Abstract
Objective:
This study evaluated associations among parenting stress, self-efficacy and involvement in relation to spoken language outcomes in young children 3 years following cochlear implantation.
Study Design:
Cross-sectional.
Setting:
Six university tertiary medical centers.
Patients:
164 young children with bilateral, severe-to-profound sensorineural hearing loss who had three years of experience with a CI; children with substantial cognitive impairments were excluded from the study.
Main Outcome Measures(s):
Family Stress Scale (FSS), Scale of Parental Involvement and Self-Efficacy (SPISE), Oral and Written Language Scales (OWLS).
Results:
Correlations were of moderate strength between FSS scores and SPISE scores (Parental Self-Efficacy, r=−0.45, p<0.01, Parental Involvement r=−0.32, p<0.01). As hypothesized, parents reporting higher levels of stress reported lower perceptions of self-efficacy and involvement. In addition, results showed that family stress had a direct, negative effect on spoken language (−4.43 [95% confidence interval: −6.97; −1.89]). After controlling for maternal education and activation age, parental self-efficacy mediated the negative effect between family stress and spoken language (indirect effect = −1.91 [3.45; −0.69]; proportion mediated = 0.43). No mediating effects were found for parental involvement.
Conclusions:
These findings highlight the need for parenting interventions that focus on reducing stressors and increasing parents’ perceptions of self-efficacy in families of children using cochlear implants. Integration of mental health screening and tailored parenting interventions in CI clinics may increase parental self-efficacy and involvement, with measurable benefits in the child’s use of spoken language.
INTRODUCTION
The benefits of pediatric cochlear implantation have been well established. For children with severe-to-profound hearing loss, use of cochlear implants (CIs) has led to increases in their ability to understand and develop spoken communication at levels that would not be obtainable using traditional hearing aids.1–3 Although studies have documented, on average, age-appropriate language skills following cochlear implantation, studies also continue to find CI users lagging behind their peers across a variety of developmental areas.4–6 Earlier research focused primarily on remediation of spoken language skill as a function of audiological and medical history in children with CIs. More recent studies have identified family and parenting predictors of post-implantation success, such as maternal sensitivity, parenting stress, and caregiver involvement.7,8 Most of these studies, however, have measured these variables in isolation, without examining their interrelationships or the potential mechanisms by which they impact spoken language development. The goal of the present study is to examine the relationships of among these variables specifically in families of children using CIs.
Parenting Stress
Parenting stress has been identified as an important factor that contributes to the quality of the parent-child relationship and children’s developmental outcomes. Specifically, higher levels of parenting stress have been linked to poorer social and emotional outcomes, higher rates of behavior problems, and worse quality of life among children with hearing loss.9–12 Importantly, context-specific measures have yielded more consistent results and clinically relevant information than studies employing global or general measures of these constructs.11 For example, inconsistent findings have been reported on general measures of parenting stress, with studies reporting normal to elevated levels of stress in parents. In contrast, consistent elevations in parenting stress have been reported in studies using context-specific measures.11 Context-specific measures assess the unique challenges parents experience in raising a deaf child. These types of measures are more sensitive for identifying parental stressors, and more accurately reflect the interrelationships among parenting factors and child behavior in relation to critical outcomes, such as communication, educational concerns, maintenance of hearing device, and being a language teacher for their child. These concerns are among the top stressors reported by parents of children undergoing CI surgery.11 Similarly, enabling one’s child to function in a hearing world and educating a child with a hearing loss were primary stressors reported in an interview study by parents of children using CIs.13
Consistent with findings for children with normal hearing, language ability has been identified as a strong predictor of parenting stress for parents of children with hearing loss.14–16 Specifically, parents whose children had language delays versus those whose language was within normal limits, reported higher levels of parenting stress, likely due to frustrations experienced by both parents and children when they are unable to communicate with one another. Family income, age at diagnosis, degree of hearing loss, and behavior problems have also been identified as predictors of parenting stress.11,17,18 In a study by Quittner and colleagues,11 language delays influenced parenting stress by way of child behavior problems. These studies have all focused on predictors of parenting stress. No studies to date have investigated the ways in which parenting stress influences other parenting variables, such as self-efficacy and involvement, which directly affect language acquisition in children using CIs. A better understanding of these relationships is needed to appropriately counsel families undergoing CI evaluation or during the post-implantation period.
Parental Involvement and Self-Efficacy
Parental self-efficacy and involvement have been identified as important predictors of children’s language abilities; however, studies have not investigated how parenting stress may affect these relationships. Parental self-efficacy is defined as parents’ perceptions of competence in their parenting role and confidence in their own abilities to perform parenting tasks.19 People with high self-efficacy believe they have adequate knowledge and understanding to persist in a given task until success is achieved. In the hearing literature, higher parental self-efficacy is linked to more positive parent-child interactions and better maternal mental health.,20,21 DesJardin and colleagues were the first to examine parental self-efficacy in children with hearing loss, including both children using hearing aids and cochlear implants22–25 and developed the Scale of Parental Involvement and Self-Efficacy (SPISE).22 DesJardin and colleagues found that parents’ self-efficacy was positively related to the frequency with which parents engaged in activities to support their child’s speech and language development at home.22 In addition, parent-reported self-efficacy and involvement using the SPISE at 12 months old was positively related to children’s receptive and expressive language skills at 36 months old. Overall, although these studies have shown that parental self-efficacy is greater for parents of children using CIs compared to hearing aids, they continue to indicate that more coaching is needed on topics, such as use of hearing devices and creating an optimal listening and language environment.25
Parental involvement is also a well-established predictor of spoken language outcomes, cognition, pre-reading skills, and future educational success.16, 26–28 Parental involvement is typically defined as a parent’s ability to follow through with intervention recommendations including attending appointments, their confidence in working with their child, and engagement in early intervention or school. These studies have also highlighted that parental involvement, and variables such as maternal sensitivity, are as predictive of spoken language scores four years post-implantation as age at implantation.8 More importantly, high-quality parent-child interactions may compensate for the speech processing deficit that some CI users experience, as well as accelerate language development.29 Thus, a body of literature has consistently found that parents are key members of the treatment team for pediatric CI recipients.
This study uses data from the largest, longitudinal, nationally representative study of pediatric CI users, the Childhood Development after Cochlear Implantation (CDaCI) study,30–32 to examine relationships among parent measures of stress, self-efficacy and involvement and their effects on spoken language development. Our major aim is to evaluate possible mechanisms through which parenting stress influences language outcomes in children using CIs. We hypothesized that the well-established link between parenting stress and language outcomes can be partially explained by parental involvement and self-efficacy. Thus, we tested a mediation model, predicting a direct negative effect of parenting stress on both self-efficacy and involvement, which in turn, would be associated with worse language outcomes. A better understanding of how parenting stress influences language will enable multidisciplinary CI teams to improve their outcomes by providing targeted parent coaching or parenting interventions.
MATERIALS & METHODS
Participants
The current investigation was a part of the prospective, longitudinal, multicenter national study of the effectiveness of pediatric cochlear implantation (CDaCI Study).30 From 2002–2004, 188 children ages 5 years or younger with bilateral, severe-to-profound sensorineural hearing loss who were CI candidates were recruited from six CI centers across the United States. To be included in the CDaCI Study, the family had to commit to educate the child in English speaking schools. Children with significant cognitive impairments on a cognitive screener, using the Bayley Scales of Infant Development (BSID II) Psychomotor Development Index33 or Leiter International Performance Scale – Revised,34 were excluded from participating. The CDaCI Study also enrolled 97 normal hearing children, who are not included in this study. The cohort was followed for 13 years, with data collected across three waves. Here, we utilized data from the first wave of data collection.
Procedures
Prior to CI surgery, families provided informed consent for the research study and participated in a variety of baseline assessments over two half-day sessions. Parents provided information on demographics, family characteristics, child medical history, and communication. Parents also completed measures of child behavior, parenting stress, self-efficacy, and involvement. Children completed audiological evaluations and speech and language testing. For more details on study assessments, refer to Fink et al., 2010.30 After the child was implanted, follow-up evaluations were completed annually. This study was approved by an Institutional Review Board at each participating CI center.
Data for the current investigation were drawn from the 3-year post-implantation visit, which was the final assessment from the first wave of the CDaCI study. This follow-up period allowed for variability in language performance to emerge, with fewer children performing at the floor on language tests. The baseline language data was not included, as the majority of children were younger than 3 years of age at baseline (111 of the 164 (68%) participants) and unable to complete the OWLS language assessment. There was only a small sample of children who were of age and had the language skills to complete the OWLS, resulting in little variability in the baseline language performance to meaningfully contribute to the analyses. The 3-year follow-up visit was also sufficiently distant from the highly stressful period of initial diagnosis and decisions surrounding implantation. The period surrounding diagnosis with hearing loss and making the decision for the child to undergo CI surgery is a highly stressful period and not necessarily reflective of the stress, self-efficacy, and involvement seen in the months and years following implantation. After 3 years of CI experience, including rehabilitation, parents and children had enough time to adjust to the CI, which facilitated our aim to examine relationships among stress, parental self-efficacy, involvement and language performance.
Measures
Family Stress Scale (FSS).
The FSS is a 16-item context-specific measure of parenting stress for caregivers of children with hearing loss. This measure assesses both general family stressors (e.g., finances, discipline) and stressors specific to childhood deafness (e.g., communication, managing hearing aids/CIs). Using a 5-point scale, parents rated each item from “not at all stressful” to “extremely stressful” and scores were averaged across all items, with higher scores indicating more stress. The FSS has been used in several CI studies with strong reliability and validity.11,12,35,36
Scale of Parental Involvement and Self-Efficacy (SPISE)27,22.
The SPISE assesses parental self-efficacy and involvement using parent ratings on a 7-point Likert scale. The parental self-efficacy items ask parents to rate their knowledge of caring for their child’s sensory device, beliefs they can make a difference in their child’s speech and language development, and knowledge and competence to develop their child’s speech and language skills. Self-efficacy ratings range from 1=“not at all” to 7=“very much,” with higher scores indicating greater self-efficacy. The parental involvement section includes questions about parents’ perceptions of difficulty working with the child’s device (1=“very easy” to 7=“very hard,” reverse-scored), their level of involvement (e.g., 1=“never” to 7=“always”) and perceptions of comfort participating in their child’s device use and early intervention services (1=“not comfortable at all” to 7=“very comfortable”). Ratings for items within each scale were averaged to create Parental Self-Efficacy and Parental Involvement scores, respectively.
Oral and Written Language Scales (OWLS)37.
The OWLS is a well-established language measure for children ages 3 to 21 years old. It consists of Listening Comprehension and Oral Expression scales and has been used with children who are deaf and hard of hearing.38–41 Children’s scores can be compared with normative data to produce a standard score (SS), with a mean of 100 and a standard deviation (SD) of 15 points. The OWLS Oral Composite SS, comprising of the two subscales, was used as a measure of spoken language for analyses reported in this study.
Statistical Analyses
Pairwise correlations were examined between key pre-implant child and family characteristics and 3-year data. We tested two mediation models, one with parental self-efficacy as the mediator between parenting stress and spoken language, and one with parental involvement as the mediator. The indirect effect was estimated using the product of coefficients method with bootstrapped confidence intervals42 using the Stata IC 15.1 (StataCorp, College Station, TX) ‘sgmediation’ program. Maternal education and age at CI activation were included as covariates in all regression models. For all analyses, oral language was centered on the sample mean and family stress, parental self-efficacy, and parental involvement were standardized prior to analysis using their own sample mean and standard deviation.
RESULTS
Participants who dropped out of the study prior to the 3-year follow-up visit (n=9) were excluded from the analyses. Of the 179 participants remaining at the 3-year visit, 164 (91.6%) completed all of the measures under investigation. Table 1 presents descriptive statistics for the key baseline (pre-CI) child and family characteristics, as well as the 3-year post-CI data of interest. The sample included children with early onset hearing loss (mean age 2.7 months) who had average IQ scores (mean standard score=99.0) and were implanted between 6 and 64 months of age (mean=28.8 months). Participants were equally distributed in terms of gender (51.2% female) and lived with parents who were largely college educated (50.6% of mothers graduated from college). At 3 years post-implantation, children still demonstrated significant oral language delays, with 73.8% evidencing standard scores below 85.
Table 1.
Baseline child and family characteristics and 3-year post-implant outcomes.
| Characteristic | Participants N=164 |
|---|---|
| Baseline | |
| CI activation age, years [range] | 2.4 (1.2) [0.6–5.3] |
| Onset age of hearing loss, months [range] | 2.7 (7.3) [0–44] |
| No. missing | 8 |
| Aided PTA better eara, dB | 74.8 (23.0) |
| Unaided PTA better eara, dB | 105.3 (16.3) |
| No. missing | 8 |
| Baseline IQb | 99.0 (18.9) |
| No. missing | 3 |
| Gender, n (%) | |
| Male | 80 (48.8) |
| Female | 84 (51.2) |
| Maternal education, n (%) | |
| Did not complete high school | 9 (5.5) |
| High school graduate or some college | 72 (43.9) |
| College graduate or higher | 83 (50.6) |
| 3-Year Follow-Up | |
| Age at 3-year follow-up visit, years | 5.4 (1.2) |
| Participants with bilateral CIs, n (%) | 36 (22.0) |
| Inter-implant interval from 1st to 2nd CI, yearsc | 1.5 (0.9) |
| Family Stress Scale score | 1.8 (0.6) |
| Parental Self-Efficacy score on SPISE | 6.2 (0.7) |
| Parental Involvement score on SPISE | 6.2 (0.7) |
| Language standard scored | 72.6 (19.2) |
| Language classification, n (%) | |
| Below normal (SS<85) | 121 (73.8) |
| Normal (SS 85–115) | 41 (25.0) |
| Above normal (SS>115) | 2 (1.2) |
Data are expressed as mean (SD) unless otherwise noted. Abbreviations: CI, cochlear implant; PTA, pure tone average; IQ, intelligence quotient; SS, standard score
Average of available thresholds for tested frequencies 500, 1000, 2000, and 4000 Hz, where at least 1 frequency was tested.
Baseline cognition assessed using Bayley Scales of Infant Development (BSID-II) Psychomotor Development Index (PDI) or Leiter International Performance Scale – Revised, depending on participant’s age.
Among participants who had received bilateral implants by the 3-year follow-up visit.
Oral and Written Language Scales (OWLS) Listening Comprehension and Oral Expression Oral Composite standard score.
The top stressors reported by parents of children using CIs were finances, educational concerns, discipline, safety, and communication (see Table 2). Overall, parents reported less self-efficacy pertaining to their ability to do speech/language activities with their child on a daily basis and knowledge on how to help their child develop sounds or words (Table 3). Parents also reported less involvement in terms of their participation in home visits or therapy, engagement in listening or language activities, and checking their child’s hearing device daily (see Table 3).
Table 2.
Context-specific stressors for parents of deaf children with cochlear implants.
| Rank | Family Stress Scale (FSS) Stressor | Mean Rating (SD) |
|---|---|---|
| 1 | Finances | 2.36 (1.26) |
| 2 | Educational concerns | 2.35 (1.14) |
| 3 | Discipline | 2.10 (0.92) |
| 4 | Safety | 2.07 (1.14) |
| 5 | Communication | 1.92 (0.95) |
| 6 | Behavioral problems | 1.86 (0.96) |
| 7 | Outings in the community | 1.79 (0.94) |
| 8 | Following routines | 1.74 (0.88) |
| 9 | Having to be a language teacher for your child | 1.72 (0.93) |
| 10 | Medical/audiological care | 1.67 (0.94) |
| 11 | Marital relationship | 1.65 (0.98) |
| 12 | Relationship with other children | 1.63 (0.77) |
| 13 | Other people’s curiosity or lack of understanding about child’s deafness | 1.59 (0.83) |
| 14 | Keeping the hearing aids/cochlear implants on and working | 1.51 (0.82) |
| 15 | Relationships with parents or extended family | 1.40 (0.79) |
| 16 | Understanding how to operate hearing aids/cochlear implants | 1.27 (0.56) |
Note: Stressors are rank ordered based on means, with higher stress scores being reported first.
Table 3.
Means for items on the SPISE for parents of deaf children with cochlear implants.
| Rank | SPISE Item | Mean Rating (SD) |
|---|---|---|
| Parental Self-Efficacy | ||
| How much do you feel that you… | ||
| 1 | know about and are able to do speech/language activities/ strategies with your child at home on a daily basis? | 5.78 (1.17) |
| 2 | know how to help your child develop sound? | 6.13 (1.06) |
| 3 | know how to help your child develop words? | 6.14 (1.04) |
| 4 | can positively affect your child’s speech development? | 6.18 (1.13) |
| 5 | can positively affect your child’s language development? | 6.26 (1.07) |
| 6 | can positively affect your child’s listening development? | 6.29 (1.03) |
| 7 | know about and are able to adjust the settings of your child’s HA (volume) or CI (programs) on a daily basis? | 6.31 (1.12) |
| 8 | know about and are able to check your child’s listening skills using the 6 Ling sounds (a oo, ee, s, sh, m) on a daily basis? | 6.35 (1.20) |
| 9 | can positively affect your child’s overall early development? | 6.38 (0.91) |
| 10 | know about and are able to check and put on your child’s HA or CI on a daily basis? | 6.65 (0.75) |
| Parental Involvement | ||
| 1 | How much are you invited to participate in the home visits/ therapy with your child?a | 5.68 (2.05) |
| 2 | How much does the teacher or speech/language therapist show you listening/language activities? | 5.82 (1.56) |
| 3 | How hard is it for you to check and listen to your child’s HA/CI everyday? (battery, ear molds, cords, microphone, settings, etc.) [R*] | 5.88 (1.49) |
| 4 | How comfortable do you feel in helping to develop your child’s IFSP or IEP? | 6.03 (1.21) |
| 5 | How much do you feel that the deaf/heard of hearing teacher includes you in the planning of your child’s IFSP or IEP?b | 6.09 (1.30) |
| 6 | How hard is it for you to check your child’s listening skills using the 6 Ling sounds (a, oo, ee, s, sh, m) everyday? [R*] | 6.09 (1.40) |
| 7 | How much are you comfortable doing the listening/ language activities with your child when the teacher/ therapist is not there? | 6.28 (1.04) |
| 8 | How much are you comfortable participating in the home visits/therapy with your child?a | 6.38 (1.29) |
| 9 | How hard is it for you to put on your child’s HA/CI everyday? [R*] | 6.61 (1.05) |
| 10 | How many days per week will your child wear his/her HA/CI? | 6.72 (1.18) |
| 11 | How many hours per day will your child wear his/her HA/CI? | 6.99 (0.16) |
Abbreviations: SPISE, Scale of Parental Involvement and Self-Efficacy; HA, hearing aid(s); CI, cochlear implant(s); [R*], reverse scored; IFSP, Individualized Family Service Plan; IEP, Individualized Education Plan.
Note:
16 participants did not respond to this item;
8 participants did not respond to this item. All other items on the Parental Involvement scale and the Parental Self-Efficacy scale were missing 5 or fewer responses. Scores on individual items of the SPISE are presented in order from most problematic area to least. Lower scores indicate less self-efficacy and/or involvement.
Pairwise correlations between key pre-CI and 3-year post-CI data are presented in Table 4. Correlations were of moderate strength between FSS scores and both SPISE composites of Parental Self-Efficacy (r=−0.45, p<0.01) and Parental Involvement (r=−0.32, p<0.01) scores. As hypothesized, parents reporting higher levels of stress reported lower perceptions of self-efficacy and involvement. The two SPISE scores were moderately, positively correlated (r = 0.56, p<.05) without any evidence of multicollinearity. Moderate associations were also found between language scores and the key baseline variables of CI activation age (r=−0.36, p<0.01) and maternal education (r=0.39, p<0.01), demonstrating that better spoken language was associated with younger activation age and higher maternal education.
Table 4.
Pairwise correlations between key pre-implant characteristics and 3-year post-implant outcomes.
| Correlations | Baseline | 3 Years Post-CI | |||||
|---|---|---|---|---|---|---|---|
| Activation Age | Maternal Education | Language Standard Scorea | Parental Self-Efficacy | Parental Involvement | FSS Score | ||
| Baseline | Activation Age | ||||||
| Maternal Education | −0.20 | ||||||
| 3 Years Post-CI | Language Standard Scorea | −0.36* | 0.39* | ||||
| Parental Self-Efficacy | −0.07 | 0.24* | 0.36* | ||||
| Parental Involvement | −0.22 | 0.05 | 0.25* | 0.56* | |||
| FSS Score | 0.01 | 0.06 | −0.21 | −0.45* | −0.32* | ||
Abbreviations: CI, cochlear implant; FSS, Family Stress Scale;
p<0.05.
Oral and Written Language Scales (OWLS) Listening Comprehension and Oral Expression Oral Composite standard score.
Results of the mediation models are reported in Figure 1. Results showed that family stress had a direct, negative effect on spoken language (−4.43 [95% confidence interval: −6.97; −1.89]). In addition, Parental Self-Efficacy mediated the negative effect between family stress and spoken language (indirect effect = −1.91 [3.45; −0.69]; proportion mediated = 0.43), after controlling for maternal education and activation age. Thus, family stress was associated with worse perceptions of parental self-efficacy, which in turn were associated with worse spoken language scores. In contrast, there was limited evidence supporting Parental Involvement as a mediator of the direct effect between family stress and language outcomes.
Figure 1. Mediation models between family stress and spoken language with parental self-efficacy and parental involvement.
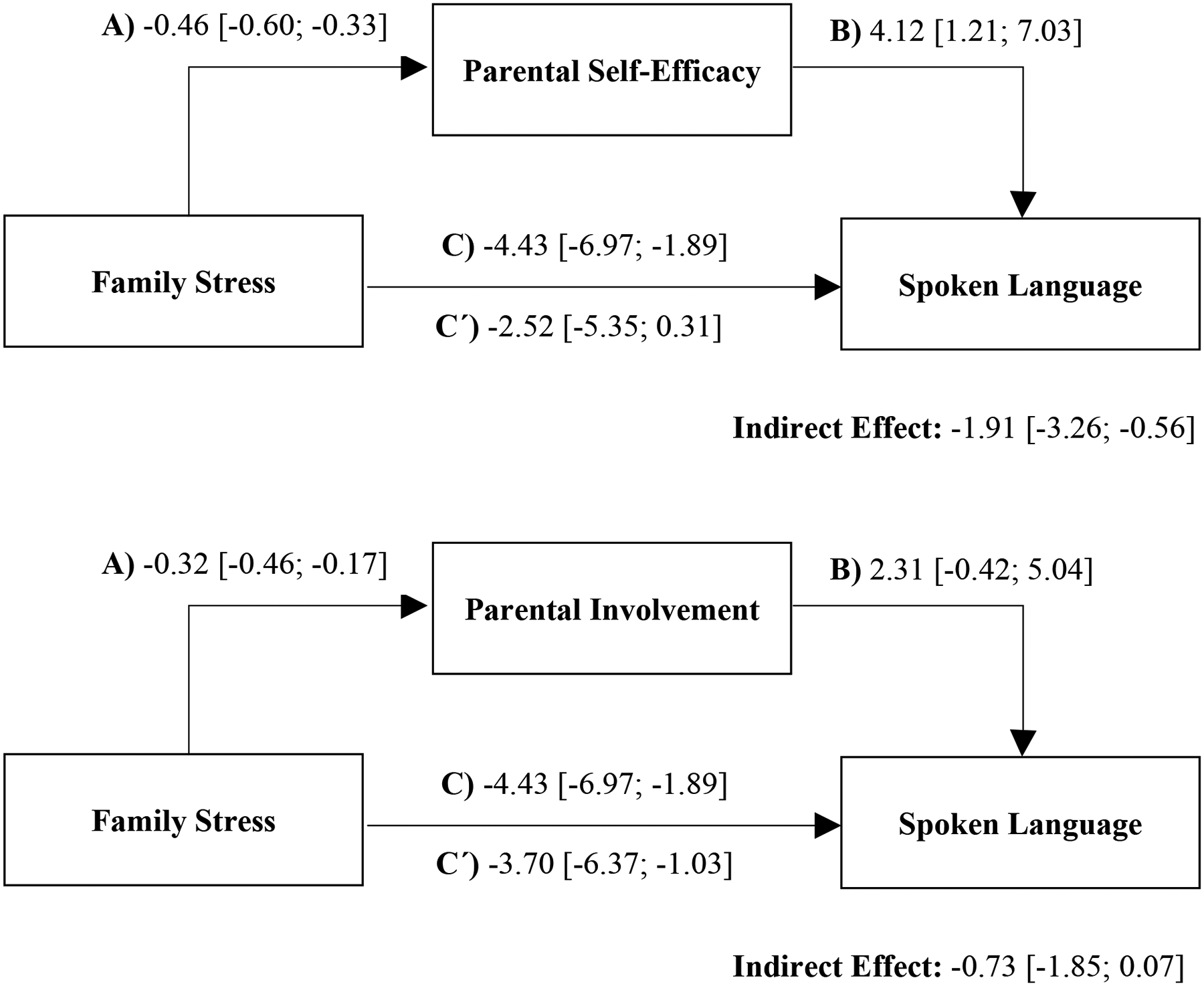
Note: Models showing the relationship between family stress (independent variable) and spoken language (dependent variable), with parental self-efficacy [top] and parental involvement [bottom] as a mediator, after 3 years of cochlear implant experience. Parameter estimates and 95% confidence intervals are shown for A) the effect of Family Stress on the mediator, B) the effect of the mediator on spoken language, C) the total effect of Family Stress on spoken language, and Ć) the direct effect of Family Stress on spoken language. Spoken language was centered at the mean of the sample (72.60), and Family Stress, Parental Self-Efficacy, and Parental Involvement were standardized prior to analysis. All analyses accounted for maternal education and age of CI activation.
DISCUSSION
The current study examined relationships among parent measures of stress, self-efficacy, and involvement, and their effects on spoken language development. Our primary aim was to identify the possible mechanisms through which parenting stress affects spoken language outcomes in children with CIs. As expected, the majority of children in the CDaCI cohort exhibited language scores below average after 3 years of implantation. This is consistent with prior studies reporting that, although CIs are effective in improving auditory access and language development for children with severe-to-profound hearing loss, many children continue to perform below age expectations.1,43 Thus, our study sought to identify parenting factors that could potentially improve outcomes in children with CIs. Specifically, we found evidence that parental self-efficacy mediates the relationship between parenting stress and language outcomes. Parents of children using CIs reporting higher levels of stress in their parenting role also reported worse perceptions of self-efficacy, which, in turn, were related to worse spoken language scores three years after implantation. In contrast, parental involvement did not mediate the relationship between stress and language outcomes.
Prior studies have examined these parenting variables in isolation, but none have examined the interrelationships or processes underlying these key parenting variables (stress, involvement, and self-efficacy) specifically in a CI population. Our data showed that parents continue to report context-specific stress related to parenting a child with CIs. At 3 years post-implantation, three of the top five stressors reflected concerns relevant to children using CIs (e.g., educational concerns, safety, communication). Theses stressors are also among the top 5 stressors reported by families prior to implantation.11 Consistent with previous literature,15,44 parenting stress was negatively associated with oral language (i.e., 4.43 oral language SS units per SD change in family stress), with these new data indicating that part of this effect is explained by the negative impact of parenting stress on self-efficacy. Although the simple, negative correlations between parenting stress and involvement were also significant, level of involvement did not mediate children’s spoken language outcomes. These findings highlight the need for interventions that reduce stressors related to raising a child with a CI and increase parental perceptions of self-efficacy, suggesting that this might have concomitant, positive effects on oral language.
Parental self-efficacy was the stronger of the two proposed mediators, accounting for 43% of the relationship between parenting stress and spoken language scores. This association between parental self-efficacy and language outcomes, after accounting for maternal education and activation age, is consistent with prior studies that demonstrated relationships between perceived parent confidence and children’s spoken language.24,25,45 These results also show that even after 3 years of implantation, parents’ knowledge and confidence related to their child’s hearing loss is variable, with implications for children’s oral language outcomes. Notably, families of CI children may have high knowledge due to many hours in clinic appointments, but may struggle to implement that knowledge in day-to-day interactions with their child. CI clinics should find better ways of evaluating parents’ strengths and needs related to their child’s auditory access and language development. By incorporating a screening measure, like the SPISE, early interventionists and hearing health providers can identify critical targets for parenting interventions.
Parental involvement was only weakly associated with oral language (r=0.25) and did not significantly mediate the relationship between parenting stress and language scores, accounting for 17% of the variance. This finding was contrary to our hypotheses and previous literature which has consistently reported a strong link between parental involvement and spoken language.15,28,29 One possible explanation for this result may lie with the self-report nature of the SPISE. Although this instrument is an easy and feasible way to assess parental involvement, it does not fully capture key indicators of parental involvement. For example, it is not clear how respondents are interpreting “involvement” on the SPISE. Questions are not squarely focused on the amount of involvement the parent has in facilitating the child’s CI use; some questions ask how often the parent is invited to therapy sessions or how much the school involves them in the IEP process. In these examples, parents do not have control over their level of involvement and thus, the scores may not reflect parental choices to be more highly involved. Further, the SPISE also lacks items measuring important features of involvement that have been shown to predict language development, such as active engagement or scaffolding of child language during play.46,47 Prior studies, using observational methods to examine parent involvement, have reported that parental sensitivity, including positive regard, respect for child’s autonomy, and stimulation are predictive of post-implantation language scores.8 In those studies, strong positive effects for involvement on spoken language outcomes are clear. Thus, the SPISE may not fully capture active engagement and/or participation of parents in their child’s interventions.
Limitations & Future Directions
This study is among the first to examine relationships among parenting stress, parental self-efficacy, involvement, and spoken language in families that have a child with a CI. Although our hypotheses and analyses were directional, the data were cross-sectional, significantly limiting causal interpretation. These cross-sectional analyses limited the ability to capture these constructs over time, which may be important in developing future interventions. In addition, this study used condition-specific measures that assessed parenting stress, self-efficacy, and involvement specifically for parents of children using CIs, which did not allow for comparisons with a control group of families of children with normal hearing. All analyses accounted for prominent third variable confounders, including age at implantation and maternal education as covariates, yet other unmeasured confounders may be present. Although maternal education was accounted for in the analyses, it should be noted that over 50% of the participants had mothers who were college educated; thus, it may affect the generalizability of the results. Directionality will need to be confirmed in future work by accounting for additional confounders and/or using longitudinal modeling. Indeed, there may be a dynamic interaction over time between language delay and parenting stress. Another potential limitation is the use of the SPISE, which does not appear to fully capture parental involvement. Future studies should utilize both observational and self-report measures to ensure consistency between parent report and provider observations during “live” sessions. Future research should also use the SPISE-R,25 which is an updated version of the SPISE that adds items that measure parents’ beliefs, knowledge, confidence, and actions. Lastly, this study focused on parents of children using CIs. Future research should be conducted with families of children with varying degrees of hearing loss to determine the generalizability and applicability of these findings to children using other hearing devices, such as hearing aids.
Conclusion
Overall, this study highlights parents’ key role in facilitating their child’s CI success. It is critical that implant centers identify and support parents who are experiencing stress or a lack of confidence related to their child’s hearing journey. CI clinicians should ensure that support systems are in place not only for the child, but also for the family. Integration of mental health and tailored parenting interventions in CI clinics may increase parental self-efficacy and involvement, with measurable benefits in the child’s use of spoken language.
Acknowledgement:
We would like to thank the children and families who participated in this study and made this work possible.
Conflicts of Interest and Source of Funding:
Dr. Cejas is on the Board of Directors for AG Bell. She has research agreements with MED-EL. All other authors have no conflicts of interest to disclose. This work was funded by a grant from the National Institute on Deafness and Other Communication Disorders (NIDCD award R01DC004797).
Footnotes
This paper is subject to the NIH Public Access Policy.
REFERENCES
- 1.Niparko JK, Tobey EA, Thal DJ, et al. Spoken language development in children following cochlear implantation. Jama. 2010;303(15):1498–1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li G, Zhao F, Tao Y, Zhang L, Yao X, Zheng Y. Trajectory of auditory and language development in the early stages of pre-lingual children post cochlear implantation: A longitudinal follow up study. Int. J. Pediatr. Otorhinolaryngol 2020;128:109720. [DOI] [PubMed] [Google Scholar]
- 3.Wie OB, Torkildsen JVK, Schauber S, Busch T, Litovsky R. Long-Term Language Development in Children With Early Simultaneous Bilateral Cochlear Implants. Ear Hear. 2020;41(5):1294–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi JE, Hong SH, Moon IJ. Academic Performance, Communication, and Psychosocial Development of Prelingual Deaf Children with Cochlear Implants in Mainstream Schools. J Audiol Otol. 2020;24(2):61–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Giacomo A, Craig F, D’Elia A, Giagnotti F, Matera E, Quaranta N. Children with cochlear implants: cognitive skills, adaptive behaviors, social and emotional skills. Int. J. Pediatr. Otorhinolaryngol 2013;77(12):1975–1979. [DOI] [PubMed] [Google Scholar]
- 6.Saki N, Bayat A, Moniri S, Moogahi NK. The influence of cochlear implantation on aggression behaviors in children. Int. J. Pediatr. Otorhinolaryngol 2019;127:109669. [DOI] [PubMed] [Google Scholar]
- 7.Kirk KI, Miyamoto RT, Ying EA, Perdew AE, Zuganelis H. Cochlear Implantation in Young Children: Effects of Age at Implantation and Communication Mode. Volta Rev. 2000;102(4):127. [Google Scholar]
- 8.Quittner AL, Cruz I, Barker DH, et al. Effects of maternal sensitivity and cognitive and linguistic stimulation on cochlear implant users’ language development over four years. J Pediatr. 2013;162(2):343–348.e343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crnic K, Low C. Everyday stresses and parenting. In: Handbook of parenting: Practical issues in parenting, Vol. 5, 2nd ed. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers; 2002:243–267. [Google Scholar]
- 10.Lederberg AR, Everhart VS. Conversations between deaf children and their hearing mothers: pragmatic and dialogic characteristics. J Deaf Stud Deaf Educ. 2000;5(4):303–322. [DOI] [PubMed] [Google Scholar]
- 11.Quittner AL, Barker DH, Cruz I, et al. Parenting Stress among Parents of Deaf and Hearing Children: Associations with Language Delays and Behavior Problems. Parent Sci Pract. 2010;10(2):136–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meserole RL, Carson CM, Riley AW, et al. Assessment of health-related quality of life 6 years after childhood cochlear implantation. Qual Life Res. 2014;23(2):719–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sach TH, Whynes DK. Paediatric cochlear implantation: the views of parents. Int. J. Audiol 2005;44(7):400–407. [DOI] [PubMed] [Google Scholar]
- 14.Gallagher TM. Interrelationships among children’s language, behavior, and emotional problems. Top Lang Disord. 1999;19(2):1–15. [Google Scholar]
- 15.Sarant J, Garrard P. Parenting stress in parents of children with cochlear implants: relationships among parent stress, child language, and unilateral versus bilateral implants. J Deaf Stud Deaf Educ. 2014;19(1):85–106. [DOI] [PubMed] [Google Scholar]
- 16.Markman TM, Quittner AL, Eisenberg LS, et al. Language development after cochlear implantation: an epigenetic model. J. Neurodev. Disord 2011;3(4):388–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pipp-Siegel S, Sedey AL, Yoshinaga-Itano C. Predictors of parental stress in mothers of young children with hearing loss. J Deaf Stud Deaf Educ. 2002;7(1):1–17. [DOI] [PubMed] [Google Scholar]
- 18.Meadow-Orlans KP. Stress, support, and deafness: Perceptions of infants’ mothers and fathers. J. Early Interv 1994;18(1):91–102. [Google Scholar]
- 19.Bandura A Regulation of cognitive processes through perceived self-efficacy. Dev. Psychol 1989;25(5):729–735. [Google Scholar]
- 20.Conrad B, Gross D, Fogg L, Ruchala P. Maternal confidence, knowledge, and quality of mother–toddler interactions: A preliminary study. Infant Ment. Health J 1992;13(4):353–362. [Google Scholar]
- 21.Teti DM, Gelfand DM. Behavioral competence among mothers of infants in the first year: the mediational role of maternal self-efficacy. Child Dev. 1991;62(5):918–929. [DOI] [PubMed] [Google Scholar]
- 22.Desjardin JL. Assessing Parental Perceptions of Self-Efficacy and Involvement in Families of Young Children with Hearing Loss. Volta Rev. 2003;103(4):391–409. [Google Scholar]
- 23.Desjardin JL. Maternal Perceptions of Self-Efficacy and Involvement in the Auditory Development of Young Children with Prelingual Deafness. J. Early Interv 2005;27(3):193–209. [Google Scholar]
- 24.DesJardin JL, Eisenberg LS. Maternal contributions: supporting language development in young children with cochlear implants. Ear Hear. 2007;28(4):456–469. [DOI] [PubMed] [Google Scholar]
- 25.Ambrose SE, Appenzeller M, DesJardin JL. Evaluating Self-Efficacy in Parents of Children with Hearing Loss. Hear J. 2020;73(9):35,36. [PMC free article] [PubMed] [Google Scholar]
- 26.Calderon R Parental Involvement in Deaf Children’s Education Programs as a Predictor of Child’s Language, Early Reading, and Social-Emotional Development. J Deaf Stud Deaf Educ. 2000;5(2):140–155. [DOI] [PubMed] [Google Scholar]
- 27.Calderon R, Naidu S. Further support for the benefits of early identification and intervention for children with hearing loss. Volta Rev. 1999;100(5):53–84. [Google Scholar]
- 28.Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106(3):E43. [DOI] [PubMed] [Google Scholar]
- 29.Moreno-Torres I, Madrid-Cánovas S, Blanco-Montañez G. Sensitive periods and language in cochlear implant users. J. Child Lang 2016;43(3):479–504. [DOI] [PubMed] [Google Scholar]
- 30.Fink NE, Wang NY, Visaya J, et al. Childhood Development after Cochlear Implantation (CDaCI) study: design and baseline characteristics. Cochlear Implants Int. 2007;8(2):92–116. [DOI] [PubMed] [Google Scholar]
- 31.Wang N-Y, Carson CM, Niparko JK, Team CD. Representativeness in studies of early cochlear implantation. Am Ann Deaf. 2012;157(3):249–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Holzinger D, Dall M, Sanduvete-Chaves S, Saldaña D, Chacón-Moscoso S, Fellinger J. The Impact of Family Environment on Language Development of Children With Cochlear Implants: A Systematic Review and Meta-Analysis. Ear Hear. 2020;41(5):1077–1091. [DOI] [PubMed] [Google Scholar]
- 33.Bayley N Bayley Scales of Infant Development (2nd ed.). 1993. [Google Scholar]
- 34.Roid GH, Miller LJ. Leiter international performance scale-revised (Leiter-R).
- 35.Plotkin RM, Brice PJ, Reesman JH. It Is Not Just Stress: Parent Personality in Raising a Deaf Child. J Deaf Stud Deaf Educ. 2013;19(3):347–357. [DOI] [PubMed] [Google Scholar]
- 36.Cejas I, Hoffman MF, Quittner AL. Outcomes and benefits of pediatric cochlear implantation in children with additional disabilities: a review and report of family influences on outcomes. Pediatric Health Med Ther. 2015;6:45–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carrow-Woolfolk E. Oral and written language scales. Vol 93: Circle Pines, MN: American Guidance Service; 1995. [Google Scholar]
- 38.DesJardin JL, Ambrose SE, Eisenberg LS. Literacy Skills in Children With Cochlear Implants: The Importance of Early Oral Language and Joint Storybook Reading. J Deaf Stud Deaf Educ. 2009;14(1):22–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Luckner JL, Bowen S. Assessment Practices of Professionals Serving Students Who Are Deaf or Hard of Hearing An Initial Investigation. Am Ann Deaf. 2006;151(4):410–417. [DOI] [PubMed] [Google Scholar]
- 40.Luetke-Stahlman B, Nielsen DC. The Contribution of Phonological Awareness and Receptive and Expressive English to the Reading Ability of Deaf Students with Varying Degrees of Exposure to Accurate English. J Deaf Stud Deaf Educ. 2003;8(4):464–484. [DOI] [PubMed] [Google Scholar]
- 41.Nielsen DC, Luetke-Stahlman B. Phonological awareness: One key to the reading proficiency of deaf children. Am Ann Deaf. 2002;147(3):11–19. [DOI] [PubMed] [Google Scholar]
- 42.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods 2004;36(4):717–731. [DOI] [PubMed] [Google Scholar]
- 43.Jorgensen LE, Benson EA, McCreery RW. Conventional Amplification for Children and Adults with Severe-to-Profound Hearing Loss. Semin Hear. 2018;39(4):364–376. doi: 10.1055/s-0038-1670699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Majorano M, Guerzoni L, Cuda D, Morelli M. Mothers’ emotional experiences related to their child’s diagnosis of deafness and cochlear implant surgery: Parenting stress and child’s language development. Int J Pediatr Otorhinolaryngol. 2020;130:109812. [DOI] [PubMed] [Google Scholar]
- 45.Stika CJ, Eisenberg LS, Johnson KC, et al. Developmental outcomes of early-identified children who are hard of hearing at 12 to 18 months of age. Early Hum Dev. 2015;91(1):47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Landry SH, Miller-Loncar CL, Smith KE, Swank PR. The role of early parenting in children’s development of executive processes. Dev Neuropsychol. 2002;21(1):15–41. [DOI] [PubMed] [Google Scholar]
- 47.Kwon K-A, Bingham G, Lewsader J, Jeon H-J, Elicker J. Structured Task Versus Free Play: The Influence of Social Context on Parenting Quality, Toddlers’ Engagement with Parents and Play Behaviors, and Parent–Toddler Language Use. Child & Youth Care Forum. 2013;42(3):207–224. [Google Scholar]


