Abstract
Purpose:
To assess if high accommodative convergence/accommodation (AC/A) ratio impacts surgical outcomes in children with esotropia (ET), and evaluate the appropriate target angle in surgical dosing in the presence of high AC/A ratio.
Methods:
A retrospective chart review identified patients who underwent primary bilateral medial rectus (BMR) recessions for ET. Patients were excluded if follow-up was ≤2 months. Basic demographic information, visual acuity, stereopsis, alignment, and target angle for surgery were collected. High AC/A was defined as ≥10 prism diopter (Δ) deviation at near compared to distance. Outcome parameters were near and distance deviations ≤10Δ within orthophoria, and/or stereopsis postoperatively. Yates’ continuity correction, unpaired t-test, regression analysis, and one-way ANOVA were used.
Results:
We identified 103 patients, 23 with high AC/A and 80 with normal AC/A, preoperatively. Mean age was 4.0 ± 2.5 years. Surgical success measured by postoperative alignment was 48% and 45% in the high AC/A and normal AC/A groups, respectively (P = 1.0). There was a statistically significant difference in preoperative near deviation between high AC/A and normal AC/A groups (P = 0.0015); however, there was no significant difference in preoperative distance deviation (P = 0.061). In addition, there was not a significant difference in preoperative or postoperative stereopsis between high AC/A and normal AC/A groups (P = 0.88 and P = 0.44, respectively). There was a significant difference in the normal AC/A and high AC/A groups when target angle was directed toward preoperative near deviation as determined by one-way ANOVA (F = 170.88, P < 0.0001 and F = 14.61, P = 0.0010, respectively).
Conclusion:
In the setting of ET treated with BMR recession, the presence of high AC/A does not affect surgical success as measured by alignment and stereopsis. In addition, when high AC/A is present, surgical dosing with a target angle toward near deviation was found to yield the best surgical outcomes in our patient population.
Keywords: Bilateral medial rectus recession, esotropia, high AC/A ratio, strabismus surgery, target angle
Patients with esotropia (ET) present frequently for ophthalmic care. Management of this type of strabismus attempts to establish normal ocular alignment to maximize binocular vision and fusion. Many patients are treated with surgical correction, particularly those with infantile ET, and those who are not fully accommodative and not managed effectively with hyperopic correction.[1] A subset of these individuals also present with a high accommodative convergence/accommodation (AC/A) ratio in which ET is greater at near than at distance. Specifically, the AC/A ratio assesses the relationship between the amount of convergence that is generated given the amount of accommodation. An abnormally high AC/A ratio can be managed optically with full hyperopic correction, and oftentimes with the addition of a bifocal to reduce the added accommodation for near fixation.[2,3] However, when there is residual misalignment at distance and/or at near, despite the use of hyperopic correction with a bifocal, surgery may be undertaken to obtain normal ocular alignment.
Treatment of patients with ET and a high AC/A ratio is more complex, and the associated increased deviation at near may theoretically yield differing outcomes after surgery. In this study, we evaluated surgical outcomes of children with ET who underwent primary bilateral medial rectus (BMR) recessions. We compared preoperative and postoperative measurements of patients with a high AC/A ratio to those with a normal AC/A ratio to identify differences in surgical outcome, specifically postoperative alignment and stereopsis. We additionally evaluated the target angle selected by the surgeons within this study.
Methods
We conducted a retrospective chart review of patients who underwent primary BMR recessions for ET at the Children’s Hospital of Michigan. The hospital’s surgical billing database was searched for a combination of current procedural terminology (CPT) codes matching BMR recessions and International Statistical Classification of Diseases and Related Health Problems, 9th and 10th. Revisions (ICD9/10) diagnostic codes matching ET between March 2007 and July 2017. Surgery was performed by eight board-certified ophthalmologists, all fellowship-trained in Pediatric Ophthalmology and Adult Strabismus. Wayne State University School of Medicine (Exemption Concurrence, August 2017).
Upon review of medical records, patients were excluded if the patient had a history of prior strabismus surgery, if BMR recessions were combined with other strabismus surgery, or if follow up was less than 2 months. The data set was further evaluated to exclude patients without near and distance deviation measurements at both preoperative (up to 3 months before surgery) and postoperative visits.
Data collection included basic demographic information, medical and ophthalmic history, visual acuity, stereopsis, angle of deviation at near and at distance, target angle for surgery, cycloplegic refraction, and use of refractive correction. Visual acuity was measured using fixation pattern, LEA Symbol® or HOTV matching, or Snellen’s chart, based on the patient’s age and cooperation level. Deviations were measured using alternate prism cover testing (APCT) when allowable by age. When cooperation limited APCT, usually in patients under 1 year of age, the deviation was measured by Krimsky’s technique. All alignment measurements were initially completed by a trained Orthoptist and confirmed by the operating surgeon prior to surgery. Stereopsis was evaluated when allowable by age and cooperation and measured with Titmus Fly test or Stereo Butterfly test (Stereo Optical Co, Chicago, IL). Cycloplegic refraction was completed on all patients, using a combination of 1% Cyclogyl and 1% tropicamide, instilled simultaneously and repeated as necessary. A cycloplegic evaluation was attempted 30 min following instillation of eyedrops and was deemed appropriate in the setting of at least 7 mm pupillary dilation with the absence of pupillary constriction in reaction to light. Patients were given spectacle correction prior to surgery if the preoperative refractive error was greater than +1.50 diopters hyperopia, −0.50 diopters myopia, and/or +1.00 astigmatism.
Additional analysis was conducted separating the patients into groups of high AC/A ratio or normal AC/A ratio. High AC/A ratio was defined as an increase of ≥10 prism diopter (D) deviation at near compared to deviation at distance, in accordance with the heterophoria method of AC/A assessment.[4] Bifocal management was undertaken in patients with high AC/A ratio if patients had persistent ET of ≥10Δ at near in full cycloplegic correction. It was not undertaken if there was residual ET of ≥10Δ at distance despite near deviation measurements, as these patients would continue to have ET at distance requiring surgery, with or without the use of bifocals.
Surgery was undertaken in patients if there was a persistent deviation of ≥10Δ at distance and/or near, despite refractive correction or use of bifocals as outlined by the criteria above. The target angle at the time of surgery was to the discretion of the operating surgeon; however, the majority of surgeons aimed toward the near deviation measurement. Surgical success was judged by the following outcome parameters: (1) near and distance deviations ≤10Δ within orthophoria, and/or (2) presence of stereopsis (positive fly or butterfly) postoperatively. These outcome parameters were compared between the high AC/A ratio and normal AC/A ratio groups. Comparisons of categorical variables were made using Yates’ continuity correction given the sample size. Unpaired t-test was utilized for comparisons of numerical values. Regression analysis was used for correlations between two variables. One-way ANOVA was used to compare two or more variables. Significance in all analyses was determined by P values of less than or equal to 0.05.
The study was compliant with the Health Insurance Portability and Accountability Act. It was approved by the institutional review board of the Children’s Hospital of Michigan and fully adhered to the tenets of the Declaration of Helsinki.
Results
Our initial search identified 296 patients of interest. Of these patients, 183 met the inclusion criteria of primary BMR recessions performed for ET. Eighty patients were excluded due to follow up of less than 2 months (23 patients) or insufficient measurements (57 patients). Of the 103 included patients, 23 patients had a high AC/A ratio compared to 80 patients with a normal AC/A ratio, preoperatively. Fifty-eight patients were capable of postoperative stereopsis measurements.
The mean age of patients at the time of surgery was 4.0 ± 2.5 years (range: 0.7 to 14.1 years) and was similar between the two groups with a mean age of 4.2 years in the high AC/A group and mean age of 3.9 years in the normal AC/A group (P value = 0.65, unpaired t-test). There were 5 patients under the age of 1 year who fit the inclusion criteria. There was a similar gender distribution, with 45 females and 58 males. In the high AC/A group, there were 10 females and 13 males, while in the normal AC/A group, there were 35 females and 45 males (P value = 0.79, Yates’ continuity correction). The mean follow-up time was 27.9 ± 21.1 months (median: 25.1 months).
There was a statistically significant difference in preoperative alignments, specifically with greater near deviation in the high AC/A group (45.9 ± 14.4D) compared to the normal AC/A group (38.1 ± 13.7D) (P value = 0.0015). Although there was not a significant difference in preoperative distance deviation between high AC/A (31.9 ± 15.3D) and normal AC/A groups (38.3 ± 13.9D), the trend approached significance with the latter having a higher distance deviation (P value = 0.061). In the high AC/A group, near deviation was 45.9 ± 14.4D and distance deviation was 31.9 ± 15.3D, with a mean AC/A ratio of 14D in this group. There was not a significant difference in preoperative stereopsis between high AC/A and normal AC/A groups with 11.1% of patients with high AC/A and 20.8% with normal AC/A having positive fly on preoperative stereopsis testing (P value = 0.88).
There was no significant difference measured in preoperative refraction between high AC/A and normal AC/A groups with an average preoperative refraction of +2.8 ± 2.2 diopters in patients with a high AC/A ratio and an average preoperative refraction of +1.8 ± 3.5 diopters with a normal AC/A ratio (P value = 0.20). Patients with refractive error meeting spectacle correction criteria (as listed in methods) were given full cycloplegic refraction. Fifty-four patients were given glasses preoperatively: 13 in the high AC/A group and 41 in the normal AC/A group. Bifocal correction with a +3.00 reading addition at near was attempted for 6 of the 23 patients with high AC/A ratio prior to surgery. It was not attempted on the remaining patients in the high AC/A group secondary to persistent ET at distance despite full hyperopic correction.
Due to the low number of infantile ET cases (5 total) in our study, we did not differentiate between patients with and without infantile ET. However, all patients with infantile ET had a normal AC/A ratio, and only one of these patients was given glasses preoperatively.
Demographic variables and preoperative characteristics of patients are shown in Tables 1 and 2.
Table 1.
Demographic variables of patients with esotropia in the presence of high AC/A ratio and normal AC/A ratio
| High AC/A ratio (n=30) | Normal AC/A ratio (n=86) | P | |
|---|---|---|---|
| Age at surgery (years) | 4.2±2.3 | 3.9±2.8 | 0.65 |
| Female | 10 | 35 | 0.79 |
| Male | 13 | 45 |
AC/A=Accommodative convergence to accommodation
Table 2.
Preoperative alignment and stereopsis of patients with esotropia in the presence of high AC/A ratio and normal AC/A ratio
| High AC/A ratio | Normal AC/A ratio | P | |
|---|---|---|---|
| Pre-op Deviations | |||
| Near (Δ) | 45.9±14.4 | 38.1±13.7 | 0.0015 |
| Distance (Δ) | 31.9±15.3 | 38.3±13.9 | 0.061 |
| Pre-op stereopsis | 0.88 | ||
| Negative fly | 8 | 19 | |
| Positive fly | 1 | 5 |
AC/A=Accommodative convergence to accommodation. Δ=Prism diopters
Average postoperative deviation at near was 7.2 ± 14.9D in the high AC/A group and 7.7 ± 14.1D in the normal AC/A group (P value = 0.88, unpaired t-test). The average postoperative deviation at distance was 1.8 ± 11.9D in the high AC/A group and 5.6 ± 13.8D in the normal AC/A group (P value = 0.24, unpaired t-test). With regards to surgical success measured by postoperative alignment within 10Δ of orthophoria at distance and at near, there was no statistically significant difference between the 2 groups, with rates of 48% and 45% in the high AC/A ratio and normal AC/A ratio groups, respectively (P value = 1.0, Yates’ continuity correction). Forty-four patients were measured with refractive correction for postoperative alignment.
For the 12 patients with a high AC/A ratio who did not achieve surgical success, 5 patients failed secondary to the persistent deviation of ≥10Δ at near, 4 due to both near and distance deviation ≥10Δ ET, and 3 were overcorrected with ≥10Δ exotropia (2 overcorrected at both distance and near, and 1 overcorrected at distance deviation only). Of the 44 patients with a normal AC/A ratio who did not achieve surgical success, 15 failed secondary to the persistent deviation of ≥10Δ at near, 20 due to both near and distance deviation ≥10Δ ET, and 9 patients were overcorrected with ≥10Δ exotropia (4 overcorrected at both distance and near, and 5 overcorrected at distance deviation only). There was no statistical significance in comparison of these findings. Further analysis revealed a resurgery rate of 28.6%. Of the 56 patients who did not achieve surgical success, 4 patients in the high AC/A group underwent additional strabismus surgery (33.3%) and 12 patients in the normal AC/A group underwent additional strabismus surgery (27.3%).
Postoperative alignment measurements in the presence of high AC/A and normal AC/A are shown in Table 3.
Table 3.
Postoperative alignment and stereopsis of patients with esotropia in the presence of high AC/A ratio and normal AC/A ratio
| High AC/A ratio | Normal AC/A ratio | P | |
|---|---|---|---|
| Post-op Deviations within 10Δ orthophoria at distance & near | 48% | 45% | 1.0 |
| Near (Δ) | 7.2±14.9 | 7.7±14.1 | 0.88 |
| Distance (Δ) | 1.8±11.9 | 5.6±13.8 | 0.24 |
| Post-op stereopsis | |||
| Negative fly | 9 | 37 | 0.44 |
| Positive fly | 4 | 8 |
AC/A=Accommodative convergence to accommodation, Δ=Prism diopters
Of the 58 patients with cooperation capable of stereopsis measurements (inclusive of both groups), 46 had negative fly (mean age 4.8 ± 2.9 years) and 12 had positive fly (mean age 5.5 ± 2.2 years) postoperatively. With regards to surgical success as measured by the presence of postoperative stereopsis, there was not a significant difference in the stereopsis outcome between the two groups, with 75% of patients with normal AC/A ratio versus 50% of patients with high AC/A having positive fly on postoperative stereopsis testing (P value = 0.53, Yates’ continuity correction). There was not a significant difference in preoperative or postoperative stereopsis between high and normal AC/A groups (P value = 0.88 and P value = 0.44, respectively). Eight patients presumably gained stereopsis. These patients had negative fly preoperatively and positive fly postoperatively. Of those, 3 patients had a high AC/A ratio and 5 patients had a normal AC/A ratio preoperatively. Overall, we had 2 patients lose stereopsis postoperatively, both with a normal AC/A ratio. Postoperative stereopsis measurements in the presence of high AC/A and normal AC/A are shown in Table 3.
Twenty-two patients (7 with high AC/A ratio and 15 with normal AC/A ratio) had an ocular alignment of 4D or less of residual postoperative microtropia at both near and distance deviations, a more stringent outcome parameter. Within this group, 10 patients were capable of stereopsis measurements, of which 5 had positive postoperative stereopsis.
In addition, there was no significance of those having surgical success and wearing glasses preoperatively in either high AC/A or normal AC/A groups (P value = 0.14 and P value = 0.18, respectively).
There was a statistically significant difference in the normal AC/A and high AC/A groups when the target angle was directed toward preoperative near deviation as determined by one-way ANOVA (F = 170.88, P < 0.0001 and F = 14.61, P = 0.0010, respectively). The target angle was aimed at preoperative near deviation in the majority of patients [R2 = 0.61, Fig. 1] with a stronger association in the normal AC/A group compared to the high AC/A group [R2 = 0.69 and R2 = 0.41, respectively, Figs. 2 and 3]. The target angle was slightly associated with preoperative distance deviation, but not as much as near deviation (R2 = 0.54). Overall, 54.2% of patients had surgical success when the target angle was equal to the preoperative near deviation.
Figure 1.
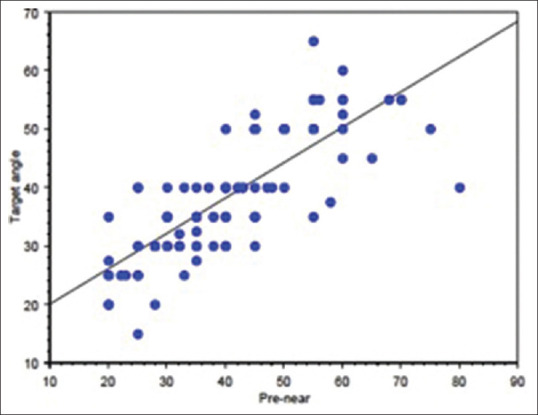
Linear regression plot of target angle aimed at preoperative near deviation (pre-near) (R2 = 0.61) in all patients
Figure 2.
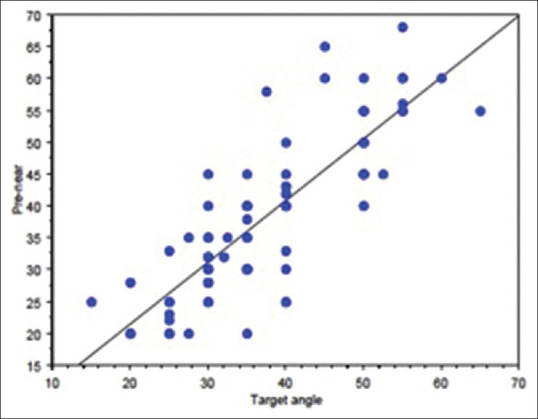
Linear regression of target angle aimed at preoperative near deviation (pre-near) in the normal AC/A group (R2 = 0.69)
Figure 3.
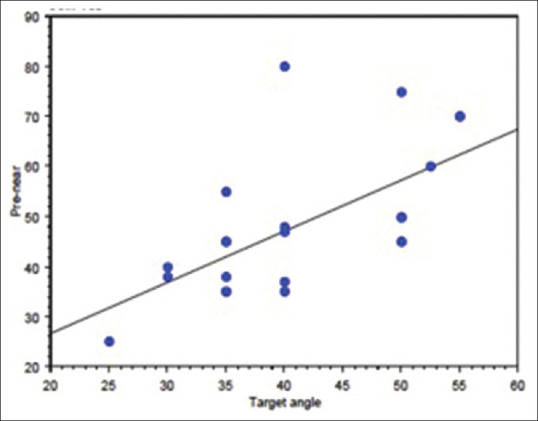
Linear regression of target angle aimed at preoperative near deviation (pre-near) in the high AC/A group (R2 = 0.41)
Of the 12 patients (3 with high AC/A ratio, 1 of which was in bifocal preoperatively, and 9 with normal AC/A ratio) overcorrected with a postoperative deviation greater than 10Δ at distance or at near, the average postoperative distance and near deviations were −19.0 ± 7.3D and −12.8 ± 16.7D, respectively. The majority of these patients had a target angle aimed at near deviation (R2 = 0.75).
Discussion
In this retrospective review, we show that the presence of a high AC/A ratio preoperatively in ET patients treated with BMR recessions does not affect surgical success as measured by postoperative alignment and stereopsis.
In regard to the surgical outcome of stereopsis, the results of our study are somewhat surprising. We hypothesized that those patients with ET associated with a high AC/A ratio are more likely to have at least partially accommodative ET, and thus, are more likely to develop stereopsis in infancy and early childhood. While stereopsis may be lost when misalignment decompensates and deviation amplitudes increase, it may be regained once normal alignment is reinstated. This is in contrast to those patients with infantile and other forms of nonaccommodative ET with normal AC/A ratio, in which stereopsis does not develop in the critical period and therefore cannot be regained even when normal alignment develops postoperatively.[5] A study by Park and Oh supports this hypothesis, retrospectively identifying a poorer stereoacuity outcome in those patients with infantile ET who underwent surgery but then had an accommodative component effectively treated with glasses, compared with fully accommodative ET never requiring surgery.[6] According to Fawcett et al.[7] the critical period for development and maintenance of stereoacuity occurs between 6 and 18 months of age. They found children with accommodative ET with an age of onset ≥25 months had better stereoacuity. Another study by Li and Sharan identified a different aspect of stereopsis recovery. They found a higher rate of sensory fusion development when initial hyperopic correction was given within 6 months of ET onset in a group of patients with high hyperopia, irrespective of time to surgery.[8] While our study does not support a differing fusional outcome among patients with high AC/A ratio, we additionally speculate that a longer follow-up period for some of our patients may have yielded differing results, as stereopsis may improve with time as children develop increased cooperation with age.
The findings of this study may be of particular interest as recent literature has pointed toward surgery over bifocal correction for patients with a high AC/A ratio, as the latter may lead to poor control of near deviation with increasing AC/A gradient over time. Whitman et al.[9] conducted a retrospective review of patients with a high AC/A ratio after treatment with bifocal glasses compared with single-vision lenses. They found that stereopsis improvement was similar with bifocal versus single-vision lenses, and those patients treated with bifocal lenses had a higher tendency toward surgery as well as a smaller improvement in near deviation over time. Another study by Tajedor et al.[10] retrospectively showed that short-term improvement in visual acuity is more rapid with bifocal glasses versus single-vision lenses, but the AC/A gradient tends to increase with time in patients managed with bifocal glasses. While it may seem logical to treat ET patients with a high AC/A ratio with bifocal lenses to prevent excessive convergence and secondary medical rectus muscle changes, there are currently no studies supporting that bifocal lenses can actually prevent this from occurring. Ludwig et al. found that the presence of a high AC/A ratio in the setting of accommodative ET led to an increased likelihood for the deterioration that could not be controlled with glasses alone and would ultimately require surgery, and this tendency increased as the AC/A ratio increased.[11,12] Overall, surgery was shown to normalize the AC/A ratio, allowing patients to maintain good alignment at both near and distance.[13] Arnoldi and Shainberg[14] have additionally supported this hypothesis. Their study, with a longer follow-up period of several years, compared bifocals, single vision hyperopic correction, and surgery in the treatment of patients with a high AC/A ratio. They showed that all three treatment modalities were effective, with surgery yielding a significant reduction of the near angle and improvement of the distance-near disparity. Additional studies, both retrospectively and prospectively, have found that strabismus surgery, specifically unilateral and BMR recessions as well as combined resection and recession of medial rectus, may be an effective alternative to long-term use of bifocals in treating patients with high AC/A ratio ET.[15,16,17,18,19] Patients in these studies had good sensory and alignment outcomes in this setting.[15,16,17,18] While our study focused on patients who had residual misalignment despite refractive correction with or without bifocal, we found that surgery in these patients with a high AC/A ratio yields similar outcomes to patients with nonaccommodative ET and a normal AC/A ratio. Surgery may ultimately be preferred over bifocal correction once distance deviation deteriorates to greater than 10Δ. Although there is limited information about the long-term effects of surgery for ET with high AC/A, surgery avoids compliance and tolerance issues that present with bifocal and single-vision lenses.
As a secondary analysis, we evaluated the target angle used by the majority of our surgeons to treat the nonaccommodative element in esotropic patients with a high accommodative convergence-accommodation ratio. It may be speculated that when near-distance disparity is present, aiming for the larger near deviation may lead to overcorrections at distance, and vice versa. The higher, near deviation was used by most surgeons in our study and yielded favorable outcomes without significant overcorrection rates. This is supported by other studies, which have demonstrated the absence of significant postoperative exotropia when aiming for the larger ET at near than distance.[16,20] In addition, the use of the larger near target angle in surgical dosing has not only been identified as a successful technique in regards to both alignment and sensory outcomes, but has been found to more likely allow discontinuation of both bifocal and spectacle correction over distance target angle dosing.[16,21] Similar to our study, a prospective, randomized, masked analysis of bilateral medial recessions aimed for distance deviation with posterior fixation suture compared to bilateral medial recession augmented for near deviation. The latter was identified as superior in achieving satisfactory alignment with discontinuation of both spectacles and bifocals postoperatively.[22]
There are several limitations that should be considered in this study including its retrospective non-randomized nature, population variety, cooperation with stereopsis, and variability among physicians performing the surgery. Cooperation with stereopsis was limited by age. In addition, the Titmus fly has many monocular cues which may have impacted our results. The Frisby or Lang test may be more appropriate for future studies as these do not require the patient to wear polaroid glasses. Krimsky’s test may also be less reliable than APCT in obtaining near and distance deviation measurements in our infantile population. Furthermore, our definition of high AC/A ratio as an increase of ≥10Δ difference between near and distance measurements may be influenced by nonaccommodative convergence excess. This method allowed us to extrapolate data in a retrospective review; however, the gradient method may be more useful in future studies. This study also included all types of ET treated with BMR recessions, and conclusions on specific types of ET may be difficult to formulate.
Conclusion
Our findings support conclusions of other recent literature that patients with a high AC/A ratio are appropriate surgical candidates. They do similarly with surgery compared to those without a high AC/A ratio. Also, the choice of surgery and target angle was to the discretion of one of eight treating surgeons. While most surgeons in our study used a target angle that was aimed at preoperative near deviation, target angle was also slightly associated with preoperative distance deviation. Despite having eight board-certified physicians included in this study, the measurements were done at a single institution with a similar office protocol between patients. A prospective study with pre-designated surgical target angles would be helpful to validate these findings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Von Noorden GK. A reassessment of infantile esotropia. XLIV Edward Jackson memorial lecture. Am J Opthalmol. 1988;105:1–10. doi: 10.1016/0002-9394(88)90113-4. [DOI] [PubMed] [Google Scholar]
- 2.Olitsky SE. High AC/A ratio esotropia:Do we really need to be using bifocals? Am Orthopt J. 2016;66:5–9. doi: 10.3368/aoj.66.1.5. [DOI] [PubMed] [Google Scholar]
- 3.Pratt-Johnson JA, Tillson G. The management of esotropia with high AC/A ratio (convergence excess) J Pediatr Ophthalmol Strabismus. 1985;22:238–42. doi: 10.3928/0191-3913-19851101-09. [DOI] [PubMed] [Google Scholar]
- 4.Havertape SA, Cruz OA, Miyazaki EA. Comparisons of methods for determining the AC/A ratio in accommodative esotropia. J Pediatr Ophthalmol Strabismus. 1999;36:178–83. doi: 10.3928/0191-3913-19990701-05. [DOI] [PubMed] [Google Scholar]
- 5.iÇerman E, Eraslan M, Ögüt MS. The relationship of age when motor alignment is achieved and the subsequent development of stereopsis in infantile esotropia. J AAPOS. 2014;18:222–5. doi: 10.1016/j.jaapos.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 6.Park KA, Oh SY. Esotropia with an accommodative component after surgery for infantile esotropia compared to primary accommodative esotropia. J AAPOS. 2017;21:9–14. doi: 10.1016/j.jaapos.2016.11.021. [DOI] [PubMed] [Google Scholar]
- 7.Fawcett S, Leffler J, Birch EE. Factors influencing stereoacuity in accommodative esotropia. J AAPOS. 2000;4:15–20. doi: 10.1016/s1091-8531(00)90006-5. [DOI] [PubMed] [Google Scholar]
- 8.Li B, Sharan S. Post-operative analysis of pediatric esotropia associated with high hypermetropia. BMC Ophthalmol. 2019;19:140. doi: 10.1186/s12886-019-1149-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whitman MC, MacNeill K, Hunter DG. Bifocals fail to improve stereopsis outcomes in high AC/A accommodative esotropia. Ophthalmology. 2016;123:690–6. doi: 10.1016/j.ophtha.2015.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tejedor J, Gutiérrez-Carmona FJ. Amblyopia in high accommodative convergence/accommodation ratio accommodative esotropia. Influence of bifocals on treatment outcome. Am J Ophthalmol. 2018;191:124–8. doi: 10.1016/j.ajo.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 11.Ludwig IH, Imberman SP, Thompson HW, Parks MM. Long-term study of accommodative esotropia. Trans Am Ophthalmol Soc. 2003;101:155–61. [PMC free article] [PubMed] [Google Scholar]
- 12.Ludwig IH, Parks MM, Getson PR, Kammerman LA. Rate of deterioration in accommodative esotropia correlated to the AC/A relationship. J Pediatr Ophthalmol Strabismus. 1988;25:8–12. doi: 10.3928/0191-3913-19880101-04. [DOI] [PubMed] [Google Scholar]
- 13.Olitsky SE, Chan EW, Farzavandi S. Strabismus:Accommodative Esotropia. 2016. Jan 20, Available from: https://www.aao.org/pediatric-center-detail/strabismus-accommodative-esotropia .
- 14.Arnoldi K, Shainberg M. High AC/A ET:Bifocals? Surgery? Or Nothing at All? Am Orthopt J. 2005;55:62–75. doi: 10.3368/aoj.55.1.62. [DOI] [PubMed] [Google Scholar]
- 15.Arnoldi KA, Tychsen L. Surgery for esotropia with a high accommodative convergence/accommodation ratio:Effects on accommodative vergence and binocularity. Ophthalmic Surg Lasers. 1996;27:342–8. [PubMed] [Google Scholar]
- 16.Kushner BJ. Fifteen-year outcome of surgery for the near angle in patients with accommodative esotropia and a high accommodative convergence to accommodation ratio. Arch Ophthalmol. 2001;119:1150–3. doi: 10.1001/archopht.119.8.1150. [DOI] [PubMed] [Google Scholar]
- 17.Procianoy E, Justo DM. Results of unilateral medial rectus recession in high AC/A ratio esotropia. J Pediatr Ophthalmol Strabismus. 1991;28:212–4. doi: 10.3928/0191-3913-19910701-06. [DOI] [PubMed] [Google Scholar]
- 18.Somer D, Cinar FG, Oral B, Ornek F. Combined recession and resection surgery in the management of convergence excess esotropia with different levels of AC/A ratio. J AAPOS. 2017;21:7.e1–7. doi: 10.1016/j.jaapos.2016.09.029. [DOI] [PubMed] [Google Scholar]
- 19.Lueder GT, Norman AA. Strabismus surgery for elimination of bifocals in accommodative esotropia. Am J Ophthalmol. 2006;142:632–5. doi: 10.1016/j.ajo.2006.05.046. [DOI] [PubMed] [Google Scholar]
- 20.O'Hara MA, Calhoun JH. Surgical correction of excess esotropia at near. J Pediatr Ophthalmol Strabismus. 1990;27:120–5. doi: 10.3928/0191-3913-19900501-04. [DOI] [PubMed] [Google Scholar]
- 21.West CE, Repka MX. A comparison of surgical techniques for the treatment of acquired esotropia with increased accommodative convergence/accommodation ratio. J Pediatr Ophthalmol Strabismus. 1994;31:232–7. doi: 10.3928/0191-3913-19940701-08. [DOI] [PubMed] [Google Scholar]
- 22.Kushner BJ, Preslan MW, Morton GV. Treatment of partly accommodative esotropia with a high accommodative convergence-accommodation ratio. Arch Ophthalmol. 1987;105:815–8. doi: 10.1001/archopht.1987.01060060101042. [DOI] [PubMed] [Google Scholar]


