Abstract
Background:
Reports detailing the rates of radiographic healing after treatment of talar osteochondritis dissecans (TOCD) remain scarce. There is also a paucity of data characterizing treatment outcomes and the risk factors associated with poor outcomes in children with TOCD.
Purpose:
To identify factors associated with healing, assess treatment outcomes, and develop a clinically useful nomogram for predicting healing of TOCD in children.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
This was a retrospective review of all patients ≤18 years of age with TOCD from a single pediatric institution over a 12-year period. Surgical treatment was left to the discretion of the treating surgeon based on standard treatment techniques. Medical records and radiographs were reviewed for patient and clinical data, lesion characteristics, and skeletal maturity. Radiographic healing was evaluated at the 1-year follow-up, and patients with complete versus incomplete healing were compared using multivariable logistic regression models to examine the predictive value of the variables.
Results:
The authors analyzed 92 lesions in 74 patients (mean age, 13.1 ± 2.7 years [range, 7.1-18.0 years]; 61% female). Of these, 58 (63%) lesions were treated surgically (drilling, debridement, microfracture, bone grafting, or loose body removal), and the rest were treated nonoperatively. Complete radiographic healing was seen in 43 (47%) lesions. In bivariate analysis, patients with complete healing were younger (P = .006), were skeletally immature (P = .013), and had a lower body mass index (BMI; P < .001) versus those with incomplete healing. In a multivariate regression model, the factors that correlated significantly with the rate of complete healing were age at diagnosis, BMI, and initial surgical treatment. The lesion dimensions were not significantly associated with the likelihood of healing. A nomogram was developed using the independent variables that correlated significantly with the likelihood of complete radiographic healing.
Conclusion:
Complete radiographic healing of TOCD lesions was more likely in younger patients with a lower BMI. The effect of initial surgical treatment on potential healing rate was greater in older patients with a higher BMI.
Keywords: osteochondritis dissecans, OCD, ankle, treatment, pediatric, child
Osteochondritis dissecans (OCD) is a condition whereby the subchondral bony support for a localized segment of adjacent articular cartilage is compromised. It has been hypothesized to occur through a combination of decreased vascular supply and repetitive microtrauma to a particular site. If the subchondral bony support is not restored, the overlying cartilage may be lost, leading to an osteochondral lesion. The talus is the third most commonly involved location for these lesions after the knee and elbow, 1 occurring most often in the medial or lateral aspect of the talar dome. 19 Depending on the clinical findings and radiographic features, these lesions can be treated operatively or nonoperatively. Stable lesions with intact overlying cartilage are often managed nonoperatively with immobilization, protected weightbearing, and/or activity modification for at least 6 months before considering surgery. Surgical treatment is usually recommended for large, unstable lesions or lesions failing initial nonoperative treatment. 2,28
Despite following aggressive treatment protocols, complete radiographic healing of talar OCD (TOCD) lesions is thought to occur at a significantly lower rate than OCDs located in other joints. In addition, the clinical response to treatment is seemingly variable, with some patients experiencing no pain despite radiographs showing persistent lesions, and others continuing to experience significant pain despite radiographic healing. 9,13,15,23 Furthermore, while some osteochondral lesions of the talus presenting in adulthood are related to trauma, 25 it is hypothesized that most of these lesions diagnosed in adults may represent incompletely healed adolescent TOCD lesions. Given that the majority of the current literature on TOCD has combined adult and pediatric cohorts, there is a paucity of information available on outcomes of TOCD specifically in pediatric populations. ∥
Patient and lesion characteristics have been used to predict full radiographic healing for OCD of the knee. 27 We sought to evaluate the rate of complete radiographic healing after treatment of TOCD lesions in children and to determine predictive factors associated with radiographic healing to develop a statistical model for estimating the probability of complete radiographic healing. We hypothesized that younger children and those with surgical fixation were more likely to heal completely.
Methods
After obtaining approval from the institutional review board at our institution (Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania), we retrospectively evaluated patients younger than 18 years who were diagnosed with OCD of the talus between January 1, 2003, and June 30, 2015. Patients with a diagnosed structural or metabolic condition that could have influenced the healing of their lesions were excluded. Patients who underwent additional concomitant procedures were also excluded. Patients were included if they had at least 1 year of follow-up or demonstrated complete radiographic evidence of healing before 1 year. Radiographic images of a representative patient with a medial talar dome OCD lesion are demonstrated in Figure 1.
Figure 1.

Representative radiographic appearance of patient with a medial talar dome osteochondritis dissecans lesion (A) before treatment and (B) 1 year after surgical arthroscopy and drilling.
Treatment Procedures
All patients were cared for by 1 of 3 fellowship-trained pediatric orthopaedic sports surgeons. The choice of treatment was left to the discretion of the treating physician in consultation with the patient/family and was based on the clinical symptoms, imaging studies, and findings at the time of surgery. Nonoperative treatment included immobilization in a short-leg cast or controlled ankle motion boot with restricted weightbearing for 6 to 8 weeks, or at least until pain free, followed by a gradual return to weightbearing and weaning from immobilization. Impact activities and sports were limited for at least 6 months.
All surgical cases included an ankle arthroscopy. Fluoroscopy was used, if required, to locate lesions during retrograde or transarticular drilling. The drilling was performed using a small (1.1 or 1.6 mm) Kirschner wire with the drill holes placed several millimeters apart. Unstable lesions were removed and debrided back to a stable rim of cartilage and a base of bleeding cancellous bone. For lesions with less than 2 to 3 mm of subchondral bone loss, microfracture was performed at the base of the lesion at 3- to 4-mm intervals using an awl. Iliac crest bone grafting was performed for deeper lesions.
Data Collection
Patient characteristics such as age, sex, and body mass index (BMI) were extracted from medical records. The width, length, and depth of the lesions were determined from the initial radiographs. The radiographs were measured by a medical student who had been thoroughly trained by an attending orthopaedic surgeon. The location of the lesion was recorded as medial, central, or lateral in the anteroposterior view, and as anterior, middle, or posterior in the lateral view. The status of the distal tibia physis was recorded as either open or closed based on appearance on plain radiographs.
Radiographs at each follow-up visit were evaluated, and a comparison was made with the initial radiographs to determine radiographic healing of the lesions. Complete radiographic healing was defined as the reossification of the lesion with no differences in radiodensity on plain radiographs. For patients who underwent nonoperative treatment alone, the lesion status at the 1-year follow-up visit was used to categorize the patient as having complete or incomplete healing. For patients who were initially treated with surgery, the lesion status at the 1-year follow-up from the time of surgery was used to categorize the patient as having complete or incomplete healing of their TOCD lesions. Patients treated with surgery all underwent a procedure within 6 months from the date of diagnosis. In addition, the Berndt and Harty outcome 3 assessment was recorded at the 1-year follow-up. In brief, this assessment categorizes the ankle as good (occasional symptoms without loss of function), fair (decreased symptoms but with persisting pain), or poor (no change in symptoms).
Statistical Analysis
All statistical analyses were performed using Stata 15 (StataCorp). Descriptive statistics (means, standard deviations, and ranges) were used to report continuous variables, and frequencies and percentages were used for the reporting of categorical variables. To compare the differences between complete or incomplete radiographic healing, the independent t test was used for parametric variables and the chi-square test/Fisher exact test and Mann-Whitney U test were used to compare groups for nonparametric variables.
In univariate analysis, we considered characteristic and measured factors—age, BMI, and skeletal maturation—as risk factors to the radiographic healing. Multivariable analysis was conducted using factors with statistical significance (P < .05). A nomogram was then created using the variables that demonstrated significant association with the rate of complete healing. The final model's predictive accuracy was assessed using the C statistic and was checked for multicollinearity. Significance was set at a 2-sided alpha level of P < .05.
Results
We identified 81 patients who were diagnosed with TOCD within the study period. Of these patients, we excluded 3 patients with juvenile idiopathic arthritis; 1 patient with a tarsal coalition; 1 patient with renal transplant; 1 patient with factor VIII deficiency; and 1 patient with club foot. The final cohort included 74 patients (92 TOCD lesions) who met our inclusion criteria. The mean age of the patients at treatment was 13.1 ± 2.7 years (range, 7.1-18.0 years), with 60.8% female participants. The average BMI was 22.8 ± 5.7 kg/m2 (range, 14.6-44.0 kg/m2). Of 92 TOCD lesions, 47 (51.0%) were in skeletally mature patients at the time of diagnosis. Five (6.8%) patients had bilateral TOCD lesions, whereas 13 (17.6%) patients had 2 or more unilateral lesions with no underlying cause identified. According to Berndt and Harty criteria, 3 23 (25.0%) lesions were stage 1, 29 (31.5%) were stage 2, 26 (28.3%) were stage 3, and 14 (15.2%) were stage 4 at the time of evaluation. The patient and lesion characteristics are summarized in Table 1.
Table 1.
Patient and Lesion Characteristics a
| Variable | Overall | Radiographic Healing at 1-y Follow-up | P | |
|---|---|---|---|---|
| Complete | Incomplete | |||
| No. of patients | 74 | 40 (54) | 34 (46) | |
| No. of TOCD lesions | 92 | 43 (47) | 49 (53) | |
| Sex | .615 | |||
| Female | 56 (61) | 25 (45) | 31 (55) | |
| Male | 36 (39) | 18 (50) | 18 (50) | |
| Age, y | 13.1 ± 2.7 | 12.4 ± 2.1 | 13.7 ± 2.6 | .006 |
| BMI, kg/m2 | 22.8 ± 5.7 | 21.0 ± 5.9 | 24.1 ± 6.1 | <.001 |
| Laterality of the lesion | .383 | |||
| Left | 40 (44) | 19 (48) | 21 (53) | |
| Right | 52 (57) | 20 (39) | 32 (62) | |
| Lesion size, mm | ||||
| AP | 7.0 ± 2.4 | 7.1 ± 2.7 | 6.9 ± 2.1 | .115 |
| Lateral | 9.3 ± 3.6 | 9.0 ± 3.9 | 9.6 ± 3.3 | .057 |
| Depth | 4.9 ± 2.2 | 4.5 ± 1.8 | 5.2 ± 2.6 | .112 |
| Location on coronal plane | .040 | |||
| Medial | 60 (65) | 26 (43) | 34 (57) | |
| Lateral | 20 (22) | 3 (15) | 17 (85) | |
| Central | 14 (15) | 10 (71) | 4 (29) | |
| Location on sagittal plane | .702 | |||
| Anterior | 3 (3) | 1 (33) | 2 (67) | |
| Posterior | 4 (4) | 2 (50) | 2 (50) | |
| Middle | 84 (91) | 36 (43) | 48 (57) | |
| Physeal status | .013 | |||
| Open | 45 (49) | 27 (60) | 18 (40) | |
| Closed | 47 (51) | 16 (34) | 31 (66) | |
| Initial Berndt and Harty stage | .899 | |||
| 1 | 23 (25) | 11 (48) | 12 (52) | |
| 2 | 29 (32) | 15 (52) | 14 (48) | |
| 3 | 26 (28) | 11 (42) | 15 (58) | |
| 4 | 14 (15) | 6 (43) | 8 (57) | |
| Initial treatment type | .413 | |||
| Nonoperative | 34 (37) | 14 (41) | 20 (59) | |
| Operative | 58 (63) | 29 (50) | 29 (50) | |
| Berndt and Harty clinical grade at 1-y follow-up | .003 | |||
| Poor | 20 (22) | 4 (20) | 16 (80) | |
| Fair | 32 (35) | 13 (41) | 19 (59) | |
| Good | 40 (44) | 26 (65) | 14 (35) | |
a Data are reported as mean ± SD or n (%). Bolded P values indicate a statistically significant difference between study groups (P < .05). AP, anteroposterior; BMI, body mass index; TOCD, talar osteochndritis dissecans.
About one-third (34/92; 37.0%) of the lesions were treated nonoperatively, while about two-thirds (58/92; 63.0%) were treated surgically. The median time to surgery from the date of diagnosis was 1.5 months (range, 0.3-5.9 months). Fine guidewire drilling was used in 23 of the surgically treated patients (23/58; 39.7%); of those patients, 3 (3/23; 13.0%) underwent retrograde drilling and the remainder underwent transarticular drilling. Surgical fixation was performed in 5 patients (5/58; 8.6%). Debridement and microfracture were performed in 21 of the surgical cases (21/58; 36.2%). Debridement with or without loose body removal was performed in 6 cases (6/58; 10.3%). Bone grafting was performed in 3 cases (3/58; 5.2%): 1 with fixation and bone grafting, 1 with microfracture and bone grafting, and 1 with an osteochondral injection.
Overall, less than half of the lesions (43/92; 46.7%) demonstrated complete radiographic healing. Patients who healed completely were younger than those in the incomplete healing group (12.4 ± 2.1 vs 13.7 ± 2.6 years, respectively; P = .006) and had lower BMI (21.0 ± 5.9 vs 24.1 ± 6.1 kg/m2, respectively; P < .001). Additionally, a significantly higher percentage of patients with open physes achieved complete radiographic healing compared with the patients with closed physes (60% vs 34%, respectively; P = .013). Patient sex, initial Berndt and Harty stage, type of initial treatment, lesion dimensions, and lesion location on sagittal plane were not significantly different between the groups (Table 1).
The Berndt and Harty outcome tool was used to assess clinical outcomes at the 1-year follow-up visit. More than 90% of the TOCD lesions that demonstrated complete radiographic healing had either good or fair clinical outcomes. In comparison, 67.3% of the lesions with incomplete radiographic healing had achieved good or fair clinical outcomes (P = .007). Univariate and multivariate regression analyses were unable to identify any other variables that correlated significantly with Berndt and Harty clinical grade (including age, sex, BMI, lesion dimension, lesion location on sagittal and coronal planes, initial Berndt and Harty class of the lesions, and treatment type).
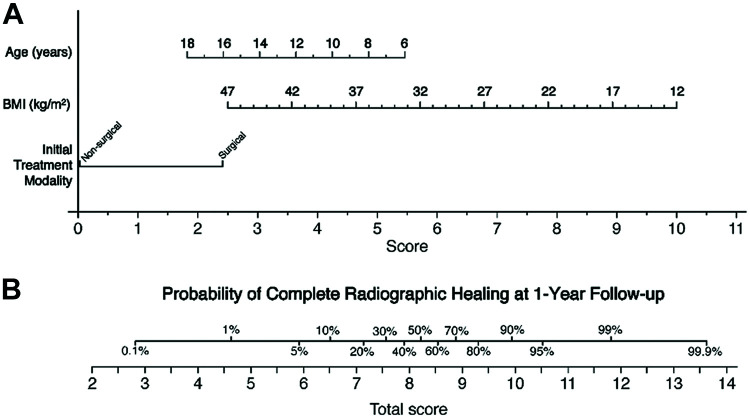
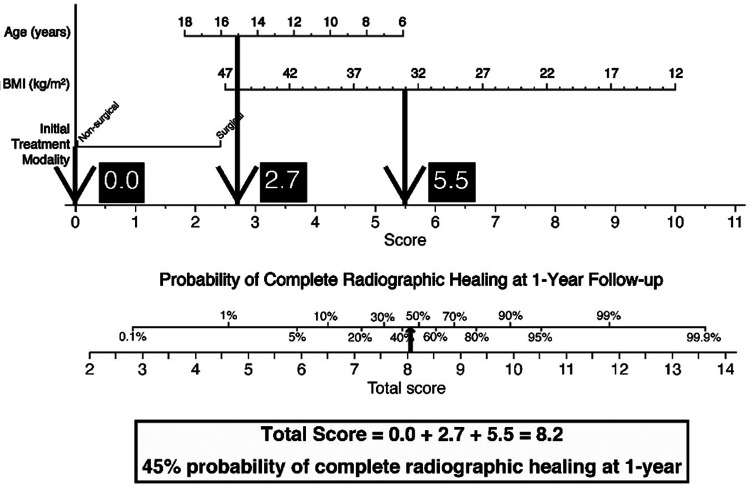
Different predictive models that included clinically relevant factors were considered to examine the predictive effects of independent variables on the rate of complete radiographic healing. A multivariable model that included age at diagnosis, type of treatment (operative vs nonoperative), and BMI reached significance for each of these 3 variables. This model was predictive of healing status with a C statistic of 0.81. Figure 2 represents the area under the receiver operating characteristic curve for this model. Of the 3 variables included in the final nomogram, initial treatment with surgery had the greatest impact on the odds of achieving complete radiographic healing (OR, 11.44; 95% CI, 2.30-56.85; P = .003). Figure 3 represents the nomogram predicting the probability of radiographic healing on the basis of age, BMI, and initial treatment type.
Figure 2.
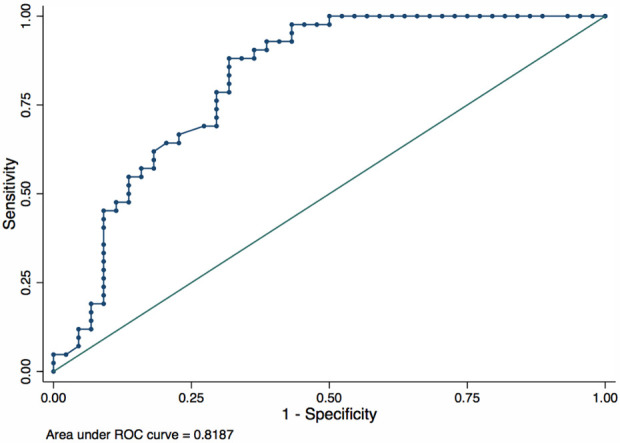
Receiver operating characteristic curve for the multivariable model that included age at evaluation, body mass index, and initial treatment approach (nonsurgical vs surgical).
Figure 3.
(A) Nomogram used to predict complete radiographic healing at the 1-year follow-up on the basis of a patient’s age, body mass index (BMI), and the type of initial treatment. To calculate the probability of complete radiographic healing, straight vertical lines should be drawn from the points corresponding to the patient’s age, BMI, and initial treatment types on the respective row corresponding to the data. Next, record the values that each of these vertical lines provide at their points of intersection on the row labeled “Score.” All recorded values should be summed. (B) This sum is then matched with a value on the line labeled “Total Score.” The corresponding percentages on the line immediately above the total score line indicate the patient-specific probability of achieving complete radiographic healing at the 1-year follow-up.
Discussion
The evaluation, treatment, and outcomes after management of TOCD in children remain poorly described in the literature. Here we have reported our findings from a retrospective study of 74 children with 92 TOCD lesions who were treated at our pediatric institution within a 12-year period. In accordance with other studies involving TOCD, we found that the majority of patients were girls (60.8%) and most of the lesions were at the medial talar dome (65.2%). 9,13,15,19 This is in contrast to adult lesions, which have a male predominance and even distribution between the medial and lateral talar domes. 5,20,22 Approximately one-third of the patients in our study were treated nonoperatively, while the remaining two-thirds were treated operatively. The principal finding of our study is that initial operative treatment yielded better radiographic healing at 1-year follow-up compared with nonoperative treatment. However, no difference was observed in clinical outcomes as assessed by the Berndt and Harty stage. Younger patients and those with a lower BMI were also more likely to achieve complete radiographic healing.
Although nonoperative treatment is generally regarded as the first-line option for stage 1 to 3 TOCD lesions, success rates with nonoperative management are highly variable in the literature. 3 Perumal et al 23 reported on 32 skeletally immature patients and noted that 16% of nonoperatively managed TOCD lesions exhibited complete radiographic healing at the 6-month follow-up. Lam and Siow 17 noted that 4 of 6 (67%) nonoperatively treated TOCD lesions showed good radiographic outcomes. Letts et al, 19 in their series of 23 nonoperatively managed stage 2 lesions, reported a 54.2% failure rate with nonoperative management. This is similar to our finding that only 41% of nonoperatively treated TOCD lesions attained complete radiographic healing. This variability in success rates after nonoperative management of TOCD is perhaps a reflection of the variability in treatment protocols among clinicians and institutions. 5,9,17,19,23 Interestingly, we did not find any correlation between presenting Berndt and Harty stage and complete radiographic healing in our series.
This study found that more than 95% of surgically treated patients underwent surgical procedures that included drilling, microfracture, fixation, or debridement/removal of loose body. While the overall complete radiographic healing rate was only 55%, the rate of good or fair clinical outcome was as high as 82% in our patient population.
Drilling the lesion is a successful technique. The literature strongly supports its effectiveness for stable OCD lesions in the knee in skeletally immature children. 4,6 There is also support for drilling OCD lesions of the talus in adults and adolescents. 10,16 Good or excellent results have been reported in up to 56% 19 to 91% 15 of TOCD lesions treated with drilling. In our study, 59% of the lesions treated with drilling attained complete radiographic healing, while 82% had either good or fair clinical outcome.
Little research assessing the efficacy of debridement and microfracture for TOCD lesions has been done in the pediatric population. One study identified recurrence of symptoms at the 1-year follow-up in 26% of skeletally immature children treated with microfracture for OCD of the knee. 7 Yet another study reported deterioration of clinical outcomes between 18 and 36 months after microfracture in adults with knee OCD. 14 Translating these results in the adult knee to the pediatric talus should be done with caution as the pathoanatomy is different. In a recent but small series by Jurina et al 11 that included 13 pediatric patients treated with arthroscopic microfracture combined with curettage, the rate of good or fair clinical outcome was reported at 100% during a median follow-up period of 5.6 years. Similarly, 85% of the patients in our series achieved either a good or fair clinical outcome at 1 year after microfracture. Although we are unable to provide evidence of the long-term efficacy of this technique, future studies with larger numbers and a longer follow-up period may be able to address the concerns surrounding the long-term efficacy of microfracture in pediatric TOCD lesions.
Internal fixation of the loose fragment has been used as an alternative treatment approach for large, detached, or unstable fragments, with 5 patients undergoing fragment fixation in this study. In terms of radiographic and clinical outcomes, fixation has been reported to have results comparable to drilling, ranging from 75% to 100%. 12,13,21 Schuh et al 26 reported good or fair outcomes in 100% of their 11 pediatric TOCD patients treated with Kirschner-wire fixation. Similarly, a high rate of clinical success has been reported with autologous bone graft. For instance, Lee et al 18 reported 100% good or excellent outcomes at 36 months for 18 TOCD lesions treated with autologous osteochondral grafting from the ipsilateral knee.
Another significant finding of the current series is that the complete healing group was younger and had a lower BMI. Kramer et al 13 found that neither the physeal status nor the lesion size affected the clinical, radiographic, or functional outcomes. In their analysis, age and skeletal maturity were not related to complete radiographic healing. However, female sex and elevated BMI were reported as significant negative predictors for clinical outcomes in their surgically treated patients. In a series of 77 lesions (67 patients) by Heyse et al, 8 61% of 76 nonoperatively treated lesions failed the initial management. The authors found older age and grade 3 lesions to be predictive factors for failure of nonoperative treatment. Similarly, our findings also demonstrated that increasing BMI and age had a negative correlation with radiographic healing. However, neither sex nor lesion stage was found to be a significant factor for predicting radiographic healing in our series.
Figure 3 represents the nomogram that can be used to help predict the probability of radiographic healing at 1 year based on the patient’s age, BMI, and initial treatment type. Figure 4 represents an example of the nomogram-predicted probability of radiographic healing at 1 year in a patient from our series. This nomogram can be used as an aid in clinical decision-making and as a counseling tool for the patients and their families.
Figure 4.
Example of nomogram-predicted probability of complete radiographic healing at 1 year in a patient from our series based on the patient’s age, body mass index (BMI), and initial treatment modality. The patient did not have complete healing at the 1-year follow-up.
There are several limitations of this study. First, it is retrospective in nature, which subjects our data to a number of biases that are inherent to studies of similar design. Even though an extensive medical-record review was performed, in many cases it was difficult to obtain documentation of a patient's compliance to nonoperative treatment protocols. Patients with poor compliance may have contributed to lower rates of healing in the nonoperative group. Similarly, clinical data that we were able to collect on symptoms, including the Berndt and Harty clinical staging, were too heterogeneous to clearly categorize them into a few distinct categories. Second, the average follow-up in our study was 13 months. While this was long enough to ascertain radiographic healing and thus was adequate for developing a predictive nomogram for this purpose, a longer follow-up period may provide a better sense of clinical and functional outcomes. Third, our sample size of 74 patients (92 lesions), while relatively large for the diagnosis of TOCD, is small for detecting overall differences in outcomes associated with various surgical treatment types. Additionally, the heterogeneity of our population may have contributed to the lesion stage, size, and location showing no significant association with the outcomes in our series. Fourth, while we compared patients treated nonoperatively with those treated surgically, there can be large differences between the different surgical treatments, further contributing to the heterogeneity of the groups. Additionally, there were no strict treatment guidelines, and specific surgical techniques were left to the discretion of the surgeon.
Conclusion
Two-thirds of all TOCD lesions in our series were treated surgically, while the remaining lesions were managed nonsurgically. The overall rate of complete radiographic healing at 1-year follow-up was approximately 50% to 60% in our patient population. In both treatment groups, complete radiographic healing was more likely in patients with younger age and lower BMI. On multivariable analysis, younger age, lower BMI, and initial treatment with surgery were positively associated with the rate of radiographic healing at 1 year. Based on our nomogram, the effects of surgical treatment on healing rate are potentially greater in older patients with a higher BMI. Besides its potential role in the treatment decision-making process, the nomogram presented in this study can be used to counsel patients and their families regarding the healing prognosis of TOCD.
Footnotes
Final revision submitted July 22, 2021; accepted August 4, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: K.J.M. has received education payments from Smith & Nephew. J.T.R.L. has received education payments from Liberty Surgical and nonconsulting fees from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Children’s Hospital of Philadelphia (No. 15-012228).
References
- 1. Aichroth P. Osteochondral fractures and their relationship to osteochondritis dissecans of the knee. An experimental study in animals. J Bone Joint Surg Br. 1971;53(3):448–454. [PubMed] [Google Scholar]
- 2. Badekas T, Takvorian M, Souras N. Treatment principles for osteochondral lesions in foot and ankle. Int Orthop. 2013;37(9):1697–1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berndt AL, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959;41:988–1020. [PubMed] [Google Scholar]
- 4. Bradley J, Dandy DJ. Results of drilling osteochondritis dissecans before skeletal maturity. J Bone Joint Surg Br. 1989;71(4):642–644. [DOI] [PubMed] [Google Scholar]
- 5. Bruns J, Rosenbach B. Osteochondrosis dissecans of the talus. Comparison of results of surgical treatment in adolescents and adults. Arch Orthop Trauma Surg. 1992;112(1):23–27. [DOI] [PubMed] [Google Scholar]
- 6. Gepstein R, Conforty B, Weiss RE, Hallel T. Surgery for early stage osteochondritis dissecans of the knee in young adults: a preliminary report. Orthopedics. 1986;9(8):1087–1089. [DOI] [PubMed] [Google Scholar]
- 7. Gudas R, Gudaite A, Pocius A, et al. Ten-year follow-up of a prospective, randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint of athletes. Am J Sports Med. 2012;40(11):2499–2508. [DOI] [PubMed] [Google Scholar]
- 8. Heyse TJ, Schuttler KF, Schweitzer A, et al. Juvenile osteochondritis dissecans of the talus: predictors of conservative treatment failure. Arch Orthop Trauma Surg. 2015;135(10):1337–1341. [DOI] [PubMed] [Google Scholar]
- 9. Higuera J, Laguna R, Peral M, Aranda E, Soleto J. Osteochondritis dissecans of the talus during childhood and adolescence. J Pediatr Orthop. 1998;18(3):328–332. [PubMed] [Google Scholar]
- 10. Jungesblut OD, Berger-Groch J, Hoffmann M, et al. Electromagnetic navigation reduces radiation exposure for retrograde drilling in osteochondrosis dissecans of the talus. BMC Musculoskelet Disord. 2021;22(1):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jurina A, Dimnjakovic D, Mustapic M, Smoljanovic T, Bojanic I. Clinical and MRI outcomes after surgical treatment of osteochondral lesions of the talus in skeletally immature children. J Pediatr Orthop. 2018;38(2):122–127. [DOI] [PubMed] [Google Scholar]
- 12. Kocher MS, Czarnecki JJ, Andersen JS, Micheli LJ. Internal fixation of juvenile osteochondritis dissecans lesions of the knee. Am J Sports Med. 2007;35(5):712–718. [DOI] [PubMed] [Google Scholar]
- 13. Kramer DE, Glotzbecker MP, Shore BJ, et al. Results of surgical management of osteochondritis dissecans of the ankle in the pediatric and adolescent population. J Pediatr Orthop. 2015;35(7):725–733. [DOI] [PubMed] [Google Scholar]
- 14. Kreuz PC, Steinwachs MR, Erggelet C, et al. Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthritis Cartilage. 2006;14(11):1119–1125. [DOI] [PubMed] [Google Scholar]
- 15. Kumai T, Takakura Y, Higashiyama I, Tamai S. Arthroscopic drilling for the treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 1999;81(9):1229–1235. [DOI] [PubMed] [Google Scholar]
- 16. Lahm A, Erggelet C, Steinwachs M, Reichelt A. Arthroscopic management of osteochondral lesions of the talus: results of drilling and usefulness of magnetic resonance imaging before and after treatment. Arthroscopy. 2000;16(3):299–304. [DOI] [PubMed] [Google Scholar]
- 17. Lam KY, Siow HM. Conservative treatment for juvenile osteochondritis dissecans of the talus. J Orthop Surg (Hong Kong). 2012;20(2):176–180. [DOI] [PubMed] [Google Scholar]
- 18. Lee CH, Chao KH, Huang GS, Wu SS. Osteochondral autografts for osteochondritis dissecans of the talus. Foot Ankle Int. 2003;24(11):815–822. [DOI] [PubMed] [Google Scholar]
- 19. Letts M, Davidson D, Ahmer A. Osteochondritis dissecans of the talus in children. J Pediatr Orthop. 2003;23(5):617–625. [DOI] [PubMed] [Google Scholar]
- 20. Loomer R, Fisher C, Lloyd-Smith R, Sisler J, Cooney T. Osteochondral lesions of the talus. Am J Sports Med. 1993;21(1):13–19. [DOI] [PubMed] [Google Scholar]
- 21. Magnussen RA, Carey JL, Spindler KP. Does operative fixation of an osteochondritis dissecans loose body result in healing and long-term maintenance of knee function? Am J Sports Med. 2009;37(4):754–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McCullough CJ, Venugopal V. Osteochondritis dissecans of the talus: the natural history. Clin Orthop Relat Res. 1979;144:264–268. [PubMed] [Google Scholar]
- 23. Perumal V, Wall E, Babekir N. Juvenile osteochondritis dissecans of the talus. J Pediatr Orthop. 2007;27(7):821–825. [DOI] [PubMed] [Google Scholar]
- 24. Reilingh ML, Kerkhoffs GM, Telkamp CJ, Struijs PA, van Dijk CN. Treatment of osteochondral defects of the talus in children. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):2243–2249. [DOI] [PubMed] [Google Scholar]
- 25. Rikken QGH, Kerkhoffs G. Osteochondral lesions of the talus: an individualized treatment paradigm from the Amsterdam perspective. Foot Ankle Clin. 2021;26(1):121–136. [DOI] [PubMed] [Google Scholar]
- 26. Schuh A, Salminen S, Zeiler G, Schraml A. Results of fixation of osteochondral lesions of the talus using K-wires. Article in German. Zentralbl Chir. 2004;129(6):470–475. [DOI] [PubMed] [Google Scholar]
- 27. Wall EJ, Vourazeris J, Myer GD, et al. The healing potential of stable juvenile osteochondritis dissecans knee lesions. J Bone Joint Surg Am. 2008;90(12):2655–2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zengerink M, Struijs PA, Tol JL, van Dijk CN. Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zinman C, Wolfson N, Reis ND. Osteochondritis dissecans of the dome of the talus. Computed tomography scanning in diagnosis and follow-up. J Bone Joint Surg Am. 1988;70(7):1017–1019. [PubMed] [Google Scholar]