Abstract
Objective:
To analyze and compare pharyngeal airflow characteristics pre- and post–mandibular setback surgery in patients with Class III skeletal dysplasia using cone beam computed tomography (CBCT) and computational fluid dynamics (CFD).
Materials and Methods:
Records of 29 patients who had received orthodontic treatment along with mandibular setback surgery were obtained. CBCT scans were obtained at three time points: T1 (before surgery), T2 (average of 6 months after surgery), and T3 (average of 1 year after surgery). Digitized pharyngeal airway models were generated from these scans. CFD was used to simulate and characterize pharyngeal airflow.
Results:
Mean airway volume was significantly reduced from 35,490.324 mm3 at T1 to 24,387.369 mm3 at T2 and 25,069.459 mm3 at T3. Significant increase in mean negative pressure was noted from 3.110 Pa at T1 to 6.116 Pa at T2 and 6.295 Pa at T3. There was a statistically significant negative correlation between the change in airway volume and the change in pressure drop at both the T2 and T3 time points. There was a statistically significant negative correlation between the amount of mandibular setback and change in pressure drop at the T2 time point.
Conclusions:
Following mandibular setback surgery, pharyngeal airway volume was decreased and relative mean negative pressure was increased, implying an increased effort required from a patient for maintaining constant pharyngeal airflow. Thus, high-risk patients undergoing a large amount of mandibular setback surgery should be evaluated for obstructive sleep apnea and the proposed treatment plan be revised based on the risk for potential airway compromise.
Keywords: Computational fluid dynamics, Upper airway changes, Obstructive sleep apnea (OSA), Mandibular setback surgery, Airway volume, Negative airway pressure
INTRODUCTION
Depending upon the population, the prevalence of Class III malocclusion has been noted to be as high as 26%.1 In extreme cases, surgical correction with orthodontics is often the treatment of choice to achieve an ideal result. One of the surgical techniques used for this correction is mandibular setback. However, an important side effect of this surgical procedure is a change in the position of the base of the tongue and, concurrently, the position of the hyoid bone. The posterior movement in the position of these anatomical structures causes a decrease in the pharyngeal airway space.1,2 The new anatomy of this region establishes a breathing pattern characteristically seen in patients with obstructive sleep apnea (OSA).3
Although the etiology of OSA is a multifactorial conundrum, obstruction of the upper airway due to collapse of the surrounding soft tissues, especially from the retropalatal and retroglossal regions, is a pivotal factor.4 Many studies have been performed to help understand the effect of mandibular setback surgery on airway volume. However, most of this existent research is based on data derived from lateral cephalograms.5–9 The major flaw with this approach is the use of a two-dimensional image to evaluate a three-dimensional structure.10
Extensive research has been performed to study the effects of maxillo-mandibular advancement surgery on the airway volume using three-dimensional (3D) imaging modalities.11 3D imaging allows the use of computational fluid dynamics (CFD) for assessing pharyngeal airflow via the vantage point of different airflow characteristics, such as velocity, turbulence, pressure drop, etc.12 Although evidence is available for the effects of mandibular setback on airway volume, to the best of our knowledge no study has been performed to evaluate the effects of mandibular setback on changes in airway pressure and, subsequently, on airflow characteristics.3,5,7–9,13–17 Thus, the aim of this study was to use CFD to evaluate the changes in pharyngeal airflow characteristics before and after mandibular setback surgery in skeletal Class III patients.
MATERIALS AND METHODS
Sample
Records of 29 patients who had received orthodontic treatment along with mandibular setback surgery to correct Class III skeletal dysplasia were obtained. The sample comprised 18 male and 11 female subjects with a mean age of 23.67 ± 6.28 years (range = 18–52 years). The sample was retrieved from the Department of Orthodontics at Busan National University Hospital, Busan, South Korea. The setback surgery consisted of bilateral sagittal split osteotomy of the mandible with rigid fixation. Cone beam computed tomography (CBCT) scans were captured at three time points: T1 (before surgery), T2 (6 months after surgery), and T3 (1 year after surgery). The inclusion criteria for this study were adult subjects with Class III skeletal deformities who had undergone mandibular setback surgery along with concurrent orthodontic treatment. The exclusion criteria were no symptoms of respiratory disease, no symptoms of temporomandibular disorders, no evidence of syndromes affecting facial morphology, and no pronounced facial asymmetry. The St Louis University Institutional Review Board approved this study.
CBCT Technique
CBCT images (DCTpro, Vatech, Seoul, South Korea) were acquired with the patients seated in an upright position and with maximum intercuspation of teeth and the Frankfort horizontal plane oriented parallel to the floor. Maximal intercuspation position of teeth was chosen over centric relation as a result of its higher reproducibility. The patients were scanned for 24 seconds using a CBCT machine with a field of view of 20 × 19 cm, a voxel size of 0.4 mm, a tube voltage of 90 kVp, and a tube current of 4.0 mA. Dolphin 11.5 3D Imaging Software (Dolphin Imaging Systems LLC, Chatsworth, Calif) and ITK-SNAP (www.itksnap.org)—a software application used to segment structures in 3D medical images—were used to view, analyze, and manipulate the CBCT scans.
Calculation of Surgical Movement
All CBCT scans were standardized in position by creating a reference plane. This plane was created by drawing a line through the sella and nasion and then subtracting by 7° to obtain a corrected horizontal plane. Subsequently, a line perpendicular to this corrected horizontal plane was constructed from the nasion. Since the amount of antero-posterior surgical movement was calculated as a linear distance between this perpendicular line and B-point, this linear distance was measured on a lateral cephalogram created from the standardized CBCT scan (Figure 1). These amounts of antero-posterior surgical movements were measured and compared presurgically and postsurgically.
Figure 1.
Measurement of surgical movement on lateral cephalogram.
Isolating the Pharyngeal Airway
CBCT scans were subsequently imported into ITK-SNAP software (www.itksnap.org) as DICOM (Digital Imaging and Communications in Medicine) files to generate a volumetric image of the scanned region. After the volumetric image was generated, the pharyngeal airway of interest was isolated. The superior border was defined by creating a plane passing through the anterior nasal spine and the posterior nasal spine; this line was then extended posteriorly. The inferior border was defined by creating a plane passing through the menton and the most antero-inferior point on the corpus of the fourth cervical vertebra. The anterior and posterior walls of the volume were defined by the anatomical borders of the pharynx (Figure 2).
Figure 2.
Airway volume model segmentation boundaries.
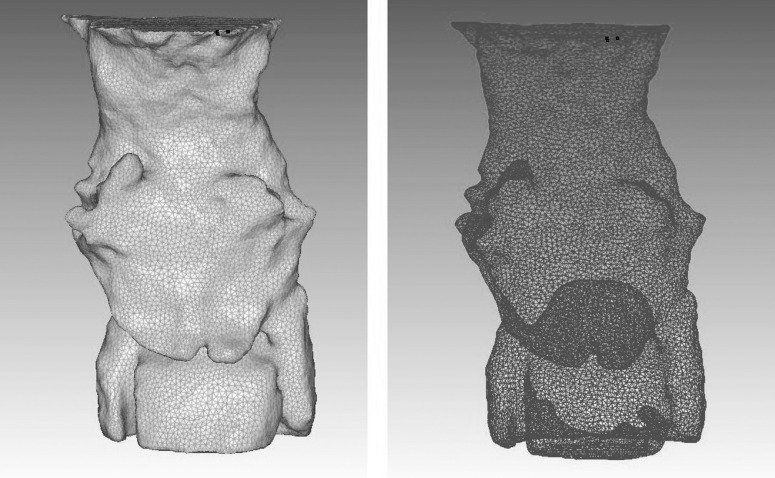
Computer Modeling and Mesh Generation
Pharyngeal airway models were imported into SC/Tetra preprocessing software (version 12.0, Software Cradle Corporation, Osaka, Japan) for model and mesh generation. Inlet, outlet, and wall boundaries were defined manually (Figure 3).
Figure 3.
(A) 3D airway model and (B) mesh model file demonstrating tetrahedral elements.
Appropriate grid size, number of tetrahedral elements, and octree size of a minimum of 0.3 mm were chosen for the mesh model. The final mesh models of the airway were used to calculate the volume via the preprocessing software, and each had a minimum of 300,000 tetrahedral elements.
Solving Methods
Mesh models were imported into SC/Tetra solver (version 12.0, Software Cradle Corporation) for airflow simulation. A turbulent flow model, the RNG k-ɛ model, was used to simulate turbulent airflow within the pharyngeal airway.
The equations for this model were the following:
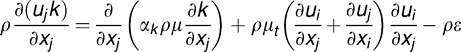 |
and
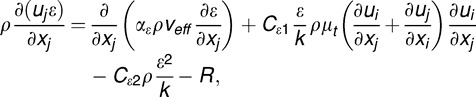 |
where
 |
In the equations above, vmol is the molecular dynamic viscosity and veff is the effective dynamic viscosity. R is the characteristic length (=√Ain/π, with Ain as the area at the inlet section), ρ is the fluid viscosity, uij is the velocity component in Cartesian coordinates, x, y, z are the coordinate axes, xij is the coordinate directions, η is the expansion parameter, and Cμ, Cɛ1, and Cɛ2 are constants equal to 0.085, 1.42, and 1.68, respectively.18
The RNG k-ɛ model was chosen because of its minimal computing power required for flow simulation. Corresponding mass flow rate (Fua) was calculated using the equation Fua = Qρ, where Q is the volumetric flow rate (340 mL/s) and ρ is the density of air. This corresponding mass flow rate (Fua) was set as the inlet boundary condition.19 The outlet boundary condition was set at a static pressure of 0 Pa. The walls of the model, which were assumed to be rigid and noncompliant, were set at no-slip conditions. Airflow simulations were completed using the SC/Tetra solver function on a PC with an Intel® Core™ i7-3740QM CPU at 2.70 GHz with 16 GB of RAM. After solver functions were completed, SC/Tetra postprocessor software (version 12.0, Software Cradle Corporation) was used to analyze and visualize the fluid flow rate.
Pressure Calculations
The postprocessor function of SC/Tetra was used to calculate the change in pressure, Δp, from the inlet to the outlet boundary over the digitized models for all 29 patients at T1, T2, and T3 time points. All measurements were recorded in the midsagittal plane of the airway.
Statistical Analysis
Analysis of the data was completed using IBM SPSS Statistics 23.0 (Armonk, NY). Descriptive statistics calculated the mean and standard deviation for percent pressure drop and percent airway volume change between T2 and T1 and between T3 and T1. Spearman's correlation coefficient was used to check the correlation among percent airway volume change, percent pressure drop, and mandibular skeletal setback between the three time points. A significance level of P < .05 was used.
RESULTS
Surgical Movement
The mean mandibular skeletal setback was 7.714 mm (6.469, 8.959) (standard error [SE]: 0.608) at 6 months after the surgery (T2-T1), and it changed to 7.056 mm (5.931, 8.180) (SE: 0.549) at a year after the surgery (T3-T1).
Volumetric Data
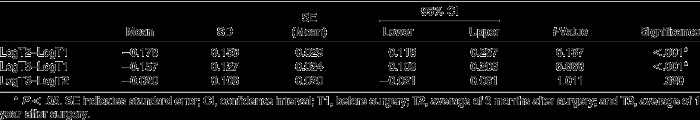
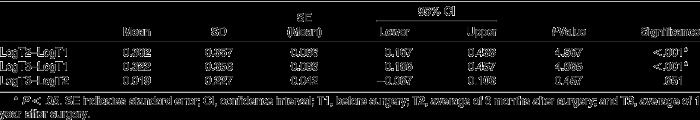
Pressure drop change and volume change variables were not normally distributed. Hence, these variables were log-transformed to calculate change in pressure drop and change in volume at the three different time points. Since the data assumed normal distribution following log transformation, it was possible to perform paired t-tests on these transformed data (Tables 1 and 2).
Table 1.
Differences in Volume Between the Three Time Points: Means, Standard Deviations (SDs), and Paired t-Tests
Table 2.
Differences in Pressure Drop Between the Three Time Points: Means, Standard Deviations (SDs), and Paired t-Tests
There was a statistically significant difference between the presurgical airway volume and the postsurgical airway volume at both the 6-month and 1-year time points. The difference in airway volume between the 6-month and 1-year time points after surgery was statistically insignificant.
Airflow Data
There was a statistically significant difference between the presurgical pressure drop and the postsurgical pressure drop at both the 6-month and 1-year timepoints. The difference in pressure drop between the 6-month and 1-year time points after surgery was statistically insignificant.
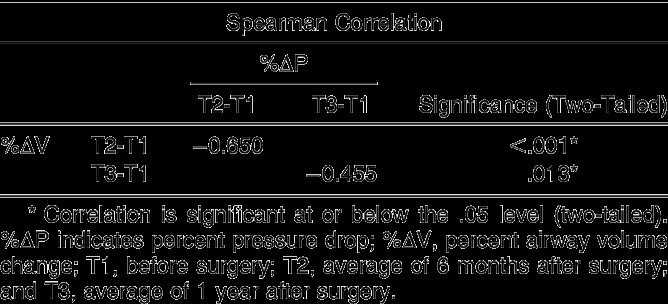
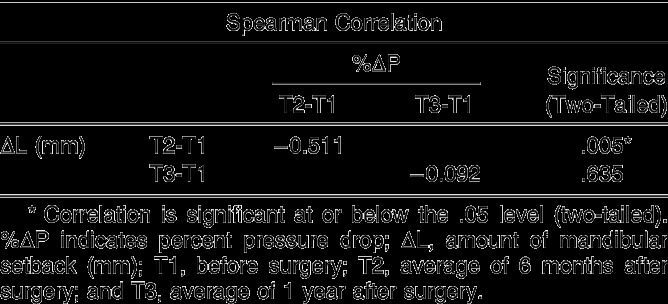
Correlation Analysis
Correlations between percent airway volume change and percent pressure drop change and between skeletal mandibular setback and percent pressure drop change are exhibited in Tables 3 and 4, respectively.
Table 3.
Correlation Between Percent Airway Volume Change and Percent Pressure Drop Change
Table 4.
Correlation Between Skeletal Mandibular Setback and Percent Pressure Drop Change
There was a statistically significant, strong, negative correlation between the percent change in pressure drop and the percent change in airway volume at both T2 and T3 time points. A statistically significant negative but weak correlation was found between the percent change in pressure drop and the amount of mandibular setback at the T2 time point. At the T3 time point, the strong negative correlation between percent change in pressure drop and the amount of mandibular setback was statistically insignificant.
DISCUSSION
Functional handicap and esthetics are some of the most important challenges faced by subjects with extreme Class III skeletal dysplasia. One of the most common treatment approaches taken to correct this is mandibular setback surgery. However, there have been reports3,5 in the past of normal patients becoming afflicted with OSA after undergoing mandibular setback surgery.
Multiple studies3,5,7–9,13–17 have attempted to demonstrate and explain the effect of mandibular setback surgery on pharyngeal airway space and volume. Most of these studies2,3,5,9,14,15,17,20 demonstrated significant reduction in airway volume after mandibular setback surgery. However, the relationship between a reduction in the airway volume and the consequent effort required to sustain normal breathing pattern has not been investigated so far.
We therefore undertook this study to compare the pharyngeal airflow characteristics before and after mandibular setback surgery using CBCT and CFD in 29 patients with Class III skeletal dysplasia. A percentage change in pressure dependent on the percentage change in volume was measured to evaluate if the reduction in airway volume space after a mandibular setback surgery would cause a subsequent change in the pressure and, thus, the effort required to push a volume of air through the respiratory airway.
Restructuring of the pharyngeal anatomy occurs after mandibular setback surgery. Ozbek et al.21 reported that there is significant downward and backward displacement of the hyoid bone immediately after mandibular setback surgery. Becker et al.20 reported that this postsurgical displacement of the hyoid bone results in decreased volume of the lower oropharynx for up to 12 months after surgery. Many authors6,13 have argued that the hyoid bone comes back to its presurgical cephalo-caudal position after this time point. However, Kawakami et al.2 claim that although the hyoid bone returns to its position in the sagittal plane, it still remains posteriorly displaced, thus causing a reduction in pharyngeal airway space. This claim has been substantiated for periods of as long as 12 years after surgery.7
In recent years, the use of CFD has become widely popular to assess the effects of treatment modalities that change the upper airway anatomy. It provides an accurate assessment of airflow by virtue of its usage of patient-specific airway geometrical characteristics.11 Researchers have used CFD to simulate the effects of improvement in breathing of OSA patients after maxillo-mandibular advancement surgery.22
Using anatomically correct airway models and a RNG κ-ɛ turbulence flow model, we found a profound increase in mean negative pressure at both the 6-month and 1-year intervals after mandibular setback surgery. A statistically significant inverse correlation was found between a reduction in the airway volume and the pressure drop in the airway. From a clinical significance standpoint, these findings show that an isolated mandibular setback surgery causes an increase in mean negative pressure with concurrent alteration in airway geometry. This might lead to an increase in the breathing effort required. However, sleep studies are required to confirm this.
Some of the limitations of this study are the limited extent of the airway under study, the fact that patients were awake during the scans and in an upright posture, the absence of a sleep study, the lack of sleepiness scales or questionnaires, the unknown stage of respiration, and the lack of tongue control. In addition, the airway is not a rigid structure, and the effect of the flaccidness of the soft tissue could not be taken into consideration.
CONCLUSIONS
There is a significant correlation between the reduction in airway volume and the increase in mean negative pressure following mandibular setback surgery.
There is a significant correlation between an average of 7.71 mm of mandibular setback and the percentage pressure drop.
These findings might be suggestive of an increased effort required for maintaining constant pharyngeal airflow. Thus, high-risk patients undergoing a large amount of mandibular setback during surgery should be evaluated for OSA and the proposed treatment plan be revised based on the risk for potential airway compromise.
REFERENCES
- 1.Ngan P, Moon W. Evolution of Class III treatment in orthodontics. Am J Orthod Dentofacial Orthop. 2015;148:22–36. doi: 10.1016/j.ajodo.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 2.Kawakami M, Yamamoto K, Fujimoto M, Ohgi K, Inoue M, Kirita T. Changes in tongue and hyoid positions, and posterior airway space following mandibular setback surgery. J Craniomaxillofac Surg. 2005;33:107–110. doi: 10.1016/j.jcms.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Liu SY, Huon LK, Iwasaki T, et al. Efficacy of maxillomandibular advancement examined with drug-induced sleep endoscopy and computational fluid dynamics airflow modeling. Otolaryngol Head Neck Surg. 2016;154:189–195. doi: 10.1177/0194599815611603. [DOI] [PubMed] [Google Scholar]
- 4.Schwab RJ, Goldberg AN. Upper airway assessment: radiographic and other imaging techniques. Otolaryngol Clin North Am. 1998;31:931–968. doi: 10.1016/s0030-6665(05)70100-6. [DOI] [PubMed] [Google Scholar]
- 5.Hochban W, Schurmann R, Brandenburg U, Conradt R. Mandibular setback for surgical correction of mandibular hyperplasia—does it provoke sleep-related breathing disorders? Int J Oral Maxillofac Surg. 1996;25:333–338. doi: 10.1016/s0901-5027(06)80024-x. [DOI] [PubMed] [Google Scholar]
- 6.Samman N, Tang SS, Xia J. Cephalometric study of the upper airway in surgically corrected Class III skeletal deformity. Int J Adult Orthod Orthognath Surg. 2002;17:180–190. [PubMed] [Google Scholar]
- 7.Eggensperger N, Smolka W, Iizuka T. Long-term changes of hyoid bone position and pharyngeal airway size following mandibular setback by sagittal split ramus osteotomy. J Craniomaxillofac Surg. 2005;33:111–117. doi: 10.1016/j.jcms.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Chen F, Terada K, Hua Y, Saito I. Effects of bimaxillary surgery and mandibular setback surgery on pharyngeal airway measurements in patients with Class III skeletal deformities. Am J Orthod Dentofacial Orthop. 2007;131:372–377. doi: 10.1016/j.ajodo.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 9.Saitoh K. Long-term changes in pharyngeal airway morphology after mandibular setback surgery. Am J Orthod Dentofacial Orthop. 2004;125:556–561. doi: 10.1016/j.ajodo.2003.04.017. [DOI] [PubMed] [Google Scholar]
- 10.Sears CR, Miller AJ, Chang MK, Huang JC, Lee JS. Comparison of pharyngeal airway changes on plain radiography and cone-beam computed tomography after orthognathic surgery. J Oral Maxillofac Surg. 2011;69:e385–e394. doi: 10.1016/j.joms.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 11.Sittitavornwong S, Waite PD, Shih AM, et al. Computational fluid dynamic analysis of the posterior airway space after maxillomandibular advancement for obstructive sleep apnea syndrome. J Oral Maxillofac Surg. 2013;71:1397–1405. doi: 10.1016/j.joms.2013.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huynh J, Kim KB, McQuilling M. Pharyngeal airflow analysis in obstructive sleep apnea patients pre- and post-maxillomandibular advancement surgery. J Fluids Eng. 2009;131:091101–10. [Google Scholar]
- 13.Athanasiou AE, Toutountzakis N, Mavreas D, Ritzau M, Wenzel A. Alterations of hyoid bone position and pharyngeal depth and their relationship after surgical correction of mandibular prognathism. Am J Orthod Dentofacial Orthop. 1991;100:259–265. doi: 10.1016/0889-5406(91)70063-3. [DOI] [PubMed] [Google Scholar]
- 14.Enacar A, Aksoy AU, Sencift Y, Haydar B, Aras K. Changes in hypopharyngeal airway space and in tongue and hyoid bone positions following the surgical correction of mandibular prognathism. Int J Adult Orthod Orthognath Surg. 1994;9:285–290. [PubMed] [Google Scholar]
- 15.Guven O, Saracoglu U. Changes in pharyngeal airway space and hyoid bone positions after body ostectomies and sagittal split ramus osteotomies. J Craniofac Surg. 2005;16:23–30. doi: 10.1097/00001665-200501000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Tselnik M, Pogrel MA. Assessment of the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg. 2000;58:282–285. doi: 10.1016/s0278-2391(00)90053-3. discussion 285–287. [DOI] [PubMed] [Google Scholar]
- 17.Turnbull NR, Battagel JM. The effects of orthognathic surgery on pharyngeal airway dimensions and quality of sleep. J Orthod. 2000;27:235–247. doi: 10.1179/ortho.27.3.235. [DOI] [PubMed] [Google Scholar]
- 18.Wilcox DC. Turbulence Modeling for CFD 1st ed. La Cãnada, Calif: DCW Industries Inc;; 1993. 460. [Google Scholar]
- 19.De Backer JW, Vanderveken OM, Vos WG, et al. Functional imaging using computational fluid dynamics to predict treatment success of mandibular advancement devices in sleep-disordered breathing. J Biomech. 2007;40:3708–3714. doi: 10.1016/j.jbiomech.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 20.Becker OE, Avelar RL, Goelzer JG. Dolzan Ado N, Haas OL Jr, De Oliveira RB. Pharyngeal airway changes in Class III patients treated with double jaw orthognathic surgery—maxillary advancement and mandibular setback. J Oral Maxillofac Surg. 2012;70:e639–e647. doi: 10.1016/j.joms.2012.07.052. [DOI] [PubMed] [Google Scholar]
- 21.Ozbek MM, Miyamoto K, Lowe AA, Fleetham JA. Natural head posture, upper airway morphology and obstructive sleep apnoea severity in adults. Eur J Orthod. 1998;20:133–143. doi: 10.1093/ejo/20.2.133. [DOI] [PubMed] [Google Scholar]
- 22.Powell NB, Mihaescu M, Mylavarapu G, Weaver EM, Guilleminault C, Gutmark E. Patterns in pharyngeal airflow associated with sleep-disordered breathing. Sleep Med. 2011;12:966–974. doi: 10.1016/j.sleep.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]