Dear Editor,
There have been several reports in the literature establishing an association between vaccination and uveitis.[1] The underlying mechanism is either inflammation secondary to vaccine additive or antigenic mimicry. Vaccine-associated uveitis is more commonly associated with hepatitis B vaccination due to delayed-type hypersensitivity reaction, a T-cell mediated response.[2,3] Lately, there have been reports of corneal graft rejection after COVID-19 vaccination (mRNA BNT162b2; Pfizer-BioNTech).[4] Cross-reactivity of the virus antigen-specific T cells with the corneal allograft endothelial cells could be the possible mechanism for graft rejection.[4] We encountered a case of reactivation of uveitis post-COVID-19 vaccination. A 27-year-old male, an established case of Juvenile Idiopathic Arthritis (JIA) with presence of HLA B-27, was diagnosed at the age of 13 years. He was on adalimumab for the last 3 years, which was discontinued in December 2019 due to unavailability of the drug locally and lockdown. He had a single episode of bilateral uveitis in 2012, which subsided with topical and oral steroids. There has been no relapse since then. Since he stopped adalimumab, he has had occasional large joints pain, which subsided with nonsteroidal anti-inflammatory drugs, but no ocular symptoms. After 2 days of the first dose of the COVID-19 vaccine (Covishield - Serum Institute of India), he experienced pain and redness in his left eye (OS). Unaided visual acuity in both eyes (OU) was 6/6. On examination, the right eye was normal while OS showed severe circumcorneal congestion, with 2+ cells in the anterior chamber with fine, fresh, nongranulomatous keratic precipitates (Fig. 1). Vitreous was clear and Fundus OU was normal. There were no clinical signs suggestive of recurrent or chronic uveitis. He responded well to topical steroids and cycloplegics. The proposed pathogenesis behind JIA is the uncontrolled activation of the innate immune system.[5] COVID-19 vaccines work by upregulating both the humoral and cellular immunity, especially in the initial week post vaccination. COVID-19 vaccination should not be deterred based on this report. We intend to highlight that relapse of uveitis could be a potential consequence of the COVID-19 vaccine. These patients should be under close follow-up post for early detection and treatment to prevent associated complications.
Figure 1.
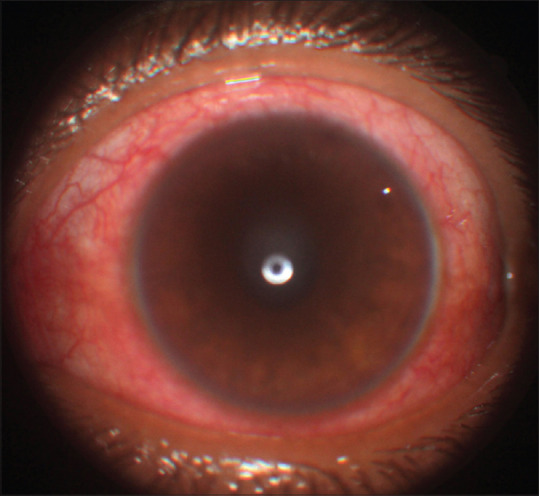
Anterior segment photo of the left eye showing severe circumcorneal congestion. The pupil is round and the lens is clear
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.London NJ, Garg SJ, Moorthy RS, Cunningham ET. Drug-induced uveitis. J Ophthal Inflamm Infect. 2013;3:43. doi: 10.1186/1869-5760-3-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benage M, Fraunfelder FW. Vaccine-associated uveitis. Mo Med. 2016;113:48–52. [PMC free article] [PubMed] [Google Scholar]
- 3.Fraunfelder FW, Suhler EB, Frederick T, Fraunfelder FT. Hepatitis B vaccine and uveitis:An emerging hypothesis suggested by review of 32 case reports. Cutan Ocul Toxicol. 2010;29:26–9. doi: 10.3109/15569520903427717. [DOI] [PubMed] [Google Scholar]
- 4.Phylactou M, Li JO, Larkin DFP. Characteristics of endothelial corneal transplant rejection following immunisation with SARS-CoV-2 messenger RNA vaccine. Br J Ophthalmol. 2021;105:893–6. doi: 10.1136/bjophthalmol-2021-319338. [DOI] [PubMed] [Google Scholar]
- 5.Adams A, Lehman TJ. Update on the pathogenesis and treatment of systemic onset juvenile rheumatoid arthritis. Curr Opin Rheumatol. 2005;17:612–6. doi: 10.1097/01.bor.0000169363.69066.d0. [DOI] [PubMed] [Google Scholar]


