Abstract
Context
Longitudinal qualitative research is an approach to research that entails generating qualitative data with the same participants over extended periods of time to understand their lived experiences as those experiences unfold. Knowing about dynamic lived experiences in medical education, that is, learning journeys with stops and starts, detours, transitions and reversals, enriches understanding of events and accomplishments along the way. The purpose of this paper is to create access points to longitudinal qualitative research in support of increasing its use in medical education.
Methods
The authors explore and argue for different conceptualisations of time: analysing lived experiences through time versus analysing lived experiences cross‐sectional or via 2‐point follow‐up studies and considering time as subjective and fluid as well as objective and fixed. They introduce applications of longitudinal qualitative research from several academic domains: investigating development and formal education; building longitudinal research relationship; and exploring interconnections between individual journeys and social structures. They provide an illustrative overview of longitudinal qualitative research in medical education, and end with practical advice, or pearls, for medical education investigators interested in using this research approach: collecting data recursively; analysing longitudinal data in three strands; addressing mutual reflexivity; using theory to illuminate time; and making a long‐term commitment to longitudinal qualitative research.
Conclusions
Longitudinal qualitative research stretches investigators to think differently about time and undertake more complex analyses to understand dynamic lived experiences. Research in medical education will likely be impoverished if the focus remains on time as fixed. Seeing things qualitatively through time, where time is fluid and the past, present and future interpenetrate, produces a rich understanding that can move the field forward.
Short abstract
Lived experiences in medical education, with their starts, stops, detours, transitions, and reversals, determine understanding of events. Longitudinal qualitative research offers a way to gain knowledge into these dynamic journeys.
1. INTRODUCTION
Longitudinal qualitative research (LQR) is an approach to research that entails generating qualitative data with the same participants for an extended time. The primary aim of LQR is to explore participants’ lived experiences in real time as these experiences unfold, in other words, to explore their journey. 1 , 2 Although a body of LQR exists, it has yet to make substantial in‐roads into medical education. 3 The purpose of this paper is to create access points to LQR in support of increasing its use in medical education.
Medical education is replete with cross‐sectional studies that focus on destinations, the place to which one is journeying: ‘Have medical students integrated their identities? What careers did they choose?’ While research questions like these could be in an LQR approach, LQR provides insights different from those acquired by asking participants at a single point in time to recall their journey. Research questions like, ‘How do medical students integrate their personal and professional identities over the course of clinical clerkships? How do medical trainees construct and reconstruct their careers as they move through training?’ capitalise on LQR’s capacity to speak to dynamic, lived experiences. Knowing about the journey, with its stops and starts, detours, transitions, and reversals, enriches understanding of events and accomplishments along the way. Knowing about the dynamic lived experience is particularly relevant in medical education due to the prolonged training required to enter the medical profession.
Nonetheless, few in medical education engage in LQR even though two of us have published short papers describing LQR. Bennett, Kajamaa and Johnston 3 introduce LQR to health professions educators as a valuable and flexible approach to exploring how and when change happens. Balmer and Richards 4 situate LQR among other qualitative research approaches and offer guiding principles for conducting LQR in medical education. In this article, we expand on our prior papers by exploring different conceptualisations of time that inform LQR and introducing applications of LQR from several academic domains. We also provide an illustrative overview of LQR in medical education and practical advice for those interested in using an LQR approach.
2. CONCEPTUALISATIONS OF TIME
In LQR, data are generated with the same individuals over an extended period to understand the dynamic, lived experiences of participants, as those experiences relate to the phenomenon of interest to the investigators. 1 , 4 This section explores key distinctions in thinking about time, as they apply to LQR: (a) through time, rather than over time, and (b) time as both fixed and fluid.
2.1. Through time
Different phrases are used colloquially to describe the passage of time, including over time and through time. The distinction between over vs through may seem inconsequential in casual conversation. However, when applied to research, these phrases carry important distinctions that are consequential because of differences in temporal perspective each term implies.
Over time carries connotations of a leap from one point in time to another. 1 , 5 For instance, interviews with medical students at the beginning and end of their clinical rotations might elicit stories of memorable peak in their journey. But these same interviews are unlikely to capture the not‐so‐memorable plateaus in between the peaks. Given this orientation, over time is not sufficient for LQR because it focuses on the destination, not the journey.
In contrast, through time carries the connotation of a crawling progression from one point in time to another to another. 1 , 5 Through time distinguishes LQR from cross‐sectional and two time point, follow‐up studies. The dynamic nature of participants’ lived experience (eg the stops and starts, detours, transitions and reversals of students’ progression through medical school) come to light when time is conceptualised as process. For example, Teunissen noted that individual trainees have unique personal experiences that shape their learning trajectory and are reified by practice. 6 This experience‐trajectory‐reification framework is grounded in the conceptualisation of through time rather than over time.
2.2. Time as fixed and time as fluid
Classical literature offers two Greek conceptualisations of time: chronos and kairos. Chronos is time in a fixed, objective and continuous sense. It is a way of conceptualising time as a quantity, the duration of a length of periodicity. 7 , 8 For example, medical school curricula are generally laid out week by week and medical students progress through training in a fixed sequence. Conversely, karios is time in a fluid, subjective and discontinuous sense. 7 , 8 It is a way of conceptualising time in which individual events, emotions and happenings are significant because of their place in sequences of circumstances, emotions and understandings. 7 For instance, experiences of shame in medical education haunt individuals across their career. They have flashbacks when their competence is questioned or when they feel burned out. 9 The past shame event is then very present.
Barbara Adam's 10 social analysis of time situates chronos and kairos in contemporary Western society. Like chronos, time is conceptualised as objective and fixed. It is embedded in clocks, timecards and calendars. Yet, everyday language sheds like on the complexity of time. People routinely speak of the ‘best time’ or ‘the worst of times’, that is, timing. Timing is idiosyncratic and context dependent. People speak of the phases of life or ‘growing old, that is, temporality. Temporality is the rhythm of time. And people speak of time ‘flying by’ or ‘standing still’, that is, tempo. Tempo is the pace and intensity of time. In sum, Adam offers different conceptualisations of time‐as‐fluid where, such as karios, time is subjective.
2.3. LQR and conceptualisations of time
All medical education research is steeped in specific conceptualisations of time that have impact on the research questions asked, the data generate that had, the analysis conducted and the insight generated. Research is structured and sequenced within a time‐as‐fixed framework. For instance, investigators build time into their research designs when they designate a timeframe for data collection or decide when to analyse data. But considerations of through time and time‐as‐fluid require different conceptualisations of time, which add complexity to the analysis but makes the findings more interesting. LQR investigators consider through time when they notice temporal patterns in their expanding LQR dataset. LQR investigators consider time‐as‐fluid when participants reflect on the past and reconstruct it in the light of recent experiences. If investigators fail to incorporate different conceptualisations of time into their research, insights about dynamic, lived experiences risk never being developed.
3. APPLICATIONS OF LQR
Investigators in other academic domains have applied LQR in ways that can inform medical education research. That said, traditions and the phenomena of interest in a given academic domain uniquely inform the use of LQR. Moreover, across academic domains, debates exist about what can be considered legitimate LQR research, how it should be defined and labelled, and if it is an approach, a methodology, a design, a sensibility or something else entirely. 11 , 12 , 13
In this section, we describe applications of LQR from three academic domains: education, clinical research and social science: investigating development and formal education, building longitudinal research relationships and exploring interconnections between individual journeys and social structures. We highlight lessons LQR investigators in medical education can learn from each application.
3.1. Investigating development and formal education
Investigators in education have used LQR to explore issues related to human development and formal education. Saldana's 5 approach to LQR—one focusing on practical questions that investigators can pose to LQR data—derived from his own experience in theatre education. Saldana's 5 approach starts with framing and descriptive questions that attend to more linear flows of events (ie time‐as‐fixed). It then moves to analytic, interpretive questions about how time impacts the phenomenon of interest. For example, framing questions (What is different from one wave of data to the next, and when does change occur?) and descriptive questions (What increases, decreases or remains constant through time?) lay the groundwork for more analytic and interpretive questions that consider time‐as‐fluid (What are conceptual rhythms through time? What is the through‐line of the story?). Taken together, framing, descriptive, analytic and interpretive questions can help investigators in medical education stay open to time‐as‐fixed and time‐as‐fluid.
3.2. Building longitudinal research relationships
Clinical researchers have used LQR to follow individuals representing specific patient populations. Calman, Brunton and Molassiotis 2 and Nevedal, Ayalon and Briller 14 share their LQR experience with oncology and geriatric patients, respectively. Richer data may be generated through time (versus over time) because of the deepening relationship between LQR investigators and participants. But generating rich data can unwittingly put participants at risk if they share personal details, feel compelled to continue or look to investigators for health‐related advice rather than health care providers. Investigators are not immune from risk; rich data can troublesome if they are unprepared to deal with distressing situations related to serious illnesses. Recommendations for building longitudinal relationships in clinical research contexts can be adapted by LQR investigators in medical education. For example, Calman, Brunton and Molassiotis 2 ending the LQR when the well‐being of either participants or investigators is in question.
3.3. Exploring interconnections between individual journeys and social structures
Investigators in social science (eg social work, social policy) have used LQR to illuminate the complex interconnections between individual journeys (micro) and social structures (macro). 15 , 16 , 17 While micro/macro could be considered an issue of scope not time, LQR investigators who follow individuals through time—year after year—find themselves detailing trajectories that do not occur in isolation but in the shadow of shared social structures. They can zoom in to analyse individual journeys and then zoom out to analyse social structures that, in turn, shape those journeys. For example, Hermanowicz 18 followed a cohort of physicists through different career stages in three types of academic institutions. Social structure within each institution (eg promotion and tenure criteria) shaped but did not predict career patterns. In fact, individual physicists deviated, at varying times and in different ways, from expected career patterns at their respective institutions.
4. EXAMPLES OF LQR FROM MEDICAL EDUCATION
In their review of LQR papers in the nursing literature, Smith‐Battle, Lorenz, Reangsing and Palmer 19 call for standardised terminology to ensure appropriate indexing for future systematic reviews. In preparing for this paper, we appreciated that conceptualisations of LQR differed and standardised terminology was lacking across the health professions literature. Therefore, we opted to narrow our review to medical education and create a targeted but inevitably incomplete collection of exemplars. Our collection is not intended to be a comprehensive, systematic appraisal, but an illustrative overview of LQR in medical education. To that end, we did not limit our overview to research labelled as LQR but included qualitative research that met the criteria we imposed: (a) involved serial rounds of qualitative data collection with the same group of participants; and (b) engaged in recursive data collection where participants looked back to their earlier narratives and imagined their future. Our intention was to identify how LQR, as defined by our criteria, has been harnessed by investigators in medical education. In the Spring 2020, one of us (DB) did a targeted search in PubMed with the assistance of a reference librarian. She added five papers from her personal collection of LQR that were not readily identifiable as longitudinal and recursive. For this illustrative overview, we included 19 papers. 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 We summarise study characteristics in Table S1 (see Appendix S1) and highlight several papers in this section.
Most examples of LQR in medical education that we found (12/19) were situated in medical school. Common foci of LQR were transitions, identity and socialisation in medical training. In terms of time‐as‐fixed, data were collected for an average of 34 months (range 6‐120 months). Sample sizes were routinely small, with an average of 18 participants (range 6‐29). One‐on‐one interviews were a data source for all but one LQR paper; audio diaries were sometimes used in conjunction with interviews. LQR datasets were often analysed via thematic analysis, template analysis or framework analysis.
Our overview of LQR examples in medical education illustrates temporal elements that LQR investigators must contend with: diachronic versus synchronic analysis, pre‐determined versus unbound time frames and handling time‐as‐fluid. Diachronic analysis considers all waves of data collection and occurs after all data are collected. Adema et al 37 took a diachronic approach in their LQR on social interactions and social relationships of clinical clerks. They collected data via longitudinal audio diaries, reviewed transcripts of audio diaries and then engaged in inductive and deductive analysis to understand the process of identity formation. In contrast, synchronic analysis is iterative. It entails analysing data after each wave of data collection and building on preliminary findings to inform future data collection and analysis. Taking a synchronic approach, Bolier et al 32 interviewed twelve medical students over 6 years to understand change in the process of emotional socialisation. In each wave of data collection, the interviewer reminded participants of what they discussed in previous interviews to investigate changes in how students were socialised through time.
Another temporal element is deciding when a study has reached an end. Nearly all of LQR papers, we reviewed occurred within pre‐determined time frames. For instance, Dube et al 22 and Babaria et al 27 invited students in their major clinical year to participate in LQR. These studies had clear start points and end points. In contrast, a few studies were ongoing, without an a priori end point. For example, Balmer and Richards 24 started a study with medical students in their first year of training but narrowed to a smaller cohort when they transitioned into residency. The authors continue to follow this cohort, publishing papers with different foci depending on the stage of training and phenomenon of interest. 24
Another temporal element is contending with time‐as‐fluid. Some investigators confronted time‐as‐fluid head on. For example, Gordon et al 23 confront time‐as‐fluid head on when they explored liminality; that is, participants’ lived experience of being between a trainee and a trained doctor. In this LQR, transition from trainee to trained doctor was not simply tied to a calendar (time‐as‐fixed). Rather, some participants preferred to occupy liminal spaces as they worked to make sense of developing their professional identities as full‐fledged, trained physicians. In contrast, Han et al 29 focused on the gap between medical students’ expectations for learning in clerkship and their actual learning experiences at mid‐point and after clerkships. Asking if expectations were met, rather than how expectations changed, circumvented time‐as‐fluid.
5. PEARLS FOR LQR IN MEDICAL EDUCATION
In this section, we share five pearls for investigators in medical education who want to conduct LQR. Our selection of pearls was shaped by our illustrative overview of the literature, and our conversations with investigators who have engaged in LQR or expressed interest in doing so. Different conceptualisations of time (through time or time‐as‐fluid) inform each pearl.
5.1. Collecting data recursively
Recursive data collection entails asking participants to reflect back on previously generated data and to imagine forward. 1 , 39 Asking participants to reflect back can elucidate how their present is shaped by their past and how their past shapes their future. Recursive data collection enables participants to narrate their own growth, with its own pace and rhythm (time‐as‐fluid). To be clear, interviews are not the only way collect data recursively; longitudinal audio diaries 21 , 23 , 25 , 28 , 40 and reflective writings 34 , 35 have also been used.
To conduct recursive interviews, investigators begin with main questions and follow‐up on prior responses to main questions (eg ‘When we talked last year, you described [ ] formative event. Where are you with that now? How do you anticipate that changing going forward, if at all?’) Responses to main questions that elicit peak experiences or trigger points can serve as milestones for individual journeys. 1 , 39 For example, Balmer et al 20 created I‐poems from responses to a main interview question that asked about peak experiences. Each participant's collection of I‐poems provided a window into a more nuanced understanding of their individual journey.
5.2. Analysing longitudinal data in three strands
In LQR, three strands of analysis—theme, case and through time—form a braid that fits into a conceptual framework to tell a cohesive story. 1 As with analysis in cross‐sectional qualitative research, themes are constructed within a wave of data collection. But in LQR, themes evolve and are constructed as data are generated through time. 41 For example, Stephens and colleagues 34 investigated how anatomy education, specifically donor dissection, shaped medical students’ perceptions of medical ethics. These authors reported thematic changes in perceptions of ethics through time; medical students, as a group, moved from dignity and personhood (wave 1), to more educational aspects of donor dissection (wave 2), to objectification of the donor and the need to learn anatomy through donor dissection (wave 3). Individual students had unique stories of how their perceptions changed, one of which served as an illustrative case. In sum, LQR helped these investigators conceptualise ethical perceptions as dynamic, not static and to appreciate how individual characteristics such as ancestry and religiosity impact ethical perceptions.
Longitudinal qualitative research is agnostic when it comes to how to analyse data. Some have used narrative analysis of data from longitudinal audio diaries to identify dominant discourses about what doctors should be, or interpretive phenomenological analysis to understand how new consultant physicians develop in their role as on‐call supervisors. 25 , 26 Regardless of how LQR investigators analyse data, it is a heavy lift attend to theme, case and time simultaneously. Creating three‐strand data displays can help investigators detect subtle, temporal patterns in coded data. In the example in Figure 1, Themes A (Identity construction) and B (Community formation) are comprised of three substantive, theoretical codes. Themes show similar temporal patterns for three participants, based on the frequency of code occurrence across six waves of data collection. Data in this three‐strand display could add support to LQR investigators hunch identity construction precedes community formation.
FIGURE 1.
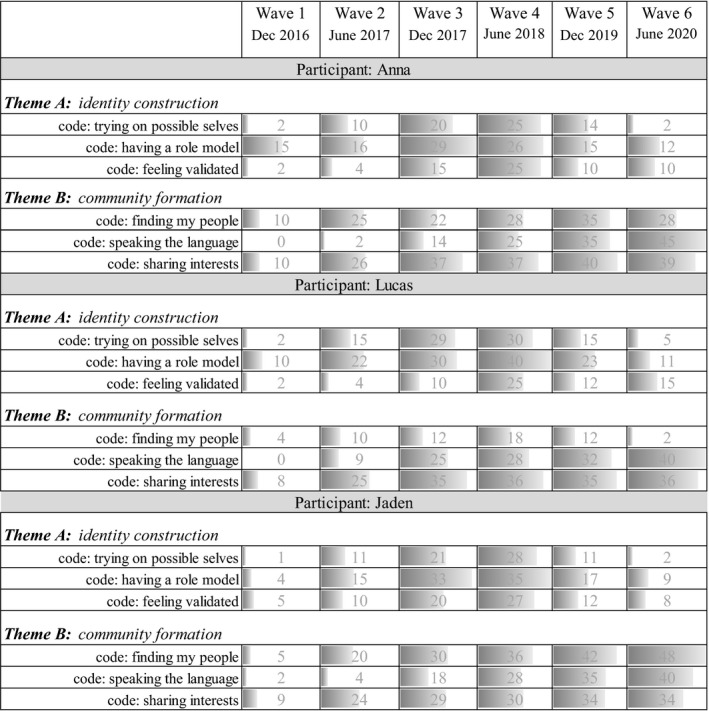
Data display for three‐strand analysis. Themes A (Identity construction) and Theme B (Community formation) are each comprised of 3 substantive, theoretical codes for three participants: Anna, Lucas and Jaden. Conditional formatting reflects the movement in the frequency of occurrence of codes through time. Note: The weight given to the presence of a topic at any given round of data collection can be based on a number of characteristics. For illustrative purposes, we have chosen frequency of codes in this figure
5.3. Addressing mutual reflexivity
As stated in the Introduction, the aim of LQR is to explore participants’ lived experiences as these experiences unfold through time. Much has been written about reflexivity in medical education, raising issues about the balance between authentic representation and confidentiality, potential power dynamics and more. 42 , 43 , 44 , 45 , 46 These issues are pertinent to LQR and have been addressed by LQR investigators (eg team reflexivity as described by Stephens, Rees and Lazarus 34 , 35 ). But another dimension of reflexivity has not been addressed: the dynamic, lived experiences of investigators and their own change through time. Epiphanies and evolution in investigators’ understanding (ie their karios moments) should be acknowledged and accommodated—not viewed as bias or messy research design. For instance, LQR investigators may start with a theory that positions individuals as agents of constructing their own identity. But these same investigators may shift to use critical theory as they are sensitised to gender inequity by the #MeToo movement and come to recognise that participants who identify as female consistently push back on constraining, gendered and social structures.
5.4. Using theory to illuminate time
Theories can deepen understanding of perplexing problems. However, not all theories are expansive enough to accommodate different conceptualisations of time, LQR needs theories that illuminate change through time and attend to the ways that the past shapes the present and the future. For example, Balmer, Rosenblatt and Boyer (unpublished data) used Wenger's 47 , 48 social learning theory as a framework for their 4‐year LQR of physicians in a graduate programme in medical education. Wenger's Community of Practice 47 was a sufficient analytic lens for data from the first 2 years of the LQR when physicians were in the graduate programme, itself a community of practice. But it was insufficient for post‐graduation data in the later 2 years of the LQR. Balmer and colleagues shifted to Landscapes of Practice 48 , 49 , 50 even as participants’ shifted in ways they engaged with different communities comprising their own landscape of practice. In sum, LQR that used socio‐cultural theory as an interpretive lens illuminated change through time in how participants navigated their landscape of practice.
5.5. Making a long‐term commitment
Longitudinal qualitative research is a commitment if nothing else. Funding for medical education research may stifle the pursuit of longitudinal studies. However, taking a few minutes after data collection to elicit participants’ perspectives on real‐time concerns such as programme implementation or evaluation can be an effective way to sustain LQR in the context of medical education. For example, an LQR that follows postgraduate medical trainees over 2 years could generate useful feedback for programme directors about a new implicit bias curriculum, unrelated to the question driving the LQR.
Funding aside, recursive data collection can create a safe space for reflection by building trust, showing respect for participants’ journey, and including participants as conversational partners. 4 Access to a safe space can be a compelling reason for participants to stay involved in LQR. Monrouxe and Sweeney's 40 experience is a telling example. In their LQR using audio diaries, they observed that ‘medical students preferred to talk to others who they felt would understand, and with whom they had developed a trusting relationship (eg peers, senior colleagues, and us as researchers)’. 40 (p.21)
6. CONCLUSION
Longitudinal qualitative research is an approach to research that stretches medical education investigators think differently about time and the dynamic lived experiences as they unfold through time. Research in medical education will likely be impoverished if the focus remains on time as fixed and quantifiable. Seeing things qualitatively though time, where time is fluid and the past, present and future interpenetrate, produces a rich understanding that can move the field forward. Applications of LQR in other academic domains, as well as illustrative examples from medical education, can be instructive. These applications and examples, along with Pearls for LQR, provide access points to LQR. Certainly, LQR demands significant time and effort. Nonetheless, investing time and effort in LQR opens the door to a depth of insight that is unique to this research approach.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Dorene Balmer conceptualised the paper, wrote the first draft and led the writing team. Lara Varpio, Deidre Bennett and Pim Teunissen made substantial contributions to paper, both conceptually and in editing/revisions; they approved the final draft that Dorene Balmer submitted.
ETHICAL APPROVAL
Not applicable.
DISCLAIMER
The views expressed herein are those of the authors and do not necessarily reflect those of the Uniformed Services University of the Health Sciences, the United States Department of Defense or other federal agencies.
Supporting information
Appendix S1
ACKNOWLEDGEMENTS
None.
Balmer DF, Varpio L, Bennett D, Teunissen PW. Longitudinal qualitative research in medical education: Time to conceptualize time. Med Educ. 2021;55(11):1253–1260. 10.1111/medu.14542
REFERENCES
- 1. Neale B. What is Qualitative Longitudinal Research? London: Bloomsbury Academic; 2019. [Google Scholar]
- 2. Calman L, Brunton L, Molassiotis A. Developing longitudinal qualitative designs: lessons learned and recommendations for health services research. BMC Med Res Methodol. 2013;13:14. 10.1186/1471-2288-13-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bennett D, Kajamaa A, Johnston J. How to … do longitudinal qualitative research. Clin Teach. 2020;17:489‐492. [DOI] [PubMed] [Google Scholar]
- 4. Balmer DF, Richards BF. Longitudinal qualitative research in medical education. Perspect Med Educ. 2017;6:306‐311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Saldana J. Longitudinal Qualitative Research: Analyzing Change through Time. Walnut Creek, CA: AltaMira Press; 2003. [Google Scholar]
- 6. Teunissen PW. Experience, trajectories, and reifications: an emerging framework of practice‐based learning in healthcare workplaces. Adv Health Sci Educ Theory Pract. 2015;20:843‐856. [DOI] [PubMed] [Google Scholar]
- 7. Smith J. Time, times, and the 'right time': "chronos" and "kairos". Monist. 1969;53:1‐13. [Google Scholar]
- 8. Kumagai AK, Naidu T. On time and tea bags: chronos, kairos, and teaching for humanistic practice. Acad Med. 2020;95:512‐517. [DOI] [PubMed] [Google Scholar]
- 9. Bynum WE, Artino AR, Uijtdehaage S, Webb AMB, Varpio L. Sentinel emotional events: the nature, triggers, and effects of shame experiences in medical residents. Acad Med. 2019;94:85‐93. [DOI] [PubMed] [Google Scholar]
- 10. Adam B. Timewatch: A Social Analysis of Time. Oxford, UK: Blackwell Publishers; 1995. [Google Scholar]
- 11. McCoy L. Longitudinal qualitative research and interpretative phenomenological analysis: philosophical connections and practical considerations. Qual Res Psych. 2017;14:442‐458. [Google Scholar]
- 12. Thomson R, Plumridge L, Holland J. Longitudinal qualitative research: a developing methodology. Int J Soc Res Methodol. 2003;6:185‐187. [Google Scholar]
- 13. Thomson R, McLeod J. New frontiers in qualitative longitudinal research: an agenda for research. Int J Soc Res Methodol. 2015;18:243‐250. [Google Scholar]
- 14. Nevedal AL, Ayalon L, Briller SH. A qualitative evidence synthesis review of longitudinal qualitative research in gerontology. Gerontol. 2019;59:e791‐e801. [DOI] [PubMed] [Google Scholar]
- 15. Plumridge L, Thomson R. Longitudinal qualitative studies and the reflexive self. Int J Soc Res Methodol. 2003;6:213‐222. [Google Scholar]
- 16. Holland J, Thomson R, Henderson S. Qualitative Longitudinal Research: A Discussion Paper. London, UK: London South Bank University; 2006. [Google Scholar]
- 17. Neale B, Flowerdew J. Time, texture and childhood: the contours of longitudinal qualitative research. Int J Soc Res Methodol. 2003;6:189‐199. [Google Scholar]
- 18. Hermanowicz J. Lives in Science: How Institutions Affect Academic Careers. Chicago, IL: University of Chicago Press; 2009. [Google Scholar]
- 19. SmithBattle L, Lorenz R, Reangsing C, Palmer JL, Pitroff G. A methodological review of qualitative longitudinal research in nursing. Nurs Inq. 2018;25:e12248. 10.1111/nin.12248 [DOI] [PubMed] [Google Scholar]
- 20. Balmer D, Devlin M, Richards B. Understanding the relation between medical students' collective and individual trajectories: an application of habitus. Perspect Med Educ. 2017;6:36‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ottrey E, Rees CE, Brock T, Monrouxe LV, Morphet J, Palermo C. Exploring healthcare graduates' conceptualisations of preparedness for practice: a longitudinal qualitative research study. Med Educ. 2021;55(9):1078‐1090. 10.1111/medu.14475 [DOI] [PubMed] [Google Scholar]
- 22. Dubé TV, Schinke RJ, Strasser R, Couper I, Lightfoot NE. Transition processes through a longitudinal integrated clerkship: a qualitative study of medical students' experiences. Med Educ. 2015;49:1028‐1037. [DOI] [PubMed] [Google Scholar]
- 23. Gordon L, Rees CE, Jindal‐Snape D. Doctors' identity transitions: choosing to occupy a state of 'betwixt and between'. Med Educ. 2020;54:1006‐1018. [DOI] [PubMed] [Google Scholar]
- 24. Balmer DF, Teunissen PW, Devlin MJ, Richards BF. Stability and change in the journeys of medical trainees. Acad Med. 2020. Online ahead of print. 10.1097/ACM.0000000000003708 [DOI] [PubMed] [Google Scholar]
- 25. Monrouxe LV. Negotiating professional identities: Dominant and contesting narratives in medical students' longitudinal audio diaries. Current Narratives. 2009;1:41‐59. [Google Scholar]
- 26. Westerman M, Teunissen PW, Fokkema JP, et al. New consultants mastering the role of on‐call supervisor: a longitudinal qualitative study. Med Educ. 2013;47:408‐416. [DOI] [PubMed] [Google Scholar]
- 27. Babaria P, Abedin S, Berg D, Nunez‐Smith M. "I'm too used to it": a longitudinal qualitative study of third year female medical students' experiences of gendered encounters in medical education. Soc Sci Med. 2012;74:1013‐1020. [DOI] [PubMed] [Google Scholar]
- 28. Gordon L, Jindal‐Snape D, Morrison J, et al. Multiple and multidimensional transitions from trainee to trained doctor: a qualitative longitudinal study in the UK. BMJ Open. 2017;7:e018583. 10.1136/bmjopen-2017-018583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Han H, Roberts NK, Korte R. Learning in the real place: medical students' learning and socialization in clerkships at one medical school. Acad Med. 2015;90:231‐239. [DOI] [PubMed] [Google Scholar]
- 30. Smith‐Han K, Martyn H, Barrett A, Nicholson H. That's not what you expect to do as a doctor, you know, you don't expect your patients to die." Death as a learning experience for undergraduate medical students. BMC Med Educ. 2016;16:108. 10.1186/s12909-016-0631-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Balmer D, Richards B, Varpio L. How students experience and navigate transition in undergraduate medical education: an application of Bourdieu's theoretical model. Adv Health Sci Educ Theory Prac. 2015;20:1073‐1085. [DOI] [PubMed] [Google Scholar]
- 32. Bolier M, Doulougeri K, de Vries J, Helmich E. 'You put up a certain attitude': a 6‐year qualitative study of emotional socialisation. Med Educ. 2018;52:1041‐1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Anandarajah G, Roseman J, Lee D, Dhandhania N. A 10‐year longitudinal study of effects of a multifaceted residency spiritual care curriculum: clinical ability, professional formation, end of life and culture. J Pain Symptom Manage. 2016;52:859‐872 e1. 10.1016/j.jpainsymman.2016.06.006 [DOI] [PubMed] [Google Scholar]
- 34. Stephens GC, Rees CE, Lazarus MD. How does donor dissection influence medical students' perceptions of ethics? A cross‐sectional and longitudinal qualitative study. Anat Sci Educ. 2019;12:332‐348. [DOI] [PubMed] [Google Scholar]
- 35. Stephens GC, Rees CE, Lazarus MD. Exploring the impact of education on preclinical medical students’ tolerance of uncertainty: a qualitative longitudinal study. Adv Health Sci Educ. 2021;26(1):53‐77. 10.1007/s10459-020-09971-0 [DOI] [PubMed] [Google Scholar]
- 36. Pratt M, Rockmann K, Kaufmann J. Constructing professional identity: the role of wok and identity learning cycles in the customization of identity among medical residents. Acad Manage J. 2006;49:235‐262. [Google Scholar]
- 37. Adema M, Dolmans D, Raat JAN, Scheele F, Jaarsma ADC, Helmich E. Social interactions of clerks: the role of engagement, imagination, and alignment as sources for professional identity formation. Acad Med. 2019;94:1567‐1573. [DOI] [PubMed] [Google Scholar]
- 38. Bierer SB, Dannefer EF. The learning environment counts: longitudinal qualitative analysis of study strategies adopted by first‐year medical students in a competency‐based educational program. Acad Med. 2016;91:S44‐S52. [DOI] [PubMed] [Google Scholar]
- 39. Hermanowicz JC. The longitudinal qualitative interview. Qual Sociol. 2013;36:189‐208. [Google Scholar]
- 40. Monrouxe LV, Sweeney K. Between two worlds. In: Figley C, Huggard P, Rees C, eds. First Do No Self Harm: Understanding and Promoting Physician Stress Resilience. Oxford Scholarship Online; 2013. 10.1093/acprof:oso/9780195383263.001.0001 [DOI] [Google Scholar]
- 41. Grossoehme D, Lipstein E. Analyzing longitudinal qualitative data: the application of trajectory and recurrent cross‐sectional approaches. BMC Res Notes. 2016;9:136. 10.1186/s13104-016-1954-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Reid AM, Brown JM, Smith JM, Cope AC, Jamieson S. Ethical dilemmas and reflexivity in qualitative research. Perspect Med Educ. 2018;7:69‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Halman M, Baker L, Ng S. Using critical consciousness to inform health professions education: a literature review. Perspect Med Educ. 2017;6:12‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. O'Brien BC, Balmer DF, Maggio LA. Finding our way through shades of gray: 6 virtues to guide researchers in planning, conducting, and writing up research. J Grad Med Educ. 2017;9:555‐559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Barrett A, Kajamaa A, Johnston J. How to … be reflexive when conducting qualitative research. Clin Teach. 2020;17:9‐12. [DOI] [PubMed] [Google Scholar]
- 46. Baker L, Phelan S, Snelgrove R, Varpio L, Maggi J, Ng S. Recognizing and responding to ethically important moments in qualitative research. J Grad Med Educ. 2016;8:607‐608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wenger E. Communities of Practice: Learning, Meaning, and Identity. New York, NY: Cambridge University Press; 1998. [Google Scholar]
- 48. Wenger‐Trayner E, Fenton‐O'Creevy M, Hutchinson S, Kubiak C, Wenger‐Traynor B. Learning in Landscapes of Practice. New York, NY: Rutledge; 2015. [Google Scholar]
- 49. Omidvar O, Kislov R. The evolution of the communities of practice approach toward knowledgeability in a landscape of practice: an interview with Etienne Wenger‐Trayner. J Manage Inquiry. 2014;23:266‐275. [Google Scholar]
- 50. Hodson N. Landscapes of practice in medical education. Med Educ. 2020;54:504‐509. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1


