Abstract
A 35-year-old male patient presented with blurring and black spots in vision after 1 month of the second dose of Covishield vaccination. His visual acuity was 6/6; both eyes and anterior and posterior segment examinations were normal. The optical coherence tomography (OCT) showed multiple hyperreflective lesions involving the nerve fiber layer with back shadowing. In addition, there were hyperreflective spots in the ganglion cell layer and outer plexiform layer with focal loss of external limiting membrane and an intact inner segment/outer segment junction involving the posterior pole in both eyes. The patient was diagnosed with paracentral acute middle maculopathy (PAMM) and acute macular neuroretinopathy (AMN) and advised observation. PAMM and AMN are unreported manifestations following the COVID-19 vaccination.
Keywords: Acute macular neuroretinopathy, paracentral acute middle maculopathy, post-covid vaccination, retinopathy
Paracentral acute middle maculopathy (PAMM) is a spectral-domain optical coherence tomography (SD-OCT) manifestation presenting with hyper-reflective band-like lesions involving the outer plexiform layer/inner nuclear layer (OPL/INL) junction resulting in permanent INL thinning.[1] Acute macular neuroretinopathy (AMN) is characterized by intraretinal, reddish-brown, wedge-shaped lesions; the apices of which tend to point toward the fovea hyper-reflective plaque between the outer plexiform and outer nuclear layers with disruption of ellipsoid zone/interdigitation zone. Various vascular pathologies have been associated with PAMM and AMN, including post-viral illness, vasoconstrictive agents, trauma, hypovolemic shock, anemia, thrombocytopenia, and hyperviscosity.[2,3] The diagnosis is based on the history and the OCT changes.
PAMM and AMN have been reported with SARS-CoV-2 infection and possibly represent post-infectious complications.[4] We report a case of bilateral PAMM and AMN following the COVID 19 vaccination.
Case Report
A 34-year-old male presented with blurring of vision, black spots in vision, and reduced brightness of vision in both eyes for 4 weeks. The patient had the first dose of SARS-CoV-2 vaccination (Covisheild). Following the first dose, the patient noticed a mild blurring of vision. After 4 weeks, he received his second dose of vaccination and noticed the visual symptoms of reduced brightness sensitivity in both eyes progressed further. On examination, his unaided vision was 6/6 in both eyes. The contrast sensitivity using the Pelli Robson chart was normal, and Amsler’s grid test and visual fields test were normal with no evidence of scotoma. The photo stress recovery test was within normal limits for both eyes.
The anterior segment examination was unremarkable in both eyes. The posterior segment evaluation revealed a normal fundus examination [Fig. 1].
Figure 1.
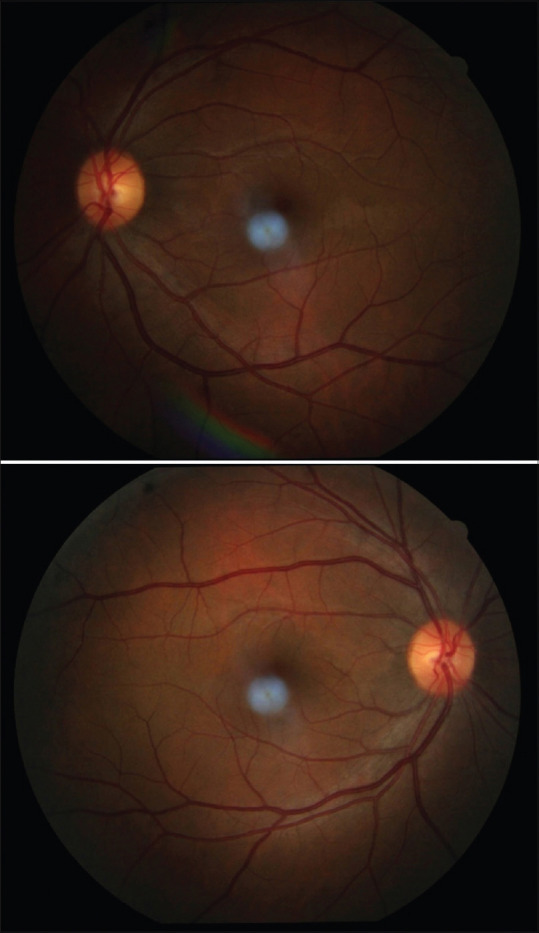
Fundus image of both eyes
The patient underwent a complete neurological examination. The magnetic resonance imaging (MRI) of the brain and MR-angiography were normal. Visual-evoked potential (VEP) showed normal P100 latency with normal NPN complex amplitude in both eyes. His blood investigations, including complete blood counts, C-reactive protein, were normal. His RT-PCR for COVID-19 was negative. The OCT macula revealed normal foveal contour with hyperreflective lesions involving the nerve fiber layer with back shadowing [Fig. 2a and b]. There were multiple small hyperreflective spots within the ganglion cell layer and faint outer plexiform layer hyperreflective changes with focal loss of external limiting membrane and intact IS/OS junction in both the eyes. All these changes were localized to the area between the retinal arcades, hence, limited to the posterior pole. These lesions on the OCT could not be correlated with any gross findings on fundus examination. The fundus auto-fluorescence revealed a normal pattern [Fig 3]. The patient was diagnosed with bilateral PAMM and AMN and was advised observation.
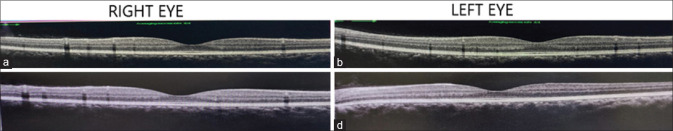
Figure 2.
(a and b) OCT of the right and left eye respectively showing normal foveal contour with hyperreflective lesions in nerve fiber and ganglion cell retinal layers causing shadowing in underlying retina. There were multiple small hyperreflective spots within the ganglion cell layer and faint outer plexiform layer hyperreflective changes with focal loss of external limiting membrane and intact IS/OS junction. (c and d) OCT of the right and left eye, respectively three weeks after observation. There is a reduction of size and number of hyperreflective lesions and thinning of the outer nuclear layer
Figure 3.
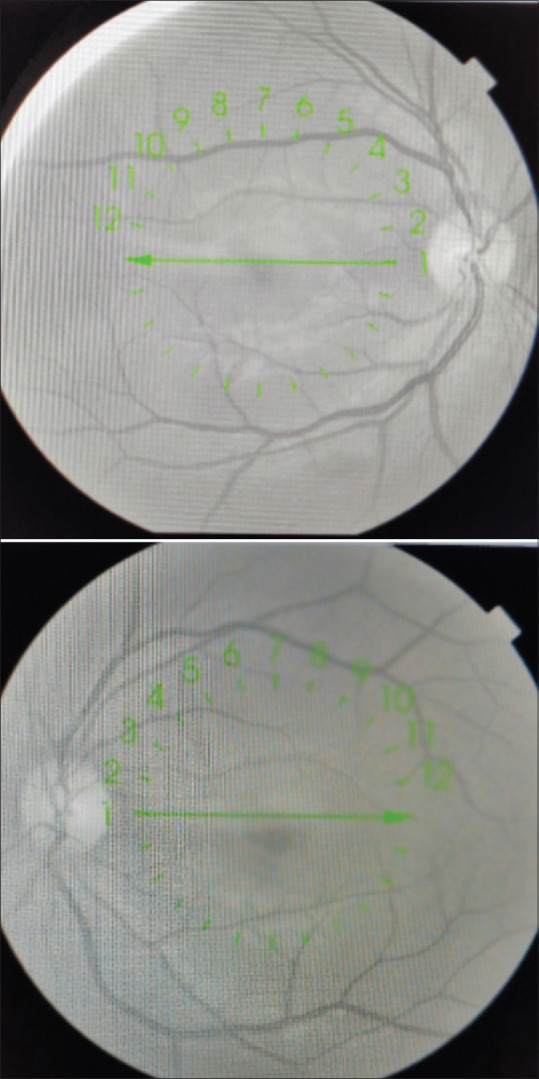
Autofluorescence images
We re-examined the patient after 3 weeks. Symptomatically. he reported slight improvement of brightness sensitivity but still complained of black spots in his central field of vision. On examination, his vision was 6/6 in both eyes. His Amsler’s grid charting was also normal. The OCT macula revealed a significant reduction in the number and size of the hyperreflective lesions noted in the nerve fibre and ganglion cell layers. There was also a reduction in the thickness of the outer nuclear layer in both eyes [Fig. 2c and d].
Discussion
The SARS-CoV-2 infection can present with various ocular manifestations ranging from mild conjunctivitis to posterior ischemic optic neuropathy.[5]
Bilateral PAMM and AMN have been reported following the SARS COV-2 infection. The manifestations are due to vascular, inflammatory, and neuronal changes triggered by the viral infection. The Covishield vaccine (recombinant, replication-deficient chimpanzee adenovirus vector encoding the SARS-CoV-2 Spike [S] glycoprotein) has been reported with mild side effects such as pain, fatigue, headache, joint pain, flu-like symptoms, and decreased appetite. Voysey et al.[6] in their study reported two cases of uveitis, probably immunologically-mediated but did not report any vasculitis-related side effects. No ocular side effects have been reported so far following vaccination.
Our case had similar findings as reported by Bhavsar et al.[2] in their study, where cases of AMN presented with acute symptomatic photopsia and paracentral scotomas with only mild visual loss. As reported in their case series, the fundus autofluorescence was unremarkable, and our case had hyperreflectivity in the outer plexiform layer. In our case, the focal hyperreflective lesions are less confluent than the lesions observed in the reported cases of both PAMM and AMN, thus, indicating an involvement of both the inner and outer parts of the retina on OCT with sparing of the ellipsoid zone.
The temporal association between the acute ocular symptoms that the patient developed immediately following vaccination and the laboratory investigations that excluded other infections, immunologic and hypercoagulable states, and his MRI and VEP being normal, point toward an association between SARS-CoV-2 vaccination and the ocular symptoms. The findings of PAMM and AMN in our patients are similar to the cases reported following a viral illness or following the H1N1 vaccination or influenza vaccination.[7,8] Though the etiology of PAMM and AMN remains incomplete, there is a possible microvascular pathology affecting the deep capillary plexus. It is possible that small vessel vasculitis induced by vaccination resulted in these findings. Hence, we hypothesize that the vasculitis changes may have led to the ischemia of the deep capillary plexus presenting as PAMM and AMN in our patient.
Conclusion
We report a unique presentation of bilateral paracentral acute middle maculopathy and acute macular neuroretinopathy following the SARS-CoV-2 vaccination that has not been described previously.
The case highlights the recent SARS-CoV-2 vaccine as a possible cause for bilateral PAMM And AMN in the form of a rare adverse effect. However, the association needs to be studied more and considered one of the SARS-CoV-2 vaccine-related ocular manifestations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rahimy E, Kuehlewein L, Sadda SR, Sarraf D. Paracentral acute middle maculopathy:What we knew then and what we know now. Retina. 2015;35:1921–30. doi: 10.1097/IAE.0000000000000785. [DOI] [PubMed] [Google Scholar]
- 2.Bhavsar KV, Lin S, Rahimy E, Joseph A, Freund KB, Sarraf D, et al. Acute macular neuroretinopathy:A comprehensive review of the literature. Surv Ophthalmol. 2016;61:538–65. doi: 10.1016/j.survophthal.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 3.Munk MR, Jampol LM, Cunha Souza E, de Andrade GC, Esmaili DD, Sarraf D, et al. New associations of classic acute macular neuroretinopathy. Br J Ophthalmol. 2016;100:389–94. doi: 10.1136/bjophthalmol-2015-306845. [DOI] [PubMed] [Google Scholar]
- 4.Virgo J, Mohamed M. Paracentral acute middle maculopathy and acute macular neuroretinopathy following SARS-CoV-2 infection. Eye. 2020;34:2352–3. doi: 10.1038/s41433-020-1069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nasiri N, Sharifi H, Bazrafshan A, Noori A, Karamouzian M, Sharifi A. Ocular Manifestations of COVID-19:A Systematic Review and Meta-analysis. J Ophthalmic Vis Res. 2021;16:103–12. doi: 10.18502/jovr.v16i1.8256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2:An interim analysis of four randomized controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397:99–111. doi: 10.1016/S0140-6736(20)32661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu JC, Nesper PL, Fawzi AA, Gill MK. Acute macular neuroretinopathy associated with influenza vaccination with the decreased flow at the deep capillary plexus on OCT angiography. Am J Ophthalmol Case Rep. 2018;10:96–100. doi: 10.1016/j.ajoc.2018.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah P, Zaveri JS, Haddock LJ. Acute macular neuroretinopathy following the administration of an influenza vaccination. Ophthalmic Surg Lasers Imaging Retina. 2018;49:e165–8. doi: 10.3928/23258160-20181002-23. [DOI] [PubMed] [Google Scholar]