Sir,
Leeches (Hirudinea) are a class of segmented invertebrates that play a useful role in modern plastic surgery, transplant surgery, cardiovascular, and cerebrovascular diseases because of their superb decongestant properties.[1]
Nowadays, in many countries such as Iran, the use of leeches for therapeutic purposes is not uncommon. They are used in different parts of the body, most common on the waist, but using directly on the eye is extremely unusual. We report a case for the first time in literature that used leeches directly on the eyes for leech therapy.
A 50-year-old male presented at ophthalmology clinic of Baqiyatallah Hospital, Tehran, Iran, with complaints of ocular discomfort, pain, redness, burning, and tearing in both eyes. The symptoms began 5 days earlier after he went to a person for leech therapy on his waist, but he accepted to put leeches directly on his eyes for few minutes because of leech therapist's recommendation. In examination, there were severe diffuse superficial and deep conjunctival injection and hyperemia with patchy subconjunctival hemorrhage in both eyes, with a small reddish bulged lesion at bulbar conjunctiva near cornea in right and a dark black-brown one in left eyeFigure 1 seemed most likely to be a dense subconjunctival hematoma after ruling out more important complications such as scleral perforation and uveal prolapse. All other examinations were within normal limits. The patient began to use topical antibiotic and corticosteroid agents, and after 2 weeks, most signs and symptoms were relieved [Figures 2 and 3].
Figure 1.
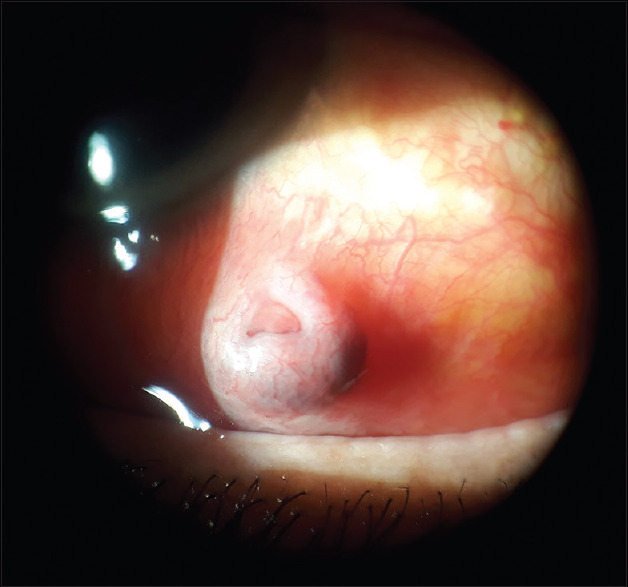
Slit lamp photograph of left eye in 1st visit showing the dark black-brown bulged lesion
Figure 2.
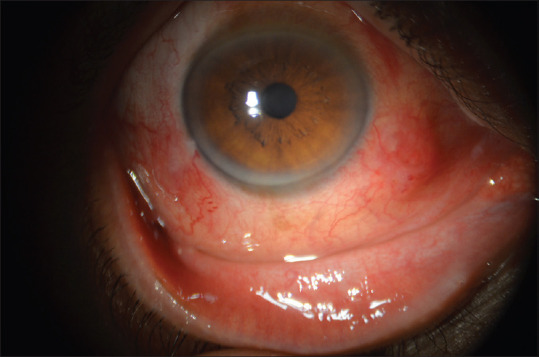
Slit lamp photograph of right eye in 2nd visit after 3 days showing improving signs
Figure 3.
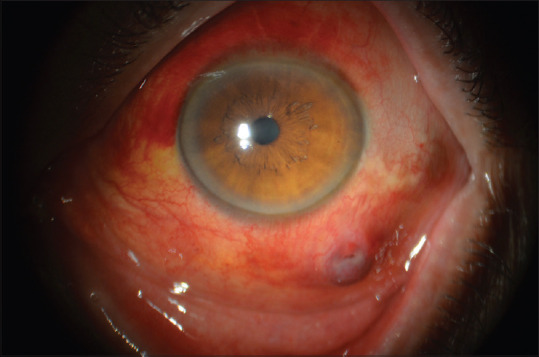
Slit lamp photograph of left eye in 2nd visit after 3 days showing improving signs
Ocular injuries caused by leeches are uncommon. As our knowledge, there are few cases reported as leech-induced ocular injuries in English literature, but all of them caused by accidental leech infestation into the eye and no one was voluntarily as leech therapy. In these cases, leech infestations occurred through different ways, such as swimming or washing face in contaminated water,[1,2,3] flicking moist soil into eye,[4] or attaching a hammock to a tree.[5] In all cases, there were live leeches adhering to the eye when patients presented to the medical centers and symptoms relieved within few days after leeches were removed by doctors through different ways. Subconjunctival hemorrhage is usually seen after leech bite because of the production of a nonenzymatic secretion termed hirudin, which prevents blood from clotting. This does not require specific measures as it disappears with time.[5]
In our case, it is the first time that leech contact was not accidental. Commonly, leech therapy is being done on several parts of the body, but putting them directly on the eyes is so unusual that we never heard about that even as a common citizen and as our knowledge, there is not any publication about using leeches on the eyes for medical purposes. It seems that “Lack of awareness” in our patient caused him to accept leech therapist's recommendation to do that.
In patients like this, differential diagnosis includes uveal prolapse due to scleral perforation, subconjunctival hematoma, pyogenic granuloma, conjunctival nevus, episcleritis, and conjunctivitis that all of them should be considered in examination and treatment.
In conclusion, the eye is not a suitable site for leech therapy because it can cause severe damages and there is no publication in the literature to prove potential benefits of doing that.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors wish to sincerely thank Mr. V. Ghorbanzadeh for his invaluable assistance in the grammatical edition and all personnel at Ophthalmology Clinic of Baqiyatallah hospital for their kindly assistance.
References
- 1.Li WW, Shen T, Jiang J. Ocular leech infestation initially misdiagnosed as conjunctival pigmented nevus. Int J Ophthalmol. 2013;6:557–8. doi: 10.3980/j.issn.2222-3959.2013.04.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shirzadeh E. Red eye due to leech in the eye. Iran J Med Sci. 2005;30:197–8. [Google Scholar]
- 3.Lee YC, Chiu CJ. Ocular leech infestation. Clin Ophthalmol. 2015;9:419–21. doi: 10.2147/OPTH.S79735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Partyka C, Fogg T. Leech on the eye: A novel use for hypertonic saline. Emerg Med Australas. 2009;21:84–5. doi: 10.1111/j.1742-6723.2009.01156.x. [DOI] [PubMed] [Google Scholar]
- 5.Lewis G, Coombes A. Adult ocular leech infestation. Eye. 2006;20:391–2. doi: 10.1038/sj.eye.6701862. [DOI] [PubMed] [Google Scholar]


