Abstract
Background
Phantom limb pain (PLP) is common and often accompanied by serious suffering. Current systematic‐review evidence suggests that recommended treatments are no more effective than placebo for reducing PLP. Given the difficulty in conducting a meta‐analysis for nonpharmacological treatments and the weak evidence for pharmacological treatments for PLP, consensus on the first‐line management of PLP needs to be reached using alternative methods.
Objective
To reach expert consensus and make recommendations on the effective management of PLP.
Design
A three‐round Delphi design was used.
Setting
The study was conducted using e‐mail and Google survey tool as the main methods of communication and providing feedback.
Participants
The study included 27 clinicians and researchers from various health disciplines who are experts in PLP management.
Method
Data were collected using three sequential rounds of anonymous online questionnaires where experts proposed and ranked the treatments for PLP. A consensus was reached on the treatments that were endorsed by 50% or more of the experts.
Results
Thirty‐seven treatments were proposed for the management of PLP at the beginning of the study. Consensus was reached on seven treatments that were considered effective for managing PLP and on two treatments that were considered ineffective. Graded motor imagery, mirror therapy, amitriptyline, sensory discrimination training, and use of a functional prosthesis were endorsed by most experts because of the available backing scientific evidence and their reported efficacy in clinical practice. Cognitive behavioral therapy and virtual reality training were endorsed by most experts because of their reported efficacy in clinical practice despite indicating a dearth of scientific evidence to support their ranking. Citalopram and dorsal root ganglion pulsed radiofrequency were rejected owing to a lack of relevant scientific evidence.
Conclusion
The results of this study suggest that the nonpharmacological treatments endorsed in this study may have an important role in the management of PLP.
Introduction
Phantom limb pain (PLP) ‐ pain felt in the missing portion of the amputated limb ‐ is a common phenomenon. 1 , 2 A recent systematic review and meta‐analysis indicates that PLP affects approximately 64% (95% CI, 60.01‐68.05) of people with amputations, thus making it the most common chronic pain condition in people with limb amputations. 3 Phantom limb pain is associated with personal suffering, interference with general daily activities, disability, and reduced health‐related quality of life. 4 , 5
Previous studies have argued that PLP is driven by ectopic‐impulse discharges from neuromas located in the residual limb, that is, peripheral mechanisms. 6 , 7 However, there are reports of persisting PLP despite the anaesthetizing of the neuroma. 8 In addition, PLP has been reported in congenital amputees who typically do not present with any nerve damage and in whom the development of a neuroma is unlikely. 9 This evidence suggests that peripheral mechanisms alone are not sufficient to explain PLP. Recent functional magnetic resonance imaging studies show that PLP may be maintained by maladaptive reorganization in the somatosensory and motor areas of the brain. 10 , 11 , 12 These studies suggest that treatments aimed at addressing maladaptive reorganization in the brain may provide pain relief.
PLP is classified as a neuropathic pain disorder in the International Classification of Diseases, Eleventh Revision (ICD‐11), and its pharmacological management is based on recommendations for neuropathic pain syndromes. 13 , 14 The National Institute for Health and Care Excellence guidelines for neuropathic pain were developed to align the assessment and management of neuropathic pain conditions to the best available evidence and to improve the quality and appropriateness of care. 15 However, current systematic review evidence suggests that three recommended pharmacological treatments (amitriptyline, duloxetine, and pregabalin) are no more effective than placebo for reducing PLP. 16 The lack of effectiveness of these treatments may be because they do not target maladaptive cortical reorganization, which has been shown to be strongly associated with the maintenance of PLP. 10 , 11 , 12 , 17 , 18 , 19
Few studies have evaluated the effectiveness of nonpharmacological treatments for reducing PLP in the last decade. However, the early evidence is promising for treatments such as graded motor imagery (GMI) and mirror therapy. 20 , 21 Given the difficulty in conducting a meta‐analysis of the nonpharmacological and interventional treatments for PLP (because of variations in study methodology, sample characteristics, treatment protocols, and the levels of risk of bias) and the weak evidence for pharmacological treatments for PLP, consensus on the first‐line management of PLP needs to be reached using alternative methods.
Aim
The aim of this study was to reach expert consensus and make recommendations on the effective treatments for PLP in people with limb amputations.
Methods
This study was conducted in accordance with the ethical principles of human research outlined in the Declaration of Helsinki. 22
Research Design
An expert‐consensus Delphi study using three sequential rounds of anonymous online questionnaires was conducted to identify expert‐recommended treatments for reducing PLP in people with limb amputations. The Delphi method is applicable when there is limited evidence on a specific topic of interest, allowing recommendations to be derived from the collective judgments of experts. 23
Research Setting
The study was conducted online, using e‐mail and the Google survey tool (https://www.google.com/forms) as the main methods of communication and providing feedback.
Participants
We targeted clinicians and researchers from developing and developed countries who are experts in PLP and who represented a range of health disciplines such as physiotherapy, psychology, occupational therapy, chiropractic, nursing, and medicine (eg, general practitioners and anesthesiologists). These disciplines are directly involved in pain management after amputations and would benefit from clinical practice guidelines and recommendations. 24 Experts were identified by screening the authors of published articles on PLP and seeking peer recommendations on leaders in PLP research and clinical practice. Currently there are no standardized criteria for defining an “expert” in Delphi studies. 23 However, the number of years of clinical experience and number of research publications have commonly been used as a proxy for participants' level of expertise. 25 Experts were considered eligible for inclusion in this study if they were 18 years or older at the time of recruitment and could communicate in the English language. Researchers were included in the study if they were the first author of at least one publication or coauthor of at least two publications on PLP. Clinicians were included if they had managed over 100 patients with PLP or had clinical experience of at least 2 years in PLP management. Only one list of criteria for either subgroup was required because the intention was to include both researchers and clinicians from different health disciplines.
Sample Size Determination
Currently, there are no guidelines or recommendations on the appropriate sample size for expert‐consensus Delphi studies, nor is there a standardized definition of a small or large sample size. 26 However, it is established that a minimum sample size of 10 experts who are representative of at least three disciplines is adequate for content validity. 27 In consideration of this, we targeted a purposive sample of 50 experts with the aim of obtaining a minimum sample of 20 experts (who were representative of at least three disciplines) at the end of the study. This sample size was chosen to ensure a fair representation of various health disciplines in this study and consequently generate a full spectrum of views on the topic. 28 , 29
Recruitment
An invitation outlining the details of the study and the eligibility criteria was sent to the identified experts (n = 63) via e‐mail. Experts who fulfilled the eligibility criteria and agreed to participate in the study were sent an electronic link to the survey where they completed the first round of the Delphi. In addition to the purposive sampling technique, we used snowball sampling where experts initially recruited by the researcher were encouraged to invite other experts meeting the studyʼs inclusion criteria from their professional circles to participate in this study. 30 The snowball sampling technique is appropriate for finding additional experts who might not be known by the researcher. 31 Furthermore, this sampling approach is thought to strengthen panelist retention, thus limiting the number of participants lost at follow‐up. 32
Instruments
We used a 5‐point Likert scale ranging between 1 and 5 (1 = Strongly agree; 2 = Agree; 3 = No opinion; 4 = Disagree; 5 = Strongly disagree) for experts to indicate their rating for statements provided during the second and third rounds of the Delphi. 33 This scale is efficient and easy to use and has been validated to facilitate the expertʼs rating of items in Delphi studies. 24 , 34
Data Collection
During the first round, each expert was sent an e‐mail asking them to propose all effective treatments for reducing PLP (Table 1). Responses to the first question were used to design a standardized questionnaire (listing all the proposed treatments) that formed the basis of the second round of the Delphi. During the second round, experts were asked to rank (on the 5‐point Likert‐type scale) whether each of the proposed treatments is effective for reducing PLP. We generated a variety of rationales for endorsing or rejecting each treatment, from which each expert was asked to select the rationale that best reflected their viewpoint (Table 1). Treatments that were considered effective by 50% or more of the experts were carried into the final round and the remainder were excluded. In the final round, experts were sent a summary of the responses and the list of treatments endorsed for managing PLP. Experts were asked to review their responses in light of the groupʼs opinion, following which a final decision on endorsed treatments for PLP was reached.
Table 1.
Questions and instructions sent to participants for each round of the Delphi study
| First round | ||||
| 1. What treatments would you propose for the management of PLP in people with limb amputations? | ||||
| Second Round | ||||
| 1. Would you say these treatment approaches are effective for reducing PLP in people with amputations? Please indicate your response by selecting one number on a scale of 1‐5. | ||||
| 1 = Strongly agree | 2 = Agree | 3 = No opinion | 4 = Disagree | 5 = Strongly disagree |
| 2. Please select from the provided list a rationale that best reflects your viewpoint for endorsing or rejecting each treatment. | ||||
| There is some scientific evidence supporting the effectiveness of the treatment | The treatment is effective in clinical practice | There is some scientific evidence supporting the effectiveness of the treatment and the treatment is effective in clinical practice | There is a lack of scientific evidence supporting the effectiveness of the treatment | The treatment is not effective in clinical practice |
| Third Round | ||||
| 1. Here are the results of the second round of the Delphi. Considering the groupʼs opinion, please review (if necessary) your ratings from the second round. | ||||
PLP = phantom limb pain.
Data Analysis
Data were coded and entered into an Excel spreadsheet for analysis. 35 Numerical demographic data were analyzed by calculating the median and ranges. We opted for this method of analysis because of the small study sample size. 36 The level of agreement on each treatment was expressed as a percentage. Consensus on each treatment was reached when 50% or more of the expects were in agreement. 37 The level of consensus was presented as low (≥50%‐60%), moderate (>60%‐70%), and high (>70%). 38 The remaining data were synthesized descriptively.
Results
Twenty‐seven experts participated in the study (response rate: 43%), and 20 (74%) completed the final round. Only two participating experts were recruited using snowball sampling. The experts who completed the study were anesthesiologists (n = 3), physiatrists (n = 3), psychologists (n = 2), neurologists (n = 2), physiotherapists (n = 8), nurse (n = 1), and occupational therapist (n = 1). Of these, 15 described themselves as clinician‐researchers, three described themselves as full‐time researchers, and two described themselves as full‐time clinicians. Full‐time researchers had a median of 8 (range: 2‐6) years of PLP research experience. Full‐time clinicians had a median of 2 (range: 2‐2) years of PLP clinical experience. Clinician‐researchers had a median of 8 (range: 2‐8) years of PLP clinical experience and 8 (range: 2‐8) years of PLP research experience. The countries in which the experts were based during data collection are presented in Figure 1.
Figure 1.
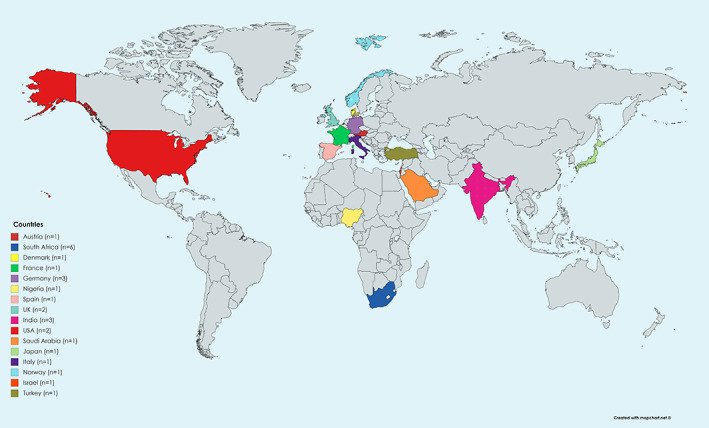
A representation of the countries in which the experts were based during data collection.
Treatments for Managing PLP
Treatments proposed by this group of experts for the management of PLP are presented in Table 2. Thirty‐seven treatments were proposed for the management of PLP at the beginning of the study. Consensus was reached on seven treatments that were considered effective for managing PLP, and on two treatments (citalopram [60%] and pulsed radiofrequency stimulation [PRFS] of the dorsal root ganglion [70%]) that were considered ineffective because of a lack of scientific evidence supporting their efficacy in people with PLP. Consensus was not reached on the remaining 28 treatments. The rationales and the number of experts who indicated their rationales for supporting each treatment are presented in Table 3. GMI, mirror therapy, and amitriptyline were endorsed by most experts because of the available supporting scientific evidence and their reported efficacy in clinical practice. Cognitive behavioral therapy (CBT), virtual reality training, and use of a functional prosthesis were endorsed by most experts because of their reported efficacy in clinical practice. However, this group of experts indicated that there is essentially no scientific evidence supporting the use of these treatments for PLP. The rationales for the effectiveness of sensory discrimination training were evenly distributed across the three domains (Table 3).
Table 2.
Treatments proposed by experts for the management of PLP
| Proposed treatments | Percentage of experts who endorsed each treatment in round 2 | Percentage of experts who endorsed each treatment in round 3 | Consensus reached? (Yes/No) | Level of consensus * |
|---|---|---|---|---|
| Nonpharmacological treatments | ||||
| Mirror therapy | 75 | 80 | Yes | High |
| Graded motor imagery | 70 | 75 | Yes | High |
| Cognitive behavioral therapy | 70 | 75 | Yes | High |
| Use of a functional prosthesis | 70 | 75 | Yes | High |
| Sensory discrimination training | 60 | 60 | Yes | Low |
| Virtual reality training | 60 | 75 | Yes | High |
| TENS† | 45 | ‐ | No | ‐ |
| Residual limb muscle exercises | 45 | ‐ | No | ‐ |
| Acceptance and commitment therapy | 45 | ‐ | No | ‐ |
| Mindfulness | 40 | ‐ | No | ‐ |
| Pain neuroscience education | 40 | ‐ | No | ‐ |
| Imagined limb‐movement exercises | 40 | ‐ | No | ‐ |
| Residual limb massage | 40 | ‐ | No | ‐ |
| Postamputation counseling | 35 | ‐ | No | ‐ |
| Active listening | 35 | ‐ | No | ‐ |
| Peripheral nerve stimulation | 35 | ‐ | No | ‐ |
| Targeted muscle reinnervation | 30 | ‐ | No | ‐ |
| Residual limb bandaging | 30 | ‐ | No | ‐ |
| Sympathetic nerve block | 30 | ‐ | No | ‐ |
| Left/right judgments | 25 | ‐ | No | ‐ |
| Dorsal root ganglion stimulation | 25 | ‐ | No | ‐ |
| Prosthesis electromagnetic shielding | 25 | ‐ | No | ‐ |
| Electromyogram biofeedback training | 20 | ‐ | No | ‐ |
| Progressive residual limb‐muscle relaxation | 15 | ‐ | No | ‐ |
| Spinal cord stimulation | 15 | ‐ | No | ‐ |
| Pharmacological treatments | ||||
| Amitriptyline | 50 | 65 | Yes | Moderate |
| Pregabalin | 45 | ‐ | No | ‐ |
| Gabapentin | 40 | ‐ | No | ‐ |
| Morphine | 35 | ‐ | No | ‐ |
| Ketamine | 30 | ‐ | No | ‐ |
| Intraforaminal infusion of dilute lidocaine | 30 | ‐ | No | ‐ |
| Fluoxetine | 15 | ‐ | No | ‐ |
| NSAIDs | 15 | ‐ | No | ‐ |
| Surgery | ||||
| Peripheral nerve surgeries | 35 | ‐ | No | ‐ |
| Residual limb surgical revision | 15 | ‐ | No | ‐ |
The level of consensus is presented as low (≥50%‐60%), moderate (>60%‐70%), or high (>70%).
NSAID = nonsteroidal anti‐inflammatory drug; PLP = phantom limb pain; TENS = transcutaneous electrical nerve stimulation.
Table 3.
The rationales and percentage of experts who provided supporting rationale for each treatment
| Treatment | The percentage of experts who provided a rationale for supporting each treatment | Total percentage of experts who provided supporting rationale for treatment | ||
|---|---|---|---|---|
| There is some scientific evidence supporting the effectiveness of the treatment | The treatment is effective in clinical practice | There is some scientific evidence supporting the effectiveness of the treatment and the treatment is effective in clinical practice | ||
| Mirror therapy | 21.1 | 15.8 | 57.9 | 94.8 |
| Graded motor imagery | 26.3 | 26.3 | 42.1 | 94.7 |
| Cognitive behavioral therapy | 5.3 | 36.8 | 36.8 | 78.9 |
| Sensory discrimination training | 21.1 | 21.1 | 26.3 | 68.5 |
| Virtual reality treatment | 10.5 | 36.8 | 21.1 | 68.4 |
| Use of functional prosthesis | 22.2 | 16.7 | 27.8 | 66.7 |
| Amitriptyline | 23.5 | 5.9 | 35.3 | 64.7 |
Discussion
Considering the lack of robust evidence on the management of PLP, we used a Delphi approach to reach expert consensus on the effective treatments for PLP in people with limb amputations. Expert consensus was reached on seven treatments that were considered effective for reducing PLP and on two treatments that were considered ineffective. Treatments that were endorsed in this study are mirror therapy, GMI, CBT, virtual reality training, sensory discrimination training, amitriptyline, and a use of a functional prosthesis. An important consideration is that the experts included in this study were highly experienced and part of a representative panel of health care professionals involved in the management of patients with PLP. The representation of a variety of pain‐treatment classifications in this study indicates an interdisciplinary approach to the management of PLP. 39 To the best of our knowledge, this is the first Delphi study to reach expert consensus on the effective treatment strategies for PLP in people with amputations.
Six of the seven treatments endorsed by experts in this study are nonpharmacologically based. This is perhaps not surprising because of the available strong evidence negating the efficacy of currently available pharmacological treatments in managing PLP, as well as the growing evidence of the positive effects of the nonpharmacological interventions endorsed in this study. 16 , 40 The results of this study support the role of nonpharmacological treatments in PLP management.
A high level of expert‐consensus was reached on mirror therapy. Mirror therapy is a movement representation technique that uses the reflection of voluntary movements of the intact limb to provide an illusion that movement of an amputated limb was performed without pain or hindrance. 41 Mirror therapy is proposed to address maladaptive cortical reorganization in the corresponding primary motor cortex. The maladaptive cortical reorganization is theorized to trigger a protective pain response because of a mismatch between movement intent, proprioception, and visual feedback from the amputated limb. 11 , 12 , 17 , 42 The visual feedback provided by mirror therapy appears to be a key component in reducing PLP, because pain reductions are not seen when limb exercises are conducted with a covered mirror. 43 , 44 , 45 It is hypothesized that the firing of mirror neurons while observing movement provides the perception of movement in the amputated limb, consequently resolving the conflict between movement intent, proprioception, and visual feedback. 46 , 47 A substantial amount of the literature on mirror therapy is based on case studies, most of which show positive outcomes. 48 , 49 , 50 , 51 , 52 , 53 The most recent systematic review on mirror therapy identified four controlled trials and all reported statistically significant improvements in PLP. 54 However, only one of these showed clinically significant reductions in pain (of 3 or more points on a 0‐10 visual analog scale) at the conclusion of treatment. 55 The expert‐recommendations provided in this study align with the supporting evidence and reported effectiveness of mirror therapy in clinical practice. However, it is worth cautioning that a few patients may experience increased pain severity following mirror therapy. 53 , 56 Initiating mirror therapy prior to progressively addressing the maladaptive changes in the sensory and premotor cortices is theorized to trigger a protective pain response that results in increased pain severity during or after treatment. 57 Based on the theory of alterations in the sensory, premotor and motor cortex representation of the amputated limb contributing to PLP, GMI may be a viable alternative with a lower risk of pain exacerbation.
GMI, a three‐step program that purportedly addresses maladaptive changes in the sensory, premotor and primary motor cortices using a graded sequence of left/right limb judgments, imagined limb movements, and mirror therapy, 57 was also supported by a high level of expert consensus. Maladaptive changes in these cortical areas have been positively associated with pain severity. 11 Targeting these changes using mirror therapy 58 and mental imagery, 17 both components of the GMI program, has been shown to result in pain reduction. It is hypothesized the progressive activation of the somatosensory and motor networks using GMI may prevent the triggering of a pain response reported by some patients undergoing mirror therapy only. 57 It would be valuable to determine whether there is a significant difference in the efficacy of GMI and mirror therapy. However, to date, there is no published study comparing these treatments. The only three randomized controlled trials on GMI for PLP showed clinically significant pain reductions at the end of treatment and at 6‐month follow‐up. 57 , 59 , 60 The high level of expert consensus in this Delphi study and the promising body of literature on GMI provide the basis for recommending GMI for managing PLP. However, further rigorous studies with a larger sample size are required to build upon the existing literature.
Virtual reality training is another treatment that uses visuo‐proprioceptive feedback from a virtual reality headset to manage PLP,61 which had high support from the expert panel. Virtual reality training may be preferable over traditional mirror therapy because of its utility during functional tasks (eg, walking). 61 In addition, virtual reality training enables patients to perform unsynchronized limb movements that are realistic and may provide richer somatosensory feedback essential for reducing pain. 62 The study of virtual reality in people with PLP is in its infancy, and the quality of evidence for this intervention is low; the evidence is based mostly on case‐control and case‐series studies, and no randomized controlled trials could be found. 63 Although clinically significant pain reductions have been reported, they appear to be momentary, with some studies reporting recurring pain a few hours after treatment. 61 , 64 , 65 Currently, there is no standardized protocol for virtual reality and its long‐term effects are unknown. However, the high level of expert consensus for the effectiveness of virtual reality training in clinical practice may warrant further studies to elucidate the effectiveness of virtual reality training in PLP management.
We found it interesting that a high level of expert consensus was reached on CBT because of its reported efficacy in clinical practice, although the experts indicated a dearth of scientific evidence to support their ranking. Indeed, we could not find any published studies that examined the efficacy of CBT for reducing PLP in people with amputations. However, there is adequate evidence to support the use of CBT in the management of other chronic pain conditions. 66 , 67 , 68 , 69 , 70 At this time, the mechanisms by which CBT reduces pain are unclear. 70 It appears that the treatment principles of CBT are in line with the Neuromatrix theory of pain, that emphasizes the role of cognitive, affective, and behavioral influences in the development and maintenance of chronic pain. 71 CBT generally improves clinical outcomes by modifying dysfunctional emotions, thoughts, and behaviors. 72 Given that amputees with PLP often present with risk factors such as depression, feelings of helplessness, and debilitating passive coping strategies, 73 , 74 it is likely that CBT targets these factors with a secondary improvement in PLP severity. The precise mechanism of action needs to be confirmed in future studies.
The use of a functional prosthesis also had high support for its reported efficacy in clinical practice despite the experts indicating a lack of scientific evidence. However, unlike CBT, the benefits of using a functional prosthesis that provides proprioceptive feedback to the residual limb during functional activities (eg, walking, lifting a cup) have been repeatedly documented in the last decade. 75 , 76 , 77 , 78 , 79 , 80 , 81 The literature shows that using a functional prosthesis is more effective than a cosmetic prosthesis for improving pain and function. 75 , 76 , 82 , 83 , 84 , 85 , 86 These findings suggest that ongoing stimulation, muscular training, and visual feedback provided by a functional prosthesis may have an important role in addressing the mechanisms proposed to maintain PLP. 75 , 81 In fact, a mechanistic neuroimaging study 87 revealed cortical reorganization in patients after starting to use a functional prosthesis that provided somatosensory feedback. Neuroimaging revealed a normalization of the cortical representation of the amputated limb that was positively associated with a reduction in PLP. 87 Furthermore, patients using prostheses with proprioceptive feedback reported improved embodiment (feeling of bodily ownership and control) of the prosthesis. The improved embodiment is thought to be essential in the improvement of PLP and function after limb amputation. 85 , 86 The high level of expert consensus for the use of a functional prosthesis in this study is in line with the positive findings in the literature. These findings provide a basis for recommending the use of a functional prosthesis that provides somatosensory feedback in the rehabilitation of people with amputations.
Sensory discrimination training is the only nonpharmacological treatment that had a low level of expert consensus on its effectiveness for reducing PLP in this study. Sensory discrimination training is a technique that uses fabrics of different softness/harshness (eg, cotton vs. velcro) to provide sensory input to areas adjacent to the distal part of the residual limb. 88 , 89 The treatment is proposed to normalize cortical reorganization by addressing a mismatch between the brainʼs sensory output and sensory feedback from the amputated limb. 41 , 90 , 91 , 92 The pain‐relieving effects of sensory discrimination training have been reported in only three available studies. 88 , 89 , 93 Therefore, a definitive conclusion on the efficacy of this treatment cannot be drawn because of a lack of evidence. However, the results of a recent study 93 suggest that home‐based sensory discrimination training may be a useful supplement to already existing therapies, such as GMI and mirror therapy.
The appropriateness of pharmacological treatments in the management of PLP have been placed in doubt because they are typically ineffective. 94 This is possibly reflected by amitriptyline being the only pharmacological treatment endorsed in this study despite almost half of the participant in this study being prescribers. Although amitriptyline is commonly used in the management of PLP, studies investigating its efficacy for reducing PLP are essentially nonexistent. 95 The most recent systematic review on pharmacological treatments for PLP identified only one relevant study. 16 The study investigated amitriptyline (titrated up to 125 mg/d for 6 weeks) versus active placebo (benztropine mesylate) for reducing chronic PLP (PLP persisting for more than 3 months). 95 The results showed that amitriptyline was no more effective than placebo for reducing chronic PLP. Overall, the rating for the effectiveness of amitriptyline for reducing PLP in this study indicates the dissonance between clinical practice guidelines and the available scientific evidence for PLP. 96
It is worth noting that two treatments (citalopram and PRFS of the dorsal root ganglion) had moderate‐high level expert consensus rejecting their efficacy for reducing PLP. Pulsed radiofrequency stimulation of the dorsal root ganglion is an invasive procedure with known adverse effects such as neurological fallout and increased pain. 97 Considering that there are safer and more effective interventions for PLP, it may not be ideal to use this treatment in a vulnerable group of people with amputations. Likewise, considering that citalopram has similar mechanisms to those of amitriptyline (ie, inhibiting the reuptake of serotonin at the synapse), it is likely that it may not yield clinically significant improvements in PLP. 98
Limitations
A withdrawal of seven experts after the first round may have been precipitated by the requirement to comment on treatments not within their scope of practice. This may have led to a nonresponse bias, in that experts who did not complete the study may have different viewpoints from those who completed the study. However, the descriptive analysis of responses generated in Round 1 showed no outlier views. We generated a variety of rationales for endorsing or rejecting each treatment, from which each expert selected the rationale that best reflected their viewpoint. We acknowledge that this might have limited the experts to fully express their opinions on the efficacy of each treatment. It would have been valuable to report on treatments endorsed by each profession. However, we could not perform subgroup analyses by profession because of the small sample size in each professional category. The level of expertise that informed the rating of treatments (pharmacological vs. nonpharmacological) varied between experts. Therefore, this variation may have influenced the results. We included option three of the Likert scale (“No opinion”) for experts to select if they had insufficient knowledge to inform their decision on a specific treatment. Using the option “no expertise in this area” instead would have provided more clarity. Injectates (eg, phenol, botulinum, and etanercept) were not proposed in this study. This may have limited the experts' opinion on the efficacy of these treatments for reducing PLP. Lastly, this study does not provide any suggestions on the dosage and methods of administration as this was not the aim. Follow‐up studies are indicated to explore dosage recommendations.
Conclusion
The results of this study suggest that nonpharmacological and noninterventional treatments: GMI, mirror therapy, CBT, virtual reality training, use of a functional prosthesis, and sensory discrimination training may have an important role in the management of PLP. There is evidence showing that these endorsed treatments reduce PLP by addressing neural mechanisms in the brain, emphasizing the dominant role of cortical reorganization in PLP. We found it interesting that experts proposed CBT as an effective treatment for PLP despite a paucity of scientific evidence to support its use in people with PLP. Given that pain is a biopsychosocial construct, it might be beneficial to examine the effects of psychological treatments and their specific mechanisms for reducing PLP. Some of the experts in this study provided additional feedback suggesting that most of the presented treatments have a meaning effect and thereby may work directly through meaning responses or that their effect may be augmented by a meaning response. Proving that a treatment has active efficacy (efficacy beyond meaning) requires the use of valid shams, which are often expensive and sometimes impossible. Therefore, we recommend that future studies must fully engage with developing valid sham treatments to explore the direct effect of the treatment and the meaning response.
In this study, expert consensus was reached to support the use of GMI, mirror therapy, CBT, virtual reality training, use of a functional prosthesis, sensory discrimination training, and amitriptyline in the management of PLP. The evidence on treatments for PLP is lacking, and further research on the treatments recommended based on their clinical efficacy is warranted.
CME Question.
Based on the results of expert consensus, which intervention for phantom limb pain is considered ineffective?
Use of a functional prosthesis
Dorsal root ganglion pulsed radiofrequency
Sensory discrimination training
Graded motor imagery
Answer online at https://onlinelearning.aapmr.org/
Acknowledgments
We thank the experts for their time and commitment to providing constructive input in this study. We thank Gillian J Bedwell for reviewing and editing this manuscript.
Disclosure: nothing to disclose
Sources of financial support: Start‐up Emerging Researcher Award, University of Cape Town.
Ethical approval to conduct this study was granted by the University of Cape Town, Faculty of Health Sciences, Human Research Ethics Committee (HREC ref: 355/2019).
All financial disclosures and CME information related to this article can be found on the Online Learning Portal (https://onlinelearning.aapmr.org/) prior to accessing the activity.
Footnotes
This journal‐based CME activity is designated for 1.0 AMA PRA Category 1 Credit and can be completed online at https://onlinelearning.aapmr.org/. This activity is FREE to AAPM&R members and available to nonmembers for a nominal fee. For assistance with claiming CME for this activity, please contact (847) 737‐6000.
Contributor Information
Katleho Limakatso, Email: katleho.limakatso@uct.ac.za.
Romy Parker, Email: romy.parker@uct.ac.za.
References
- 1. Hanyu‐Deutmeyer AA, Dulebohn SC. Pain, phantom limb. 2017. www.ncbi.nlm.nih.gov/books/NBK448188/. Accessed July 22, 2020.
- 2. Subedi B, Grossberg GT. Phantom limb pain: mechanisms and treatment approaches. Pain Res Treat. 2011;2011:864605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Limakatso K, Bedwell GJ, Madden VJ, Parker R. The prevalence and risk factors for phantom limb pain in people with amputations: A systematic review and meta‐analysis. PLoS One. 2020;15(10):e0240431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fuchs X, Flor H, Bekrater‐Bodmann R. Psychological factors associated with phantom limb pain: a review of recent findings. Pain Res Manag. 2018;2018:5080123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Björkman B, Lund I, Arnér S, Hydén L‐C. Phantom phenomena – their perceived qualities and consequences from the patientʼs perspective. Scand J Pain. 2012;3(3):134‐140. [DOI] [PubMed] [Google Scholar]
- 6. Bek D, Demiralp B, Kömürcü M, Ateşalp S. The relationship between phantom limb pain and neuroma. Acta Orthop Traumatol Turc. 2006;40(1):44‐48. [PubMed] [Google Scholar]
- 7. Vaso A, Adahan H‐M, Gjika A, et al. Peripheral nervous system origin of phantom limb pain. PAIN. 2014;155(7):1384‐1391. [DOI] [PubMed] [Google Scholar]
- 8. Siddiqui S, Sifonios AN, Le V, Martinez ME, Eloy JD, Kaufman AG. Development of phantom limb pain after femoral nerve block. Case Rep Med. 2014;2014:238453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Melzack R, Israel R, Lacroix R, Schultz G. Phantom limbs in people with congenital limb deficiency or amputation in early childhood. Brain. 1997;120(9):1603‐1620. [DOI] [PubMed] [Google Scholar]
- 10. Andoh J, Diers M, Milde C, Frobel C, Kleinböhl D, Flor H. Neural correlates of evoked phantom limb sensations. Biol Psychol. 2017;126:89‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Flor H, Nikolajsen L, Jensen TS. Phantom limb pain: a case of maladaptive CNS plasticity? Nat Rev Neurosci. 2006;7(11):873. [DOI] [PubMed] [Google Scholar]
- 12. Karl A, Birbaumer N, Lutzenberger W, Cohen LG, Flor H. Reorganization of motor and somatosensory cortex in upper extremity amputees with phantom limb pain. J Neurosci. 2001;21(10):3609‐3618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Finnerup NB, Otto M, Jensen TS, Sindrup SH. An evidence‐based algorithm for the treatment of neuropathic pain. MedGenMed. 2007;9(2):36. [PMC free article] [PubMed] [Google Scholar]
- 14. Scholz J, Finnerup NB, Attal N, et al. The IASP classification of chronic pain for ICD‐11: chronic neuropathic pain. Pain. 2019;160(1):53‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Centre for Clinical Practice at NICE (UK) . Neuropathic Pain: The Pharmacological Management of Neuropathic Pain in Adults in Non‐Specialist Settings. London: National Institute for Health and Care Excellence, (UK); 2010. [PubMed] [Google Scholar]
- 16. Alviar MJM, Hale T, Dungca M. Pharmacologic interventions for treating phantom limb pain. Cochrane Database Syst Rev. 2016;10(10):CD006380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lotze M, Flor H, Grodd W, Larbig W, Birbaumer N. Phantom movements and pain an fMRI study in upper limb amputees. Brain. 2001;124(11):2268‐2277. [DOI] [PubMed] [Google Scholar]
- 18. Flor H, Elbert T. Phantom‐limb pain as a perceptual correlate of cortical reorganization following arm amputation. Nature. 1995;375(6531):482. [DOI] [PubMed] [Google Scholar]
- 19. MacIver K, Lloyd D, Kelly S, Roberts N, Nurmikko T. Phantom limb pain, cortical reorganization and the therapeutic effect of mental imagery. Brain. 2008;131(8):2181‐2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Thieme H, Morkisch N, Rietz C, Dohle C, Borgetto B. The efficacy of movement representation techniques for treatment of limb pain—a systematic review and meta‐analysis. J Pain. 2016;17(2):167‐180. [DOI] [PubMed] [Google Scholar]
- 21. Bowering KJ, OʼConnell NE, Tabor A, et al. The effects of graded motor imagery and its components on chronic pain: a systematic review and meta‐analysis. J Pain. 2013;14(1):3‐13. [DOI] [PubMed] [Google Scholar]
- 22. General Assembly of the World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dent. 2014;81(3):14. [PubMed] [Google Scholar]
- 23. Avella JR. Delphi panels: research design, procedures, advantages, and challenges. Int J Doct Stud. 2016;11(1):305‐321. [Google Scholar]
- 24. Hsu C‐C, Sandford BA. The Delphi technique: making sense of consensus. Pract. Assess., Res. Eval. 2007;12(10):1‐8. [Google Scholar]
- 25. Heiko A. Consensus measurement in Delphi studies: review and implications for future quality assurance. Technol Forecast Soc Change. 2012;79(8):1525‐1536. [Google Scholar]
- 26. Wilhelm WJ. Alchemy of the oracle: the Delphi technique. Delta Pi Epsilon J. 2001;43(1):6‐26. [Google Scholar]
- 27. de Villiers MR, de Villiers PJ, Kent AP. The Delphi technique in health sciences education research. Med Teach. 2005;27(7):639‐643. [DOI] [PubMed] [Google Scholar]
- 28. McIntyre‐Hite L. A Delphi study of effective practices for developing competency‐based learning models in higher education. J Competency‐Based Educ. 2016;1(4):157‐166. [Google Scholar]
- 29. Løhre ET, Klepstad P, Bennett MI, et al. From “breakthrough” to “episodic” cancer pain? A European Association for Palliative Care Research Network Expert Delphi Survey toward a common terminology and classification of transient cancer pain exacerbations. J Pain Symptom Manage. 2016;51(6):1013‐1019. [DOI] [PubMed] [Google Scholar]
- 30. Heckathorn DD. Comment: snowball versus respondent‐driven sampling. Sociol Methodol. 2011;41(1):355‐366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sharma G. Pros and cons of different sampling techniques. Int J Appl Res. 2017;3(7):749‐752. [Google Scholar]
- 32. Rowe G, Wright G. The Delphi technique: Past, present, and future prospects—introduction to the special issue. Technol Forecast Soc Change. 2011;78(9):1487‐1490. [Google Scholar]
- 33. Johns R. Likert items and scales. Survey Question Bank: Methods Fact Sheet. 2010;1:1‐11. [Google Scholar]
- 34. Giannarou L, Zervas E. Using Delphi technique to build consensus in practice. Int J Business Sci Appl Manage. 2014;9(2):65‐82. [Google Scholar]
- 35. StatSoft, I. , STATISTICA (data analysis software system), version 6. Tulsa, USA, 2001. 150 .
- 36. Morgan CJ. Use of proper statistical techniques for research studies with small samples. Am J Physiol Lung Cell Mol Physiol. 2017;313(5):L873‐L877. [DOI] [PubMed] [Google Scholar]
- 37. Ramos D, Arezes P, Afonso P. Application of the Delphi method for the inclusion of externalities in occupational safety and health analysis. Dyna. 2016;83(196):14‐20. [Google Scholar]
- 38. Diamond IR, Grant RC, Feldman BM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67(4):401‐409. [DOI] [PubMed] [Google Scholar]
- 39. Goesling J, Lin LA, Clauw DJ. Psychiatry and pain management: at the intersection of chronic pain and mental health. Curr Psychiatry Rep. 2018;20(2):12. [DOI] [PubMed] [Google Scholar]
- 40. Finnerup NB, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta‐analysis. Lancet Neurol. 2015;14(2):162‐173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ramachandran VS, Brang D, McGeoch PD. Size reduction using mirror visual feedback (MVF) reduces phantom pain. Neurocase. 2009;15(5):357‐360. [DOI] [PubMed] [Google Scholar]
- 42. Chan AW‐Y, Bilger E, Griffin S, et al. Visual responsiveness in sensorimotor cortex is increased following amputation and reduced after mirror therapy. Neuroimage Clin. 2019;23:101882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Chan BL, Witt R, Charrow AP, et al. Mirror therapy for phantom limb pain. N Engl J Med. 2007;357(21):2206‐2207. [DOI] [PubMed] [Google Scholar]
- 44. Finn SB, Perry BN, Clasing JE, et al. A randomized, controlled trial of mirror therapy for upper extremity phantom limb pain in male amputees. Front Neurol. 2017;8:267‐267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ramadugu S, Nagabushnam SC, Katuwal N, Chatterjee K. Intervention for phantom limb pain: a randomized single crossover study of mirror therapy. Indian J Psychiatry. 2017;59(4):457‐464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rossi S, Tecchio F, Pasqualetti P, et al. Somatosensory processing during movement observation in humans. Clin Neurophysiol. 2002;113(1):16‐24. [DOI] [PubMed] [Google Scholar]
- 47. Rizzolatti G, Fogassi L, Gallese V. Mirrors of the mind. Sci Am. 2006;295(5):54‐61. [DOI] [PubMed] [Google Scholar]
- 48. Kim SY, Kim YY. Mirror therapy for phantom limb pain. Korean Journal Pain. 2012;25(4):272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Darnall BD. Self‐delivered home‐based mirror therapy for lower limb phantom pain. Am J Phys Med Rehabil. 2009;88(1):78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Anghelescu DL, Kelly CN, Steen BD, et al. Mirror therapy for phantom limb pain at a pediatric oncology institution. Rehabil Oncol. 2016;34(3):104‐110. [PMC free article] [PubMed] [Google Scholar]
- 51. Clerici CA, Spreafico F, Cavallotti G, et al. Mirror therapy for phantom limb pain in an adolescent cancer survivor. Tumori. 2012;98(1):e27‐e30. [DOI] [PubMed] [Google Scholar]
- 52. Wilcher DG, Chernev I, Yan K. Combined mirror visual and auditory feedback therapy for upper limb phantom pain: a case report. J Med Case Rep. 2011;5(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mercier C, Sirigu A. Training with virtual visual feedback to alleviate phantom limb pain. Neurorehabil Neural Repair. 2009;23(6):587‐594. [DOI] [PubMed] [Google Scholar]
- 54. Herrador Colmenero L, Perez Marmol JM, Martí‐García C, et al. Effectiveness of mirror therapy, motor imagery, and virtual feedback on phantom limb pain following amputation: a systematic review. Prosthetics and orthotics international. 2018;42(3):288‐298. [DOI] [PubMed] [Google Scholar]
- 55. Tilak M, Isaac SA, Fletcher J, et al. Mirror therapy and transcutaneous electrical nerve stimulation for management of phantom limb pain in amputees—a single blinded randomized controlled trial. Physiother Res Int. 2016;21(2):109‐115. [DOI] [PubMed] [Google Scholar]
- 56. Darnall BD, Li H. Home‐based self‐delivered mirror therapy for phantom pain: a pilot study. J Rehabil Med. 2012;44(3):254‐260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Moseley GL. Graded motor imagery for pathologic pain: a randomized controlled trial. Neurology. 2006;67(12):2129‐2134. [DOI] [PubMed] [Google Scholar]
- 58. Foell J, Bekrater‐Bodmann R, Diers M, Flor H. Mirror therapy for phantom limb pain: brain changes and the role of body representation. Eur J Pain. 2014;18(5):729‐739. [DOI] [PubMed] [Google Scholar]
- 59. Limakatso K, Madden VJ, Manie S, Parker R. The effectiveness of graded motor imagery for reducing phantom limb pain in amputees: a randomised controlled trial. Physiotherapy. 2019;109:65–74. [DOI] [PubMed] [Google Scholar]
- 60. Hinkel M. Graded motor imagery for the treatment of phantom limb pain. Arch. Phys. Med. Rehabil. 2017;98(10):e72. [Google Scholar]
- 61. Ambron E, Miller A, Kuchenbecker KJ, Buxbaum LJ, Coslett H. Immersive low‐cost virtual reality treatment for phantom limb pain: evidence from two cases. Front Neurol. 2018;9:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Perry BN, Mercier C, Pettifer SR, Cole J, Tsao JW. Virtual reality therapies for phantom limb pain. Eur J Pain. 2014;18(7):897‐899. [DOI] [PubMed] [Google Scholar]
- 63. Dunn J, Yeo E, Moghaddampour P, Chau B, Humbert S. Virtual and augmented reality in the treatment of phantom limb pain: a literature review. NeuroRehabilitation. 2017;40(4):595‐601. [DOI] [PubMed] [Google Scholar]
- 64. Rutledge T, Velez D, Depp C, et al. A virtual reality intervention for the treatment of phantom limb pain: development and feasibility results. Pain Med. 2019;20(10):2051‐2059. [DOI] [PubMed] [Google Scholar]
- 65. Ortiz‐Catalan M, Sander N, Kristoffersen MB, Håkansson B, Brånemark R. Treatment of phantom limb pain (PLP) based on augmented reality and gaming controlled by myoelectric pattern recognition: a case study of a chronic PLP patient. Front Neurosci. 2014;8:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Vitoula K, Venneri A, Varrassi G, et al. Behavioral therapy approaches for the management of low back pain: an up‐to‐date systematic review. Pain Ther. 2018;7(1):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Knoerl R, Lavoie Smith EM, Weisberg J. Chronic pain and cognitive behavioral therapy: an integrative review. West J Nurs Res. 2016;38(5):596‐628. [DOI] [PubMed] [Google Scholar]
- 68. Ehde DM, Dillworth TM, Turner JA. Cognitive‐behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol. 2014;69(2):153‐166. [DOI] [PubMed] [Google Scholar]
- 69. Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: A review of meta‐analyses. Cognit Ther Res. 2012;36(5):427‐440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Williams A, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012;11(11):CD007407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Melzack R. Pain and the neuromatrix in the brain. J Dent Educ. 2001;65(12):1378‐1382. [PubMed] [Google Scholar]
- 72. Fenn K, Byrne M. The key principles of cognitive behavioural therapy. InnovAiT. 2013;6(9):579‐585. [Google Scholar]
- 73. Ahmed A, Bhatnagar S, Mishra S, Khurana D, Joshi S, Ahmad SM. Prevalence of phantom limb pain, stump pain, and phantom limb sensation among the amputated cancer patients in India: a prospective, observational study. Indian J Palliat Care. 2017;23(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Richardson C, Glenn S, Nurmikko T, Horgan M. Incidence of phantom phenomena including phantom limb pain 6 months after major lower limb amputation in patients with peripheral vascular disease. Clin J Pain. 2006;22(4):353‐358. [DOI] [PubMed] [Google Scholar]
- 75. Dietrich C, Nehrdich S, Seifert S, et al. Leg prosthesis with somatosensory feedback reduces phantom limb pain and increases functionality. Front Neurol. 2018;9:270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Dietrich C, Walter‐Walsh K, Preißler S, et al. Sensory feedback prosthesis reduces phantom limb pain: proof of a principle. Neurosci Lett. 2012;507(2):97‐100. [DOI] [PubMed] [Google Scholar]
- 77. Tyler DJ. Neural interfaces for somatosensory feedback: bringing life to a prosthesis. Curr Opin Neurol. 2015;28(6):574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Klaes C, Shi Y, Kellis S, Minxha J, Revechkis B, Andersen RA. A cognitive neuroprosthetic that uses cortical stimulation for somatosensory feedback. J Neural Eng. 2014;11(5):056024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Hsiao SS, Fettiplace M, Darbandi B. Sensory feedback for upper limb prostheses. Prog Brain Res. 2011;192:69‐81. [DOI] [PubMed] [Google Scholar]
- 80. Svensson P, Wijk U, Björkman A, Antfolk C. A review of invasive and non‐invasive sensory feedback in upper limb prostheses. Expert Rev Med Devices. 2017;14(6):439‐447. [DOI] [PubMed] [Google Scholar]
- 81. Preißler S, Dietrich C, Seifert S, Hofmann GO, Miltner WH, Weiss T. The feeling prosthesis—somatosensory feedback from the prosthesis foot reduces phantom limb pain dramatically. Pain Med. 2018;19(8):1698‐1700. [DOI] [PubMed] [Google Scholar]
- 82. Hoffer, J.A. , Electrical stimulation system and methods for treating phantom limb pain and for providing sensory feedback to an amputee from a prosthetic limb. 2007, Google Patents.
- 83. Murray C. Amputation, Prosthesis Use, and Phantom Limb Pain: An Interdisciplinary Perspective. Vol 14. Berlin, Germany: Springer; 2009. [Google Scholar]
- 84. Alphonso, A.L. , Monson B.T., Zeher M.J., Armiger R.S., Weeks S.R., Burck J.M., Moran C., Davoodie R., Loeb G.E., and Pasquina P.F., Use of a Virtual Integrated Environment in Prosthetic Limb Development and Phantom Limb Pain. 2012;181:305–309. [PubMed] [Google Scholar]
- 85. Rognini G, Petrini FM, Raspopovic S, et al. Multisensory bionic limb to achieve prosthesis embodiment and reduce distorted phantom limb perceptions. J Neurol Neurosurg Psychiatry. 2019;90(7):833‐836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Page DM, George JA, Kluger DT, et al. Motor control and sensory feedback enhance prosthesis embodiment and reduce phantom pain after long‐term hand amputation. Front Hum Neurosci. 2018;12:352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Lotze M, Grodd W, Birbaumer N, Erb M, Huse E, Flor H. Does use of a myoelectric prosthesis prevent cortical reorganization and phantom limb pain? Nat Neurosci. 1999;2(6):501‐502. [DOI] [PubMed] [Google Scholar]
- 88. Moseley GL, Wiech K. The effect of tactile discrimination training is enhanced when patients watch the reflected image of their unaffected limb during training. PAIN. 2009;144(3):314‐319. [DOI] [PubMed] [Google Scholar]
- 89. Flor H, Denke C, Schaefer M, Grüsser S. Effect of sensory discrimination training on cortical reorganisation and phantom limb pain. Lancet. 2001;357(9270):1763‐1764. [DOI] [PubMed] [Google Scholar]
- 90. Chrastina, J. and Svízelová H., Mirror therapy in post amputation patients with phantom limb pain: a mapping study. 2019.
- 91. Saleh Velez FG, Pinto CB, Bailin ES, et al. Real‐time video projection in an mri for characterization of neural correlates associated with mirror therapy for phantom limb pain. J Vis Exp. 2019;20(146):e58800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Hernández A, Zainos A, Romo R. Neuronal correlates of sensory discrimination in the somatosensory cortex. Proc Natl Acad Sci U S A. 2000;97(11):6191‐6196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Wakolbinger R, Diers M, Hruby LA, Sturma A, Aszmann OC. Home‐based tactile discrimination training reduces phantom limb pain. Pain Pract. 2018;18(6):709‐715. [DOI] [PubMed] [Google Scholar]
- 94. Knotkova H, Cruciani RA, Tronnier VM, Rasche D. Current and future options for the management of phantom‐limb pain. J Pain Res. 2012;5:39‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Robinson LR, Czerniecki JM, Ehde DM, et al. Trial of amitriptyline for relief of pain in amputees: results of a randomized controlled study. Arch Phys Med Rehabil. 2004;85(1):1‐6. [DOI] [PubMed] [Google Scholar]
- 96. Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ. Amitriptyline for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;7:CD008242. 10.1002/14651858.CD008242.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Malik K, Benzon HT. Radiofrequency applications to dorsal root gangliaa literature review. Anesthesiology. 2008;109(3):527‐542. [DOI] [PubMed] [Google Scholar]
- 98. Hieronymus F, Lisinski A, Nilsson S, Eriksson E. Efficacy of selective serotonin reuptake inhibitors in the absence of side effects: a mega‐analysis of citalopram and paroxetine in adult depression. Mol Psychiatry. 2018;23(8):1731‐1736. [DOI] [PubMed] [Google Scholar]


