Abstract
Aim
To describe: (1) the frequency and types of sleep problems, (2) parent‐rated satisfaction with their child’s and their own sleep, and (3) child factors related to the occurrence of sleep problems in children with cerebral palsy (CP) and their parents. The secondary objective was to compare the sleep outcomes of children with CP with those from typically developing children and their parents.
Method
The Sleep section of the 24‐hour activity checklist was used to assess the sleep of children with CP and their parents and the sleep of typically developing children and their parents.
Results
The sleep outcomes of 90 children with CP (median age 5y, range 0–11y, 53 males, 37 females, 84.4% ambulatory) and 157 typically developing peers (median age 5y, range 0–12y; 79 males, 78 females) and their parents were collected. Children with CP were more likely to have a sleep problem than typically developing children. Non‐ambulatory children with CP were more severely affected by sleep problems than ambulatory children. The parents of non‐ambulatory children were less satisfied about their child’s and their own sleep. Waking up during the night, pain/discomfort in bed, and daytime fatigue were more common in children with CP and more prevalent in children who were non‐ambulatory.
Interpretation
These findings highlight the need to integrate sleep assessment into routine paediatric health care practice.
What this paper adds.
Children with cerebral palsy (CP) are more likely to have a sleep problem than typically developing peers.
Non‐ambulatory children with CP are more severely affected by sleep problems.
One‐third of parents of children with CP report feeling sleep‐deprived often or always compared to a quarter of parents of typically developing children.
What this paper adds
Children with cerebral palsy (CP) are more likely to have a sleep problem than typically developing peers.
Non‐ambulatory children with CP are more severely affected by sleep problems.
One‐third of parents of children with CP report feeling sleep‐deprived often or always compared to a quarter of parents of typically developing children.
This original article is commented by McDonald on page 1247 of this issue.
A growing body of evidence supports the importance of sleep for optimal child health and development. 1 Cerebral palsy (CP) represents one of the most common physical childhood disabilities worldwide. 2 Children with CP are a population at risk for the occurrence of sleep problems, with parent‐reported prevalence rates varying between 23% and 46% 3 , 4 , 5 compared to 20% to 30% in typically developing children. 6 Commonly reported sleep problems in children with CP include difficulty falling asleep, frequent night‐time waking, sleep‐related breathing disorders, early‐morning waking, and excessive daytime fatigue. 7 , 8 , 9 , 10 , 11
Despite widespread recommendations for systematically enquiring about sleep and sleep problems in paediatric health care, 12 , 13 sleep health is frequently overlooked in rehabilitation settings. 14 According to the parents of children with CP, clinicians rarely ask about sleep during routine health assessments, with even less attention paid to parental sleep and the impact on the family. 15 This is worrisome because in addition to the negative implications for the child, sleep problems in children with CP are a major source of family stress. 15 , 16 A recent review showed that parents of children with neurodevelopmental disabilities, including CP, report poorer sleep quality than parents of typically developing children. 17 To improve the sleep of both children and parents, and thereby optimize their health and well‐being, we first have to recognize sleep problems.
Originating from a need for a brief, practical tool that can be easily applied in routine care, we recently developed a 24‐hour activity checklist as part of a more general clinical practice guide for children with CP. 18 In addition to providing an insight into the physical activities of children with CP, the checklist was designed to guide clinicians in determining whether a more thorough assessment or referral is warranted when sleep problems are detected. Now, 1 year after the implementation of the 24‐hour activity checklist, we have the opportunity to explore the extent to which sleep problems can be detected in children with CP and their parents.
The primary purpose of this study was to describe in children with CP and their parents: (1) the frequency and types of parent‐reported sleep problems, (2) parent‐rated satisfaction with their child’s sleep and their own sleep, and (3) child factors related to the occurrence of sleep problems. Since children with CP have both sleep problems that are similar to typically developing children and specific sleep problems related to CP, it is important to place findings in the context of children without CP. Therefore, the secondary purpose of this study was to compare the sleep outcomes of children with CP and their parents with comparative data collected from typically developing children and their parents.
METHOD
A multicentre, cross‐sectional study was conducted involving children with CP and their parents. In addition, a convenience sample of typically developing children and their parents was recruited from the general population as a comparison group. The study was approved by the medical ethics research committee of De Hoogstraat Rehabilitation Center, Utrecht, the Netherlands.
Participants
The study population consisted of children with CP (aged 0–11y, 53 males, 37 females, 84.4% ambulatory) and their parents receiving care from three paediatric rehabilitation settings (a rehabilitation centre, a special education school, and the rehabilitation department of a children’s hospital) in the Utrecht province of the Netherlands. Inclusion criteria were children diagnosed with CP across all Gross Motor Function Classification System (GMFCS) levels and between the ages of 0 to 12 years. All families who were scheduled for a follow‐up appointment with their rehabilitation physician received a paper‐and‐pencil 24‐hour activity checklist at home as part of routine care. Parents were instructed to complete the questionnaire before their appointment and hand in the checklist during the upcoming consultation with their rehabilitation physician, who would in turn discuss the responses with the parents and collect the checklists. The parents of children with CP who agreed for their questionnaire to be used for research signed an informed consent form for participation in the study. All checklists collected between April 2019 and August 2020 that were returned complete with signed consent and met the inclusion criteria were used for data analysis.
The comparison group consisted of typically developing children (79 males, 78 females) aged between 0 and 12 years without any known physical, developmental, intellectual, or behavioural disability (based on parental report). The parents of typically developing children were recruited via the (social) networks of colleagues and acquaintances. They were invited to participate in the study by e‐mail and their responses were collected via an Internet‐based version of the same questionnaire. To ensure anonymity, no socio‐demographic information, other than sex and age of the child, was collected.
The 24‐hour activity checklist
Parents completed the 24‐hour activity checklist, a brief questionnaire developed to assess the physical activity and sleep patterns of the child and parental sleep. 18 For the purpose of the present study, responses to the Sleep section of the 24‐hour activity checklist (Fig. S1, online supporting information) were used. In this section, parents were asked to rate the frequency of child and parent sleep problems within the past month on a 5‐point Likert‐type scale (Table 1). Since the checklist assesses the occurrence of different types of sleep problems that are not necessarily correlated (i.e. a formative model), analyses regarding structural validity and internal consistency were not relevant 19 and subsequently not reported.
Table 1.
Items, questions, and response format of the Sleep section of the 24‐hour activity checklist
| Item | Question | Response format a |
|---|---|---|
| Child sleep | ||
| C1 | Are you satisfied with the sleep of your child? | 5‐point scale from never to always |
| C2 | Does it take more than 30 minutes before your child falls asleep? | 5‐point scale from never to always |
| C3 | Does your child wake up more than three times a night OR is your child awake for more than 20 minutes during the night? | 5‐point scale from never to always |
| C4 | Do you think your child wakes up too early? | 5‐point scale from never to always |
| C5 | How often does your child snore at night? | 5‐point scale from never to always |
| C6 | Do you think your child experiences pain or discomfort in bed? | 5‐point scale from never to always |
| C7 | How often does your child experience nightmares? | 5‐point scale from never to always |
| C8 | Does your child seem overtired or sleepy during the day? | 5‐point scale from never to always |
| C9 | Does your child use sleep medication/tablets (e.g. melatonin)? | Yes/no. If yes: type, dose, and frequency of drug |
| Parent sleep | ||
| P1 | Are you satisfied with your own sleep? | 5‐point scale from never to always |
| P2 | Do you think you have lack of sleep? | 5‐point scale from never to always |
The 5‐point scale options are as follows: 1=never (less than once per month), 2=seldom (1–2 times per month), 3=sometimes (1–3 times per week/less than half of the week), 4=often (4–6 times per week/more than half of the week), 5=always (daily/nightly). All items, except for C9, included a ‘don’t know’ option.
Statistical analysis
Data were analysed per study group (children with CP and typically developing children) and within CP subgroups. CP subgroup analyses were performed by sex, age group (preschool age, 0–3y vs school‐age, 4–12y) and walking ability (ambulatory, GMFCS levels I–III vs non‐ambulatory, GMFCS levels IV and V) to determine child factors related to the occurrence of sleep problems in children with CP.
Descriptive statistics were performed on the responses given to each of items C2 to C8 (Table 1) separately. To determine whether these sleep problems were more often reported by children with CP compared to typically developing children and whether there were differences within subgroups of CP, the difference in distribution of responses (i.e. the proportion of sleep problems reported to occur never, seldom, sometimes, often, or always) for each item was analysed using a non‐parametric Mann–Whitney U test.
To calculate the total number of sleep problems per child, the responses to items C2 to C8 were dichotomized for the presence of a sleep problem (yes/no) and summed, yielding a possible score ranging from 0 to 7 sleep problems; difficulties occurring often or always (i.e. more than half of the week) were considered a sleep problem, whereas items answered with never, seldom, or sometimes (i.e. less than half of the week) or as ‘don’t know’ were scored as no problem. Based on these dichotomized values, the frequencies of individual sleep problems and the distribution of the total number of sleep problems per child across study groups and within CP subgroups were calculated. To analyse whether children with CP were more likely to have a sleep problem than typically developing children and whether non‐ambulatory children were more likely to have a sleep problem than ambulatory children with CP, Fisher’s exact tests were performed on the proportion of children having at least one sleep problem based on dichotomized values between groups. To determine whether children with CP suffered from more sleep problems than typically developing children and whether there were differences within subgroups of CP, the difference in distribution of the total number of sleep problems (i.e. the proportion of children having zero, one, two, three, or more than three sleep problems based on dichotomized values) were assessed using Mann–Whitney U tests.
Since the use of sleep medication can be considered both a problem or solution to a sleep problem, item C9 (Table 1) was not included in the dichotomized ‘total number of sleep problems’ per child; the proportion of medication use across groups was analysed separately using Fisher’s exact test.
The two items on sleep satisfaction (i.e. C1, P1; Table 1) measured different aspects of sleep, that is, subjective perceptions, in contrast to all other items of the questionnaire, which were more objective in nature (i.e. frequencies of factual events, such as snoring); therefore, their outcomes are reported separately and were analysed using Mann–Whitney U tests.
Data were analysed using SPSS v26 (IBM Corp., Armonk, NY, USA). Significance level was set at p<0.05.
Results
In total, 110 responses were collected from children with CP and their parents; one checklist was returned largely (>75%) incomplete and 19 checklists were returned by the same family for a second follow‐up evaluation and were therefore excluded from analysis. For the typically developing comparison group, a total of 168 responses were collected from typically developing children and their parents, of which three responses were excluded because of the presence of a disability, six responses had unknown ages, and two children were older than 12 years and were therefore excluded from the analysis. The final sample consisted of 90 children with CP and 157 typically developing children (group characteristics are presented in Table 2). Study groups did not differ with respect to sex or age (both p>0.05). The majority of children with CP (84.4%) were ambulatory (i.e. classified in GMFCS levels I–III), with a similar distribution across age groups (preschool age 88.9%, school‐age 82.5%; Fisher’s exact test, p>0.05).
Table 2.
Group characteristics of children with CP and their typically developing peers
|
Children with CP n=90 |
Typically developing children n=157 |
p | |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 53 (58.9) | 79 (50.3) | 0.233 a |
| Female | 37 (41.1) | 78 (49.7) | |
| Age, y | |||
| Range | 0–11 | 0–12 | 0.974 b |
| Median | 5 | 5 | |
| Age group, n (%) | |||
| 0–3y | 27 (30) | 57 (36.3) | 0.332 a |
| 4–12y | 63 (70) | 100 (63.7) | |
| GMFCS level, n (%) | |||
| I | 52 (57.8) | ||
| II | 19 (21.1) | ||
| III | 5 (5.6) | ||
| IV | 7 (7.8) | ||
| V | 7 (7.8) | ||
Fisher’s exact test.
Mann–Whitney U test. CP, cerebral palsy.
Frequency and types of parent‐reported sleep problems
Child sleep
Total number of sleep problems
Children with CP were more likely to have a sleep problem than typically developing children (Fisher’s exact test, p<0.001); 72.2% of children with CP were reported to have at least one sleep problem occurring often or always compared to 46.4% in typically developing children. The child‐by‐child distribution of the total number of sleep problems in children with CP was significantly different from those observed in typically developing children, with a considerably higher total number of sleep problems reported by parents of children with CP (U=4779.5, z=−4.53, p<0.001); in children with CP, zero sleep problems were present in 27.8%, one sleep problem was present in 38.9%, two sleep problems were present in 17.8%, three sleep problems were present in 12.2%, and more than three sleep problems were present in 3.3% compared to 53.5%, 31.8%, 12.7%, 1.9%, and 0% in typically developing children respectively.
Types of sleep problems
Figure 1 shows the frequencies of different parent‐reported sleep problems in children with CP compared to typically developing children. Daytime fatigue (33.3%), difficulty falling sleep (30%), and early‐morning waking (26.7%) were the most frequently reported sleep problems occurring often or always in children with CP. The most frequently reported sleep problems in typically developing children were difficulty falling asleep (22.3%) and early‐morning waking (19.7%). Significant differences were observed between children with CP and typically developing children in the distribution of responses to the items regarding daytime fatigue (U=4249, z=−5.42, p<0.001), waking up during the night (U=4800, z=−4.31, p<0.001), and pain or discomfort in bed (U=4412, z=−5.49, p<0.001), with the parents of children with CP consistently reporting a higher frequency in the occurrence of these sleep problems. Use of medication for sleep purposes was reported in 6.7% (n=6; n=4 melatonin; n=2 baclofen) of children with CP, a proportion that did not differ from the 3.2% (n=5, all melatonin) observed in typically developing children (Fisher’s exact test, p>0.05).
Figure 1.
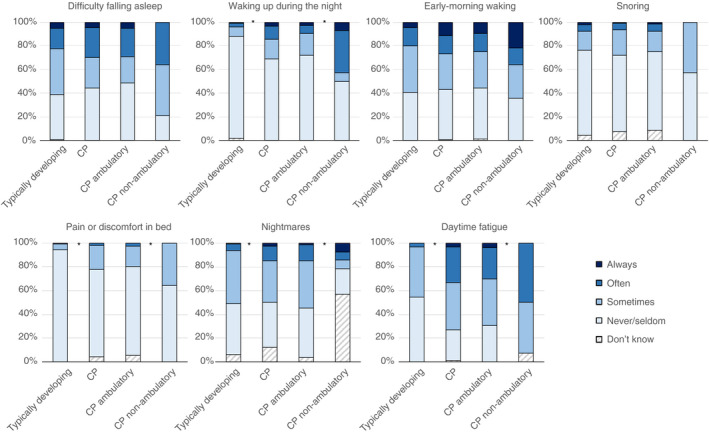
Parent‐reported sleep problems in children with cerebral palsy (CP; total, ambulatory, and non‐ambulatory) compared to typically developing children. The single asterisk indicates a significant difference (Mann–Whitney U test, p<0.05) between the CP and typically developing study groups or between ambulatory and non‐ambulatory children with CP.
Sleep satisfaction
The parents of typically developing children were more satisfied with their child’s sleep than the parents of children with CP (U=5728, z=−2.8, p<0.01; Fig. 2). The parents of children with CP reported to be never or seldom satisfied about their child’s sleep in 8.9% of cases compared to a significantly lower proportion (1.3%) of parents of typically developing children (Fisher’s exact test, p=0.006).
Figure 2.
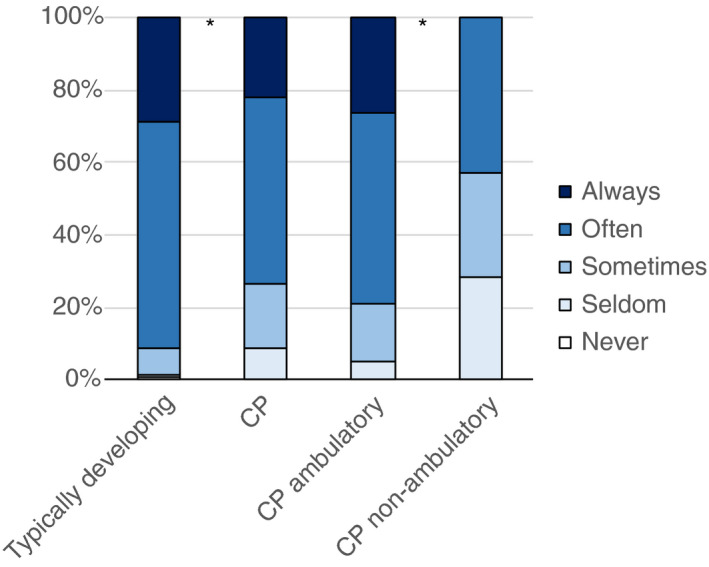
Parent‐reported satisfaction about child sleep in children with cerebral palsy (CP; total, ambulatory, and non‐ambulatory) compared to typically developing children. The single asterisk indicates a significant difference (Mann–Whitney U test, p<0.05) between the CP and typically developing study groups or between ambulatory and non‐ambulatory children with CP.
Parent sleep
No differences were observed in the distribution of responses on the two parental sleep items of sleep satisfaction (P1) and sleep deprivation (P2) between the parents of children with CP and the parents of typically developing children (both p>0.05). Of the parents of children with CP, 13.6% reported to be never or seldom satisfied about their own sleep compared to 8.9% recorded in the parents of typically developing children (Fig. 3). When parents were asked whether they felt sleep‐deprived, one‐third (34.1%) of parents of children with CP reported feeling sleep‐deprived often or always compared to a quarter (24.8%) of parents of typically developing children.
Figure 3.
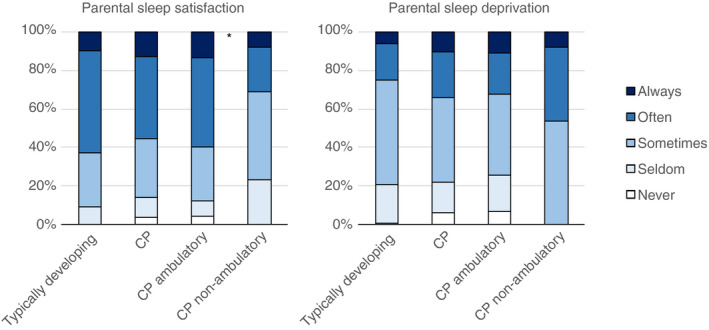
Self‐rated sleep satisfaction and sleep deprivation in the parents of children with cerebral palsy (CP; total, ambulatory, and non‐ambulatory) compared to the parents of typically developing children. The single asterisk indicates a significant difference (Mann–Whitney U test, p<0.05) between ambulatory and non‐ambulatory children with CP.
Child factors and sleep problems in children with CP
Sex
No differences were found between males and females regarding child sleep problems (individual items and total number of sleep problems), use of sleep medication, sleep satisfaction, or parental sleep (all p>0.05).
Age
The parents of older children reported that their child would wake less frequently during the night than the parents of younger children (U=671.5, z=−1.71, p<0.05) and the parents of older children were more often satisfied with their child’s sleep compared to those of younger children (U=625.5, z=−2.08, p<0.02). No other differences were found with regard to age (all p>0.05).
Walking ability
Although no association was found between walking ability and the presence of a sleep problem (i.e. having at least one sleep problem occurring often or always; Fisher’s exact test, p>0.05), the child‐by‐child distribution of the total number of sleep problems was significantly higher for non‐ambulatory children (U=355.50, z=−2,06, p<0.05). Specifically, waking up during the night (U=286, z=−2.89, p<0.01), pain or discomfort in bed (U=348.5, z=−1.96, p<0.05), and daytime fatigue (U=319, z=−2.14, p<0.05) were significantly more frequently reported by the parents of non‐ambulatory children compared to ambulatory children (Fig. 1), while the parents of non‐ambulatory children more often reported to ‘not know’ whether their child had nightmares. No difference was found between the proportion of children using sleep medication across walking ability (Fisher’s exact test, p>0.05).
Satisfaction about child sleep was significantly differently distributed across walking ability; the parents of ambulatory children were more often satisfied about their child’s sleep (U=264, z=−3.24, p<0.001, Fig. 2).
With regard to parental sleep, the parents of ambulatory children were more often satisfied about their own sleep (U=347.5, z=−1.75, p<0.05) than the parents of non‐ambulatory children (Fig. 3). Moreover, the parents of non‐ambulatory children seemed to feel sleep‐deprived more often than the parents of ambulatory children, although this difference was not significant (U=364, z=−1.54, p=0.06).
Discussion
We found that sleep problems are commonly reported by the parents of children with CP and that these children are more likely to have a sleep problem compared to their typically developing peers. In addition, non‐ambulatory children with CP were more severely affected by sleep problems than ambulatory children and their parents were less satisfied about their child’s and their own sleep. Also, a large group of parents reported feeling sleep‐deprived.
Children with CP have a spectrum of sleep problems similar to typically developing children, with both difficulty falling sleep and early‐morning waking being signs of (behavioural) insomnia, the most prevalent sleep disorder across childhood. This is supported by findings from our study, which found that the most frequently reported sleep problems in typically developing children were difficulty falling sleep (22.3%) and early‐morning waking (19.7%), which were reported in comparably high frequencies by the parents of children with CP (30% and 26.7% respectively). In addition to these similarities, we found that children with CP were more likely to have other sleep disruptions, especially night‐time waking and pain or discomfort in bed, compared to typically developing children. Also, daily functioning was more impaired; one‐third (33.3%) of children with CP were reported to suffer from fatigue during the day often or always compared to 3.2% of typically developing children.
Although recognizing and addressing sleep problems will likely be beneficial for all children with CP, this may be especially worthwhile for those classified in higher GMFCS levels. In our study, non‐ambulatory children showed a higher total number of sleep problems, which is in line with previous studies reporting higher frequencies of abnormal total sleep scores with increasing GMFCS level. 20 , 21 First, waking up during the night for the total group of children with CP (14.4%) is lower than in other studies reporting night‐time waking in children with CP, ranging from 23.2% to 36%. 22 , 23 However, for children with CP who are non‐ambulatory, we found that 42.9% (compared to 9.2% of ambulatory children) of parents reported frequent night‐time waking. Second, pain or discomfort in bed was more frequently reported in children who were more severely affected. Physical discomfort and pain are increased by muscle spasms and joint contractures; together with an impaired ability to change sleep positions, these are likely to adversely affect the child’s sleep quality. 24 Third, children with CP who are non‐ambulatory were reported to suffer from daytime fatigue or sleepiness often or always in 50% of cases compared to 30.3% of ambulatory children. These rates are comparable to previous studies reporting on the prevalence of daytime sleepiness in children with CP, which ranges from 12.8% to 63.5%. 3
In line with previous research on sleep outcomes in the parents of children with neurodevelopmental disabilities, 7 , 17 we found that poor sleep quality was reported by a large group of parents and especially by those with non‐ambulatory children. However, it should be noted that the parental sleep items did not specifically enquire about the cause of poor parent sleep quality; therefore, there could have been other disruptors at play unrelated to or in addition to their child’s sleep. Children with physical disabilities, including CP, are more likely to require night‐time parental attention, 25 which may contribute to greater sleep disturbance for caregivers. 16 Mothers experiencing the highest number of sleep disruptions have children with the highest care needs. 26 In addition to affecting parental sleep, child sleep problems and night‐time care requirements have repeatedly been associated with increased psychological exhaustion and decreased well‐being among parents. 7 , 16 , 27 , 28 , 29 Clearly, sleep problems in children with CP and the impact that they have on the family should be addressed, and this includes paying attention to parental sleep.
Children with CP showed higher frequencies of sleep problems compared to typically developing children but these differences were not as great as expected. This might be explained by the fact that frequencies, not severity, were reported; therefore, more severe problems might be at play that are reported with the same frequency. Also, the reference of parents with children with CP may be different from that of parents with typically developing children, giving rise to parents accepting abnormal sleep patterns because they think it is to be expected when dealing with CP. 15
This study has several strengths and limitations. First, all sleep outcome measures were based on parental reports; although this is likely to be the primary source of information in the paediatric clinical setting, reporter bias may have occurred. However, the results reflect the extent to which parents perceive their child’s sleep as problematic, which has also been shown to affect family well‐being. 15 Second, the checklist is not a validated screening instrument but was designed as a practical tool to open and facilitate the conversation about sleep with parents in the health care setting. 18 In contrast to more extensive sleep screening tools like the Sleep Disturbance Scale for Children, the 24‐hour activity checklist includes questions about parental sleep. This not only gives an insight into the impact of sleep problems beyond the child, it also stimulates a family‐centred care for sleep, an important wish of parents of children with CP. 15 Although the number of children classified in the higher GMFCS levels IV and V in our study is small (n=14; 15.6%), the distribution of ambulatory and non‐ambulatory children with CP is comparable to cohort data from the Netherlands. 30 Children with CP who have additional comorbidities such as epilepsy, visual, and cognitive impairments have more sleep problems than children without comorbidities, although the effects of comorbidities on the prevalence of sleep problems are not consistent. 3 We did not collect such additional information from the children’s medical files; therefore, comorbidities could potentially have contributed, especially in the more complex non‐ambulatory group, to excess night‐time waking and daytime fatigue. Also, no further background information on the socio‐demographic aspects of our samples were collected and this may influence the generalizability of the findings. Finally, a strength of this study is the use of reference data, which allowed us to place the findings on sleep problems in children with CP in the context of those reported by the parents of typically developing children.
In conclusion, the findings of this study demonstrate that: (1) sleep problems are more common in children with CP than in their typically developing peers, (2) non‐ambulatory children with CP are more severely affected by sleep problems than ambulatory children both in frequency and number of sleep problems, and (3) a large group of parents (of both children with CP and typically developing children) is sleep‐deprived. These results call for more attention to be placed on the importance of sleep in paediatric health care, especially in more vulnerable populations like children with CP and their parents, to improve their sleep health and well‐being.
Supporting information
Figure S1: The sleep section of the 24‐hour activity checklist.
Acknowledgements
The authors express their gratitude to the children and parents who participated in this study and the health care professionals and colleagues who helped to collect data from patients and from the general population. We thank Ron Hulst for entering the data, Eline Scholten for statistical advice, Sebas van Baarsen for providing feedback on graphic colour design, and CP Nederland and OuderInzicht for their contribution to the development of the 24‐hour activity checklist. The authors have stated they had no interests that might be perceived as posing a conflict or bias.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
- 1. Chaput J‐P, Gray CE, Poitras VJ, et al. Systematic review of the relationships between sleep duration and health indicators in school‐aged children and youth. Appl Physiol Nutr Metab 2016; 41: S266–82. [DOI] [PubMed] [Google Scholar]
- 2. Odding E, Roebroeck ME, Stam HJ. The epidemiology of cerebral palsy: incidence, impairments and risk factors. Disabil Rehabil 2006; 28: 183–91. [DOI] [PubMed] [Google Scholar]
- 3. Horwood L, Li P, Mok E, Shevell M, Constantin E. A systematic review and meta‐analysis of the prevalence of sleep problems in children with cerebral palsy: how do children with cerebral palsy differ from each other and from typically developing children? Sleep Health 2019; 5: 555–71. [DOI] [PubMed] [Google Scholar]
- 4. Dutt R, Roduta‐Roberts M, Brown C. Sleep and children with cerebral palsy: a review of current evidence and environmental non‐pharmacological interventions. Children (Basel) 2015; 2: 78–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Petersen S, Francis KL, Reddihough DS, Lima S, Harvey A, Newall F. Sleep problems and solution seeking for children with cerebral palsy and their parents. J Paediatr Child Health 2020; 56: 1108–13. [DOI] [PubMed] [Google Scholar]
- 6. Owens J. Classification and epidemiology of childhood sleep disorders. Prim Care 2008; 35: 533–46. [DOI] [PubMed] [Google Scholar]
- 7. Adiga D, Gupta A, Khanna M, Taly AB, Thennarasu K. Sleep disorders in children with cerebral palsy and its correlation with sleep disturbance in primary caregivers and other associated factors. Ann Indian Acad Neurol 2014; 17: 473–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Horwood L, Li P, Mok E, Oskoui M, Shevell M, Constantin E. Health‐related quality of life in Canadian children with cerebral palsy: what role does sleep play? Sleep Med 2019; 54: 213–22. [DOI] [PubMed] [Google Scholar]
- 9. Newman CJ, O’Regan M, Hensey O. Sleep disorders in children with cerebral palsy. Dev Med Child Neurol 2006; 48: 564–8. [DOI] [PubMed] [Google Scholar]
- 10. Sandella DE, O’Brien LM, Shank LK, Warschausky SA. Sleep and quality of life in children with cerebral palsy. Sleep Med 2011; 12: 252–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Romeo DM, Brogna C, Quintiliani M, et al. Sleep disorders in children with cerebral palsy: neurodevelopmental and behavioral correlates. Sleep Med 2014; 15: 213–8. [DOI] [PubMed] [Google Scholar]
- 12. Honaker SM, Meltzer LJ. Sleep in pediatric primary care: a review of the literature. Sleep Med Rev 2016; 25: 31–9. [DOI] [PubMed] [Google Scholar]
- 13. Hulst RY, Pillen S, Voorman JM, Rave N, Visser‐Meily JMA, Verschuren O. Sleep health practices and sleep knowledge among healthcare professionals in Dutch paediatric rehabilitation. Child Care Health Dev 2020; 46: 703–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Verschuren O, Gorter JW, Pritchard‐Wiart L. Sleep: an underemphasized aspect of health and development in neurorehabilitation. Early Hum Dev 2017; 113: 120–8. [DOI] [PubMed] [Google Scholar]
- 15. Hulst RY, Voorman JM, Pillen S, Ketelaar M, Visser‐Meily JMA, Verschuren O. Parental perspectives on care for sleep in children with cerebral palsy: a wake‐up call. Disabil Rehabil 2020: 1–10. 10.1080/09638288.2020.1770873 (Online ahead of print). [DOI] [PubMed] [Google Scholar]
- 16. Mörelius E, Hemmingsson H. Parents of children with physical disabilities: perceived health in parents related to the child’s sleep problems and need for attention at night. Child Care Health Dev 2014; 40: 412–8. [DOI] [PubMed] [Google Scholar]
- 17. Micsinszki SK, Ballantyne M, Cleverley K, Green P, Stremler R. Sleep outcomes for parents of children with neurodevelopmental disabilities: a systematic review. J Fam Nurs 2018; 24: 217–49. [DOI] [PubMed] [Google Scholar]
- 18. Verschuren O, Hulst RY, Voorman J, et al. 24‐hour activity for children with cerebral palsy: a clinical practice guide. Dev Med Child Neurol 2021; 63: 54–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Prinsen CAC, Mokkink LB, Bouter LM, et al. COSMIN guideline for systematic reviews of patient‐reported outcome measures. Qual Life Res 2018; 27: 1147–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Munyumu K, Idro R, Abbo C, et al. Prevalence and factors associated with sleep disorders among children with cerebral palsy in Uganda: a cross‐sectional study. BMC Pediatr 2018; 18: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Romeo DM, Brogna C, Musto E, et al. Sleep disturbances in preschool age children with cerebral palsy: a questionnaire study. Sleep Med 2014; 15: 1089–93. [DOI] [PubMed] [Google Scholar]
- 22. Zuculo GM, Knap CC, Pinato L. Correlation between sleep and quality of life in cerebral palsy. Codas 2015; 26: 447–56. [DOI] [PubMed] [Google Scholar]
- 23. Elsayed RM, Hasanein BM, Sayyah HE, El‐Auoty MM, Tharwat N, Belal TM. Sleep assessment of children with cerebral palsy: using validated sleep questionnaire. Ann Indian Acad Neurol 2013; 16: 62–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lélis AL, Cardoso MVLM, Hall WA. Sleep disorders in children with cerebral palsy: an integrative review. Sleep Med Rev 2016; 30: 63–71. [DOI] [PubMed] [Google Scholar]
- 25. Hemmingsson H, Stenhammar AM, Paulsson K. Sleep problems and the need for parental night‐time attention in children with physical disabilities. Child Care Health Dev 2009; 35: 89–95. [DOI] [PubMed] [Google Scholar]
- 26. Bourke‐Taylor H, Pallant JF, Law M, Howie L. Relationships between sleep disruptions, health and care responsibilities among mothers of school‐aged children with disabilities. J Paediatr Child Health 2013; 49: 775–82. [DOI] [PubMed] [Google Scholar]
- 27. Wright M, Tancredi A, Yundt B, Larin HM. Sleep issues in children with physical disabilities and their families. Phys Occup Ther Pediatr 2006; 26: 55–72. [PubMed] [Google Scholar]
- 28. Barlow JH, Cullen‐Powell LA, Cheshire A. Psychological well‐being among mothers of children with cerebral palsy. Early Child Dev Care 2006; 176: 421–8. [Google Scholar]
- 29. Wayte S, McCaughey E, Holley S, Annaz D, Hill CM. Sleep problems in children with cerebral palsy and their relationship with maternal sleep and depression. Acta Paediatr 2012; 101: 618–23. [DOI] [PubMed] [Google Scholar]
- 30. Smits D‐W, Gorter JW, Riddell CA, et al. Mobility and self‐care trajectories for individuals with cerebral palsy (aged 1–21 years): a joint longitudinal analysis of cohort data from the Netherlands and Canada. Lancet Child Adolesc Health 2019; 3: 548–57. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1: The sleep section of the 24‐hour activity checklist.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


