Abstract
The rapid deployment of video visits during COVID-19 may have posed unique challenges for home-based primary care (HBPC) practices due to their hands-on model of care and older adult population. This qualitative study examined provider perceptions of video visits during the first wave of the COVID-19 crisis in New York City (NYC) through interviews with HBPC clinical/medical directors, program managers, nurse practitioners/nurse managers, and social work managers (n=13) at 6 NYC-area practices. Providers reported a combination of commercial (health system-supported) and consumer (e.g., FaceTime) technological platforms was essential. Video visit benefits included triaging patient needs, collecting patient information, and increasing scheduling capacity. Barriers included cognitive and sensory abilities, technology access, reliance on caregivers and aides, addressing sensitive topics, and incomplete exams. Effectively integrating video visits requires considering how technology can be proactively integrated into practice. Policy that promotes platform flexibility will be crucial in fostering video integration.
Keywords: primary care, homebound, home health, telehealth, telemedicine, COVID-19
Introduction
Each year more older adults in the U.S. become homebound than enter nursing homes (Ornstein, Garrido & Bollens-Lund, 2020). Home-based primary care (HBPC) delivers medical care to homebound patients in private residences or assisted living facilities who experience disability, multi-morbidity, cognitive impairment, and excessive rates of hospitalization (Ritchie & Leff, 2018; Leff et al., 2015; Schuchman, Fain, & Cornwell, 2018). HBPC facilitates access to care for patients and families who otherwise have difficulty traveling to office-based practices, and provides invaluable perspectives on the patient’s life and social circumstances that significantly affect health (Leff et al., 2015; Schuchman, Fain, & Cornwell, 2018).
Prior to the COVID-19 pandemic, video visits that allow providers and patients to meet remotely through HIPAA-compliant video conferencing platforms had emerged as an important innovation in health care delivery. These video visits mimic features of the in-home encounter while eliminating travel time for providers, allowing practices to respond more quickly to patient needs. During video encounters, HBPC physicians can examine a wound, visually review patients’ medications, or view home conditions that might interfere with patients’ health and well-being. However, there are potential limitations, including concerns over access, technical and administrative challenges, and limits to what can be seen through a video screen (Kim, Gellis, Bradway, & Kenaley, 2019; Kozikowski et al., 2019; Latus-Olaifa et al., 2019). Access challenges in particular may be important for homebound patients, who commonly have limited incomes and may not have access to necessary technology, such as a smartphone or broadband service (Abrashkin, Poku., Ball, Brown, & Rhodes, 2020; Kalicki. Moody, Franzosa, Gliatto, & Ornstein, 2021). Patients with limited incomes are also less likely to use physician-interfacing technologies like electronic health record patient portals (Sarkar et al., 2011). Only 43% of Americans over age 65 use the Internet, a number which declines sharply with age (Ornstein et al., 2015). Moreover, 56-80% of homebound older adults have cognitive impairments and sensory impairments such as sight or hearing loss are common (Lam, Lu, Shi, & Covinsky, 2020; Ornstein et al., 2015) adding a layer of complexity to video encounters.
The benefits and challenges of video telehealth were heightened by the COVID-19 crisis. While many HBPC practices had little or no experience with the technology prior to the pandemic, COVID-related disruptions to in-home visits and outpatient care forced providers to rapidly implement video visits in order to maintain care for their patients. This adoption was facilitated by relaxation of the Health Insurance Portability and Accountability Act of 1996 (HIPAA) regulations to allow for the use of non-HIPAA compliant platforms (e.g., FaceTime, WhatsApp, and Zoom) in the “good faith provision of telehealth” and the temporary increase in telehealth reimbursement rates for Medicare and Medicaid patients (Centers for Medicare and Medicaid Services, 2020). However, providers also faced the challenge of rapidly consenting and orienting patients to telehealth while also managing established technological barriers and cognitive and sensory issues (Abrashkin, Poku, Ball, Brown, & Rhodes, 2020; Franzosa et al., 2021; Kalicki. Moody, Franzosa, Gliatto, & Ornstein, 2021). While some of these challenges have been documented, there is less understanding of the specific circumstances and considerations under which video visits may be successful or not, and which of these may be modifiable.
The experiences of HBPC practices during the COVID-19 pandemic may provide valuable insights into the use of video visits not only for home-based providers, but all practices serving similar populations. The aim of this qualitative study was to better understand HBPC practices’ use of video visits during the initial pandemic surge in New York City (NYC), barriers and facilitators to its use, and considerations for engaging older, medically complex patients in video visits in the future.
Methods
Participants and their practices
Because HBPC is by definition multi-disciplinary, we interviewed leaders across different practice roles (medical, nursing and social work) from multiple sites to obtain a range of perspectives and experiences. We recruited participants through a combination of purposeful and snowball sampling. Using the study team’s professional networks and HBPC professional associations, we first identified nine NYC-area practices representing a range of characteristics (health system-based/independent; profit status, size) and providing care in private homes, aiming to recruit at least one practice per characteristic. We recruited practices by phone and email, and six responded to our request. We asked respondents to refer us to their practice’s clinical directors and nursing and social work leadership for recruitment, continuing this process until reaching thematic saturation.
Approach
Data Collection.
Interviews were conducted from May-July 2020 and queried respondents about their experiences during the initial NYC COVID-19 surge (March-June 2020). We (EF and KG) obtained informed verbal consent and conducted 30-45 minute semi-structured interviews via videoconference. Interviews were recorded and transcribed verbatim. Participants also completed a 10-question online survey about practice characteristics. The authors developed the interview guide collaboratively around three topics: 1) major practice challenges due to COVID-19; 2) adaptations to these challenges; and 3) advice for practices. We probed how practices were managing specific issues including telehealth/video visits, care of COVID patients, end-of-life care, and staffing. Participants were asked to describe their roles and tenure. We piloted the guide with three providers in the Mount Sinai Visiting Doctors practice, refining the structure and language based on their feedback. As the overall content of the guide remained the same and the pilot practice met our inclusion criteria, we chose to include pilot data in our analysis.
Data Analysis.
We conducted a qualitative thematic analysis through a combined deductive and inductive approach, using focused coding to address our specific research questions (role of video visits; barriers and facilitators; relevance to future practice) and open coding to capture broader emergent themes (Creswell, 2012). To ensure rigor of the findings, consistent with Lincoln and Guba’s criteria for trustworthiness (Guba, 1981; Lincoln & Guba, 1986), two coders (EF and KG) reviewed the same two interviews independently to identify COVID-related practice adaptations. For this analysis, we then reviewed all “telehealth” codes for a priori and emergent concepts, developing an initial codebook through analytic memos and discussion. We applied the codebook to these two interviews, comparing, discussing, and refining it with additional researchers (KO and AF) until no new codes emerged. We then coded the remaining interviews independently and reviewed each other’s coding, using these codes to draw larger themes (Nowell, Norris, White, & Moules, 2017). We recorded our analytic decision-making process with detailed notes throughout the research design and coding process, as well as memos reflecting on our own assumptions to limit our biases and strengthen our interpretation. We returned to this audit trail throughout our analysis to confirm our interpretations and coding decisions and ensure that no relevant data was inadvertently or systematically excluded. We also triangulated our findings by comparing our results to relevant telehealth literature. Data were analyzed using Dedoose qualitative software (SocioCultural Research Consultants, 2015). Research activities were approved by the Institutional Review Board of the Icahn School of Medicine at Mount Sinai (protocol #15-0950). This article adheres to the Consolidated Criteria for Reporting Qualitative Research (COREQ) reporting guidelines (Tong, Sainsbury, & Craig, 2007).
Results
Participant Characteristics
We interviewed 13 participants from 6 practices: 6 medical/clinical directors (CDs), 1 program manager (PM); 3 nurses in nurse practitioner or manager roles (NCs); and 3 social work managers (SWs). Participants had worked in their practices for a median of 12 years. Practices were primarily private, non-profit and hospital-based, although we included two independent and one public practice. Median practice size as of March 1, 2020 was 900 patients and ranged from 45 to 1,400 patients. [See Table 1]
Table 1:
Participant and Practice Characteristics
| Participant characteristics | N |
|---|---|
| Total participants | 13 |
| Role | |
| Medical/clinical director | 6 |
| Program manager | 1 |
| Nurse/nursing coordinator | 3 |
| Social worker/social work coordinator | 3 |
| Years working in program | |
| Median (range) | 12 (1-18) |
| Practice characteristics | N |
| Total Practices | 6 |
| Area served | |
| Urban | 5 |
| Suburban | 1 |
| Primary sponsor/owner | |
| Health system | 4 |
| Independent provider/group | 2 |
| Profit status | |
| For-profit | 1 |
| Non-profit | 5 |
| Sector | |
| Private | 5 |
| Public | 1 |
| Practice size before 3/1/2020 | |
| Median (range) of patients | 900 (45-1400) |
| Years in existence | |
| Mean | 13.5 |
| Range | 1-25 |
| Participants interviewed per program | |
| Min | 1 |
| Max | 4 |
Flexibility of telehealth platforms was necessary for success
Pre-pandemic, participants described a range of experience with phone and video telehealth; larger, hospital-based practices and one smaller start-up used video apps or platforms integrated into the patient portal of their electronic health records, while other independent practices were accustomed to phone consultations, but not video, to supplement home visits. Still, all practices rapidly expanded or initiated phone and video visits to substitute for in-home care. While participants generally expressed pride in how quickly they and their patients adapted, they also described limitations of commercial platforms, including the need to rapidly consent patients, set up patient portal accounts, and learn a new system quickly. To supplement HIPAA-compliant platforms, all practices employed “backdoor” consumer tools such as text, email, FaceTime and WhatsApp to maintain care as privacy rules were relaxed and telehealth reimbursement expanded. As one clinical director explained, “we’ve been using a lot of ‘hey, can you take a picture of that for me?’” (CD, Practice 5) Even in practices with video visit experience, rapid expansion proved challenging with regard to orienting clinical staff and consenting patients. Many staff experimented with multiple platforms to find one that was easiest for providers and patients. Several providers stressed the importance of redundancy and having a “backup platform” so that you could “go down the line [with a patient] until you find one that works.” (SW, Practice 5)
Overall, providers noted the diversity of options (institutional platforms, other HIPAA-compliant commercial platforms, and consumer platforms) allowed greater access to patients than would otherwise have been possible. Providers appreciated the ease of texting images of a skin condition or meeting quickly by FaceTime and hoped this flexibility could continue as privacy rules were enforced again. “We just did whatever we really felt was needed for that patient, and it’s going to be spoiled going back to the regular [institutional platform] way,” noted one social worker (Practice 1). [See Table 2]
Table 2.
HBPC Provider Perceptions of Video Telehealth: Key Themes and Subthemes
1. Flexibility of telehealth platforms was necessary for success
|
2. Use of video telehealth improves provider efficiency and capacity
|
3. Use of video telehealth is limited by patient, clinical, and technological factors
|
4. Video telehealth is a substitute for human touch – but only temporarily
|
Benefits of video visits: Improving efficiency, capacity and collaboration
Video as a tool for triage, efficient visits, and a step-wise approach to care.
Many providers reported using video visits to triage patient needs and determine if an in-person visit or service was necessary, helping “[pare] down what’s really an emergency and what’s just a bruise” (CD, Practice 5). Clinicians also found video visits valuable for gathering patient information ahead of an in-person visit to “prep the visit to be the most efficient and effective that it can be” (SW, Practice 1). Providers frequently described a step-wise approach to incorporating video; scheduling video visits as a first attempt, moving to phone calls if patients were not able to use or not comfortable with video, and finally, defaulting to in-person visits if neither modality sufficed. For instance, one practice established a new category of “pressing” in-person visits if “we have attempted video or telephone calls and it’s just not cutting it” (CD, Practice 6), meaning they were either not able to make the technology work, or to get the patient information needed.
Expanding capacity and improving efficiency of urgent care.
Providers reported video was particularly useful for scheduling urgent care visits quickly, and determining if follow-up in-person care was necessary. As one clinical director explained, prior to COVID-19 urgent care visits had to be requested and scheduled before the day’s visits began, but “now a person could call at noon, and we could do a video urgent visit at two.” (CD, Practice 6) Several participants noted that by eliminating travel time, practices could expand their reach and capacity, potentially allowing them to take on larger panels with fewer staff and less overhead in the future and improving practice viability.
Facilitating provider collaboration and specialty care.
Participants noted commercial video platforms allowed for greater collaboration between providers and easier access to and integration of specialists. “If you and I wanted to share in a discussion with a particular patient, we could just both get in the link simultaneously,” explained one medical director. “I’ve been in conversations with up to four people and that’s been easy to facilitate” (Practice 2). Providers could also share information from multiple locations; for instance, one provider explained that if a patient lacked technology, “the nurse [at the in-person visit] will use her own phone or computer to initiate a telehealth visit with the provider.” (NC, Practice 6) In other cases, providers partnered with community paramedics to deliver equipment such as pulse oximeters to COVID-suspect patients, and then conduct daily remote check-ins to monitor their condition.
Limits of video visits: Patient abilities, dependence on caregivers, establishing trust, incomplete information
Patient abilities.
Barriers to video visits included technological literacy, lack of access to equipment and reliable internet service, and patients’ manual dexterity, hearing or vision loss, and cognitive ability. As one program manager noted, “Our normal primary care patients are already struggling with telehealth…we know those barriers are just going to be that much more difficult to surmount in our geriatric population.” (Practice 3) However, providers also noted the ability and desire to use video varied greatly among patients regardless of age or disability, explaining that “you’ll have 95-year-olds who are like, ‘I’ll FaceTime you’, then you have some like, ‘I have a rotary phone on my wall.’” (NC, Practice 1)
Reliance on caregivers and aides to facilitate video visits.
Providers often enlisted caregivers and home health aides to assist with video visits, which also presented challenges. Both caregivers and aides, also often older adults, could have difficulty connecting to or using the platform. Once accessed, family caregivers might dominate the conversation (“okay, it’s great to see you Mr. So-and-so, but I really need to see your wife.” (NP, Practice 1)), while relying on paid caregivers often meant using the aides’ own phone and data plan. As one provider asked, “is someone reimbursing [the aide] for that [data]? Is there Wi-Fi in the home? Do they [the aide] even have a smartphone?” (CD, Practice 6). In addition, access to commercial telehealth platforms was generally restricted to patients’ proxies, not paid caregivers, limiting aides’ ability to assist.
Concerns over an “incomplete picture”.
HBPC providers were accustomed to high-touch, ongoing personal care as well as the information gathered from home visits. Many expressed concern that they might “miss” important information in video visits. “I saw somebody last week who was falling and we really needed a clear assessment of his home and there’s concern about cognitive delays and hearing loss, and it was hard to really get the full picture even with a video,” shared one clinical director (Practice 2). A nurse practitioner similarly described feeling guilty over the deaths of patients she had seen only virtually, noting that “maybe if things were different and I was able to go in and make visits, I could pick up other issues quicker.” (Practice 4)
Problems of establishing trust and addressing sensitive topics.
Providers noted longitudinal home-based care required establishing trust with patients and making them physically and emotionally comfortable, something they did not feel was always possible through video. For instance, several participants felt older patients in particular were not comfortable with video exams. One medical director said that when an older patient refused to lift his shirt so she could assess his skin, “I just couldn’t get as much information because they weren’t comfortable,” (CD, Practice 1) Similarly, it could be difficult to establish a rapport with new patients by video. “When you open a new patient via telehealth, you don’t have that same [trust] like when you go to a doctor for the first time…because they don’t meet us person to person,” explained one nursing coordinator (Practice 1).
Discussing sensitive topics could also be challenging. While providers felt video visits were valuable for specific acute concerns (“they’ve got a new rash, they’ve got a new swelling”), they were not as effective for “human to human” interactions like “a goals of care conversation or something as really emotionally charged.” (CD, Practice 1) As one nurse practitioner who considered herself highly skilled at these conversations explained, “it was a whole different thing having a face-to-face conversation in person as opposed to [saying over video], “I’m sorry. Mom’s dying. What do we want to do?” (Practice 1)
A substitute for human touch – but only temporarily
Providers reported video visits were an important and “reassuring” face-to-face connection to patients, especially those who lived alone or were socially isolated. “There is something very personal about seeing someone’s face that’s nicer than the telephone,” explained one social worker (Practice 6), while another noted that “people just trust you [on video]. If they see you’re smiling, you can do a lot…even if it freezes here and there, it’s still better than a phone call” (SW, Practice 1). Several providers described emotional benefits; as one social worker explained, “the mental health side of this has been bad [for patients], but I can’t imagine how much worse it would’ve been if people couldn’t have virtually connected.” (Practice 1)
However, providers also felt video was only a temporary substitute for human touch. “They’re very excited [about video visits] but they’re all still waiting for me to come,” said one physician. “They want the in-person visits still.” (Practice 6) This was also true for providers; “I miss that touch, like actually being there. Seeing them. They miss it. The patients miss it too.” (NC, Practice 1) Providers generally agreed ideally, a mix of video and in-person visits would best support patient care in the future. As one social worker explained, “I don’t think HBPC programs could go 100 percent video. I don’t see how that would work,” but that “once that relationship [with a patient] is established, in-between visits, I think that’s something we’re going to be definitely using.” (Practice 1)
Discussion
COVID-19 has highlighted the importance of virtual care as a tool in home-based practice. The accelerated pace of change driven by the pandemic and resulting changes in regulation and reimbursement have also allowed for rapid HBPC practice innovations that would not otherwise have been possible.
Our study participants adapted rapidly to incorporating video visits into care, and overall found them valuable. However, in practice they experienced substantial drawbacks to commercial platforms, especially those integrated with patients’ medical records and requiring additional steps such as downloading apps and logging into secure patient portals. To overcome these challenges, providers created redundancies through back-up commercial and consumer platforms, and feared losing this flexibility post-pandemic once HIPAA rules were again tightened and telehealth reimbursement limited. To maintain flexibility and access, practices and health systems may consider employing back-up systems or multiple platforms rather than limiting providers to a single option. It is also worth noting that participants in our study did not mention, and we did not probe, potential privacy risks posed by the use of consumer platforms during the height of the crisis when providers’ priority was to reach patients by any means possible. As access to consumer platforms is again restricted, developers should aim to ensure HIPAA-compliant products are both secure and user-friendly (Shachar, Engel, & Elwyn, 2020). Some commercial platforms have already added features allowing providers to send patients direct, secure links for visits rather than requiring complex logins, or to call patients through encrypted apps. In addition, commercial platforms should incorporate person-centered design for older adults who may experience sensory or dexterity issues, as well as easy-to-use communication functions common to consumer platforms, such as text messaging or group chat capabilities (Wosik et al., 2020). Finally, policies governing telehealth should support the needs of end users, ensuring that security requirements do not come at the expense of restricting access to care and reimbursing telehealth visits at a level that makes them viable for providers.
Participants also reported that video visits improved efficiency by allowing them to triage patients’ needs quickly and determine when in-person care was needed, for example, during an urgent care visit. Eliminating travel time allowed providers to schedule more visits, a critical benefit when many practices were short-staffed due to redeployments and illness, and improved access to specialists, a particular concern for the homebound population (Jain, Dasari, Soriano, DeCherrie, & Kerr, 2011). The ability to expand capacity though video encounters could be a valuable asset for HBPC practices that are often financially challenged (Desai, Smith, & Boal, 2008; Eric De Jonge et al., 2014). However, these benefits must be considered against potential limitations; for instance, the ability to conduct a higher number of visits via video is not a benefit if important patient information is missed, or if time formerly spent traveling is now used helping a patient log in to a video platform.
Some limitations providers identified, such as access to technology, are well documented (Kim et al., 2019; Kozikowski et al., 2019). Practices, health systems and payers can play an important role in addressing these issues. For example, Medicare Advantage plans might leverage the CHRONIC Care Act to provide non-medical devices such as tablets to participants, helping to close the technology divide for lower-income patients and caregivers (Hostetter M, 2020; Willink & DuGoff, 2018). Universal efforts to address inequities in internet access, such as municipal broadband, could also improve access for this population providing that such services address barriers to use (Baker, Hanson, & Myhill, 2009). Other limitations appeared specific to this population, such as the reliance on caregivers and aides. These concerns demonstrate the heightened demands already placed on family caregivers and the home health workforce during the pandemic (Dang et al., 2020; Sterling, Tseng, et al., 2020), and the need to provide them with greater resources, funding and support. They also highlight the need to include aides as essential care partners when regulating access to patient information (Sterling, Dell, et al., 2020).
Finally, our participants noted that “human to human” interaction was central to their care model. Both providers and patients appreciated the temporary connection video visits provided, but longed for a return to in-person care. This was especially prevalent when sensitive health issues like goals of care and end-of-life care conversations arose, but was also important to day-to-day care of socially isolated homebound patients. Balancing video and in-person care will require consideration of providers’ and patients’ preferences for personal connection, as well as health care needs.
Lessons for the future: Proactively integrating video visits into home-based care
Providers in our study worked hard to deploy video visits rapidly in an emergency and under extraordinary strain. While their efforts were largely successful, the pandemic forced practices to use this technology reactively, as a substitute for in-person care. As video visits and remote monitoring become more embedded in practice, they have the potential to be used more deliberately to complement and ultimately enhance in-person care by incorporating the technology into workflows and visit algorithms. For example, practices might provide briefer, more frequent check-ins with high risk patients between in-person visits.
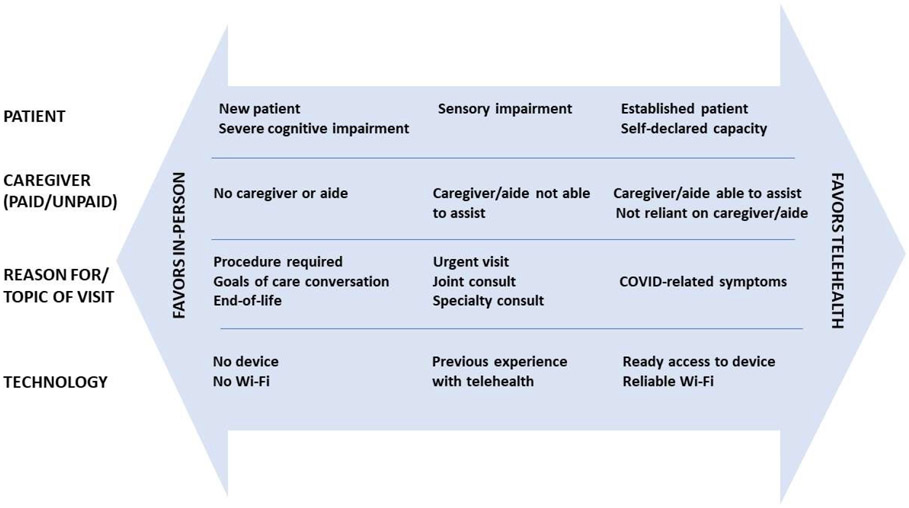
As a first step toward integrating video technology more proactively, our study identified several issues to consider, including patient (physical/cognitive ability), caregiver (reliance on caregiving and caregivers’ ability to assist), visit (urgent care, acute issues, goals of care conversations) and technology (devices and internet) factors. Importantly with this population, hands-on care was sometimes unavoidable. In planning for the future, practices must consider which patients, and under which circumstances, video telehealth is optimal and where more in-person care may be necessary. For instance, if a caregiver is not able to assist with telehealth visits, practices might have a nurse coach the patient or caregiver through using the system. To establish trust with a new patient while limiting potential COVID exposure, a practice might perform the majority of the intake assessment via video, and then send a clinician to meet the patient briefly in person. [See Figure 1]
Figure 1.
Factors to Consider in Implementing Video Visits
Our study had several strengths and some limitations. We began interviews shortly after the initial peak of NYC cases, reducing recall bias. We included a diversity of practice types and multiple interviewees across practices. However, our sample represents fewer than 25% of NYC area HBPC practices (Pepper, Michener, & Kinosian, 2019), and practices were primarily urban, non-profit, and private. The experiences of different types of practices across the country may be substantially different and will be investigated in additional studies. In addition, we only interviewed practice leadership, not staff, and did not interview patients and caregivers, and their perspectives may differ. Finally, our findings must be considered in light of the rapidly evolving pandemic.
Conclusion
NYC HBPC practices adapted rapidly to incorporate and expand the use of video visits during the initial NYC COVID-19 surge. While video visits present some challenges, practices can develop strategies to address them by considering intersecting patient, caregiver, health condition and technology factors. While video visits cannot fully replace hands-on care for this population, incorporating them as an additional tool in the diagnostic and clinical arsenal may improve delivery of care, as well as the viability of home-based primary care practices and other practices serving older, medically complex adults.
Supplementary Material
Funding Acknowledgement
This study is funded by the National Institute on Aging (NIA, 1R01AG052557). The sponsors played no role in any of the design, conduct, or preparation of this article.
Footnotes
- Dr. Brody reports funding from the National Institutes of Health and the Patient-Centered Outcomes Research Institute (PCORI) and personal fees from Abbott Nutrition.
- Dr. Ritchie reports funding from the National Institutes of Health, The John A Hartford Foundation, Centene Foundation; royalties from Wiley Inc and Wolters Kluer and is a consultant for the American Academy of Hospice and Palliative Medicine.
- Dr. Leff reports personal fees from Medzed, and grants from the John A. Hartford Foundation, Centene Foundation, and the California Healthcare Foundation
- Dr. Kinosian is a Board member of the American Academy of Home Care Medicine.
- Dr. Ornstein reports funding from the National Institute on Aging during the conduct of the study
- Dr. Federman reports funding from the National Institute on Aging during the conduct of the study.
- Drs. Franzosa, Gorbenko and Sheehan have no conflicts of interest to report
Human Subjects Approval
This project has been reviewed and approved by the Icahn School of Medicine at Mount Sinai Institutional Review Board, Study #15-0950.
Contributor Information
Emily Franzosa, Brookdale Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, 1 Gustave L. Levy Pl, New York, NY 10029; Geriatrics Research, Education, and Clinical Center (GRECC), James J. Peters VA Medical Center, Bronx, NY.
Ksenia Gorbenko, Department of Population Health Science and Policy, Institute of Healthcare Delivery Science, Icahn School of Medicine at Mount Sinai, 1 Gustave L. Levy Pl, New York, NY 10029.
Abraham A. Brody, Hartford Institute of Geriatric Nursing, Rory Meyers College of Nursing, New York University, 433 1st Avenue 5th floor, New York, NY 10010.
Bruce Leff, Center for Transformative Geriatric Research, Division of Geriatrics, Department of Medicine, School of Medicine, Johns Hopkins University, 2024 E Monument St, Baltimore, MD 21287.
Christine S. Ritchie, Division of Palliative Care and Geriatric Medicine, Mongan Institute Center for Aging and Serious Illness, Massachusetts General Hospital, Harvard Medical School, 450 Brookline Avenue, Boston, MA 02215.
Bruce Kinosian, Leonard Davis Institute of Health Economics, University of Pennsylvania, 3641 Locust Walk # 210, Philadelphia, PA 19104; Division of Geriatrics, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA.
Orla C. Sheehan, Center for Transformative Geriatric Research, Division of Geriatrics, Department of Medicine, School of Medicine, Johns Hopkins University, 2024 E Monument St, Baltimore, MD 21287; Center on Aging and Health, Johns Hopkins University School of Medicine.
Alex D. Federman, Department of Medicine, Icahn School of Medicine at Mount Sinai, 1 Gustave L. Levy Pl, New York, NY 10029.
Katherine A. Ornstein, Brookdale Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, 1 Gustave L. Levy Pl, New York, NY 10029.
References
- Abrashkin KA, Poku A, Ball T, Brown ZJ, & Rhodes KV (2020). Ready or not: Pivoting to video visits with homebound older adults during the COVID-19 pandemic. Journal of the American Geriatrics Society, 68(11), 2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker P, Hanson J, & Myhill WN (2009). The promise of municipal WiFi and failed policies of inclusion: The disability divide. Information Polity, 14(1, 2), 47–59. [Google Scholar]
- Creswell JW (2012). Qualitative inquiry and research design: Choosing among five approaches: Sage. [Google Scholar]
- Dang S, Penney LS, Trivedi R, Noel PH, Pugh MJ, Finley E, … Leykum L (2020). Caring for caregivers during COVID-19. Journal of the American Geriatrics Society. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai NR, Smith KL, & Boal J (2008). The positive financial contribution of home-based primary care programs: The case of the Mount Sinai Visiting Doctors. Journal of the American Geriatrics Society, 56(4), 744–749. [DOI] [PubMed] [Google Scholar]
- Eric De Jonge K, Jamshed N, Gilden D, Kubisiak J, Bruce SR, & Taler G (2014). Effects of home-based primary care on Medicare costs in high-risk elders. Journal of the American Geriatrics Society, 62(10), 1825–1831. [DOI] [PubMed] [Google Scholar]
- Franzosa E, Gorbenko K, Brody AA, Leff B, Ritchie CS, Kinosian B, … & Federman AD (2021). “At home, with care”: lessons from New York City home-based primary care practices managing COVID-19. Journal of the American Geriatrics Society, 69(2), 300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostetter M, K. S. (2020). In Focus: CHRONIC Care Act Prompts Some Medicare Advantage Plans to Incorporate Social Services. Retrieved from https://www.commonwealthfund.org/publications/2020/jan/focus-chronic-care-act-prompts-some-medicare-advantage-plans-incorporate
- Jain R, Dasari S, Soriano T, DeCherrie L, & Kerr LD (2011). Rheumatologists on the road: A subspecialist's role in caring for the homebound. Arthritis care & research, 63(10), 1482–1485. [DOI] [PubMed] [Google Scholar]
- Kalicki AV, Moody KA, Franzosa E, Gliatto PM, & Ornstein KA (2021). Barriers to telehealth access among homebound older adults. Journal of the American Geriatrics Society. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E, Gellis ZD, Bradway C, & Kenaley B (2019). Key determinants to using telehealth technology to serve medically ill and depressed homebound older adults. J Gerontol Soc Work, 62(4), 451–474. doi: 10.1080/01634372.2018.1499575 [DOI] [PubMed] [Google Scholar]
- Kozikowski A, Shotwell J, Wool E, Slaboda JC, Abrashkin KA, Rhodes K, … Norman GJ (2019). Care team perspectives and acceptance of telehealth in scaling a home-based primary care program: Qualitative study. JMIR Aging, 2(1), e12415. doi: 10.2196/12415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam K, Lu AD, Shi Y, & Covinsky KE (2020). Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA internal medicine, 180(10), 1389–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latus-Olaifa O, Norman GJ, Kurliand M, Slaboda JC, Abrashkin KA, Smith KL, … Rhodes K (2019). Not yet ready for prime time: Video visits in a home-based primary care program. Journal of the American Geriatrics Society, 67(10), 2202–2204. [DOI] [PubMed] [Google Scholar]
- Leff B, Weston CM, Garrigues S, Patel K, Ritchie C. Home-based primary care practices in the United States: current state and quality improvement approaches. J Am Geriatr Soc. 2015;63(5):963–969. [DOI] [PubMed] [Google Scholar]
- Nowell LS, Norris JM, White DE, & Moules NJ (2017). Thematic analysis: Striving to meet the trustworthiness criteria. International Journal of Qualitative Methods, 16(1), 1609406917733847. [Google Scholar]
- Ornstein KA, Leff B, Covinsky KE, et al. Epidemiology of the homebound population in the United States. JAMA Intern Med. 2015;175(7):1180–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornstein KA, Garrido MM, Bollens-Lund E, et al. Estimation of the incident homebound population in the US among older Medicare beneficiaries, 2012 to 2018. JAMA Intern Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper L, Michener A, & Kinosian B (2019). US House Call Practices in 2014: Mismatch of providers, practices, and patients. Paper presented at the Journal of the American Geriatrics Society. [Google Scholar]
- Ritchie CS, Leff B. Population health and tailored medical care in the home: The roles of home-based primary care and home-based palliative care. Journal of pain and symptom management. 2018;55(3):1041–1046. [DOI] [PubMed] [Google Scholar]
- Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, Lopez A, & Schillinger D (2011). Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc, 18(3), 318–321. doi: 10.1136/jamia.2010.006015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuchman M, Fain M, Cornwell T. The resurgence of home-based primary care models in the United States. Geriatrics (Basel, Switzerland). 2018;3(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shachar C, Engel J, & Elwyn G (2020). Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA, 323(23), 2375–2376. [DOI] [PubMed] [Google Scholar]
- SocioCultural Research Consultants, L. L. C. (2015). Dedoose Version 6.1.18, web application for managing, analyzing, and presenting qualitative and mixed method research data. In.
- Sterling MR, Dell N, Piantella B, Cho J, Kaur H, Tseng E, … Silva AF (2020). Understanding the workflow of home health care for patients with heart failure: challenges and opportunities. Journal of general internal medicine, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling MR, Tseng E, Poon A, Cho J, Avgar AC, Kern LM, … Dell N (2020). Experiences of home health care workers in New York City during the coronavirus disease 2019 pandemic: a qualitative analysis. JAMA internal medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong A, Sainsbury P, & Craig J (2007). Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. [DOI] [PubMed] [Google Scholar]
- Willink A, & DuGoff EH (2018). Integrating medical and nonmedical services-the promise and pitfalls of the CHRONIC Care Act. N Engl J Med, 378(23), 2153–2155. [DOI] [PubMed] [Google Scholar]
- Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, … Ferranti J (2020). Telehealth transformation: COVID-19 and the rise of virtual care. Journal of the American Medical Informatics Association, 27(6), 957–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.