Abstract
Background
Sleep problems interfere with work performance. Decreased work productivity due to health problems is defined as presenteeism. Although empirical data on the improvement of presenteeism by sleep interventions have been published, a systematic review elucidating whether there is a difference in the improvement of presenteeism across various types of sleep interventions has not yet been published. This systematic review of studies aimed to clarify which sleep interventions are more likely to be effective in improving presenteeism.
Methods
The electronic databases PubMed, PsycINFO, and MEDLINE were used to perform a literature search (the start and end search dates were October 20, 2019, and March 11, 2020, respectively). A combination of terms such as “employee*,” “sleep,” “insomnia,” and “presenteeism” was used for the search. Both randomized and non-randomized control trials were included in this systematic review.
Results
Six types of sleep interventions were identified, including cognitive behavioral therapy for insomnia (CBT-I), sleep hygiene education, yoga, mindfulness, weight loss program, and changing the color temperature of fluorescent lights in the workplace. Only CBT-I improved both sleep problems and presenteeism compared with a control group. The results of this review also show that there is heterogeneity in the measurement of presenteeism.
Conclusions
The results of this systematic review suggested that CBT-I could be adapted for workers with sleep problems and presenteeism. We discussed whether CBT-I improved both sleep problems and presenteeism compared with other interventions. In addition, methods for measuring presenteeism in future research are proposed.
Keywords: Sleep, Insomnia, Presenteeism, Systematic review
Background
Presenteeism is an indicator of productivity loss and is characterized by the loss of productivity due to health problems, even though workers are present at work [1]. For example, presenteeism can be assessed from time management demands, physical demands, mental-interpersonal demands, and output demands [2]. Presenteeism increases the risk of absences in the long term [3, 4]. Presenteeism is not only a predictor of productivity loss but also a predictor of sickness absence due to health problems. To improve presenteeism, it is important to focus on the health status of workers.
Sleep plays an important role in mental and physical health. Individuals with insomnia symptoms had higher rates of physical and psychiatric illnesses and presenteeism than individuals without insomnia symptoms [5]. Insomnia symptoms can cause depressive symptoms [6], suicidal ideation [7], metabolic syndrome [8], and work-related accidental deaths [9]. Those with a risk of insomnia have 5.49-times higher rates of presenteeism than those without risk of insomnia [10]. In a study of the general working population, severe insomnia symptoms were found to intensify presenteeism, regardless of sex [11]. Sleep duration also affects presenteeism; 7–8 h of sleep result in lower presenteeism than less than 6 h or more than 9 h, and the relationship between sleep duration and presenteeism follows a U-shaped curve [12, 13]. Short sleep duration can have effects on the economy and induce losses worldwide [14]. Therefore, improving sleep problems leads to improved presenteeism.
Several previous studies have shown that sleep interventions can improve presenteeism. The sleep medication eszopiclone has been reported to improve presenteeism [15]. Internet-based cognitive behavioral therapy for insomnia (CBT-I) and internet-based sleep hygiene education have been reported to improve presenteeism [16, 17]. Thus, improving sleep problems may have an important role in improving presenteeism.
CBT-I, mindfulness meditation, physical activity, and light therapy have been demonstrated to improve sleep problems in systematic reviews and meta-analyses [18–23]. However, no systematic review or meta-analysis has found that sleep interventions improve functioning in daily life. Although empirical data on the improvement of presenteeism by sleep interventions have been previously published, a systematic review on whether there is a difference in the improvement of presenteeism between the various types of sleep interventions has not yet been published. Sleep and physical and mental health are closely related. Therefore, a systematic review of which sleep interventions improve presenteeism may provide guidance for effective intervention for presenteeism. As such, this study sought to clarify which sleep interventions are more likely to be effective in improving presenteeism using a systematic review of the studies.
Materials and methods
Search strategies
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [24] and A MeaSurement Tool to Assess Systematic Reviews (AMSTAR 2) guidelines [25]. The literature search strategy was based on the literature search terms of a systematic review that examined the effectiveness of workplace health promotion in improving presenteeism [26]. We used a combination of terms such as “employee*,” “sleep,” “insomnia,” and “presenteeism.” The electronic databases PubMed, PsycINFO, and MEDLINE were used to search the literature (the start and end search dates were October 20, 2019, and March 11, 2020).
Study selection
The inclusion criteria for papers were as follows: (1) the presence of employees, (2) sleep intervention must be performed, (3) sleep problems must be measured, (4) presenteeism must be measured, (5) written in English or Japanese, and (6) publication in a peer-reviewed journal. The selection of studies was carried out by YT, SI, and SA. Papers written in English or Japanese were included in the study since the authors were well-versed in both Japanese and English, but not in other languages.
Data extraction
Information on subject selection criteria, study design, implementation program, duration, program contents, measurement of sleep problems, measurement of presenteeism, sleep problems outcome results, and presenteeism outcome results were extracted from the studies included in the systematic review. Extraction was carried out independently by YT and SI.
Study quality assessments
Because this review included randomized (RCTs) and non-randomized control trials (non-RCTs), we used different tools for assessing the risk of bias for RCTs and non-RCTs. The risk of bias was assessed independently by YT and SA using the Cochrane Collaboration’s tool for assessing the risk of bias in RCTs [27]. This tool for assessing the risk of bias was based on (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective outcome reporting, and (7) other sources of bias. Other sources of bias addressed differences between groups regarding outcome measures at baseline. The tool evaluates each domain as having a “low risk of bias,” “high risk of bias,” and “unclear risk of bias.” The Risk of Bias In Non-randomized Studies of Interventions tool (ROBINS-I tool) was used to assess the risk of bias in non-RCTs [28]. This tool assesses the risk of bias by (1) bias due to confounding, (2) bias in the selection of participants for the study, (3) bias in the classification of interventions, (4) bias due to deviations from intended interventions, (5) bias due to missing data, (6) bias in the measurement of outcomes, and (7) bias in the selection of the reported results. The tool evaluates each domain and the overall assessment as having a “low risk of bias,” “moderate risk of bias,” “serious risk of bias,” “critical risk of bias,” and “no information.”
Results
Search findings
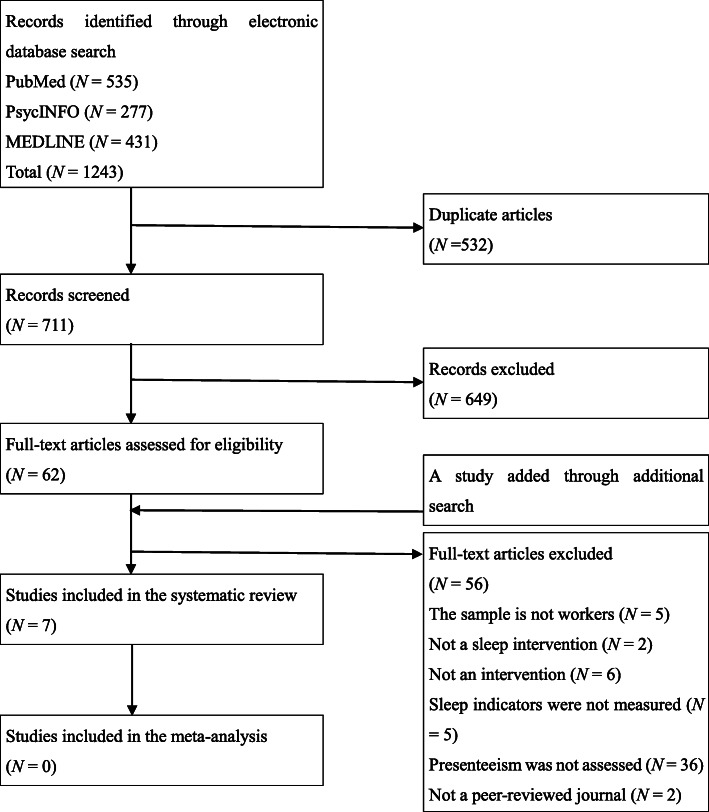
Studies included in the review were selected by the first and third authors. Altogether, 1243 studies were screened for duplication. Following the screening, a total of 711 studies were selected, of which 62 studies were selected after evaluating the abstract against the eligibility criteria. YT and SI evaluated the full text of the 62 studies using the eligibility criteria. Finally, six studies were selected for inclusion in this review. One study was added through an additional search. This study was not found by the search formula because “presenteeism” was not included in the abstract. However, the study was included in the review after discussion among the first, second, and third authors who conducted the literature review, because it had been collected in PubMed and met the selection criteria for this study. Finally, seven studies were included in this systematic review. Because of heterogeneity in the measures of sleep problems and presenteeism, we could not perform a meta-analysis (Fig. 1).
Fig. 1.
PRISMA flow diagram of the systematic search carried out in this study
Study quality assessments
The risk of bias was assessed for each of the four RCTs that were included in the systematic review (Table 1). In the domains of blinding of outcome assessment and other sources of bias, 3/4 studies were assessed as having a low risk of bias. Random sequence generation, allocation concealment, and incomplete outcome data indicated a low risk of bias in 2/4 studies. In the domain of blinding of participants and personnel, 1/4 of the studies were determined to have a low risk of bias. There were no reports with a low risk of bias in selective outcome reporting. Moreover, 3/4 of the studies did not include information about the study protocol, which may have caused potential reporting bias.
Table 1.
Risk of bias items for each included randomized control trial study
| Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective outcome reporting | Other sources of bias | |
|---|---|---|---|---|---|---|---|
| Bostock et al. [16] | + | + | ? | + | ? | ? | + |
| Behrendt et al. [29] | + | + | – | + | – | – | ? |
| Wolever et al. [30] | ? | ? | ? | ? | + | ? | + |
| Morgan et al. [31] | – | ? | + | + | + | ? | + |
Low risk of bias is “+”. High risk of bias is “-”. Unclear risk of bias is “?”
The risk of bias was assessed for three non-RCT studies that were included in the systematic review (Table 2). In the domains of bias in the selection of participants for the study and bias in the classification of interventions, all three studies were assessed as having a low risk of bias. In contrast, there were no studies assessed as having a low risk of bias in domains other than bias in the selection of participants for the study and bias in the classification of interventions. In the domains of bias due to missing data and bias in the measurement of outcomes, 2/3 studies were assessed as having a critical risk of bias. Because these domains assessed the post-intervention phase, there may be bias in the post-intervention process.
Table 2.
Risk of bias items for each included non-randomized control trial study
| Bias due to confounding | Bias in the selection of participants for the study | Bias in classification of interventions | Bias due to deviations from intended intervention | Bias due to missing data | Bias in measurement of outcomes | Bias in the selection of the reported results | Overall | |
|---|---|---|---|---|---|---|---|---|
| Espie et al. [11] | Serious | Low | Low | Serious | Critical | Critical | Serious | Critical |
| Burton et al. [17] | Serious | Low | Low | Serious | Critical | Critical | Serious | Critical |
| Mills et al. [32] | Serious | Low | Low | Serious | Moderate | Moderate | Serious | Serious |
In addition, because of the small number of studies included in the review, attention should be paid to the risk of bias of each study in the overall assessment.
Study characteristics
The characteristics of the studies included in the systematic review are shown in Table 3.
Table 3.
Characteristics of the studies included in the systematic review
| Study | Age | Sex | Country | Job type | Design | Intervention | Duration | Program components |
|---|---|---|---|---|---|---|---|---|
| Bostock et al. (2016) [16] |
CBT-I 33.9 ± 6.41 years WLC 33.3 ± 5.59 years All 33.6 ± 6.01 years |
CBT-I Men: 88 Women: 47 WLC Men: 92 Women: 43 |
United States | Office-based staff | RCT (vs. WLC) | CBT-I (digital cognitive behavioral therapy: Sleepio) |
6 weeks (6 sessions) |
Sleep restriction, stimulus control, relaxation, paradoxical intention, belief restructuring, mindfulness |
| Espie et al. (2018) [11] | 50.0 ± 11.14 years |
Men: 147 Women: 67 |
United States |
Office Plant Retail & service |
Single arm |
CBT-I (digital cognitive behavioral therapy: Sleepio) |
6 weeks (6 sessions) |
Sleep restriction, stimulus control, relaxation, paradoxical intention, belief restructuring, mindfulness |
| Behrendt et al. (2020) [29] |
CBT-I 46.1 ± 9.5 years WLC 46.7 ± 9.7 years All 46.5 ± 9.8 years |
CBT-I Men: 29 Women: 59 WLC Men: 32 Women: 57 |
German | Diverse job categories recruited via media | RCT (vs. WLC) | Internet-delivered CBT-I |
6 weeks (6 sessions) |
Psychoeducation, sleep hygiene, sleep restriction, stimulus control, relaxation, metacognitive therapy, potential future application |
| Burton et al. (2016) [17] |
20–35 years: 78 36–50 years: 163 ≥51 years: 116 |
Men: 86 Women: 271 |
United States | Financial service | Single arm | Sleep hygiene education | 5 months | Psychoeducation, sleep hygiene, identification of sleep disorders and information on the sleep disorders, relaxation, mindfulness |
| Wolever et al. (2012) [30] |
Yoga: 41.6 ± 10.1 years Mindfulness: 44.3 ± 9.4 years WLC 42.7 ± 9.7 years |
Yoga Men: 24 Women: 66 Mindfulness Men: 22 Women: 74 WLC Men: 10 Women: 43 |
United States | Insurance | RCT (vs. WLC) | Yoga or mindfulness |
Yoga: 12 weeks (12 h) Mindfulness: 12 weeks (14 h) |
Yoga Yoga poses, breathing techniques, relaxation, mental techniques Mindfulness Mindfulness meditation |
| Morgan et al. (2012) [31] |
Intervention 44.8 ± 8.3 years WLC 43.7 ± 9.1 years All 44.4 ± 8.6 years |
Only men (N = 110) | Australia | Aluminum smelter | RCT (vs. WLC) | The workplace power program | 14 weeks | Education for weight loss, weekly weight reports, daily diet, and exercise with a pedometer |
| Mills et al. (2007) [32] | N/A | N/A | United Kingdom | Call-handler |
Control trail (2900 K) |
Changing the color temperature of fluorescent lights in the workplace | 14 weeks | 17,000 K vs. 2900 K |
CBT-I Cognitive behavioral therapy for insomnia, WLC Waiting list control, RCT Randomized control trial, N/A Not applicable
Inclusion criteria for participants
In total, 4/7 studies had inclusion criteria for participants, including poor subjective sleep quality, voluntary participation in the program, perceived stress scale score of 10 or more, and body mass index (BMI) in the range of 25 to 40 kg/m2. On the other hand, 3/7 studies did not have any selection criteria for participants. In all seven studies, presenteeism was not included in the inclusion criteria for participants.
Measurements
Measures of sleep problems included the sleep condition indicator (N = 2), insomnia severity index (N = 1), Mayo clinic tool (N = 1), Pittsburgh Sleep Quality Index (N = 1), Epworth sleepiness scale (N = 1), and Columbia jet lag scale (N = 1).
Measures of presenteeism included the Work Limitation Questionnaire (WLQ; N = 3), Work Productivity and Activity Impairment questionnaire (WPAI; N = 2), the number of days that work efficiency is reduced due to ill health (N = 1), and the World Health Organization Health and Work Performance Questionnaire (WHO-HPQ; N = 1).
Study designs
With regard to study design, 4/7 studies that were RCTs had a waitlist control. Moreover, 3/7 studies had a non-RCT study design, and 1/3 studies with a non-RCT design had a control group.
Effectiveness of sleep interventions
Six different types of sleep interventions were identified, including CBT-I, sleep hygiene education, yoga, mindfulness, weight loss program, and changing the color temperature of fluorescent lighting in the workplace. The type of intervention, outcome measures of sleep problems, outcome measures for and statistical significance of presenteeism, and risk of bias were summarized for each study (Table 4).
Table 4.
Sleep and presenteeism outcomes for each study included in the systematic review
| Study | Intervention | Sleep outcomes | Presenteeism outcomes | Statistical significance (Presenteeism) | Risk of bias (Cochrane Collaboration’s tool) | Risk of bias (ROBINS-I) |
|---|---|---|---|---|---|---|
| Bostock et al. (2016) [16] |
CBT-I (Digital cognitive behavioral therapy: Sleepio) Intervention vs. control |
SCI | WPAI | F (1, 485) = 10.99, p < 0.001, d = 0.67 |
Low risk of bias: 4/7 High risk of bias: 0/7 Unclear risk of bias: 3/7 |
N/A |
| Espie et al. (2018) [11] |
CBT-I (Digital cognitive behavioral therapy: Sleepio) Pre vs. post |
SCI | WPAI | t (87) = 4.83, p < 0.01 | N/A | Critical |
| Behrendt et al. (2020) [29] |
Internet-delivered CBT-I Intervention vs. control |
ISI | Self-report of the number of days in the past 3 months that work efficiency has decreased due to ill health |
Posttreatment N/A 6-months follow-up mean difference between groups = −6.455, p < 0.001, d = 0.83 |
Low risk of bias: 3/7 High risk of bias: 3/7 Unclear risk of bias: 1/7 |
N/A |
| Burton et al. (2016) [17] |
Sleep hygiene education Pre vs. post |
Mayo Clinic tool |
WLQ Time-management demands Physical demands Mental-interpersonal demands Output demands Overall |
No description of the coefficient of the chi-square test Time-management demands p < 0.001 Physical demands n.s. Mental-interpersonal demands p < 0.001 Output demands p < 0.001 Overall p < 0.001 |
N/A | Critical |
| Wolever et al. (2012) [30] |
Yoga Mindfulness Intervention vs. control |
PSQI | WLQ (overall) | F (2, 233) = 2.07, n.s., η2 = 0.02 |
Low risk of bias: 2/7 High risk of bias: 0/7 Unclear risk of bias: 5/7 |
N/A |
| Morgan et al. (2012) [31] |
The workplace power program Intervention vs. control |
ESS |
WLQ Time-management demands Physical demands Mental-interpersonal demands Output demands Overall |
Time-management demands mean difference between groups is 7.7, p = 0.20, d = 0.37 Physical demands mean difference between groups is 9.8, p = 0.04, d = 0.41 Mental-interpersonal demands mean difference between groups is 5.0, p = 0.11, d = 0.35 Output demands mean difference between groups is 6.1, p = 0.23, d = 0.29 Overall mean difference between groups is 2.0, p = 0.01, d = 0.56 |
Low risk of bias: 4/7 High risk of bias: 1/7 Unclear risk of bias: 2/7 |
N/A |
| Mills et al. (2007) [32] |
Changing the color temperature of fluorescent lights in the workplace (17,000 K vs. 2900 K) Intervention vs. control Pre vs. post |
Item 9 of Columbia Jet Lag Scale (sleepiness during the day) | WHO-HPQ |
Overall t (67) = −2.72, n.s. Intervention change t (45) = − 6.07, p < 0.001 Control change t (22) = − 1.16, n.s. |
N/A | Serious |
ROBINS-I Risk of Bias In Non-randomized Studies of Interventions, CBT-I Cognitive behavioral therapy for insomnia, SCI Sleep Condition Indicator, WPAI Work Productivity and Impairment questionnaire, N/A Not applicable, ISI Insomnia Severity Index, WLQ Work Limitation Questionnaire, n.s. not significant, PSQI Pittsburgh Sleep Quality Index, ESS Epworth Sleepiness Scale, WHO-HPQ World Health Organization Health and Work Performance Questionnaire
Cognitive behavioral therapy for insomnia (CBT-I)
CBT-I was conducted in three studies [11, 16, 29]. Of these, 2/3 studies had an RCT design, and 1/3 studies had a single-arm design. The program included sleep restriction, stimulus control, relaxation, and cognitive reconstruction as common components. All three studies used a weekly program of six sessions, 2/3 studies used the iOS app “Sleepio,” and 1/3 studies used internet-delivered self-help CBT-I. All three studies were internet-based interventions and were not face-to-face.
CBT-I significantly improved insomnia symptoms and presenteeism in all three studies.
Sleep hygiene education
Only one study provided sleep hygiene education [17]. The study had a single-arm design. The program included understanding the relationship between sleep and health and productivity, acquiring healthy sleep hygiene habits, identifying and treating sleep disorders, and relaxation and mindfulness. The program was conducted once a month for five sessions. The program was delivered via an internet-based intervention.
Sleep hygiene education significantly improved with insomnia symptoms. On the other hand, significant improvements in presenteeism were observed in time management demands, mental-interpersonal demands, and output demands, except for physical demands.
Yoga or mindfulness
Only one study provided a yoga or mindfulness intervention [30]. The study had an RCT design. The yoga intervention included yoga postures, breathing techniques, relaxation, and mental techniques. The mindfulness intervention was mindfulness meditation. Both yoga and mindfulness were conducted for 12 weeks. However, the total duration of yoga was 12 h for 12 weeks and the total duration of mindfulness was 14 h for 12 weeks. Yoga was conducted face-to-face, and mindfulness was conducted face-to-face or via the internet.
Both yoga and mindfulness significantly improved insomnia symptoms, but not presenteeism.
Workplace-based weight loss program
Only one study provided a workplace-based weight loss program [31]. The study had an RCT design. The program consisted of weight loss instructions and a pedometer report of activity and diet. The duration of the program was 14 weeks. The program was conducted in the form of both face-to-face and online meetings.
The weight loss program did not significantly improve daytime sleepiness. Only physical demands significantly improved presenteeism, while it was not significantly improved by time management demands, mental-interpersonal demands, and output demands.
Changing the color temperature of fluorescent lighting in the workplace
Only one study provided a change in the color temperature of fluorescent lighting in the workplace [32]. The study had a control trial design. The intervention was to change the color temperature of fluorescent lighting on the floor (17,000 K vs. 2900 K).
There was no significant improvement in daytime sleepiness or presenteeism between groups as a result of changing the color temperature of the fluorescent lights (17,000 K vs. 2900 K). However, daytime sleepiness and presenteeism were significantly improved in the 17,000 K group, while the 2900 K group did not show significant improvement in daytime sleepiness and presenteeism in the within-group comparison.
Discussion
This study sought to identify in a systematic manner which sleep interventions were more likely to improve presenteeism and provide guidelines for effective intervention for presenteeism caused by sleep problems. CBT-I is expected to be highly effective in improving presenteeism. However, this study could not explore the effectiveness of intervention methods for sleep other than CBT-I in improving presenteeism because only a few studies have been conducted to date.
Heterogeneity in the measurement methods of presenteeism
In this study, a meta-analysis could not be conducted because of the small number of studies included and the use of different methods of measuring presenteeism. Three CBT-I studies were conducted; however, we could not conduct a meta-analysis because of the different measurement methods used in the studies. We were unable to integrate the measures of presenteeism because they were either a standardized self-reported scale or the number of days of reduced work efficiency due to ill health, and integration of these measures would increase heterogeneity and prevent a fair assessment of the quality of the evidence. Heterogeneity in the measurement of presenteeism has also been shown to be a limitation in previous studies [26] that have reviewed the effectiveness of workplace health promotion. The results of this study revealed that there has been no standardized method for measuring presenteeism over the past 10 years. Heterogeneity in the way in which presenteeism is measured arises because of the different definitions of presenteeism in the U.S. and Europe. In the U.S., presenteeism is defined as a decline in work productivity due to workers’ health problems. In Europe, on the other hand, it is defined as people who go to work when they have health conditions that require them to take time off. Each definition has different advantages: the U.S. definition allows us to measure the economic burden of health problems, while the European definition allows for a wide range of research into why people exhibit presenteeism [33]. Future studies will hopefully be able to conduct meta-analyses using both a standardized self-reported scale and the number of days of reduced work efficiency due to ill health as outcome measures and will be able to refine programs to improve presenteeism.
Effectiveness of sleep interventions
Only CBT-I improved both sleep problems and presenteeism compared with a control group. In other words, CBT-I might be adapted for workers with sleep problems and presenteeism. The results of meta-analyses have suggested that CBT-I is effective in improving insomnia symptoms in the short-term and long-term [18–20]. CBT-I is mediated by work-related rumination and worry in the process of insomnia symptom improvement [29]. In addition, CBT-I not only improves insomnia symptoms, but also improves functional health, psychological well-being, and sleep-related impairment by improving insomnia symptoms [34]. Therefore, CBT-I improves not only insomnia symptoms but also daily life functions impaired by insomnia symptoms. Thus, CBT-I may be effective in improving presenteeism.
The decision to apply CBT-I to workers would need to take into account whether or not they work shifts. Most of the participants of CBT-I in the studies included in the review were office workers. However, it is doubtful whether CBT-I is sufficiently effective in improving insomnia symptoms when administered to shift workers. For example, when shift workers (e.g., nurses, bakers, cabin attendants, security personnel, and land transportation personnel) underwent group CBT-I, self-help CBT-I, and sleep hygiene education, there was no difference in the improvement of insomnia symptoms between groups [35]. Moreover, group CBT-I also did not affect the overall improvement of insomnia in participants whose working areas were stores, offices, warehouses, or logistics workplaces. However, when shift workers (warehouse and logistics) were excluded, there was an improvement in insomnia symptoms [36]. Therefore, the effectiveness of CBT-I for improving presenteeism may be limited to non-shift workers (e.g., office workers) rather than all workers.
CBT-I improved not only subjective insomnia symptoms but also objective sleep onset latency, total wake time, wake time after sleep onset, early-morning awakening, and sleep efficiency [19]. Therefore, interventions that can improve not only subjective sleep indicators but also objective sleep indicators might improve presenteeism.
Sleep hygiene education, mindfulness, yoga, weight loss programs, and changing the color temperature of workplace fluorescent lighting were not effective in improving both insomnia symptoms and presenteeism. These interventions can improve subjective insomnia symptoms, but they do not improve objective insomnia symptoms or are unknown [21, 22, 37, 38]. It remains unclear whether these interventions improve functioning in daily life due to insomnia symptoms. These points are different from CBT-I. Therefore, presenteeism may not have improved. However, since this study included only one study of each intervention, it is not possible to discuss what effect these interventions had on the improvement of presenteeism.
Inclusion and exclusion criteria for participants
Presenteeism was not included as a criterion for the selection of participants in all of the studies included in this review. This is due to the unclear criterion of presenteeism. The cutoff point for presenteeism is a WHO-HPQ score of 40 points or less for Japanese workers [39]. In the future, the criteria for presenteeism will become clearer as more studies establish cutoff points on existing standardized measures of presenteeism.
One study included in this review had a BMI in the range of 25–40 kg/m2 as an inclusion criterion for participants [31]. Being overweight increases the risk of presenteeism [40], but weight loss is not associated with improved presenteeism [41]. However, a study included in this review showed that daytime sleepiness did not improve, but a part of presenteeism did [31]. Therefore, the impact of being overweight on the intervention program is not clear. Thus, having a BMI of 25 or more may be a confounding factor for the intervention effect. Except for weight loss programs, a BMI of 25 or greater should be one of the individual variables to be controlled.
Study quality assessments
In this study, the risk of bias in RCTs and non-RCTs was assessed separately. The results suggested that RCTs are more likely to have a risk of bias with regard to random sequence generation, allocation concealment, incomplete outcome data, and selective outcome reporting. The results suggested that non-RCTs are more likely to have a risk of bias in response to missing data and selective outcome reporting. These risks of bias can be addressed at the study protocol stage. It is hoped that future RCTs and non-RCTs will provide high-quality interventions by appropriately addressing the areas of potential bias risk identified in this study.
In addition, because of the small number of studies included in the review, attention should be paid to the risk of bias of each study in the overall assessment.
Limitation
None of the studies included in this review included Asian countries other than Japan. Therefore, generalization of the results of this study to other Asian countries should be made with caution. In particular, Japan has a higher rate of economic loss due to short sleep duration than the United States and Europe [14]. Future, empirical studies are necessary to determine whether sleep interventions can improve presenteeism among Japanese and other Asian populations.
Conclusion
Although it should be noted that the evidence that CBT-I improves presenteeism remains limited due to the small number of studies included in this study, as well as the inability to conduct a meta-analysis, the results demonstrated that CBT-I might be adapted to daytime workers (e.g., office workers) with sleep problems and presenteeism. Interventions for sleep that improve presenteeism may require improvement in subjective and objective insomnia symptoms and in the functioning of daily life due to insomnia symptoms. Future research is warranted to reveal sleep interventions that can improve not only sleep problems but also daily functioning.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Abbreviations
- BMI
Body mass index
- CBT-I
Cognitive behavioral therapy for insomnia
- RCT
Randomized controlled trial
- WHO-HPQ
World Health Organization Health and Work Performance Questionnaire
Authors’ contributions
YT conceived the study, reviewed the study, and wrote and edited the manuscript. SI and SA reviewed the study and wrote and edited the manuscript. NN and YS wrote, edited, and provided overall guidance for the development of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by JSPS KAKENHI Grant Number JP21K03101.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Burton WN, Pransky G, Conti DJ, Chen CY, Edington DW. The association of medical conditions and presenteeism. J Occup Environ Med. 2004;46(6):S38–S45. doi: 10.1097/01.jom.0000126687.49652.44. [DOI] [PubMed] [Google Scholar]
- 2.Lerner D, Amick BC, 3rd, Rogers WH, Malspeis S, Bungay K, Cynn D. The work limitations questionnaire. Med Care. 2001;39(1):72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Janssens H, Clays E, Clercq BD, De Bacquer D, Braeckman L. The relationship between presenteeism and different types of future sickness absence. J Occup Health. 2013;55(3):132–141. doi: 10.1539/joh.12-0164-OA. [DOI] [PubMed] [Google Scholar]
- 4.Suzuki T, Miyaki K, Song Y, Tsutsumi A, Kawakami N, Shimazu A, et al. Relationship between sickness presenteeism (WHO-HPQ) with depression and sickness absence due to mental disease in a cohort of Japanese workers. J Affect Disord. 2015;180:14–20. doi: 10.1016/j.jad.2015.03.034. [DOI] [PubMed] [Google Scholar]
- 5.Bolge SC, Doan JF, Kannan H, Baran RW. Association of insomnia with quality of life, work productivity, and activity impairment. Qual Life Res. 2009;18(4):415–422. doi: 10.1007/s11136-009-9462-6. [DOI] [PubMed] [Google Scholar]
- 6.Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Kato T. Insomnia symptoms, depressive symptoms, and suicide ideation in Japanese white-collar employees. Int J Behav Med. 2014;21:506–510. doi: 10.1007/s12529-013-9364-4. [DOI] [PubMed] [Google Scholar]
- 8.Troxel WM, Buysse DJ, Mathews KA, Kip KE, Strollo PJ, Hall M, et al. Sleep symptoms predict the development of the metabolic syndrome. Sleep. 2010;33(12):1633–1640. doi: 10.1093/sleep/33.12.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Åkerstedt T, Fredlund P, Gillberg M, Jansson B. A prospective study of fatal occupational accidents relationship to sleeping difficulties and occupational factors. J Sleep Res. 2002;11(1):69–71. doi: 10.1046/j.1365-2869.2002.00287.x. [DOI] [PubMed] [Google Scholar]
- 10.Swanson LM, Arnedt JT, Rosekind MR, Belenky G, Balkin TJ, Drake C. Sleep disorders and work performance: findings from the 2008 national sleep foundation sleep in America poll. J Sleep Res. 2011;20(3):487–494. doi: 10.1111/j.1365-2869.2010.00890.x. [DOI] [PubMed] [Google Scholar]
- 11.Espie CA, Pawlecki B, Waterfield D, Fitton K, Radocchia M, Luik AI. Insomnia symptoms and their association with workplace productivity: cross-sectional and pre-post intervention analyses from a large multinational manufacturing company. Sleep Health. 2018;4(3):307–312. doi: 10.1016/j.sleh.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 12.Guertler D, Vandelanotte C, Short C, Alley S, Schoeppe S, Duncan MJ. The association between physical activity, sitting time, sleep duration, and sleep quality as correlates of presenteeism. J Occup Environ Med. 2015;57(3):321–328. doi: 10.1097/JOM.0000000000000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burton WN, Chen CY, Schultz AB, Li X. Association between employee sleep with workplace health and economic outcomes. J Occup Environ Med. 2017;59(2):177–183. doi: 10.1097/JOM.0000000000000934. [DOI] [PubMed] [Google Scholar]
- 14.Hafner M, Stepanek M, Taylor J, Troxel WM, van Stolk C. Why sleep matters-the economic costs of insufficient sleep: a cross-country comparative analysis. Rand Health Q. 2017;6(4):11. [PMC free article] [PubMed] [Google Scholar]
- 15.Walsh JK, Krystal AD, Amato DA, Rubens R, Caron J, Wessel TC, et al. Nightly treatment of primary insomnia with eszopiclone for six months: effect on sleep, quality of life, and work limitations. Sleep. 2007;30(8):959–968. doi: 10.1093/sleep/30.8.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bostock S. Luik Ai, Espie CA. Sleep and productivity benefits of digital cognitive behavioral therapy for insomnia: a randomized controlled trial conducted in the workplace environment. J Occup Environ Med. 2016;58(7):683–689. doi: 10.1097/JOM.0000000000000778. [DOI] [PubMed] [Google Scholar]
- 17.Burton WN, Chen CY, Li X, McCluskey M, Erickson D, Barone D, et al. Evaluation of a workplace-based sleep education program. J Occup Environ Med. 2016;58(9):911–917. doi: 10.1097/JOM.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 18.Murawski B, Wade L, Plotnikoff RC, Lubans DR, Duncan MJ. A systematic review and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Sleep Med Rev. 2018;40:160–169. doi: 10.1016/j.smrv.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Okajima I, Komada Y, Inoue Y. A meta-analysis on the treatment effectiveness of cognitive behavioral therapy for primary insomnia. Sleep Biol Rhythms. 2011;9:24–34. doi: 10.1111/j.1479-8425.2010.00481.x. [DOI] [Google Scholar]
- 20.van der Zweerde T, Bisdounis L, Kyle SD, Lancee J, van Straten A. Cognitive behavioral therapy for insomnia: a meta-analysis of long-term effects in controlled studies. Sleep Med Rev. 2019;48:101208. doi: 10.1016/j.smrv.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 21.Rusch HL, Rosario M, Levison LM, Olivera A, Livingston WS, Wu T, et al. The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Ann N Y Acad Sci. 2019;1445(1):5–16. doi: 10.1111/nyas.13996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Banno M, Harada Y, Tanifuchi M, Tobita R, Tsujimoto H, Tsujimoto Y, et al. Exercise can improve sleep quality: a systematic review and meta-analysis. PeerJ. 2018;6:e5172. doi: 10.7717/peerj.5172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Maanen A, Meijer AM, van der Heijden B, Oort FJ. The effects of light therapy on sleep problems: a systematic review and meta-analysis. Sleep Med Rev. 2016;29:52–62. doi: 10.1016/j.smrv.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 24.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomized or non-randomised studies of healthcare interventions, or both. BMJ. 2017;21(358):j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cancelliere C, Cassidy JD, Ammendolia C, Côte P. Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health. 2011;11:395. doi: 10.1186/1471-2458-11-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Higgins JPT, Altman DG. Chapter 8: assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane handbook for systematic review of intervention. Chichester (UK): John Wiley & Sons; 2008. pp. 187–241. [Google Scholar]
- 28.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Behrendt D, Ebert DD, Spiegelhalder K, Lehr D. Efficacy of a self-help web-based recovery training in improving sleep in workers: randomized controlled trial in the general working population. J Med Internet Res. 2020;22(1):e13346. doi: 10.2196/13346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wolever RQ, Bobinet KJ, McCabe K, Mackenzie ER, Fekete E, Kusnick CA, et al. Effective and viable mind-body stress reduction in the workplace: a randomized controlled trial. J Occup Health Psychol. 2012;17(2):246–258. doi: 10.1037/a0027278. [DOI] [PubMed] [Google Scholar]
- 31.Morgan PJ, Collins CE, Plotnikoff RC, Cook AT, Berthon B, Mitchell S, et al. The impact of a workplace-based weight loss program on work-related outcomes in overweight male shift workers. J Occup Environ Med. 2012;54(2):122–127. doi: 10.1097/JOM.0b013e31824329ab. [DOI] [PubMed] [Google Scholar]
- 32.Mills PR, Tomkins SC, Schlange LJM. The effect of high correlated colour temperature office light on employee wellbeing and work performance. J Circadian Rhythms. 2007;11(5):2. doi: 10.1186/1740-3391-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lohaus D, Habermann W. Presenteeism: a review and research directions. Hum Resour Manag Rev. 2019;29(1):43–58. [Google Scholar]
- 34.Espie CA, Emsley R, Kyle SD, Gordon C, Drake CL, Siriwardena AN, et al. Effect of digital cognitive behavioral therapy for insomnia on health, psychological well-being, and sleep-related quality of life: a randomized clinical trial. JAMA Psychiatry. 2019;76(1):21–30. doi: 10.1001/jamapsychiatry.2018.2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Järnefelt H, Härmä M, Sallinen M, Virkkala J, Paajanen T, Martimo KP, et al. Cognitive behavioural therapy interventions for insomnia among shift workers: RCT in an occupational health setting. Int Arch Occup Environ Health. 2020;93(5):535–550. doi: 10.1007/s00420-019-01504-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schiller H, Söderström M, Lekander M, Rajaleid K, Kecklund G. A randomized controlled intervention of workplace-based group cognitive behavioral therapy for insomnia. Int Arch Occup Environ Health. 2018;91(4):413–424. doi: 10.1007/s00420-018-1291-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chung KF, Lee CT, Yeung WF, Chan MS, Chung EW, Lin WL. Sleep hygiene education as a treatment of insomnia: a systematic review and meta-analysis. Fam Pract. 2018;35(4):365–375. doi: 10.1093/fampra/cmx122. [DOI] [PubMed] [Google Scholar]
- 38.Afonso RF, Hachul H, Kozasa EH, De Souza OD, Goto V, Rodrigues D, et al. Yoga decreases insomnia in postmenopausal women: a randomized clinical trial. Menopause. 2012;19(2):186–193. doi: 10.1097/gme.0b013e318228225f. [DOI] [PubMed] [Google Scholar]
- 39.Suzuki T, Miyaki K, Sasaki Y, Song Y, Tsutsumi A, Kawakami N, et al. Optimal cutoff values of WHO-HPQ presenteeism scores by ROC analysis for preventing mental sickness absence in Japanese prospective cohort. PLoS One. 2014;9(10):e111191. doi: 10.1371/journal.pone.0111191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schultz AB, Edington SW. Employee health and presenteeism: a systematic review. J Occup Rehabil. 2007;17(3):547–579. doi: 10.1007/s10926-007-9096-x. [DOI] [PubMed] [Google Scholar]
- 41.Harden SM, You W, Almeida FA, Hill JL, Linnan LA, Allen KC, et al. Does successful weight loss in an internet-based worksite weight loss program improve employee presenteeism and absenteeism? Health Educ Behav. 2015;42(6):769–774. doi: 10.1177/1090198115578751. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.