Abstract
We present epidemiological data to examine trends in COVID-19 incidence, morbidity and mortality in Israel as well as changes in vaccine effectiveness, and discuss the impact of the delta variant and the third, “booster”, vaccine.
A retrospective-archive study was conducted from February 27th 2020 to October 16th, 2021. Data were obtained from the Israeli Ministry of Health's open COVID 19 database, including PCR-confirmed cases, number hospitalized - including severe cases, death rate, all by age and vaccination status, case fatality rate and changing effectiveness of the vaccine.
After three COVID waves, confirmed cases rose from under 30 new daily cases in mid-June to a high of 11,000 in early September 2021. Severe hospitalized cases and death rates were lower than in previous waves and largely restricted to those not fully vaccinated. In the first three months of the vaccination campaign, non-vaccinated population demonstrated much higher morbidity rates. Four months after vaccination began, this gap was attenuated, with low rates of infection and hospitalization in all groups. The gap was regained following uptake of the third vaccine. Data from the fourth wave show reduced hospitalizations and mortality compared to previous waves and suggest that this may be related to high vaccine coverage. These trends suggest that countries with high vaccination might adopt a more permissive approach towards COVID even in the face of new variants.
Keywords: COVID-19, Infectious diseases, Vaccination, Delta, Variant, Israel, Vaccine effectiveness
1. Introduction
Twelve months after the first COVID-19 cases were reported in Wuhan, China (Gao et al., 2020) the first COVID vaccine was authorized by the US FDA for emergency use and many countries initiated national vaccine drives (Oliver et al., 2020).
In Israel, the Pfizer mRNA COVID-19 vaccine BNT162b2 was available from December 2020 as the only vaccine brand, and was offered first to healthcare workers, the elderly (aged 60+) and at-risk populations with underlying disease. On February 20, 2021 vaccination was opened up to the entire adult (16+) population and in June 2021, it was offered for the first time to 12–15 year olds. Individuals recovered from COVID infection were given a single vaccine dose. In the first three months of the vaccination campaign, Israel had the largest share of the population having received at least one vaccine dose (Coronavirus (COVID-19) Vaccinations, 2021). As of 6th July, 66% of the Israeli population (total population: 9.354 million people) (Population of Israel on the Eve of 2021, 2021) has been fully vaccinated and more than 90% of those aged 60+ have received both vaccine doses.(https://datadashboard.health.gov.il/COVID-19/general, n.d.)
Following three COVID waves between March 2020 and March 2021, the national vaccination drive resulted in a drop in infections, allowing gradual removal of almost all public health measures by May–June 2021. A feeling of “liberation” disseminated among the Israeli public. However, having reduced in mid-May down to less than 30 new daily cases, in June the daily number of new confirmed cases began to rise. As of July 2021, the new Delta COVID variant was estimated to account for more than 90% of new cases, similar to the UK where this variant contributed to the recent increase in new cases since June 2021 (O'Dowd, 2021).
This study presents epidemiological data to examine trends in COVID-19 incidence, morbidity and mortality in Israel since the beginning of the vaccination campaign, and discusses the impact of the new delta variant.
2. Methods
A retrospective-archive study was conducted in Israel from February 27th (the patient zero case) to October 16, 2021. Data were obtained from the Israeli Ministry of Health's (MOH) open COVID 19 database, (https://data.gov.il/dataset/covid-19).
We present here data on new confirmed COVID-19 cases (positive PCR test in the last 24 h), severe disease (including critically ill patients) (Marshall et al., 2020) among those hospitalized with COVID-19, number of deaths from COVID-19 and reproduction number (R), calculated as the mean number of infections resulting from a single case, and reported with an average 10 day lag (Dietz, 1993). The latter index tracks trends of viral spread at the national level, in addition to daily confirmed cases.
In addition, we present weekly number and rate of confirmed cases, hospitalizations, and deaths by vaccination status (vaccinated with 1 dose, 2 dose2, 3 doses and non-vaccinated). Non-vaccinated were defined as those who had not received any vaccine (or were less than 1 week after their first dose). Fully vaccinated were defined as those with two doses, and at least a week following the second dose, up to September 292,021, and after this date those with three doses (and at least a week following the last dose). Partially vaccinated were defined as those with one vaccine (up to late September 2021) or two doses from September 29, 2021 and on. These data were collated and presented in graph form, detailing morbidity between 20/12/20–16/10/21.in people who had received the first, second and third vaccine doses.
Number of deaths by age and vaccination status is an approximation since periods with less than 5 deaths were noted in the database as <5 which we substituted for n = 3 which could be an overestimation.
Case fatality rate (CFR) was calculated from MOH data as the number of deaths divided by the number of confirmed cases (Yang et al., 2020).
Rates of infection and severe disease were calculated from MOH data and presented per 100,000 in vaccinated and unvaccinated populations, with significant difference between rates compared using chi-squared test.
3. Results
To date there were four waves of COVID-19 in Israel, the first in March–April 2020, the second beginning at the end of June 2020 until October 2020, and the third, with higher rates of infection compared with the first two waves, beginning December 2020 (Fig. 1a). By May 2021, confirmed COVID-19 cases were down to less than 30 daily new cases. However, beginning in June 2021, a fourth wave began with new infections starting to rise, reaching a peak of 11,300 new daily cases in early September 2021. Rate of positive tests out of all those tested (Fig. 1b) shows a lower proportion of positive tests in the fourth, compared to the peaks of earlier waves.
Fig. 1.
Daily COVID-19 activity, February 12, 2020 to October 16, 2021.
1a: Daily numbers of confirmed COVID-19 cases and 7-day moving average.
1b: Daily percent of positive tests.
While daily numbers of newly diagnosed infections reached an all-time high in the fourth wave, severe hospitalized cases, which did climb in September to a cumulative number around 600 or around 8 per 100,000 population, did not reach the same levels as previous waves (13 per 100,000 population). (Fig. 2 ).
Fig. 2.
Severe hospitalized cases per 100,000 population, October 23, 2020 to October 21, 2021.
The reproduction rate, which was below 1.0 during March–May 2021, began to rise in mid-June, up to 2.47 on the 15th June and decreased to 1.43 towards the end of June, falling below 1 from mid-September 2021 (not shown).
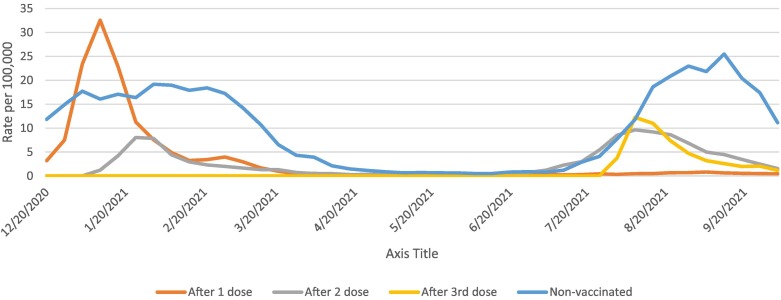
Fig. 3 presents data on population rate of weekly confirmed cases (Fig. 3a), hospitalizations (Fig. 3b), and deaths (Fig. 3c) by vaccination status, dating from the beginning of the vaccination drive (January 2021) till mid- October 2021. In the first three months after the start of the vaccination campaign, there was a significant gap in both confirmed cases, hospitalizations and mortality between vaccinated and non-vaccinated populations, with much higher rates in non-vaccinated. At week 16, four months after vaccination drive began, this gap was attenuated, with low rates of infection and hospitalization in both vaccinated and non-vaccinated. COVID deaths also reduced dramatically. With the advent of the fourth delta wave, confirmed cases rose in both vaccinated and non-vaccinated populations but the gap re-emerged with much higher case rates, hospitalizations and deaths in non-vaccinated or partially vaccinated from late August–September onwards (with the beginning of the third booster vaccination campaign).
Fig. 3.
COVID-19 activity and outcomes by vaccination status, 20/12/2020–16/10/2021.
3A. Rate of confirmed cases per 100,000 population.
3B: Rate of hospitalizations per 100,000 population.
3C: Rate of deaths per 1,00,000 populations.
Following high vaccination coverage in the adult population, the largest proportion of non-vaccinated people are therefore now (as of October 2021) children, with those under 12 years of age still ineligible for vaccine uptake during the study period. The vaccine was approved for children aged 12–15 on 21st June 2021. This explains the highest rate of confirmed cases in 0–19 year olds, as seen in Fig. 4a , however hospitalizations and deaths remain highest in the older age-groups (Figs. 4b&4c). The highest number and rate of deaths in all age groups occurred in non-vaccinated people (Fig. 4c). Mortality related to COVID throughout the pandemic period was very low in children and young people (Fig. 4c&4d). Furthermore, case fatality rate (CFR) was 0.61% over the whole period in Israel (8029 deaths out of 1,319,902 cases), but during the last month (20 September-20 October), CFR decreased to 0.052% of confirmed cases (421 out of 80,515 cases) (Fig. 4d) and remained extremely low in under-60s.
Fig. 4.
Confirmed cases, hospitalizations and deaths by vaccination status and age group, 20/12/2020–16/10/2021.
4a. Cumulative number of confirmed cases.
4b. Rate of hospitalizations per 100,000 confirmed cases.
4c. Number of cumulative deaths.
4d. Case fatality rate.
Detailed monthly data for the study period is presented in Table 1 , which demonstrates rates of severe disease that were 6 times higher for non-vaccinated, compared with vaccinated individuals, in February 2021 (13.09 and 2.18 cases per 100,000 vaccinated and non-vaccinated population, respectively). In May 2021 the gap narrowed, and in June rates decreased in both groups to almost equalize (0.81 and 0.14 per 100,000 population of vaccinated and non-vaccinated, respectively). In August this gap increased again to be 5 times higher in the unvaccinated population. In late September the gap further increased, with rates among vaccinated being 6 times lower compared with non-vaccinated or partially vaccinated (2.69 and 17.54 per 100,000 population, respectively) (Table 1). Rate of infection followed the same pattern, being much higher in the unvaccinated population, with the gap reducing in June–July, and increasing again from August to October.
Table 1.
New cases, rate of infection and severe disease by vaccination status.
| Vaccinated |
Unvaccinated (or out of date) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Period | No. vaccinated | Total new confirmed cases | Rate of infection/100,000 | Severe disease⁎ | Rate of severe disease/100,000 | No. unvaccinated | Total new confirmed cases | Rate of infection/100,000 | Severe disease⁎ | Rate of severe disease/100,000 | P value⁎⁎ for infection | P value⁎⁎ for severe disease |
| 1–28/2 | 3,341,059 | 3129 | 93.6 | 73 | 2.18 | 6,012,941 | 106,928 | 1778.3 | 787 | 13.09 | <0.0001 | <0.0001 |
| 1–31/3 | 4,719,680 | 2445 | 51.8 | 53 | 1.12 | 4,634,320 | 43,844 | 946.1 | 539 | 11.63 | <0.0001 | <0.0001 |
| 1–30/4 | 5,051,097 | 586 | 11.6 | 39 | 0.77 | 4,302,903 | 4166 | 96.8 | 274 | 6.37 | <0.0001 | <0.0001 |
| 1–31/5 | 5,138,842 | 189 | 3.7 | 10 | 0.19 | 4,215,158 | 729 | 17.3 | 86 | 2.04 | <0.0001 | <0.0001 |
| 1–30/6 | 5,174,777 | 942 | 18.2 | 7 | 0.14 | 4,179,223 | 1376 | 32.9 | 34 | 0.81 | <0.0001 | <0.0001 |
| 1–31/7 | 5,383,082 | 16,242 | 301.7 | 93 | 1.73 | 4,029,921 | 15,473 | 383.9 | 99 | 2.46 | <0.0001 | 0.0143 |
| 1–31/8 | 5,474,113 | 64,493 | 1178.1 | 164 | 2.99 | 3,938,890 | 129,465 | 3286.8 | 612 | 15.54 | <0.0001 | <0.0001 |
| 1–30/9 | 5,616,464 | 38,749 | 689.9 | 151 | 2.69 | 3,796,539 | 159,403 | 4198.6 | 666 | 17.54 | <0.0001 | <0.0001 |
| 1–16/10 | 5,681,551 | 3496 | 61.5 | 75 | 1.32 | 3,731,452 | 27,751 | 743.7 | 512 | 13.72 | <0.0001 | <0.0001 |
Peak number hospitalized with severe COVID disease per period.
Chi-squared test of significance.
4. Discussion
Israel has experienced four waves of the COVID-19 pandemic, with multiple lockdowns, a death toll of over 8000, and significant economic ramifications. Having almost eradicated COVID in April 2021, cases began to rise in June, reaching the peak of a fourth wave in September 2021. However, while an increase in confirmed cases and a rising R rate was reported, the rate of severe hospitalized cases and deaths was lower than in previous waves.
Indeed, Ministry of Health figures show that the effectiveness of the Pfizer vaccine against the new delta variant, reduced with regard to preventing infection, but remained high against severe disease and death. On 6th July 2021, the MOH published data on the changing effectiveness of the 2-dose Pfizer vaccine, demonstrating high effectiveness that decreased with the advent of the Delta variant in Israel (first documented in Israel on 16th April 2021) (MOH, n.d.). Effectiveness against infection reduced from around 95% in February–May down to 64% in June 2021. However, effectiveness against hospitalization remained relatively high, with a small decrease from 98% in March–May to 93% in June 2021. Effectiveness rates for severe disease among hospitalized patients showed a similar, small decrease from March–May to June. Other studies also showed reduced effectiveness of vaccines against the delta variant, particularly following a single dose (Bernal et al., 2021).
While in previous waves a rising number of confirmed cases was associated with a parallel increase in hospitalizations and deaths, the rate of severe cases and deaths was lower than in previous waves. Back in February 2021, there was a stark difference between rate of severe disease between vaccinated and non-vaccinated individuals, but this gap gradually closed by June 2021 and re-opened in August 2021.
A similar pattern has been seen in the UK, with a steeply rising infection rate in June 2021, but a much smaller rise in hospitalizations, and fewer new deaths compared to previous waves, figures which led the British government to decide on gradually releasing most restrictions during July–August 2021 (BBC News, 2021). A risk assessment of the delta variant conducted by Public Health England reported a high risk of elevated transmissibility (Health England P., 2021), compared to the alpha strain, but its analysis revealed that two doses of vaccine gave a high degree of protection against hospital admission, estimated to be more than 90% (O'Dowd, 2021). The UK has also reached a high proportion of vaccinations per population compared to other countries (Coronavirus (COVID-19) Vaccinations, 2021). While the UK has now reached higher rates of vaccination, compared with Israel, this is because it has a higher mean age, while around a third of Israel's population is under 18, having a smaller population eligible for the vaccine. Of note, Israel achieved high vaccine coverage earlier than most countries (60% of the population who received the first dose by March 22), while Canada and the UK achieved this threshold on June 4, 2021 (Coronavirus (COVID-19) Vaccinations, 2021). Reduced effectiveness of the vaccine against infection may be associated with waning immunity and falling antibody levels in a population that was vaccinated over 6 months ago (Levin et al., 2021). US data, published by the Center for Disease Control and Prevention, also demonstrated a reduction of the gap in number of confirmed COVID cases between fully vaccinated and unvaccinated population in June–July 2021 and widening of the gap in August–September 2021 (CDC, 2021).
Increased numbers of confirmed COVID cases in children and younger population is expected since the majority of the adult Israeli population are fully vaccinated. In the past month (30/9–30/10/21) 58% of new cases were among 0–19 year olds. This might partially explain why the recent increase in new infections has not been matched by an increase in severe disease or mortality, since COVID is known to cause greatest morbidity in older age-groups (Starke et al., 2020). For the vast majority of children, COVID presents a minimal threat. Furthermore, the small risk in children of severe disease has become even smaller in recent months, with the rate of children under 10 being ventilated due to COVID being 0.008% since the start of the pandemic, reducing to 0.004% in the last 3 months; and the case fatality rate reducing from 0.002% to 0.0008% (Israel Ministry of Health COVID-19 dashboard, 2021). This may be due to better recognition of the disease and better treatment options. Despite the lower severity of the acute-phase COVID among children (Hertting, 2021), questions remain regarding the prevalence of long COVID in children, however according to some reports reported symptoms do not seem to exceed the prevalence of symptoms such as headache or cough among the pediatric population (Bhopal and Absoud, 2021).
The disappearing gap in infections and severe disease between vaccinated and non-vaccinated populations, three months after the national vaccine drive began, suggested that the high rate of population vaccination succeeded in giving protection to non-vaccinated people, and overall reduction of the number of infections. However once cases began to rise again with the fourth wave, the gap opened up again with a higher rate of severe cases and deaths among those unvaccinated or partially vaccinated population. Following the sharp reduction in cases that marked the end of the third pandemic wave, most restrictions and public health measures were removed in Israel in April/May 2021 once cases dropped, including revoking the need for masks in indoor spaces. However several restrictions, including the “Green pass” incentives for those vaccinated, were reintroduced in September 2021 given the rising R and number of confirmed cases. In an attempt to reduce quarantine of whole classes in October 2021, the ‘green classroom’ system was trialed, whereby instead of sending a whole class into quarantine following one confirmed cases, children complete daily tests but continue to go to school. COVID risk should also be placed in the context of other viral diseases. While prior to the vaccination campaign, CFR for COVID was highr (0.77% in Israel, 2.2% reported worldwide) (COVID-19 Map, 2020-2021), it has currently decreased in Israel to 0.36% (last 3 months). For comparison, a systematic review of case fatality risk from H1N1 influenza estimated risk within the range of 0.1% - 5% (Wong et al., 2013).
The delta variant hit Israel when the majority of the population at risk was already vaccinated, however since mass vaccination of this population took place 5–6 previously, in January–March 2021, questions arose surrounding waning levels of antibodies and how long the vaccine gives protection for. The Israeli data raised concerns on whether a third, booster dose, of the Pfizer and many other vaccines, is required, even earlier than previously thought. On 8th July, Pfizer issued a written statement that, based on “real world evidence released from the Israel Ministry of Health”, it is developing a COVID booster shot to target the highly transmissible delta variant (CNBC, 2021). This booster was launched in Israel on July 30, 2021, for people aged 60+ who have received the second vaccine dose at least 5 months before. Those who received the third dose indeed demonstrated lower rates of infection, hospitalization, severe disease and death (Bar-On et al., 2021, Barda et al., 2021). Indeed studies have identified people at risk of breakthrough infections even following two doses of the vaccine to include frail older adults and those in deprived areas (Antonelli et al., 2021) – these groups may be good candidates for a booster.
Limitations that should be considered are that indices of disease severity, such as CFR, are dependent on the number of cases identified, and asymptomatic cases of COVID have been widely reported, resulting in over-estimation of CFR. Furthermore, it should be noted that individuals vaccinated with a single dose may have recovered from COVID-19 since this group was eligible to receive just a single dose, yet may have similar levels of immunity to double dosed individuals.
5. Conclusions
While Israel experienced a serious fourth wave, the vast majority of severe cases and deaths are now occurring in unvaccinated or not fully vaccinated individuals. Based on current data, continued effectiveness of the Pfizer vaccine – including the booster dose - against severe disease including the delta variant, and mild illness in the vast majority of cases, it is suggested that policy-makers in countries with high vaccination rates should now base their decisions regarding public health measures on rates of severe illness and mortality, and not just on the infection rate or R number. The situation has changed from the early waves of the COVID-19 pandemic, where the older population was at significant risk, and there was genuine concern about overwhelming the healthcare system. In the current circumstances of highly vaccinated risk groups, and a lower case fatality rate, approaches towards COVID might take a different perspective. Vaccines, including the booster, should continue to be made widely available, and trends must continue to be monitored, so that informed decisions can be made about the safe and timely lifting of restrictions.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
None.
References
- Antonelli M., Penfold Rose S., Bmbc Jordi Merino, P, Carole H Sudre P, Erika Molteni P, Sarah Berry P. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID symptom study app: a prospective, community-based, nested, case-control study. Lancet. September 1, 2021:1–13. doi: 10.1016/S1473-3099(21)00460-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barda N., Dagan N., Cohen C., Hernan M.A., Lipsitch M., Balicer R.D. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: an observational study. Lancet. October 29, 2021:1–8. doi: 10.1016/S0140-6736(21)02249-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bar-On Y.M., Goldberg Y., Mandel M., Bodenheimer O., Freedman L., Kalkstein N., Huppert A. Protection of BNT162b2 vaccine booster against covid-19 in Israel. N. Engl. J. Med. 2021;385(15):1393–1400. doi: 10.1056/NEJMoa2114255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BBC News . July 10, 2021. What's the roadmap of lifting lockdown.https://www.facebook.com/watch/?v=523963812088281 Availalbe at: [Google Scholar]
- Bernal J., Andrews N., Gower C., et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (Delta) variant. N. Engl. J. Med. 2021;385:585–594. doi: 10.1056/NEJMoa2108891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhopal S.S., Absoud M. Vaccinating children to prevent long covid? More caution is needed in interpreting current epidemiological data. BMJ. 2021;372 doi: 10.1136/BMJ.N520. [DOI] [PubMed] [Google Scholar]
- CDC COVID Data Tracker, United States at a glance. Center for Disease Control. 2021. https://covid.cdc.gov/covid-data-tracker/#rates-by-vaccine-status September 2021.
- CNBC . 2021. Pfizer says it is developing a Covid booster shot to target the highly transmissible delta variant. [Google Scholar]
- Coronavirus (COVID-19) Vaccinations . 2021. Statistics and Research - Our World in Data.https://ourworldindata.org/covid-vaccinations Availalbe at: [Google Scholar]
- COVID-19 Map . 2020-2021. Johns Hopkins Coronavirus Resource Center.https://coronavirus.jhu.edu/map.html Availalbe at: [Google Scholar]
- Dietz K. The estimation of the basic reproduction number for infectious diseases. Stat. Methods Med. Res. 1993;2(1):23–41. doi: 10.1177/096228029300200103. [DOI] [PubMed] [Google Scholar]
- Gao Q., Hu Y., Dai Z., Xiao F., Wang J., Wu J. The epidemiological characteristics of 2019 novel coronavirus diseases (COVID-19) in Jingmen, Hubei, China. Medicine (Baltimore) 2020;99(23) doi: 10.1097/MD.0000000000020605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health England P . 2021. 25 June 2021 Risk assessment for SARS-CoV-2 variant: Delta (VOC-21APR-02, B.1.617.2) Public Health England Indicator RAG* Confidence Assessment and rationale. [Google Scholar]
- Hertting O. More research is needed on the long-term effects of COVID-19 on children and adolescents. Acta Paediatr. 2021;110(3):744. doi: 10.1111/APA.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- https://datadashboard.health.gov.il/COVID-19/general
- Israel Ministry of Health COVID-19 dashboard . 2021. datadashboardba.health.gov.il/COVID-19/general. [Google Scholar]
- Levin E.G., Lustig Y., Cohen C., et al. Waning Iimmune humoral response to BNT162b2 covid-19 vaccine over 6 months. N. Engl. J. Med. October 6, 2021:1–11. doi: 10.1056/NEJMoa2114583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall J.C., Murthy S., Diaz J., et al. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect. Dis. 2020;20(8):e192–e197. doi: 10.1016/S1473-3099(20)30483-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MOH Ministry of Health Announcement: The efficacy of the COVID-19 vaccine. July 06, 2021. https://www.gov.il/BlobFolder/news/06072021-04/he/NEWS_Corona_vaccine-eficacy.pdfM
- O’Dowd A. Covid-19: cases of delta variant rise by 79%, but rate of growth slows. BMJ. 2021;373 doi: 10.1136/BMJ.N1596. [DOI] [PubMed] [Google Scholar]
- Oliver S.E., Gargano J.W., Marin M., et al. The advisory committee on immunization practices’ interim recommendation for use of Pfizer-BioNTech COVID-19 vaccine — United States, December 2020. Morb. Mortal. Wkly Rep. 2020;69(50):1922. doi: 10.15585/MMWR.MM6950E2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Population of Israel on the Eve of 2021.; 2021.
- Starke K.R., Petereit-Haack G., Schubert M., et al. The age-related risk of severe outcomes due to COVID-19 infection: a rapid review, meta-analysis, and meta-regression. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/IJERPH17165974. Page 5974. 2020;17(16):5974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong J.Y., Kelly H., Ip D.K.M., Wu J.T., Leung G.M., Cowling B.J. Case fatality risk of influenza a(H1N1pdm09): a systematic review. Epidemiology. 2013;24(6):830–841. doi: 10.1097/EDE.0B013E3182A67448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang S., Cao P., Du P., Wu Z., Zhuang Z., Yang L., Yu X., Zhou Q., Feng X., Wang X., Li W., Liu E., Chen J., Chen Y., He D. On behalf of COVID-19 evidence and recommendations working group. Early estimation of the case fatality rate of COVID-19 in mainland China: a datadriven analysis. Ann Transl Med. 2020;8(4):1–6. doi: 10.21037/atm.2020.02.66. [DOI] [PMC free article] [PubMed] [Google Scholar]