Abstract
Objective:
To investigate posttreatment changes in the maxillary and mandibular arches in patients who underwent orthodontic treatment during the mixed and permanent dentitions.
Materials and Methods:
The sample was collected retrospectively from three private practices and consisted of 42 patients who were at least 10 years out of orthodontic treatment. The longitudinal records of study casts and cephalometric radiographs were analyzed to quantify posttreatment changes.
Results:
Minimal changes in maxillary and mandibular irregularity occurred after an average of 16.98 years from completion of treatment. More than 10 years posttreatment, approximately 81% of the maxillary anterior teeth and 88% of the mandibular anterior teeth showed clinically acceptable incisor alignment (<3.5 mm). Mandibular fixed retainers greatly aided in maintaining the stability of the mandibular incisor alignment. However, posttreatment changes in maxillary incisor irregularity did not appear to be influenced by the presence of a mandibular fixed retainer. When compared with longitudinal changes observed in untreated subjects, the increase in incisor irregularity resembled a pattern similar to the regression line of untreated subjects and seems to be entirely age related. Arch width and arch depth was consistently decreased after treatment, but the magnitude of change was minimal at about 1 mm. No associations were found between any of the cephalometric measurements and changes in incisor irregularities.
Conclusions:
Orthodontic treatment stability can be achieved and mandibular fixed retention appears to be a valuable contributor, especially in patients with further growth expected.
Keywords: Long-term stability, Posttreatment, Retention, Incisor irregularity, Mandibular fixed retainer
INTRODUCTION
Clinicians are aware that despite proper diagnosis and carefully rendered mechanotherapy, treatment results may not be stable over time and often undergo significant posttreatment changes. From the series of investigations on long-term stability of mandibular incisors conducted at the University of Washington, Little reported that the success of maintaining satisfactory alignment was less than 30% across various therapeutic approaches.1,2 Similarly, longitudinal studies of untreated subjects have shown that crowding increases over time and the rate of increase is greater during adolescence than in adulthood.3,4 A recent study reiterated that adolescents showed significantly greater posttreatment increases in mandibular incisor irregularity than adults.5 A number of studies indicate that changes in posttreatment crowding may be related to an individual's growth potential, but the degree of individual misalignment is unpredictable.1–7
Several studies concerning long-term stability of orthodontic treatment have been published, but limitations include sample selection biases, a short postretention follow-up period, and a lack of long-term stability of maxillary anterior tooth alignment. In addition, only a few studies have examined posttreatment changes in patients treated in the mixed dentition.2,8 Therefore, the purpose of this study was to answer the following questions:
At least 10 years after completing orthodontic treatment in the mixed and permanent dentitions, what percentage of patients present with clinically acceptable maxillary and mandibular incisor alignment (incisor irregularity < 3.5 mm)?
Does a mandibular fixed retainer aid in maintaining the stability of incisor alignment in the maxillary and mandibular arches?
Are changes in incisor irregularity after orthodontic treatment greater than those of untreated subjects?
To what extent are posttreatment changes in incisor alignment associated with changes in arch dimensions and cephalometric measurements?
MATERIALS AND METHODS
The long-term posttreatment sample consisted of 42 patients, obtained from a previously collected study sample at the Craniofacial Research Instrumentation Laboratory at the University of the Pacific, who were at least 10 years out of orthodontic treatment. The original study sample consisted of random samples of patient records drawn retrospectively from the private practices of three experienced orthodontic clinicians. From a total of 487 patients in the archived study sample, 216 patients who completed treatment at least 10 years prior to recall were eligible for the present study. An attempt was made to contact patients by mailing a letter requesting their participation in the study. Mailing addresses were obtained either from the original new patient forms or through Internet searches (http://www.peoplefinders.com).
No attempts were made to select patients based on type of treatment or type of retainer. We anticipated that some patients either lost their retainers, stopped wearing them, or had their fixed retainers removed, which would allow for comparing patients with and without long-term retention. Two hundred sixteen contact attempts were made, and 42 patients (12 males and 30 females) returned for a recall examination. For those who were examined, the mean time since orthodontic treatment was completed was 16.98 ± 5.3 years, with a range of 10.2 to 30.7 years. Twenty-nine patients had received mixed dentition treatment with or without fixed appliance therapy in the permanent dentition, and 13 patients had undergone single-phase treatment in the permanent dentition.
Early mixed dentition treatment included a maxillary 2 × 4 appliance, a headgear if Class II correction was required, and a mandibular lingual arch. A maxillary quad helix or hyrax expander was used to correct posterior crossbites. Following Phase 1 treatment, maxillary retainers were delivered and the mandibular lingual arches were continued. Once the permanent second molars erupted, new records were examined to determine whether further treatment was indicated. For some patients, a second phase of treatment was not recommended or not elected, and final retainers were delivered (Phase 1-only group).8 The patients who required and accepted further treatment underwent full-bonded fixed appliance therapy in the permanent dentition (two-phase group).
Comprehensive fixed appliance therapy was employed for patients who presented in the permanent dentition between 12 and 15 years of age (single-phase group). All three clinicians used full banded/bonded appliances with or without extractions but employed their own individualized treatment mechanics. All three clinicians routinely used removable retainers for maxillary retention (Hawley-type or vacuum-formed), but both removable and fixed retainers for the mandibular arch.
At the recall appointment, lateral cephalograms, facial and intraoral photographs, and study casts were obtained. In addition, informed consent was obtained and an interview questionnaire was completed. Lateral cephalograms could not be taken on two patients because they were pregnant. As a result, a total of 42 study casts and 40 lateral cephalograms were analyzed for the present study.
Changes in mandibular incisor irregularity in untreated subjects were collected as norms from data obtained from previous studies.9,10
This study was approved by the Institutional Review Board of the University of the Pacific (#13-05).
Measurement Methods
Study cast analysis
Physical study casts were scanned using a 3-D model scanner (3Shape Inc, Copenhagen, Denmark). For each time point, the irregularity index, arch width, and arch depth were measured on the maxillary and mandibular arches by using Ortho Analyzer 3-D software (3Shape) and changes between time points were calculated (Figure 1). Definitions of the measurements made on the study casts were as follows:
Figure 1.
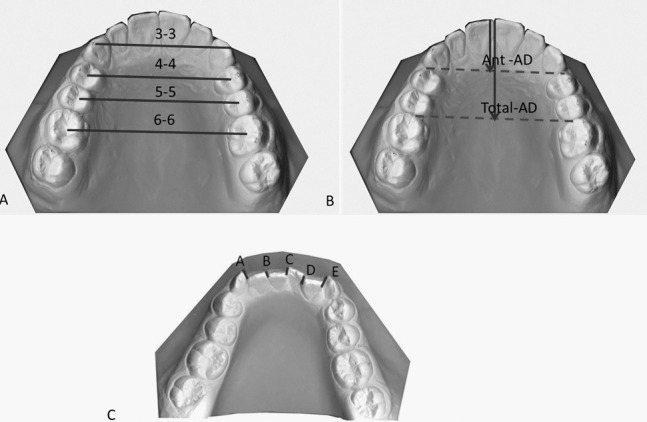
Dental arch measurements. (A) Arch width measurements. (B) Arch depth measurements. (C) Incisor irregularity = A + B + C + D + E.11
Irregularity index—summed displacement of the anatomic contact points of the anterior teeth11
Intercanine width—distance between cusp tips or estimated cusp tips in cases with wear facets
Interpremolar width—distance between centroids of the first and second premolars or the primary first and second molars
Intermolar width—distance between centroids of the first molars
Anterior arch depth—perpendicular distance between facial aspect of the central incisors at the embrasure to a line connecting the distal surfaces of the canines
Total arch depth—perpendicular distance from the facial aspect of the central incisors at the embrasure to a line connecting the mesial surfaces of the permanent first molars
Lateral Cephalometric Analysis
Lateral cephalometric landmarks were digitized independently by two or more judges. Outliers were excluded based on the landmark-specific envelopes of error. Average values were recorded in a numerical database in which the measurements for most standard cephalometric analyses were calculated by computer operations (Figure 2).
Figure 2.
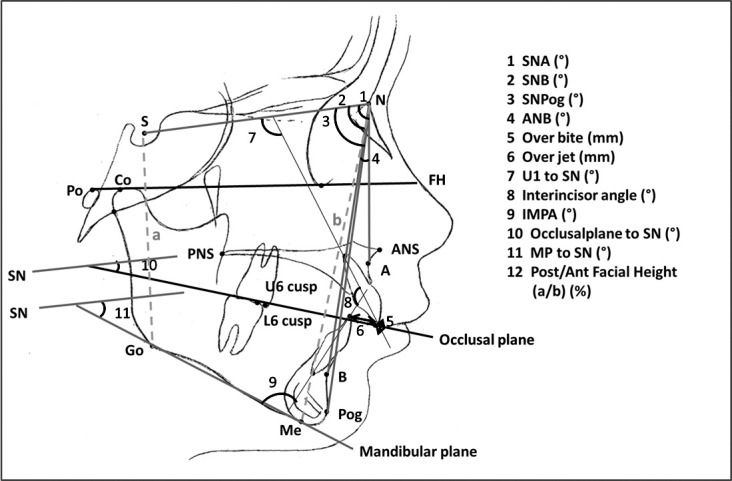
Cephalometric measurements.
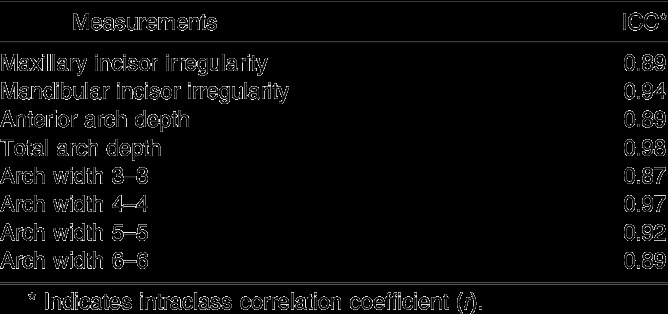
Statistical Analysis
Incisor irregularity and dental arch measurements on the study casts were measured by two judges, and the average values were used for statistical analysis. An intraclass correlation coefficient statistical analysis was used to assess interrater reliability for study cast measurements. Interrater reliability was excellent, ranging from 0.87 to 0.98 (Table 1). Descriptive statistics were generated to report the mean, standard deviation, range, and proportions. Statistics in this study include paired and unpaired t tests, analysis of variance (ANOVA) and covariance ANOVA, regression analysis, and Pearson correlation. Statistical values were computed using the SAS statistical package (version 9.1, SAS, Cary, NC).
Table 1.
Interrater Reliability
RESULTS
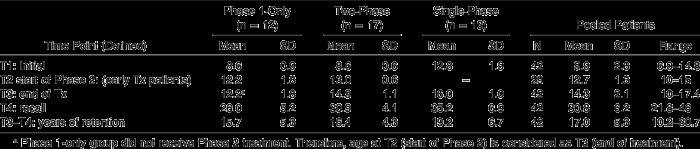
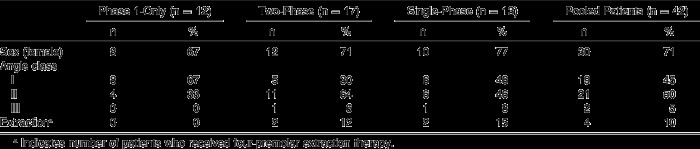
From a sample of 42 patients, three different treatment groups were identified: Phase 1-only group, two-phase group, single-phase group. The mean elapsed time between end of treatment and recall was 17.0 ± 5.3 years, and the mean age at recall was 30.8 ± 6.2 years (Table 2). The number of Class I and Class II malocclusions was similar for the pooled patients. Four patients had four premolars extracted (Table 3).
Table 2.
Mean Ages (y) at T1, T2, T3, T4 and Years of Retention for the Phase 1-Only, Two-Phase, and Single-Phase Groups
Table 3.
Sample Distribution by Sex, Angle Class, and Extraction Status
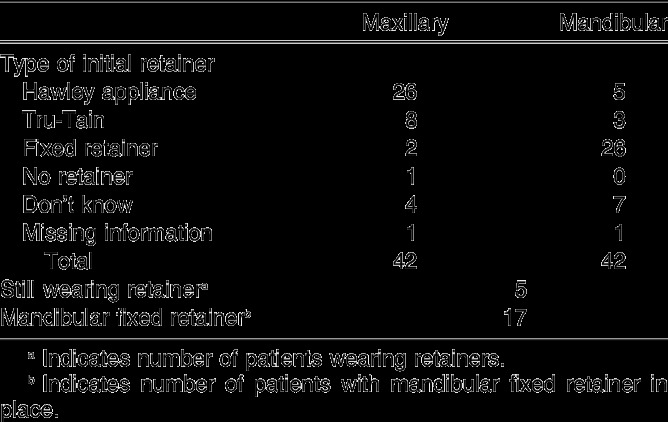
The extent and degree of retainer use was variable (Table 4). The maxillary Hawley appliance and mandibular fixed retainer were most widely used. Five patients were still wearing their removable retainers on a nightly basis at the time of recall. Of the 26 patients who received a mandibular fixed canine-to-canine retainer at the end of treatment, 17 still had them in place at recall: 11 from the two-phase group, 6 from the single-phase group, but none from the Phase 1-only group.
Table 4.
Retention Information From Survey Questionnaire and Treatment Chart
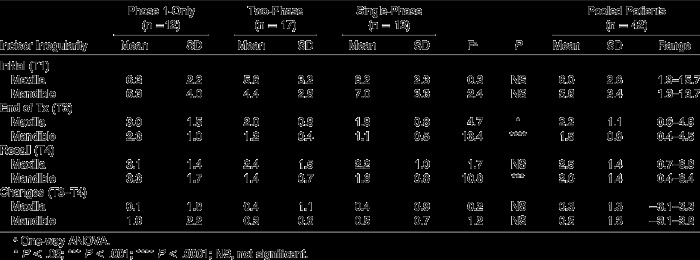
The pretreatment irregularity index ranged from 1.3 to 16 mm, with no statistical differences between the three groups (Table 5). At recall, the means of incisor irregularity for all patients were 2.5 ± 1.4 mm and 2.0 ± 1.4 mm for the maxillary and mandibular arches, respectively. The mean increases in incisor irregularity between T3 and T4 were minor at 0.3 ± 1.3 mm in the maxillary arch and 0.5 ± 1.3 mm in the mandibular arch.
Table 5.
Incisor Irregularity for Phase 1-Only, Two-Phase, and Single-Phase Treatment Groups
The one-way ANOVA and posthoc Bonferroni (Dunn) t test revealed that mandibular incisor irregularity for the Phase 1-only group at the end of treatment (T3) and recall (T4) were statistically different from those of both the two-phase and single-phase groups, wherein full fixed appliances were employed (at T3, P < .0001; at T4, P < .001). However, there were no statistically significant differences in mean changes in incisor irregularity for either arch between the end of treatment and recall (T3–T4) among the three groups (Table 5).
Figure 3 shows histograms of distributions of the incisor irregularity. At recall, eight patients presented with a greater than 3.5 mm irregularity index in the maxillary arch and five patients did so in the mandibular arch. Based on Little's clinically acceptable range criteria (<3.5 mm),1 stable incisor alignment was observed in 34 out of 42 cases (81%) of the maxillary arch and 37 out of 42 cases (88%) of the mandibular arch.
Figure 3.
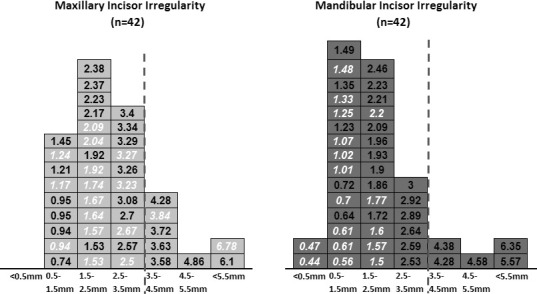
Distribution of incisor irregularity in the maxillary and mandibular arches at recall. Each cell in each histogram represents 1 patient and contains the incisor irregularity. The red vertical line indicates the clinically acceptable range for incisor irregularity (<3.5 mm). Values for patients with a mandibular fixed-retainer are shown in italics with white lettering.
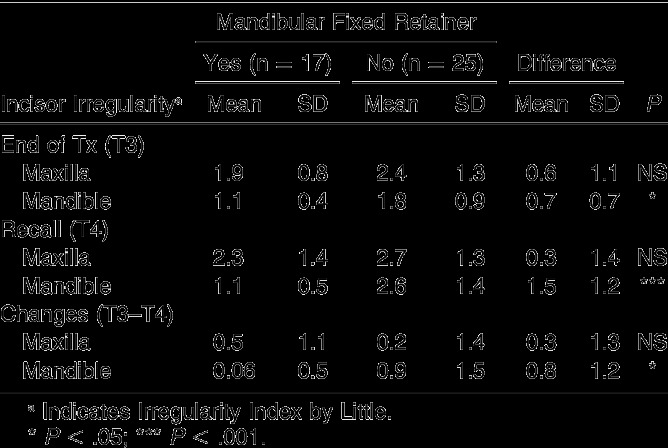
Effects of a Mandibular Fixed Retainer on Posttreatment Stability
As shown in Table 6, patients in the mandibular fixed retainer group showed almost no changes in mandibular incisor irregularity (0.06 ± 0.5 mm); a statistically significant difference was found when comparing the patients not having mandibular fixed retainers (0.9 ± 1.5 mm; P < .001). However, the mandibular fixed retainer had little effect on the stability of maxillary incisor alignment; no difference was found in maxillary incisor irregularity at recall between patients with or without mandibular fixed retention. A wide distribution in maxillary incisor irregularity was observed among patients who still had a mandibular fixed retainer in place (Figure 3).
Table 6.
Comparison of Incisor Irregularity Between Patients With and Without a Mandibular Fixed Retainer
Changes in Incisor Irregularity
Available data from previous studies9,10 were plotted, and regression equations relating age to mandibular incisor irregularity were calculated for untreated subjects (Figure 4). Figure 5 shows the plot comparing the means of incisor irregularity observed in the three treated groups against incisor irregularity observed in untreated subjects. For the Phase1-only group, an increase in incisor irregularity followed the regression line for untreated subjects and seemed to be entirely age related. The two-phase and single-phase groups with a mandibular fixed retainer showed no relapse. Without it, the changes in incisor irregularity during retention resembles the pattern of untreated subjects of the same ages. Thus, the mandibular fixed retainer reduced the magnitude and variability of relapse in incisor alignment.
Figure 4.
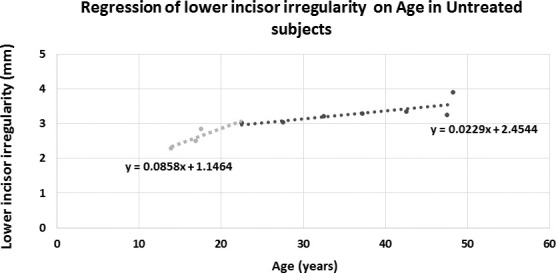
Regression of mandibular incisor irregularity by age of untreated subjects. The regression equation was calculated for untreated subjects based on previous studies.9,10 The curve is steeper for subjects 22 years and younger; this segment was used as a norm for the start and end of treatment. A flatter line appeared for subjects 22 years and older; this regression line was used as a norm for recall.
Figure 5.
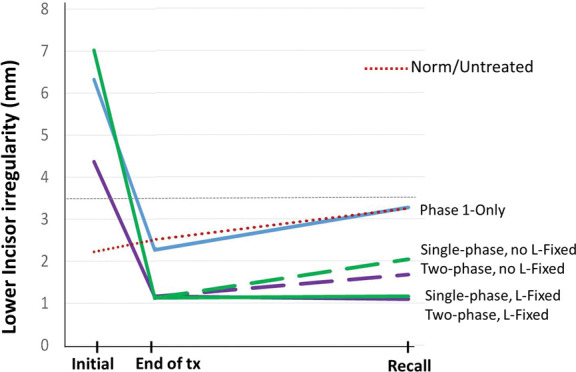
Plots comparing the mean incisor irregularities observed in the three treated groups and age-normed incisor irregularity observed in the untreated subjects. The red dotted line indicates age-normed incisor irregularity regression for the untreated subjects calculated in Figure 4. The horizontal broken line indicates the clinically acceptable incisor irregularity (3.5 mm).1
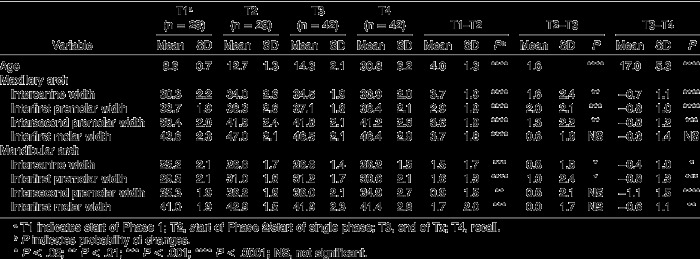
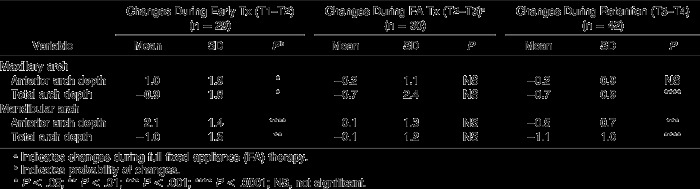
Changes in Maxillary and Mandibular Arch Dimension
During fixed appliance therapy (T2–T3), there was a statistically significant increase in all arch width measures, except for interfirst molar width. Mean posttreatment changes (T3–T4) were slight, but they were statistically significant—less than 1 mm of decrease in most arch width measures in both the maxillary and mandibular arches (Table 7). For maxillary and mandibular arch depth measurements, no statistically significant changes were found during fixed appliance therapy (Table 8). However, a statistically significant reduction was observed in all arch depth measurements during the retention period (T3–T4), except for maxillary anterior arch depth.
Table 7.
Changes in Arch Width (mm) During Treatment and Posttreatment
Table 8.
Changes in Arch Depth (mm) During Treatment (T1–T2 and T2–T3) and Posttreatment (T3–T4)
There was no statistically significant association found between arch dimensional changes and incisor irregularity.
Cephalometric Evaluation
Significant changes were observed in several cephalometric measurements: The SNPog angle increased by 0.8° and overjet decreased by 0.3 mm. The maxillary and mandibular incisors were uprighted, resulting in a statistically significant reduction in the interincisal angle (6.2° ± 5.6°, P < .0001). In addition, both the occlusal plane-SN and mandibular plane-SN angles were decreased by 1.1° ± 2.6° and 2.2° ± 1.8°, respectively (Table 9). However, none of the cephalometric measurements correlated with changes in maxillary and mandibular incisor irregularity.
Table 9.
Posttreatment Changes in Cephalometric measurements
DISCUSSION
It has been well established that a considerable amount of continuous change in the skeletal, dental, and soft tissues within the craniofacial region occurs even after general skeletal growth is completed.9,10,12,13 The literature indicates that long-term instability results from both orthodontic treatment and normal physiologic changes in the dentition and its surrounding tissues over time.1–13 It has been repeatedly stated that incisor irregularity of untreated subjects shows the greatest rate of increase during adolescence; the rates progressively decrease thereafter.4,9,10
The present study included patients who received Phase 1-only treatment. Their mandibular incisor irregularity decreased from an average of 6.4 ± 4.0 mm at T1 to 2.3 ± 1.0 mm at T2. Phase 1 treatment was completed at a mean age of 10.5 years, which implies that a considerable amount of growth was still expected. After Phase 1 treatment, the increase in incisor irregularity followed the regression line for untreated subjects of similar ages and seems to be entirely age related (Figure 5). The patients in both the two-phase and single-phase groups completed their treatment at a mean age of 14.3 years, and further growth was also anticipated after the completion of treatment. Without a mandibular fixed retainer, changes in incisor irregularity during retention resembled that of untreated subjects of the same ages (Figure 5).
The Phase 1-only group showed slightly greater incisor irregularity in both the maxillary and mandibular anterior teeth at recall. This could be explained by the fact that patients in the Phase 1-only group had more growth for a longer period of time after completion of treatment in the mixed dentition and that only two patients received a mandibular fixed retainer. In addition, none of them continued to wear retainers. Therefore, we believe that maintaining incisor alignment with a mandibular fixed retainer through the adolescent growth period would be advantageous.
Cephalometric measurements showed that the mandibular plane angle decreased by about 2° and the maxillary and mandibular incisors were further uprighted, which suggests that significant skeletal and dental changes can be anticipated after the completion of orthodontic treatment. However, no association was observed among changes in cephalometric measurements or incisor irregularity.
The present study showed relatively small posttreatment changes in incisor irregularity in both the maxillary and mandibular arches (<1 mm) despite further skeletal and dental changes after treatment. In contrast to some commonly cited studies,1,2 the small posttreatment changes observed indicate that orthodontic treatment may not be as inherently unstable as we expected.5–8,13
Several factors can be postulated to explain this relatively stable result. One factor could be the relatively small changes in arch width and depth (<1 mm) during treatment. This indicates that the clinicians did not increase arch perimeter by overexpanding or overproclining the teeth. Another factor could have been that 17 of the 42 patients in our sample still had their mandibular fixed retainers in place. In fact, patients in the mandibular fixed retainer group showed almost no changes in mandibular incisor irregularity. This finding indicates that mandibular fixed retainers aid in maintaining mandibular incisor alignment and should be kept in place as long as possible, not just until growth is completed. Although periodontal concerns surround mandibular fixed retainers, a recent study showed no negative effect on periodontal health from long-term application of a bonded mandibular canine-to-canine retainer.14 In the present study, four patients had their mandibular fixed retainers in place for more than 20 years and their periodontal health did not seem to be compromised (Figure 6).
Figure 6.
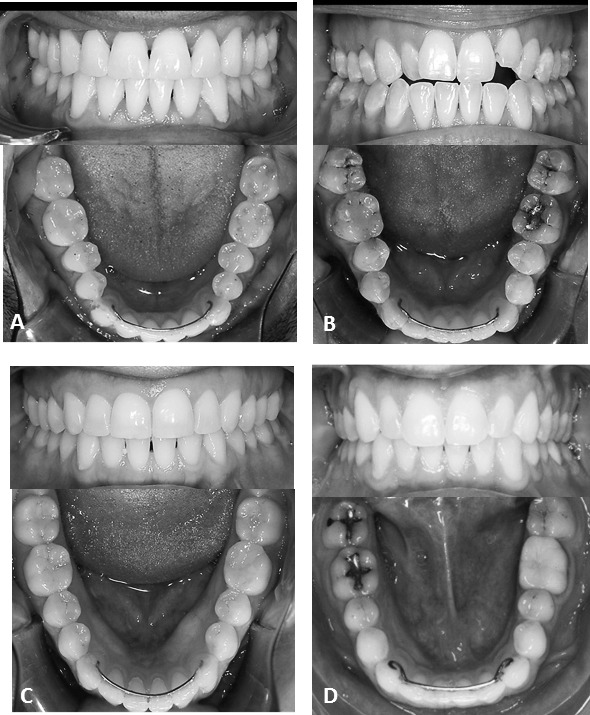
The four patients with long-term mandibular fixed retainers. (A), 41-year-old male patient, 26.3 years posttreatment; (B), 38-year-old female, 23 years posttreatment; (C), 36-year-old female, 22 years posttreatment; (D), 37-year-old male, 21 years posttreatment.
Instability after orthodontic treatment has multiple causes. In the short term, gingival and periodontal forces largely contribute to instability, but in the long term, the continued growth into adulthood is probably paramount.15 Therefore, it is critical that the patient be well informed about the nature of posttreatment changes in the dentition and motivated to cooperate in the retention phase to avoid relapse.
CONCLUSIONS
Minimal changes in maxillary and mandibular irregularity occurred more than 10 years after completion of treatment. Approximately 81% of the maxillary and 88% of the mandibular arches showed clinically acceptable, stable incisor alignment (<3.5 mm).
Mandibular fixed retainers aid in maintaining the stability of mandibular incisor alignment. However, posttreatment changes in maxillary incisor irregularity did not appear to be influenced by the presence of a mandibular fixed retainer.
The increase in incisor irregularity in treated patients resembles the regression line of untreated subjects and seems to be entirely age related.
Arch width and arch depth consistently decreased after treatment, but the magnitude was minimal at about 1 mm.
No associations were found between cephalometric measurements and changes in incisor irregularity.
ACKNOWLEDGMENT
This study was supported by a grant from Biomedical Research Award of the American Association of Orthodontists Foundation.
REFERENCES
- 1.Little RM, Wallen T, Riedel RA. Stability and relapse of mandibular anterior alignment: first premolar extraction cases treated by traditional edgewise orthodontics. Am J Orthod Dentofacial Orthop. 1981;80:349–365. doi: 10.1016/0002-9416(81)90171-8. [DOI] [PubMed] [Google Scholar]
- 2.Little RM. Stability and relapse of mandibular anterior alignment: University of Washington studies. Semin Orthod. 1999;5:191–204. doi: 10.1016/s1073-8746(99)80010-3. [DOI] [PubMed] [Google Scholar]
- 3.Sinclair P, Little R. Maturation of untreated normal occlusions. Am J Orthod Dentofacial Orthop. 1983;83;:114–123. doi: 10.1016/s0002-9416(83)90296-8. [DOI] [PubMed] [Google Scholar]
- 4.Eslambolchi S, Woodside DG, Rossouw PE. A descriptive study of mandibular incisor alignment in untreated subjects. Am J Orthod Dentofacial Orthop. 2008;133:343–353. doi: 10.1016/j.ajodo.2006.04.038. [DOI] [PubMed] [Google Scholar]
- 5.Park H, Boley JC, Alexander RA, Buschang PH. Age-related long-term posttreatment occlusal and arch changes. Angle Orthod. 2010;80:247–253. doi: 10.2319/042109-226.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glenn G, Sinclair PM, Alexander RG. Nonextraction orthodontic therapy: posttreatment dental and skeletal stability. Am J Orthod Dentofacial Orthop. 1987;92:321–328. doi: 10.1016/0889-5406(87)90333-7. [DOI] [PubMed] [Google Scholar]
- 7.Myser SA, Campbell PM, Boley J, Buschang PH. Long-term stability: postretention changes of the mandibular anterior teeth. Am J Orthod Dentofacial Orthop. 2013;144:420–429. doi: 10.1016/j.ajodo.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Dugoni SA, Lee JS, Varela J, Dugoni AA. Early mixed dentition treatment: postretention evaluation of stability and relapse. Angle Orthod. 1995;65:311–320. doi: 10.1043/0003-3219(1995)065<0311:EMDTPE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Carter GA, McNamara JA. Longitudinal dental arch changes in adults. Am J Orthod Dentofacial Orthop. 1998;114:88–99. doi: 10.1016/s0889-5406(98)70243-4. [DOI] [PubMed] [Google Scholar]
- 10.Buschang PH, Shulman JD. Incisor crowding in untreated persons 15–50 years of age: United States, 1988–1994. Angle Orthod. 2003;73:502–508. doi: 10.1043/0003-3219(2003)073<0502:ICIUPY>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Little RM. The irregularity index: a quantitative score for mandibular anterior alignment. Am J Orthod. 1975;68:554–563. doi: 10.1016/0002-9416(75)90086-x. [DOI] [PubMed] [Google Scholar]
- 12.Sinclair P, Little R. Dentofacial maturation of untreated normals. Am J Orthod Dentofacial Orthop. 1985;88:146–156. doi: 10.1016/0002-9416(85)90239-8. [DOI] [PubMed] [Google Scholar]
- 13.Driscoll-Gilliland J, Buschang PH, Behrents RG. An evaluation of growth and stability in untreated and treated subjects. Am J Orthod Dentofacial Orthop. 2001;120:588–597. doi: 10.1067/mod.2001.118778. [DOI] [PubMed] [Google Scholar]
- 14.Booth FA, Edelman JM, Proffit WR. Twenty-year follow-up of patients with permanently bonded mandibular canine-to-canine retainers. Am J Orthod Dentofacial Orthop. 2008;133:70–76. doi: 10.1016/j.ajodo.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 15.Melrose C, Millett DT. Toward a perspective on orthodontic retention? Am J Orthod Dentofacial Orthop. 1998;113:507–513. doi: 10.1016/s0889-5406(98)70261-6. [DOI] [PubMed] [Google Scholar]