Abstract
Purpose:
Dry eye disease (DED) is a multifactorial disease, more prevalent among visual display terminal users. Reduced blink rate is a risk factor to dry eye disorder, innovative means to remind to blink while using computers can be helpful.
Methods:
Single-blinded Randomized Control Trial enrolled computer users with dry eye. Allocation concealment was done using opaque envelope and principal investigator was blinded. After baseline examination, eligible participants were randomized to intervention group (appearance of bars is 8 times/min) and control group (appearance of bars is 1 time/min). Participants from both groups used the software for 15 days, came for first follow up, and did not use the software for next 15 days until second follow-up examination. During each visit, detailed eye examination was done including blink rate, tear film break up time, and Ocular Surface Disease Index score.
Results:
Forty-six participants (women n = 31; men n = 15) with a mean age of 28.02 (±6.295) years completed the study. Four participants were excluded from analysis because of early dropout. In the intervention group (n = 23) and control group (n = 23), participants were allocated. At the end of first phase, there was statistically significant difference in OSDI score (P = 0.021). Statistically significant difference was noticed in OSDI (P = 0.014) and blink rate (P = 0.049) as baseline, and final visit data were compared.
Conclusion:
“Blink–Blink” software with 8 reminders/min improved DED-related symptoms by increasing the blink rate. The carry-over effect after cessation of Blink-Blink software in improving blink rate was maintained even after 1 month.
Trial Registration: Clinical Trials Registry-India (CTRI): CTRI/2018/08/015176
Keywords: “Blink-Blink” animated software, blink rate, dry eye disease, randomized control trial
The prevalence of dry eye disease (DED) has been approximated to be 5–30% in age group of ≥ 50 years old, and it is hypothesized to increase with age and reported to be higher in women than men.[1] “Dry eye is a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities act as etiological roles”.[2]
The prevalence of DED has been reported to be at high risk among the profound computers and visual display terminal (VDT) users distinctly in those who use for 4 h or more every day.[3,4,5,6] The risk factors to be associated with the incidence of DED are adulthood, increasing age, and professional workers[7]
A normal blink rate generally ranges from 10 to 16 blinks/min, but while using digital gadgets, it is observed to reduce to 5–- blinks/min. The reduction in blink rate among VDT users can be associated with the decreased endogenous blink rate while engaged in focused activity. The higher the cognitive demand, the fewer endogenous blinks occur, resulting in a considerable reduction in the number of blinks during computer work. While concentrating on a computer screen, cortically driven blink inhibition occurs and an increase in cognitive behavior load leads to a decrease in blink rate.[8,9]
Blink rates are reduced with prolonged use of VDT and extended exposure to computer screen resulting in increased evaporation of the tear film from the ocular surface, which can lead to DED.[6] Wu et al. demonstrated that sensory simulation of ocular surface leading tearing is connected to blinking and interblink intervals.[10]
Hence, it is essential that VDT users are carefully evaluated for ocular surface disorders and are offered preventive as well as therapeutic care if required. Innovative methods to help remind them to blink while using computers will help increase their blink rate. Behavioral change toward enhancing blink rate will probably help improve the quality of life among VDT users.[11] Though there are numerous nonpharmacological methods available like software programs that darken the computer screen for few minutes, an external device like humidifier to increase blink rate in computer users, very few interventions have been accepted for wider clinical application. Nosch et al. reported in a cross-sectional study using the beta version of the “Blink-Blink” animation software program to simulate the blink action. The software was developed by the Institute of Optometry, FHNW, CH-Olten, and programmed by Google, CH-Zurich.[9] The software was developed and applied with the idea of stimulating the blink action in computer users. This study shows an increase in blink frequency and improvement in subjective symptoms of dry eyes during prolonged work.
There is however insufficient evidence to demonstrate the effectiveness and sustainability of “Blink-Blink” software because objective clinical tests were not performed, animation presentations were less, and software was not given for prolongs time. The purpose of current study is single-blinded Randomized controlled trial was to explore the efficacy of the “Blink-Blink” software in computer users (>4 h/day) with DED, in view of the improvement in both, blink rate and dry eye symptoms.
Methods
This was the block, single-blinded, randomization study on the efficacy of “Blink-Blink” software in improving the blink rate and dry eye symptoms among patients with DED using VDTs.
Fifty subjects with ≥4 h of daily computer use were recruited prospectively. Ethical clearance was obtained from the Institutional Ethical Committee and before starting the trial it was registered at Clinical Trial Registry (CTRI)-India. Also, the study was conducted in accordance with Helsinki Declaration as revised in 2013. Eligible participants were informed about the study in detail including procedures, chances of risks in the study, benefits they get from this study, and the voluntary option of participation, before signing consent form. Participants were volunteers from the various departments. The study was conducted in the Preclinical lab of Optometry Department.
Inclusion criteria were age ≥18 years, daily computer use ≥4 h, DED with regular use of tear supplements, OSDI score ≥13, and Tear film break up time (TBUT) less than 10 s in both eyes.[11] Exclusion criteria were history of ocular surgery or injury, active ocular infection, contact lens use, and use of any topical prescription ophthalmic medication other than tear supplementation.
A simple, block randomization method was used to allocate the participants with a dry eye to the interventional and control group. The random allocation sequence was generated by using the random number allocation software by one of the study team members (RSVe) and the allocation ratio was 1:1. Each allocated number was put into an opaque concealed envelope and access to this was restricted only to two members (RSVe, NW) of the study excluding the principal investigator. To eligible participants, randomly allocated into intervention (Group 1) or control (Group 2) was assured by opening the envelope in sequential order. Concealed opaque envelopes were opened by independent team member (NW) and participants were allocated to intervention or control group in sequential order. One independent team member (NW) installed the software in computers or laptops of these participants into intervention group (“Blink-Blink” frequency of 8 times/minute) and control group (“Blink-Blink” frequency of 1 time/min). Software was installed in participant’s computer/laptop in their working place (during working hours).
All clinical examinations were carried out by the principal investigator (PI- ADL), including preliminary (base-line) examination, verification of eligibility, and follow-up examinations. Care was taken to avoid any undue disclosure of the allocation to any other team member especially to PI, and participants were requested not to reveal the frequency of blink simulation to the PI during follow-up clinical examination visits. The allocation concealment groups were revealed only after the study analysis including final statistical report was prepared.
The “Blink-Blink” software projects “Two semitransparent bars from the top and bottom of the computer screen, moving toward each other simultaneously.” These animations appear in regular intervals when the application or computer is in use. Customizable options such as the coverage area of the screen, opacity of bars, frequency and duration of a presentation, as well as the color of the bars, can be adjusted in the software.[9] The software settings for the current study were set as follows: duration of 1 s for each animation, coverage of 20% of the computer screen on the top and bottom screen (40% in total), and gray color bars with 25% opacity.
For the interventional group, the frequency of the appearance of the bar was set at 8 s (that is 7–8 times/min). For the control group, it was set at 60 s once (that is 1 time/min). Participants were instructed to blink twice for each animation, in order to achieve a physiological blink rate of 16 blinks/min in the intervention group. The appearance of blink animations did not affect the computer’s performance in any way (minimal proportion of working memory required). Participants were instructed to blink twice every time bars appeared on the computer screen so that the physiological ideal of 16 blinks/min could be achieved.
Clinical and study procedure
Participants underwent comprehensive baseline anterior eye slit-lamp examinations. Eligible participants with dry eyes were recruited for the study and were randomly allocated to the groups. Concealed opaque envelopes were opened by independent team members and participants were allocated to intervention or control group in sequential order.
TBUT was performed using a Fluorescein strip.[8] The test was repeated three times in each eye and the mean value was calculated. Value of fewer than 10 s in both the eyes was considered as indicative of tear film instability. The OSDI questionnaire was conducted to all participants including during the follow-up examinations by PI (ADL). Score >13 points considered as DED.[10] Also, permission was obtained from the author before starting the data collection. Blink rate was assessed by reviewing video recordings taken using an iPhone 6, while the participant read a book on the computer screen. All participants provided informed consent toward video recording and the process of deleting the video personal information at the end of the study. The content of the book was a neutral story and does not have any emotional effect on the reader. Participants were asked to read for a duration of 5 min, while the video was taken and assessed for the number of blinks per minute, the mean value of blink rate was noted for analysis. In addition to this objective measurement of blink rate, the number of blinks per minute was recorded subjectively (by observing the blink rate), while participants were filling in the OSDI questionnaire. Both subjective and objective blink rate measured because spontaneous blink rate varies depending on one’s cognitive state. While higher-order information processing is involved in controlling spontaneous blink.
Participants were required to use the “Blink-Blink” software during computer work for duration 15 working days. The usage of the software that is number of days, time with minutes, was recorded automatically by a log which was installed while installing the software. During the study period, the participants’ automatic sleep time settings were also modified such that the software paused once they were not using the computer and that it started again when they resumed their computer work. Participants were advised and counseled to avoid ergonomical factors such as sitting position in front of air condition, or a bright light source that could influence dry symptoms during the study period.
The first follow-up eye examinations of both the groups were carried out after the 15 day period of software use. Subsequently, participants from both groups were asked to not use the software for the next 15 days, after which the final follow-up examination was performed after a total of 30 days of study participation. The purpose of this carry-over visit was to provide a potential insight into behavioral changes of the participants’ blink rates using the software, in order to better estimate its effect on dry eye symptoms. The software was uninstalled latter half of the study only in the participants who do not wish to use it later. The decision to let the software for future use was one of the benefits the participants get after the end of the study. We reviewed the log and ensured that during the second half the participants did not use it during the trial
Outcomes
The study’s main outcome measures were OSDI score, Blinks/minute (observed), Blinks/minute (recorded), and TBUT values.
Statistical analysis
Statistical analysis was carried out by using IBM, Statistical Package for the Social Sciences statistics version 20 (IBM Inc.). The data were analyzed for normality test by using the Kolmogorov–Smirnov test, and data was not normally distributed. So nonparametric tests are performed for further analysis. The Wilcoxon signed-rank test was used to compare outcomes within each group. The Mann–Whitney U test was performed to compare the differences between the intervention and control groups. For both these tests, a P value ≤0.05 was considered statistically significant. Descriptive data were presented as median (Intraquartile range (Q1–Q3) and categorical data as a number of participants unless otherwise stated.
Results
Participants
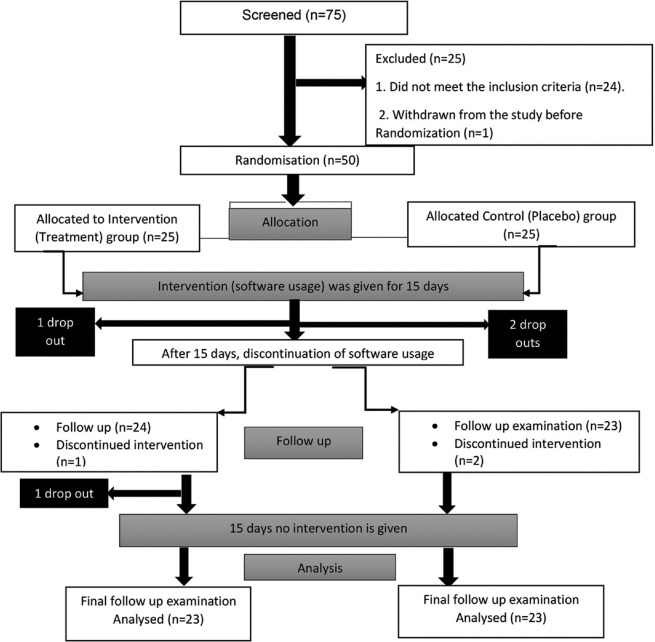
A total of 75 participants underwent comprehensive eye examinations for verification of inclusion criteria. Of these, 50 eligible participants with definite and newly diagnosed DED (men, n = 17; women, n = 33; 28.02 ± 6.295 years, range: 18–45 years) were enrolled. Twenty-five participants were randomly allocated to the intervention, and 25 participants to the control group [Fig. 1].[12] Four participants (two from each group) did not complete the follow-up visits and were consequently excluded from the trial. Data from a total of 46 participants (23 in each group) were included.
Figure 1.
It shows the participant details and Randomized Control Trial protocol
Participant profiles
The participants’ demographic data are shown in Table 1. The mean ages of the participants in the intervention and control groups were 29.09 ± 6.067 and 26.96 ± 6.407 years, respectively. Participants in both groups had similar parameters at baseline.
Table 1.
Demographic details of participants
| Groups | P | |||
|---|---|---|---|---|
|
| ||||
| Total | Intervention | Control | ||
| No. of participants | 46 | 23 | 23 | - |
| Age* (mean±SD) | 28.02 (±6.295) years | 29.09 (±6.067) years | 26.96 (±6.407) years | p=0.256 |
| Gender (n) | F: 31; M: 15 | F: 16; M: 07 | F: 15; M: 08 | p=0.543 |
| Working hours/day* (mean±SD) | 6.59 (±1.127) h/day | 6.83 (±1.072) h/day | 6.35 (±1.152) h/day | p=0.152 |
| Occupations (n) | ||||
| Faculty (n) | 21 | 12 | 09 | p≥0.05 |
| Office workers (n) | 09 | 05 | 04 | p≥0.05 |
| PhD (n) | 02 | 01 | 01 | p≥0.05 |
| Students (n) | 14 | 05 | 09 | p≥0.05 |
| “Blink-Blink “Software-usage per day*† (mean±SD) | 3.120 (±0.804) h/day | 3.201 (±0.760) h/day | 3.040 (± 0.856) h/day | p=0.502 |
| Baseline values‡ | ||||
| OSDI | 14.50 (14.00-17.00) | 15.00 (14.00-17.00) | 14.00 (13.00-17.00) | p=0.178 |
| Blink rate (obs) | 9.00 (6.75-12.00) | 9.00 (6.00-11.00) | 9.00 (7.00-12.00) | p=0.658 |
| Blink rate (rec) | 6.00 (3.75-12.00) | 6.00 (3.00-11.00) | 7.00 (4.00-12.00) | p=0.466 |
| Tear film break up time | 5.00 (3.00-6.00) | 4.00 (3.00-6.000 | 5.00 (3.00-6.00) | p=0.303 |
*Results are expressed in mean±SD (age, working hours/day, and Software usage/day) and numbers (gender& occupation), †Mean number of hours per day of “Blink-Blink” software as per the log records. ‡Baseline values represented in median (Q1-Q3). OSDI: Ocular surface disease index
Adverse events
There were no adverse events reported during the trial.
Comparison of postintervention outcomes between the groups
A statistically significant difference in OSDI score was observed between the treatment and control group after the intervention phase of this study (P = 0.045). However, no statistically significant differences were obtained for observed or recorded blink rate (P = 0.790 and P = 0.834, respectively), nor for TBUT (P = 0.073) shown in Table 2.
Table 2.
Median values postintervention (after the 15 days usage of the software) for OSDI score, blink rate, and tear film break up time values of each group and compared between the groups
| Postintervention (n=46) | Intervention vs. Control group | ||
|---|---|---|---|
|
| |||
| Intervention group | Control group | Intervention vs. control | |
| OSDI score* | 12.00 (8.00-15.00) | 14.00 (10.00-17.00) | 12.00 (10.00-15.50); p=0.045 |
| Blink rate [blink/minute] (obs)* | 10.00 (8.00-12.00) | 10.00 (7.00-12.00) | 10.00 (7.75-12.00); p=0.790 |
| Blink rate [blink/minute] (rec)* | 9.00 (5.00-15.00) | 9.00 (6.00-12.00) | 9.00 (6.00-13.00); p=0.834 |
| Tear film break up time [seconds] (no. of eyes)* | 5.00 (4.00-6.00) | 5.00 (4.00-5.00) | 5.00 (4.00-5.00); p=0.073 |
*Results are expressed in median (Q1-Q3) and P - Mann-Whitney U test. OSDI: Ocular surface disease index
Carryover effect of the software
In the second phase of the analysis, the carry-over effect of the software was assessed by comparing the parameters of the postintervention (after the usage of software for 15 days) and parameters of post-follow-up of 15 days (without the software usage). Participants used the software every day during the intervention phase, with mean ± SD duration of 3.201 ± 0.760 h in the intervention group and a mean ± SD duration of 3.040 ± 0.856 h per day in the control group, respectively. In the intervention group, it observed to be no significant difference in OSDI, Blink rate (observed), Blink rate (recorded), and TBUT (P = 0.453, P = 0.106, P = 0.930, and P = 0.338), respectively. In the control group, there was no significant difference in OSDI (P = 0.528), Blink rate (observed) (P = 0.080), Blink rate (recorded) (P = 0.218), and TBUT (P = 0.166) [Fig. 2]. Between the groups, no statistically significant difference in OSDI score (P = 0.956), observed blink rate (P = 0.883), recorded blink rate (P = 0.510), and TBUT values (P = 0.215) could be observed.
Figure 2.
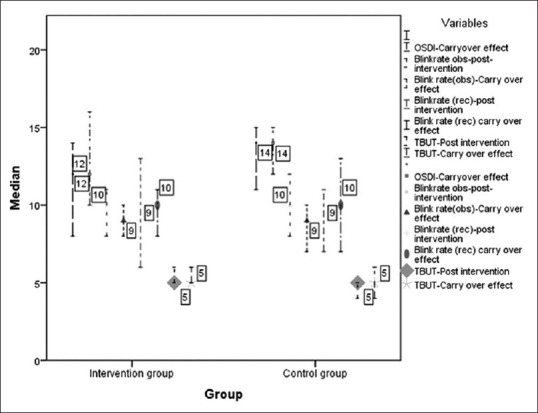
It shows the median values of OSDI, observed blink rate, recorded blink rate, and tear film break up time values postintervention and wash out phase, for both the groups
Comparison of the baseline and carry-over effect of the software
All baseline and final follow-up measurements were compared, in order to assess the effect of the software after 1 month. The OSDI scores were found to improve to a statistically significant degree within the treatment group (P = 0.021) and also when compared to the control group (P = 0.014), respectively [Table 3]. Also, a statistically significant difference was obtained for the observed blink rate, when comparing the two groups with each other (P = 0.049). In the intervention group as well as the control group, recorded blink rate increased significantly (P = 0.008 and P = 0.001, respectively). No significant difference was found in TBUT values for either group, nor when comparing the two groups.
Table 3.
Median differences of the outcomes of the baseline and carry-over effect of the software in groups and between the groups
| Baseline and carry-over effect of software after 15 days (n=46) | Groups | ||
|---|---|---|---|
|
| |||
| Intervention | Control | Intervention vs. Control | |
| OSDI* | -4.00 (-8.00-[-2.00]); p=0.021 | -1.00 (-3.00-2.00); p=0.301 | -2.00 (-4.00-1.00); p=0.014 |
| Blink-rate (Observed) * | 1.00 (0.00-2.00); p=0.095 | 0.00 (-2.00-1.00); p=0.674 | 1.00 (-1.00-2.00); p=0.049 |
| Bink-rate (recorded) * | 3.00 (1.00-5.00); p=0.008 | 2.00 (1.00-5.00); p=0.001 | 3.00 (1.00-5.00); p=0.707 |
| Tear film break up time (No. of eyes)* | 0.0 (-0.25-1.25); p=0.055 | 1.00 (-1.00-1.00); p=0.381 | 0.50 (-1.00-1.00); p=0.601 |
*Results are expressed in median (Q1-Q3) and P values from the Wilcoxon Signed-Rank test and Mann-Whitney U test. OSDI: Ocular Surface Disease Index
Discussion
In this single-blinded, randomized, control trial, the efficacy of the “Blink-Blink” animation program was assessed with regards to the variables TBUT, OSDI scores, and blink rate during a period of 15 days and an additional 15 days of washout period. Dry eye symptoms improved to a statistically significant degree in the treatment group.
OSDI-based dry eye symptom improved with “Blink-Blink” software, with eight animation presentations per minute in this study. Similar results of improvement in dry eye symptoms were reported by Nosch DS, et al. in 2015 using the earlier version of “Blink-Blink” software.[9] In the current study, updated version of “Blink-Blink” software was used. In this, a user can adjust the coverage, degree of opacity, frequency, color, and duration of the animation presentation as required. In the earlier Nosch et al. study, they had basic version of the software used with default options.[9] With this basic version software, there was an improvement in dry eye symptoms and blink rate. Outcomes of the study were OSDI symptom score and blink rate. Clinical objective tests were not performed.
In the current study, the blink rate at the end of the final visit improved in both intervention (3 times more than baseline) and control group (2 times more than baseline) [Table 3]. In the placebo group, instead of no intervention, we had included one animation reminder per minute of the “Blink-Blink” software; the study showed that the use of such software showed an improvement in the blink rate. More reminders have a better outcome in improving the blinking rate and this software can be a healthy alternative as a nonpharmacological. The carry-over effect of blinking behavior lasted for 30 days from the date of enrollment in both intervention and control groups. Evans SR in 2010 state that effect of any treatment given in a trial stays minimum of 5 times the half of the period of treatment given.[13] Blinking being a physiological activity controlling the participant to only blink when the reminders appear is not feasible, and in the current study, the “Blink-Blink” software was used as an additional.
Participants were requested to blink twice for every reminder by the “Blink-Blink” software. The software was found to be more user-friendly because of the fewer number of presentations per minute. Though participant’s experiences of using software were not studied extensively in this study, most of them gave a positive response toward using the “Blink-Blink” software and preferred to use this even after this study. Some also shared that they get adapted to the blink reminder and occasionally they do not see the flickering bars. Customizable options on the flicker duration, color, flicker frequency, etc., are available and if the user could make these personalized setting to enhance user experience. We noted that compliance to blink along with “Blink-Blink” was more observed among motivated or symptomatic participants, and they preferred to use the software for prolong time.
The effect of software on symptomatic dry eye participants was analyzed by observing the changes seen in the tear film break-up time values across trials. “Blink-Blink” software was useful in treating the dry eye condition especially in those who had symptomatic dry eye and blink rate improved along with tear film stability.
Limitations
The period of software usage should be increased so that it would be more useful to check the carryover effect of the software and behavioral changes that happened due to software. Limiting the participant to only blink as per the software reminder was not feasible in this study. This has probably resulted in the improvement in blink rate in the Intervention and control group in this study. Though the current study documented blink rate objectively and subjectively, the participants were relatively more conscious as these measurements were done during clinical visits. With due consent and ethical approval to remotely activate the web camera while participants use laptop and record blink rate could give us the effect of “Blink-Blink” software in real time.
Future scope
Evidence toward efficacy of “Blink-Blink” animation software has been reported in this study and by earlier studies by Nosch et al.[9] The benefits of improving blink rate and reducing symptoms have a good application preventive eye care measure among VDT users. This “Blink-Blink” animation software can be included as a mandatory or optional feature as part of the operating system and wide-scale applications of this software need to be evaluated.
There is scope to develop “Blink-Blink” animation programs that can be developed for operating systems other than windows. Considering the increase in smartphone, tablets, virtual reality, etc., among VDT users, and current version of translucent bars may affect or obstruct user experiences in small screens. There is good scope develop innovative version of blink reminder software to suit these VDT interfaces without influencing their task or activity.
Conclusion
“Blink-Blink” software with 8 reminders/min improved DEDs-related symptoms by increasing the blink rate. The carry-over effect after cessation of Blink-Blink software in improving blink rate was maintained even after 1 month.
Trial registration
Clinical Trials Registry-India: CTRI/2018/08/015176.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Farrand KF, Fridman M, Stillman IÖ, Schaumberg DA. Prevalence of diagnosed dry eye disease in the United States among adults aged 18 years and older. Am J Ophthalmol. 2017;182:90–8. doi: 10.1016/j.ajo.2017.06.033. [DOI] [PubMed] [Google Scholar]
- 2.Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83. doi: 10.1016/j.jtos.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Titiyal JS, Falera RC, Kaur M, Sharma V, Sharma N. Prevalence and risk factors of dry eye disease in North India:Ocular surface disease index-based cross-sectional hospital study. Indian J Ophthalmol. 2018;66:207–11. doi: 10.4103/ijo.IJO_698_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rossi GC, Scudeller L, Bettio F, Pasinetti GM, Bianchi PE. Prevalence of dry eye in video display terminal users:A cross-sectional Caucasian study in Italy. Int Ophthalmol. 2019;39:1315–22. doi: 10.1007/s10792-018-0947-6. [DOI] [PubMed] [Google Scholar]
- 5.Schaefer TM, Schaefer AR, Abib FC, José NK. Comparative study of the blinking time between young adult and adult video display terminal users in indoor environment. Arq Bras Oftalmol. 2009;72:682–6. doi: 10.1590/s0004-27492009000500017. [DOI] [PubMed] [Google Scholar]
- 6.Yokoi N, Uchino M, Uchino Y, Dogru M, Kawashima M, Komuro A, et al. Importance of tear film instability in dry eye disease in office workers using visual display terminals:The Osaka study. Am J Ophthalmol. 2015;159:748–54. doi: 10.1016/j.ajo.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 7.Donthineni PR, Kammari P, Shanbhag SS, Singh V, Das AV, Basu S. Incidence, demographics, types and risk factors of dry eye disease in India:Electronic medical records driven big data analytics report I. Ocul Surf. 2019;17:250–6. doi: 10.1016/j.jtos.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Ledger H. The effect cognitive load has on eye blinking. The Plymouth Student Scientist. 2013;6:206–23. [Google Scholar]
- 9.Nosch DS, Foppa C, Tóth M, Joos RE. Blink animation software to improve blinking and dry eye symptoms. Optom Vis Sci. 2015;92:e310–5. doi: 10.1097/OPX.0000000000000654. [DOI] [PubMed] [Google Scholar]
- 10.Wu Z, Begley CG, Port N, Bradley A, Braun R, King-Smith E. The effects of increasing ocular surface stimulation on blinking and tear secretion. Invest Ophthalmol Vis Sci. 2015;56:4211–20. doi: 10.1167/iovs.14-16313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15:539–74. doi: 10.1016/j.jtos.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P. CONSORT statement for randomized trials of nonpharmacologic treatments:A 2017 update and a CONSORT extension for nonpharmacologic trial abstracts. Ann Intern Med. 2017;167:40–7. doi: 10.7326/M17-0046. [DOI] [PubMed] [Google Scholar]
- 13.Evans SR. Clinical trial structures. J Exp Stroke Transl Med. 2010;3:8–18. doi: 10.6030/1939-067x-3.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]