Abstract
Purpose:
To compare the bleb morphology by Anterior Segment Optical Coherence Tomography (ASOCT) and clinical outcome after Phacotrabeculectomy with either mitomycin C or Ologen implant.
Methods:
In a prospective interventional active controlled study, 93 patients aged 18 years and above underwent phacotrabeculectomy with either mitomycin C (53 eyes) or ologen implant (40 eyes), followed up for 12 months. The primary outcome measure was to note the evolution of bleb morphology by ASOCT in the two groups over 12 months. Secondary outcome measures were mean IOP, reduction in the need for anti-glaucoma medications, and complications seen in the two groups.
Results:
All parameters in the two groups were comparable preoperatively (P>0.05). Best corrected visual acuity at 12 months was 0.38±0.27 in mitomycin group and 0.31±0.23 in ologen group (P=0.151). Post-operative IOP at 12 months was 14.09±3.1mmHg (95%CI 13.22-14.97) in mitomycin group, and 13.25±2.5 mmHg (95%CI 12.40-14.30) in ologen group (P=0.254).The mean number of medications was 0.36±0.68 in mitomycin group and 0.38+/-0.70 in ologen group at 12 months (P=0.91). Overall success was achieved in 98.1 % of patients in mitomycin group and 90 % of patients in ologen group at 12 months. No major sight-threatening complications were noted in any group. AS-OCT imaging at 12 months showed multiform reflectivity with multiple large cystic spaces in both groups, with good IOP control.
Conclusion:
Phacotrabeculectomy using Mitomycin C and Ologen implant resulted in similar morphologic and functioning blebs at one year with comparable efficacy in controlling intraocular pressure.
Keywords: AS-OCT, mitomycin C, Ologen, phacotrabeculectomy
The outcome of trabeculectomy depends on the formation of the functioning filtering bleb that determines the level of intraocular pressure and the long term success of surgery.[1] Bleb morphology is an essential clinical parameter determining bleb function, indicator of IOP control, and predictor of bleb-related complications.[2,3]
Wound healing associated with excess fibrosis and scar formation is an important reason for failure of trabeculectomy. Antifibrotic agents like mitomycin-C (MMC) and 5-fluorouracil (5FU) have been used for wound modulation to improve the success of the filtering surgery.[4,5] However, these agents are associated with complications such as leakage, infection, hypotony, and endophthalmitis.[5,6] Tissue-engineered biodegradable collagen glycosaminoglycan co-polymer matrix implant was created as an alternative which decreases postoperative scarring. Its porous structure allows conjunctival fibroblasts and myofibroblasts to grow into the pores and secrete connective tissue in the form of a loose matrix reducing scar formation and wound contraction. After implantation, the device usually completely degrades within 90–180 days.[7,8]
Early bleb morphological features correlate with the outcome of trabeculectomy and may help to identify patients with an increased risk of failure.[9] Bleb morphology and function can be assessed at the slit lamp using Moorfield’s Bleb Grading System (MBGS),[7] which evaluates bleb area, height, and vascularity. Clinical evaluation and grading have been found to correlate with bleb imaging with anterior segment optical coherence tomography (ASOCT).[10] ASOCT is a noninvasive technique which shows cross-sectional images of the bleb morphology, which may increase understanding of the healing process and help differentiate functional and non-functional blebs.[1,3,11,12,13,14,15,16] There are studies from India that describe the bleb morphology using ASOCT following trabeculectomy with MMC[1] but no comparative study of the imaging of blebs after trabeculectomy or phacotrabeculectomy done with MMC and collagen matrix. This study was planned to study the evolution of the morphology of the filtering bleb by ASOCT and to compare the clinical outcomes in patients undergoing phacotrabeculectomy with either MMC or collagen matrix (Ologen) followed up for a period of one year.
Methods
This was an open label, non-randomized, prospective interventional active control study conducted between December 2016 and December 2018 after approval from the institutional ethics committee. The study adhered to the tenets of the Declaration of Helsinki.
Sample size calculation
The primary objective of the study was to assess the difference of bleb morphology between the two groups. In a study by Boey et al.,[17] the mean bleb height in patients undergoing phacotrabeculectomy with Ologen group at 90 days was 0.74 + 0.2 mm. Taking this as reference to detect a 20% difference (20/100 × 0.74 = 0.148 mm) compared to another group, sample size calculation for difference of means between two groups was as follows.
Sample size = n = (Zα/2 + Zα)2 * 2 *ϭ2/d2
Where Zα/2 is the critical value of the normal distribution at α/2 (e.g., for a confidence level of 95%, a is 0.05 and the critical value is 1.96), Zβ is the critical value of the normal distribution at β (e.g., for a power of 80%, β is 0.2, and the critical value is 0.84), σ2(0.74) is the population variance, and d (0.148) is the difference we would like to detect.
The calculated sample size was 30 in each group, for 80% power, and significance level of 0.05. As this was a follow-up study, considering a dropout rate of 20%, the calculated sample size should satisfy 80% of the final sample size. Hence, sample size of each group was 30 × 100/80 = 37.5 = 38.
The procedure and cost of the two procedures were explained to the patients. Commercially available MMC and Collagen matrix implant were used for the surgeries. This study was not funded from any source. Hence, patients made a choice of the procedure depending on their economic capability. The authors have no financial interest in either of the adjunctive agent used.
Patients included in the study were ≥ 40 years of age, having primary open-angle glaucoma (POAG) or primary angle-closure glaucoma (PACG) not controlled with medications and visually significant cataract. Patients with a single functioning eye, history of previous intraocular surgery, acute angle-closure glaucoma, secondary glaucoma, coexisting retinal or corneal pathology were excluded.
Informed consent for surgery was taken from all patients after explaining the risks and benefits of the two procedures. All patients underwent the following examinations including best-corrected distance visual acuity (BCVA) by LogMAR chart, slit lamp examination, indentation gonioscopy by Sussman four mirror lens, Goldmann applanation tonometry, standard white on white automated perimetry (Humphrey 30-2 test), stereoscopic disc and fundus evaluation.
Single site phacotrabeculectomy was performed with either MMC or Collagen matrix (Ologen, Aeon Astron Europe B. V. The Netherlands) by two glaucoma surgeons (VC, VKS) under peribulbar anesthesia. A fornix-based conjunctival flap was dissected at the superior limbus. In the MMC group, sponges soaked in 0.2 mg/ml of MMC were applied for 2 min to the surgical site and thoroughly washed with Ringer’s lactate. A 4 × 4 mm partial-thickness triangular scleral flap was fashioned. The anterior chamber was entered under the scleral flap and phacoemulsification completed. A block of deep sclera was excised using Kelly’s punch followed by peripheral iridectomy. The scleral flap was sutured using three simple interrupted 10-0 monofilament nylon sutures. In the collagen matrix group, apex suture was left a little loose, and collagen matrix implant of 6 × 2 mm was placed over the apex suture. Conjunctiva was closed using absorbable sutures. All patients were given standard antibiotic and steroid regimen postoperatively. Postoperative visits were scheduled at day one, one week, one month, 3, 6, 9, and 12 months. BCVA, IOP, clinical characteristics of the bleb using MBGS, bleb imaging, complications, and need for additional anti-glaucoma medications were assessed at every follow-up visit.
The primary outcome measure was to note the evolution of bleb morphology by ASOCT in the two groups over 12 months. Secondary outcome measures were mean IOP at 12 months, reduction in the need for anti-glaucoma medications, and complications in the two groups. Complete success was defined as an IOP >6 mmHg and ≤18 mmHg, without any anti-glaucoma medications; qualified success was defined as IOP ≤18 mmHg with maximum of two additional anti-glaucoma medications. Failure was defined as need for needling with the use of antimetabolite or any re-surgery.
Clinically the blebs were evaluated and scored using MBGS for area, height, and vascularity. Slit-lamp images were compared with reference photographs. The central area over the scleral flap and maximum area of bleb visible were given a score of 1-5, height (flat, low, moderately elevated or maximally elevated, scored as 1-4), vascularity (central area, peripheral extent of the bleb and surrounding non-bleb conjunctiva were assessed) was graded from 1-5.
Imaging was done using ASOCT (Carl Zeiss, Meditec, USA, Cirrus HD-OCT Model 500). The patient was asked to look down, upper lid gently retracted to visualize the bleb to obtain the images.[1,14,18] Standard ASOCT images were obtained for each bleb through the site of maximal bleb elevation, a radial section perpendicular to the limbus, and a section tangential to the limbus as described by earlier investigators.[1,14] Multiple images were taken, and the best image was used for evaluation.
The blebs were evaluated for wall reflectivity and hyporeflective spaces in the subconjunctival space. The bleb wall reflectivity was taken as uniform when hyperreflective wall and no hyporeflective spaces were visible in the bleb wall or subconjunctival area. Reflectivity was taken as multiform when multiple hyporeflective areas were seen in the bleb wall and the subconjunctival space with the formation of multiple layers. These could be small or large hyporeflective spaces suggestive of multiple small and large fluid-filled cysts.[1,12,16]
Statistical analysis
The data was analyzed using Statistical Package for the Social Sciences (SPSS) version 20 (IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp). Data was expressed as Mean ± SD (95% confidence intervals), numbers (percentages), and median (interquartile range). The Chi-square test and Fisher’s Exact test were used to assess the association between categorical variables. Continuous variables were compared using the Student’s t-test (for normally distributed data). The level of significance in the study was P value < 0.05.
Results
100 patients were included in the study. 56 patients underwent phacotrabeculectomy with MMC (MMC group) and 44 underwent phacotrabeculectomy with collagen matrix implant, Ologen (OLO group). Three patients in the MMC group and four patients in OLO group were lost to follow up after 6 months; hence, they were excluded from the outcome analysis. 93 patients were included in the analysis, 53 in the MMC group and 40 in the OLO group. Patients in the two treatment groups did not differ significantly in age, gender, preoperative vision and intraocular pressure, type of glaucoma, mean number of medications, and visual field indices [Table 1].
Table 1.
Preoperative characteristics of patients
| MMC | Ologen | P | |
|---|---|---|---|
| Age (years) | 64.26 | 64.03 | 0.898 |
| Gender (M/F) | 38/15 | 29/11 | 0.932 |
| BCVA (mean +-SD) | 0.62 (0.37) | 0.54 (0.35) | 0.298 |
| POAG | |||
| Type of glaucoma | 45 | 33 | 0.754 |
| PACG | 8 | 7 | 0.865 |
| IOP (mean±SD) | 22.00 (8.15) | 19.65 (6.07) | 0.13 |
| MD (median±interquartile range) | -14.15 (21.24) | -8.86 (9.01) | 0.08 |
| PSD (median±interquartile range) | 5.31 (4.75) | 5.69 (4.16) | 0.38 |
MMC: Mitomycin C, BCVA: Best-corrected visual acuity, POAG: Primary open angle glaucoma, PACG: Primary angle closure glaucoma, IOP: Intraocular pressure, MD: Mean deviation, PSD: Pattern standard deviation
Slit-lamp evaluation of blebs was done using the MBGS. The mean bleb area in the MMC group at one month was significantly more than the OLO group. The mean bleb height score was significantly more in the OLO group as compared to the MMC group up to 6 months; collagen matrix was absorbed in 35 (86%) patients by six months indicated by decrease in height of the bleb by MBGS and imaging. The vascularity scores were clinically higher in the collagen implant group than MMC group at first month, and remained higher in patients who developed bleb fibrosis in the early postoperative period. The area, height, and vascularity differed in the initial postoperative period but did not differ on an intragroup and intergroup basis at the end of 12 months [Table 2].
Table 2.
Changes in the mean bleb height, area, and vascularity on MBGS
| Parameters | MMC | Ologen | P |
|---|---|---|---|
| Mean bleb height (Mean±S. D) (mm) | |||
| 1 month | 1.26±0.44 | 2.98±0.733 | 0.0001 |
| 3 months | 1.47±0.50 | 2.40±0.672 | 0.0001 |
| 6 months | 1.75±0.51 | 2.08±0.572 | 0.006 |
| 12 months | 1.79±0.53 | 1.78±0.423 | 0.865 |
| Mean bleb area (mean±S. D)(mm2) | |||
| 1 month | 2.77±0.891 | 2.30±0.791 | 0.009 |
| 3 months | 3.08±0.730 | 3.03±0.768 | 0.747 |
| 6 months | 3.34±0.678 | 3.40±0.632 | 0.663 |
| 12 months | 3.58±0.745 | 3.70±0.723 | 0.457 |
| Mean vascularity score (Mean±S. D) | |||
| 1 month | 2.83±0.727 | 3.13±0.966 | 0.096 |
| 3 months | 2.43±0.605 | 2.43±0.675 | 0.946 |
| 6 months | 2.04±0.619 | 2.13±0.563 | 0.486 |
| 12 months | 1.64±0.653 | 1.78±0.480 | 0.279 |
MMC: Mitomycin C
Fig. 1 shows the ASOCT images of the filtering blebs. At one month, the bleb wall was hyperreflective in both groups, more in collagen matrix blebs. Nearly half of the cases in both groups showed no hyporeflective areas, while half showed small scattered hyporeflective areas (microcysts) in the bleb wall and subconjunctival space, indicative of early multiform blebs, more prominent in the OLO group. The number of hyporeflective spaces increased in number and size in the 3, 6, and 12-month visits in both groups, suggestive of the evolution of multiform appearance. By 12 months, the reflectivity of the wall was similar in the two groups with multiple large hyporerflective spaces in the subconjunctival space.
Figure 1.
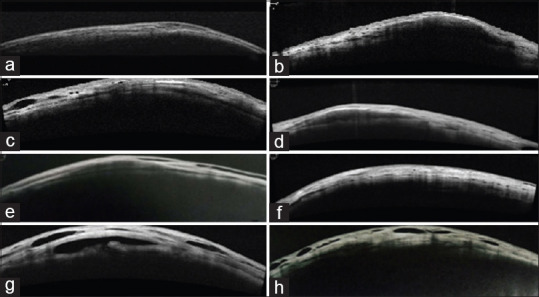
ASOCT images of the bleb. (a) MMC bleb, 1 month, (b) Ologen bleb, 1 month, (c) MMC bleb, 3 months (d) Ologen bleb, 3 months, (e) MMC bleb, 6 months, (f) Ologen bleb, 6 months, (g) MMC bleb, 12 months, (h) Ologen bleb, 12 months. Small hyporeflective spaces and early multiform appearance seen at 1 month, prominently in Ologen blebs. At 3 and 6 months, the cystic spaces have increased in size and number and by 12 months multiple large spaces and multiform reflectivity seen in both the groups
At one month, 43% of patients in the MMC group and 52% in the OLO group showed multiform bleb reflectivity. By 12 months, 92% of patients in the MMC group and 90% in the OLO group developed a multiform reflectivity and multiple large cystic spaces (P = 0.676 Student’s t-test).
Fibrosed bleb revealed very high reflectivity of the wall, with no hyporeflective areas or channels in the wall and subconjunctival space, with a large underlying area of no reflectivity [Fig. 2].
Figure 2.
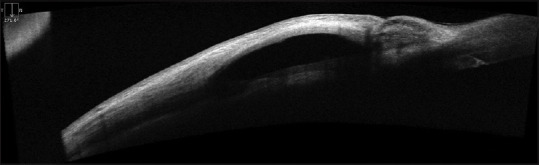
ASOCT image of a fibrotic bleb showing hyperreflective wall with no hyporeflective areas in the bleb wall and subconjunctival spaces and an underlying area of non-reflectivity
Postoperative vision improved in both groups and was statistically similar in the two groups at 12 months. The postoperative IOP was lower than the preoperative level at all time points with no intergroup difference (P > 0.05) [Table 3].
Table 3.
Comparison of mean postoperative IOP between the two groups
| IOP (mmHg) | Mean | Std. Deviation | 95% Confidence interval | P | |
|---|---|---|---|---|---|
| 1 month | |||||
| MMC | 14.17 | 4.759 | 12.86-15.48 | 0.977 | |
| OLOGEN | 14.20 | 5.065 | 12.58-15.82 | ||
| 3 months | |||||
| MMC | 13.34 | 4.009 | 12.23-14.44 | 0.691 | |
| OLOGEN | 13.05 | 2.572 | 12.23-13.87 | ||
| 6 months | |||||
| MMC | 13.70 | 3.360 | 12.77-14.62 | 0.857 | |
| OLOGEN | 13.58 | 3.096 | 12.58-14.57 | ||
| 1 year | |||||
| MMC | 14.09 | 3.182 | 13.22-14.97 | 0.254 | |
| OLOGEN | 13.35 | 2.983 | 12.40-14.30 |
MMC: Mitomycin C
The mean number of patients requiring additional medication was higher in the OLO group in the first month; because of early scarring and loss of IOP control, at 6 and 12 month visits, a marginally higher number of patients in the MMC group required medications for IOP control. The mean number of anti-glaucoma medications were significantly reduced in both groups, from a preoperative level of 2.5 ± 0.63 to 0.36 ± 0.68 (P = 0.00) in the MMC group and 2.7 ± 0.63 to 0.38 ± 0.70 (P = 0.00) in the OLO group, with no intergroup difference at 12 months (P = 0.91).
Few postoperative complications were seen in both groups. Hypotony was seen in two patients in each group. Three cases resolved with conservative management, and one case in the MMC group required an additional suture of the scleral flap. Bleb fibrosis was seen in one patient in the MMC group at 3 weeks, and four patients in the OLO group between 3–4 weeks after surgery. All patients required needling of the bleb along with 5 Fluorouracil injection. Two patients in OLO group and one patient in MMC group required addition of maximum of two anti-glaucoma medications. One patient in the MMC group developed choroidal detachment, which resolved with conservative management. However, using the Chi-square test, there was no statistically significant difference in the occurrence of the complications between the two groups.
Complete success was achieved in 75.4% of patients in the MMC group and 67.5% in the OLO group at 12 months (P = 0.745). Qualified success was achieved in 22.7% of patients in MMC group and 22.5% in the OLO group at 12 months. Failure was seen in 1.8% patient in MMC group and 10% patients in OLO group.
None of the patients in either group required a repeat trabeculectomy in the given follow-up period. No case of blebitis or endophthalmitis was seen in our study.
Discussion
In this open-label, case-control study, we looked at the evolution of morphology of the filtering bleb by ASOCT following phacotrabeculectomy augmented with mitomycin C and collagen matrix implant (Ologen). The bleb morphology, IOP, and mean medications were comparable in the two groups at the end point.
We found apparent difference in the height, area, vascularity of the blebs in the two groups in the early postoperative period. The bleb height was higher in the collagen matrix group at first and third postoperative month, which reduced over the next 3 months indicative of absorption of the collagen matrix implant. The increased height in the early postoperative period was attributed to the physical presence of the collagen matrix. The eyes in the MMC group had a lower height as the aqueous pockets were seen to be formed 6 months onwards. 12 month imaging showed multiple hyporeflective aqueous filled spaces in both groups; the MMC group showed a clear aqueous lake formation which was not so evident in the collagen implant blebs.
The vascularity was greater in the OLO group, while bleb area was more in the MMC group in the first postoperative month. The increased vascularity seen in the OLO group progressed to increased fibrotic response and scarring of the blebs in 4 patients. One patient in the MMC group developed scarring of bleb. Although this difference was clinically significant, there was no statistical difference by Chi-square test. All patients responded to needling and half of them required additional antiglaucoma medications to achieve IOP control. The reason for increased fibrotic response in the OLO group could be explained as follows. Collagen matrix provides a scaffold for growth of fibroblasts through its pores, causing remodeling of the tissue and reducing scar formation. On the contrary mitomycin C inhibits fibroblast proliferation. Ologen functions as a wound modulator and does not have any antifibrotic properties to counter the scarring response.[7,19] Younger age and ethnicity have been known to increase fibrosis in the filtering blebs. [19,20] Mitomycin blebs showed a better function in the early postoperative period than the collagen implant blebs in terms of fibrosis, but both showed a similar morphology and IOP control over a 12 month period.
The mean number of patients requiring additional medication was higher in the OLO group in the first month because of scarring and loss of IOP control. At 6 and 12 months, a marginally higher number of patients in the MMC group required medications for IOP control. Bleb needling also reduced the need for medication. This could explain the mean medications not being significantly different despite the large difference in the number of eyes deemed as failure in the OLO group.
Earlier studies have shown thickened bleb wall with discrete hyporeflective spaces[13] and bleb walls with multiform reflectivity and multiple internal layers[1] are associated with increased success of filtering blebs. We found that more than 90% of eyes in both groups showed multiform reflectivity and hyporeflective spaces, suggestive of functioning blebs.
The bleb area characteristics in our study were found to be similar to those observed by Cillino et al.[13] and Boey et al.[15] We found a higher bleb height score in the OLO group up to 6 months, while Cillino et al.[13] found mean bleb height score higher in Ologen group at 3 months, maintained higher till 24 months. In contrast, Boey et al.[17] found that the bleb height score was lower in the Ologen group at the end of 90 days.
We found vascularity scores were higher in OLO group at 1 month, and similar results were seen by Boey et al.,[17] while Cillino et al.[13] found no intergroup difference over time.
We found equal control of IOP at all time points with no inter group difference at 12 months which was similar to the results by Wlaz et al.[21] In contrast, Narayanaswamy et al.[22] found a greater percentage reduction of IOP in MMC group than in Ologen group at one year; however, IOP decrease at one year was not statistically different in the two groups, while Boey et al.[17] reported greater mean IOP reduction in MMC group as compared to OLO group at 90 days. There was no intergroup difference in the mean number of medications at end point in our study, which was similar to that found by other authors.[13,21]
We achieved qualified success of 98.1% in the MMC group and 90% in the Ologen group at 12 months, comparable to the results seen by Wlaz et al.[21]
The postoperative complications in our study were similar to those seen by Cillino et al.[13] We performed needling in one patient of MMC group and four patients of OLO group. Narayanaswamy et al.[22] also noted that Ologen group required more frequent needling than in MMC group (P = 0.003). Cillino et al.[13] reported the need for needling of encapsulated blebs in MMC and Ologen groups equally.
None of the patients in our study developed any Ologen specific side effects like allergy, translocation or expulsion of the implant, as reported by other authors.[13,23,24]
The limitation of our study is that this was not a randomized controlled trial, although it was a prospective active controlled study. A randomized study would eliminate a selection bias. We followed the patients for one year, but this is a short time period to note the long term IOP control and complications like thin avascular cystic blebs seen with the use of MMC, which could potentially lead to additional complications. Seven patients were lost to follow up after 6 months; this was a limitation of our study.
Conclusion
In conclusion, we found that phacotrabeculectomy with MMC or Ologen resulted in multiform blebs with multiple internal layers and hyporeflective spaces at 12 months. Both groups resulted in similar control of intraocular pressure at one year. Complications were similar in the two groups, but collagen matrix (Ologen) blebs were found to be more prone to scarring.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Khamar M, Soni S, Mehta S, Srivastava S, Vasavada V. Morphology of functioning trabeculectomy blebs using anterior segment optical coherence tomography. Indian J Ophthalmol. 2014;62:711. doi: 10.4103/0301-4738.136227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Narita A, Morizane Y, Miyake T, Seguchi J, Baba T, Shiraga F. Characteristics of successful filtering blebs at 1 year after trabeculectomy using swept-source three-dimensional anterior segment optical coherence tomography. Jpn J Ophthalmol. 2017;61:253–9. doi: 10.1007/s10384-017-0504-2. [DOI] [PubMed] [Google Scholar]
- 3.Golez E, Latina M. The use of anterior segment imaging after trabeculectomy. Semin Ophthalmol. 2012;27:155–9. doi: 10.3109/08820538.2012.707275. [DOI] [PubMed] [Google Scholar]
- 4.Lin ZJ, Li Y, Cheng JW, Lu XH. Intraoperative mitomycin C versus intraoperative 5-fluorouracil for trabeculectomy:A systematic review and meta-analysis. J Ocul Pharmacol Ther. 2012;28:166–73. doi: 10.1089/jop.2011.0117. [DOI] [PubMed] [Google Scholar]
- 5.Vijaya L, Manish P, Ronnie G, Shantha B. Management of complications in glaucoma surgery. Indian J Ophthalmol. 2011;59(Suppl(Suppl 1)):S131–40. doi: 10.4103/0301-4738.73689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yoon PS, Singh K. Update on antifibrotic use in glaucoma surgery, including use in trabeculectomy and glaucoma drainage implants and combined cataract and glaucoma surgery. Curr Opin Ophthalmol. 2004;15:141–6. doi: 10.1097/00055735-200404000-00015. [DOI] [PubMed] [Google Scholar]
- 7.He M, Wang W, Zhang X, Huang W. Ologen implant versus mitomycin C for trabeculectomy:A systematic review and meta-analysis. PLoS One. 2014;9:e85782. doi: 10.1371/journal.pone.0085782. doi:10.1371/journal.pone. 0085782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zelefsky JR, Hsu WC, Ritch R. Biodegradable collagen matrix implant for trabeculectomy. Expert Rev Ophthalmol. 2008;3:613–7. [Google Scholar]
- 9.Sacu S, Rainer G, Findl O, Georgopoulos M, Vass C. Correlation between the early morphological appearance of filtering blebs and outcome of trabeculectomy with mitomycin C. J Glaucoma. 2003;12:430–5. doi: 10.1097/00061198-200310000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Wells AP, Crowston JG, Marks J. A pilot study of a system forgrading drainage blebs after glaucoma surgery. J Glaucoma. 2004;13:454–60. doi: 10.1097/00061198-200412000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Ciancaglini M, Carpineto P, Agnifili L, Nubile M, Lanzini M, Fasanella V, et al. Filtering bleb functionality:A clinical, anterior segment optical coherence tomography and in vivo confocal microscopy study. J Glaucoma. 2008;17:308–17. doi: 10.1097/IJG.0b013e31815c3a19. [DOI] [PubMed] [Google Scholar]
- 12.Mastropasqua R, Fasanella V, Agnifili L, Curcio C, Ciancaglini M, Mastropasqua L. Anterior segment optical coherence tomography imaging of conjunctival filtering blebs after glaucoma surgery. Biomed Res Int. 2014;2014:610623. doi: 10.1155/2014/610623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cillino S, Di Pace F, Cillino G, Casuccio A. Biodegradable collagen matrix implant vs mitomycin-C as an adjuvant in trabeculectomy:A 24-month, randomized clinical trial. Eye. 2011;25:1598–606. doi: 10.1038/eye.2011.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cillino S, Casuccio A, Di Pace F, Cagini C, Ferraro LL, Cillino G. Biodegradable collagen matrix implant versus mitomycin-C in trabeculectomy:Five-year follow-up. BMC Ophthalmol. 2016;16:24. doi: 10.1186/s12886-016-0198-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh M, Chew PT, Friedman DS, Nolan WP, See JL, Smith SD, et al. Imaging of trabeculectomy blebs using anterior segment optical coherence tomography. Ophthalmology. 2007;114:47–53. doi: 10.1016/j.ophtha.2006.05.078. [DOI] [PubMed] [Google Scholar]
- 16.Singh M, See JLS, Aquino MC, Thean LSY, Chew PTK. High-definition imaging of trabeculectomy blebs using spectral domain optical coherence tomography adapted for the anterior segment. Clin Exp Ophthalmol. 2009;37:345–51. doi: 10.1111/j.1442-9071.2009.02066.x. [DOI] [PubMed] [Google Scholar]
- 17.Boey PY, Narayanaswamy A, Zheng C, Perera SA, Htoon HM, Tun TA, et al. Imaging of blebs after phacotrabeculectomy with Ologen collagen matrix implants. Br J Ophthalmol. 2011;95:340–4. doi: 10.1136/bjo.2009.177758. [DOI] [PubMed] [Google Scholar]
- 18.Fakhraie G, Kohansal S, Eslami Y, Jabbarvand M, Zarei R, Rafizadeh SM, et al. Correlation between filtering bleb clinical morphology, anterior segment optical coherence tomography findings, and intraocular pressure. Iran J Ophthalmol. 2011;23:21–8. [Google Scholar]
- 19.Singh K, Bhattacharyya M, Mutreja A, Dangda S. Trabeculectomy with subconjunctival collagen implant in Indian eyes:Long-term results. Indian J Ophthalmol. 2018;66:1429–34. doi: 10.4103/ijo.IJO_462_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong TT, Khaw PT, Aung T, Foster PJ, Htoon HM, Oen FT, et al. The Singapore 5-Fluorouracil trabeculectomy study:Effects on intraocular pressure control and disease progression at 3 years. Ophthalmology. 2009;116:175–84. doi: 10.1016/j.ophtha.2008.09.049. [DOI] [PubMed] [Google Scholar]
- 21.Wlaź A, Wilkos-Kuc A, Rozegnał-Madej A, Żarnowski T. Phacotrabeculectomy using collagen matrix implant (Ologen®) versus mitomycin C:A prospective randomized controlled trial. Acta Ophthalmol. 2019;97:e817–26. doi: 10.1111/aos.14102. [DOI] [PubMed] [Google Scholar]
- 22.Narayanaswamy A, Perera SA, Htoon HM, Hoh S-T, Seah SK, Wong TT, et al. Efficacy and safety of collagen matrix implants in phacotrabeculectomy and comparison with mitomycin C augmented phacotrabeculectomy at 1 year. Clin Experiment Ophthalmol. 2013;41:552–60. doi: 10.1111/ceo.12058. [DOI] [PubMed] [Google Scholar]
- 23.Senthil S, Rao HL, Babu JG, Mandal AK, Garudadri CS. Comparison of outcomes of trabeculectomy with mitomycin C vs. ologen implant in primary glaucoma. Indian J Ophthalmol. 2013;61:338–42. doi: 10.4103/0301-4738.109520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ichhpujani P, Dada T, Bhartiya S. Biodegradable collagen implants in trabeculectomy. J Curr Glaucoma Pract. 2015;9:24–7. doi: 10.5005/jp-journals-10008-1179. [DOI] [PMC free article] [PubMed] [Google Scholar]


