Abstract
The COVID-19 vaccines are limited in supply which requires vaccination by priority. This study proposes a spatial priority-based vaccine rollout strategy for Bangladesh. Demographic, economic and vulnerability, and spatial connectivity – these four types of factors are considered for identifying the spatial priority. The spatial priority is calculated and mapped using a GIS-based analytic hierarchy process. Our findings suggest that both demographic and economic factors are keys to the spatial priority of vaccine rollout. Secondly, spatial connectivity is an essential component for defining spatial priority due to the transmissibility of COVID-19. A total of 12 out of 64 districts were found high-priority followed by 22 medium-priorities for vaccine rollout. The proposed strategy by no means suggests ending mass vaccination by descending age groups but an alternative against limited vaccine supply. The spatial priority of the vaccine rollout strategy proposed in this study might help to curb down COVID-19 transmission and to keep the economy moving. The inclusion of granular data and contextual factors can significantly improve the spatial priority identification which can have wider applications for other infectious and transmittable diseases and beyond.
Keywords: Pandemic, Demography, Economy, Vulnerable groups, GIS, Bangladesh
Pandemic; Demography; Economy; Vulnerable groups; GIS; Bangladesh.
1. Introduction
Vaccination against COVID-19 is a precondition for normalizing daily life and opening up economic activities. The rising number of COVID-19 cases globally – potentially the third wave, mostly by the Delta variant – from March 2021 onwards is a renewed concern for the world, especially in the worst affected countries like the UK, the USA, Indonesia, India and Brazil. The public sentiment is against an all-out lockdown as the pandemic has caused a 3.5 percent contraction of the global economy in 2020 [1]. The social costs of the pandemic are understood yet have mostly remained unaccounted for. Curbing the pandemic through vaccination is a challenge because the availability of vaccines varies across countries, especially the low-income countries are lagging considerably [1, 2].
Globally, the number of available vaccines is in short supply, and vaccine rollout is prioritized in every country. The Advisory Committee on Immunization Practices (ACIP) in the US recommended vaccine rollout with the goal in mind “to decrease death and serious illness due to COVID-19 as much as possible, to maintain the functioning of society and to reduce the extra burden on people already facing disparities.” Health care personnel and care home residents are the first to receive the vaccination. Frontline workers and people over the age of 75 received vaccination in the second phase followed by descending age groups in the third phase [3]. The UK approach to vaccine rollout is similar to the USA with added categories of ethnic minorities, obese and deprived communities [4].
The sheer scarcity of vaccines has led to a vaccine hoarding situation where well-to-do countries have invested heavily in vaccine procurement. The poorer nations are expected to receive the lion's share of their vaccines from the COVAX initiative, a coalition among the Coalition for Epidemic Preparedness Innovations (CEPI), the Vaccine Alliance (GAVI) and the World Health Organization (WHO). As of 21 July 2021, the COVAX program has delivered over 138 million COVID-19 vaccines [5], which is far short of the global demand. As a result, most countries i.e., Bangladesh are relying on national procurement and partisan treaty. The scarcity of vaccines has led some nations to budget vaccination according to their national priority. For example, Indonesia has prioritized the working-age people over the older ones, a move criticized as a very economic one.1
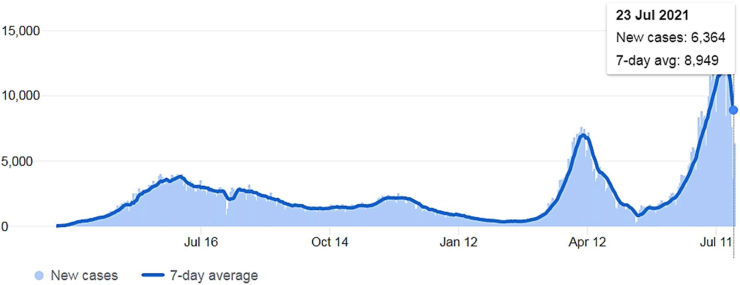
Bangladesh, which is the focus of this study, has a similar experience with the global trend of the third wave (Figure 1) [6]. The first phase of vaccination prioritized the healthcare service providers and frontline workers, and population over the age of 40. So far, the country has received 10.3 million out of 30 million doses of Oxford-AstraZeneca COVID-19 vaccine produced by the Serum Institute of India under a tripartite agreement. The rest of the vaccine delivery hit rock-bottom as India prioritized national demand over export due to the worsening coronavirus condition. As of 24 July 2021, the country received 100,620 doses of Pfizer-BioNTech and 5.5 million Moderna vaccines through the COVAX [5] 2. Additionally, Bangladesh has purchased 15 million doses of Sinopharm vaccines, of which 2 million are already been delivered in an addition to 1.1 million as a gift.3 However, the number of vaccines is far too short for mass vaccination of the country's more than 165 million population. Bangladesh ranks 29th in the world in vaccination per 100 people, only 2.6% are fully and 1.06% are partially vaccinated [7]. The country is forced to prioritize the vaccine rollout against faltering supply and limited stock.
Figure 1.
COVID-19 case trend in Bangladesh [7].
The objective of this research is to propose a spatial priority of the COVID-19 vaccine rollout strategy for Bangladesh. In doing so, we first consider the spatial distributions of COVID-19 cases by districts, which is highly skewed toward cities. In addition, we consider demographic, economic, vulnerable groups and spatial factors as keys for vaccination priority. So far the Bangladesh government's mass-vaccination policy has resulted in thinly distributing the limited vaccine supply. We hypothesize that vaccine rollout needs to be spatially prioritized based on the aforementioned factors.
Numerous studies are in circulation concerning the causes and consequences of COVID-19. One set of studies link COVID-19 cases with urbanization [8, 9, 10]. Cities and urban areas are more susceptible to COVID-19 than rural areas due to four key reasons: high density and connectivity, crowded living, and exposed occupation [11].4 However, such urban concentration of the virus is challenged as the spread is shifting towards rural areas [12] 5. Another set of studies link pandemic transmission vulnerability to the urban poor and marginalized communities [13, 14]. A few studies recommend better knowledge on pandemic adaptive urban planning as pandemic frequency is expected to be on the rise in the future [15, 16]. However, there is very little research on how vaccination is a key to pandemic emergency response against the backdrop of a limited supply; this paper expects to fill in this research gap.
An analytical hierarchy process (AHP) is applied to weigh the multiple factors to measure their respective priority. Spatial information on priority areas is calculated and mapped using geographic information system (GIS). Against this background, the second section of the paper highlights the vaccine rollout priorities and the third section explains the method and data. The fourth section is results followed by discussion and conclusion in the fifth and sixth sections, respectively.
2. Vaccine rationing against limited supply
Suppressive interventions including lockdown, contact tracing and quarantine, and social distancing are short-term measures against the COVID-19 pandemic [17]. A quick rebound of transmission if suppressive interventions are relaxed [18], the possibility of simultaneous outbreaks [19], and the spread of local variants, such as the Delta variant – these factors leave no alternative but to mass-vaccination as a priority to end the pandemic [17, 20]. An extraordinary amount of discussion has been directed to equitable distribution of the already approved vaccines, which is in line with WHO's slogan “no one is safe until everyone is safe” (see for example, [21, 22, 23, 24]). Not to curtail the success of the COVAX program, the global vaccine supply has been more or less nationalized where the rich nations outstrip the low-income countries by a large margin in vaccination rate (see [25]).
Secondly, from the economic point of view, unequal distribution of the COVID-19 vaccines could result in loss of the global economy up to US $1.2 trillion per year in GDP [26]. Suppressing measures against the pandemic transmission has costed the low-income countries dearly, and the lower socio-economic groups are the hardest hit [27]. Easing social distancing restrictions and opening up economic activities despite pandemic rebound is a fact for developing and emerging economies. Thirdly, the spatial distribution of COVID-19 cases has been a key consideration for the fight against the pandemic. Cities, in particular, have the highest concentration of COVID-19 cases due to density [28]. Urban areas act as transmission nodes for virus spread. Additionally, cities are engines of economic and administrative activities. Therefore, cities are a priority for vaccine rollout from the spatial perspective.
Drawing on the WHO's Pandemic Influenza Risk Management guidance, vaccination priority must be based on ethical consideration and local risk assessment [29]. At the same time, the WHO guidelines for managing scarce COVID-19 prevention and care resources recommend consideration of the local context and extent of scarcity [2, 17, 30]. In contrast to the Bangladesh government's descending age category except for the selected groups i.e., public university and medical students, we prioritize vaccine rollout in Bangladesh based on four criteria:
-
•
demographic factors – the number of confirmed COVID-19 cases, age bracket (40+), and population distribution and density are considered under this criteria.
-
•
economic factors – Bangladesh has been on on-and-off lockdown, restricted mobility, and social distancing since March 2020, causing an enormous economic impact. The service sector employment of the country is 40.38 percent of the total, followed by the agricultural (38.3%) and industrial (21.32) sectors ([31]; see also [32]). The service and industrial sectors have been heavily impacted by the pandemic. In response, the government has issued several stimulus packages to support the service and industrial sectors [11]. Therefore, easing restrictions and opening up economic activities are priorities for vaccine rollout.
-
•
high risk and vulnerable groups – this includes essential health and service providers i.e., cleaners and bankers, and population over the age of 40, the poor, and people with disabilities. The essential health workers and service providers are excluded from the vaccine roll-out priority as they have been vaccinated in the first phase.
-
•
spatiality – the COVID-19 dashboard in Bangladesh provides data at the district level, and vaccine rollout has been through the district health administration. We, therefore, are unable to perform granular scale vaccination priority and resorted to district-level analysis.
A number of researches highlight the environmental factors of the pandemic [33, 34]. However, we do not incorporate environmental factors in our analysis due to a lack of data at the district level.
3. Method and data
3.1. Description of the study area
Bangladesh is one of the fastest-growing economies in the world [35]. The country has a population of over 165 million and consists of 64 administrative districts. On 08 March 2020, three COVID-19 positive patients were confirmed for the first time [36]. As of 24 July 2021, a total of 1,153,344 confirmed COVID-19 cases and 19,046 deaths were officially reported (Figure 1). Figure 2 (a) illustrates the district-wise distribution of COVID-19 confirmed cases. As of 24 July 2021, a total of 6,033,439 first doses and 4,289,518 second doses of COVID-19 vaccines have been administered nationwide [7].
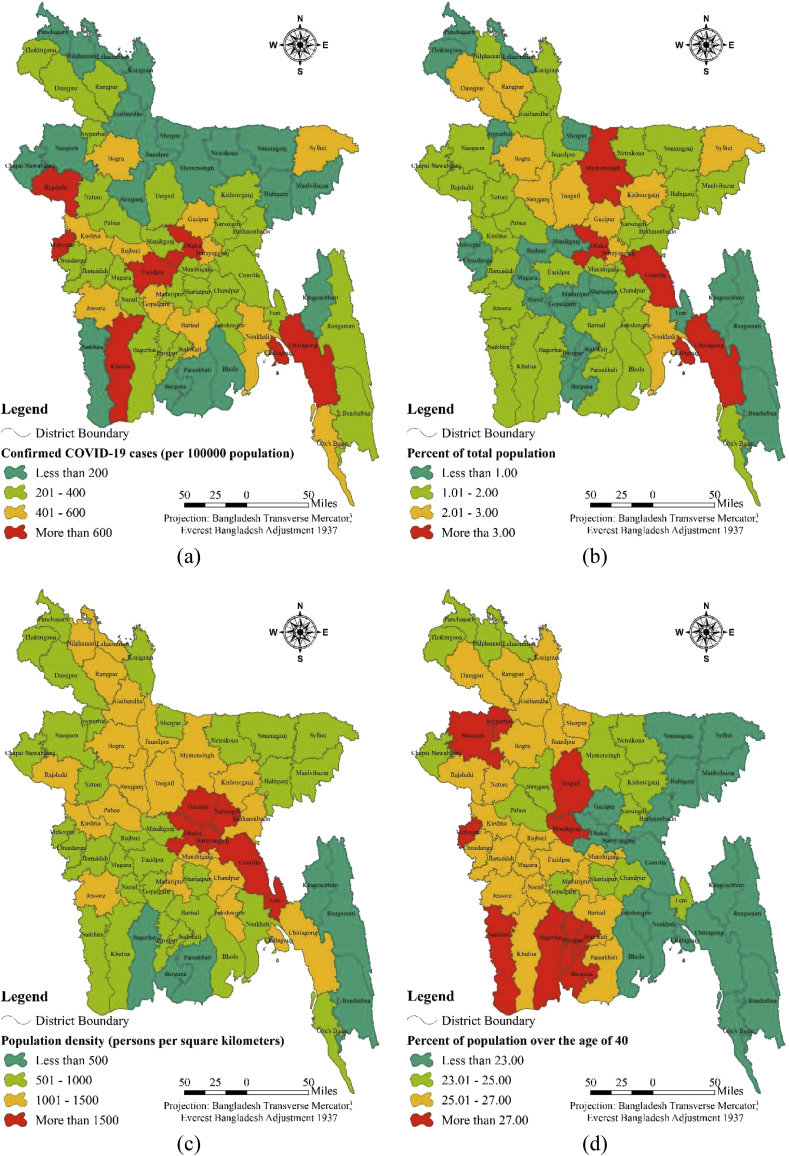
Figure 2.
Spatial priority of the factors: (a) confirmed COVID-19 cases (per 100000 population), (b) percent of total population, (c) population density (persons per square kilometers), (d) percent of population over the age of 40, (e) percent of urban population, (f) percent of working-age people, (g) percent of industrial workers, (h) percent of the service sector employment, (i) percent of poor people, (j) percent of households with disability.
3.2. GIS-based priority mapping
The research applied a knowledge-based approach (i.e., multi-criteria) to assess the vaccine rollout priority of districts in Bangladesh. GIS-based priority mapping by using the analytical hierarchy process (AHP) is a widely used method in the field of multi-criteria decisions [37], which uses mathematical and psychological principles for investigating multi-criteria decisions [38]. Numerous studies have addressed COVID-19 related issues using the GIS-based AHP method (for example, susceptibility/risk mapping [39, 40, 41], and prioritization of activities and facilities [42]). However, literature on GIS-based AHP for vaccine rollout is scarce. This research utilized a GIS-based AHP method for priority mapping for COVID-19 vaccine rollout. For an initial investigation, each factor was randomly classified into four sub-factors and the factor maps were prepared. The hierarchy of factors using pairwise comparisons helps to discover and correct logical inconsistencies in AHP [43, 44]. Pairwise comparisons of two factors or two sub-factors under a factor were conducted. Weights (i.e., equal importance, more importance, and less importance) [45, 46] were given for differentiating two factors or two sub-factors under a factor. A 9-point continuous scale (i.e., 1/9, 1/8, 1/7, 1/6, 1/5, 1/4, 1/3, 1/2, 1, 2, 3, 4, 5, 6, 7, 8, 9) was used for weight rating [47, 48]. The given weight rating was used for calculating the eigenvalues and consistency ratio (CR). CR was calculated using the following Eq. (1) [49, 50].
| (1) |
where, RI = mean consistency index; CI = consistency index.
The consistency index (CI) was calculated using the following Eq. (2).
| (2) |
where, ymax = the largest eigenvalue; N = order of the comparison matrix.
The CR values < 10% was accepted [51]. The factor maps were reclassified based on the calculated weights of sub-factors. Finally, priority maps were prepared using GIS-based weighted overly using reclassified factor maps and weights of factors. The following Eq. (3) was used for priority level calculation.
| (3) |
where, Wj = weight of causative factor j; wij = weighted value of class i of causative factor j.
The 64 districts were classified into three classes based on priority level based on the Jenks’ natural break method: (1) high priority; (2) medium priority; and (3) low priority.
All districts of Bangladesh are spatially inter-connected and influence each other in COVID-19 transmission. To address the influence of other districts on the priority level of one district, we integrated the distance function with the priority map calculated from the GIS-based AHP. We proposed a relationship between priority level based on district weight from AHP and road distance between districts (in Table 1). Finally, the spatial priority of vaccine rollout was calculated using the priority level and road distance function. The 64 districts were further reclassified into three classes based on spatial priority level using the Jenks’ natural break method: (1) high priority; (2) medium priority; and (3) low priority.
Table 1.
Proposed relationship between priority level and road distance.
| Percent of influence of a district on others | Distance between districts (km) |
|---|---|
| 50% | ≤100 |
| 25% | 101–200 |
| 12.50% | 201–300 |
| 6.25% | 301–400 |
| 3.13% | 401–500 |
| 1.56% | 501–600 |
| 0.78% | 601–700 |
3.3. Data
Four key areas are considered for vaccine roll-out priority: demographic factors, economic factors, vulnerability, and spatiality. Five demographic (i.e., number of confirmed COVID cases, percent of the population, population density, percent of the urban people, percent of the population over the age of 40), three economic (i.e., percent of the working-age people, percent of the industrial workers, percent of the service sector employment), and two vulnerability (i.e., percent of poor people, percent of households with disability) factors were used for multi-criteria based priority ranking. Finally, spatial priority is calculated based on road distance between districts. This research is based on secondary data that are mentioned in Table 2.
Table 2.
Description of data.
| Data with units | Mean | Minimum | Maximum | Standard deviation | Source with year |
|---|---|---|---|---|---|
| Confirmed COVID-19 cases (per 100000 population) | 339.50 | 84.81 | 2965.84 | 369.73 | Institute of Epidemiology Disease Control and Research (2021) |
| Percent of total population | 1.56 | 0.27 | 8.36 | 1.20 | Bangladesh Bureau of Statistics (2011 Census) |
| Population density (persons per square kilometres) | 1107.69 | 86.00 | 8111.00 | 1030.07 | |
| Percent of population over the age of 40 | 24.61 | 17.07 | 28.90 | 2.52 | |
| Percent of urban population | 17.84 | 8.80 | 77.10 | 10.15 | |
| Percent of working-age people | 59.96 | 52.81 | 70.70 | 3.86 | |
| Percent of industrial workers | 3.12 | 0.64 | 22.78 | 3.46 | |
| Percent of the service sector employment | 9.23 | 5.49 | 27.69 | 3.29 | |
| Percent of poor people | 32.25 | 3.59 | 63.72 | 11.95 | |
| Percent of households with disability | 5.92 | 3.04 | 7.92 | 0.92 | |
| District boundary (shapefile) | - | - | - | - | Geological Survey of Bangladesh (2020) |
4. Results
4.1. Sub-factors mapping and weighting
The spatial distribution of sub-factors is presented in Figure 2, and their respective values based on pairwise comparison are in the Table 3. The factors of spatial priority are in three broad categories: demographic, economic and vulnerability. Under the demographic category, five factors – the number of confirmed COVID-19 cases, percent of the total population, population density, percent of the urban people, and percent of the population over the age of 40 – are considered. Of these five factors, the highest eigenvalue (i.e., 0.66) was found for the ‘more than 600 confirmed COVID-19 cases per 100,000 population’ sub-factor.
Table 3.
Pairwise comparison matrix, consistency ratio and weights of the sub-factor.
| Factors | (1) | (2) | (3) | (4) | Eigenvalues |
|---|---|---|---|---|---|
| Confirmed COVID-19 cases (per 100000 population) | |||||
| (1) Less than 200 | 1 | 0.04 | |||
| (2) 201-400 | 3 | 1 | 0.10 | ||
| (3) 401-600 | 5 | 3 | 1 | 0.20 | |
| (4) More than 600 | 9 | 7 | 5 | 1 | 0.66 |
| Consistency Ratio = 0.062802 | |||||
| Percent of total population | |||||
| (1) Less than 1.00 | 1 | 0.08 | |||
| (2) 1.01–2.00 | 2 | 1 | 0.13 | ||
| (3) 2.01–3.00 | 3 | 2 | 1 | 0.23 | |
| (4) More than 3.00 | 5 | 5 | 3 | 1 | 0.56 |
| Consistency Ratio = 0.021753 | |||||
| Population density (persons per square kilometers) | |||||
| (1) Less than 500 | 1 | 0.06 | |||
| (2) 501-1000 | 3 | 1 | 0.12 | ||
| (3) 1001-1500 | 5 | 3 | 1 | 0.26 | |
| (4) More than 1500 | 9 | 4 | 3 | 1 | 0.56 |
| Consistency Ratio = 0.031177 | |||||
| Percent of population over the age of 40 | |||||
| (1) Less than 23.00 | 1 | 0.10 | |||
| (2) 23.01–25.00 | 2 | 1 | 0.16 | ||
| (3) 25.01–27.00 | 3 | 2 | 1 | 0.27 | |
| (4) More than 27 | 4 | 3 | 2 | 1 | 0.47 |
| Consistency Ratio = 0.011357 | |||||
| Percent of urban population | |||||
| (1) Less than 15 | 1 | 0.07 | |||
| (2) 15.01–20.00 | 2 | 1 | 0.14 | ||
| (3) 20.01–25.00 | 5 | 2 | 1 | 0.29 | |
| (4) More than 25 | 7 | 3 | 2 | 1 | 0.50 |
| Consistency Ratio = 0.00652 | |||||
| Percent of working-age people | |||||
| (1) Less than 55.00 | 1 | 0.06 | |||
| (2) 55.01–60.00 | 4 | 1 | 0.15 | ||
| (3) 60.01–65.00 | 5 | 3 | 1 | 0.28 | |
| (4) More than 65 | 6 | 3 | 3 | 1 | 0.51 |
| Consistency Ratio = 0.076849 | |||||
| Percent of industrial workers | |||||
| (1) Less than 1.50 | 1 | 0.04 | |||
| (2) 1.51–3.00 | 5 | 1 | 0.12 | ||
| (3) 3.01–4.50 | 7 | 3 | 1 | 0.26 | |
| (4) More than 4.50 | 9 | 6 | 3 | 1 | 0.58 |
| Consistency Ratio = 0.068109 | |||||
| Percent of the service sector employment | |||||
| (1) Less than 7.00 | 1 | 0.05 | |||
| (2) 7.01–9.00 | 4 | 1 | 0.15 | ||
| (3) 9.01–11.00 | 5 | 2 | 1 | 0.24 | |
| (4) More than 11.00 | 7 | 4 | 3 | 1 | 0.56 |
| Consistency Ratio = 0.038256 | |||||
| Percent of poor people | |||||
| (1) Less than 20.00 | 1 | 0.07 | |||
| (2) 20.01–30.00 | 3 | 1 | 0.16 | ||
| (3) 30.01–40.00 | 4 | 2 | 1 | 0.28 | |
| (4) More than 40.00 | 5 | 4 | 2 | 1 | 0.49 |
| Consistency Ratio = 0.026708 | |||||
| Percent of households with disability | |||||
| (1) Less than 5.00 | 1 | 0.09 | |||
| (2) 5.01–6.00 | 2 | 1 | 0.13 | ||
| (3) 6.01–7.00 | 3 | 2 | 1 | 0.22 | |
| (4) More than 7.00 | 4 | 4 | 4 | 1 | 0.56 |
| Consistency Ratio = 0.052439 | |||||
The demographic category hardly shows a spatial pattern except for the capital city Dhaka and its surrounding districts, and for Chittagong and Khulna districts (the second and third largest cities, respectively). Dhaka region, Chittagong and Khulna rank high up in the total number of confirmed COVID-19 cases. Expectedly, districts having the major cities clearly show a higher agglomeration of population and urban population than others. However, the population over the age of 40 shows a different priority as the younger population is located in urban and city areas. Therefore, spatial priority for vaccine rollout from the demographic perspective is not conclusive.
Secondly, the economic category consists of three factors: percent of service sector employment, percent of industrial employment and percent of working-age people. Among the employment category, industrial workers more than 4.50 percent, service sectors more than 11 percent, and working-age population more than 65 percent have the highest eigenvalues (0·58, 0·56 and 0·51, respectively). From Figure 2, Dhaka and Chittagong have spatial monopolies in the agglomeration of industrial and service sector employment. Expectedly, major cities like Dhaka and its surrounding districts, Chittagong, Khulna and Sylhet show a high concentration of service and industrial employment. However, there is no clear spatial pattern among the 64 districts when the working-age population and poverty distribution are considered.
The vulnerability category consists of two factors: percent of poor people and percent of households with disabilities. Households with disabilities more than 7 percent and the poor more than 40 percent have the highest eigenvalues (0.56 and 0.49, respectively) among the categories.
4.2. Factors weighting
The pairwise comparison matrix among the selected ten spatial variables is in Table 4. The number of confirmed COVID-19 cases and population density have the highest eigenvalues (0·31 and 0·20, respectively). Therefore, these two factors combined (eigenvalue 0·51) explain more than half of the spatial priority for vaccine rollout. The percent of the working-age people has the third-highest eigenvalue (0·11) followed by industrial employment (0·09), service sector workers (0·08) and urban population (0·07), respectively.
Table 4.
Pairwise comparison matrix, consistency ratio and weighs of the factors.
| Factors | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | Eigenvalues |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Confirmed COVID-19 cases | 1 | 0.31 | |||||||||
| (2) Percent of total population | 1/4 | 1 | 0.03 | ||||||||
| (3) Population density | 1/3 | 5 | 1 | 0.20 | |||||||
| (4) Percent of population over the age of 40 | 1/7 | 2 | 1/4 | 1 | 0.05 | ||||||
| (5) Percent of urban population | 1/8 | 5 | 1/5 | 3 | 1 | 0.07 | |||||
| (6) Percent of working-age people | 1/5 | 3 | 1/3 | 2 | 3 | 1 | 0.11 | ||||
| (7) Percent of industrial workers | 1/4 | 4 | 1/3 | 3 | 1 | 1/2 | 1 | 0.09 | |||
| (8) Percent of the service sector employment | 1/4 | 4 | 1/4 | 3 | 1 | 1/2 | 1 | 1 | 0.08 | ||
| (9) Percentage of poor people | 1/5 | 1/2 | 1/7 | 1/4 | 1/2 | 1/4 | 1/5 | 1/3 | 1 | 0.03 | |
| (10) Percent of households with disability | 1/7 | 3 | 1/5 | 1/3 | 1/2 | 1/3 | 1/4 | 1/3 | 1 | 1 | 0.03 |
| Consistency Ratio = 0.076259 | |||||||||||
Percent of the poor, population over the age of 40, percent of total population and percent of households with disability – these four factors have the lowest weights (eigenvalue 0·05, 0·03, 0·03 and 0·03, respectively). Bangladesh government's current strategy is mass-vaccination for all over the age of 40 (recently updated to over 25 years). However, the pairwise comparison matrix shows that the population over the age of 40 has low priority in vaccination compared to the rest of the spatial factors.
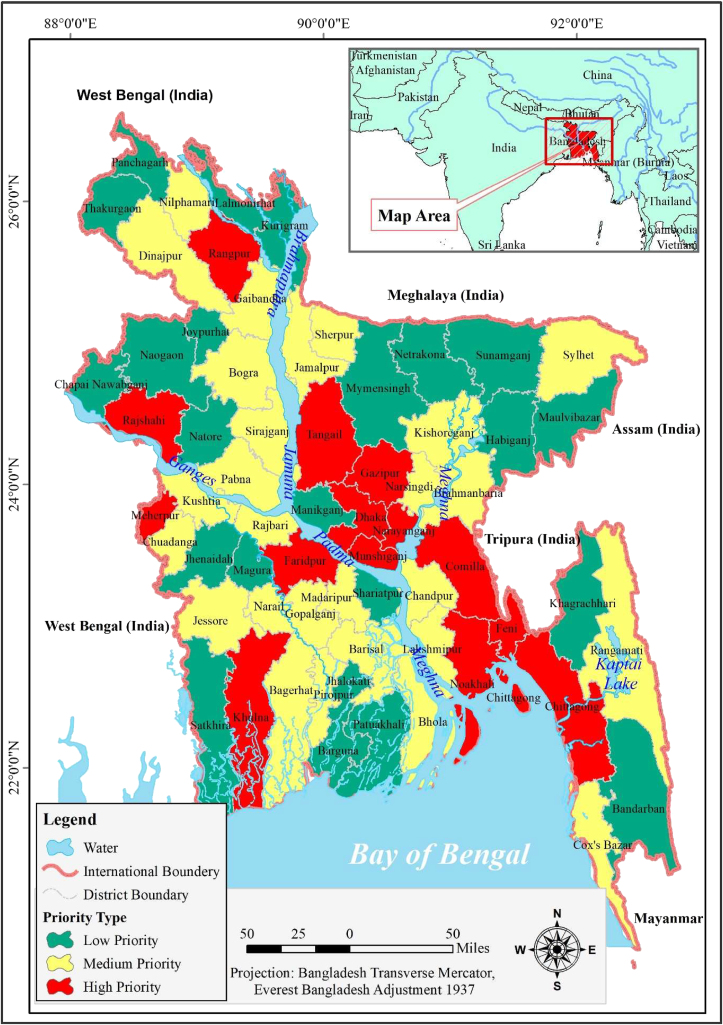
4.3. Spatial overlay and priority districts
Priority indices of the individual sub-factors and factors using the spatial overlay are in Table 5. The priority indices are then categorized into three categories (i.e., high, medium and low priority districts for vaccine roll-out). The spatial distribution of priority districts are presented in Figure 3.
Table 5.
Priority Index and Spatial Priority Index of 64 districts.
| District Name | Priority Index | Priority Level | Spatial Priority Index | Spatial Priority Level | District Name | Priority Index | Priority Level | Spatial Priority Index | Spatial Priority Level |
|---|---|---|---|---|---|---|---|---|---|
| Dhaka | 0.53082 | High | 0.643308 | High | Dinajpur | 0.163483 | Medium | 0.216454 | Medium |
| Narayanganj | 0.353231 | High | 0.461572 | High | Rajbari | 0.16212 | Medium | 0.264371 | Medium |
| Chittagong | 0.331456 | High | 0.380961 | High | Madaripur | 0.15961 | Medium | 0.276893 | Low |
| Khulna | 0.32721 | High | 0.417278 | High | Rangamati | 0.158353 | Medium | 0.198107 | Low |
| Meherpur | 0.32571 | High | 0.404698 | High | Chuadanga | 0.156537 | Medium | 0.240709 | Low |
| Faridpur | 0.322547 | High | 0.432961 | High | Cox's Bazar | 0.155463 | Medium | 0.176069 | Low |
| Rajshahi | 0.293057 | High | 0.36414 | High | Bhola | 0.155037 | Medium | 0.224889 | Low |
| Rangpur | 0.290958 | High | 0.351997 | High | Bagerhat | 0.153684 | Medium | 0.239346 | Low |
| Munshiganj | 0.28545 | High | 0.389385 | High | Gopalganj | 0.153037 | Medium | 0.252566 | Low |
| Comilla | 0.273631 | High | 0.3637 | High | Lalmonirhat | 0.144803 | Low | 0.191036 | Low |
| Gazipur | 0.269777 | High | 0.378119 | High | Chapai Nawabganj | 0.144515 | Low | 0.200241 | Low |
| Feni | 0.266634 | High | 0.340891 | High | Panchagarh | 0.141587 | Low | 0.176902 | Low |
| Tangail | 0.249647 | High | 0.350213 | Medium | Jhalokati | 0.138974 | Low | 0.226515 | Low |
| Noakhali | 0.248108 | High | 0.324828 | Medium | Mymensingh | 0.138095 | Low | 0.223498 | Low |
| Bogra | 0.231672 | Medium | 0.317982 | Medium | Natore | 0.13703 | Low | 0.22658 | Low |
| Narsingdi | 0.220499 | Medium | 0.322879 | Medium | Joypurhat | 0.135645 | Low | 0.207764 | Low |
| Jamalpur | 0.215843 | Medium | 0.287509 | Medium | Bandarban | 0.129836 | Low | 0.162818 | Low |
| Chandpur | 0.206429 | Medium | 0.299478 | Medium | Sunamganj | 0.129078 | Low | 0.159241 | Low |
| Jessore | 0.195266 | Medium | 0.294147 | Medium | Thakurgaon | 0.12842 | Low | 0.170215 | Low |
| Sherpur | 0.189497 | Medium | 0.25559 | Medium | Shariatpur | 0.125589 | Low | 0.224081 | Low |
| Pabna | 0.187436 | Medium | 0.277439 | Medium | Magura | 0.123619 | Low | 0.225351 | Low |
| Brahmanbaria | 0.184291 | Medium | 0.265546 | Medium | Patuakhali | 0.121881 | Low | 0.194973 | Low |
| Pirojpur | 0.179444 | Medium | 0.266014 | Medium | Kurigram | 0.121792 | Low | 0.167831 | Low |
| Lakshmipur | 0.17882 | Medium | 0.266944 | Medium | Jhenaidah | 0.120833 | Low | 0.218677 | Low |
| Barisal | 0.17863 | Medium | 0.264875 | Medium | Satkhira | 0.117416 | Low | 0.187916 | Low |
| Kushtia | 0.176827 | Medium | 0.280892 | Medium | Netrakona | 0.112779 | Low | 0.185222 | Low |
| Kishoreganj | 0.169399 | Medium | 0.252599 | Medium | Naogaon | 0.112141 | Low | 0.186334 | Low |
| Narail | 0.169071 | Medium | 0.265231 | Medium | Barguna | 0.110202 | Low | 0.167807 | Low |
| Gaibandha | 0.168646 | Medium | 0.233767 | Medium | Khagrachhari | 0.108035 | Low | 0.150283 | Low |
| Nilphamari | 0.166908 | Medium | 0.216769 | Medium | Habiganj | 0.103245 | Low | 0.167264 | Low |
| Sirajganj | 0.166516 | Medium | 0.259954 | Medium | Manikganj | 0.096881 | Low | 0.205223 | Low |
| Sylhet | 0.164131 | Medium | 0.207934 | Medium | Maulvibazar | 0.096653 | Low | 0.147648 | Low |
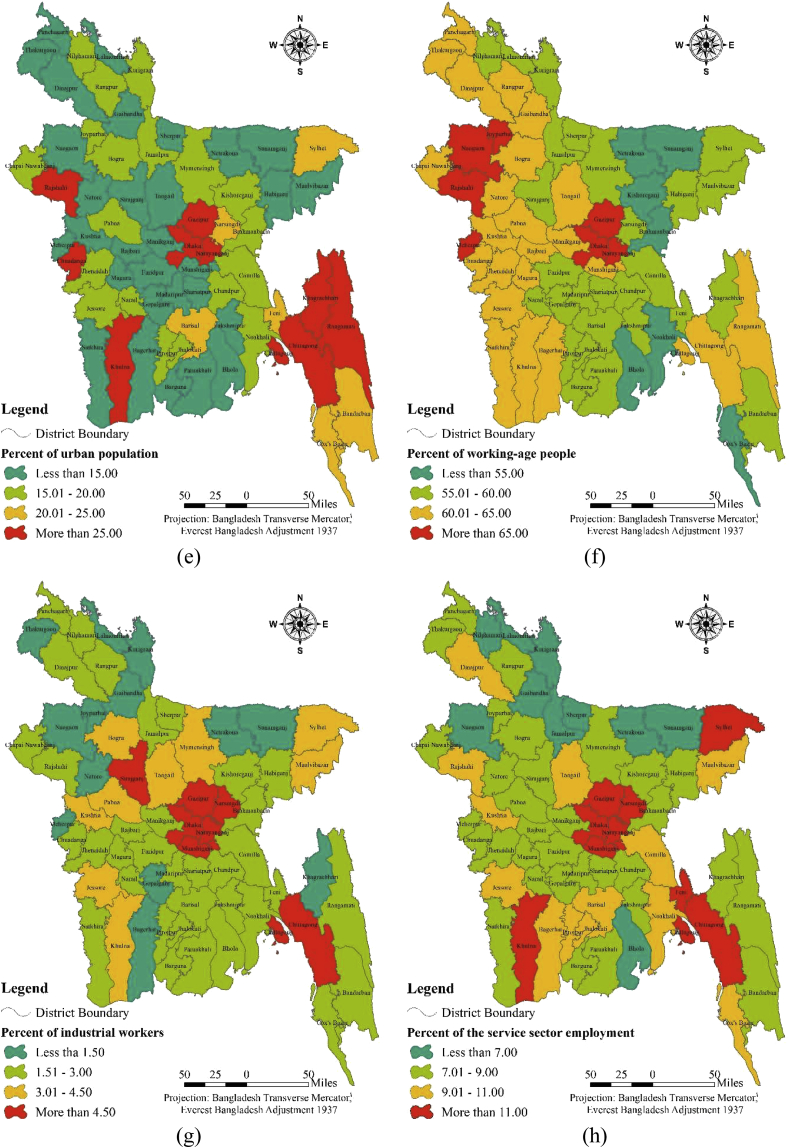
Figure 3.
Spatial priority of 64 districts for vaccine rollout.
Figure 3 shows that Dhaka and its surrounding districts have a high priority for vaccine rollout. Similarly, Chittagong, Khulna and Rangpur districts – these divisional (2nd tier) cities have high priority. Because the number of confirmed cases and population density are the two biggest factors (eigenvalue 0·31 and 0·20, respectively; in Table 4) for vaccine rollout priority, understandably, the divisional cities and their surrounding districts have the highest priority for vaccine rollout. Secondly, the medium priority districts are spatially clustered around the high priority districts whereas the low priority ones are scattered. Based on the weights of the ten factors, 14 districts were identified as high, 27 as medium and 23 as low priority for vaccine rollout.
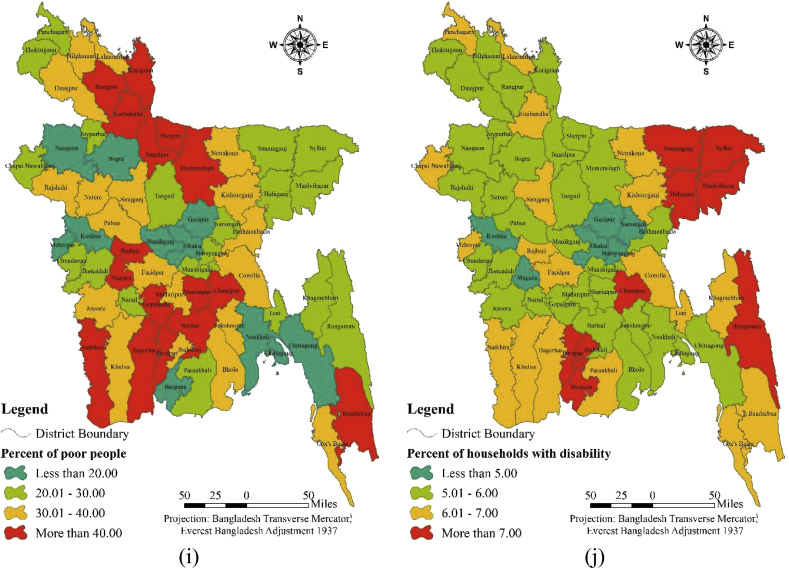
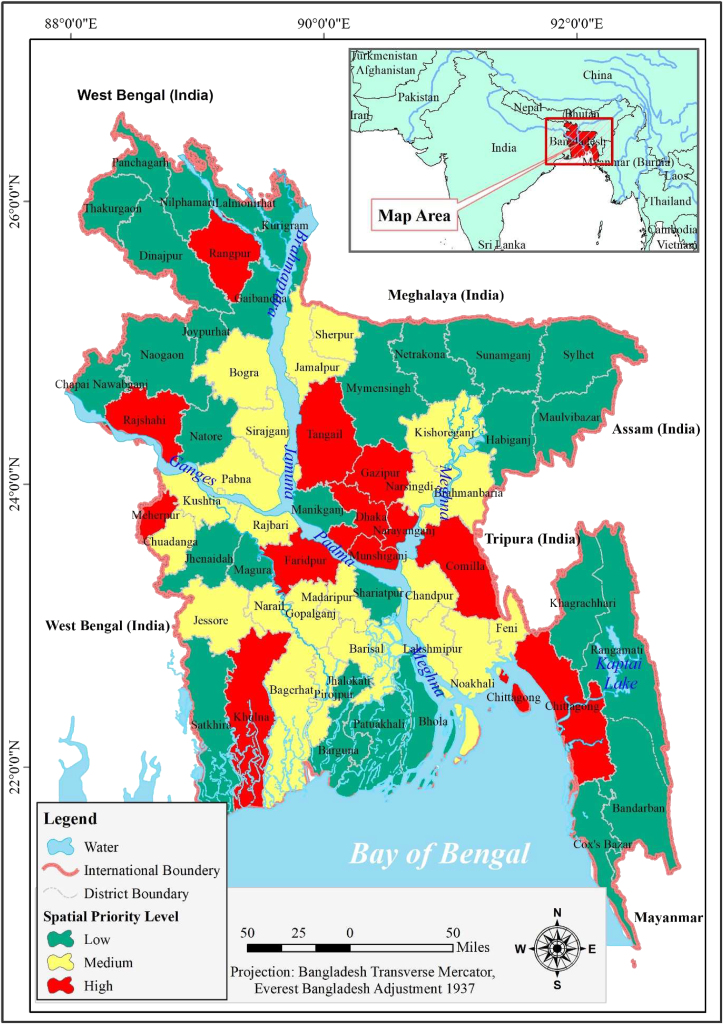
Finally, the spatial priority of districts by incorporating distance function is presented in Figure 4, which has marked the high, medium and low priority districts for vaccine rollout. Out of the 64 districts, 12 are found as high priority, followed by 22 and 30 districts as medium and low priority, respectively.
Figure 4.
Proposed spatial priority of 64 districts for vaccine rollout.
5. Discussion
Mass vaccination is hardly a judicial strategy without ensuring vaccine availability. Therefore, the COVID-19 vaccine roll-out must be rationed and prioritized. The rollout strategy presented in this study is in line with the CDC and WHO guidelines. Four key factors i.e., demographic, economic, vulnerable groups and spatiality are considered for vaccine roll-out against limited supply. Among the vulnerable groups, the percent of households with disabilities and the poor are taken into consideration as the health workers and essential service providers are already been covered in the first phase of vaccination. Vaccine rollout strategies worldwide have overwhelmingly prioritized the descending age categories as they are the most vulnerable to COVID infection. Two major criticism to this mass-vaccination strategy is obvious. First, the supply of vaccines is limited against demand, and secondly, vaccine nationalization is an addition to the already strained supply chain. For example, India, the biggest producer of Oxford-AstraZeneca COVID-19 vaccine is prioritizing national demand over export. The economic cost of the pandemic is forecasted to aggravate due to unequal and limited supply of vaccines (see for example, [26]). Even after the third wave has leveled or even surpassed the first wave of the 2020s confirmed cases worldwide, a lockdown strategy is hardly an acceptable option due to economic and social costs, and lockdown fatigue. This, however, points to the importance of prioritizing the vulnerable groups, economic factors, and age-based vaccine rollout strategy.
Numerous studies link the number of COVID-19 cases to demographic factors, connectivity, exposed occupation, and urban poor and marginalized communities [11, 13, 14, 52]. Urban areas present a perfect combination of the aforementioned factors resulting in the soaring number of COVID-19 cases. However, urban areas contribute to more than 80% of the World's GDP, making it a priority for vaccine rollout. In the case of Bangladesh, urban areas present the largest concentration of industrial (i.e., ready-made garments) and service sector (i.e., transportation) employment of exposed nature, making vaccination the only way out for opening up economic activities and maintaining the functioning of the society.
Multi-criteria analysis using AHP of this study, therefore, accounts for the demographic, economic and vulnerability components to demonstrate spatial vaccine rollout strategy among 64 administrative districts in Bangladesh. The overlay of weighted sub-factors and factors identifies 14 high-priority districts for vaccine rollout (Figure 3). The 29 March 2021 press briefing by the Ministry of Health suggests that 29 of the 64 districts have the highest transmission trend in Bangladesh; 13 of which overlaps with the priority districts of this study. The findings of this study suggest that aside from the number of COVID-19 cases, population density (eigenvalue 0·20), percent of urban population (0·07), percent of the working-age population (0·11), and percent of industrial (0·09) and service sector employment (0·08) overwhelmingly indicate urban area a priority for vaccine rollout. This spatial distribution, however, is an indication that COVID-19 cases spread from urban centers to hinterland areas. Therefore, contrary to the finding of Boterman [12], our study shows a clear pattern of urbanization of cases, and thus, a priority for Bangladesh's national vaccination strategy.
In addition to the multi-criteria analysis for vaccine rollout, we consider the study districts spatially inter-connected. Therefore, the distance between the districts is inversely correlated with the COVID-19 transmission. We measured additional weight due to the inter-district distance factor (Figure 4). A total of 12 districts were identified as high-priority for vaccine rollout followed by 22 districts as medium priority. Similar to the multi-criteria analysis, the spatially high-priority districts comprise of the capital city Dhaka and the second-tier cities like Chittagong, Khulna, Rajshahi, and Rangpur. This, however, is an indication that urban population and population density are considerable factors for the vaccine roll-out strategy. Secondly, the priority districts include industrial and service center hubs like Narayanganj, Tangail and Munshiganj, meaning, the economic factors are accounted for in the spatial priority for vaccine roll-out.
The analysis presented in this study is at the district level due to a lack of data availability at a smaller scale. Several studies have highlighted the potential of cluster analysis for identifying the spatial distribution of COVID-19 cases at a small scale (see for example, [53, 54, 55]). Additionally, technological advancements like contract tracing applications have created new opportunities for identifying COVID-19 cases at a granular scale (see for example, [56, 57, 58]). GIS can play a critical role in mapping and visualizing the COVID-19 scenario at a spatial level. Thus, GIS is a visual aid in reaching a wider audience through cluster and spatial priority analysis, mapping and visualization in spatial policy regarding COVID-19. Despite the lack of granular scale analysis, this paper offers a sound methodological approach to spatial vaccine roll-out strategy against limited supply.
The Bangladesh government strategy has been mass-vaccination over the age of 40 (25 + as of 29 July 2021), which appears to be a mistake considering the uncertain and limited supply of vaccines. Therefore, it is pragmatic to have a national strategy that combines prolonged COVID-19 emergency preparedness, sustained economic activities, and reduced transmissibility against the shortage of vaccine supply. The data-driven spatial priority districts presented in this study can be a framework with ample opportunity for data addition and modification, and is replicable considering local and contextual priority for vaccine rollout strategy.
6. Conclusion
The COVID-19 vaccine shortage is to continue due to global high demand and limited supply. Bangladesh's mass-vaccination policy – currently, over the age of 25 – is sure to fall short of the COVID-19 vaccine supply. In a limited vaccine supply scenario, we have proposed an alternative spatial priority-based vaccine rollout strategy by weighing a combination of ten demographic, economic and vulnerability factors, and an additional spatial factor, for 64 districts of Bangladesh. The most significant factors of vaccine rollout strategy are the number of confirmed COVID-19 cases followed by population density, percent of the working-age people, percent of industrial and service sector employment, and percentage of the urban population. Based on the ten factors and a spatial distance factor, 12 districts were identified as high-priority, 22 as medium-priority and the rest as low-priority for vaccine rollout. A total of 9 of the 12 high-priority districts overlap with the findings of the Ministry of Health that marked 29 districts with the highest COVID-19 transmission trend. Our findings by no means recommend stopping mass vaccination but spatially prioritize vaccination against limited supply that can curb down COVID-19 transmission as well as keep the economy moving.
One of the major limitations of this study is the lack of granular scale analysis due to the lack of data availability. However, the methodological approach of this study can be applied on a small scale, and has ample opportunities for data aggregation while designing vaccine roll-out strategy according to any local context. Secondly, the study shows a spatial mapping of the COVID-19 factors weights as well as spatial connectivity as factors for virus transmission. This offers a practical method for creating a buffer within and between spatial units to curb COVID transmission through local suppressing measures. Finally, the proposed method can have broader application for spatial priority identification for suppressive and pro-active measures against other infectious and transmittable diseases like Tuberculosis and Dengue in Bangladesh and beyond.
Declarations
Author contribution statement
Showmitra Kumar Sarkar and Md. Manjur Morshed: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
We are thankful to the Editors of this journal and the anonymous reviewer for insightful comments and suggestions on the earlier version of this manuscript.
Footnotes
References
- 1.World Bank . 2021. Global Economic Prospects: Washington, DC. [Google Scholar]
- 2.Degeling C., Williams J., Carter S.M., Moss R., Massey P., Gilbert G.L., Shih P., Braunack-Mayer A., Crooks K., Brown D., McVernon J. Priority allocation of pandemic influenza vaccines in Australia – recommendations of 3 community juries. Vaccine. 2021;39:255–262. doi: 10.1016/j.vaccine.2020.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Center for Disease Control and Prevention . 2021. How CDC Is Making COVID-19 Vaccine Recommendations.https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations.html [Google Scholar]
- 4.Department of Health & Social Care . 2021. UK COVID-19 Vaccines Delivery Plan.https://www.gov.uk/government/publications/uk-covid-19-vaccines-delivery-plan [Google Scholar]
- 5.GAVI . 2021. COVAX Vaccine Roll-Out.https://www.gavi.org/covax-vaccine-roll-out [Google Scholar]
- 6.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Directorate General of Health Services . 2021. COVID-19 Vaccination Dashboard for Bangladesh.http://103.247.238.92/webportal/pages/covid19-vaccination-update.php [Google Scholar]
- 8.Mishra S.V., Gayen A., Haque S.M. COVID-19 and urban vulnerability in India. Habitat Int. 2020;103:102230. doi: 10.1016/j.habitatint.2020.102230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parvin F., Ali S.A., Hashmi S.N.I., Ahmad A. Spatial prediction and mapping of the COVID-19 hotspot in India using geostatistical technique. Spat. Inf. Res. 2021 [Google Scholar]
- 10.Sarkar S.K., Ekram K.M.M., Das P.C. Spatial modeling of COVID-19 transmission in Bangladesh. Spat. Inf. Res. 2021 [Google Scholar]
- 11.Islam T., Talukder A.K., Siddiqui N., Islam T. Tackling the COVID-19 pandemic : the Bangladesh perspective. J. Publ. Health Res. 2020;9:389–397. doi: 10.4081/jphr.2020.1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boterman W.R. Urban-rural polarisation in times of the corona outbreak? The early demographic and geographic patterns of the SARS-CoV-2 epidemic in the Netherlands, Tijdschr. Voor Econ. En Soc. Geogr. 2020;111:513–529. doi: 10.1111/tesg.12437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qiu Y., Chen X., Shi W. Impacts of social and economic factors on the transmission of coronavirus disease 2019 (COVID-19) in China. MedRxiv. 2020:1127–1172. doi: 10.1007/s00148-020-00778-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wade L. An unequal blow. Science (80-) 2020;368:700–703. doi: 10.1126/science.368.6492.700. [DOI] [PubMed] [Google Scholar]
- 15.Connolly C., Ali S.H., Keil R. On the relationships between COVID-19 and extended urbanization. Dialogues Hum. Geogr. 2020;10:213–216. [Google Scholar]
- 16.Sharifi A., Khavarian-Garmsir A.R. The COVID-19 pandemic: impacts on cities and major lessons for urban planning, design, and management. Sci. Total Environ. 2020;749:1–3. doi: 10.1016/j.scitotenv.2020.142391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yamey G., Schäferhoff M., Hatchett R., Pate M., Zhao F., McDade K.K. Ensuring global access to COVID-19 vaccines. Lancet. 2020;395:1405–1406. doi: 10.1016/S0140-6736(20)30763-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferguson N., Laydon D., Nedjati Gilani G., Imai N., Ainslie K., Baguelin M., Bhatia S., Boonyasiri A., Cucunuba Perez Z., Cuomo-Dannenburg G., Dighe A., Dorigatti I., Fu H., Gaythorpe K., Green W., Hamlet A., Hinsley W., Okell L., Van Elsland S., Thompson H., Verity R., Volz E., Wang H., Wang Y., Walker P., Walters C., Winskill P., Whittaker C., Donnelly C., Riley S., Ghani A. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. Imp. Coll. 2020:1–20. https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf COVID-19 Response Team. [Google Scholar]
- 19.Ahmed K. Guard; 2020. World’s Most Vulnerable in “Third Wave” for COVID-19 Support, Experts Warn.https://www.theguardian.com/global-development/2020/mar/20/worlds-most-vulnerable-in-third-wave-for-covid-19-support-warn-experts [Google Scholar]
- 20.Zhang S.X., Wang Y., Rauch A., Wei F. Unprecedented disruption of lives and work: health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatr. Res. 2020;288:112958. doi: 10.1016/j.psychres.2020.112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bollyky T.J., Gostin L.O., Hamburg M.A. The equitable distribution ofCOVID-19 therapeutics and vaccines. JAMA, J. Am. Med. Assoc. 2020;323:2462–2463. doi: 10.1001/jama.2020.6641. [DOI] [PubMed] [Google Scholar]
- 22.Nkengasong J.N., Ndembi N., Tshangela A., Raji T. COVID-19 vaccines: how to ensure Africa has access. Nature. 2020;586:197–199. doi: 10.1038/d41586-020-02774-8. [DOI] [PubMed] [Google Scholar]
- 23.Gostin L.O., Karim S.A., Mason Meier B. Facilitating access to a COVID-19 vaccine through global health law. J. Law Med. Ethics. 2020;48:622–626. doi: 10.1177/1073110520958892. [DOI] [PubMed] [Google Scholar]
- 24.Bassi L.L. Allocating COVID-19 vaccines globally: an urgent need. JAMA Health Forum. 2021;2 doi: 10.1001/jamahealthforum.2021.0105. e210105–e210105. [DOI] [PubMed] [Google Scholar]
- 25.Ritchie H., Ortiz-Ospina E., Beltekian D., Mathieu E., Hasell J., Macdonald B., Giattino C., Appel C., Roser M. Our World Data; 2020. Coronavirus Pandemic (COVID-19) - Statistics and Research. [Google Scholar]
- 26.Hafner M., Yerushalmi E., Fays C., Dufresne E., Van Stolk C. COVID-19 Cost Vaccine Natl; 2020. COVID-19 and the Cost of Vaccine Nationalism. [PMC free article] [PubMed] [Google Scholar]
- 27.The Lancet, Redefining vulnerability in the era of COVID-19. Lancet. 2020;395:1089. doi: 10.1016/S0140-6736(20)30757-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cao W., Chen C., Li M., Nie R., Lu Q., Song D., Li S., Yang T., Liu Y., Du B., Wang X. Important factors affecting COVID-19 transmission and fatality in metropolises. Publ. Health. 2021;190:e21–e23. doi: 10.1016/j.puhe.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Black A.J., Geard N., McCaw J.M., McVernon J., Ross J.V. Characterising pandemic severity and transmissibility from data collected during first few hundred studies. Epidemics. 2017;19:61–73. doi: 10.1016/j.epidem.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization . Who; 2020. Who Sage Roadmap for Prioritizing Uses of Covid 19 Vaccines in the Context of Limited Supply; pp. 1–13.https://apps.who.int/iris/bitstream/handle/10665/334299/WHO-2019-nCoV-SAGE_Framework-Allocation_and_prioritization-2020.1-eng.pdf [Google Scholar]
- 31.O’Neill A. Statista; 2021. Employment by Economic Sector in Bangladesh 2019.https://www.statista.com/statistics/438359/share-of-economic-sectors-in-the-gdp-in-bangladesh/ [Google Scholar]
- 32.Bangladesh Bank . 2017. The Real Economy. [Google Scholar]
- 33.Kong J.D., Tekwa E.W., Gignoux-Wolfsohn S.A. Social, economic, and environmental factors influencing the basic reproduction number of COVID-19 across countries. PLoS One. 2021;16:1–17. doi: 10.1371/journal.pone.0252373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Poirier C., Luo W., Majumder M.S., Liu D., Mandl K.D., Mooring T.A., Santillana M. The role of environmental factors on transmission rates of the COVID-19 outbreak: an initial assessment in two spatial scales. Sci. Rep. 2020;10:1–11. doi: 10.1038/s41598-020-74089-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Bank . 2021. The World Bank in Bangladesh (Overview)https://www.worldbank.org/en/country/bangladesh/overview [Google Scholar]
- 36.World Health Organization Coronavirus disease 2019 (COVID-19)- situation report – 49 (31 March 2020) WHO Bull. 2020;2019:1–19. https://pers.droneemprit.id/covid19/ [Google Scholar]
- 37.Hammami S., Zouhri L., Souissi D., Souei A., Zghibi A., Marzougui A., Dlala M. Application of the GIS based multi-criteria decision analysis and analytical hierarchy process (AHP) in the flood susceptibility mapping (Tunisia) Arab. J. Geosci. 2019;12 [Google Scholar]
- 38.Pourghasemi H.R., Pradhan B., Gokceoglu C. Application of fuzzy logic and analytical hierarchy process (AHP) to landslide susceptibility mapping at Haraz watershed, Iran. Nat. Hazards. 2012;63:965–996. [Google Scholar]
- 39.Sarkar S.K. COVID-19 susceptibility mapping using multicriteria evaluation. Disaster Med. Publ. Health Prep. 2020 doi: 10.1017/dmp.2020.175. [DOI] [PubMed] [Google Scholar]
- 40.Badillo-Rivera E.N., Fow-Esteves A.J., Alata-López F.E., Virú-Vásquez P.H., Medina-Acuña M.S. Environmental and social analysis as risk factors for the spread of the novel coronavirus (SARS-CoV-2) using remote sensing, GIS and analytical hierarchy process (AHP): case of Peru. MedRxiv. 2020:1–33. [Google Scholar]
- 41.Rahman M.R., Islam A.H.M.H., Islam M.N. Geospatial modelling on the spread and dynamics of 154 day outbreak of the novel coronavirus (COVID-19) pandemic in Bangladesh towards vulnerability zoning and management approaches, Model. Earth Syst. Environ. 2020;7:2059–2087. doi: 10.1007/s40808-020-00962-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Singh R., Avikal S. COVID-19: a decision-making approach for prioritization of preventive activities. Int. J. Health Manag. 2020;13:257–262. [Google Scholar]
- 43.Poudyal C.P., Chang C., Oh H.J., Lee S. Landslide susceptibility maps comparing frequency ratio and artificial neural networks: a case study from the Nepal Himalaya. Environ. Earth Sci. 2010;61:1049–1064. [Google Scholar]
- 44.Feizizadeh B., Blaschke T. GIS-multicriteria decision analysis for landslide susceptibility mapping: comparing three methods for the Urmia lake basin, Iran. Nat. Hazards. 2013;65:2105–2128. [Google Scholar]
- 45.Podvezko V. Application of AHP technique. J. Bus. Econ. Manag. 2009;10:181–189. [Google Scholar]
- 46.Saaty T.L. Archive of SID the analytic network process archive of SID. Network. 2006;1:1–26. http://www.springerlink.com/index/p9r45787g7u914n9.pdf [Google Scholar]
- 47.Lootsma F.A. Theory and Methodology Conflict resolution via pairwise comparison of concessions. Eur. J. Oper. Res. 1989;40:109–116. [Google Scholar]
- 48.Lane E.F., Verdini W.A. A consistency test for AHP decision makers. Decis. Sci. J. 1989;20:575–590. [Google Scholar]
- 49.Reis S., Yalcin A., Atasoy M., Nisanci R., Bayrak T., Erduran M., Sancar C., Ekercin S. Remote sensing and GIS-based landslide susceptibility mapping using frequency ratio and analytical hierarchy methods in Rize province (NE Turkey) Environ. Earth Sci. 2012;66:2063–2073. [Google Scholar]
- 50.Franek J., Kresta A. Judgment scales and consistency measure in AHP. Procedia Econ. Financ. 2014;12:164–173. [Google Scholar]
- 51.Saaty T.L. A scaling method for priorities in hierarchical structures. J. Math. Psychol. 1977;15:234–281. [Google Scholar]
- 52.Sarkar S.K. COVID-19 susceptibility mapping using multicriteria evaluation. Disaster Med. Publ. Health Prep. 2020:1–17. doi: 10.1017/dmp.2020.175. [DOI] [PubMed] [Google Scholar]
- 53.Liu M., Liu M., Li Z., Zhu Y., Liu Y., Wang X., Tao L., Guo X. The spatial clustering analysis of COVID-19 and its associated factors in mainland China at the prefecture level. Sci. Total Environ. 2021;777:145992. [Google Scholar]
- 54.Cordes J., Castro M.C. Spatial analysis of COVID-19 clusters and contextual factors in New York City. Spat. Spatiotemporal. Epidemiol. 2020;34:100355. doi: 10.1016/j.sste.2020.100355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ruiz-Correa S., López-Revilla R., Díaz-Barriga F., Marmolejo-Cossío F., del Carmen Robledo-Valero V., Hernández-Huérfano E.E., Álvarez-Rivera L., Rangel-Martínez M.L., Lutzow-Steiner M.Á., Ortiz-Vázquez L.A., Mendoza-Lara A.R., Olivo-Rodríguez M., Galván-Ramírez M.S., Morales-Neri Á.E., Martínez-Donjuan V.U., Cervantes-Irurzo M.I., Comas-García A., Hernández-Maldonado F., Aguilar-Acosta C. Health Sentinel: a mobile crowdsourcing platform for self-reported surveys provides early detection of COVID-19 clusters in San Luis Potosí, Mexico. Int. J. Med. Inf. 2021;153:104508. doi: 10.1016/j.ijmedinf.2021.104508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shahroz M., Ahmad F., Younis M.S., Ahmad N., Kamel Boulos M.N., Vinuesa R., Qadir J. COVID-19 digital contact tracing applications and techniques: a review post initial deployments. Transport Eng. 2021;5:100072. [Google Scholar]
- 57.Grekousis G., Liu Y. Digital contact tracing, community uptake, and proximity awareness technology to fight COVID-19: a systematic review. Sustain. Cities Soc. 2021;71:102995. doi: 10.1016/j.scs.2021.102995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fernández-Niño J.A., Economist C. Peña-Maldonado., Rojas-Botero M., Rodríguez-Villamizar L.A. Effectiveness of contact tracing to reduce fatality from COVID-19: preliminary evidence from Colombia. Publ. Health. 2021 doi: 10.1016/j.puhe.2021.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.