as students should approach clinical problems using clinical reasoning in a more structured way (Croskerry, 2009, Harasym et al., 2008, Yazdani et al., 2017). This also necessitates the change in the way clinical reasoning is developed in the students. A comprehensive model proposed by Curter and colleagues that encompasses knowledge development, data gathering, data processing and metacognition, can be adopted (Cutrer et al., 2013). We also recommend that clinical reasoning should be introduced to the students in the early years of their pharmacy education as it is a gradual developmental process over time. This was mentioned by the majority of our students and had also been recommended by Furze and colleagues who explored students’ clinical reasoning development in physical education therapy (Furze et al. 2015).
The approach to clinical reasoning is influenced by culture (Lee et al. 2021). The above discussion of our findings provides an insight into the clinical reasoning practice by Saudi students and their perceptions regarding it. Unlike the Western students (Findyartini et al. 2016), our students were found to be tutor-dependent rather than independent thinkers. Our observations regarding employing clinical reasoning with these students revealed that they approach the case scenarios with the aim of checking the accuracies in medicines management based on the medicines information resources only. The students were prompted to think critically that every patient is different and therefore, medicines managenment is required to be optimized according to the patient in the given clinical scenario with reasoning. Moreover, the students' approach to developing pharmaceutical care plans was not holistic and the students had to be prompted by the tutors to think beyond the medicines management while developing pharmaceutical care plans.
Reflection through a debriefing with the tutor or preceptor after a clinical reasoning session has proved to be very useful which allows the students to identify their strengths and areas for improvement as well the gaps in their knowledge (Vyas et al. 2011). One of the limitations of our study is that we could not have a debriefing session after the clinical reasoning sessions due to time constraints with the tutors. However, our students were allowed to provide structured reflection through FORM A and FORM B which we included in the analysis. Moreover, this was a single-institute study conducted with one cohort and, therefore, this may compromise the generalizability of the findings.
5. Conclusion
Students found the practice of clinical reasoning using the ‘think aloud’ method very helpful in working through given cases and taking clinical decisions. The majority of them mentioned that they learned more from it than any other teaching and assessment method and suggested that this should be employed from the early years in the pharmacy curriculum. This method can be feasibly and widely employed in pharmacy education and practice. Further studies should explore how the students propagate the clinical reasoning developed during their pharmacy education program to their professional practice.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not for-profit sectors.
Authors’ contributions
MA conceived and designed the study. All authors (except EC and ID) were involved in data collection, analysis, and interpretation. EC and ID supervised the project. All authors contributed to the drafting and critical review of the manuscript and have approved the final draft of the manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank all the students who participated in this research project.
Footnotes
Peer review under responsibility of King Saud University.
References
- Abuzour A.S., Lewis P.J., Tully M.P. A qualitative study exploring how pharmacist and nurse independent prescribers make clinical decisions. J Adv Nurs. 2018;74(1):65–74. doi: 10.1111/jan.13375. [DOI] [PubMed] [Google Scholar]
- Accreditation Council for Pharmacy Education (ACPE). 2015. Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree (Standards 2016). Acpe-accredit.org. [accessed 9 March 2021]. https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf.
- Ali, M., Schifano, F., Robinson, P., et al. Impact of community pharmacy diabetes monitoring and education programme on diabetes management: a randomized controlled study. Diabet Med. 29:e326-e333. https://doi.org/10.1111/j.1464-5491.2012.03725.x. [DOI] [PubMed]
- Atayee, R., Lockman, K., Brock, C., et al. 2018. Multicentered study evaluating pharmacy students’ perception of palliative care and clinical reasoning using script concordance testing. Am J Hosp Palliat Med. 35:1394-1401. https://doi.org/10.1177/1049909118772845. [DOI] [PubMed]
- Barnes, R. 2019. Toward enhancement of clinical judgment and critical thinking: simulation in the classroom. PhD dissertation (Indiana State University). [accessd 15 August 2020]. https://search.proquest.com/openview/7a4d04405751b2ec761c3c90d984e716/1?pq-origsite=gscholar&cbl=51922&diss=y.
- Banning, M. 2008. The think aloud approach as an educational tool to develop and assess clinical reasoning in undergraduate students. Nurse Educ Today. 28:8-14. https://doi.org/10.1016/j.nedt.2007.02.001. [DOI] [PubMed]
- Cooper N., Frain J. Wiley Blackwell; West Sussex, UK: 2017. ABC of Clinical Reasoning. [Google Scholar]
- Croft H., Gilligan C., Rasiah R., Levett-Jones T., Schneider J. Thinking in pharmacy practice: a study of community pharmacists’ clinical reasoning in medication supply using the think-aloud method. Pharmacy. 2017;6:1–14. doi: 10.3390/pharmacy6010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croskerry P. A universal model of diagnostic reasoning. Acad Med. 2009;84(8):1022–1028. doi: 10.1097/ACM.0b013e3181ace703. [DOI] [PubMed] [Google Scholar]
- Cutrer W.B., Sullivan W.M., Fleming A.E. Educational strategies for improving clinical reasoning. Curr Probl Pediatr Adolesc Health Care. 2013;43(9):248–257. doi: 10.1016/j.cppeds.2013.07.005. [DOI] [PubMed] [Google Scholar]
- Daniel M., Rencic J., Durning S.J., Holmboe E., Santen S.A., Lang V., Ratcliffe T., Gordon D., Heist B., Lubarsky S., Estrada C.A., Ballard T., Artino A.R., Sergio Da Silva A., Cleary T., Stojan J., Gruppen L.D. Clinical reasoning assessment methods. Acad Med. 2019;94(6):902–912. doi: 10.1097/ACM.0000000000002618. [DOI] [PubMed] [Google Scholar]
- Durning S.J., Artino A.R., Schuwirth L., van der Vleuten C. Clarifying assumptions to enhance our understanding and assessment of clinical reasoning. Acad Med. 2013;88(4):442–448. doi: 10.1097/ACM.0b013e3182851b5b. [DOI] [PubMed] [Google Scholar]
- Facione, P. 2006. Critical Thinking: what it is and why it counts. Insight assessment. [accessd 2 August 2020]. http://faculty.uml.edu/robert_gamache/85.503/Facione2006CriticalThinking.pdf.
- Findyartini A., Hawthorne L., McColl G., Chiavaroli N. How clinical reasoning is taught and learned: Cultural perspectives from the University of Melbourne and Universitas Indonesia. BMC Med Educ. 2016;16:185. doi: 10.1186/s12909-016-0709-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furze J., Black L., Hoffman J., Barr J.B., Cochran T.M., Jensen G.M. Exploration of students’ clinical reasoning development in professional physical therapy education. J Phys Ther Educ. 2015;29(3):22–33. doi: 10.1097/00001416-201529030-00005. [DOI] [Google Scholar]
- Gonzalez L. Teaching clinical reasoning piece by piece: a clinical reasoning concept-based learning method. J Nurs Educ. 2018;57(12):727–735. doi: 10.3928/01484834-20181119-05. [DOI] [PubMed] [Google Scholar]
- Graham R.W. Illustrating triangulation in mixed-methods nursing research. Nurse Res. 2005;12(4):7–18. doi: 10.7748/nr2005.04.12.4.7.c5955. [DOI] [PubMed] [Google Scholar]
- Harasym P.H., Tsai T.-C., Hemmati P. Current trends in developing medical students' critical thinking abilities. Kaohsiung J Med Sci. 2008;24(7):341–355. doi: 10.1016/S1607-551X(08)70131-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes R. Agency for Healthcare Research and Quality; Rockville, MD: 2008. Patient Safety And Quality. [Google Scholar]
- Hwang S., Yen M., Lee B., Huang M., Tseng H. A critical thinking disposition scale for nurses: short form. J Clin Nurs. 2010;19:3171–3176. doi: 10.1111/j.1365-2702.2010.03343.x. [DOI] [PubMed] [Google Scholar]
- Kassirer J., Kopelman R. 1st ed. Williams & Wilkins; Baltimore, MD: 1991. Learning Clinical Reasoning. [Google Scholar]
- Lasater K. Clinical judgment development: using simulation to create an assessment rubric. J Nurs Educ. 2007;46:496–503. doi: 10.3928/01484834-20071101-04. [DOI] [PubMed] [Google Scholar]
- Lee, C.Y., Jenq, C.C., Chandratilake, M., et al. 2021. A scoping review of clinical reasoning research with Asian healthcare professionals. Adv in Health Sci Educ. [Published online]. https://doi.org/10.1007/s10459-021-10060-z. [DOI] [PMC free article] [PubMed]
- Linn, A., Khaw, C., Kildea, H., Tonkin, A. 2012. Clinical reasoning: A guide to improving teaching and practice. Aust Fam Physician. 41:18-20. [PubMed]
- Nolt V., Cain J., Wermeling D. Design and delivery of a new clinical reasoning course. Curr Pharm Teach Learn. 2018;10(8):1113–1123. doi: 10.1016/j.cptl.2018.05.012. [DOI] [PubMed] [Google Scholar]
- Page, G., Matthan, J., Silva, A., McLaughlin, D. 2016. Mapping the delivery of ‘Clinical Reasoning’ in UK undergraduate medical curricula. Unpublished. https://doi.org/10.13140/RG.2.2.19976.93444.
- Pinnock R., Fisher T.-L., Astley J. Think aloud to learn and assess clinical reasoning. Med Educ. 2016;50(5):585–586. doi: 10.1111/medu.2016.50.issue-510.1111/medu.13006. [DOI] [PubMed] [Google Scholar]
- Pinnock R., Young L., Spence F., Henning M., Hazell W. Can think aloud be used to teach and assess clinical reasoning in graduate medical education? J Grad Med Educ. 2015;7:334–337. doi: 10.4300/jgme-d-14-00601.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin H., Gi Park C., Shim K. The korean version of the lasater clinical judgment rubric: a validation study. Nurse Educ Today. 2015;35(1):68–72. doi: 10.1016/j.nedt.2014.06.009. [DOI] [PubMed] [Google Scholar]
- Shin H., Shim K., Lee Y., Quinn L. Validation of a new assessment tool for a pediatric nursing simulation module. J Nurs Educ. 2014;53(11):623–629. doi: 10.3928/01484834-20141023-04. [DOI] [PubMed] [Google Scholar]
- Sommers C. Measurement of critical thinking, clinical reasoning, and clinical judgment in culturally diverse nursing students – A literature review. Nurse Educ Pract. 2018;30:91–100. doi: 10.1016/j.nepr.2018.04.002. [DOI] [PubMed] [Google Scholar]
- Sylvia L. A lesson in clinical reasoning for the pharmacy preceptor. Am J Health Syst Pharm. 2019;76:944–951. doi: 10.1093/ajhp/zxz083. [DOI] [PubMed] [Google Scholar]
- Tietze K.J. Clinical reasoning model for pharmacy students. Clin Teach. 2018;16(3):253–257. doi: 10.1111/tct.2019.16.issue-310.1111/tct.12944. [DOI] [PubMed] [Google Scholar]
- Turner S.F., Cardinal L.B., Burton R.M. Research design for mixed methods. Organ Res Methods. 2017;20(2):243–267. doi: 10.1177/1094428115610808. [DOI] [Google Scholar]
- Victor-Chmil J. Critical thinking versus clinical reasoning versus clinical judgment. Nurse Educ. 2013;38:34–36. doi: 10.1097/nne.0b013e318276dfbe. [DOI] [PubMed] [Google Scholar]
- Vyas D., Ottis E.J., Caligiuri F.J. Teaching clinical reasoning and problem-solving skills using human patient simulation. Am J Pharm Educ. 2011;75(9):189. doi: 10.5688/ajpe759189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzel K., Walters E., Taylor J. Teaching clinical problem solving: A preceptor’s guide. Am J Health Syst Pharm. 2012;69:1588–1599. doi: 10.2146/ajhp110521. [DOI] [PubMed] [Google Scholar]
- Yazdani S., Hoseinzadeh M., Hosseini F. Models of clinical reasoning with a focus on general practice: a critical review. J Adv Med Educ Prof. 2017;5:177–184. [PMC free article] [PubMed] [Google Scholar]
- Yu D., Zhang Y., Xu Y., Wu J., Wang C. Improvement in critical thinking dispositions of undergraduate nursing students through problem-based learning: a crossover-experimental study. J Nurs Educ. 2013;52:574–581. doi: 10.3928/01484834-20130. [DOI] [PubMed] [Google Scholar]