Abstract
Purpose:
Developmental models link sexual well-being to physical, mental/emotional, and social well-being, yet little empirical literature evaluates these relationships in adolescents. Better understanding of how and when sexuality complements other aspects of health may yield important points to enhance existing health education and prevention efforts.
Methods:
Data were drawn from a 10-year longitudinal cohort study of sexual relationships and sexual behavior among adolescent women (N = 387; 14–17 years at enrollment). Sexual health data were drawn from quarterly partner-specific interviews and were linked to physical, mental/emotional, and social health information in annual questionnaires. Random intercept, mixed effects linear, ordinal logistic, or binary logistic regression were used to estimate the influence of sexual health on health and well-being outcomes (Stata, v.23, StataCorp, College Station, TX). All models controlled for participant age and race/ethnicity.
Results:
Higher sexual health was significantly associated with less frequent nicotine and substance use, lower self-reported depression, lower thrill seeking, higher self-esteem, having fewer friends who use substances, higher religiosity, better social integration, lower frequency of delinquent behavior and crime, and more frequent community group membership. Sexual health was not associated with the number of friends who used cigarettes.
Conclusions:
Positive sexually related experiences in romantic relationships during adolescence may complement physical, mental/emotional, and social health. Addressing specific aspects of healthy sexual development during clinical encounters could dually help primary prevention and health education address other common adolescent health issues.
Keywords: Adolescent, Sexual health, Substance use, Self-esteem, Depression, Crime, Education
As articulated by several national and international health governing bodies, sexual health broadly encompasses the multiple factors that contribute to an individual’s sexual well-being throughout their lifetime [1,2]. Among young people, rather than stressing the potential adverse outcomes associated with sexuality (e.g., unintended pregnancy or sexually transmitted infection), the sexual health perspective emphasizes the positive developmental contributions that sexuality provides to adolescent well-being within the context of emerging romantic relationships [3]. Participation in several different dating partnerships is normative during the teenage years [4]. Experiences in these relationships can help adolescents hone the array positive skills—such as emotional self-regulation, interpersonal communication, and negotiation—that they will need to manage healthy relationships in adulthood [5-8].
The centrality of sexuality and relationships during the adolescent years could mean they also play a critical role in the development of young people’s physical, mental/emotional, and social health [3,9-11]. The correlation of sexuality with overall health and well-being is well documented among adults but is less delineated among adolescents. For example, among midage and older age adults, frequency of partnered sex, sexual, and relational satisfaction correlates with better overall self-reported physical and psychological health [12,13]. Such findings are echoed in emerging adults, among whom sexual enjoyment and sexual satisfaction are linked to higher quality daily interpersonal interactions, increased autonomy, and improved empathy [14,15]. Similar work in adolescents, however, is mixed—some studies suggest that sexuality, sexual experience, and relationships are associated with both higher and lower levels of health and well-being, while other studies show no relationship [16-18].
One explanation for this conflicting set of findings among adolescents is that most studies only examine the impact of one or two single sexual health indicators rather than a full set of healthy sexual development measures, as predictors of health. Three widely cited sexual health definitions, as well as our own empirical research, support using a multidimensional approach to assessing sexual health in adolescents and linking this measure to different nonsexual health and well-being outcomes. For example, The World Health Organization defines sexual health as “…a state of physical, emotional, mental and social well-being related to sexuality,” [1] and the National Consensus on Adolescent Sexual Health additionally emphasizes that for adolescents these dimensions are closely linked with “sexual development and reproductive health, as well interpersonal relationships…” [19] These statement affirm that adolescent sexual health arises from four dimensions of sexual well-being—emotional, attitudinal, physical, and social—that also represent key relationship-based experiences adolescents use to learn how to manage sexuality in adulthood. Our empirical studies on sexual health have operationalized these definitions [20-22], demonstrating that these four dimensions work collectively as a single measure, with this measure predicting fewer partners, more frequent condom use, lower sexually transmitted infection (STI), and less frequent sexual coercion [20-22]. We utilize a similar measurement approach to sexual health in the current article.
Finally, a third definition offered by a former Surgeon General of the United States endorses the close integration of positive aspects of sexuality with well-being, emphasizing that “…sexual health…is connected with both physical and mental health, and…is important throughout the entire lifespan, not just the reproductive years.” [8] While certainly important at every age, drawing from positive youth development and prevention science perspectives, we argue that sexual health may be particularly associated with health and well-being during adolescence. The primacy of learning and skill development in the context of romantic relationships and sexuality could mean that emerging sexual health dimensions are the same competencies young women need to support positive health behaviors and to protect themselves from a variety of health-related risks [23,24]. For example, the self-efficacy young women use to negotiate condom use and to refuse unwanted sex may also help them resist peer pressure for tobacco, alcohol and drug use [25], or for engaging in delinquent behaviors [26]. Likewise, a relationship characterized by intimacy and trust may foster better overall happiness and self-esteem [27]. Finally, the ability to balance or reconcile intense emotions is linked to lower levels of depression and thrill seeking [28], perhaps indicating ongoing experiences with partners would elicit a similar effect. No work, however, has linked a multidimensional model of sexual health to indicators of health and well-being.
In order to be useful from clinical, developmental, and public health perspectives, scientific efforts to understand the association between sexual health and health and well-being must both operationalize sexual health dimensions using a range of measures related to healthy sexual development and link the totality of these dimensions to a range of health-related outcomes. Accordingly, building on existing studies generally linking one or two single sexuality-related measures to health and on our own sexual health research [20-22], the objective of the current article was to understand the ability of a multidimensional construct of sexual health to predict physical, mental/emotional, and social health outcomes among adolescent women [20-22].
Methods
Larger study design and participants
Data were collected as part of a larger longitudinal cohort study of sexual relationships, sexual behaviors, and STIs among young women in middle-to-late adolescence (1999–2009) [29]. Participants (n = 38) were adolescent women receiving health care as part of the patient population in one of three primary care adolescent health clinics in Indianapolis, Indiana. These clinics serve primarily lower- and middle-income families residing in areas with high rates of early childbearing and STI. The average maternal education level was 12th grade. Eligibility included being 14–17 years of age, English speaking, and not being pregnant. Neither sexual experience nor sexual orientation was entry criterion in either study. Recruitment strategies remained the same during the duration of the study.
At quarterly intervals, participants contributed quantitative individual- and partner-specific interview data on sexual history, sexual attitudes, sexual behavior, and contraception. In each interview, participants could provide information on up to five “partners”—identified by initials or first name—including friends, dating partners, boyfriends, and sexual partners. While most studies define “partner” in the context of previous coital contact, the definition was broadened to include “personal relationships associated with close physical contact (like having sex, kissing, or holding hands) or spending time together.” Such a focus permits understanding of how ongoing relationship-related dynamics impact health and well-being for young women, independent of the relatively static status labels (e.g., “main” or “casual”) that may be associated with these relationships. Thus, relationships in this study could either include or exclude different types of sexual contact between a participant and her named partner, and this activity could change by the next interview. However, because the sexual health perspective is anchored in understanding the factors that precede sexual decision making [1,2], the presence or absence of sexual activity per se in a given relationship is not the primary focus of this article. In the larger study, participants contributed a total of 5,151 quarterly interviews; the median number of interviews completed per participant was 15 (range 1–47), while the median number completed per partner was four (range: 1–27). The number of completed interviews did not differ by participant baseline age (p = .229), number of lifetime sexual partners (p = .282), race/ethnicity (p = .778), STI status (p = .979), or coital (vaginal or anal sex: p = .266–.923) and noncoital (manual or oral genital: p = .140–.667) experience. All sexual health items were drawn from these interviews.
In addition to the quarterly interviews, participants provided annual questionnaires about their academic, social experiences, family/peer interactions, general mental health, and health-related activities (e.g., substance use). No partner information was assessed in the annual information. In the larger study, a total of 6,130 (range: 1–9) questionnaires were completed. All participants contributed at least one enrollment questionnaire, and the majority (70.6%: n = 272) completed four consecutive questionnaires (enrollment through year four). The number of completed questionnaires did not differ by participant baseline age (p = .178), number of lifetime sexual partners (p = .653), race/ethnicity (p = .156), STI status (p = .788), or coital (vaginal or anal sex: p = .456–.611) and noncoital (manual or oral genital: p = .142–.946) experience. All physical, mental/emotional, and social health measures were taken from these questionnaires.
Both quarterly and annual data collection were conducted by trained interviewers, usually in the home of the adolescent, or in a mutually acceptable public location, like a library or a space in one of the adolescent clinics. Data collection procedures remained the same throughout the duration of the study. This research was approved by the institutional review board of Indiana University/Purdue University at Indianapolis. Informed consent was obtained from each participant and permission obtained from a parent or legal guardian.
The current study
For the current study, we drew a subset of data consisting of any annual questionnaires whose collection date overlapped with quarterly interviews. This means, e.g., we linked all enrollment questionnaires with enrollment interviews, any questionnaires available at the start of year two with the quarterly interviews available at the start of year two, and so on. This selection process results in 715 data points for analysis (11.5%: 715/5,151 of total interviews taken in the study; 11.3% 715/6,308 of total questionnaires taken in the study). Our subset of data had a higher participant mean age (mean [M] = 15.47, standard deviation [SD] = 1.05) than the larger data set (M = 15.35, SD = 1.06) (t = 2.87, p = .002) but did not differ from the larger data set in terms of participant time in the study (t = .30, p = .765), having an STI (t = 1.88, p = .059), reporting any vaginal sex (t = 1.19, p = .232), number of partners reported (−t = −.99, p = .321), or sexual health level (−t = −1.84, p = .06). All participants contributed data for this subset.
Conceptual model development
We initiated analyses by specifying a conceptual model linking the underlying dimensions of sexual health, the sexual health construct itself, and the health and well-being measures (Figure 1). Guided by the World Health Organization [30] and National Commission on Adolescent Sexual Health (NCASH) [19] definitions of sexual health, as well as our own empirical research [20-22], we first identified four dimensions of well-being—emotional, physical, mental/attitudinal, and social—related to sexuality. As described earlier, these dimensions represent a range of normative developmental experiences working together to promote positive sexuality. In this way, these experiences can be argued to underpin, or anchor, a single larger construct of sexual health. We then selected 13 quarterly interview scales to operationalize these well-being dimensions, hypothesizing that these measures would coalesce, or hang together, as a single construct, to predict our health and well-being outcomes of interest. Empirical evaluation of these steps is described in more detail below.
Figure 1.
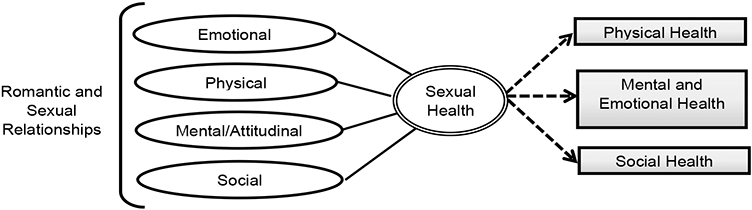
Conceptual model of the relationship between sexual health and physical, mental/emotional, and social health among adolescent women.
Measures
Predictor variable: sexual health.
The primary predictor variable, sexual health, was constructed in several different steps. In keeping with our conceptual model, we first identified the quarterly interview items used to operationalize the domains underlying sexual health. These items have been used in our prior sexual health research [20-22]. Example questions in each individual scale, as well as scale reliability information, are provided below and in Table 1.
Table 1.
Sexual health measure scale information
| Interview scale item | Scale structure and reliability | Reliability (alpha) |
WHO sexual health domain |
|---|---|---|---|
| Relationship quality | (6, 4-point items; SD to SA; e.g., “I feel happy when we are together”) | .95 | Emotional |
| Partner meets needs | (3, 4-point items; SD to SA; e.g., “[X] meets my needs for friendship”) | .98 | Emotional |
| Sexual autonomy | (3, 4-point items; SD to SA; e.g., “It is easy for me to say no if I do not wantto have sex”) | .83 | Physical |
| Absence of genital pain | (5, 4-point items; SD to SA; e.g., “It is painful if [X] touches my genitalarea” [recoded]) | .80 | Physical |
| Sexual satisfaction | (5, 7-point semantic differential items; e.g., “Very bad to very good”) | .94 | Physical |
| Fertility control attitudes | (3, 4-point items; SD to SA; e.g., “I am committed to not getting pregnant”) | .76 | Mental/attitudinal |
| Condom use efficacy | (5, 4-point items; SD to SA; e.g., “It will be easy to use a condom if we have sex”) | .89 | Mental/attitudinal |
| Sexual negativity | (6, 4-point items; SD to SA; e.g., “Sometimes I feel guilty about.sexual behavior” [recoded]) | .90 | Mental/attitudinal |
| Partner sexual communication | (3, 4-point items; SD to SA; e.g., “I can talk to [X] about birth control”) | .92 | Social |
| Closeness to family | (6, 4-point items; SD to SA; e.g., “I am close to my [mother]”) | .95 | Social |
| Partner closeness to family | (6, 4-point items; SD to SA; e.g. “[X] knows my [mother] well”) | .92 | Social |
| Family communication | (6, 4-point items; SD to SA; e.g., “I can talk about personal things withmy [mother]”) | .95 | Social |
| Family STD Communication | (6, 4-point items; SD to SA; e.g., “I can talk about STDs with my [mother]”) | .87 | Social |
SA = strongly agree; SD = strongly disagree; STD = sexually transmitted disease; WHO = World Health Organization.
The emotional domain included two items: relationship quality (six, four-point Likert type items (strongly disagree [SD] to strongly agree [SA]: α = .94; e.g., “We have a strong emotional relationship”; used in prior research) and partner meets needs (three, four-point items; SD to SA: α = .98; e.g. “[X] meets my needs for friendship;” developed for the larger study by the investigators).
The physical domain was comprised of: sexual satisfaction (five, seven-point semantic differential items assessing a participant’s feelings about the sexual relationship with that partner: α = .94; e.g., “very bad to very good”), absence of genital pain (five, four-point items; SD to SA: α = .80; e.g., “It is painful if my partner touches my genital area; developed for the larger study by the investigators), and sexual autonomy (three, four-point items; SD to SA: α = .82; e.g., “It’s easy for me to say no if I don’t want to have sex”).
The mental/attitudinal domain included: fertility control attitudes (three, four-point items; SD to SA: α = 76; e.g., “I am committed to not getting pregnant”), condom use efficacy (five, four-point items; SD to SA: α = 89; e.g., “It will be easy to use a condom if we have sex”) and sexual negativity (six, four-point items; SD to SA: α = 90; e.g., “Sometimes I feel guilty about…sexual behavior” [recoded]).
The social domain invoked: partner sexual communication three, four-point items; SD to SA: α = .92; e.g., “I can talk to [X] about birth control”), participant closeness to family (six, four-point items; SD to SA: α = .95; e.g., “I am close to my [mother]”), partner closeness to family (six, four-point items; SD to SA: α = .92; e.g., “[X] knows my [mother] well”), participant general communication with family (six, four-point items; SD to SA: α = .95; e.g., “I can talk about personal things with my [mother]”) and participant STD communication with family (six, four-point items; SD to SA: α = .87; e.g., “I can talk about STDs with my [mother].”
Finally, to construct our larger single sexual health measure, we standardized each of the 13 interview items to place them on the same metric and created a single additive index of these standardized measures. This final measure was used as the main predictor in all statistical models.
Outcome variables.
We selected 17 annual questionnaire items broadly covering young women’s physical, mental/emotional, and social health.
Physical health measures included:
participant alcohol, marijuana, or cigarette use (all single five-point items; not at all to every day; dichotomized for analysis: none/any).
Mental/emotional health variables were:
feeling depressed (four-item index; e.g., “How often…did you feel down?”; α = .85), thrill seeking (three-item index, e.g., “How often did you…Take chances with your safety because it was exciting?”; α = .81), and self-esteem (10-item additive index, e.g., “I take positive attitude about myself”; α = .92), attitudes toward (four-item index; e.g., “How often have you had sex when you really didn’t want to?”; α = .91), anticrime attitudes (four-item index; e.g., “How wrong is it to….shoplift?”; α = .81), and antideviance attitudes (four-item index; e.g., “How wrong is it to….lie to your parents?”; α = .83).
Social health included:
peer marijuana use and peer alcohol use (both single five-point items: number of friends; none to all), religiosity (four-item index; e.g., “How important is it…to believe in God?”; α = .80), attitudes toward education (four-item index; e.g., “Doing well in school is important to me”; α = .84), community group membership (single three-point item: none to 2+), any school club/group membership (single three-point item: 0–2+), school club/group membership (three-point item: none to 2+), and volunteer work (single three-point item: never to often).
Statistical procedure
Random intercept, two-level (level 1: time, level 2: participant) mixed effects linear (for continuous measures), ordinal logistic regression (for categorical measures), and binary logistic regression (for dichotomous measures) were used to estimate the influence of sexual health on health and well-being outcomes. The mixed effects approach was chosen to adjust model estimates for multiple quarterly interview and annual visit information contributed by the same participant. We conducted one model per health measure, resulting in a total of 17 total models. All models were conducted in Stata, 12.0 and controlled for participant age and race/ethnicity.
Results
Sample characteristics
Participants (n = 385) were an average age of 16.67 (SD = 2.18) and were primarily (89%) African-American. The average maternal education was 12th grade. At enrollment, many (87%–90%) reported experience with hand holding, kissing, and breast touching; fewer had experience with oral genital (33%–56%), vaginal sex (34%), or anal sex (12%). The median number of lifetime sexual partners at enrollment was two, and about one fifth (17.6%) had ever had an STI.
Multivariate estimates
Model estimates, including unstandardized betas with standard errors, or odds ratios (ORs) with 95% confidence intervals, are presented in Table 2.
Table 2.
The impact of sexual health on adolescent women’s (n = 372) physical and mental/emotional and social health, controlling for participant age and race/ethnicity
| Health outcomes | β (SE) | OR (95% CI) |
|---|---|---|
| Physical health | ||
| Any alcohol use (past 2 months: yes) | — | .87 (.78–.96) |
| Any marijuana use (past 2 months: yes) | — | .88 (.79–.96)** |
| Any cigarette use (past 2 months: yes) | ||
| Mental/emotional health | ||
| Self-reported depression | −.41 (.06)*** | — |
| Thrill seeking | −.92 (.22)*** | — |
| Self-esteem | .48 (.08)*** | — |
| Social health | ||
| Peer cigarette use (number of friends) | — | .98 (.81–1.19) |
| Peer alcohol use (number of friends) | — | .83 (.73–.95)* |
| Peer marijuana use (number of friends) | — | .87 (.77–.92)* |
| Religiosity | .16 (.06)*** | — |
| Education attitudes | .32 (.17)*** | − |
| Antisocial attitudes | −.91 (.15)*** | — |
| Social integration | .12 (.05)* | — |
| Frequency of delinquent behavior/crime | −.43 (.08)*** | — |
| Community group membership | — | 2.54 (1.22–5.34)* |
| School club/group membership | — | 1.29 (.28–5.10) |
| Volunteer work | — | 1.39 (.81–2.40) |
p < .05
p < .01
p < .000.
CI = confidence interval; OR = odds ratio; SE = standard error.
Controlling for age and race/ethnicity, young women’s sexual health was associated with better aspects of physical health, including less frequent alcohol use (OR = .87) and less frequent marijuana use (OR = .88) in the prior 2 months. Sexual health was also positively associated with improved mental health, including lower self-reported depression (β = −.41), lower thrill seeking (β = −.92), and higher self-esteem (β = .48).
Finally, sexual health predicted better social health, including a young woman’s having fewer friends who used alcohol (OR = .83) or marijuana (OR = .87), higher religiosity (β = .16), more positive attitudes toward education (β = .32), lower antisocial attitudes (β = −.91), better social integration (β = .12), lower frequency of delinquent behavior and crime (β = −.43), and more frequent community group membership (OR = 2.54). Sexual health was not associated with the number of friends who used cigarettes.
Discussion
Developmentally focused approaches to adolescent health emphasize the complementarity of sexual health with nonsexual aspects of a young person’s overall well-being [31], yet existing data in adolescent poorly articulate the nature of this association. Our data address this gap by linking a multidimensional measure of sexual health to different physical, mental/emotional, and social health variables in a cohort of adolescent women. Our findings may provide support for the idea that cultivating and exercising skills associated with emerging healthy sexuality—such as learning communication, developing self-efficacy, and managing emotion—may also reinforce the skills needed to avoid a variety of health-related risks [23,24], including lower self-reported cigarette and substance use; having fewer friends who use cigarettes, alcohol, or marijuana; better self-esteem and lower self-reported depression; as well as greater social, educational, and religious integration. Our data also begin to challenge outdated, but still widely prevalent, risk-based frameworks that discount the possibility of young people’s having “healthy” sex during adolescence [32,33]. A key contribution of these data is their demonstration that higher physical, mental/emotional, and social health may concomitantly emerge with the developmentally normal range of sexually related experiences young people have during adolescence [34].
From a clinical perspective, these findings provide information about how addressing specific aspects of health sexual development during clinical visits could dually help primary prevention and health education address other common adolescent health issues. For example, young women’s ability to practice open sexual communication could bolster her confidence to refuse tobacco, alcohol, or marijuana [25]. Likewise, a relationship with a partner with whom a young woman shares trust and intimacy could enhance happiness and self-esteem [27] or promote prosocial shared activities [35], such as doing homework or studying together [36], going to a church or religious group together, or volunteering together. Lower sexual risk—perhaps through the ability to refuse unwanted sex or successfully negotiate condom use—has been associated with lower depression [37]. Finally, having a partner who is tightly integrated into one’s friend and/or family network, and who does not smoke or use substances, may promote a young woman’s affiliation with friends who are uninvolved with tobacco, alcohol, or marijuana [38]. Ongoing efforts to realign adolescent health initiatives—both sexual and nonsexual—away from risk-based perspectives and toward skill-based perspectives will continue to benefit from empirical understanding of the specific contexts in which adolescent experiences overlap.
Some limitations associated with the current data should be considered. While these analyses provide important information on impact of sexual health on nonsexual aspects of physical, mental/emotional, and social health in an urban sample of racially/ethnically diverse young women, additional data will be needed to evaluate our findings in other demographically and geographically balanced samples. Moreover, it is unclear how sexual health may promote nonsexual health in young women who choose same-sex partners or those who choose both same-sex and opposite sex relationships. As acknowledged in existing literature [39], substantial revisions may need to be made to existing nationally representative surveys in order to reach appropriate numbers of sexual minority youth. We also do not have a clear understanding of how the structure of sexual health and related nonsexual behaviors function in the relationships of young men. Future studies may seek to replicate these results to better understand whether sexual health could offer the same type and magnitude of protection. Additionally, we are unable to examine how a partner’s perspective on a young woman’s health behaviors may impact the likelihood of different outcomes. Future research may seek to deeply explore the ways in which dyad members mutually influence each other’s propensity to choose or not choose health promoting behaviors. We also did not address any bidirectionality between our sexual health measure, and the markers of physical, mental/emotional, and social health. It is possible that shifting levels in these health outcomes may reciprocally influence sexual health over time among young women. Ongoing work will need to explore both the presence and pattern of such reciprocity. Finally, the current study relied on participant’s self-reported measures of physical, mental/emotional, and social health. While the prospective measurement approach does help to reduce reliability issues like recall bias, additional research may find it useful to integrate established clinical measures as a more standardized gauge of some outcomes.
Even within the context of these limitations, the data presented here provide evidence as to the potential intersection between young women’s experiences with sexual health and other nonsexual outcomes. We suggest that successfully learning to navigate emerging sexuality may strengthen the self-regulatory competencies that adolescent women use to make good decisions about their physical, mental/emotional, and social health. Our perspective challenges existing risk-based assumptions about the mutual exclusivity of “sexuality” and “health” in adolescence, and we suggest that clinicians and health educators can leverage sexuality to more effectively support health promotion.
IMPLICATIONS AND CONTRIBUTION.
Higher sexual health in adolescent women is associated with improved physical, mental/emotional, and social health, including lower nicotine and substance use, lower self-reported depression, higher self-esteem, more positive attitudes toward school and less frequent delinquency/crime. Experience in romantic/sexual relationships may complement skills needed to support positive health behavior.
Acknowledgments
The authors thank the staff of the Young Women’s Project. A previous version of this work was presented at the 2012 Society for Adolescent Health and Medicine annual meeting.
Funding Sources
This study was supported by NICHD grants NIH U19AI43924–06 and R01HD044387-03.
References
- [1].World Health Organization. Defining Sexual Health: Report of a technical consultation on sexual health. Available at: http://www.who.int/reproductive-health/publications/sexualhealth/index.html. Accessed March 16, 2011.
- [2].Centers for Disease Control and Prevention. A public health approach for advancing sexual health in the United States: Rationale and options for implementation, meeting report of an external consultation; 2010. Atlanta, GA. Available at: https://www.cdc.gov/sexualhealth/docs/SexualHealthReport-2011-508.pdf. Accessed July 25, 2016. [Google Scholar]
- [3].Tharp AT, Carter M, Fasula AM, et al. Advancing adolescent sexual and reproductive health by promoting healthy relationships. J Women’s Health 2013;22:911–4. [DOI] [PubMed] [Google Scholar]
- [4].Connolly J, McIsaac C. Romantic relationships in adolecence. In: Underwood MK, Rosen LH, eds. Social Development: Relationships in Infancy, Childhood, and Adolescence. New York, NY: Guilford Press; 2011:180–206. [Google Scholar]
- [5].Norona JC, Roberson PN, Welsh DP. “I learned things that make me happy, things that bring me down” lessons from romantic relationships in adolescence and emerging adulthood [e-pub ahead of print]. J Adolesc Res 2015. doi: 10.1177/0743558415605166. [DOI] [Google Scholar]
- [6].Giordano PC, Manning WD, Longmore MA. Adolescent romantic relationships: An emerging portrait of the their nature and significance. In: Crouter AC, Booth A, eds. Romance and Sex in Adolescence and Emerging Adulthood: Risks and Opportunities. New York, NY: Lawrence Earlbaum; 2014:127–48. [Google Scholar]
- [7].Hensel DJ, Fortenberry JD. Lifespan sexuality through a sexual health perspective. In: Tolman DL, Diamond LM, eds. APA Handbook on Sexuality and Psychology. Washington, D.C.: APA Press; 2013. [Google Scholar]
- [8].Satcher D. The Surgeon General’s call to action to promote sexual health and responsible sexual behavior. Am J Health Education 2001;32:356–68. [PubMed] [Google Scholar]
- [9].Harden KP. A sex-positive framework for research on adolescent sexuality. Perspect Psychol Sci 2014;9:455–69. [DOI] [PubMed] [Google Scholar]
- [10].Anderson RM. Positive sexuality and its impact on overall well-being. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz 2013;56:208–14. [DOI] [PubMed] [Google Scholar]
- [11].George WH, Norris J, Nguyen HV, et al. Sexuality and health. In: Tolman DL, Diamond LM, Bauermeister JA, et al. , eds. APA Handbook of Sexuality and Psychology, Vol. 1: Person-based Approaches. Washington, D.C.: American Psychological Association; 2014:655–96. [Google Scholar]
- [12].Herbenick D, Reece M, Schick V, et al. Sexual behaviors, relationships, and perceived health status among adult women in the United States: Results from a national probability sample. J Sex Med 2010;7:277–90. [DOI] [PubMed] [Google Scholar]
- [13].Laumann EO, Paik A, Glasser DB, et al. A cross-national study of subjective sexual well-being among older women and men: Findings from the global study of sexual attitudes and behaviors. Arch Sex Behav 2006;35:143–59. [DOI] [PubMed] [Google Scholar]
- [14].Vasilenko SA, Lefkowitz ES, Maggs JL. Short-term positive and negative consequences of sex based on daily reports among college students. J Sex Res 2012;49:558–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Galinsky AM, Sonenstein FL. The association between developmental assets and sexual enjoyment among emerging adults. J Adolesc Health 2011;48:610–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Valois RF, Zullig KJ, Huebner ES, et al. Association between life satisfaction and sexual risk-taking behaviors among adolescents. J Child Fam Stud 2002;11:427–40. [Google Scholar]
- [17].Shrier L, Koren S, Aneja P, de Moor C. Affect regulation, social context, and sexual intercourse in adolescents. Arch Sex Behav 2010;39:695–705. [DOI] [PubMed] [Google Scholar]
- [18].Horne S, Zimmer-Gembeck MJ. Female sexual subjectivity and well-being: Comparing late adolescents with different sexual experiences. Sex Res Social Policy 2005;2:25–40. [Google Scholar]
- [19].Haffner DW. Facing facts: Sexual health for America’s adolescents. New York, NY: National Commision on Adolescent Sexual Health, Sexuality Information and Educational Council of the United States; 1995:40. [Google Scholar]
- [20].Fortenberry JD, Hensel DJ. Adolescent sexual health and sexually transmitted infections: A conceptual and empirical demonstration. In: Aral SO, Fenton KA, Lipshutz JA, eds. The New Public Health and STD/HIV Prevention. New York: Springer; 2013:293–305. [Google Scholar]
- [21].Hensel DJ, Fortenberry JD. A multidimensional model of sexual health and sexual and prevention behavior among adolescent women. J Adolesc Health 2013;52:219–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hensel DJ, Fortenberry JD. Adolescent women’s relationship-based sexual health and STI-associated behaviors. Health Education Monogr Ser 2014; 31:7–14. [Google Scholar]
- [23].Fergus S, Zimmerman MA. Adolescent resilience: A framework for understanding healthy development in the face of risk. Annu Rev Public Health 2005;26:399–419. [DOI] [PubMed] [Google Scholar]
- [24].Catalano RF, Fagan AA, Gavin LE, et al. Worldwide application of prevention science in adolescent health. Lancet 2012;379:1653–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Wolfe DA, Crooks CV, Chiodo D, et al. Observations of adolescent peer resistance skills following a classroom-based healthy relationship program: A post-intervention comparison. Prev Sci 2012;13:196–205. [DOI] [PubMed] [Google Scholar]
- [26].Haynie DL, Giordano PC, Manning WD, Longmore MA. Adolescent romantic relationships and delinquency involvement. Criminology 2005;43:177–210. [Google Scholar]
- [27].Robinson KJ, Cameron JJ. Self-esteem is a shared relationship resource: Additive effects of dating partners’ self-esteem levels predict relationship quality. J Res Personal 2012;46:227–30. [Google Scholar]
- [28].Boschloo L, Vogelzangs N, Van den Brink W, et al. The role of negative emotionality and impulsivity in depressive/anxiety disorders and alcohol dependence. Psychol Med 2013;43:1241–53. [DOI] [PubMed] [Google Scholar]
- [29].Fortenberry JD, Temkit MH, Tu W, et al. Daily mood, partner support, sexual interest, and sexual activity among adolescent women. Health Psychol 2005;24:252–7. [DOI] [PubMed] [Google Scholar]
- [30].World Health Organization. What constitutes sexual health? Progress in reproductive health research; 2004:2–3. 67. [Google Scholar]
- [31].Diamond LM, Huebner DM. Is good sex good for you? Rethinking sexuality and health. Social Personal Psychol Compass 2012;6:54–69. [Google Scholar]
- [32].Halpern CT. Reframing research on adolescent sexuality: Healthy sexual development as part of the life course. Perspect Sex Reprod Health 2010; 42:6–7. [DOI] [PubMed] [Google Scholar]
- [33].Fortenberry JD. Adolescent sex and the rhetoric of risk. In: Romer D, ed. Reducing adolescent risk: Toward an integrated approach. Thousand Oaks, CA: Sage Publications, Inc; 2003:293–300. [Google Scholar]
- [34].Fortenberry JD. Adolescent sexual well-being in the 21st century. J Adolesc Health 2016;58:1–2. [DOI] [PubMed] [Google Scholar]
- [35].Carlson W, Rose AJ . Brief report: Activities in heterosexual romantic relationships: Grade differences and associations with relationship satisfaction. J adolescence 2012;35:219–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Giordano PC, Phelps KD, Manning WD, Longmore MA. Adolescent academic achievement and romantic relationships. Social Sci Res 2008;37:37–54. [Google Scholar]
- [37].Khan MR, Kaufman JS, Pence B, et al. Depression, sexually transmitted infection, and sexual risk behavior among young adults in the United States. Arch Pediatr Adolesc Med 2009;163:644–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kreager DA, Haynie DL, Hopfer S. Dating and substance use in adolescent peer networks: A replication and extension. Addiction 2013;108:638–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Ivankovich MB, Leichliter JS, Douglas JM Jr. Measurement of sexual health in the US: An inventory of nationally representative surveys and surveillance systems. Public Health Rep 2013;128(Suppl. 1):62–72. [DOI] [PMC free article] [PubMed] [Google Scholar]


