ABSTRACT
Emergence of SARS-CoV-2 with high transmission and immune evasion potential, the so-called variants of concern (VOC), is a major concern. We describe the early genomic epidemiology of SARS-CoV-2 recovered from vaccinated health care professionals (HCP). Our postvaccination COVID-19 symptoms-based surveillance program among HCPs in a 17-hospital network identified all vaccinated HCPs who tested positive for COVID-19 after routine screening or after self-reporting. From 1 January 2021 to 30 April 2021, 23,687 HCPs received either mRNA-1273 or BNT162b2 mRNA vaccine. All available postvaccination SARS-CoV-2 samples and a random collection from nonvaccinated patients during the similar time frame were subjected to VOC screening and whole-genome sequencing (WGS). Sixty-two percent (23,697/37,500) of HCPs received at least one vaccine dose, with 60% (22,458) fully vaccinated. We detected 138 (0.58%, 138/23,697) COVID-19 cases, 105 among partially vaccinated and 33 (0.15%, 33/22,458) among fully vaccinated. Five partially vaccinated required hospitalization, four with supplemental oxygen. VOC screening from 16 fully vaccinated HCPs identified 6 (38%) harboring N501Y and 1 (6%) with E484K polymorphisms; percentage of concurrent nonvaccinated samples was 37% (523/1,404) and 20% (284/1,394), respectively. There was an upward trend from January to April for E484K/Q (3% to 26%) and N501Y (1% to 49%). WGS analysis from vaccinated and nonvaccinated individuals indicated highly congruent phylogenies. We did not detect an increased frequency of any receptor-binding domain (RBD)/N-terminal domain (NTD) polymorphism between groups (P > 0.05). Our results support robust protection by vaccination, particularly among recipients of both doses. Despite VOCs accounting for over 40% of SARS-CoV-2 from fully vaccinated individuals, the genomic diversity appears to proportionally represent VOCs among nonvaccinated populations.
IMPORTANCE A number of highly effective vaccines have been developed and deployed to combat the COVID-19 pandemic. The emergence and epidemiological dominance of SARS-CoV-2 mutants with high transmission potential and immune evasion properties, the so-called variants of concern (VOC), continue to be a major concern. Whether these VOCs alter the efficacy of the administered vaccines is of great concern and a critical question to study. We describe the initial genomic epidemiology of SARS-CoV-2 recovered from partial/fully vaccinated health care professionals and probe specifically for VOC enrichment. Our findings support the high level of protection provided by full vaccination despite a steep increase in the prevalence of polymorphisms associated with increased transmission potential (N501Y) and immune evasion (E484K) in the nonvaccinated population. Thus, we do not find evidence of VOC enrichment among vaccinated groups. Overall, the genomic diversity of SARS-CoV-2 recovered postvaccination appears to proportionally represent the observed viral diversity within the community.
KEYWORDS: SARS-CoV-2, variants of concern, vaccine, breakthrough, spike protein, COVID-19
INTRODUCTION
Since the beginning of the pandemic in 2020, SARS-CoV-2 has infected and spread within an immunologically naive global population (1, 2). With the application of convalescent plasma and therapeutic antibody treatment, along with highly effective vaccines, the virus is now starting to experience the immune pressure that will ultimately shape its evolutionary trajectory (3). Recent evidence indicates that SARS-CoV-2 can mutate and evade immunity and challenge the efficacy of emerging vaccines and intrinsic and extrinsic antibodies (i.e., natural by infection and antibody therapeutics) (3, 4).
The reports of mutants, known as variants of concerns (VOCs), that exhibit increased transmission or immune evasion, or both, have been reported in different global regions, and predominant lineages have been genotyped (5). Of note, three VOCs, B.1.1.7 (recently named Alpha) (6), B.1.351 (Beta) (7), and P.1 (Gamma) (8) containing prominent mutations in the spike protein emerged in the United Kingdom, South Africa, and Brazil, respectively, and more recently, B.1.617.2 (Delta) (9) emerged in India and has spread to dominate the global SARS-CoV-2 population. The mapping of specific mutations in the spike protein has revealed strong evidence of convergent evolution and particularly the E484K polymorphism, which is able to evade certain monoclonal therapy and is less responsive to neutralizing antibodies from recovered patients. This mutant shows reduced response to convalescent plasma and reported reinfections, and it has been identified in discrete lineages in different geographic locations and associated with variant clones with increased incidence (4). The impact of these antibody escape mutants harboring VOCs on driving community incidence and whether they alter the efficacy of the administered vaccines are of great concern.
In this report, we describe the initial genomic epidemiology of SARS-CoV-2 recovered from partially and fully vaccinated health care professionals (HCPs) within a large health care network in New Jersey. We specifically probe whether specific SARS-CoV-2 variants skew viral diversity indicative of vaccine-induced selection and compare against a random collection of SARS-CoV-2 recovered from nonvaccinated individuals during the same time period. Although we find steep increases in variants harboring E484K and N501Y among community samples, our early genomic assessment does not indicate specific variant enrichment among postvaccinated individuals. We find that viral genomes among vaccinated individuals largely reflect the viral diversity among nonvaccinated populations.
RESULTS
COVID-19 postvaccination surveillance program: demographic and clinical characteristics of COVID-19 cases.
From December 2020 to April 2021, 23,697 of 37,500 HCPs (62%) received at least one dose of an mRNA vaccine, and 22,458 (60%, 22,458/37,500) received both vaccine doses. Among vaccinated HCPs, 12,878 (54%) received mRNA-1273 (Moderna) and 10,819 (46%) received BNT162b2 (Pfizer/BioNTech) mRNA COVID-19 vaccine. Of the 23,697 vaccinated (single and both doses) HCPs, our surveillance program detected 138 (0.58%, 138/23,697) COVID-19 cases; 105 of these were among HCPs who received only one dose and 33 (0.15%, 33/22,458) were among those with both doses.
Among the 138 postvaccinated COVID-19 cases, 74 were vaccinated with the Pfizer/BioNTech vaccine and 64 were vaccinated with the Moderna preparation. Cases were reported from nine hospitals. Demographic information was not available for 17 employees. Of the remaining 121 employees, most cases were white (68%) and female (74%) with a median age of 45 (ranging from 19 to 77). Twenty-one employees (17%) were documented to have asymptomatic infection. Of those that were symptomatic, five individuals requiring hospitalization received only one dose and had recorded body mass index (BMI) of >25 (4 individuals with BMI of >30) and four of these patients required supplemental oxygen. The majority of the infections, 76% (105/138), occurred from 1 to 113 days after the initial dose with a median of 10 days, while 23% (33/138) occurred 4 to 104 days after the second dose with a median of 22 days. Among the 33 who had received two doses, 20 individuals (61%) were considered fully vaccinated and considered vaccine breakthrough infections.
Screening of postvaccinated SARS-CoV-2 infections indicates the rise in E484K and N501Y variants.
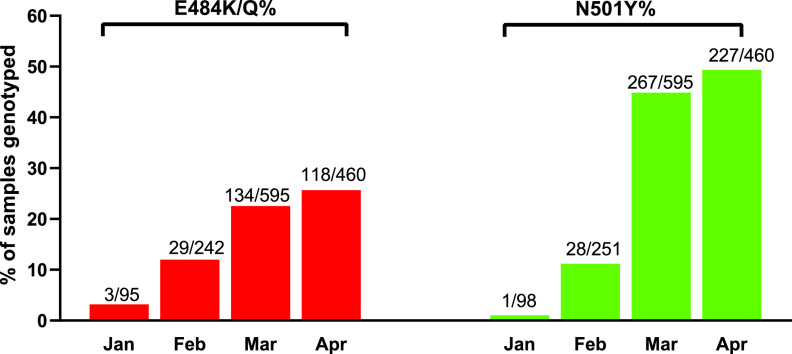
To further characterize the SARS-CoV-2 genotypes recovered from the postvaccinated individuals, we examined the spread of key mutations underlying VOCs (i.e., B.1.1.7) in New Jersey using a high-throughput molecular beacon assay designed to screen for polymorphisms N501Y/T and E484K/Q in the receptor-binding domain (RBD) region (10). Among 138 HCPs, 83 swabs were available for rapid screening providing 76 genotypic results (60 from partially and 16 from fully vaccinated). There were 3 and 6 viral samples with E484K and N501Y polymorphisms, respectively (Fig. 1). Among 16 fully vaccinated HCPs, we found 1 (6.3%) and 6 (38%) samples with E484K and N501Y mutations, respectively.
FIG 1.
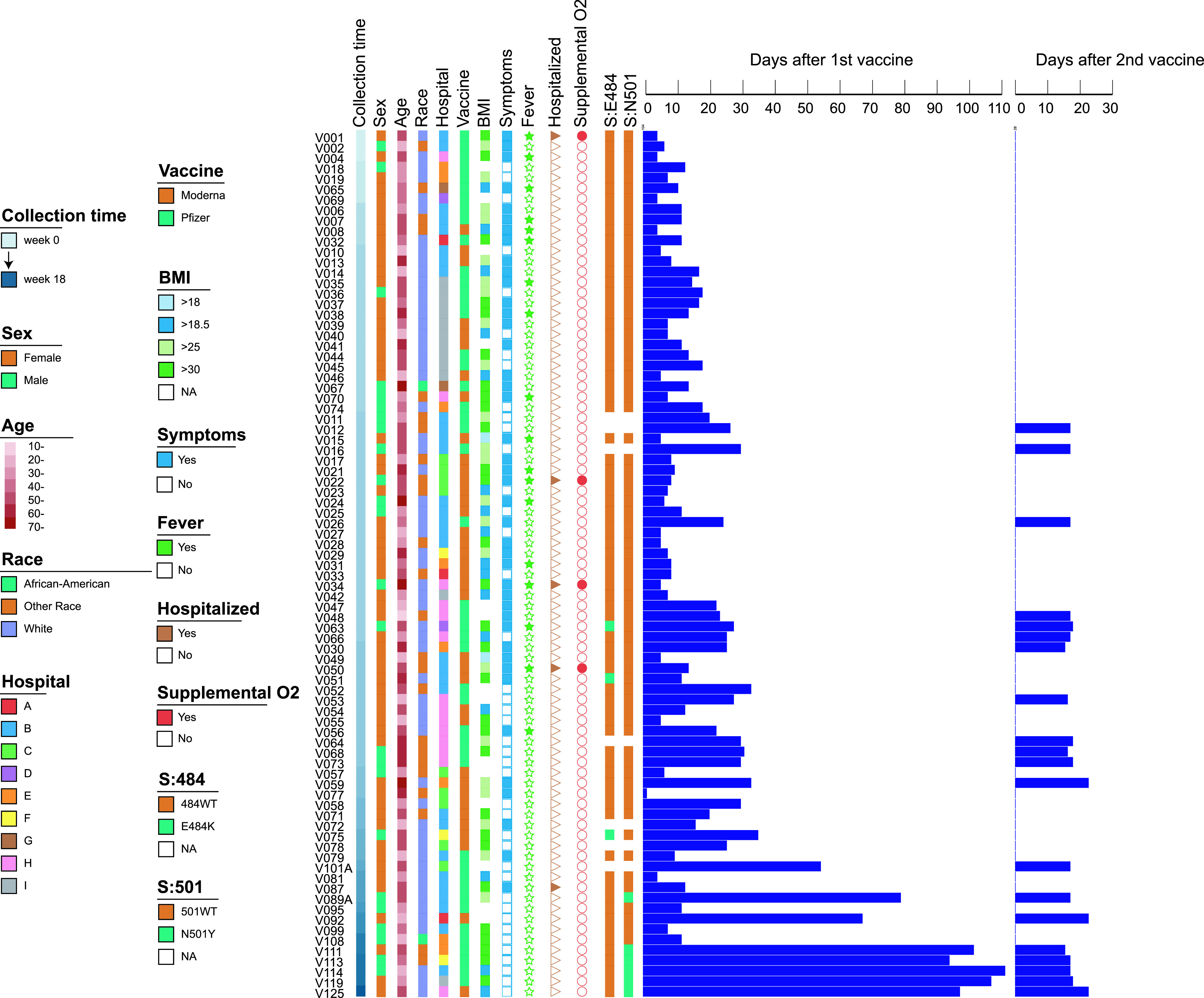
Clinical characteristics of 83 COVID-19-vaccinated HCPs and their SARS-CoV-2 S protein E484 and N501 genotypes. The samples were ordered by the time of diagnosis, with the first case detection week denoted as “0”. The swab collection time is denoted as a gradient color bar, while sex (male and female), age (>10 to >70), race (African-American, White, and other), hospital (A to I), vaccine type (Pfizer and Moderna), BMI (>18 to >30), and the SARS-CoV-2 S protein 484 and 501 mutations are shown as color boxes. The presence or absence of symptoms, fever, hospitalization, and supplemental O2 treatment are illustrated as binary color boxes (Yes or No). The days after the 1st and 2nd vaccine are illustrated as color bars in the right panel.
To contextualize the prevalence of E484K and N501Y mutations among the nonvaccinated population, we sampled 1,404 from a total of 3,000 SARS-CoV-2-positive swabs (47%), representing every other positive COVID-19 swab, from January 2021 to April 2021 within our hospital network. Overall, we detected 284 E484K/Q (284/1,392, 20.4%; 12 samples failed in the E484 detection in comparison with N501Y) and 523 N501Y (523/1,404, 37.3%) mutants (Fig. 2). The prevalence of E484K/Q and N501Y from January to April was 3.2% to 25.7% and 1.0% to 49.3%, respectively (Fig. 2).
FIG 2.
Prevalence of E484K/Q and N501Y mutants among SARS-Cov-2 samples from nonvaccinated individuals from January to April 2021.
SARS-CoV-2 from vaccinated individuals is diverse and does not indicate predominant genotypes or genetic characteristics.
To understand the population structure of SARS-CoV-2 postvaccination, we first analyzed whole-genome sequencing (WGS) data for 68 available SARS-CoV-2 isolates from 83 symptomatic COVID-19 cases included in this study. WGS failed for 15 samples with high cycle threshold (Ct) values (Ct values ranging from 33 to 38), suggestive of low viral burden. We specifically probed whether specific variants or mutations were overrepresented among SARS-CoV-2 recovered from partially and fully vaccinated individuals. The 68 genomes were divided into 21 different Pangolin lineages with B.1.2 the most common (24/68, 35%) (Fig. 3). We noted distinct amino acid changes or deletions at 20 sites within the N-terminal domain (NTD) or receptor-binding domain (RBD) regions of the spike protein. Mutations associated with antibody evasion—L452R, T478K, E484K, and S494P—were found in 3, 1, 3, and 2 genomes, respectively. We did not detect any genomes with more than two of the four polymorphisms. The N501Y mutation was found in 4% (3/68) of the genomes, and all belonged to the VOC B.1.1.7 lineage. We recorded 3 viral samples harboring the E484K mutation, two belonging to the B.1.526 lineage first identified in New York (11, 12) and one from the R.1 lineage. Importantly, among the 9 individuals fully vaccinated (i.e., ≥14 days post-second dose), with available molecular data we note 1 and 2 samples harboring E484K and N501Y polymorphisms, respectfully. There were no samples from fully vaccinated HCPs with both E484K and N501Y.
FIG 3.
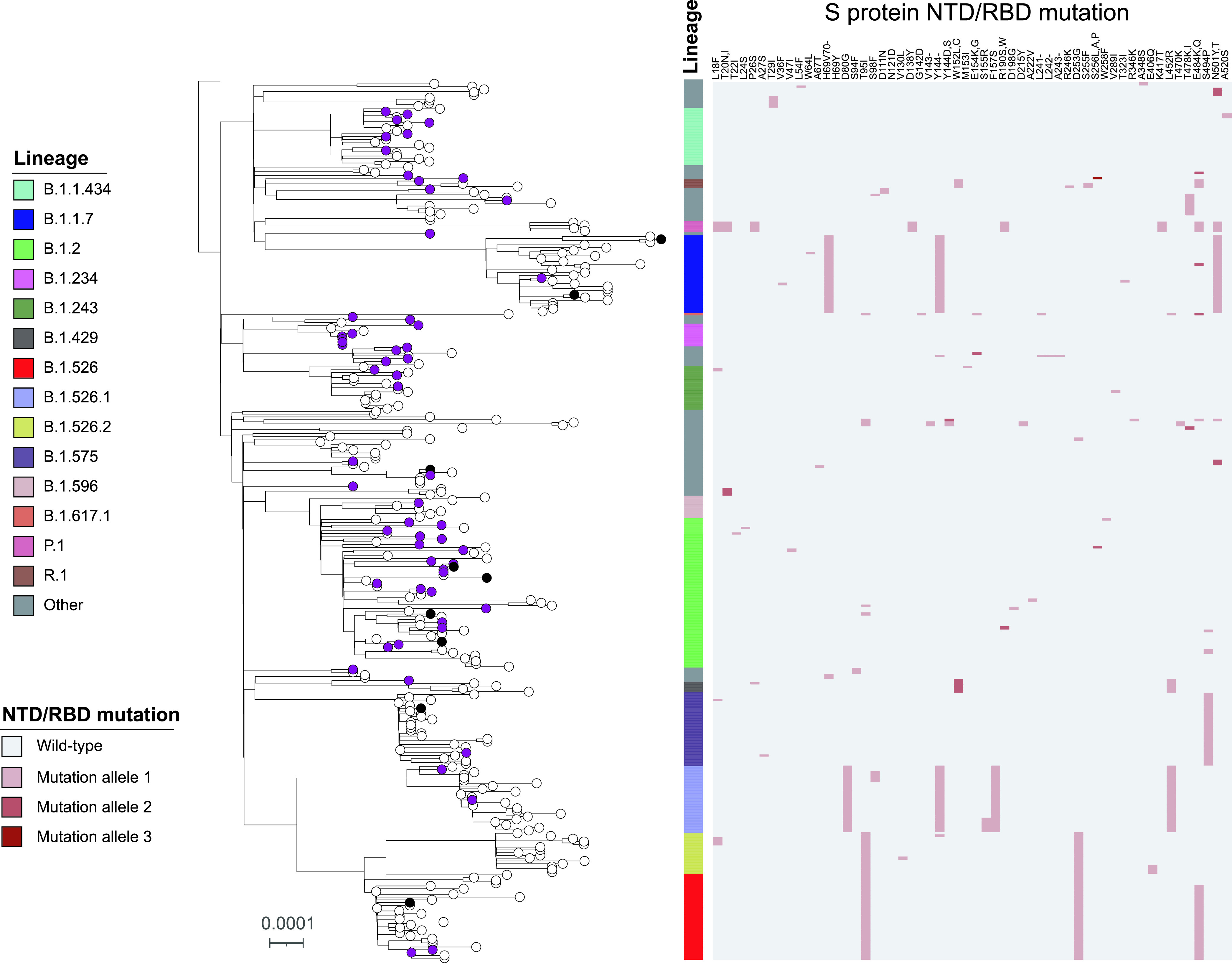
Maximum-likelihood phylogenetic tree of 349 SARS-CoV-2 genomes isolated from vaccinated and nonvaccinated populations. The tree is rooted to the SARS-CoV-2 Wuhan-Hu-1 reference genome (NC_045512.2). The scale represents 0.0001 nucleotide substitutions per site. The vaccination conditions are color coded at the tree tips: purple, black, and white tips denote single dose, fully vaccinated, and nonvaccinated, respectively. The SARS-CoV-2 Pangolin lineage is illustrated as a color bar, and the S protein NTD/RBD mutations are shown as a heatmap on the right panel. The S protein NTD/RBD amino acid changes are shown on the column labels in the heatmap, and different mutation alleles are separated by a comma if more than one allele is detected at the same site.
To compare viral diversity from vaccinated (partial and full) and nonvaccinated individuals, we randomly selected 281 SARS-CoV-2 samples recovered from nonvaccinated patients within the Hackensack Meridian Health (HMH) network during the same time period for genomic characterization by WGS (Fig. 3). Among them, 38 different Pangolin lineages were identified, including 18 lineages found in the vaccinated population. B.1.526 (n = 33) and its sublineages (B.1.526.1, n = 26, and B.1.526.2, n = 15) were the most common (74/281, 26.3%), followed by B.1.2 (35, 12.5%), B.1.1.7 (28, 10%), and B.1.575 (26, 9.3%). In addition, 5 P.1 (20J/501Y.V3) and 1 B.1.617.1 (Kappa) were found among the 281 samples. Mutations or deletions were detected in 54 sites within the S protein RBD or NTD region, including 18 sites found in the vaccinated samples. L452R, T478K/I, E484K/Q, and S494P mutations were identified in 32, 8, 40, and 29 genomes, respectively. Compared with that among the nonvaccinated samples, we did not detect a significant increase in the frequency of any RBD/NTD mutations or deletions among the (partially and fully) vaccinated group (P > 0.05).
DISCUSSION
Rapid expansion and contraction of SARS-CoV-2 populations coupled with increasing anti-CoV-2 immunity dynamics have contributed to pandemic phases accompanied by emergent genomic signatures (1, 13). Extensive polymorphisms in the spike protein have been documented, including N501Y and E484K mutations that are particularly concerning (14). In this report, we present early genomic analysis of SARS-CoV-2 from an ongoing postvaccination COVID-19 surveillance program among HCPs in New Jersey.
We detected SARS-CoV-2 in 33 (0.15%) HCPs who were fully vaccinated, none of whom required hospitalization. All symptomatic cases were noted among partially vaccinated HCPs and were self-limiting, with only 5 requiring hospitalization. Although our passive surveillance system was intended to capture the HCP vaccinated population who self-reported symptoms or who were exposed to a COVID-19-positive case, and not able to report true prevalence of infections (i.e., mild or asymptomatic infections may be missed), our findings are consistent with emerging reports of incidents of postvaccination SARS-CoV-2 infections (15–18). A recent multicenter prospective cohort study in England found vaccine effectiveness upwards of 85% (19). Our results support high levels of protection afforded by vaccination, particularly among recipients of both doses (9, 15, 20–24). The majority of cases in our study were among partially vaccinated individuals, emphasizing the importance of personal protective measures and susceptibility to infection particularly until fully vaccinated (19, 24–27).
Steep transmission gradients reported locally and regionally have been partly attributed to VOCs, including B.1.1.7 in Europe and United States, P.1 in Brazil, B.1.351 in South Africa, B.1.617.2 in India, and B.1.526 in New York State (6–8, 11, 28). Although the pathogen characteristics attributable to the spread of these variants at the population level are difficult to assess, mathematical modeling, genomic, and experimental studies have demonstrated increased transmissibility and immune evasion properties, including reduced vaccine-induced antibody neutralization in vitro (2, 3, 6, 14). Whether the rollout of vaccination would offer selective advantage to VOCs is a critical question to determine.
A recent study from Washington State found that all SARS-CoV-2 vaccine breakthroughs were VOCs. Of significance, those VOCs harboring immune evasion properties (B.1.351, B.1.427, B.1.429, and P1) were enriched compared to B.1.1.7 lineages among vaccine breakthrough cases and among cases in the general population (29). Other outbreaks have been reported among vaccinated individuals implicating SARS-CoV-2 strains harboring E484K, a noted immune evasion-conferring polymorphism (20). A recent study where two VOCs (B.1.351 and B.1.1.7) dominate the viral population indicates reduced vaccine effectiveness against both variants at specific time windows. Reduced effectiveness against B.1.351 at least 7 days after the second BNT162b2 dose and against B.1.1.7 between 2 weeks after the first dose and 6 days after the second dose were reported (24). However, among fully vaccinated HCPs, the VOC proportions between cases and controls were comparable, consistent with our findings. These studies reinforce the need to fully vaccinate to achieve high levels of protection afforded by vaccination (9).
In our study, despite an increasing trend in the proportion of N501Y and E484K variants in the overall population (Fig. 2), we do not find early evidence of genotypic enrichment of polymorphisms within the NTD or RBD region of the spike protein gene among our fully vaccinated HCPs. Although 44% of the strains recovered from fully vaccinated HCPs harbored mutations of concern (6 N501Y and 1 E484K), they were similar in proportion to strains circulating in the community during the same time period. Our WGS analysis suggests that N501Y-harboring strains belong to the B1.1.7 lineage and the E484K mutants to the B.1.526 lineage, both highly prevalent lineages in the Northeastern United States (12, 30). All N501Y mutants were detected among fully vaccinated HCPs, half of which failed to generate WGS data due to higher Ct values, a likely consequence of vaccination (31). We acknowledge that community samples recovered from nonvaccinated individuals may not represent an ideal comparator group (versus samples from vaccinated individuals) since they are not necessarily from the same source population. Therefore, our results may be subject to selection bias. However, our results are highly congruent with local and regional genomic epidemiology of SARS-CoV-2, lending credence to our findings (12, 30).
A recent report showed that B.1.1.7 upregulates key innate immune antagonists likely increasing the transmission potential of this VOC (32). Interestingly, mRNA vaccines have shown high levels of efficacy against B.1.1.7 infections (22). Overall, the genomic diversity of SARS-CoV-2 recovered postvaccination appears to proportionally represent the observed viral diversity within the community. We acknowledge that our estimates may be skewed by undersampling of asymptomatic infections among fully vaccinated individuals (33) and are likely affected by test-seeking behavioral bias (24). However, our results are consistent with those from a large nationwide surveillance program of COVID-19 vaccine breakthrough infections that found the proportion of reported vaccine breakthrough infections attributed to VOCs to be similar to the proportion of these variants circulating throughout the United States (27).
There is mounting evidence that currently available vaccines, including those used in our population, are highly effective against VOCs. The reports of VOC enrichment among postvaccinated individuals, despite small sample sizes, warrant surveillance. Our study findings are preliminary yet highlight the importance of full vaccination against circulating variants, including VOCs, such as Delta (14), and the need to continue SARS-CoV-2 genomic surveillance as vaccination coverage expands, pathogen evolves, and immunity wanes.
MATERIALS AND METHODS
Postvaccination COVID-19 surveillance program.
Since the first mRNA vaccines were administered in December 2020 among the 37,500 HMH health care professionals (i.e., employees working within the hospital network with direct or indirect patient contact or supportive administrative roles), we initiated a symptoms-based surveillance program to identify and report the status of each vaccinated person in the electronic medical record (EMR). This regularly updated list was cross-referenced daily against the results of all SARS-Cov-2 nucleic acid amplification tests (NAAT) in the HMH network. As a result, we were able to identify all vaccinated employees who tested positive for COVID-19 by NAAT after routine screening or after reporting out sick. Non-team members who were vaccinated at our mass-vaccination site or by physician report (and were thus in the HMH EMR) and subsequently tested positive for COVID-19 by NAAT were also similarly identified. The study was approved by Hackensack Meridian Health Institutional Review Board (IRB).
Whole-genome sequencing and phylogenetic analysis.
SARS-CoV-2 targeted assay libraries were prepared using the Molecular Loop viral RNA target capture kit (Molecular Loop) or QIAseq FX DNA Library UDI kit (Qiagen), in accordance with the manufacturer’s recommendations. Final libraries were quantified using fluorescent-based assays, including PicoGreen (Life Technologies), Qubit Fluorometer (Invitrogen), and Fragment Analyzer (Advanced Analytics). Final libraries were sequenced on a NovaSeq 6000 sequencer (v1 chemistry) with 2 × 150 bp.
For QIAseq libraries, read pairs that did not contain a single 19-bp seed k-mer in common with the SARS-CoV-2 genome reference (NC_045512.2) were discarded. Adapter sequences and low-quality bases (Q < 20) were trimmed from the 3′ end of the remaining reads using Cutadapt v2.10 (34). Sequences corresponding to the amplicon primers were also clipped from the 5′ end of reads. Processed read pairs were then aligned to the SARS-CoV-2 reference genome using BWA-MEM v0.7.17 (35), and only read pairs with at least one alignment spanning a minimum of 50 bp in the reference were kept.
For Molecular Loop libraries, the two 5-bp unique molecular identifiers (UMIs) located at the 5′ end of each mate were first clipped and combined into a single UMI tag. Additional 25 bp, corresponding to the molecular inversion probes, were also clipped from the 5′ end of each read. Next, read pairs that did not contain a single 19 bp seed k-mer in common with the SARS-CoV-2 genome reference (NC_045512.2) were discarded and adapter sequences and low-quality bases (Q < 20) were trimmed from the 3′ end of the remaining reads, using Cutadapt v2.10 (34). Processed reads pairs were then merged using NGmerge v0.2 (36), allowing for dovetailed alignments. The resulting single-end reads were mapped against the SARS-CoV-2 genome reference using BWA-MEM v0.7.17 (35) and the resulting alignments filtered using the following criteria: (i) reference span of ≥50 bp, (ii) quality of ≥60, and (iii) maximum soft-clip length on either end of ≤30 bp. Next, reads representing the same original molecule were identified based on their shared UMI and alignment position and used to draw the molecule consensus sequence, taking into account base quality scores. Molecule sequences were then realigned to the SARS-CoV-2 genome reference using BWA-MEM v0.7.17 (35). Finally, genome sequences were determined either by read (QIAseq) or molecule (Molecular Loop) alignment pileup consensus calling with a minimum support of 5 reads/molecules.
The resulting SARS-CoV-2 viral genome sequences were characterized by Nextclade CLI (v1) (https://clades.nextstrain.org/) to assign Nextstrain clades (37). SARS-CoV-2 lineages were determined using Pangolin v3.1.3 (https://github.com/cov-lineages/pangolin), and GISAID clades were determined based upon the clade-specific marker variants from https://www.gisaid.org (38). The genomes were aligned using nextalign v1.0.0 (https://github.com/neherlab/nextalign) using the default setting. A maximum-likelihood phylogenetic tree was constructed using IQ-TREE v2.1.2 (39) with automatic model selection and 1,000-bootstrap replicates. The resulting tree was annotated using ITOL v6 (40).
Population sampling and screening of SARS-CoV-2.
SARS-CoV-2-positive swabs collected from seven HMH network hospitals were shipped to CDI on a weekly basis and stored at −80°C. From a total of 3,000 swabs collected during the same time frame, 1,404 swabs were selected representing every other sample in the collection. These samples were subjected to a molecular beacon-based real-time asymmetric PCR and melting curve analysis to identify the SARS-CoV-2 E484K/Q and N501Y mutations, as described previously (10). In brief, 50-μl aliquots of SARS-CoV-2 swab specimens were treated by proteinase K and heated at 95°C for 5 min. A total of 5 μl of heat-inactivated sample was used as the template for the asymmetric real-time PCR (RT-PCR) testing on a Mic Real Time PCR Cycler (Bio Molecular Systems, software micPCRv2.8.13). Based on the different melting profiles (Tm) of E484 and N501 molecular beacons in each sample, the E484K and N501Y mutations were determined.
Definitions.
We define vaccinated as receiving at least one dose of SARS-CoV-2 vaccine. Postvaccination SARS-CoV-2 is defined as having a positive RT-PCR test result after 1st or 2nd doses. Partially vaccinated refers to individuals who have not completed the recommended dosing regimen (e.g., only 1 of two mRNA doses). Fully vaccinated refers to individuals ≥14 days after receiving both recommended mRNA vaccine doses. Finally, vaccine breakthrough is defined as detection of SARS-CoV-2 RNA in a respiratory specimen collected from a person ≥14 days after they have completed all recommended doses of a U.S. Food and Drug Administration (FDA)-authorized COVID-19 vaccine.
Statistical analysis.
Fisher’s exact or chi-square tests, as appropriate, were used to examine whether the spike protein NTD/RBD mutations were enriched in the vaccinated HCPs (n = 68) in comparison with those in the nonvaccinated patients (n = 281). SPSS version 17.0 (IBM Corp., Armonk, NY) was used for statistical analyses, and two-tailed P values of ≤0.05 were considered statistically significant.
Data availability.
The SARS-CoV-2 genomes sequenced in this study were deposited in GISAID (https://www.gisaid.org). Sequences can be accessed by searching records from both the originating lab at Hackensack Medical Center and the submitting lab at the New York Genome Center.
Contributor Information
Barry N. Kreiswirth, Email: Barry.Kreiswirth@hmh-cdi.org.
S. Wesley Long, Houston Methodist Hospital
REFERENCES
- 1.Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. 2020. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science 368:860–868. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hodcroft EB, Zuber M, Nadeau S, Vaughan TG, Crawford KHD, Althaus CL, Reichmuth ML, Bowen JE, Walls AC, Corti D, Bloom JD, Veesler D, Mateo D, Hernando A, Comas I, González-Candelas F, González-Candelas F, Goig GA, Chiner-Oms Á, Cancino-Muñoz I, López MG, Torres-Puente M, Gomez-Navarro I, Jiménez-Serrano S, Ruiz-Roldán L, Bracho MA, García-González N, Martínez-Priego L, Galán-Vendrell I, Ruiz-Hueso P, De Marco G, Ferrús ML, Carbó-Ramírez S, D’Auria G, Coscollá M, Ruiz-Rodríguez P, Roig-Sena FJ, Sanmartín I, Garcia-Souto D, Pequeno-Valtierra A, Tubio JMC, Rodríguez-Castro J, Rabella N, Navarro F, Miró E, Rodríguez-Iglesias M, Galán-Sanchez F, Rodriguez-Pallares S, de Toro M, Escudero MB, SeqCOVID-SPAIN consortium, et al. 2021. Spread of a SARS-CoV-2 variant through Europe in the summer of 2020. Nature 595:707–712. doi: 10.1038/s41586-021-03677-y. [DOI] [PubMed] [Google Scholar]
- 3.Starr TN, Greaney AJ, Addetia A, Hannon WW, Choudhary MC, Dingens AS, Li JZ, Bloom JD. 2021. Prospective mapping of viral mutations that escape antibodies used to treat COVID-19. Science 371:850–854. doi: 10.1126/science.abf9302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greaney AJ, Loes AN, Crawford KHD, Starr TN, Malone KD, Chu HY, Bloom JD. 2021. Comprehensive mapping of mutations in the SARS-CoV-2 receptor-binding domain that affect recognition by polyclonal human plasma antibodies. Cell Host Microbe 29:463–476.e6. doi: 10.1016/j.chom.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boehm E, Kronig I, Neher RA, Eckerle I, Vetter P, Kaiser L, Geneva Centre for Emerging Viral Disease. 2021. Novel SARS-CoV-2 variants: the pandemics within the pandemic. Clin Microbiol Infect 27:1109–1117. doi: 10.1016/j.cmi.2021.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Volz E, Mishra S, Chand M, Barrett JC, Johnson R, Geidelberg L, Hinsley WR, Laydon DJ, Dabrera G, O'Toole A, Amato R, Ragonnet-Cronin M, Harrison I, Jackson B, Ariani CV, Boyd O, Loman NJ, McCrone JT, Goncalves S, Jorgensen D, Myers R, Hill V, Jackson DK, Gaythorpe K, Groves N, Sillitoe J, Kwiatkowski DP, Consortium C-GU, Flaxman S, Ratmann O, Bhatt S, Hopkins S, Gandy A, Rambaut A, Ferguson NM, COVID-19 Genomics UK (COG-UK) consortium. 2021. Assessing transmissibility of SARS-CoV-2 lineage B.1.1.7 in England. Nature 593:266–269. doi: 10.1038/s41586-021-03470-x. [DOI] [PubMed] [Google Scholar]
- 7.Tegally H, Wilkinson E, Giovanetti M, Iranzadeh A, Fonseca V, Giandhari J, Doolabh D, Pillay S, San EJ, Msomi N, Mlisana K, von Gottberg A, Walaza S, Allam M, Ismail A, Mohale T, Glass AJ, Engelbrecht S, Van Zyl G, Preiser W, Petruccione F, Sigal A, Hardie D, Marais G, Hsiao NY, Korsman S, Davies MA, Tyers L, Mudau I, York D, Maslo C, Goedhals D, Abrahams S, Laguda-Akingba O, Alisoltani-Dehkordi A, Godzik A, Wibmer CK, Sewell BT, Lourenco J, Alcantara LCJ, Kosakovsky Pond SL, Weaver S, Martin D, Lessells RJ, Bhiman JN, Williamson C, de Oliveira T. 2021. Detection of a SARS-CoV-2 variant of concern in South Africa. Nature 592:438–443. doi: 10.1038/s41586-021-03402-9. [DOI] [PubMed] [Google Scholar]
- 8.Faria NR, Mellan TA, Whittaker C, Claro IM, Candido DDS, Mishra S, Crispim MAE, Sales FCS, Hawryluk I, McCrone JT, Hulswit RJG, Franco LAM, Ramundo MS, de Jesus JG, Andrade PS, Coletti TM, Ferreira GM, Silva CAM, Manuli ER, Pereira RHM, Peixoto PS, Kraemer MUG, Gaburo N, Jr, Camilo CDC, Hoeltgebaum H, Souza WM, Rocha EC, de Souza LM, de Pinho MC, Araujo LJT, Malta FSV, de Lima AB, Silva JDP, Zauli DAG, Ferreira ACS, Schnekenberg RP, Laydon DJ, Walker PGT, Schluter HM, Dos Santos ALP, Vidal MS, Del Caro VS, Filho RMF, Dos Santos HM, Aguiar RS, Proenca-Modena JL, Nelson B, Hay JA, Monod M, Miscouridou X, et al. 2021. Genomics and epidemiology of the P.1 SARS-CoV-2 lineage in Manaus, Brazil. Science 372:815–821. doi: 10.1126/science.abh2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu J, Liu Y, Xia H, Zou J, Weaver SC, Swanson KA, Cai H, Cutler M, Cooper D, Muik A, Jansen KU, Sahin U, Xie X, Dormitzer PR, Shi PY. 2021. BNT162b2-elicited neutralization of B.1.617 and other SARS-CoV-2 variants. Nature 596:273–275. doi: 10.1038/s41586-021-03693-y. [DOI] [PubMed] [Google Scholar]
- 10.Zhao Y, Lee A, Composto K, Cunningham MH, Mediavilla JR, Fennessey S, Corvelo A, Chow KF, Zody M, Chen L, Kreiswirth BN, Perlin DS. 2021. A novel diagnostic test to screen SARS-CoV-2 variants containing E484K and N501Y mutations. Emerg Microbes Infect 10:994–997. doi: 10.1080/22221751.2021.1929504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Annavajhala MK, Mohri H, Wang P, Nair M, Zucker JE, Sheng Z, Gomez-Simmonds A, Kelley AL, Tagliavia M, Huang Y, Bedford T, Ho DD, Uhlemann AC. 2021. Emergence and expansion of SARS-CoV-2 B.1.526 after identification in New York. Nature 597:703–708. doi: 10.1038/s41586-021-03908-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thompson CN, Hughes S, Ngai S, Baumgartner J, Wang JC, McGibbon E, Devinney K, Luoma E, Bertolino D, Hwang C, Kepler K, Dell Castillo C, Hopkins M, Lee H, DeVito AK, Rakeman JL, Fine AD. 2021. Rapid emergence and epidemiologic characteristics of the SARS-CoV-2 B.1.526 variant - New York City, New York, January 1-April 5, 2021. MMWR Morb Mortal Wkly Rep 70:712–716. doi: 10.15585/mmwr.mm7019e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cobey S, Larremore DB, Grad YH, Lipsitch M. 2021. Concerns about SARS-CoV-2 evolution should not hold back efforts to expand vaccination. Nat Rev Immunol 21:330–335. doi: 10.1038/s41577-021-00544-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang P, Nair MS, Liu L, Iketani S, Luo Y, Guo Y, Wang M, Yu J, Zhang B, Kwong PD, Graham BS, Mascola JR, Chang JY, Yin MT, Sobieszczyk M, Kyratsous CA, Shapiro L, Sheng Z, Huang Y, Ho DD. 2021. Antibody resistance of SARS-CoV-2 variants B.1.351 and B.1.1.7. Nature 593:130–135. doi: 10.1038/s41586-021-03398-2. [DOI] [PubMed] [Google Scholar]
- 15.Bouton TC, Lodi S, Turcinovic J, Weber SE, Quinn E, Korn C, Steiner J, Schechter-Perkins EM, Duffy E, Ragan EJ, Taylor BP, Schaeffer B, Miller N, Davidoff R, Hanage WP, Connor J, Pierre C, Jacobson KR. 2021. COVID-19 vaccine impact on rates of SARS-CoV-2 cases and post vaccination strain sequences among healthcare workers at an urban academic medical center: a prospective cohort study. medRxiv. https://www.medrxiv.org/content/10.1101/2021.03.30.21254655v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daniel W, Nivet M, Warner J, Podolsky DK. 2021. Early evidence of the effect of SARS-CoV-2 vaccine at one medical center. N Engl J Med 384:1962–1963. doi: 10.1056/NEJMc2102153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keehner J, Horton LE, Pfeffer MA, Longhurst CA, Schooley RT, Currier JS, Abeles SR, Torriani FJ. 2021. SARS-CoV-2 infection after vaccination in health care workers in California. N Engl J Med 384:1774–1775. doi: 10.1056/NEJMc2101927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Teran RA, Walblay KA, Shane EL, Xydis S, Gretsch S, Gagner A, Samala U, Choi H, Zelinski C, Black SR. 2021. Postvaccination SARS-CoV-2 infections among skilled nursing facility residents and staff members - Chicago, Illinois, December 2020-March 2021. MMWR Morb Mortal Wkly Rep 70:632–638. doi: 10.15585/mmwr.mm7017e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hall VJ, Foulkes S, Saei A, Andrews N, Oguti B, Charlett A, Wellington E, Stowe J, Gillson N, Atti A, Islam J, Karagiannis I, Munro K, Khawam J, Chand MA, Brown CS, Ramsay M, Lopez-Bernal J, Hopkins S, Group SS, SIREN Study Group. 2021. COVID-19 vaccine coverage in health-care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): a prospective, multicentre, cohort study. Lancet 397:1725–1735. doi: 10.1016/S0140-6736(21)00790-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cavanaugh AM, Fortier S, Lewis P, Arora V, Johnson M, George K, Tobias J, Lunn S, Miller T, Thoroughman D, Spicer KB. 2021. COVID-19 outbreak associated with a SARS-CoV-2 R.1 lineage variant in a skilled nursing facility after vaccination program - Kentucky, March 2021. MMWR Morb Mortal Wkly Rep 70:639–643. doi: 10.15585/mmwr.mm7017e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, Hernan MA, Lipsitch M, Reis B, Balicer RD. 2021. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med 384:1412–1423. doi: 10.1056/NEJMoa2101765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, Brooks N, Smaja M, Mircus G, Pan K, Southern J, Swerdlow DL, Jodar L, Levy Y, Alroy-Preis S. 2021. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet 397:1819–1829. doi: 10.1016/S0140-6736(21)00947-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Angel Y, Spitzer A, Henig O, Saiag E, Sprecher E, Padova H, Ben-Ami R. 2021. Association Between vaccination with BNT162b2 and incidence of symptomatic and asymptomatic SARS-CoV-2 infections among health care workers. JAMA 325:2457. doi: 10.1001/jama.2021.7152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kustin T, Harel N, Finkel U, Perchik S, Harari S, Tahor M, Caspi I, Levy R, Leshchinsky M, Ken Dror S, Bergerzon G, Gadban H, Gadban F, Eliassian E, Shimron O, Saleh L, Ben-Zvi H, Keren Taraday E, Amichay D, Ben-Dor A, Sagas D, Strauss M, Shemer Avni Y, Huppert A, Kepten E, Balicer RD, Netzer D, Ben-Shachar S, Stern A. 2021. Evidence for increased breakthrough rates of SARS-CoV-2 variants of concern in BNT162b2-mRNA-vaccinated individuals. Nat Med 27:1379–1384. doi: 10.1038/s41591-021-01413-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abu-Raddad LJ, Chemaitelly H, Butt AA, National Study Group for C-V. 2021. Effectiveness of the BNT162b2 Covid-19 vaccine against the B.1.1.7 and B.1.351 variants. N Engl J Med 385:187–189. doi: 10.1056/NEJMc2104974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chodick G, Tene L, Rotem RS, Patalon T, Gazit S, Ben-Tov A, Weil C, Goldshtein I, Twig G, Cohen D, Muhsen K. 2021. The effectiveness of the TWO-DOSE BNT162b2 vaccine: analysis of real-world data. Clin Infect Dis. doi: 10.1093/cid/ciab438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.CDC COVID-19 Vaccine Breakthrough Case Investigations Team. 2021. COVID-19 vaccine breakthrough infections reported to CDC - United States, January 1-April 30, 2021. MMWR Morb Mortal Wkly Rep 70:792–793. doi: 10.15585/mmwr.mm7021e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Candido DS, Claro IM, de Jesus JG, Souza WM, Moreira FRR, Dellicour S, Mellan TA, Du Plessis L, Pereira RHM, Sales FCS, Manuli ER, Theze J, Almeida L, Menezes MT, Voloch CM, Fumagalli MJ, Coletti TM, da Silva CAM, Ramundo MS, Amorim MR, Hoeltgebaum HH, Mishra S, Gill MS, Carvalho LM, Buss LF, Prete CA, Jr, Ashworth J, Nakaya HI, Peixoto PS, Brady OJ, Nicholls SM, Tanuri A, Rossi AD, Braga CKV, Gerber AL, de CGAP, Gaburo N, Jr, Alencar CS, Ferreira ACS, Lima CX, Levi JE, Granato C, Ferreira GM, Francisco RS, Jr, Granja F, Garcia MT, Moretti ML, Perroud MW, Jr, Castineiras T, Lazari CS, Brazil-UK Centre for Arbovirus Discovery, Diagnosis, Genomics and Epidemiology (CADDE) Genomic Network, et al. 2020. Evolution and epidemic spread of SARS-CoV-2 in Brazil. Science 369:1255–1260. doi: 10.1126/science.abd2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McEwen AE, Cohen S, Bryson-Cahn C, Liu C, Pergam SA, Lynch J, Schippers A, Strand K, Whimbey E, Mani NS, Zelikoff AJ, Makarewicz VA, Brown ER, Mohamed BS, Baker NR, Castor J, Livingston RJ, Huang M-L, Jerome KR, Greninger AL, Roychoudhury P. 2021. Variants of concern are overrepresented among post-vaccination breakthrough infections of SARS-CoV-2 in Washington State. medRxiv. 10.1101/2021.05.23.21257679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.West AP, Wertheim JO, Wang JC, Vasylyeva TI, Havens JL, Chowdhury MA, Gonzalez E, Fang CE, Di Lonardo SS, Hughes S, Rakeman JL, Lee HH, Barnes CO, Gnanapragasam PNP, Yang Z, Gaebler C, Caskey M, Nussenzweig MC, Keeffe JR, Bjorkman PJ. 2021. Detection and characterization of the SARS-CoV-2 lineage B.1.526 in New York. bioRxiv. https://www.biorxiv.org/content/10.1101/2021.02.14.431043v3 [DOI] [PMC free article] [PubMed]
- 31.Levine-Tiefenbrun M, Yelin I, Katz R, Herzel E, Golan Z, Schreiber L, Wolf T, Nadler V, Ben-Tov A, Kuint J, Gazit S, Patalon T, Chodick G, Kishony R. 2021. Initial report of decreased SARS-CoV-2 viral load after inoculation with the BNT162b2 vaccine. Nat Med 27:790–792. doi: 10.1038/s41591-021-01316-7. [DOI] [PubMed] [Google Scholar]
- 32.Thorne LG, Bouhaddou M, Reuschl AK, Zuliani-Alvarez L, Polacco B, Pelin A, Batra J, Whelan MVX, Ummadi M, Rojc A, Turner J, Obernier K, Braberg H, Soucheray M, Richards A, Chen KH, Harjai B, Memon D, Hosmillo M, Hiatt J, Jahun A, Goodfellow IG, Fabius JM, Shokat K, Jura N, Verba K, Noursadeghi M, Beltrao P, Swaney DL, Garcia-Sastre A, Jolly C, Towers GJ, Krogan NJ. 2021. Evolution of enhanced innate immune evasion by the SARS-CoV-2 B.1.1.7 UK variant. bioRxiv. https://www.biorxiv.org/content/10.1101/2021.06.06.446826v1
- 33.Hay JA, Kennedy-Shaffer L, Kanjilal S, Lennon NJ, Gabriel SB, Lipsitch M, Mina MJ. 2021. Estimating epidemiologic dynamics from cross-sectional viral load distributions. Science 373. doi: 10.1126/science.abh0635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kechin A, Boyarskikh U, Kel A, Filipenko M. 2017. cutPrimers: a new tool for accurate cutting of primers from reads of targeted next generation sequencing. J Comput Biol 24:1138–1143. doi: 10.1089/cmb.2017.0096. [DOI] [PubMed] [Google Scholar]
- 35.Li H, Durbin R. 2009. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25:1754–1760. doi: 10.1093/bioinformatics/btp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gaspar JM. 2018. NGmerge: merging paired-end reads via novel empirically-derived models of sequencing errors. BMC Bioinformatics 19:536. doi: 10.1186/s12859-018-2579-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hadfield J, Megill C, Bell SM, Huddleston J, Potter B, Callender C, Sagulenko P, Bedford T, Neher RA. 2018. Nextstrain: real-time tracking of pathogen evolution. Bioinformatics 34:4121–4123. doi: 10.1093/bioinformatics/bty407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elbe S, Buckland-Merrett G. 2017. Data, disease and diplomacy: GISAID's innovative contribution to global health. Glob Chall 1:33–46. doi: 10.1002/gch2.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nguyen LT, Schmidt HA, von Haeseler A, Minh BQ. 2015. IQ-TREE: a fast and effective stochastic algorithm for estimating maximum-likelihood phylogenies. Mol Biol Evol 32:268–274. doi: 10.1093/molbev/msu300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Letunic I, Bork P. 2019. Interactive Tree Of Life (iTOL) v4: recent updates and new developments. Nucleic Acids Res 47:W256–W259. doi: 10.1093/nar/gkz239. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The SARS-CoV-2 genomes sequenced in this study were deposited in GISAID (https://www.gisaid.org). Sequences can be accessed by searching records from both the originating lab at Hackensack Medical Center and the submitting lab at the New York Genome Center.