Abstract
Introduction
Dog bites are a significant health concern in the pediatric population. Few studies published to date have stratified the injuries caused by dog bites based on surgical severity to elucidate the contributing risk factors.
Methods
We used an electronic hospital database to identify all patients ≤17 years of age treated for dog bites from 2013–2018. Data related to patient demographics, injury type, intervention, dog breed, and payer source were collected. We extracted socioeconomic data from the American Community Survey. Data related to dog breed was obtained from public records on dog licenses. We calculated descriptive statistics as well as relative risk of dog bite by breed.
Results
Of 1,252 injuries identified in 967 pediatric patients, 17.1% required consultation with a surgical specialist for repair. Bites affecting the head/neck region were most common (61.7%) and most likely to require operating room intervention (P = 0.002). The relative risk of a patient being bitten in a low-income area was 2.24, compared with 0.46 in a high-income area. Among cases where the breed of dog responsible for the bite was known, the dog breed most commonly associated with severe bites was the pit bull (relative risk vs German shepherd 8.53, relative risk vs unknown, 3.28).
Conclusion
The majority of injuries did not require repair and were sufficiently handled by an emergency physician. Repair by a surgical specialist was required <20% of the time, usually for bites affecting the head/neck region. Disparities in the frequency and characteristics of dog bites across socioeconomic levels and dog breeds suggest that public education efforts may decrease the incidence of pediatric dog bites.
INTRODUCTION
With over 4.5 million dog bite injuries reported each year in the United States, dog bites continue to be a significant public health concern.1 Children are at high risk for dog bite injury, with many incidents reported at or near a victim’s home.2 The current global pandemic has necessitated virtual learning, and children are spending more time at home. The latest report from the US Centers for Disease Control and Prevention on the frequency of dog bites reported that 800,000 individuals sought medical attention for a dog-bite injury in 2001.3 These numbers are expected to surge due to stay-at-home guidelines during the current pandemic.
Many studies have identified trends in pediatric dog-bite injuries and interventions,4–15 but few studies have stratified injury severity based on the type of surgical treatment required. Significant damage to the face, which is the area most commonly affected in children who sustain dog bites, may require the specialized skills of a subspecialist who can reconstruct the complex functional and aesthetic components of the affected anatomy.16 In younger patients, delicate anatomy and limited compliance may require treatment in the operating room (OR), instead of a bedside procedure. The surgical approach is also determined by injury severity, which has previously been shown to be associated with socioeconomic factors in adults with dog bites.17 We sought to examine the interplay among these factors in pediatric patients who presented for treatment of dog-bite injuries at our institution.
Orange County, CA, where our institution resides, is the sixth largest county by population in the US, with many low-income and affluent communities in close proximity to one another. Our academic pediatric trauma center is the only pediatric hospital serving this diverse population of over three million. This makes our institution an ideal setting for an investigation of the etiology and treatment of pediatric dog-bite injuries. In this study, we describe our five-year experience and aim to characterize the settings in which a surgeon is required for the treatment of pediatric dog-bite injury. We also collected information from public records and healthcare databases to evaluate external risk factors that may increase risk for dog bites, such as socioeconomic status and breed of dog. Delineating the injury patterns in this high-risk population may both streamline care and guide future prevention efforts.
METHODS
This was a retrospective cross-sectional study of all children aged 0 to 17 years treated for dog-bite injury during the period from 2013–2018 at our institution. The inclusion criteria were all pediatric patients presenting to the pediatric emergency department (ED) during the study period and identified in the electronic health record (EHR) as having an acute dog bite injury (International Classification of Diseases, Ninth Revision and Tenth Revision, Clinical Modification [ICD-9] E906.0 and ICD-10-CM W54.0). Exclusion criteria were bite wounds that had already received a procedure at another institution and transferred to our institution for delayed reconstruction, patients who presented > 24 hours after the injury, and any subsequent visits related to the same initial injury. Two unblinded abstractors were uniformly trained to use a pilot-tested, standardized, online data abstraction form with coding rules. Data abstraction was routinely monitored to ensure systematic data collection including refresher training and review of coding rules. We did not exclude records with missing data; missing values for categorical variables were documented as unknown.
Population Health Research Capsule.
Dog bites are a significant health concern in children. Most dog bites occur from age 1–5, and affect the head and neck region.
What was the research question?
Do sociodemographic factors and dog breed impact pediatric dog-bite injuries and their severity?
What was the major finding of the study?
Lower socioeconomic status increased risk for dog bites. Larger dogs were associated with more severe injury.
How does this improve population health?
This study informs injury prevention efforts that may target communities at risk including those with lower socioeconomic status.
The descriptive features captured in this study included the following: sociodemographic information (age, race, gender, ethnicity, payer source, and median income associated with residence ZIP code); clinical variables (wound depth, wound diameter, level of intervention required, number of body sites wounded, and anatomical site of injury); and information on the dog (relationship to dog, breed of dog). Wound depth was categorized as superficial (partial thickness skin wounds, scratches, excoriations, dermabrasions), deep (full-thickness skin wounds without trauma to underlying tissue), and complex (full thickness wounds with trauma to underlying tissues such as tendons, nerves, vessels). Information on the dog breed, patient’s relationship to the dog, and location where the injury occurred were first abstracted from the provider notes in the EHR and then cross-referenced with information included in the Animal Bite Human Reporting Form sent to the county health department.
Socioeconomic data such as median income was extracted from the American Community Survey (ACS).18 We obtained county records of city-level dog populations from the county animal shelter.19 The relative proportions of various dog breeds in the county were applied to city-level estimates of dog population to determine the relative risk of dog bite. We further stratified the data analyzed for each dog breed based on bite severity and median income in the area where the dog bite occurred. A phylogenetic tree of dog breeds was constructed using data from the National Human Genome Research Institute Dog Genome project.21 We constructed the phylogenetic tree using a circular tree plot to visualize bite frequency across genetic groups.
Statistical Analysis
We calculated the relative risk of being bitten by a specific breed of dog, the relative risk of being bitten in a lower-income area, and the relative risk of sustaining a severe, rather than moderate or mild, dog-bite injury. The relative risk of being bitten by a specific breed of dog was calculated using dog population data collected by the animal shelters of our county, which collect data for all licensed dogs in the county. We ranked dog breeds according to relative risk of bite, compared to the risk of being bitten by any member of the dog population in the county. The relative risk of dog bite was mapped onto each breed in the phylogenetic tree. If no bite data was observed for a specific dog breed, the relative risk was set to one.
We calculated P-values using the chi-square test for cell size >100 and Fisher’s exact test for cell size <100. In this study, the Fisher’s and chi-square P-values measured distribution of a given variable after stratification by another categorical variable, in comparison to the distribution of all other categories summed. For continuous measures such as bite diameter, a Wilcoxon rank-sum test was used to measure the difference in distribution among continuous measures. We used the R programming language to conduct these analyses. Income and dog-bite frequency were mapped using the Choroplethr package (R Foundation for Statistical Computing, Vienna, Austria).20
RESULTS
From 2013 to 2018, 967 pediatric patients at our children’s hospital were identified as victims of a dog bite. The mean and median ages of pediatric patients who sustained dog-bite injuries were six years and five years, respectively. The mode of the age variable in this study was three years. After stratification into age categories of 1–5 years, 6–10 years, and >10 years of age, the 1–5 age group was identified as the group of patients that made up the greatest proportion of those bitten (53.4%). The risk for dog-bite injury was inversely correlated with age, with a Pearson correlation coefficient of −0.76 (Figure 1). Regardless of age, children are bitten most frequently by a dog living in their own home (33.4%), followed by pets belonging to family and friends (22.4%) (Supplemental Table).
Figure 1.
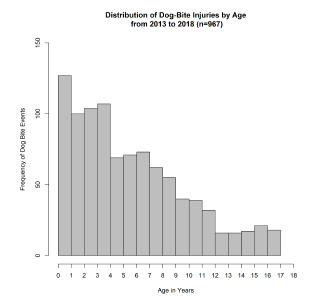
Distribution of dog bite injuries by age.
Our analysis of the sociodemographic data collected revealed that the racial distribution of pediatric patients who sustained dog-bite injuries was similar to the racial make-up of the community, with 64.6% of patients in the study identifying as White/Caucasian. It should be noted that patient families identifying as Latino were disproportionately represented in this survey. The 2017 ACS reported that 34.2% of the residents in the county identified as Latino, while 55.2% of the patient population in this study identified as Latino (with only 1.16% of study participants refusing to answer this question). It should also be noted that a large proportion of the patient families included in this study were covered by Medicare (22.4%) or Medicaid (29.5%); 41.4% were covered by private insurance, and the remaining 6.6% were self-pay (Table 1).
Table 1.
Characteristics of pediatric dog-bite victims who presented to the emergency department from 2013–2018.
| Characteristics | Frequency n (%)* |
|---|---|
| Number of patients | 943 |
| Age (year) | |
| Mean | 6.04 |
| Median | 5 |
| Mode | 3 |
| Gender | |
| Female | 408 (43.2%) |
| Male | 535 (56.7%) |
| Race | |
| White | 610 (64.6%) |
| Black | 12 (1.3%) |
| Asian | 55 (5.8%) |
| American Indian | 2 (0.2%) |
| Hispanic | 19 (2.0%) |
| Native Hawaiian | 8 (0.8%) |
| Other | 215 (22.7%) |
| Refused | 19 (2.0%) |
| Ethnicity | |
| Not Latino | 421 (44.6%) |
| Latino | 521 (55.2%) |
| Refused | 11 (1.2%) |
| Payer | |
| Medicare | 212 (22.4%) |
| Medicaid | 279 (29.5%) |
| Private | 391 (41.4%) |
| Self-pay | 40 (4.2%) |
| Other | 21 (2.2%) |
Frequencies reported are limited to all patients with clinical and demographic data.
Level of Intervention
Most injuries did not require specialist or OR services; 71.8% of bites did not require wound repair, while 17.1% of patients required specialist consultation for wound repair in the ED or the OR. The distribution of bite severity mirrored this pattern, with 70.5% of bites classified as “superficial” (partial thickness, scratches, excoriations, abrasions); 21.1% of bites classified as “deep” (full thickness without trauma to underlying structures); and 8.5% of bites classified as “complex” (full thickness with trauma to underlying structures such as tendons, nerves, and/or vessels). Analysis of the data to determine which anatomical area was most commonly affected revealed that 61.7% of bites were inflicted on the head or neck, 20.6% on the hands or arms, and 13.0% on the feet or legs (Table 2).
Table 2.
Characteristics of dog-bite injuries.
| Characteristics | Frequency n (%) |
|---|---|
| Number of injuries | 1,252 |
| Level of intervention | |
| No repair | 677 (54.0%) |
| Repair by EP | 413 (32.9%) |
| Repair by specialist in ED | 23 (1.8%) |
| Repair in OR | 139 (11.1%) |
| Depth* | |
| Superficial | 861 (70.5%) |
| Deep | 258 (21.1%) |
| Complex | 102 (8.3%) |
| Anatomic site | |
| Head/neck | 774 (61.7%) |
| Upper extremity hand | 153 (12.2%) |
| Upper extremity arm | 105 (8.4%) |
| Lower extremity foot | 18 (1.4%) |
| Lower extremity leg | 145 (11.6%) |
| Other | 57 (4.5%) |
The depth variable was incomplete; thus, the percentages represent the number of injuries within each depth category out of the total number of injuries with complete wound depth data (n = 1,221)
When we investigated the relationship between anatomical site of injury (head, upper extremity, lower extremity, other) and type of intervention (no repair, emergency physician repair [EP], surgical specialist repair in ED, specialist repair in OR), we found that head and neck injuries were significantly more likely to require repair (P = <.0001). When stratifying injuries by different levels of repair (EP, surgical specialist in ED, and specialist repair in OR) there were statistically significant differences in the proportion of observed injuries across different anatomic sites. The largest difference in proportion was observed in head and neck injuries, which contributed to 41.2% of cases not requiring repair, and 86.2%, 69.6%, and 88.5% to cases requiring repair by EPs, surgical specialists in the ED, and repair performed by specialists in the OR, respectively. This association persisted even when “no repair” patients were removed from the dataset (P = 0.002). This data is presented in Table 3 and Figure 2.
Table 3.
Level of intervention by injury location and payer source.
| Characteristic | No repair | Repair by EP | Repair by surgical specialist in ED | Repair by specialist in OR |
|---|---|---|---|---|
| Total | 677 | 413 | 23 | 139 |
| Injury Location | ||||
| Head/neck | 279 (41.2%) | 356 (86.2%) | 16 (69.6%) | 123 (88.5%) |
| Upper extremity arm | 141 (20.8%) | 12 (2.9%) | 0(0%) | 0 (0%) |
| Upper extremity hand | 80 (11.8%) | 18 (4.4%) | 1 (4.4%) | 6 (4.3%) |
| Lower extremity leg | 17 (2.5%) | 0 (0%) | 1 (4.3%) | 0 (0%) |
| Lower extremity foot | 118 (17.4%) | 21 (5.1%) | 3 (13.0%) | 3 (2.2%) |
| Other | 42 (6.2%) | 6 (1.5%) | 2 (8.7%) | 7 (5.0%) |
| P-value | <.0001 | |||
| Payer source | ||||
| Medicare | 114 (16.8%) | 109(26.4%) | 8 (34.8%) | 54 (38.8%) |
| Medicaid | 227 (33.5%) | 71 (17.2%) | 1 (4.3%) | 24 (17.3%) |
| Private | 288 (42.5%) | 174 (42.1%) | 11 (47.8%) | 51 (36.7%) |
| Self-Pay | 23 (3.4%) | 26 (6.3%) | 0 (0%) | 6 (4.3%) |
| Other | 17 (2.5%) | 12 (2.9%) | 0 (0%) | 0 (0%) |
| P-value | <.0001 | |||
| Wound severity | ||||
| Superficial | 657 (98.5%) | 188 (47.5%) | 9 (39.1%) | 7 (51.4%) |
| Deep | 4 (0.5%) | 205 (51.8%) | 4 (17.3%) | 45 (33.0%) |
| Complex | 6 (0.8%) | 2 (0.5%) | 10 (43.4%) | 84 (61.7%) |
| P-value | 0.0001 | |||
EP, emergency physician; ED, emergency department; OR, operating room.
Figure 2.
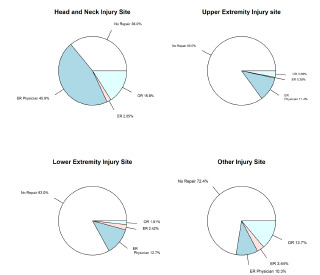
Level of intervention by anatomic site of injury.
When we examined the association between requirement for surgical treatment and bite severity, the data showed that 82.3% of complex wounds (full thickness with trauma to underlying structures such as tendons, nerves, and/or vessels) were treated in the OR, 9.8% of complex wounds were treated by a specialist in the ED, and 1.9% of wounds were repaired by a general EP. This observed pattern contrasted with that observed for deep wounds (full thickness without trauma to underlying structures), for which the majority (79.4%) were treated by an EP. The majority of superficial wounds (76.3%) required no repair.
Socioeconomic Status
We used ZIP codes to map city-level reports of median income from the ACS. The ZIP code was used to approximate the economic status of a patient family to evaluate the association between economic status and the frequency of bites. According to the 2017 ACS, the median income in the county is $89,000. Analysis of the study data showed that 67.9% of patients lived in areas with median annual income greater than $42,000, and 32.1% of patients lived in areas with median income of $42,000 or less (Figure 3). Using population-based estimates of the total dog population for each area, the relative risk of a pediatric patient being bitten in a low-income area (median income ≤ $42,000) was 2.24-fold greater than the baseline risk of being bitten in the county. In contrast, the relative risk of a pediatric patient being bitten in a high-income area (median annual income > $42,000) was 0.46. The relative proportion of biting dogs in the general dog population was significantly greater in low- vs high-income areas (P <.0001). These differences are illustrated in Figure 4; there was a significant difference in the proportion of dogs inflicting bites in neighborhoods with median income <$42,000 compared to the proportion of dogs inflicting bites in neighborhoods with median income >$42,000.
Figure 3.
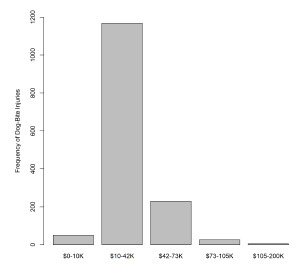
Distribution of dog bite injuries by level of annual income.
Figure 4.
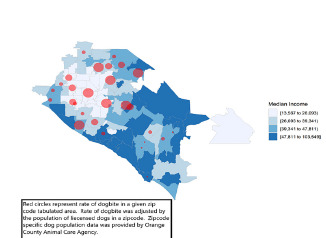
Distribution of dog bite injuries based on zip code and median income quartile.
We performed an analysis of the distribution of bites across insurance payer and level of intervention, with insurance status used as a proxy for economic status. Patients who used private insurance to pay for hospital services were significantly more likely to receive treatment by a specialist or treatment in the OR than patients who used Medicaid or Medicare to pay for hospital services (P <.0001) (Table 3). Medicaid patients accounted for only 15% of those with injuries treated by specialists. Among those who received OR treatment for dog bites, 75% used Medicare or private insurance to pay for hospital services (Figure 5).
Figure 5.
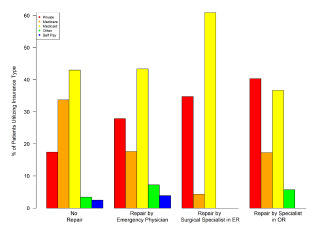
Level of intervention by insurance payer group.
Dog Breed
In 61.4% of cases included in the study, the breed of the dog that had bitten a particular patient was unknown. Among the cases where the breed of the dog responsible for the injury was reported, representation was as follows: Chihuahua mix, 7%; pit bull mix, 7.6%; German shepherd mix, 3.3%; other or mixed breed, 20.4%. No significant relationship was found between dog breed and anatomical site of injury, or between dog breed and median income in the area where the dog bite occurred. There was, however, a significant association between breed and the requirement for surgical treatment by a specialist (Table 4). The likelihood that the patient had been bitten by a pit bull increased as the level of intervention increased from no repair (6.0%) to repair in the OR (25.8%) (Figure 6).
Table 4.
Dog-bite visits by breed of dog from 2013–2018.
| Characteristic | Pit Bull | Mixed Breed | German Shepherd | Other | Unknown | Chihuahua |
|---|---|---|---|---|---|---|
| Body region injured | ||||||
| Head/neck | 60(57.6%) | 20(74.0%) | 34(70.8%) | 172(66.6%) | 449(60.8%) | 37(49.3%) |
| Upper extremity (hand/arm) | 22(21.1%) | 2(7.4%) | 9(18.7%) | 54(20.9%) | 150(20.3%) | 20(26.6%) |
| Lower ectremity (leg/foot) | 14(13.4%) | 2(7.4%) | 2(4.2%) | 23(8.9%) | 110(14.9%) | 12(16.0%) |
| Other | 8(7.7%) | 3(11.1%) | 3(6.3%) | 9(3.5%) | 29(3.9%) | 6(8%) |
| P-value | 0.4 | 0.34 | 0.19 | 0.09 | 0.07 | 0.08 |
| Median Income by city reported by ACS | ||||||
| <$42,000/year | 23(32.3%) | 7(38.8%) | 10(32.2%) | 53(30.8%) | 191(33.2%) | 16(23.5%) |
| >$42,000/year | 48(67.6%) | 11(61.1%) | 21(67.7%) | 119(69.1%) | 384(66.7%) | 52(76.4%) |
| P-value | 1 | 0.6 | 1 | 0.71 | 0.38 | 0.13 |
| Level of intervention | ||||||
| No repair | 41(39.4%) | 16(59.2%) | 17(35.4%) | 109(42.2%) | 424(57.4%) | 69(92.0%) |
| Repair by EP | 23(22.1%) | 10(37.0%) | 23(47.9%) | 104(40.3%) | 247(33.4%) | 5(6.6%) |
| Repair by surgical specialist in ED | 4(3.8%) | 0(0%) | 0(0%) | 15(5.8%) | 4(0.5%) | 0 |
| Repair by specialist in OR | 26(34.6%) | 1(3.7%) | 8(3.7%) | 30(11.6%) | 63(8.5%) | 1(1.3%) |
| P-value | 0.001 | 0.69 | 0.01 | <.0001 | 0.004 | <.0001 |
ACS, American Community Survey; EP, emergency physician; ED, emergency department; OR, operating room.
Figure 6.
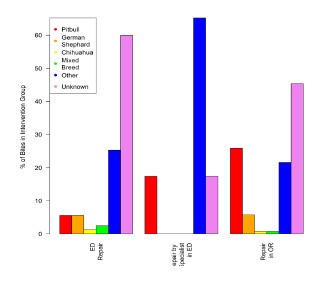
Level of intervention by breed of dog.
Dog breed was a significant predictor of bite severity (P <.0001) and of bite diameter (P <.0001). Pit bull bites were found to be significantly larger, deeper, and/or more complex than the average dog bites included in this study (Figure 7). Patients included in this study were more than four times as likely to have been bitten by a pit bull than by a German shepherd, and more than twice as likely to have been bitten by a pit bull, when compared with a dog of unknown breed. Furthermore, the relative risk of a pit bull inflicting a complex (full thickness with trauma to underlying structures) or deep (full thickness without trauma to underlying structures) bite was 17 times that observed for non-pit bull dogs. The relative risk of a German shepherd inflicting a complex or deep bite was 2.66, and the relative risk that a dog of unknown breed would inflict a complex or deep bite was 0.23. The relative risk of being bitten by a pit bull did not differ greatly between high-income cities and low-income cities, with relative risk of 8.06 and 8.17, respectively (Table 5).
Figure 7.
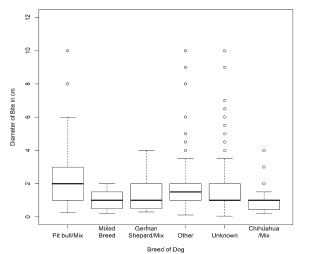
Distribution of bite diameter by breed of dog.
Table 5.
Relative risk* of bite by dog breed using estimated dog population.
| Dog breed | Number of bite events attributed to breed | Proportion of bites in database attributed to breed | Estimated population of dog breed in county | Proportion of bite events with >1 body site bitten | Average bite diameter in cm | RR of breed biting compared to general dog population | RR of inflicting deep or complex wound | RR of bite occurring in a low median income city | RR of bite occurring in a high median income city |
|---|---|---|---|---|---|---|---|---|---|
| Pit bull | 75 | 7.75% | 34,464(2.90%) | 32.67% | 2.9 | 8.53 | 17.07 | 8.17 | 8.06 |
| German shepherd | 32 | 3.30% | 142,60(1.20%) | 16.00% | 1.62 | 2.02 | 2.66 | 1.97 | 1.95 |
| Chihuahua mix | 68 | 7.03% | 534,78(4.50%) | 29.10% | 0.99 | 3.35 | 0.51 | 2.46 | 3.78 |
| Mixed breed | 18 | 1.86% | 118,841(10.0%) | 44.40% | 0.95 | 0.2 | 1.7 | 0.24 | 0.18 |
| Cocker spaniel | 7 | 0.72% | 142,60(1.20%) | 28.57% | 1.21 | 0.53 | 0.74 | 1.66 | 0* |
| Other breed | 180 | 18.6% | 818,817(68.9%) | 36.20% | 1.817 | 0.27 | 0.23 | 0.25 | 0.27 |
| Unknown breed | 593 | 61.3% | 133,102(11.2%) | 19.07% | 1.63 | 3.28 | 2.5 | 3.3 | 5.39 |
All relative risks in comparison to rate observed in general dog population.
RR, relative risk; cm, centimeter.
We constructed a phylogenetic tree of dog breeds to identify clades with an increased relative risk of bite, compared to the general dog population (Figure 8). This visualization revealed increased relative risk for dog bite in dog breeds designated as “working dogs” by the American Kennel Club. The breeds in this group associated with high relative risk for bite-related injury were bulldog, boxer, French bulldog, pit bull, mastiff, Great Dane, Rottweiler, and Doberman pinscher. Siberian husky, chow chow, and Akita breeds also had increased risk of dog bite compared to the general population of dogs in the county. This latter group of dogs is classified on the side of the canine phylogenetic tree most distant from dogs classified as “working dogs.” Among all dogs within the phylogenetic tree, husky, chow chow, and Akita breeds are most closely related to the common ancestor of all canines, the wolf. Although the husky is classified as a working dog, it is not closely related to the clade of working dogs listed above. The dogs with decreased relative risk of bite (basset hound, beagle, and dachshund) were clustered in a group of dogs classified by the American Kennel Club as hounds (relative risk, < 1.00).
Figure 8.
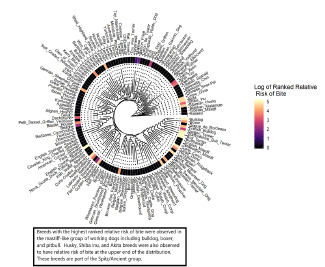
Phylogenetic tree of dog breeds associated with risk for dog bite within the county.
DISCUSSION
Dog bite injuries continue to be prevalent in the pediatric population, especially among young children. Similar to previous studies,4,5,7–9 our analysis showed that the majority of dog bites in our study affected children 1–5 years of age, with risk for dog bite decreasing as age increased. Dogs may perceive the behavior of young children as threatening.22–24 Infants, toddlers, and preschool children are less cautious, tend to explore their environments with their hands and mouths, and exhibit unpredictable behaviors, such as suddenly kissing, biting, grabbing, and climbing upon a dog. Because of its proximity to the floor, the head and neck region of children is particularly susceptible to dog-bite injury; in adults, the extremities are most susceptible.17 Our analysis supports prior studies4,5,11,12 demonstrating that the majority of dog bites in children affect the head and neck region (61.7%), followed by the hand or arms (20.6%).
A previous study by our group of dog-bite injuries in the county showed that 60% of dog bites in adult patients received no intervention.17 Because the facial region is frequently involved when a dog bites a child, the families of children with dog-bite injuries are also more likely to seek medical attention than adults who have sustained dog bites.25 Pediatric patients may, therefore, be more likely to present to the ED with superficial dog-bite injuries,6 which may partially account for the increased incidence of reported dog bites in children compared to adults. Of the pediatric patients who presented to the ED at our institution during the study period, 71.9% required no intervention because their injuries were superficial. Of the pediatric patients in our study requiring intervention, the greatest proportion of dog-bite injuries that necessitated repair in the OR affected the head and neck areas. Dog-bite injury to the facial region not only threatens function but may also have a lasting impact on physical appearance as the child grows into adulthood. The complex nature of head and neck physiology and anatomy, therefore, often merits consultation with a specialist and intervention in the OR.15,26 In our study, complex and deep injuries with larger diameters were likely to require specialist intervention.
Our analysis goes further to reveal how socioeconomic factors influence the management of dog-bite injury. A median annual income below $42,000 conferred a 2.24 relative risk for pediatric dog-bite injury, compared to a 0.46 relative risk in regions with high median annual income. This trend is consistent with the findings of a study by Ruiz-Casares et al, which demonstrated that children in low-income families are the most vulnerable to unintentional injury.27 Parents in low-income households may need to attend to work obligations and may, therefore, be unavailable to supervise young children and without the means to pay for daycare services. Young children supervised by older siblings have increased risk for injury, compared to young children supervised by their parents.28,29 Because adults are generally able to protect themselves, the risk for dog bite and associated patterns of injury in adults does not seem to be impacted by annual income.17 Furthermore, dogs in low-income households are less likely to be supervised, less likely to be sufficiently trained, and less likely to be kept in an area enclosed by fencing or gates.30 Low-income households are also more likely to have large-breed dogs for protective purposes.30 This combination of inadequate resources for child supervision and large-breed dogs without robust training may account for the increased incidence of pediatric dog-bite injury in low-income households.
In our analysis, insurance type was used as an index for socioeconomic status. Our study shows that children in families with Medicaid or self-pay status were more likely to experience a dog-bite injury, but less likely to have their injuries repaired by specialists in the OR. It is unclear whether the difference in service utilization between private insurance payers vs Medicaid or self-payers reflects systemic obstacles or, rather, a parental preference for ED intervention based on financial concerns. While Essig et al showed that the surgical management of pediatric facial dog-bite injuries by specialists in either the ED or OR had no significant effect on the risk for surgical-site infection or reoperation,31 it would be interesting to study the outcomes of dog-bite injuries treated by ED clinicians, compared with similar injuries that were treated by surgical specialists. The results of a comparative cohort study might reveal whether treatment by a specialist decreased the incidence of infection, scarring, or later return to the OR. A significant difference in the outcomes of pediatric dog-bite injury with specialist vs non-specialist treatment might ultimately result in a change in treatment patterns and improved public health.
Many studies have attempted to elucidate the role of dog breed in bite injuries. In the literature the dog breeds most commonly associated with pediatric dog-bite injuries include the pit bull, Rottweiler, German shepherd, terrier, and mixed.9,10,32 In our analysis, German shepherds were responsible for the highest number of pediatric dog-bite injuries, but pit bulls were responsible for the most severe injuries. In a related study conducted at a Level I pediatric trauma center, Alizadeh et al showed that 47.8% of pediatric dog bites that involved a pit bull required surgical intervention.33 Many studies have reported similar results of pit bull-related aggression, and this particular breed has been considered a public health risk; several countries and US cities have introduced breed-specific bans.34,35
It should be noted that aggressive canine behavior is multifactorial, with genetic as well as human interference-related contributing factors.36,37 However, breed-specific legislation has been criticized for being ineffective, difficult to implement, and harmful to the welfare of dogs. Breed-specific bans may also be based on incomplete data from health records or sensationalized media reports.8,38,39 We agree that rather than breed-specific laws, efforts to decrease the frequency of pediatric dog-bite injury should focus on identifying the precipitating factors. Clinicians should be educated to include as part of their history questions about whether the child presenting for care was supervised and whether the dog was partitioned from the child, in addition to questions about the age, gender, breed, and level of training of the dog. A more complete health record would increase the accuracy of the data related to dog-bite injury in pediatric patients.
LIMITATIONS
There were several limitations to our study. The socioeconomic data that we extracted from the ACS was not a true measure of family income, as these pooled data represent neighborhood-level rather than individualized patient information. The data presented in this analysis is specific to a high-volume, academic healthcare institution that serves a large and diverse community. The findings may, therefore, not be generalizable to all institutions and populations. We did not stratify the data used for analysis based on surgical subspecialty or type of dog-bite injury. Not all bites could be attributed to a specific breed or mixed breed of dog. As a result, the relative risk of bite in some breeds may have been under-reported. Additional bias may occur in breeds with small reported populations in the community; these breeds may have instability in the estimates of relative risk of bite due to small samples that are not representative of a given dog breed.
Additional studies will be designed to elucidate whether plastic surgeons, otolaryngologists, or general surgeons are more frequently involved with certain types of pediatric dog-bite injuries. Such an investigation would help to streamline workflow and to increase the use of a multidisciplinary approach in pediatric EDs. With interest, we continue to monitor and study how trends in the etiology and management of pediatric dog-bite injuries may change as social distancing alters the way that children interact with their environments.
CONCLUSION
Our findings support previous reports that pediatric dog-bite injuries occur more frequently in children aged 1–5 years. Most dog-bite injuries in this study were caused by encounters with large dogs, and bites from pit bulls were associated with significantly more severe injury. The anatomical site affected most commonly was the head and neck region. The dog-bite injuries that most frequently require subspecialist surgical intervention are those affecting the head and neck region and those involving extensive soft tissue damage. Low socioeconomic status may increase the risk of dog-bite injury. Pediatric patients with private health insurance were more likely than others to receive surgical intervention for dog-bite injuries.
Supplementary Information
Footnotes
Section Editor: Pierre Borczuk, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
REFERENCES
- 1.American Veterinary Medical Association Task Force on Canine Aggression and Human-Canine Interactions. A community approach to dog bite prevention. J Am Vet Med Assoc. 2001;218(11):1732–49. doi: 10.2460/javma.2001.218.1732. [DOI] [PubMed] [Google Scholar]
- 2.Ozanne-Smith J, Ashby K, Stathakis VZ. Dog bite and injury prevention: analysis, critical review, and research agenda. Inj Prev. 2001;7(4):321–6. doi: 10.1136/ip.7.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Nonfatal dog bite-related injuries treated in hospital emergency departments--United States, 2001. MMWR Morb Mortal Wkly Rep. 2003;52(26):605–10. [PubMed] [Google Scholar]
- 4.Cook JA, Sasor SE, Soleimani T, et al. An epidemiological analysis of pediatric dog bite injuries over a decade. J Surg Res. 2020;246:231–5. doi: 10.1016/j.jss.2019.09.013. [DOI] [PubMed] [Google Scholar]
- 5.McLoughlin RJ, Cournoyer L, Hirsh MP, et al. Hospitalizations for pediatric dog bite injuries in the United States. J Pediatr Surg. 2020;55(7):1228–33. doi: 10.1016/j.jpedsurg.2019.06.025. [DOI] [PubMed] [Google Scholar]
- 6.McGuire C, Morzycki A, Simpson A, et al. Dog bites in children: a descriptive analysis. Plast Surg. 2018;26(4):256–62. doi: 10.1177/2292550318767924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fein J, Bogumil D, Upperman JS, et al. Pediatric dog bites: a population-based profile. Inj Prev. 2019;25(4):290–4. doi: 10.1136/injuryprev-2017-042621. [DOI] [PubMed] [Google Scholar]
- 8.Bykowski MR, Shakir S, Naran S, et al. Pediatric dog bite prevention: Are we barking up the wrong tree or just not barking loud enough? Pediatr Emerg Care. 2019;35(9):618–23. doi: 10.1097/PEC.0000000000001132. [DOI] [PubMed] [Google Scholar]
- 9.Chen HH, Neumeier AT, Davies BW, et al. Analysis of pediatric facial dog bites. Craniomaxillofac Trauma Reconstr. 2013;6(4):225–31. doi: 10.1055/s-0033-1349211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaye AE, Belz JM, Kirschner RE. Pediatric dog bite injuries: a 5-year review of the experience at the Children’s Hospital of Philadelphia. Plast Reconstr Surg. 2009;124(2):551–8. doi: 10.1097/PRS.0b013e3181addad9. [DOI] [PubMed] [Google Scholar]
- 11.Schalamon J, Ainoedhofer H, Singer G, et al. Analysis of dog bites in children who are younger than 17 years. Pediatrics. 2006;117(3):e374–e379. doi: 10.1542/peds.2005-1451. [DOI] [PubMed] [Google Scholar]
- 12.Brogan TV, Bratton SL, Dowd MD, et al. Severe dog bites in children. Pediatrics. 1995;96(5 Pt 1):947–50. [PubMed] [Google Scholar]
- 13.Daniels DM, Ritzi RB, O’Neil J, et al. Analysis of nonfatal dog bites in children. J Trauma. 2009;66(3 Suppl):S17–S22. doi: 10.1097/TA.0b013e3181937925. [DOI] [PubMed] [Google Scholar]
- 14.Gilchrist J, Sacks JJ, White D, et al. Dog bites: still a problem? Inj Prev. 2008;14(5):296–301. doi: 10.1136/ip.2007.016220. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell RB, Nañez G, Wagner JD, et al. Dog bites of the scalp, face, and neck in children. Laryngoscope. 2003;113(3):492–5. doi: 10.1097/00005537-200303000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Ambro BT, Wright RJ, Heffelfinger RN. Management of bite wounds in the head and neck. Facial Plast Surg. 2010;26(6):456–63. doi: 10.1055/s-0030-1267720. [DOI] [PubMed] [Google Scholar]
- 17.Lee CJ, Santos PJF, Vyas RM. Epidemiology, socioeconomic analysis, and specialist involvement in dog bite wounds in adults. J Craniofac Surg. 2019;30(3):753–7. doi: 10.1097/SCS.0000000000005201. [DOI] [PubMed] [Google Scholar]
- 18.United States Census Bureau. “Summary File.” 2012–2016. American Community Survey. 2015. [Accessed December 1, 2019]. Available at: http://ftp2.census.gov/
- 19.OC Animal Care. Orange County City Level Dog Populations: Public Data Request. 2020. [Accessed June 2020]. Available at: https://www.ocpetinfo.com/
- 20.Lamstein A. Choroplethr. Simplify the creation of choropleth maps in R. 2020. [Accessed December 1, 2019]. Available at: https://CRAN.R-project.org/package=choroplethr.
- 21.Plassais J, Kim J, Davis BW, et al. Whole genome sequencing of canids reveals genomic regions under selection and variants influencing morphology. Nat Commun. 2019;10(1):1489. doi: 10.1038/s41467-019-09373-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhu N, Cruz Walma A, Troulis MJ, et al. Facial dog bites treated at the Massachusetts General Hospital over a 20-year period. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;130(2):136–143. doi: 10.1016/j.oooo.2020.02.009. [DOI] [PubMed] [Google Scholar]
- 23.Rezac P, Rezac K, Slama P. Human behavior preceding dog bites to the face. Vet J. 2015;206(3):284–8. doi: 10.1016/j.tvjl.2015.10.021. [DOI] [PubMed] [Google Scholar]
- 24.Davis AL, Schwebel DC, Morrongiello BA, et al. Dog bite risk: an assessment of child temperament and child-dog interactions. Int J Environ Res Public Health. 2012;9(8):3002–13. doi: 10.3390/ijerph9083002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Quinlan KP, Sacks JJ. Hospitalizations for dog bite injuries. JAMA. 1999;281(3):232–3. doi: 10.1001/jama.281.3.232. [DOI] [PubMed] [Google Scholar]
- 26.Vasconez HC, Buseman JL, Cunningham LL. Management of facial soft tissue injuries in children. J Craniofac Surg. 2011;22(4):1320–6. doi: 10.1097/SCS.0b013e31821c9377. [DOI] [PubMed] [Google Scholar]
- 27.Ruiz-Casares M, Nazif-Muñoz J, Iwo R, et al. Nonadult supervision of children in low- and middle-income countries: results from 61 national population-based surveys. Int J Environ Res Public Health. 2018;15(8):1564. doi: 10.3390/ijerph15081564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morrongiello B, Schmidt S, Schell SL. Sibling supervision and young children’s risk of injury: a comparison of mothers’ and older siblings’ reactions to risk taking by a younger child in the family. Soc Sci Med. 2010;71(5):958–65. doi: 10.1016/j.socscimed.2010.05.047. [DOI] [PubMed] [Google Scholar]
- 29.Schnitzer PG, Dowd MD, Kruse RL, et al. Supervision and risk of unintentional injury in young children. Inj Prev. 2015;21(e1):e63–70. doi: 10.1136/injuryprev-2013-041128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shuler CM, DeBess EE, Lapidus JA, et al. Canine and human factors related to dog bite injuries. J Am Vet Med Assoc. 2008;232(4):542–6. doi: 10.2460/javma.232.4.542. [DOI] [PubMed] [Google Scholar]
- 31.Essig GF, Sheehan CC, Niermeyer WL, et al. Treatment of facial dog bite injuries in the emergency department compared to the operating room. OTO Open. 2019;3(3) doi: 10.1177/2473974X19858328. 2473974X1985832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Horswell BB, Chahine CJ. Dog bites of the face, head and neck in children. W V Med J. 2011;107(6):24–7. [PubMed] [Google Scholar]
- 33.Alizadeh K, Shayesteh A, Xu ML. An algorithmic approach to operative management of complex pediatric dog bites: 3-year review of a Level I regional referral pediatric trauma hospital. Plast Reconstr Surg - Glob Open. 2017;5(10):e1431. doi: 10.1097/GOX.0000000000001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Collier S. Breed-specific legislation and the pit bull terrier: Are the laws justified? J Vet Behav. 2006;1(1):17–22. [Google Scholar]
- 35.Position Statement on Breed-Specific Legislation. American Society for the Prevention of Cruelty to Animals; [Accessed August 9, 2020]. Available at: https://www.aspca.org/about-us/aspca-policy-and-position-statements/position-statement-breed-specific-legislation. [Google Scholar]
- 36.Kogan LR, Schoenfeld-Tacher RM, Hellyer PW, et al. Small animal veterinarians’ perceptions, experiences, and views of common dog breeds, dog aggression, and breed-specific laws in the United States. Int J Environ Res Public Health. 2019;16(21):4081. doi: 10.3390/ijerph16214081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Caffrey N, Rock M, Schmidtz O, et al. Insights about the epidemiology of dog bites in a Canadian city using a dog aggression scale and administrative data. Animals (Basel) 2019;9(6):324. doi: 10.3390/ani9060324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arluke A, Cleary D, Patronek G, et al. Defaming Rover: error-based latent rhetoric in the medical literature on dog bites. J Appl Anim Welf Sci. 2018;21(3):211–23. doi: 10.1080/10888705.2017.1387550. [DOI] [PubMed] [Google Scholar]
- 39.Podberscek AL. Dog on a tightrope: The position of the dog in British society as influenced by press reports on dog attacks (1988 to 1992) Anthrozoös. 1994;7(4):232–41. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


